Abstract
Introduction
The ability to track improvement against racial/ethnic disparities in mental health care is hindered by the varying methods and disparity definitions used in previous research.
Data
Nationally representative sample of whites, blacks, and Latinos from the 2002 to 2006 Medical Expenditure Panel Survey. Dependent variables are total, outpatient, and prescription drug mental health care expenditure.
Methods
Rank- and propensity score-based methods concordant with the Institute of Medicine (IOM) definition of health care disparities were compared with commonly used disparities methods. To implement the IOM definition, we modeled expenditures using a two-part GLM, adjusted distributions of need variables, and predicted expenditures for each racial/ethnic group.
Findings
Racial/ethnic disparities were significant for all expenditure measures. Disparity estimates from the IOM-concordant methods were similar to one another but greater than a method using the residual effect of race/ethnicity. Black–white and Latino–white disparities were found for any expenditure in each category and Latino–white disparities were significant in expenditure conditional on use.
Conclusions
Findings of disparities in access among blacks and disparities in access and expenditures after initiation among Latinos suggest the need for continued policy efforts targeting disparities reduction. In these data, the propensity score-based method and the rank-and-replace method were precise and adequate methods of implementing the IOM definition of disparity.
Keywords: Access/demand/utilization of services, determinants of health/population health/socioeconomic causes of health, mental health, racial/ethnic differences in health and health care
BACKGROUND/SIGNIFICANCE
Previous research, as summarized by the Surgeon General's Mental Health Report Supplement on Culture, Race, and Ethnicity (2001), found racial and ethnic differences in mental health care. Since the time of the Surgeon General's report, black–white and Latino–white disparities in mental health care have widened (Cook, Miranda, and McGuire 2007). Blacks and Latinos have fewer mental health visits to both generalist and specialty mental health care providers than whites do, and blacks suffering from mood and anxiety disorders are less likely than whites to receive care (Wells et al. 2001; Alegria et al. 2002, 2008; Wang et al. 2005; AHRQ 2008c). These treatment disparities may contribute to more chronic episodes of depression and greater functional limitation among minority groups (Breslau et al. 2005; Williams et al. 2007;).
Our study extends these previous findings by separately assessing disparities in any mental health treatment and expenditures given treatment for total, outpatient, and prescription drug mental health treatment. We focus on outpatient and prescription drug mental health care because outpatient treatment is the most common type of mental health care and mental health–related prescription drug expenditures are the primary reason for increases in mental health care expenditures over the last decade (Frank, Goldman, and McGuire 2009).
Disparities in mental health care are driven by several factors. First, many individuals diagnosed with a mental illness are not receiving mental health care services (AHRQ 2008c); conversely, many individuals without a diagnosed mental illness are receiving mental health services (Alegria et al. 2008). Second, socioeconomic factors mediate mental health care disparities. Poverty is a significant contributor to Latino–white and black–white differences in mental health specialty care (Alegria et al. 2002; Chow, Jaffee, and Snowden 2003;). Third, disparities are mediated by large differences in insurance status among racial/ethnic groups (DeNavas-Walt, Proctor, and Smith 2008) and the varying coverage of mental health services across insurance plans. Some generous plans cover most or all mental health services and pay providers on a fee-for-service basis; other insurance plans including “carved out” behavioral health care plans may restrict the number and type of mental health visits. State Medicaid plans also vary widely in their generosity of coverage of mental health services (Frank, Goldman, and Hogan 2003). Fourth, differences due to discrimination (whether because of biases, prejudice, or statistical discrimination) contribute to disparities in mental health care (Balsa and McGuire 2001; Balsa, McGuire, and Meredith 2005;).
Previous studies of mental health disparities use different methods to account for these underlying mechanisms of disparities. For example, the National Healthcare Disparities Reports (NHDR), published each year by the Agency of Healthcare Research and Quality (AHRQ), compares unadjusted means and assesses race coefficients in multivariate regression models (AHRQ 2008c). Other studies have estimated differences with and without adjustment for socioeconomic status (SES) variables and interpreted changes in race coefficients across these successive models as an indication of the mediation of SES variables (Wells et al. 2001; Alegria et al. 2002; Fiscella et al. 2002; Wang et al. 2005;). Other mental health care disparities studies (McGuire et al. 2006; Cook, Miranda, and McGuire 2007;) have implemented the Institute of Medicine (IOM) definition of health care disparity presented in Unequal Treatment (IOM 2002) as does the present study. This definition distinguishes between differences and disparities in quality of health care. Racial differences combine three distinct categories of effects:
Differences among groups in clinical appropriateness and need and patient preferences
Differential impact on groups of the operation of health care systems and the legal and regulatory climate, possibly due to differences in SES
Discrimination
According to the IOM, disparities exclude differences due to (1) but include differences due to (2) and (3). Implementing this definition requires measurement of these three sets of factors. In our analysis, we identify individual-level variables in the dataset that most closely represent each of the categories, considering variables related to mental health and health status to be indicators of clinical appropriateness and need, variables related to SES to identify differential treatment by the operation of the health care system, and racial/ethnic group for discrimination.1 Thus, using individual-level data, we balance mental health and health status measures across racial/ethnic groups but allow differences mediated by SES variables to be part of the disparity calculation. If the impact of the health care system and legal and regulatory policies is more detrimental to lower SES groups, and racial/ethnic minorities are disproportionately located in these lower SES groups, then these mediated differences should be considered part of a disparity. Differences due to discrimination (because of biases, prejudice, or statistical discrimination) also contribute to disparities in quality of health care.
Consistent use of the IOM definition would allow for comparisons between studies and across health care measures so that changes in disparities can be tracked over time. However, the definition is not easily implemented with commonly used analytic tools because it calls for the inclusion of some group differences but not others. Simple differences are not adjusted for health status variables, but race coefficients in multivariate regressions that adjust for all available variables do not capture the contribution to the disparity of racial/ethnic differences in SES.
In the current study, we define a method as “IOM-concordant” (Cook et al. 2009a) if it estimates the difference between the mental health care of white and minority (black or Latino) populations selected or adjusted to have the following characteristics: (1) the same distribution of health status; and (2) marginal distributions of SES that are like whites and minorities, respectively, with that distribution of health status. We recognize that there are numerous joint distributions for the nonwhite counterfactual group that can be specified under this definition. We prefer methods that preserve correlations in a plausible fashion, but we do not require a specific counterfactual joint distribution in order to avoid causal assumptions about the relationship between health status and SES.
We have identified two IOM-concordant methods of health status adjustment that are applicable in the context of nonlinear models: the rank-and-replace method (McGuire et al. 2006) and a method that combines propensity scores and the rank-and-replace method (Cook et al. 2009a). The rank-and-replace method adjusts health status by ranking each sample by a summary index of health status and replacing the health status of each minority individual with that of the correspondingly ranked white, thus preserving the ranking of health status and its rank correlation with SES measures. The propensity score-based method weights minority and white individuals to have the same health status distribution and then uses a rank-based method to restore the minority's original distribution of SES variables. This paper details differences in the methods' properties, applies these methods to mental health care, and assesses the sensitivity of findings to different mental health care measures. The mental health care sector is a particularly appropriate sector of health care to compare methods of implementation of the IOM framework because socioeconomic factors such as health insurance coverage, income, and education are strong mediators of mental health care (AHRQ 2008c), and mental health status and discrimination factor largely into racial/ethnic differences in access to mental health care (Balsa, McGuire, and Meredith 2005; Breslau et al. 2005;). An additional benefit is that the Medical Expenditure Panel Survey (MEPS) dataset contains detailed information regarding individuals' needs for mental health services, socioeconomic factors, and varying types and costs of mental health care utilization.
In this paper, we improve upon and implement methods concordant with the IOM definition to assess disparities in total mental health care expenditures and two subcategories of mental health care (outpatient treatment and prescription drug use). To better understand these disparities, we assess disparities in any treatment and expenditures given treatment.
DATA
We used the household components of the 2002–2006 MEPS, a nationally representative survey of families and individuals, their medical providers, and employers that collects information on individuals' health care expenditures, demographic characteristics, SES, health insurance status, payment sources, and health status. To add citizenship status and variables related to limitations due to mental illness, we link individual responses from the 2002–2006 MEPS with corresponding responses to the 2000–2004 National Health Interview Survey (NHIS) (AHRQ 2008a).
We focus on the application of IOM-concordant methods to three dependent variables: total mental health care expenditure, prescription drug expenditure, and outpatient mental health expenditure. These variables were generated from compiled claims data and self-reported out-of-pocket expenditure and standardized to 2006 dollars. In order to implement the IOM definition of health care disparities, we classified covariates other than race/ethnicity into two broad categories: SES variables and variables indicating mental health care need (from now on, referred to as “need” variables). SES variables include education, income, region of the country, residence in a metropolitan statistical area (MSA), citizenship status, insurance coverage, and participation in a health maintenance organization (HMO). Need variables include self-reported mental and physical health; the mental and physical health components of the SF-12; any limitation at work due to anxiety, depression, or other mental illness; gender; age; and marital status. Physical health variables are also considered as variables indicating need given the high rates of comorbidity between physical ailments and mental disorders (Alexopoulos et al. 1997; Afari et al. 2001; de Groot et al. 2001; Clarke and Meiris 2007;) and include any limitation due to physical health, body mass index (BMI), and a list of 11 chronic illnesses.
The sample size of the 5 years of MEPS data was initially 175,309 but was trimmed to 111,914 given our inclusion criteria of being 18 years of age or older, non-Latino white, black, or Latino, nonmilitary, and noninstitutionalized. MEPS surveys could not be linked with the NHIS for 3,775 respondents including persons who become eligible in the middle of the survey year, and a few cases found to be NHIS nonrespondents. Our final 2002–2006 MEPS sample contains 108,139 individuals with 64,196 whites, 16,949 blacks, and 26,994 Latinos. The MEPS lacked SF-12 physical and mental health component scores for about 7 percent of our sample, while most other variables were missing in <1 percent of the sample. We multiply imputed missing items to create five completed datasets, analyzed each set, and used standard rules to combine the estimates and adjust standard errors for the uncertainty due to imputation (Rubin 1998; Little and Rubin 2002;).
METHODS
Disparity estimation proceeded in three steps. The first was to fit a multivariate two-part model for mental health care expenditure (one each for total, outpatient, and prescription drug) as a function of all relevant independent covariates, including appropriate interactions. We separately modeled the probability of any expenditures and the level of expenditure conditional on positive expenditures using generalized linear models (GLMs) (McCullagh and Nelder 1989). This avoids the potential inconsistency from fitting an OLS model to logged expenditures in the second part without adequate retransformation (Manning 1998; Mullahy 1998;). For the positive part of the distribution of expenditures, we modeled the expected expenditures E(y|x, y>0) directly as μ(x′β) where μ is the link between the observed raw scale of expenditure, y, and the linear predictor x′β, where x is a vector of the predictors. The GLM also allows for heteroscedastic residual variances related to the predicted mean (Buntin and Zaslavsky 2004). The conditional variance of y given that y>0 is assumed to be a power of expected expenditures, conditional on x. Thus, we can characterize the mean and variance functions as
| (1) |
Using diagnostics in Manning and Mullahy (2001) and Buntin and Zaslavsky (2004), we identified the optimal GLM to have a log link, and residual variance proportional to mean squared (λ=2). We used the modified Hosmer–Lemeshow test to assess systematic misfit overall in terms of predicted expenditures, as well as the model misfit for major covariates.
The second step was to adjust the minority distribution of need to match the white distribution while preserving the distributions of SES variables for each racial/ethnic group using the rank-and-replace method or propensity score-based method, described below. Finally, predicted expenditures were calculated using the two-part GLM and the adjusted health status distributions, and compared across racial groups.
Adjustment Method #1: The Rank-and-Replace Method
The rank-and-replace adjustment method creates a counterfactual population of black or Latino individuals with the white distribution of need without adjustment for SES covariates. Multivariate indicators of need are summarized with a univariate need-based linear predictor (Cook, Miranda, and McGuire 2007; Cook et al. 2009a;) defined as the sum of the terms (coefficient times covariate) of the fitted model corresponding to need variables.2 Different models were fit for the first and second parts of the two-part model, where covariates included race/ethnicity indicators, SES and need variables, but no race/ethnicity-by-need interactions. Individuals were then assigned survey-weighted ranks within their race based on this need predictor, and the need variable values of each minority individual were replaced by those of the equivalently ranked white individual. Thus, a black individual with a need-based predictor at the p-th percentile for blacks would be reassigned the need variable values of the white individual at the p-th percentile for whites.
Predicted use and expenditure for each minority individual were then calculated using the coefficients from the original two-part model and the adjusted need covariate values. The means of these predictions were then subtracted from the means of white's predictions to estimate an IOM-concordant disparity.
We prefer this method to an alternative rank-and-replace method that adjusts each individual need variable separately (McGuire et al. 2006; Cook 2007; Cook, McGuire, and Zuvekas 2009b;). The latter does not deal systematically with associations among the covariates, and it faces difficulties with dichotomous variables because these have so many ties at 0 and 1. We also prefer this method to replacing the need-based linear predictor itself (Cook, Miranda, and McGuire 2007; Cook et al. 2009a;) because the latter adjusts racial/ethnic differences in coefficients as well as characteristics.
Adjustment Method #2: Combining a Health Status Propensity Score Method with SES Adjustment
A second method of adjustment for need combines propensity scores with the rank-and-replace method. The first part of this method weighted each individual based on the propensity of being a white (in a combined white–minority population) conditional on a vector of observed covariates. Because we only want to balance on need variables, we obtain a propensity score, ê (Hi), from the predicted probabilities generated by a logistic model for being white conditional on need covariates (age, gender, mental health status, and health status variables), but not SES variables. Separate models were fit for blacks and Latinos. Conditional on the propensity score, the distributions of observed need covariates are the same for minorities and whites (Rubin 1997).
We used the propensity score to weight minority individuals by their probability to be white (ê (Hi)), and white individuals by their probability to be minority (1−ê (Hi)), both in weighted regressions conditional on need covariates. These weights were multiplied by the survey weights to ensure that the weighted samples were balanced on need. These weights place more emphasis on individuals with ê (Hi) close to 0.5, whose health status distributions could be either white or minority. If the model for ê (Hi) is well specified, this weighting scheme adjusts the weighted need distributions to be the same for whites and minorities. The resulting white/minority counterfactual has need variables corresponding to the intersection of the white and minority populations' need distributions.
If SES and need variables are correlated, however, this propensity score adjustment is not concordant with the IOM definition since the weighting then also alters the distribution of SES variables.3 To undo the unintended alteration of the distribution of SES values, we applied a rank-and-replace adjustment of SES variables similar to that described above to adjust the propensity-score-weighted SES distributions in each group to match the corresponding preadjustment SES distributions. The resulting SES distributions for blacks and Latinos are, in effect, unadjusted, and marginal SES distributions for these groups end up identical to the original data.
For all three measures of mental health expenditures, we compared the disparity predictions and standard errors measured by (1) the rank-and-replace method; (2) the propensity score-based method; and other methods used previously in the literature: (3) differences in unadjusted means (e.g., AHRQ 2008c); and (4) a prediction method based on the race/ethnicity coefficient of the regression model. The latter prediction method, the “residual direct effect (RDE)” (McGuire et al. 2006) (also called “predictive margins” [Graubard and Korn 1999], or “recycled predictions” [see Davern et al. 2007; Blewett et al. 2008; Wells et al. 2008;]), generates predictions based on the coefficient of interest (in this case, the racial/ethnic group identifier) while adjusting for all other observed characteristics. For total mental health expenditures, we graphed, by method, each racial/ethnic groups' estimated disparity (white–minority) in probability of expenditure (part 1 of the two-part model), average predicted expenditure given care (part 2), and overall predicted expenditure.
Variance Calculation
Variance estimates account for both the complex sample design and the multiple imputation of missing data. Stratum and primary sampling unit (PSU) variables were standardized across pooled years (AHRQ 2008b) using publicly available strata and PSU variables that specify a common variance structure for MEPS respondents across multiple years of data. Variance estimates for predicted expenditures, rates, and disparities were calculated using a balanced-repeated-replication (BRR) procedure (Wolter 1985). This method repeats the estimation process used on the full sample on 64 subsamples of the population, each of which is half of the full sample size, and calculates the variance of these 64 estimates. The final step in standard error estimation accounts for multiple imputation by averaging the BRR-estimated standard errors across the five imputed datasets and adding 6/5 of the variance of those five estimates (Little and Rubin 2002).
RESULTS
Table 1 shows significant unadjusted differences between blacks and whites in nearly all mental health, need, and SES measures. Unadjusted expenditures and rates of any expenditure were significantly lower for blacks and Latinos compared with whites for total mental health expenditure, outpatient, and prescription drug mental health expenditure (p<.05).
Table 1.
2002–2006 Medical Expenditure Panel Survey (MEPS)-Weighted Population Characteristics for Non-Hispanic Whites, Blacks, and Hispanics Age≥18 (n=108,139)†
| White | Black | Hispanic | |
|---|---|---|---|
| Variable | (n=64,196) | (n=16,949) | (n=26,994) |
| Mental health care access variables | |||
| Total mental health expenditures (U.S.$FY 2006) | U.S.$197.95 | U.S.$140.80* | U.S.$100.14* |
| Any mental health expenditure | 15.7% | 8.1%* | 7.6%* |
| Outpatient mental health expenditure | U.S.$69.24 | U.S.$48.46* | U.S.$38.21* |
| Rx mental health expenditure | U.S.$97.10 | U.S.$54.96* | U.S.$44.52* |
| Mental health and health status variables | |||
| Self-reported mental health status | |||
| Good, very good, or excellent | 93.0% | 91.1%* | 93.6%* |
| Self-reported physical health status | |||
| Good, very good, or excellent | 87.7% | 81.6%* | 84.3%* |
| Scales | |||
| SF-12 mental health | 51.01 | 50.58* | 50.54* |
| SF-12 physical health | 49.49 | 48.66* | 50.65* |
| BMI | 26.98 | 28.96* | 27.74* |
| Chronic conditions | |||
| Diabetes | 6.6% | 10.0%* | 7.5%* |
| Asthma | 9.8% | 10.4%* | 6.9%* |
| High blood pressure | 26.7% | 32.2%* | 15.9%* |
| CHD | 3.9% | 2.4%* | 1.3%* |
| Angina | 2.6% | 1.6%* | 0.9%* |
| MI | 3.6% | 2.3%* | 1.2%* |
| Stroke | 2.8% | 2.9% | 1.1%* |
| Emphysema | 1.8% | 0.8%* | 0.3%* |
| Joint pain | 38.6% | 30.4%* | 22.6%* |
| Arthritis | 23.6% | 19.0%* | 10.6%* |
| Other heart condition | 7.3% | 4.8%* | 2.7%* |
| Any limitation of activity | |||
| Due to mental health | 1.5% | 1.5% | 1.2%* |
| Due to physical health | 29.1% | 27.1%* | 17.4%* |
| Age | |||
| 18–24 | 11.2% | 15.5%* | 18.4%* |
| 25–34 | 16.1% | 19.8%* | 26.8%* |
| 35–44 | 18.7% | 21.7%* | 23.3%* |
| 45–54 | 19.9% | 19.1%* | 15.1%* |
| 55–64 | 15.3% | 12.1%* | 8.4%* |
| 65–74 | 9.7% | 7.1%* | 4.9%* |
| 75+ | 9.1% | 4.7%* | 3.1%* |
| Gender | |||
| Female | 51.8% | 55.3%* | 48.7%* |
| Marital status | |||
| Married | 58.8% | 35.4%* | 53.4%* |
| SES variables | |||
| Poverty status | |||
| Below poverty line | 7.7% | 20.4%* | 17.9%* |
| Near poverty | 3.2% | 5.8%* | 7.3%* |
| Low-income | 10.9% | 17.1%* | 21.5%* |
| Middle income | 30.5% | 31.7%* | 33.4%* |
| High income | 47.7% | 25.0%* | 19.9%* |
| Education | |||
| <HS | 10.6% | 20.2%* | 42.1%* |
| HS graduate | 32.6% | 36.5%* | 27.6%* |
| Some college | 24.0% | 23.4% | 16.0%* |
| College graduate | 32.8% | 19.9%* | 14.3%* |
| Health insurance | |||
| Private insurance | 78.7% | 60.8%* | 48.3%* |
| Public insurance | 11.6% | 22.3%* | 17.7%* |
| Uninsured | 9.7% | 16.9%* | 34.0%* |
| HMO | 28.2% | 34.1%* | 29.8%* |
| Region | |||
| Northeast | 20.1% | 17.3%* | 14.4%* |
| Midwest | 26.5% | 18.1%* | 8.3%* |
| South | 33.7% | 55.8%* | 35.9%* |
| West | 19.7% | 8.8%* | 41.4%* |
| Lives in metropolitan area | 79.0% | 88.3%* | 92.4%* |
| Citizenship | |||
| United States | 98.3% | 95.6%* | 61.9%* |
Significant at the p<0.05 level.
Calculations are weighted to be representative of the entire U.S. population.
For total mental health expenditure, we present coefficients from the two-part model to identify significant correlates of mental health expenditure (Table 2). The race/ethnicity coefficient was significant for blacks but not for Latinos in the logit model for any expenditure. As expected, poorer self-reported mental health status, poorer self-reported physical health status, having any limitation due to mental or physical illness, lower scores on the MCS-12 (signifying worse mental health), and a number of chronic conditions positively predicted mental health expenditure. Being female, more highly educated, and a U.S. citizen, having a higher BMI, and residing in a metropolis were also positive predictors. Negative predictors were having three or more chronic conditions, being married, and being uninsured. Among those with positive expenditures, neither the black nor Latino coefficient was a significant predictor of quantity. Predictors of larger expenditures among positive spenders were poorer self-reported mental health status, having a limitation of activity due to physical or mental health, higher scores on the PCS-12 (indicating better physical health), being a college graduate, and having public insurance. Significant negative predictors were higher scores on the MCS-12, having joint pain, being above age 65, female, and married, and living in the South or West.
Table 2.
Two-Part GLM Model of Total Mental Health Expenditures (U.S.$2006) in Last Year (Independent Covariates Include Race, Demographic, SES, and Health Status Variables)†,‡ (n=108,139)
| Part 1—Any Expenditure |
Part 2—Expenditure if U.S.$>0 |
|||
|---|---|---|---|---|
| Variable | Coefficient | SE | Coefficient | SE |
| Race | ||||
| Non-Latino White | Referent | |||
| Black | −0.49* | 0.21 | 0.09 | 0.30 |
| Latino | −0.21 | 0.21 | −0.30 | 0.26 |
| Health status variables | ||||
| Self-reported mental health status | ||||
| Excellent | Referent | |||
| Very good | 0.31* | 0.10 | 0.00 | 0.16 |
| Good | 0.64* | 0.08 | 0.27* | 0.16 |
| Fair | 1.55* | 0.09 | 0.55* | 0.15 |
| Poor | 2.11* | 0.23 | 0.78* | 0.19 |
| Self-reported health status | ||||
| Excellent | Referent | |||
| Very good | 0.32* | 0.10 | 0.16 | 0.12 |
| Good | 0.26* | 0.09 | 0.23 | 0.14 |
| Fair | 0.40* | 0.10 | 0.21 | 0.13 |
| Poor | 0.51* | 0.11 | 0.10 | 0.15 |
| Any limitation of activity | ||||
| Due to physical health | 0.36* | 0.04 | 0.17* | 0.05 |
| Due to mental health | 1.71* | 0.10 | 0.48* | 0.07 |
| Scales | ||||
| BMI | 0.005* | 0.002 | 0.000 | 0.003 |
| PCS12 (0–100) | −0.003 | 0.01 | 0.026* | 0.01 |
| MCS12 (0–100) | 0.0004 | 0.01 | −0.025* | 0.01 |
| PCS12_squared | 0.0001 | 0.0001 | −0.0003* | 0.0001 |
| MCS12_squared | −0.0005* | 0.0001 | 0.0002 | 0.0001 |
| Conditions | ||||
| Diabetes | 0.14* | 0.05 | −0.10 | 0.06 |
| Asthma | 0.29* | 0.05 | 0.07 | 0.07 |
| High BP | 0.29* | 0.04 | −0.04 | 0.06 |
| CHD | 0.06 | 0.09 | −0.15 | 0.13 |
| Angina | 0.42* | 0.08 | 0.09 | 0.13 |
| MI | −0.07 | 0.09 | −0.10 | 0.14 |
| Stroke | 0.37* | 0.08 | −0.13 | 0.10 |
| Emphysema | 0.33* | 0.10 | 0.02 | 0.10 |
| Joint pain | 0.10* | 0.03 | −0.10* | 0.04 |
| Arthritis | 0.33* | 0.04 | −0.04 | 0.05 |
| Other heart disease | 0.27* | 0.05 | −0.02 | 0.08 |
| 3 or more conditions | −0.16* | 0.05 | 0.02 | 0.08 |
| 5 or more conditions | −0.37* | 0.09 | 0.10 | 0.10 |
| Age (referent 35–44) | ||||
| 18–24 | −0.28* | 0.07 | −0.15 | 0.09 |
| 25–34 | −0.15* | 0.05 | −0.09 | 0.08 |
| 35–44 | Referent | |||
| 45–54 | 0.02 | 0.04 | −0.10 | 0.06 |
| 55–64 | −0.06 | 0.05 | −0.06 | 0.09 |
| 65–74 | −0.42* | 0.06 | −0.27* | 0.09 |
| 75+ | −0.76* | 0.06 | −0.26* | 0.12 |
| Gender | ||||
| Female | 0.52* | 0.06 | −0.30* | 0.10 |
| Marital status | ||||
| Married | −0.16* | 0.04 | −0.20* | 0.05 |
| SES variables | ||||
| Poverty status | ||||
| Below poverty line | Referent | |||
| Near poverty | 0.06 | 0.07 | −0.07 | 0.09 |
| Low income | −0.07 | 0.05 | −0.12 | 0.07 |
| Middle income | −0.06 | 0.05 | −0.03 | 0.07 |
| High income | 0.02 | 0.06 | −0.05 | 0.07 |
| Education | ||||
| < High school | Referent | |||
| HS graduate | 0.19* | 0.07 | 0.00 | 0.12 |
| Some college | 0.24* | 0.08 | 0.01 | 0.12 |
| College graduate | 0.61* | 0.09 | 0.26* | 0.11 |
| Health insurance | ||||
| Privately insured | Referent | |||
| Public insurance | 0.03 | 0.05 | 0.27* | 0.06 |
| Uninsured | −0.80* | 0.06 | −0.11 | 0.09 |
| HMO | −0.04 | 0.04 | −0.02 | 0.05 |
| Region | ||||
| Northeast | Referent | |||
| Midwest | −0.01 | 0.05 | −0.01 | 0.07 |
| South | −0.02 | 0.05 | −0.21* | 0.07 |
| West | 0.00 | 0.06 | −0.13* | 0.07 |
| Citizenship (referent: non-U.S. citizen) | ||||
| U.S. citizen | 0.52* | 0.07 | 0.01 | 0.12 |
| City | ||||
| MSA | 0.09* | 0.04 | 0.05 | 0.07 |
| Constant | −0.34 | 0.30 | 7.59* | 0.39 |
Source: 2002–2006 Medical Expenditure Panel Survey (MEPS).
Significant at p<0.05 level.
Coefficients and standard errors take into account sampling weights and stratification used to make MEPS sample representative of U.S. population.
Model includes interactions between race and sex, self-reported mental health status, self-reported overall health status, education, and income variables, yet only the main effect coefficients are displayed here. Main effects with interactions included were centered (Kraemer and Blasey 2004) before fitting the model. Year of survey indicator variables were also included in the regression but are not presented.
We found statistically significant racial/ethnic disparities in total, outpatient, and prescription drug expenditures (Table 3) for all methods of calculating disparity (unadjusted, RDE of race, rank-and-replace, and propensity score-based method), and for both blacks and Latinos. Whites spent an average of U.S.$198 on mental health care. The rank-and-replace method estimated the disparities (white–minority) to be U.S.$80 for blacks and U.S.$90 for Latinos, and the propensity score-based method estimated disparities of U.S.$104 for blacks and U.S.$91 for Latinos. For outpatient mental health care, whites spent an average of U.S.$69. Using the rank-and-replace method, blacks and Latinos spent U.S.$28 less. Using the propensity score-based method, blacks and Latinos spent U.S.$38 and U.S.$32 less, respectively. For prescription drug mental health care, whites spent an average of U.S.$97. Using the rank-and-replace method, blacks and Latinos spent U.S.$53 and U.S.$49 less, respectively, and using the propensity score-based method, blacks and Latinos spent U.S.$64 and U.S.$48 less. For each of the three dependent variables, the IOM-concordant disparity estimates were generally lower than unadjusted rates for Latinos and higher for blacks, and significantly greater than RDE prediction estimates for Latinos.
Table 3.
Comparing Disparity Estimates for Different Types of Mental Health Expenditures
| White |
Black |
Latino |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mental Health Expenditures | Mean (SE) | Mean (SE) | Difference/ Disparity (SE) | Mean (SE) | Difference/ Disparity (SE) | |||||
| Total | ||||||||||
| Unadjusted | 197.95 | (7.31) | 140.80 | (15.24) | 57.15 | (15.94) | 100.14 | (10.20) | 97.81 | (11.00) |
| Rank and replace | 197.95 | (7.31) | 114.84 | (13.49) | 83.11 | (14.46) | 107.61 | (8.97) | 90.34 | (9.47) |
| Propensity score (W–B) | 240.73 | (10.28) | 129.92 | (13.85) | 110.81 | (15.06) | ||||
| Propensity score (W–L) | 200.18 | (8.70) | 101.88 | (11.03) | 98.30 | (11.81) | ||||
| RDE (full adjustment) | 195.92 | (7.42) | 99.61 | (12.60) | 96.31 | (13.68) | 147.04 | (10.31) | 48.88 | (10.33) |
| Outpatient | ||||||||||
| Unadjusted | 69.24 | (3.64) | 48.46 | (4.08) | 20.78 | (5.21) | 38.21 | (3.50) | 31.03 | (4.21) |
| Rank and replace | 69.24 | (3.64) | 39.45 | (4.54) | 29.79 | (5.43) | 39.79 | (3.41) | 29.45 | (3.98) |
| Propensity score (W–) | 84.90 | (4.72) | 44.04 | (3.75) | 40.86 | (5.47) | ||||
| Propensity score (W–L) | 73.92 | (4.31) | 39.32 | (3.71) | 34.60 | (4.55) | ||||
| RDE (full adjustment) | 67.46 | (3.65) | 36.41 | (3.44) | 31.05 | (4.79) | 55.22 | (3.93) | 12.24 | (4.44) |
| Prescription drug | ||||||||||
| Unadjusted | 97.10 | (3.13) | 54.96 | (5.40) | 42.14 | (5.62) | 44.52 | (4.45) | 52.58 | (5.01) |
| Rank and replace | 97.10 | (3.13) | 44.17 | (4.86) | 52.93 | (4.79) | 48.24 | (4.61) | 48.86 | (5.27) |
| Propensity score (W–B) | 115.77 | (4.14) | 48.99 | (4.93) | 66.78 | (5.08) | ||||
| Propensity score (W–L) | 95.21 | (3.98) | 45.07 | (4.81) | 50.14 | (5.69) | ||||
| RDE (Full adjustment) | 98.88 | (3.13) | 34.47 | (4.43) | 64.41 | (4.61) | 65.99 | (5.43) | 32.89 | (6.02) |
Source: Combined Medical Expenditure Panel Survey (MEPS) data from 2002 to 2006.
All disparity estimates are significant.
Standard errors are in parentheses.
RDE, Residual Direct Effect of Race/Ethnicity Prediction Method Based on Race/Ethnicity Coefficient; W–B, White–Black differences; W–L, White–Latino differences.
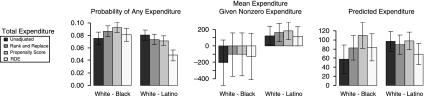
The larger share of mental health care expenditure disparities was attributable to differences in the predicted probabilities of any mental health expenditure (Figure 1). For example, using the rank-and-replace method, blacks and Latinos were about half as likely to have any mental health care expenditure (7.0 percent of blacks, 8.3 percent of Latinos, and 15.7 percent of whites). Disparities in predicted probability of any expenditure were also significant for outpatient care and prescription drug expenditures using both IOM-concordant methods (data not shown). Among those who used care, there were no differences between blacks and whites on predicted expenditures and Latinos had significantly lower predicted expenditure. These trends held across all three dependent variables, and across unadjusted estimates, RDE predictions, and both IOM-concordant methods.
Figure 1.
Mental Health Expenditure by Race/Ethnicity
Note. Unadjusted differences, two IOM-concordant predictions (rank-and-replace and propensity score-based methods), and RDE predictions are presented. Source: 2002–2006 Medical Expenditure Panel Surveys (MEPS). RDE, residual direct effect of race/ethnicity prediction method based on race/ethnicity coefficient error bars represent 95 percent confidence interval generated from standard estimation using a combination of balanced repeated replication and multiple imputation methods.
DISCUSSION
We found black–white and Latino–white disparities in total, outpatient, and prescription drug mental health care expenditures that were robust to adjusting for need using two different methods. The disparities in reaching the first mental health visit, outpatient visit and filling the first prescription highlight the importance of reducing barriers to access to mental health care for racial/ethnic minorities. On the other hand, we did not find black–white disparities among those using mental health care services, complementing previous findings that African Americans were less likely than whites to fill an antidepressant prescription but were similar to whites in having an adequate trial of antidepressant medication (Harman, Edlund, and Fortney 2004). These latter results provide preliminary evidence that equitable use of mental health care services for African Americans is being provided once it is initiated, but that Latino–white disparities persist in mental health care use even after accessing care.
Eliminating disparities in any use of mental health care will require intervention at multiple levels, including reducing the numbers of uninsured, changing provider practices, and reducing barriers to care. As in previous studies (Zuvekas and Taliaferro 2003; McGuire et al. 2006; Cook, Miranda, and McGuire 2007;), we found that blacks and Latinos were more likely than whites to be uninsured, and that lack of insurance was a strong negative predictor of any utilization of mental health care. At the provider level, physicians were found to be less likely to identify mental illness among racial/ethnic minority patients compared to white patients, possibly because of the inadequacy of standardized screening and diagnostic instruments to detect mental illness in minority populations (Ryu, Young, and Kwak 2002), or greater levels of miscommunication between patient and provider because of different language, culture, or communications patterns (Balsa, McGuire, and Meredith 2005). Blacks and Latinos are more likely than whites to perceive stigma and financial barriers to mental health care, disproportionately endorsing “embarrassment to discuss problems,”“loss of pay from work,” and “concern of losing employment,” as barriers to receiving mental health treatment (Ojeda and McGuire 2006).
A limitation of the data is the lack of information in the MEPS regarding preferences for mental health care, a predictor of mental health care use that has been shown to vary significantly by racial/ethnic group (Diala et al. 2001; Cooper et al. 2003;), and which should be controlled for in disparity calculations according to the IOM definition of health care disparities. Even if preferences measures were included, their adjustment would be problematic given that patients are rarely fully informed about their clinical options when deciding to access health care (Braddock et al. 1999; IOM 2002; Ashton et al. 2003;), and because preferences may have been influenced by previous experiences with discrimination or with inadequate or inaccessible care (Cooper-Patrick et al. 1997). Without accounting for the association between preferences, SES, and previous discrimination, the inclusion and adjustment of preferences in disparities models may lead to biased disparity estimates. Another limitation of our data is that the MEPS does not provide adequate sample size to measure disparities among Latino and African American subethnic groups (e.g., Mexican, Puerto Rican, Cuban, Afro-Caribbean) while adjusting for other covariates. Prior research (Alegria et al. 2007; Jackson et al. 2007;) found significant mental health service use differences between these subethnic groups, suggesting this more in-depth investigation of disparities would be worthwhile given a larger dataset.
In this paper, we offer two methods of implementing the IOM definition of health care disparities. We advocate for the continued use of IOM-concordant methods because they measure the part of racial/ethnic differences in health care that is most relevant and amenable to change at the health system level, distinct from underlying differences in need characteristics that are beyond the immediate reach of health care. Similar to previous studies (McGuire et al. 2006; Cook, McGuire, and Zuvekas 2009b;), we found important differences between IOM-concordant methods and other typically used disparity methods in the magnitude of disparities estimated. IOM-concordant methods estimated black–white disparities to be greater than a comparison of unadjusted means, and Latino–white disparities to be greater than the RDE method. The comparison of the IOM-concordant methods with the RDE prediction method identified a significant mediating role of SES-related factors (education, income, insurance, citizenship, and regional characteristics) for Latinos, but not blacks in these data. Decomposing the contributions of these variables to disparity estimates (results not shown) shows that, for blacks, change in disparity estimates due to adjustments to SES were small in comparison with the main black race effect. For Latinos, the smaller disparities estimated using the RDE prediction method were largely driven by adjustments to the education, insurance status, and citizenship status variables.
We compared the propensity score-based and rank-and-replace implementations of the IOM definition of health care disparities. While both methods are IOM-concordant, adjusting white and minority need distributions to be the same, the resulting distribution differs between the two methods. The rank-and-replace method replaces minority need with that of whites. The propensity score-based method adjusts the need distributions of both races to that of a subset of whites and blacks reflecting their overlap on need characteristics and therefore is more similar to that of blacks and reflects higher need.
These differing counterfactual need distributions can lead to differing disparity estimates because of the nonlinearity of the models. Race and SES effects are modeled additively on the logit (for probabilities) or log (for conditional costs) scale, and when applied to a population with greater baseline level, the retransformed difference is larger on the natural scale (probability or dollars, respectively).
The methods also differ in their use of outcome variables; the rank-and-replace method adjusts the health status distributions as they affect expenditure, while the propensity score-based method adjusts health status distributions ignoring expenditure. Thus, the propensity score-based method provides the same adjustment for both parts of the two-part model and for any desired dependent variables, while the rank-and-replace adjustment differs according to the model and the response.
Each method has appealing methodological features. The counterfactual minority population created by the rank-and-replace method is constructed to match two observable distributions: the marginal health status distribution of whites and the marginal SES distribution of minorities. On the other hand, the counterfactual population created by the propensity score-based method may be more plausible because it conducts comparisons in populations of white and minority individuals selected (by weighting) to have similar distributions of health status characteristics. By explicitly modeling the outcome variable in each part of the two-part model, the rank-and-replace method ensures identical distributions of health status variables as they affect our quantities of interest, while by ignoring the outcome variable in the main adjustment step, the propensity score provides protection against data dredging or manipulation of the model to achieve a desired result. Using both methods provides a check on the sensitivity of estimates to alternative modeling assumptions. In this study, both methods found that fewer mental health care resources, whether overall, outpatient, or prescription drug related, were spent on blacks and Latinos, and that the large part of the disparity was attributable to differences in initial use of these services.
Acknowledgments
Joint Acknowledgment/Disclosure Statement: We would like to acknowledge funding from the National Institute of Mental Health (R03 MH 082312 and P50 MHO 73469). The opinions expressed here are not those of the Harvard Medical School, Harvard University, the Cambridge Health Alliance, or the National Institute of Mental Health. We would like to thank audience members at the 2009 AcademyHealth conference for their comments and suggestions. Any remaining errors are those of the authors.
Disclosures: None.
Disclaimers: None.
NOTES
Using the effect of race/ethnicity after adjustment for other observed covariates as a proxy for discrimination, we follow upon previous analyses (e.g., Barsky et al. 2002). We recognize that this residual effect may include the effect of other omitted variables besides discrimination that differ by race/ethnicity (National Research Council 2004) but use this strategy in the absence of validated, objective measures of discrimination.
This method is an adaptation of a replacement strategy proposed by Fairlie (2006) in which one group's values are sequentially replaced with another's, based on a respondent's predicted probability of having the outcome of interest.
The propensity score method is discordant from the IOM definition for similar reasons to the discordance of a regression of expenditure on health status variables, ignoring SES variables (e.g., preliminary models in Saha, Arbelaez, and Cooper 2003). Leaving SES out of the model will load racial differences in SES onto the race coefficient, allowing for an approximation of the IOM-defined disparity (Balsa, Cao, and McGuire 2007), but it will not identify the contribution of racial differences in SES that is mediated by health status.
SUPPORTING INFORMATION
Additional supporting information may be found in the online version of this article:
Appendix SA1: Author Matrix.
Please note: Wiley-Blackwell is not responsible for the content or functionality of any supporting materials supplied by the authors. Any queries (other than missing material) should be directed to the corresponding author for the article.
REFERENCES
- Afari N, Schmaling KB, Barnhart S, Buchwald D. Psychiatric Comorbidity and Functional Status in Adult Patients with Asthma. Journal of Clinical Psychology in Medical Settings. 2001;8(4):245–52. [Google Scholar]
- AHRQ. Linkage File for 2006 MEPS and 2004/2005 NHIS Public-use Files. Rockville, MD: Agency for Healthcare Research and Quality; 2008a. [Google Scholar]
- AHRQ. MEPS HC-036BRR: 1996–2006 Replicates for Calculating Variances File. Rockville, MD: Agency for Healthcare Research and Quality; 2008b. [Google Scholar]
- AHRQ. National Healthcare Disparities Report, 2008. Rockville, MD: Agency for Healthcare Research and Quality; 2008c. [Google Scholar]
- Alegria M, Canino G, Rios R, Vera M, Calderon J, Rusch D, Ortega A. Inequalities in Use of Specialty Mental Health Services among Latinos, African Americans, and Non-Latino Whites. Psychiatric Services. 2002;53(12):1547–55. doi: 10.1176/appi.ps.53.12.1547. [DOI] [PubMed] [Google Scholar]
- Alegria M, Chatterji P, Wells K, Cao Z, Chen C, Takeuchi D, Jackson J, Meng XL. Disparity in Depression Treatment among Racial and Ethnic Minority Populations in the United States. Psychiatric Services. 2008;59(11):1264–72. doi: 10.1176/appi.ps.59.11.1264. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alegria M, Mulvaney-Day N, Woo M, Torres M, Gao S, Oddo V. Correlates of Past-Year Mental Health Service Use among Latinos: Results from the National Latino and Asian American Study. American Journal of Public Health. 2007;97(1):76–83. doi: 10.2105/AJPH.2006.087197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alexopoulos GS, Meyers BS, Young RC, Campbell S, Silbersweig D, Charlson M. Vascular Depression' Hypothesis. Archives of General Psychiatry. 1997;54(10):915–22. doi: 10.1001/archpsyc.1997.01830220033006. [DOI] [PubMed] [Google Scholar]
- Ashton CM, Haidet P, Paterniti DA, Collins TC, Gordon HS, O'Malley K, Petersen LA, Sharf BF, Suarez-Almazor ME, Wray NP, Street RL., Jr Racial and Ethnic Disparities in the Use of Health Services: Bias, Preferences, or Poor Communication? Journal of General Internal Medicine. 2003;18(2):146–52. doi: 10.1046/j.1525-1497.2003.20532.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Balsa A, Cao Z, McGuire T. Does Managed Health Care Reduce Unfair Differences in Health Care Use between Minorities and Whites? Journal of Health Economics. 2007;26(1):101–21. doi: 10.1016/j.jhealeco.2006.06.001. [DOI] [PubMed] [Google Scholar]
- Balsa A, McGuire T. Statistical Discrimination in Health Care. Journal of Health Economics. 2001;20(6):881–907. doi: 10.1016/s0167-6296(01)00101-1. [DOI] [PubMed] [Google Scholar]
- Balsa AI, McGuire TG, Meredith LS. Testing for Statistical Discrimination in Health Care. Health Services Research. 2005;40(1):227–52. doi: 10.1111/j.1475-6773.2005.00351.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barsky R, Bound J, Charles KK, Lupton JP. Accounting for the Black–White Wealth Gap. Journal of the American Statistical Association. 2002;97(459):663–73. [Google Scholar]
- Blewett LA, Davidson G, Bramlett MD, Rodin H, Messonnier ML. The Impact of Gaps in Health Insurance Coverage on Immunization Status for Young Children. Health Services Research. 2008;43(5, part 1):1619–36. doi: 10.1111/j.1475-6773.2008.00864.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Braddock CH, III, Edwards KA, Hasenberg NM, Laidley TL, Levinson W. Informed Decision Making in Outpatient Practice: Time to Get Back to Basics. JAMA. 1999;282(24):2313–20. doi: 10.1001/jama.282.24.2313. [DOI] [PubMed] [Google Scholar]
- Breslau J, Kendler KS, Su M, Gaxiola-Aguilar S, Kessler RC. Lifetime Risk and Persistence of Psychiatric Disorders across Ethnic Groups in the United States. Psychological Medicine. 2005;35(3):317–27. doi: 10.1017/s0033291704003514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buntin MB, Zaslavsky AM. Too Much Ado about Two-Part Models and Transformation? Comparing Methods of Modeling Medicare Expenditures. Journal of Health Economics. 2004;23(3):525–42. doi: 10.1016/j.jhealeco.2003.10.005. [DOI] [PubMed] [Google Scholar]
- Chow JC, Jaffee K, Snowden L. Racial/Ethnic Disparities in the Use of Mental Health Services in Poverty Areas. American Journal of Public Health. 2003;93(5):792–7. doi: 10.2105/ajph.93.5.792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clarke JL, Meiris DC. Building Bridges: Integrative Solutions for Managing Complex Comorbid Conditions. American Journal of Medical Quality. 2007;22(2 suppl):5S–16S. doi: 10.1177/1062860607299242. [DOI] [PubMed] [Google Scholar]
- Cook BL. Effect of Medicaid Managed Care on Racial Disparities in Health Care Access. Health Services Research. 2007;42(1):124–45. doi: 10.1111/j.1475-6773.2006.00611.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook BL, McGuire TG, Zaslavsky AM, Meara E. Adjusting for Health Status in Non-Linear Models of Health Care Disparities. Health Services Outcomes and Research Methodology. 2009a;9(1):1–21. doi: 10.1007/s10742-008-0039-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook BL, McGuire TG, Zuvekas SH. Measuring Trends in Racial/Ethnic Health Care Disparities. Medical Care Research and Review. 2009b;66(1):23–48. doi: 10.1177/1077558708323607. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cook BL, Miranda J, McGuire TG. Measuring Trends in Mental Health Care Disparities, 2000–2004. Psychiatric Services. 2007;58(12):1533–40. doi: 10.1176/ps.2007.58.12.1533. [DOI] [PubMed] [Google Scholar]
- Cooper LA, Gonzales JJ, Gallo JJ, Rost KM, Meredith LS, Rubenstein LV, Wang NY, Ford DE. The Acceptability of Treatment for Depression among African-American, Hispanic, and White Primary Care Patients. Medical Care. 2003;41(4):479–89. doi: 10.1097/01.MLR.0000053228.58042.E4. [DOI] [PubMed] [Google Scholar]
- Cooper-Patrick L, Powe NR, Jenckes MW, Gonzales JJ, Levine DM, Ford DE. Identification of Patient Attitudes and Preferences Regarding Treatment of Depression. Journal of General Internal Medicine. 1997;12(7):431–38. doi: 10.1046/j.1525-1497.1997.00075.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davern M, Rodin H, Blewett LA, Call KT. Are the Current Population Survey Uninsurance Estimates Too High? An Examination of the Imputation Process. Health Services Research. 2007;42(5):2038–55. doi: 10.1111/j.1475-6773.2007.00703.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Groot M, Anderson R, Freedland KE, Clouse RE, Lustman PJ. Association of Depression and Diabetes Complications: A Meta-Analysis. American Psychosomatic Society. 2001;63(4):619–30. doi: 10.1097/00006842-200107000-00015. [DOI] [PubMed] [Google Scholar]
- DeNavas-Walt C, Proctor BD, Smith JC. U.S. Census Bureau, Current Population Reports, P60–235, Income, Poverty, and Health Insurance Coverage in the United States: 2007. Washington, DC: U.S. Government Printing Office; 2008. [Google Scholar]
- Diala C, Muntaner C, Walrath C, Nickerson KJ, LaVeist TA, Leaf P. Racial/Ethnic Differences in Attitudes Toward Seeking Professional Mental Health Services. American Journal of Public Health. 2001;91(5):805–7. doi: 10.2105/ajph.91.5.805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fairlie R. 2006. An Extension of the Blinder-Oaxaca Decomposition Technique to Logit and Probit Models. IZA Discussion Papers. Bonn, Germany: I. f. t. S. o. L. (IZA)
- Fiscella K, Franks P, Doescher MP, Saver BG. Disparities in Health Care by Race, Ethnicity, and Language among the Insured: Findings from a National Sample. Medical Care. 2002;40(1):52–9. doi: 10.1097/00005650-200201000-00007. [DOI] [PubMed] [Google Scholar]
- Frank RG, Goldman HH, Hogan M. Medicaid and Mental Health: Be Careful What You Ask For. Health Affairs. 2003;22(1):101–13. doi: 10.1377/hlthaff.22.1.101. [DOI] [PubMed] [Google Scholar]
- Frank RG, Goldman HH, McGuire TG. Trends in Mental Health Cost Growth: An Expanded Role for Management? Health Affairs. 2009;28(3):649–59. doi: 10.1377/hlthaff.28.3.649. [DOI] [PubMed] [Google Scholar]
- Graubard BI, Korn EL. Predictive Margins with Survey Data. Biometrics. 1999;55(2):652–9. doi: 10.1111/j.0006-341x.1999.00652.x. [DOI] [PubMed] [Google Scholar]
- Harman JS, Edlund MJ, Fortney JC. Disparities in the Adequacy of Depression Treatment in the United States. Psychiatric Services. 2004;55(12):1379–85. doi: 10.1176/appi.ps.55.12.1379. [DOI] [PubMed] [Google Scholar]
- IOM. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academies Press; 2002. [PubMed] [Google Scholar]
- Jackson JS, Neighbors HW, Torres M, Martin LA, Williams DR, Baser R. Use of Mental Health Services and Subjective Satisfaction with Treatment among Black Caribbean Immigrants: Results from the National Survey of American Life. American Journal of Public Health. 2007;97(1):60–7. doi: 10.2105/AJPH.2006.088500. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kraemer HC, Blasey CM. Centering in Regression Analyses: A strategy to Prevent Errors in Statistical Inference. International Journal of Methods in Psychiatric Research. 2004;13(3):141–51. doi: 10.1002/mpr.170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Little RJA, Rubin DB. Statistical Analysis with Missing Data. Hoboken, NJ: Wiley; 2002. [Google Scholar]
- Manning W, Mullahy J. Estimating Log Models: To Transform or Not to Transform? Journal of Health Economics. 2001;20(4):461–94. doi: 10.1016/s0167-6296(01)00086-8. [DOI] [PubMed] [Google Scholar]
- Manning WG. The Logged Dependent Variable, Heteroscedasticity, and the Retransformation Problem. Journal of Health Economics. 1998;17(3):283–95. doi: 10.1016/s0167-6296(98)00025-3. [DOI] [PubMed] [Google Scholar]
- McCullagh P, Nelder JA. Generalized Linear Models. London: Chapman & Hall; 1989. [Google Scholar]
- McGuire TG, Alegria M, Cook BL, Wells KB, Zaslavsky AM. Implementing the Institute of Medicine Definition of Disparities: An Application to Mental Health Care. Health Services Research. 2006;41(5):1979–2005. doi: 10.1111/j.1475-6773.2006.00583.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mullahy J. Much Ado About Two: Reconsidering Retransformation and the Two-Part Model in Health Econometrics. Journal of Health Economics. 1998;17(3):247–81. doi: 10.1016/s0167-6296(98)00030-7. [DOI] [PubMed] [Google Scholar]
- National Research Council. Measuring Racial Discrimination. In: Blank RM, Dabady M, Citro CF, editors. Panel on Methods for Assessing Discrimination. Washington, DC: National Academy Press; 2004. pp. 121–28. [Google Scholar]
- Ojeda V, McGuire T. Gender and Racial/Ethnic Differences in Use of Outpatient Mental Health and Substance Use Services by Depressed Adults. Psychiatric Quarterly. 2006;77(3):211–22. doi: 10.1007/s11126-006-9008-9. [DOI] [PubMed] [Google Scholar]
- Rubin DB. Estimating Causal Effects from Large Data Sets Using Propensity Scores. Annals of Internal Medicine. 1997;127(8, part 2):757–63. doi: 10.7326/0003-4819-127-8_part_2-199710151-00064. [DOI] [PubMed] [Google Scholar]
- Rubin DB. Multiple Imputation of Nonresponse in Surveys. New York: Wiley; 1998. [Google Scholar]
- Ryu H, Young WB, Kwak H. Differences in Health Insurance and Health Service Utilization among Asian Americans: Method for Using the NHIS to Identify Unique Patterns between Ethnic Groups. International Journal of Health Planning and Management. 2002;17:55–68. doi: 10.1002/hpm.652. [DOI] [PubMed] [Google Scholar]
- Saha S, Arbelaez JJ, Cooper LA. Patient-Physician Relationships and Racial Disparities in the Quality of Health Care. American Journal of Public Health. 2003;93(10):1713–9. doi: 10.2105/ajph.93.10.1713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- U.S. Surgeon General. Mental Health: Culture, Race, and Ethnicity. A Supplement to Mental Health: A Report of the Surgeon General. Washington, DC: U.S. Department of Health and Human Services; 2001. [Google Scholar]
- Wang PS, Lane M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-Month Use of Mental Health Services in the United States: Results from the National Comorbidity Survey Replication. Archives of General Psychiatry. 2005;62(6):629–40. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- Wells K, Klap R, Koike A, Sherbourne C. Ethnic Disparities in Unmet Need for Alcoholism, Drug Abuse, and Mental Health Care. American Journal of Psychiatry. 2001;158(12):2027–32. doi: 10.1176/appi.ajp.158.12.2027. [DOI] [PubMed] [Google Scholar]
- Wells KB, Tang L, Miranda J, Benjamin B, Duan N, Sherbourne CD. The Effects of Quality Improvement for Depression in Primary Care at Nine Years: Results from a Randomized, Controlled Group-Level Trial. Health Services Research. 2008;43(6):1952–74. doi: 10.1111/j.1475-6773.2008.00871.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Gonzalez HM, Neighbors H, Nesse R, Abelson JM, Sweetman J, Jackson JS. Prevalence and Distribution of Major Depressive Disorder in African Americans, Caribbean Blacks, and Non-Hispanic Whites: Results from the National Survey of American Life. Archives of General Psychiatry. 2007;64(3):305–15. doi: 10.1001/archpsyc.64.3.305. [DOI] [PubMed] [Google Scholar]
- Wolter K. Introduction to Variance Estimation. New York: Springer-Verlag; 1985. [Google Scholar]
- Zuvekas SH, Taliaferro GS. Pathways to Access: Health Insurance, the Health Care Delivery System, and Racial/Ethnic Disparities, 1996–1999. Health Affairs (Millwood) 2003;22(2):139–53. doi: 10.1377/hlthaff.22.2.139. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.