Abstract
Severe RSV-induced bronchiolitis has been associated with a mixed “Th1” and “Th2” cytokine storm. We hypothesized that differentiation of “alternatively activated” macrophages (AA-Mϕ) would mediate resolution of RSV-induced lung injury. RSV induced IL-4 and IL-13 by murine lung and peritoneal macrophages, IL-4Rα/STAT6-dependent AA-Mϕ differentiation, and significantly enhanced inflammation in lungs of IL-4Rα−/− mice. Adoptive transfer of wild type (WT) macrophages to IL-4Rα−/− mice restored RSV-inducible AA-Mϕ phenotype and diminished lung pathology. RSV-infected TLR4−/− and IFN-β−/− macrophages and mice also failed to express AA-Mϕ markers, but exhibited sustained proinflammatory cytokine production (e.g., IL-12) in vitro and in vivo and epithelial damage in vivo. TLR4 signaling is required for PPARγ expression, a DNA-binding protein that induces AA-Mϕ genes, while IFN-β regulates IL-4, IL-13, IL-4Rα, and IL-10 expression in response to RSV. RSV-infected cotton rats treated with a COX-2 inhibitor increased expression of lung AA-Mϕ. These data suggest new treatment strategies for RSV that promote AA-Mϕ differentiation.
INTRODUCTION
Respiratory Syncytial Virus (RSV) is the most significant cause of serious lower respiratory tract infection in infants and young children worldwide1, and has been identified as an increasing cause of morbidity and mortality in the elderly and immunodeficient. A pathological immune mechanism has long been suspected, based on failed clinical trials of the mid-1960s in which infants vaccinated with a formalin-inactivated (FI) RSV became much sicker or died when RSV was subsequently contracted.2 Induction of a “cytokine storm” underlies the inflammatory pathology associated with severe RSV. 3
RSV first infects airway epithelial cells, inducing an antiviral milieu mediated by IFN-β and IFN-β-inducible genes.4 RSV stimulates TLR4, TLR2, and the intracellular sensors, retinoic acid-induce gene I (RIG-I) and TLR3, leading to induction of many NF-κB-dependent proinflammatory genes.3,5–8 RSV-induced cytokines and chemokines recruit and activate neutrophils, monocytes, eosinophils, basophils, dendritic cells, and T cells9 that, in addition to fixed lung macrophages, produce proinflammatory mediators such as TNF-α and COX-2 that contribute to lung damage and pathology.10 Depletion of lung macrophages in vivo significantly inhibits the early cytokine response to RSV.8,11
“Classically activated” macrophages (CA-Mϕ) differentiate in response to inflammatory stimuli, such as IFN-γ, in combination with TLR activation by microbial stimuli, such as lipolysaccharide (LPS). CA-Mϕ kill intracellular pathogens and secrete inflammatory cytokines that amplify Th1 immune responses. CA-Mϕ are also associated with the pathology seen in many inflammatory diseases and produce iNOS, the enzyme that generates nitric oxide (NO) that can damage cells. “Alternatively activated” macrophages (AA-Mϕ) differentiate in response to Th2 cytokines, IL-4 and IL-13, and are functionally and biochemically distinct from CA-Mϕ. AA-Mϕ produce arginase-1 that competes with iNOS for arginine to produce L-ornithine and urea, rather than NO.12 Murine AA-Mϕ express "markers" not expressed by CA-Mϕ, including “found in inflammatory zone 1” (FIZZ1), Ym1, mannose receptor (MR), and others.13, 14 Macrophages exhibit extraordinary “plasticity” and can alter their differentiation state based on changing environmental signals.
Although much work on the response to RSV has focused on whether a “Th1” or “Th2” adaptive immune response mediates disease, it is surprising that essentially no attention has been paid to RSV-induced differentiation of CA-Mϕ vs. AA-Mϕ since their cytokine profiles mirror that of Th1 and Th2 cells, respectively. Our data support the conclusion that RSV induces alveolar macrophages to produce IL-4 and IL-13 that contribute to AA-Mϕ differentiation and disease resolution through IL-4Rα/STAT6-, TLR4-, and IFN-β-dependent signaling pathways in vitro and in vivo. Thus, the innate, macrophage-mediated, “Th2-like” response that develops early in RSV infection, prior to the development of the adaptive immune response, may represent the host’s initial attempt to mitigate lung damage. Moreover, one’s capacity for eliciting this early response may dictate severity of RSV-mediated disease.
RESULTS
RSV infection induces AA-Mϕ
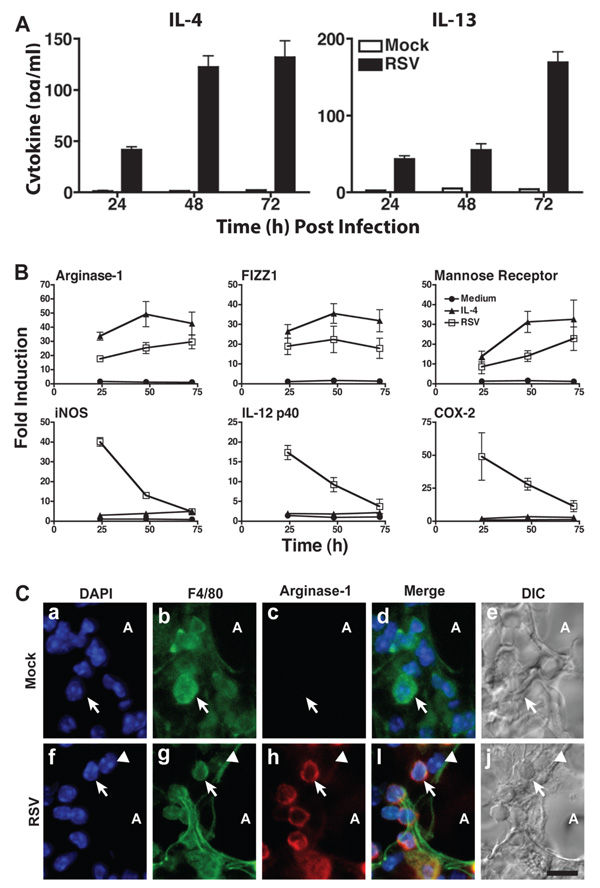
Differentiation of AA-Mϕ requires IL-4 and/or IL-13, cytokines associated with strong Th2 responses. However, Francisella tularensis induces IL-4 and IL-13 in murine primary peritoneal macrophages and in the RAW 264.7 macrophage cell line that develop into AA-Mϕ.15 RSV infection of WT purified murine bronchoalveolar lavage (BAL) macrophages (Fig. 1A), primary peritoneal macrophages, and RAW 264.7 macrophages (Fig. S1A) also induced IL-4 and IL-13 in vitro. Lung tissue homogenized 4 days (d) after RSV infection also contained significantly elevated levels of IL-4 and IL-13 (Fig. S1B). BAL cells derived from mock- or RSV-infected mice 4 d post-infection (p.i.) were enriched for macrophages (see supplemental methods) and stained for DAPI (a nuclear marker), F4/80 (a macrophage marker), and intracellular IL-4. Intracellular IL-4 was detected in the majority of mononuclear F4/80+ cells from RSV-infected mice (Fig. S1C, e–h), and not in macrophages from mock-infected mice (a–d).
Fig. 1. RSV infection induces differentiation of AA-Mϕ.
(A) Highly purified WT BALB/c BAL macrophage cultures were treated with medium only or infected with RSV. Supernatants were collected at the indicated time points and analyzed for IL-4 and IL-13 by ELISA. (B) WT BALB/c BAL macrophages were treated with medium alone, rIL-4, or RSV. Gene expression was analyzed by real-time PCR. Data are means ± SEM from a single representative experiment (N = 4). (C) WT C57BL/6 mice were mock- or RSV-infected and lungs harvested 4 d p.i. Frozen lung sections were stained for nuclei (DAPI; blue), F4/80 (green), and arginase-1 (red), then viewed by confocal microscopy. Arrows are positioned identically on each panel within a treatment to provide a reference point. The arrowhead in panels f–j illustrates a rare cell that is positive for F4/80, but not for arginase-1.
To determine if RSV infection also leads to AA-Mϕ differentiation, purified BAL macrophages (Fig. 1B) or peritoneal exudate macrophages (Fig. S2A) were stimulated in vitro with medium, rIL-4, or RSV-infected. Like rIL-4, RSV induced gene expression for AA-Mϕ markers, e.g., arginase-1, FIZZ1, MR (Fig. 1B), and Ym1 (data not shown) with similar kinetics, while RSV-induced proinflammatory gene expression waned. FACS analysis of RSV-infected mouse (Fig. S2B) or cotton rat (Fig. S2C) peritoneal macrophages revealed increased arginase-1, FIZZ1, and MR protein comparable to that induced by rIL-4. UV-inactivated RSV failed to induce AA-Mϕ mRNA or protein in either species. Figure S2E illustrates that the level of arginase-1 mRNA induced by RSV is comparable to that induced by rIL-4, while that induced by UV-RSV is similar to medium-treated murine macrophages. Fig. S2F confirms this for arginase-1 and FIZZ1 protein expression as measured by FACS.
In vivo, WT mice were mock- or RSV-infected (106 PFU/mouse intranasal (i.n.)) and sacrificed 4 d p.i. Fig. 1C (a–e) shows a representative lung section containing an alveolus from a mock-infected mouse. None of the mononuclear (blue), F4/80+cells (i.e., macrophages; green) expressed arginase-1 (red) (Fig. 1C, a–e). In contrast, RSV induced expression of arginase-1 in the majority of F4/80+macrophages (Fig. 1C, f–j). This was confirmed in BAL cells derived from RSV-infected cotton rats in which both FIZZ1 and arginase-1 mRNA peaked 4 d p.i. (Fig. S2D). Together, this data suggests that both interstitial and alveolar macrophages are capable of producing AA-Mϕ markers during RSV infection. Arginase-1 mRNA was induced equivalently in lungs of in WT and Rag2−/− mice 4 d p.i. (Fig. S3). Thus, RSV infection induces T and B cell-independent differentiation of AA-Mϕ in vitro and in vivo. Moreover, the finding that only mononuclear F4/80+ cells produce the IL-4 and arginase-1 in vivo in lung sections and in BAL cells from infected mice strongly suggests that macrophages, and not other potential sources of IL-4 (e.g., polymorphonuclear eosinophils, basophils), are the primary source of IL-4 in the early response to RSV.
Failure of RSV to Induce AA-Mϕ Prolongs the Proinflammatory Response
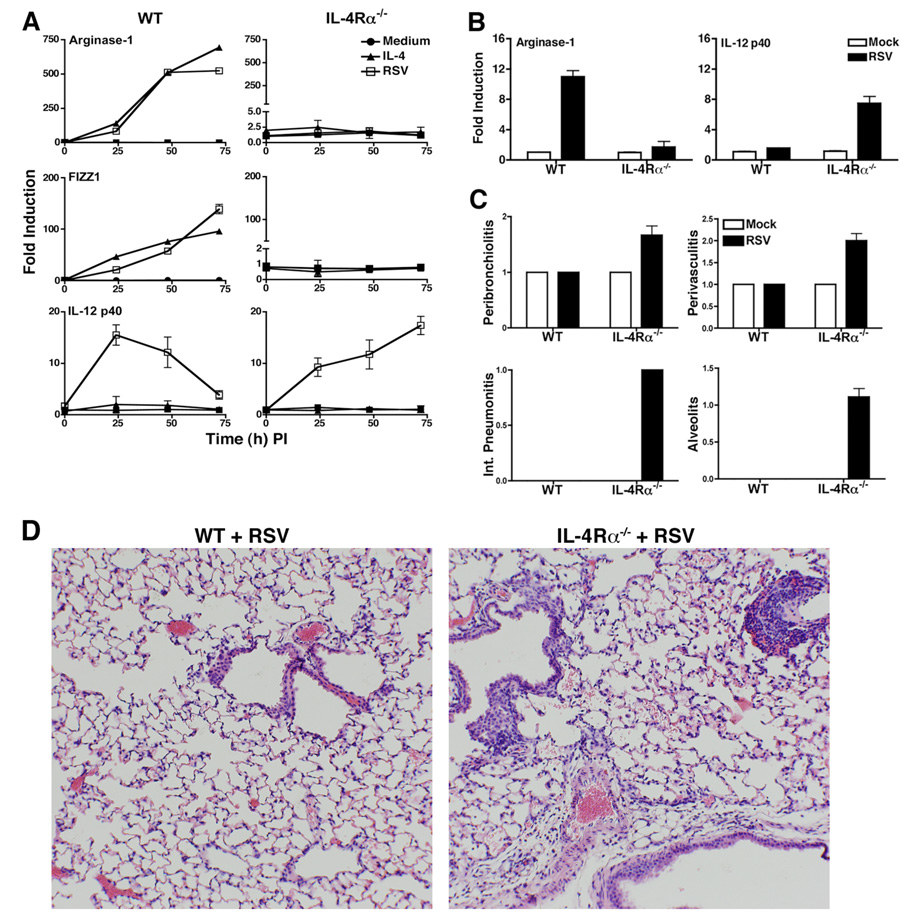
Both IL-4 and IL-13 utilize the IL-4Rα chain16 to activate STAT6-mediated transcription of genes that encode AA-Mϕ markers.17–19 Macrophages from WT BALB/c or IL-4Rα−/− mice were stimulated with medium only, rIL-4, or RSV-infected, followed by analysis of AA-Mϕ and CA-Mϕ gene expression and protein. Arginase-1 and FIZZ1 mRNA (Fig. 2A) and arginase-1 protein (Fig. S4, top graph) were increased comparably in rIL-4- or RSV-infected WT, but not in IL-4Rα−/− macrophages, although low levels of IL-4 and IL-13 were produced by the latter (data not shown). Conversely, RSV-infected IL-4Rα−/− macrophages, but not WT macrophages, expressed sustained steady-state levels of IL-12 p40 mRNA (Fig. 2A, bottom graphs) and iNOS protein (Fig. S4A), both associated with CA-Mϕ. Both COX-2 and iNOS mRNA remained elevated in RSV-infected IL-4Rα−/−, but not WT macrophages (Fig. S4B). No detectable arginase-1 mRNA, but elevated IL-12 p40 mRNA, was confirmed in lungs from IL-4Rα−/− mice (Fig. 2B). Identical results were obtained with STAT6−/− macrophages (data not shown). RSV-infected Rag2−/− x IL-4Rα−/− mice also failed to produce arginase-1 (Fig. S3).
Fig. 2. Failure to induce AA-Mϕ prolongs CA-Mϕ phenotype.
(A) WT BALB/c and IL-4Rα−/− peritoneal macrophages were treated as in Fig. 1 and mRNA expression measured. Data are derived from a single representative experiment (N = 3). (B) WT and IL-4Rα−/− mice were mock- or RSV-infected. Mice were sacrificed 4 d p.i., and arginase-1 and IL-12 p40 mRNA measured in lungs by real-time PCR. (C) WT and IL-4Rα−/− mice were treated as in (B). Lung pathology was scored as described in Methods. Results are compiled from 3 independent experiments. (D) WT and IL-4Rα−/− mice were mock- or RSV-infected. Lungs were harvested 4 d p.i. Lung pathology was scored (N = 4; 4 mice/treatment). Images shown are at 100x.
Other studies of RSV infection in mice have been carried out using more virus than used in our in vivo analyses or immune-deficient mouse strains to elicit frank pathology; however, we used only 106 PFU/mouse to enable us to determine if the lack of specific genes known to regulate the innate immune response contributed to the regulation of RSV-induced pathology. Under these conditions, WT mice exhibit a relatively low level of inflammation after RSV infection. Analysis of lung sections from RSV-infected IL-4Rα−/− mice revealed significantly greater pathology scores (Fig. 2C) for each histological parameter compared to RSV-infected WT mice as seen in the corresponding micrographs (Fig. 2D). Thus, the IL-4Rα-STAT6 signaling axis is required for RSV-induced AA-Mϕ differentiation that mitigates pathology. This is unlikely to be a consequence of differential viral clearance since in WT and all of the mice with targeted mutations used in this study, viral NS1 protein levels peaked one day p.i., declined rapidly thereafter, but remained detectable for 8 d (data not shown).
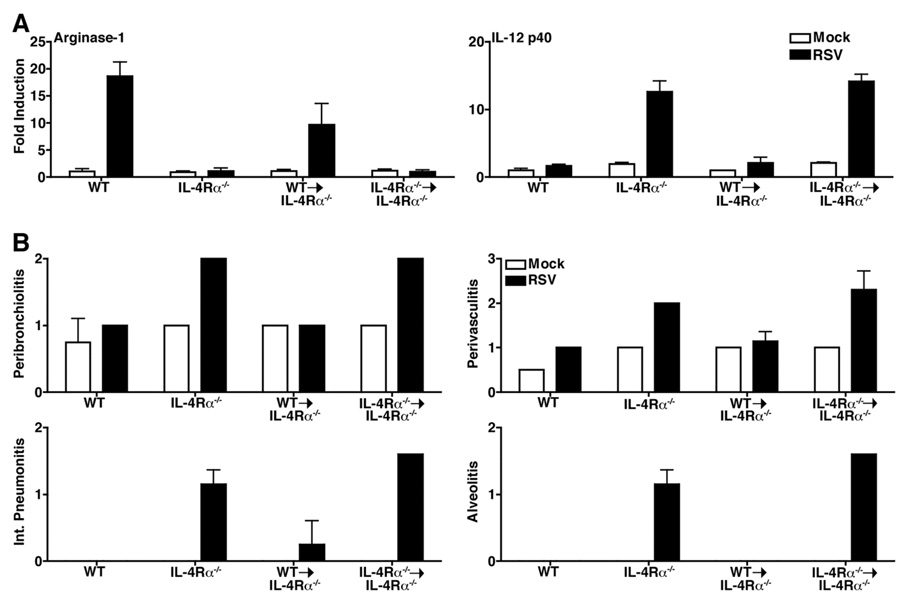
To support the role of AA-Mϕ in the prevention or resolution of RSV-induced disease, purified WT or IL-4Rα−/− macrophages were adoptively transferred to IL-4Rα−/−mice and RSV-infected 5 d later. Lungs of chimeric mice that received WT macrophages (WT→IL-4Rα−/−) expressed IL-4Rα mRNA 4 d p.i. (Fig. S5). This demonstrates that the WT macrophages homed to the lung. These same samples exhibited a 9.5-fold increase in arginase-1 mRNA (Fig. 3A). Conversely, in IL-4Rα−/− mice given IL-4Rα−/−macrophages (IL-4Rα−/−→ IL-4Rα−/−), RSV infection failed to induce arginase-1 mRNA, but induced elevated levels of IL-12 p40 similar to IL-4Rα−/− control mice. FIZZ1 was also increased in the mice that received WT macrophages, while iNOS and COX-2 were elevated in both the IL-4Rα−/− control mice or those that received IL-4Rα−/− macrophages (data not shown). Histological analysis revealed decreased lung pathology in WT→IL-4Rα−/− mice comparable to that seen in WT control mice (Fig. 3B). RSV-infected IL-4Rα−/− control mice and IL-4Rα−/−→ IL-4Rα−/− mice exhibited comparably increased histopathology (Fig. 3B). These data further support a protective or reparative role for AA-Mϕ in RSV-induced pathology.
Fig. 3. Adoptive transfer of WT macrophages reconstitutes AA-Mϕ phenotype in IL-4Rα−/− mice.
(A) WT BALB/c and IL-4Rα−/− mice, along with IL-4Rα−/− mice that received either 1.5 × 107 WT (WT→IL-4Rα−/−) or IL-4Rα−/− (IL-4Rα−/−→IL-4Rα−/−) macrophages i.p., were mock- or RSV-infected 5 d post-transfer. Lungs were harvested 4 d p.i. and analyzed for gene expression by real-time PCR. (B) Lung sections from mice in (A) were H&E stained and scored for lung pathology. Data represent one of 2 separate experiments with similar outcomes (10 mice/treatment).
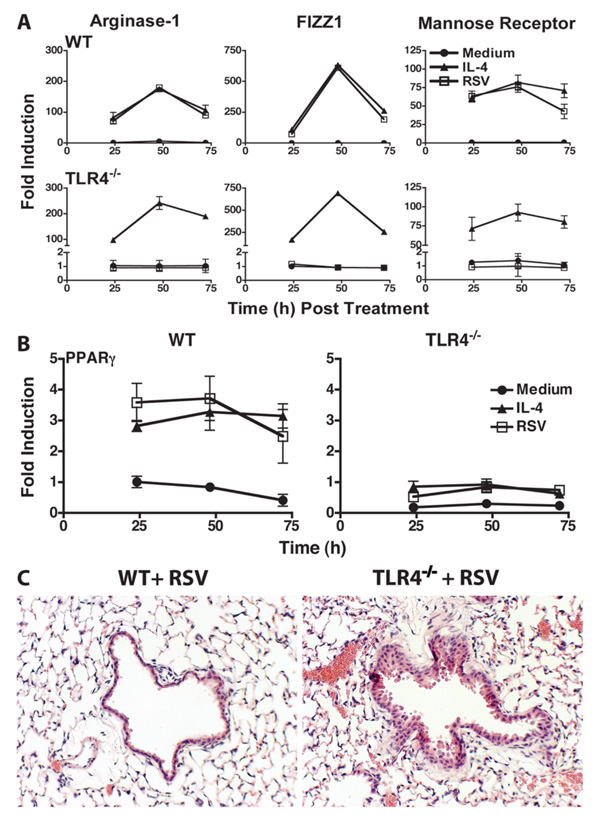
RSV-induced AA-Mϕ differentiation is TLR4- and IFN-β-dependent
RSV activates multiple pattern recognition receptors, including TLR4.5,8,20 RSV failed to elicit arginase-1, FIZZ1, or MR mRNA in TLR4−/− peritoneal macrophages, despite the fact that rIL-4 induced these markers comparably in WT and TLR4−/−macrophages (indicating that IL-4Rα was fully functional in TLR4−/− macrophages) (Fig. 4A). In contrast, induction of IFN-β, COX-2, and iNOS mRNA by RSV-infected TLR4−/−macrophages was not affected (Fig. S6A), supporting a previous report that RSV induces IFN-β primarily through RIG-I.7 RSV-infection of TLR4−/− mice also failed to induce arginase-1 mRNA in the lungs, but exhibited increased expression of IL-12 p40 mRNA compared to WT mice (Fig. S6B). PPARγ, a nuclear hormone receptor that regulates AA-Mϕ differentiation and infiltration21–23, was down-regulated basally and in RSV-infected TLR4−/− macrophages (Fig. 4B) and in the lungs of RSV-infected TLR4−/− mice (data not shown). RSV-infected TLR4−/− mice exhibited bronchiolar epithelial hyperplasia and some metaplasia with moderate increases in peribronchiolar and perivascular inflammation, compared to infected WT lungs (Fig. 4C).
Fig. 4. Differentiation of AA-Mϕ by RSV is TLR4-dependent.
(A) WT C57BL/6 and TLR4−/− peritoneal macrophages were treated as indicated in Fig. 1 and analyzed for mRNA gene expression by real-time PCR (N = 3). (B) WT and TLR4−/− macrophages were treated as in (A) and analyzed for PPARγ mRNA gene expression by real-time PCR. (C) WT and TLR4−/− mice were mock- or RSV-infected. Lungs were harvested 4 d p.i. Lung pathology was scored (N = 4; 4 mice/treatment). Images shown are at 200x.
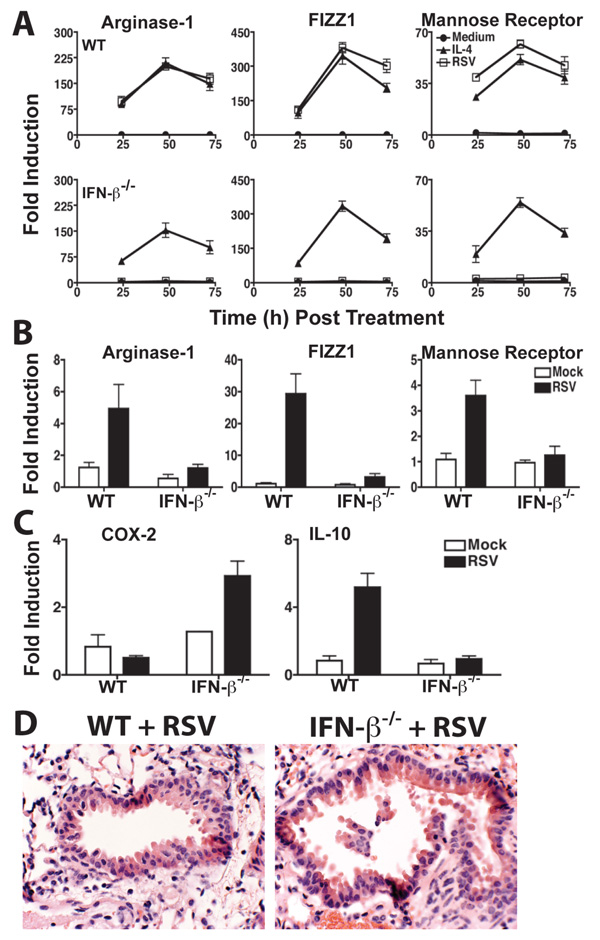
IFN-β is a potent antiviral cytokine associated with recovery from RSV infection. As observed for TLR4−/− macrophages (Fig. 4A), RSV failed to induce expression of AA-Mϕ genes in IFN-β−/− macrophages (Fig. 5A) or in vivo (Fig. 5B). Expression of the antiinflammatory cytokine, IL-10, was significantly decreased in IFN-β−/− lung mRNA samples, while COX-2 mRNA, previously associated with RSV-induced pathology10, was significantly increased (Fig. 5C). These findings were confirmed in RSV-infected WT and IFN-β−/− macrophages (data not shown). RSV-infected IFN-β−/− mice also exhibited enhanced lung pathology, characterized by hyperplasia and excess epithelial shedding, as well as minor peribronchiolitis and perivasculitis (Fig. 5D).
Fig. 5. RSV-induced AA-Mϕ and IL-10 production are IFN-β-dependent.
(A) WT and IFN-β−/− peritoneal macrophages were treated as indicated and analyzed for mRNA by real-time PCR (N = 2). (B) WT or IFN-β−/− mice were mock- or RSV-infected. At 4 d p.i., mice were sacrificed and lungs analyzed for arginase-1, FIZZ1, and MR mRNA. (C) IL-10 and COX-2 mRNA were measured in the lungs of RSV-infected mice (see legend to (B)). (C) Mice were infected as in (B) and lungs fixed and stained with H&E 4 d p.i. (N = 4; 4 mice/treatment). Images shown are at 400x.
TLR4−/− macrophages responded to RSV with WT levels of IL-4 and IL-13 mRNA through 48 h, with a precipitous loss of IL-4 mRNA at 72 h (Fig. S6C), but no effect on levels of IL-4Rα mRNA (Fig. S6D). Notably, RSV-infected IFN-β−/−macrophages produced significantly less IL-4 and IL-13 than WT macrophages at all time points (Fig. S7A, top graphs), a finding confirmed in vivo (Fig. S7A, bottom graphs). IFN-β−/− mice also exhibited significantly diminished expression of lung IL-4Rα mRNA than WT mice that was not altered by RSV infection (Fig. S7B). rIFN-β or RSV infection of WT macrophages increased IL-4Rα mRNA expression at 24 h p.i. and declined thereafter (Fig. S7C). Thus, together, TLR4 and IFN-β, regulate levels of PPARγ, IL-4, IL-13, and the IL-4Rα chain that are required for AA-Mϕ differentiation and amelioration of lung epithelial damage.
AA-Mϕ in re-infection and in response to COX-2 inhibitors
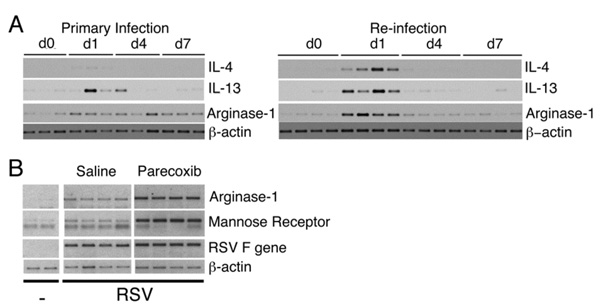
In humans, re-infection with RSV is common. To examine the effect of reinfection on AA-Mϕ differentiation, cotton rats were infected once or twice (60 d later) with RSV. Cotton rats are a preferred model of RSV infection because, compared to mice, the pathology is more similar to that seen in humans.24,25 IL-4 and IL-13 mRNA were detected in the lungs during primary infection, but these genes, as well as arginase-1 mRNA, were more strongly activated after re-infection (Fig. 6A). These data are consistent with the faster resolution of inflammation seen in secondary infection of cotton rats.26
Fig. 6. Rapid activation of AA-Mϕ in cotton rats during re-infection and in response to COX-2 inhibition.
(A) Cotton rats (4/group) were administered saline or infected with RSV. Animals were then RSV-infected 60 d after initial treatment. Lungs were harvested, total RNA isolated, and analyzed for IL-4, IL-13, and arginase-1 mRNA by RT-PCR and Southern blotting. (B) Cotton rats were mock- or RSV-infected. Infected rats were treated on day 3 p.i. with vehicle (saline) or paracoxib (100 mg/kg) i.p. All animals were sacrificed 4 d p.i. and lung samples evaluated for mRNA expression for the indicated genes. Each lane represents RNA from one cotton rat and results are representative of 3 separate experiments.
Parecoxib, a non-steroidal anti-inflammatory drug, specifically inhibits COX-2-, but not COX-1-mediated, production of prostaglandins (PGs).27 To test the hypothesis that COX-2 production and AA-Mϕ differentiation are inversely regulated, cotton rats were infected with RSV, and then treated with saline or parecoxib. RSV-infected cotton rats treated with saline exhibited increased arginase-1 and MR mRNA 4 d p.i.; however, RSV-infected cotton rats treated with parecoxib exhibited much stronger induction of these AA-Mϕ markers (Fig. 6B). This suggests that COX-2 production inhibits AA-Mϕ differentiation, thereby reducing the capacity of AA-Mϕ to effect tissue repair in the lung.
DISCUSSION
RSV elicits rapid production of proinflammatory cytokines and chemokines, IFN-β3,8,9, and COX-2, previously implicated in RSV-induced lung pathology.10 However, counter-regulatory cytokines, e.g., IL-4, IL-13, and IL-10, are also produced during RSV infection. Our data strongly support a central role for IL-4/13-induced AA-Mϕ in the mitigation of lung pathology induced by RSV. AA-Mϕ-produced arginase-1, MR, FIZZ1, and Ym1 have long been implicated in lung repair and remodeling after infection18,28,29, consistent with our observation that in IL-4Rα−/− mice, RSV-induced inflammation is significantly worsened. Coupled with the observation that passive transfer of WT macrophages reversed the phenotype of the IL-4Ra−/− mice with respect to cytokine production, AA-Mϕ differentiation, and pathology, our data implicate AA-Mϕ as central effectors in the regulation of RSV-induced lung damage. NS-1 mRNA, the first RSV gene transcribed, peaked at 1 day p.i. and then waned (data not shown), and similar kinetics were observed in all of the strains of mice studied. Thus, while viral replication was controlled by a very early immune response, control of lung pathology depends on the later development of AA-Mϕ.
While RSV-induced IL-4 and IL-13 have been largely attributed to Th2 cells9, both are produced by other cell types including macrophages15,30 and basophils.31 That IL-4 and IL-13 are induced in RSV-infected lung, peritoneal, or cell line-derived macrophages in vitro and BAL and interstitial lung macrophages in vivo, even in Rag2−/−mice, suggests that these cytokines are present prior to the generation of an adaptive Th2 immune response and act in an autocrine/paracrine manner to induce or sustain the AA-Mϕ phenotype. Although prior studies have implicated basophils and eosinophils as a source of IL-49, our immunocytochemistry results indicate that the IL-4- and arginase-1-producing cells are clearly both mononuclear and F4/80+, indicating that these are interstitial or infiltrating macrophages. While Moore et al. showed that depletion of basophils in RSV-infected mice reduced lung IL-4 expression31, their analysis was carried out at 7 d p.i., and not at 4 d, the time at which we find that macrophages are a major source of IL-4. Signaling through IL-4Rα is required for both RSV-induced AA-Mϕ differentiation and to limit pathology, and our data suggests that the balance of pro-and anti-inflammatory cytokines dictates disease severity. The finding that adoptive transfer of highly purified, WT macrophages to IL-4Rα−/− mice reversed the IL-4Rα−/−phenotype, at the level of AA-Mϕ marker expression, cytokine production, and pathology, strengthens the concept that AA-Mϕ, rather than basophils, limit RSV-induced lung damage. This macrophage-dependent, IL-4Rα- and STAT6-dependent response to RSV contrasts with a non-STAT6-dependent pathway for AA-Mϕ described for M. tuberculosis.32
Both TLR4 and IFN-β contribute to RSV-induced AA-Mϕ in vitro and in vivo, since AA-Mϕ fail to develop in TLR4−/− or IFN-β−/− macrophages, accompanied by increased RSV-induced epithelial damage compared to WT mice (Fig. 4 and Fig. 5). TLR4 signaling was not required for RSV-induced IFN-β (Fig. S6A). At this time, the TLR4 ligand(s) that induce AA-Mϕ differentiation in RSV infection is(are) not known. Kurt-Jones et al.5 reported that RSV fusion protein is a TLR4 agonist and Imai et al. demonstrated that in response to influenza infection, host-derived phospholipids are generated and act as TLR4 agonists.33 Haeberle et al.8 showed that mice depleted of alveolar macrophages or that lack TLR4 fail to activate NF-κB early in infection. Recently, Odegaard et al.21 reported that the PPARγ/retinoic X receptor heterodimer is the primary transactivating factor for arginase-1 expression. Furthermore, Coste et al.22 showed that PPARγ promotes MR expression on macrophages via IL-13 induction of the PPARγ ligand, 15d–PGJ2. PPARγ-deficient macrophages showed reduced arginase-1 expression and activity in response to IL-4, and failed to respond to IL-4 to counteract secretion of LPS-induced pro-inflammatory cytokines. TLR4-mediated PPARγ expression has been reported in colonic epithelial cells.34 That untreated or RSV-infected TLR4−/− macrophages express reduced PPARγ mRNA (Fig. 4B) suggests a molecular mechanism by which AA-Mϕ fail to be induced by RSV infection of TLR4−/− mice and macrophages, even though IL-4 and IL-13 were produced at WT levels. Recently, Malur et al. showed that the deletion of PPARγ in alveolar macrophages causes a skewing towards a Th1 pulmonary inflammatory response.35 The precipitous drop in IL-4 production at 72 h p.i. in RSV-infected TLR4−/− macrophages could also contribute to a failure to develop AA-Mϕ.
Failed clinical trials in the mid-1960s revealed that children immunized with FI-RSV exhibited much more severe disease than in children who were not immunized. Previous studies from our laboratories first pointed to an important role for TLR4 signaling in the mitigation of RSV-induced enhanced lung injury.3 Cotton rats immunized with the FI-RSV vaccine experience “enhanced disease” mediated by a “cytokine storm” in response to RSV infection in which both “Th1” and “Th2” type cytokines are produced. However, co-administration of FI-RSV with the non-toxic, TLR4 agonist, monophosphoryl lipid A, counteracted the enhanced pathology and overexuberant gene expression profile induced by RSV in FI-RSV-vaccinated animals.
Our data presented herein also reveal that IFN-β contributes to induction of AA-Mϕ through regulation of IL-4, IL-13, and IL-4Rα (Fig. S5B, C). Elevated COX-2 in RSV-infected IFN-β−/− mice (Fig. 5) extends previous findings of mitigated RSV-induced lung pathology by COX-2 inhibition and that COX-2−/− mice exhibit less pathology in response to influenza.10,36 That COX-2 inhibition by paracoxib increased arginase-1 mRNA in vivo (Fig. 6) suggests a previously unappreciated negative feedback mechanism.
Differentiation of AA-Mϕ in response to RSV may result in a cytokine milieu that dictates the course of the adaptive Th1/Th2 response to subsequent infection. Didierlaurent et al. showed that primary infection of mice with influenza or RSV led to alveolar macrophages that, even months after infection, failed to respond to TLR agonists.37 Thus, the anti-inflammatory state induced by RSV-driven AA-Mϕ may persist for an extended period of time, suggesting that such macrophages mediate a prolonged anti-inflammatory state that limits inflammation induced by subsequent RSV infection.4,26,38 RSV infection in young children can lead to chronic airway diseases such as asthma.39 Kim et al. recently showed that in response to Sendai virus, a virus related to RSV, mice exhibited increased airway hyperreactivity that was maximal 49 d after infection.40 Long-term production of AA-Mϕ products, such as arginase-1, FIZZ1, and Ym1, may also contribute to chronic airway diseases such as asthma through lung remodeling.41
In this study, we confirmed a report showing induction of IL-10 during RSV infection.3 Based on its well-characterized anti-inflammatory actions, IL-10 would be expected to counteract production of proinflammatory cytokines and, thereby, facilitate disease resolution. That IL-10 is poorly induced in RSV-infected IFN-β−/− mice (Fig. 5C) and macrophages (data not shown) supports a previous report that IFN-β is required for the induction of IL-1042 and suggests a novel role for IFN-β in AA-Mϕ differentiation. Thus, the balance of “Th1”- and “Th2”-type cytokines is critical for maintaining a balance between the damage induced by viruses such as RSV and sensitization to subsequent allergic triggers.
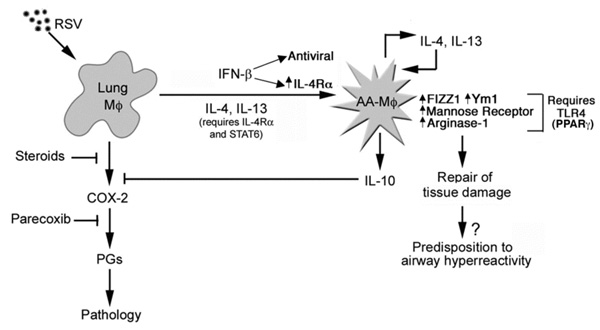
Fig. 7 presents a model supported by our findings. While airway epithelial cells are the initial target of RSV infection, RSV also infects lung macrophages, leading to the early release of potent cytokines and chemokines that recruit inflammatory cell types (including monocytes) and increase levels of inflammatory cytokines and COX-2 that mediate pathology.10,43 Later in infection, AA-Mø differentiation, a process that is IL-4Rα-, TLR4-, and IFN-β-dependent, counteracts the early inflammatory response, in part through (i) the anti-inflammatory effects of IL-10 on cytokine production, (ii) TLR4-induced PPARγ, (iii) IFN-β-induced IL-4, IL-13, and IL-4Rα, and (iv) repair of tissue damage through induction of enzymes such as FIZZ1, Ym1, and arginase-1. However, if the AA-Mϕ phenotype persists, it may lead to an adaptive immune response that is “Th2”-skewed, leading to hypersensitivity to allergic triggers as observed in children who have had RSV infection early in life.
Fig. 7. Hypothetical model for the role of AA-Mϕ during RSV infection.
METHODS
Reagents
Isotype control antibodies and fluorescently labeled secondary antibodies were purchased: mouse IgG2a and IgG1, rat IgG2b, goat IgG, and rabbit IgG (Sigma, St. Louis, MO); Cy2-conjugated donkey anti-rabbit IgG, Cy2-conjugated donkey anti-mouse IgG, donkey anti-rat biotin, Cy2-conjugated streptavidin, Cy3-conjugated donkey anti-mouse IgG, and Cy3-conjugated donkey anti-goat IgG (Jackson ImmunoResearch Labs).
RSV Long strain (group A) was obtained from American Type Culture Collection (Manassas, VA), and propagated as described.4 Parecoxib was obtained from Exim-Pharm International, Mumbai, India.
Mice and macrophage cell cultures
Six to 8-week old, WT C57BL/6J and BALB/cByJ mice were purchased (Jackson Laboratory, Bar Harbor, ME). TLR4−/− mice (provided by Shizuo Akira, Osaka, Japan) and IFN-β−/− mice (provided by Eleanor Fish, Toronto, Canada), both on a C57BL/6 background, and IL-4Rα−/− mice (BALB/c background; provided by Nancy Noben-Trauth (Rockville, MD) and William Paul (Bethesda, MD)) were bred in UMB’s accredited facility. Rag2−/− mice (BALB/c background) were purchased from Taconic (Rockville, MD). Inbred cotton rats (Sigmodon hispidus) were bred at Virion Systems, Inc. (Rockville, MD). All animal experiments were conducted with institutional approval.
Highly purified (>97%) murine or cotton rat thioglycollate-elicited peritoneal macrophages, and murine BAL (>98%) macrophages were enriched as described in supplemental methods. Macrophages were plated in 6-well (4 × 106 cells/well), 12-well (2 × 106 cells/well for peritoneal or RAW 264.7 macrophages), and 24-well (2.5 × 105 cells/well for BAL macrophages) tissue culture plates. Due to the low yield of BAL macrophages, most experiments were performed with peritoneal macrophages. Macrophages were stimulated with medium alone, or murine or cotton rat rIL-4 (40 ng/ml; R&D Systems, Inc.), or infected with RSV (multiplicity of infection = 2) and incubated at 37° C for the indicated times.
Cytokine Measurements
Cytokine levels were measured by ELISA (Cytokine Core Laboratory, UMB).
Real-time PCR
Total RNA isolation and real-time PCR were performed as described.8,44,45 Levels of mRNA for specific genes are reported as relative gene expression normalized to medium-treated samples.
Analysis of gene expression in lungs of cotton rats was performed by RT-PCR and Southern analysis.4,46 Cotton rat primers are listed in supplemental methods.
Viral infection and tissue processing
To detect arginase-1 in situ, lungs were inflated and perfused with 0.9% saline followed by 4% PFA, then post-fixation for 4 h, washed in 0.1 M phosphate buffer (PB) for 15 min, and placed in 30% sucrose in 0.1 M PB for 48 h at 4° C. Lungs were embedded in Tissue-Tek optimal cutting compound (OTC; Sakurak Finetek, Torrance, CA), frozen on dry ice-cooled isopentane, and stored at −70° C until sectioning.
Intracellular staining and confocal microscopy
Lung sections were incubated for 30 min with PBST (PB, 1% BSA, 1% normal donkey serum, 0.3% Triton X-100) at RT. F4/80 was visualized by immunofluorescence using rat MAb against the C-terminus of mouse F4/80, followed by Cy2-conjugated donkey anti-rat IgG. Arginase-1 was detected using a MAb IgG2b against mouse arginase-1 (BD Bioscience, San Jose, CA), followed by a Cy3-conjugated donkey anti-mouse IgG. Nuclei were visualized using DAPI stain. Coverslips were mounted on slides using an anti-fading fluorescent mounting medium and viewed with an Olympus FluoView 500 confocal microscope (60x, NA 1.4 objective) fitted with standard excitation and emission filters for the visualization of UV, Cy2, and Cy3.
Macrophage Transfer Experiments
WT and IL-4Rα−/− peritoneal exudate macrophages (>98% F4/80+) were enriched and cultured as described in Supplemental Methods. Plates were placed on an ice bath for 15 min and cells were detached with a rubber policeman, centrifuged, and resuspended in saline. IL-4Rα−/− mice were injected i.p. with 1.5 × 107 WT or IL-4Rα−/−macrophages as described.47 Five d later, control (untreated WT or IL-4Rα−/−) or chimeric mice were infected with RSV (106 pfu/animal i.n.). Lungs were harvested 4 d later for RNA and histopathology.
Histopathology
Fixed sections (10 µm) of paraffin-embedded lungs were stained with hematoxylin and eosin (H&E). Four inflammatory parameters were scored independently from 0 – 4 for each section26: peribronchiolitis (inflammatory cells, primarily lymphocytes, surrounding a bronchiole), perivasculitis (inflammatory cells, primarily lymphocytes, surrounding a blood vessel), alveolitis (inflammatory cells within alveolar spaces), and interstitial pneumonitis (increased thickness of alveolar walls associated with inflammatory cells). Slides were randomized, read blindly, and scored for each. Epithelial damage was also evaluated.
Statistics
Statistical differences between two groups were determined using an unpaired, two-tailed Student’s t test with significance set at p <0.05. For comparisons between three or more groups, analysis was done by one-way ANOVA followed by a Tukey’s multiple comparison test with significance determined at p < 0.05.
Supplementary Material
Acknowledgements
This work was supported by NIH grants AI-057575 (JB), AI-18797 (SNV), and AI-38985 and AI59775 (ADK).
Dr. Prince is President, and CEO of VSI. Dr. Blanco and Ms. Pletneva are fulltime employees of VSI. VSI performs contracted research for AstraZeneca, and receives royalty income from the sale of Synagis®. Neither Dr. Blanco nor Ms. Pletneva derives financial benefit from AstraZeneca. No other potential conflict of interest was reported.
Footnotes
Supplemental Data
Supplemental data include 7 Figs. and expanded experimental procedures.
References
- 1.Welliver RC. Review of epidemiology and clinical risk factors for severe respiratory syncytial virus (RSV) infection. J. Pediatr. 2003;143:S112–S117. doi: 10.1067/s0022-3476(03)00508-0. [DOI] [PubMed] [Google Scholar]
- 2.Blanco JCG, Boukhvalova M, Pletneva L, Prince GA, Vogel SN. Rethinking respiratory syncytial virus vaccines. Recent Res. Devel. Experimental Med. 2004;1:75–94. Appendix 1. [Google Scholar]
- 3.Boukhvalova MS, Prince GA, Soroush L, Harrigan DC, Vogel SN, Blanco JC. The TLR4 agonist, monophosphoryl lipid A, attenuates the cytokine storm associated with respiratory syncytial virus vaccine-enhanced disease. Vaccine. 2006;24:5027–5035. doi: 10.1016/j.vaccine.2006.03.064. [DOI] [PubMed] [Google Scholar]
- 4.Pletneva LM, Haller O, Porter DD, Prince GA, Blanco JC. Interferon-inducible Mx gene expression in cotton rats: cloning, characterization, and expression during influenza viral infection. J. Interferon Cytokine Res. 2006;26:914–921. doi: 10.1089/jir.2006.26.914. [DOI] [PubMed] [Google Scholar]
- 5.Kurt-Jones EA, et al. Pattern recognition receptors TLR4 and CD14 mediate response to respiratory syncytial virus. Nat. Immunol. 2000;1:398–401. doi: 10.1038/80833. [DOI] [PubMed] [Google Scholar]
- 6.Murawski MR, et al. Respiratory syncytial virus activates innate immunity through Toll-like receptor 2. J. Virol. 2009;83:1492–1500. doi: 10.1128/JVI.00671-08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Liu P, Jamaluddin M, Li K, Garofalo RP, Casola A, Brasier AR. Retinoic acid-inducible gene I mediates early antiviral response and Toll-like receptor 3 expression in respiratory syncytial virus-infected airway epithelial cells. J. Virol. 2007;81:1401–1411. doi: 10.1128/JVI.01740-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Haeberle HA, et al. Respiratory syncytial virus-induced activation of nuclear factor-kappaB in the lung involves alveolar macrophages and toll-like receptor 4-dependent pathways. J. Infect. Dis. 2002;186:1199–1206. doi: 10.1086/344644. [DOI] [PubMed] [Google Scholar]
- 9.Bueno SM, et al. Host immunity during RSV pathogenesis. International Immunopharmocology. 2008;8:1320–1329. doi: 10.1016/j.intimp.2008.03.012. [DOI] [PubMed] [Google Scholar]
- 10.Richardson JY, et al. Respiratory syncytial virus (RSV) infection induces cyclooxygenase 2: a potential target for RSV therapy. J. Immunol. 2005;174:4356–4364. doi: 10.4049/jimmunol.174.7.4356. [DOI] [PubMed] [Google Scholar]
- 11.Pribul PK, et al. Alveolar macrophages are a major determinant of early responses to viral lung infection but do not influence subsequent disease development. J. Virol. 2008;82:4441–4448. doi: 10.1128/JVI.02541-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Munder M, Eichmann K, Morán JM, Centeno F, Soler G, Modelell M. Th1/Th2-regulated expression of arginase isoforms in murine macrophages and dendritic cells. J. Immunol. 1999;163:3771–3777. [PubMed] [Google Scholar]
- 13.Gordon S. Alternative activation of macrophages. Nat. Rev. Immunol. 2003;3:23–35. doi: 10.1038/nri978. [DOI] [PubMed] [Google Scholar]
- 14.Raes G, Noël W, Beschin A, Brys L, DeBaetselier P, Gholamreza Hassandsadeh G. FIZZ1 and Ym as tools to discriminate between differentially activated macrophages. Develop. Immunol. 2002;9:151–159. doi: 10.1080/1044667031000137629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Shirey K, Cole LE, Keegan AD, Vogel SN. Francisella tularensis live vaccine strain induces macrophage alternative activation as a survival mechanism. J. Immunol. 2008;181:4159–4167. doi: 10.4049/jimmunol.181.6.4159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kelly-Welch AE, Hanson EM, Boothby MR, Keegan AD. Interleukin-4 and interleukin-13 signaling connection maps. Science. 2003;300:1527–1528. doi: 10.1126/science.1085458. [DOI] [PubMed] [Google Scholar]
- 17.Stein M, Keshav S, Harris N, Gordon S. IL-4 potently enhances murine macrophage mannose receptor activity; a marker for alternative immunologic macrophage activation. J. Exp. Med. 1992;176:287–292. doi: 10.1084/jem.176.1.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Welch JS, Escoubet-lozach L, Sykes DB, Liddiard K, Greaves DR, Glass CK. TH2 cytokines and allergic challenge induce Ym1 expression in macrophages by a STAT6-dependent mechanism. J. Biol. Chem. 2002;277:42821–42829. doi: 10.1074/jbc.M205873200. [DOI] [PubMed] [Google Scholar]
- 19.Liu T, et al. Regulation of found in inflammatory zone 1 expression in bleomycin-induced lung fibrosis: role of IL-4/IL-13 and mediation via STAT-6. J. Immunol. 2004;173 doi: 10.4049/jimmunol.173.5.3425. 3425–3421. [DOI] [PubMed] [Google Scholar]
- 20.Haynes LM, Moore DD, Kurt-Jones EA, Finberg RW, Anderson LJ, Tripp RA. Involvement of toll-like receptor 4 in innate immunity to respiratory syncytial virus. J. Virol. 2001;75:10730–10737. doi: 10.1128/JVI.75.22.10730-10737.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Odegaard JI, et al. Macrophage-specific PPARγ controls alternative activation and improves insulin resistance. Nature. 2007;447:1116–1120. doi: 10.1038/nature05894. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Coste A, et al. PPARγ promotes mannose receptor gene expression in murine macrophages and contributes to the induction of this receptor by IL-13. Immunity. 2003;19:329–339. doi: 10.1016/s1074-7613(03)00229-2. [DOI] [PubMed] [Google Scholar]
- 23.Stienstra R, Duval C, Keshtkar S, van der Laak J, Kersten S, Müller M. Peroxisome proliferator-activated receptor γ activation promotes infiltration of alternatively activated macrophages into adipose tissue. J Biol. Chem. 2008;283:22620–22627. doi: 10.1074/jbc.M710314200. [DOI] [PubMed] [Google Scholar]
- 24.Prince GA, Jenson AB, Horswood RL, Camargo E, Chanock RM. The pathogenesis of respiratory syncytial virus infection in cotton rats. Am. J. Pathol. 1978;93:771–791. [PMC free article] [PubMed] [Google Scholar]
- 25.Prince GA, Curtis SJ, Yim KC, Porter DD. Vaccine-enhanced respiratory syncytial virus disease in cotton rats following immunization with Lot 100 or a newly prepared reference vaccine. J. Gen. Virol. 2001;82:2881–2888. doi: 10.1099/0022-1317-82-12-2881. [DOI] [PubMed] [Google Scholar]
- 26.Prince GA, Prieels JP, Slaoui M, Porter DD. Pulmonary lesions in primary respiratory syncytial virus infection, reinfection, and vaccine-enhanced disease in the cotton rat (Sigmodon hispidus) Lab. Invest. 1999;79:1385–1392. [PubMed] [Google Scholar]
- 27.McMurray RW, Hardy KJ. Cox-2 inhibitors: today and tomorrow. Am. J. Med. Sci. 2002;323:181–189. doi: 10.1097/00000441-200204000-00003. [DOI] [PubMed] [Google Scholar]
- 28.Albina JE, Mills CD, Henry WL, Jr, Caldwell MD. Temporal expression of different pathways of l-arginine metabolism in healing wounds. J. Immunol. 1990;144:3877–3880. [PubMed] [Google Scholar]
- 29.Kodelja V, Muller C, Tenorio S, Schebesch C, Orfanos CE, Goerdt S. Differences in angiogenic potential of classically vs alternatively activated macrophages. Immunobiology. 1997;197:478–493. doi: 10.1016/S0171-2985(97)80080-0. [DOI] [PubMed] [Google Scholar]
- 30.Varin A, Gordon S. Alternative activation of macrophages: Immune function and cellular biology. Immunobiology. 2009;214 doi: 10.1016/j.imbio.2008.11.009. 630–241. [DOI] [PubMed] [Google Scholar]
- 31.Moore ML, et al. STAT1 negatively regulates lung basophil IL-4 expression induced by Respiratory Syncytial Virus infection. J. Immunol. 2009;183:2016–2026. doi: 10.4049/jimmunol.0803167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.El Kasmi KC, et al. Toll-like receptor-induced arginase 1 in macrophages thwarts effective immunity against intracellular pathogens. Nat. Immunol. 2008;9:1399–1406. doi: 10.1038/ni.1671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Imai Y, et al. Identification of oxidative stress and Toll-like receptor 4 signaling as a key pathway of acute lung injury. Cell. 2008;133:235–249. doi: 10.1016/j.cell.2008.02.043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dubuquoy L, et al. Impaired expression of peroxisome proliferator-activated receptor γ in ulcerative colitis. Gastro. 2003;124:1265–1276. doi: 10.1016/s0016-5085(03)00271-3. [DOI] [PubMed] [Google Scholar]
- 35.Malur A, et al. Deletion of PPARγ in alveolar macrophages is associated with a Th-1 pulmonary inflammatory response. J. Immunol. 2009;182:5816–5822. doi: 10.4049/jimmunol.0803504. [DOI] [PubMed] [Google Scholar]
- 36.Carey MA, Bradbury JA, Seubert JM, Langenbach R, Zeldin DC, Germolec DR. Contrasting effects of cyclooxygenase-1 (COX-1) and COX-2 deficiencey on the host response to Influenza A viral infection. J. Immunol. 2005;175:6878–6884. doi: 10.4049/jimmunol.175.10.6878. [DOI] [PubMed] [Google Scholar]
- 37.Didierlaurent A, et al. Sustained desensitization to bacterial Toll-like receptor ligands after resolution of respiratory influenza infection. J. Exp. Med. 2008;205:323–329. doi: 10.1084/jem.20070891. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Boukhvalova MS, Prince GA, Blanco JC. Respiratory syncytial virus infects and abortively replicates in the lungs in spite of preexisting immunity. J. Virol. 2007;81:944–950. doi: 10.1128/JVI.00102-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Sigurs N, Bjarnason R, Sigurbergsson F, Kjellman B, Bjorksten B. Asthma and immunoglobulin E antibodies after respiratory syncytial virus bronchiolitis: a prospective cohort study with matched controls. Pediatrics. 1995;95:500–505. [PubMed] [Google Scholar]
- 40.Kim EY, et al. Persistent activation of an innate immune response translates respiratory viral infection into chronic lung disease. Nat. Med. 2008;14:633–640. doi: 10.1038/nm1770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Anthony RM, Rutizky LI, Urban JF, Jr, Stadecker MJ, Gause WC. Protective immune mechanism in helminth infection. Nat. Rev. Immunol. 2007;7:975–987. doi: 10.1038/nri2199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Chang EY, Guo B, Doyle SE, Cheng G. Cutting Edge: Involvement of the type I IFN production and signaling pathway in lipopolysaccharide-induced IL-10 production. J. Immunol. 2007;178:6707–6709. doi: 10.4049/jimmunol.178.11.6705. [DOI] [PubMed] [Google Scholar]
- 43.Prince GA, Mathews A, Curtis SJ, Porter DD. Treatment of respiratory syncytial virus bronchiolitis and pneumonia in a cotton rat model with systemically administered monoclonal antibody (Palivizumab) and glucocorticosteriod. J. Infect. Dis. 2000;182:1326–1330. [Google Scholar]
- 44.Cuesta N, Salkowski CA, Thomas KE, Vogel SN. Regulation of lipopolysaccharide sensitivity by IFN regulatory factor-2. J. Immunol. 2003;170:5739–5747. doi: 10.4049/jimmunol.170.11.5739. [DOI] [PubMed] [Google Scholar]
- 45.Cole LE, et al. Immunological consequences of Francisella tularensis live vaccine strain infection: role of the innate immune response in infection and immunity. J. Immunol. 2006;176:6888–6899. doi: 10.4049/jimmunol.176.11.6888. [DOI] [PubMed] [Google Scholar]
- 46.Blanco JC, Pletneva L, Boukhvalova M, Richardson JY, Harris KA, Prince GA. The cotton rat: an underutilized animal model for human infectious diseases can now be exploited using specific reagents to cytokine, chemokines and interferons. J. Interferon Cytokine Res. 2004;24:21–28. doi: 10.1089/107999004772719873. [DOI] [PubMed] [Google Scholar]
- 47.Ford AQ, Smith E, Noben-Trauth N, Keegan AD. Alternatively Activated Macrophages Participate in the Recruitment of Eosinophils to the Lung in a Murine Model of Allergic Lung Inflammation. Suppl. J. Immunol. 2009 April;182 79.2. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.