Abstract
Non-radicular neck pain arising from local musculoskeletal structures, known as mechanical neck pain or somatic dysfunction, is highly prevalent in the fighter jet aviator population. The management of this problem includes both therapeutic and aeromedical decisions. In addition to non-steroidal anti-inflammatory medications, waiver guides recommend therapeutic exercise and manipulative therapy as treatments for somatic spine pain in aviators, and such treatments are employed in many military locations. However, there are currently no published studies that describe the use of manipulative therapy for fighter jet aviators. We report the case of an F/A-18 instructor pilot who experienced long-term relief of uncomplicated mechanical neck pain following interdisciplinary management that included manipulation and a home exercise program. Diagnostic considerations, conservative treatment options, and aeromedical concerns are discussed.
Keywords: neck pain, manual therapy, aviation, exercise therapy, manipulation, spinal
Abstract
Douleur au cou non radiculaire découlant des structures musculosquelettiques locales, connue sous le nom de douleur mécanique au cou ou trouble somatique, très prévalente auprès des pilotes d’avion de combat à réaction. La gestion de ce problème inclut des décisions à la fois d’ordre thérapeutique et aeromédicale. En plus de médicaments anti-inflammatoires non stéroïdiens, les guides de dérogation recommandent de l’exercice thérapeutique et de la thérapie manuelle comme traitement pour la douleur somatique de la colonne vertébrale chez les pilotes. Ces traitements sont employés dans de nombreuses installations militaires. Toutefois, il n’existe à présent aucune étude publiée qui décrit l’usage de la thérapie manuelle chez les pilotes d’avion de combat à réaction. Nous rapportons le cas d’un pilote instructeur de F/A-18 qui a éprouvé un soulagement à long terme d’une douleur mécanique au cou non complexe à la suite d’une gestion interdisciplinaire qui incluait la thérapie manuelle et un programme d’exercices à domicile. Les considérations diagnostiques, les options de traitement conservatrices et les soucis au plan aéromédical font l’objet d’une discussion.
Keywords: douleur au cou; thérapie manuelle; aviation; rééducation par l’exercice; manipulation, colonne vertébrale
Introduction
Fighter jet aviators are exposed to large tensile, axial compression, and shear forces when flying, especially during aerial combat maneuvers (ACM).1 Non-radicular neck pain arising from mechanical structures in the neck (somatic pain) is a common outcome of exposure to high gravitational (G) forces.2 The weight of the helmet and oxygen mask and the various non-neutral head postures assumed when observing for enemy aircraft contribute to this problem.1 Spinal disorders can result in disability3 and conditions that may disqualify pilots from flight duties.4 Thus, neck pain in the fighter jet aviator population has a negative impact on work performance, productivity, and is a threat to combat readiness.5 In addition to non-steroidal anti-inflammatory drugs (NSAIDs) and short courses of analgesics, the US Navy Aeromedical Reference and Waiver Guide and the US Air Force Waiver Guide recommend mobilization exercises and manipulative therapy in the management of mechanical non-radicular spine pain.6,7 Despite recommendations by these guides and the high prevalence of neck pain,8 we could find no published studies that describe the use of manual therapy, spinal manipulation, or spinal mobilization and therapeutic exercise for managing mechanical neck pain in aviators. In this article we present the case of a jet fighter aviator with uncomplicated mechanical neck pain who had a favorable response to conservative interdisciplinary management using manual therapy and therapeutic exercise.
Case report
A 38-year-old male active duty US Marine Corps F/A-18 instructor pilot with 2693 total flight hours, of which 2134 were in the F/A-18 (fighter/attack aircraft), was referred by his flight surgeon to one of the naval hospital’s on-station doctors of chiropractic for treatment of intermittent neck pain. The neck pain was experienced intermittently over a period of two years, the most recent episode being initiated after assuming an instructor role that involved flying frequent ACM training sorties during the previous eight weeks. The pain was located in the right side of his neck and worsened when he turned or laterally flexed his head to the right. The neck pain became more bothersome during and after ACM. Typically the pain was described as being dull and aching in character; however it could become sharp with rapid right rotation of the neck or under high G situations. He experienced difficulty turning his head to the “check six” position because of pain and decreased range of motion, thereby interfering with his ACM capabilities. The patient was referred to the chiropractor when it had not resolved with a two-week course of acetaminophen, flight grounding, and topical applications of heat and had been present for more than 8 weeks. The pain did not interfere with sleeping and had no features related to time of day. He denied radiating pain, paresthesia, upper or lower extremity weaknesses, bowel or bladder incontinence, visual disturbances, dizziness, or headache. His numerical pain scale rating for severity was 3/10 (10 represented by ‘the worst pain imaginable’) and his Neck Disability Index9 score was 6%. The patient was a very healthy male Marine engaging in multiple forms of exercise per week, including running, yoga, weightlifting, Marine fitness training, and mountain biking. He did not smoke or drink, was not under any new stress and had a stable married home life.
His gross active neck range of motion was visibly decreased for right rotation and right lateral flexion. Stiffness was observed by both the patient and the doctor at the end range of passive right rotation as well as with right lateral flexion. The patient experienced pain on the right side of the neck with axial loading of the neck in the neutral position.10 In the sitting position, manual axial traction11 decreased his pain and increased his active range of motion. Neural tensioning through contralateral rotation and extension of the neck while the upper extremity was abducted with the elbow, wrist, and fingers passively extended11 elicited no radiating pain, numbness, or tingling in the upper extremities. Tenderness to palpation was present in the right cervico-thoracic paravertebral and upper trapezius muscles.12 No signs of infection were present, and there were no abnormal neurological findings detected with dermatome assessment, deep tendon reflex testing, upper extremity myotomal strength testing, or Valsalva’s maneuver.
The patient was diagnosed with Grade I neck pain,13 also known as mechanical neck pain or somatic pain, and dysfunction of the cervicothoracic junction. Fracture, disc herniation, and dislocation were considered unlikely differential diagnoses due to the patient having no history of frank trauma, the relatively low level of pain severity and disability, the absence of neurological signs or symptoms, and the absence of any red flags suggesting more ominous processes.12 Imaging was not obtained, consistent with the best available evidence of the limited utility of plain radiographs, CT, or MRI for patients with non-acute, non-radicular neck pain.12
As recommended by the US Navy Aeromedical Reference and Waiver Guide and the US Air Force Waiver Guide, in addition to the medication already tried, the management plan included mobilization exercises and manipulative therapy. No findings in the history or examination were present that would contraindicate spinal manipulation. The patient was treated by a chiropractic practitioner with more than 600 hours of training in spinal manipulation/manual therapy and over 16 years of practice experience. Four treatments occurred over five weeks; treatments were modified based upon the patient’s improved signs and symptoms at each consecutive visit. During the first office visit, the patient was treated using high velocity, low amplitude, manual manipulation of the upper thoracic and lower cervical spine to improve right lateral flexion and right rotation. These manipulations were selected based upon the presence of pain, decreased symmetry in active and passive range of motion, and tenderness to palpation.14 The cervical spine was manipulated in the supine position using a spinous process contact and the thoracic spine in the prone position using a modified pisiform contact.14 Active stretching of the right upper trapezius muscle was also performed while digital pressure was applied by the provider to tender areas located in the muscle. In addition, home stretches for the upper trapezius muscles15 were prescribed 3–5 times daily and the patient was advised to hold each stretching position for 30 seconds. The patient reported an immediate reduction in pain and improved mobility after the first visit. At the three-week follow up, he had stiffness without pain and had been returned to flying, but had only flown two ACM missions. The previous treatment was repeated.
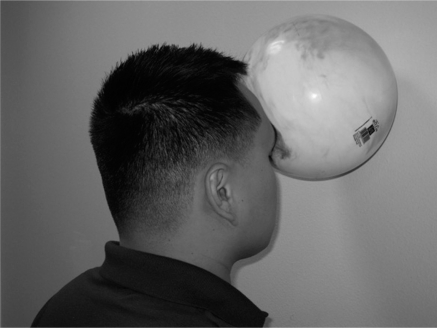
At the four-week follow up visit (third treatment), improvements in outcome measures included minor limited range of motion, mild tenderness to palpation, and stiffness with no neck pain. He had flown a few ACM missions to ascertain a rigorous response to treatment. Since he was still having some residual stiffness, reduced range of motion, and tenderness to palpation, the treatment protocol was repeated once more. Standing multiplanar isometric endurance home exercises for the neck musculature16 were prescribed in an effort to enhance paracervical muscular strength and endurance, based upon the increased physical demands of the neck musculature during flight (Figure 1). These exercises were aimed at functional restoration and therefore modified to closely mimic the tasks associated with flying the F/A-18.
Figure 1.
Standing isometric neck exercises. The patient stands upright, slightly contracts his abdominal muscles for stability, and pushes his forehead against a ball that is held against a wall (isometric neck flexor contraction) for at least 10 seconds. The patient is then instructed to position his body 45 degrees to the ball and repeat the isometric procedure, thereby exercising the neck with combined muscle groups. Isometric exercises are prescribed for each successive 45 degree radius for a total of 8 positions and the patient is asked to perform 2 repetitions of each position and 2 sets of these exercises daily.
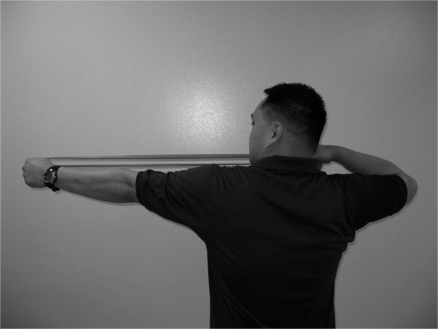
At the five-week follow up visit (fourth treatment), he reported no neck pain, including during and after ACM. He had no tenderness to palpation and nearly full restoration of neck range of motion. He reported that he had been compliant with the neck isometric exercises and felt that they were of benefit. Based upon his apparent improvements with the isometric exercises, the patient was provided isotonic exercises aimed at further improving the strength and endurance of the posterior neck musculature and scapular stabilizers (Figure 2). These exercises were intended to provide a therapeutic delivery of load, simulating those forces placed on the neck during ACM.
Figure 2.
Standing isotonic scapular stabilization exercises. The patient stands upright and slightly contracts the abdominal and interscapular muscles for stability. An elastic therapy band is used to create resistance and the patient simulates the movement associated with shooting an arrow from a bow. These exercises employ 2-second concentric muscle contractions from the starting point to the point of tension, a 5-second isometric hold at the point of maximum tension, and a 5-second eccentric contractions back to the starting point. These can be performed with the leading arm parallel to the floor and also angled 45 degrees toward the ceiling and toward the floor. Ten repetitions of each exercise vector were prescribed.
At the eight-week follow up (fifth visit, no treatment, re-examination only), he reported no pain and no stiffness and had flown numerous ACM missions without a recurrence of neck pain. His Neck Disability Index score was 0/50. Examination revealed full active and passive ranges of cervical motion and no tenderness to palpation. The patient had no subsequent neck pain episodes that were reported to his flight surgeon or chiropractic physician over the ensuing 6 months and deployed to the combat theater without incident.
Discussion
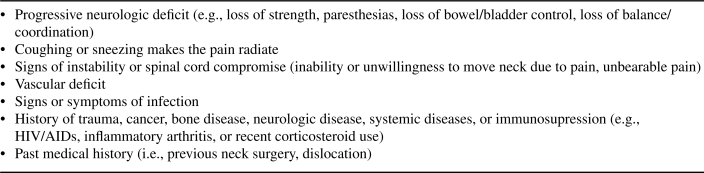
Mechanical neck pain is a common disorder in the general population13 and is typically described as a local, non-radicular pain that is sometimes increased with movements of the neck.17 The anatomical sources of mechanical neck pain typically include muscles, ligaments, and joints of the cervical spine.17 Uncomplicated mechanical neck pain must be differentiated from radicular pain, in which neurologic pathology is present (e.g., disc herniation, nerve root entrapment) as these conditions may be managed differently.18 A thorough history and physical examination will help to determine if neck pain is mechanical and to rule out signs or symptoms of major pathology, such as fracture, myelopathy, neoplasm, or systemic disease.12 These pathologies (i.e., “red flags”) should receive immediate and additional investigation. Red flags for neck pain history are presented in Figure 3. Diagnostic imaging and laboratory studies are not typically necessary for mechanical neck pain unless they are needed to rule out potentially pathologic conditions.12
Figure 3.
Red flags for neck pain, which suggest more ominous underlying pathology than uncomplicated mechanical neck pain and may require further evaluation (adapted from reference 18).
The Neck Pain Task Force has established an updated classification of neck pain. These include: Grade I (no signs or symptoms of major pathology and minor interference with activities of daily living); Grade II (no signs or symptoms of major pathology and major interference with activities of daily living); Grade III (no signs or symptoms of major pathology and presence of neurologic signs, which may include decreased deep tendon reflexes, sensory, or motor deficits); and Grade IV (signs or symptoms of major pathology, such as fracture, neoplasm, systemic disease, or myelopathy).13 Conservative methods for the treatment of neck pain may include NSAIDS (e.g., ibuprofen, naproxen). However prolonged treatment with NSAIDS is not recommended due to some of their associated complications (e.g., gastric bleeding). Sometimes muscle relaxants are prescribed (e.g., cyclobenzaprine, metaxalone), but they are considered temporarily disqualifying from flight duties due to the potential side effects (e.g., dizziness, drowsiness). Cervical collars are typically not recommended, as the research evidence does not support their use.19 Manual therapies (e.g., mobilization, manipulation) and physical treatments (e.g., physiotherapy, exercise) have evidence to support their use for uncomplicated neck pain without severe neurologic deficit.19,20 To address mechanical dysfunction, manipulative and physical therapies in addition to exercise may assist with treatment of the current episode and the prevention of future neck pain. Manipulation should be performed by healthcare providers who are trained in this procedure. If a flight surgeon does not have this training, he or she can work in conjunction with an on-station osteopath, chiropractor, or physical therapist who is trained in these procedures.
While the management of mechanical neck pain in the aviation community may be similar to that of the general population, there are some important differences of which flight surgeons and other healthcare providers should be aware. Of special consideration are the prevalence of neck pain in this population and the aeromedical consequences when managing these patients. The prevalence of neck pain in fighter jet aviators ranges from 26.8%5 to 89.1%,21 and because of its commonality has been called a work-related musculoskeletal disorder of fighter jet aviators.8 In comparison, the 12-month prevalence of neck pain in the general population ranges from 30–50%.22 Neck pain not only diminishes pilot concentration and function during flight23 but also can be severe enough to ground pilots or result in decreased flying time.4 Since neck pain can result in disability or progress to a non-waiverable flight disqualification,4 neck pain in the fighter jet aviator population has a negative impact on performance and is a threat to combat readiness.5
The US Navy Aeromedical Reference and Waiver Guide states that neck and back pain from biomechanical derangements of the spine and resulting muscle aches and spasms, known as somatic dysfunction,6 are not considered to be disqualifying for flight status unless the condition is persistent or has required hospitalization.6 For pain that does not require a waiver, the Waiver Guide recommends mobilization exercises, physical therapy, manipulation, and occasional use of flight surgeon prescribed NSAIDs for a short-term course of care to manage back or neck pain.6,7 These medications are considered disqualifying for flight if used chronically and would then require a waiver.6 Muscle relaxants are considered disqualifying and should not be used by military aviators while on flying status. The use of therapeutic exercises,6,7 manual therapy provided by a physician,6 or manipulation7 are not considered disqualifying for flight. Thus, for this unique population, conservative non-pharmaceutical management may be considered when developing a treatment plan.
The literature discussed below suggests that individuals who have neck pain have diminished muscle control and coordination. It has been noted that fighter pilots who do not have neck pain possess greater efficiency of neck extensor muscles (more antagonistic muscle EMG activity) than non-pilot subjects24 and greater neck extensor muscle strength than pilots with neck pain.25 However, Seng et al have demonstrated that asymptomatic pilots do not have greater isometric strength than non-pilot controls and advocate for on-land neck muscle strengthening exercises for aviators.26 O’Leary, Falla, and Jull identified that neck pain subjects have altered coordination between the superficial and deep neck muscles, poorer kinesthetic sense, and higher rates of muscular fatigue when exposed to sustained loads,27 which may explain the difference in muscle strength between pilots with and without neck pain, as noted by Ang et al.25 Exposure to G forces during regular flying has been associated with limited increases in isometric neck muscle strength,28 suggesting that flight-induced gains in strength are negligible to counteract the forces placed on the body during ACM.
Several authors have investigated the potential use of strengthening programs to prevent neck pain in this population. It has been shown that pilots who engage in muscle endurance training have less acute in-flight neck pain,29 and pilots engaged in a supervised neck-specific strength and flexibility program demonstrated significant increases in neck strength and endurance compared to pilots provided a home exercise program.30 Recently, it has been shown that certain isotonic elastic band exercises and resistance machine neck strengthening exercises can generate similar neck muscle activation to G forces in the z axis measured in-flight and may represent a useful and job-specific physical training program for pilots involved in ACM.31 However, to our knowledge, there are no prospective controlled investigations of the efficacy of neck exercises for neck pain in fighter pilots that can inform clinical practice decisions.
While there are anecdotal reports of aviators receiving manipulative therapy for neck pain,8,23 the effectiveness of this therapy in managing neck pain in fighter jet aviators is not reported in the literature. It is known that manual therapy is an effective non-pharmacological and non-surgical treatment option for whiplash and non-whiplash associated neck pain in the general population,19 and it would seem rational to extend those results to the fighter aviator population. Hence, it is theoretically plausible that pilots with somatic neck pain may benefit from a rehabilitation program that includes proprioceptive activities, spinal manipulation or mobilization, muscle co-activation, and neck muscle strength and endurance training. This was the rationale employed in the rehabilitation of the pilot in this case.
In the highly work-motivated flight community it is vitally important that members of the medical team work together to minimize patient recovery time while ensuring maximum flight safety. Flight surgeons are best qualified to interpret aviation safety guidelines, such as those in the US Navy Aeromedical Reference and Waiver Guide, and therefore, a close working relationship between the manual therapist and the pilot’s flight surgeon is invaluable. In this manner, appropriate modalities can be maximized, consistent follow-up can be ensured, and all regulations can be closely followed. By utilizing the skills and knowledge unique to each medical team member, the pilot can be maintained on flight status, or returned to it quickly, without breaking any aviation safety regulations or endangering the aviator.
There are limitations to this case report. Although the patient improved and was released from care after only five visits, the time over which these treatments were given was considered suboptimal. The patient was not able to be seen as frequently as desired due to scheduling conflicts. A higher treatment frequency over a shorter duration would have been preferred to optimize treatment response related to manipulative and soft tissue therapy.32 Range of motion assessment, such as dual inclinometry, would have been preferred over visual assessment. Limitations inherent to the case report design prevent one from generalizing beyond this single case since this was a non-controlled retrospective study. The natural history of neck pain is episodic and recurrent13 and may possibly explain the short term resolution of his neck pain. Summarily, this case study reports one pilot presenting with neck pain that was interfering with his job performance, who was motivated to maintain a high level of job-related function, and who appeared to have a favorable response to a conservative management approach that is under-reported within this population. We hope this report stimulates further research interest in the treatment and prevention of neck pain in this population.
Conclusion
Neck pain is highly prevalent in fighter jet aviators and can compromise mission safety and aviator function.3,8 Chronic neck pain and some medications may be considered disqualifying for flight for military pilots according to the US Navy Aeromedical Reference and Waiver Guide. Manual therapy and therapeutic exercise are recommended for treating this problem and are not considered disqualifying. Therefore, applying these conservative options that help with managing pain and function for aviators could be considered. In this case, a pilot with neck pain was managed following these recommendations and was able to successfully continue flying without return of pain or dysfunction.
Footnotes
Endnotes
The views expressed in this article are those of the authors and do not reflect the official policy or position of the Department of the Navy, Department of Defense, or the United States Government.
References
- 1.Coakwell MR, Bloswick DS, Moser R., Jr High-risk head and neck movements at high G and interventions to reduce associated neck injury. Aviat Space Environ Med. 2004;75(1):68–80. [PubMed] [Google Scholar]
- 2.Green ND, Brown L. Head positioning and neck muscle activation during air combat. Aviat Space Environ Med. 2004;75(8):676–680. [PubMed] [Google Scholar]
- 3.Voge VM, Tolan GD, Nixon WE. Chronic back disability: USAF officers at separation and exposure to +Gz. Mil Med. 1996;161(4):221–224. [PubMed] [Google Scholar]
- 4.Bailey DA, Gilleran LG, Merchant PG. Waivers for disqualifying medical conditions in U.S. Naval aviation personnel. Aviat Space Environ Med. 1995;66(5):401–407. [PubMed] [Google Scholar]
- 5.Yacavone DW, Bason R. Cervical injuries during high G maneuvers: a review of Naval Safety Center data, 1980–1990. Aviat Space Environ Med. 1992;63(7):602–605. [PubMed] [Google Scholar]
- 6.Acromite MT. U. S. Navy Aeromedical Reference and Waiver Guide. Pensacola: U.S. Navy, 2008. Available from: http://www.med.navy.mil/SITES/NAVMEDMPTE/NOMI/NAMI/ARWG/Pages/AeromedicalReferenceandWaiverGuide.aspx
- 7.U.S.AirForce Air Force waiver guide.: U.S. Air Force, 2007. Available from: http://aviationmedicine.com/resources/files/PDF/VFS_attachments_07/USAF%20Wavier%20Guide%20PDF.pdf
- 8.Drew WED. Spinal symptoms in aviators and their relationship to G-exposure and aircraft seating. Aviat Space Environ Med. 2000;71:22–30. [PubMed] [Google Scholar]
- 9.Vernon H. The Neck Disability Index: state-of-the-art, 1991–2008. J Manipulative Physiol Ther. 2008;31(7):491–502. doi: 10.1016/j.jmpt.2008.08.006. [DOI] [PubMed] [Google Scholar]
- 10.Wainner RS, Fritz JM, Irrgang JJ, Boninger ML, Delitto A, Allison S. Reliability and diagnostic accuracy of the clinical examination and patient self-report measures for cervical radiculopathy. Spine. 2003;28(1):52–62. doi: 10.1097/00007632-200301010-00014. [DOI] [PubMed] [Google Scholar]
- 11.Rubinstein S, Pool J, Tulder Mv, Riphagen I, Vet Hd. A systematic review of the diagnostic accuracy of provocative tests of the neck for diagnosing cervical radiculopathy. Eur Spine J. 2007;16:307–319. doi: 10.1007/s00586-006-0225-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nordin M, Carragee EJ, Hogg-Johnson S, Weiner SS, Hurwitz EL, Peloso PM, et al. Assessment of neck pain and its associated disorders: results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. Spine. 2008;33(4 Suppl):S101–22. doi: 10.1097/BRS.0b013e3181644ae8. [DOI] [PubMed] [Google Scholar]
- 13.Haldeman S, Carroll L, Cassidy JD, Schubert J, Nygren A.The Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders: executive summary Spine (Phila Pa 1976) 2008334 SupplS5–7. [DOI] [PubMed] [Google Scholar]
- 14.Peterson D, Bergmann T. Chiropractic technique: principles and procedures. 2nd ed. St. Louis: Mosby; 2002. [Google Scholar]
- 15.Valachi B, Valachi K. Preventing musculoskeletal disorders in clinical dentistry. J Am Dent Assoc. 2003;134:1604–1612. doi: 10.14219/jada.archive.2003.0106. [DOI] [PubMed] [Google Scholar]
- 16.Ierna GF. Rehabilitation of sports injuries. In: Hyde TE, Gengenbach M, editors. Conservative management of sports injuries. 2nd ed. Sudbury: Jones and Bartlett; 2005. pp. 157–206. [Google Scholar]
- 17.Manchikanti L, Boswell MV, Singh V, Benyamin RM, Fellows B, Abdi S, et al. Comprehensive evidence-based guidelines for interventional techniques in the management of chronic spinal pain. Pain Physician. 2009;12(4):699–802. [PubMed] [Google Scholar]
- 18.Guzman J, Haldeman S, Carroll LJ, Carragee EJ, Hurwitz EL, Peloso P, et al. Clinical practice implications of the Bone and Joint Decade 2000–2010 Task Force on neck pain and its associated disorders: From Concepts and Findings to Recommendations Spine (Phila Pa 1976) 200833S199–S213. [DOI] [PubMed] [Google Scholar]
- 19.Hurwitz EL, Carragee EJ, van der Velde G, Carroll LJ, Nordin M, Guzman J, et al. Treatment of neck pain: noninvasive interventions: results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders Spine (Phila Pa 1976) 2008334 SupplS123–52. [DOI] [PubMed] [Google Scholar]
- 20.Bronfort G, Haas M, Evans R, Bouter L. Efficacy of spinal manipulation and mobilization for low back pain and neck pain: a systematic review and best evidence synthesis. The Spine Journal. 2004;4(3):335–356. doi: 10.1016/j.spinee.2003.06.002. [DOI] [PubMed] [Google Scholar]
- 21.Kikukawa A, Tachibana S, Yagura S. G-related musculoskeletal spine symptoms in Japan Air Self Defense Force F-15 pilots. Aviat Space Environ Med. 1995;66(3):269–272. [PubMed] [Google Scholar]
- 22.Hogg-Johnson S, van der Velde G, Carroll LJ, Holm LW, Cassidy JD, Guzman J, et al. The burden and determinants of neck pain in the general population: results of the Bone and Joint Decade 2000–2010 Task Force on Neck Pain and Its Associated Disorders. Spine. 2008;33(4 Suppl):S39–51. doi: 10.1097/BRS.0b013e31816454c8. [DOI] [PubMed] [Google Scholar]
- 23.Simon-Arndt CM, Yuan H, Hourani LL. Aircraft type and diagnosed back disorders in U.S. Navy pilots and aircrew. Aviat Space Environ Med. 1997;68(11):1012–1018. [PubMed] [Google Scholar]
- 24.Lecompte J, Maisetti O, Guillaume A, Skalli W, Portero P. Neck strength and EMG activity in fighter pilots with episodic neck pain. Aviat Space Environ Med. 2008;79(10):947–952. doi: 10.3357/asem.2167.2008. [DOI] [PubMed] [Google Scholar]
- 25.Ang B, Linder J, Harms-Ringdahl K. Neck strength and myoelectric fatigue in fighter and helicopter pilots with a history of neck pain. Aviat Space Environ Med. 2005;76(4):375–380. [PubMed] [Google Scholar]
- 26.Seng KY, Lam PM, Lee VS. Acceleration effects on neck muscle strength: pilots vs. non-pilots. Aviat Space Environ Med. 2003;74(2):164–168. [PubMed] [Google Scholar]
- 27.O’Leary S, Falla D, Jull G. Recent advances in therapeutic exercise for the neck: implications for patients with head and neck pain. Aust Endod J. 2003;29(3):138–142. doi: 10.1111/j.1747-4477.2003.tb00540.x. [DOI] [PubMed] [Google Scholar]
- 28.Burnett AF, Naumann FL, Burton EJ. Flight-training effect on the cervical muscle isometric strength of trainee pilots. Aviat Space Environ Med. 2004;75(7):611–615. [PubMed] [Google Scholar]
- 29.Hamalainen O, Vanharanta H, Bloigu R. Determinants of +Gz-related neck pain: a preliminary survey. Aviat Space Environ Med. 1993;64(7):651–652. [PubMed] [Google Scholar]
- 30.Alricsson M, Harms-Ringdahl K, Larsson B, Linder J, Werner S. Neck muscle strength and endurance in fighter pilots: effects of a supervised training program. Aviat Space Environ Med. 2004;75(1):23–28. [PubMed] [Google Scholar]
- 31.Netto KJ, Burnett AF, Coleman JL. Neck exercises compared to muscle activation during aerial combat maneuvers. Aviat Space Environ Med. 2007;78(5):478–484. [PubMed] [Google Scholar]
- 32.Haas M, Groupp E, Aickin M, Fairweather A, Ganger B, Attwood M, et al. Dose response for chiropractic care of chronic cervicogenic headache and associated neck pain: a randomized pilot study. J Manipulative Physiol Ther. 2004;27(9):547–553. doi: 10.1016/j.jmpt.2004.10.007. [DOI] [PubMed] [Google Scholar]