Abstract
Objective:
Heat illnesses contribute to significant morbidity and occasional mortality in athletic populations. Sunburn increases the risk of various skin carcinomas. This report provides an overview of the etiology, symptomatology, risk identification, prevention, and treatment for heat related illnesses and sunburn.
Clinical Features:
Four cases are presented to illustrate the diagnosis and immediate treatment of exercise related heat illness and sunburn.
Intervention and Outcome:
Identification of signs and symptoms combined with prompt treatment, achieved resolution in three athletes presenting with exercise related heat illness and one athlete with sunburn.
Conclusion:
The best treatment approach is prevention. Chiropractors can be an important resource for information regarding prevention and treatment strategies. For mild to moderate heat illness, quick identification of signs and symptoms, followed by rapid cooling and re-hydration comprises treatment. For heat stroke, rapid and aggressive cooling is essential to reduce mortality. Best evidence treatment of sunburn is symptomatic relief with emollients and pain control via medications.
Keywords: heat illness, sunburn, diagnosis, chiropractor
Abstract
Objectif :
Les coups de chaleur contribuent significativement à la morbidité et occasionnellement à la mortalité pour plusieurs athlètes. Les coups de soleil augmentent le risque de développer divers carcinomes de la peau. Ce rapport présente un survol de l’étiologie, de la symptomatologie, de l’identification du risque, de la prévention et du traitement pour les coups de chaleur et les coups de soleil.
Caractéristiques cliniques :
Ce rapport présente quatre cas qui illustrent le diagnostic et le traitement immédiat des coups de chaleur et des coups de soleil en lien avec l’activité physique.
Intervention et résultat :
L’identification des signes et des symptômes, combinée à un traitement prompt, a permis de soulager trois athlètes qui souffraient de coups de chaleur en lien avec l’activité physique et un athlète souffrant d’un coup de soleil.
Conclusion :
La meilleure approche thérapeutique est la prévention. Les chiropraticiens peuvent être une ressource importante pour diffuser l’information au sujet des stratégies de prévention et de traitement. Pour les coups de chaleur bénins à modérés, le traitement consiste en une identification rapide des signes et des symptômes, suivie d’un refroidissement et d’une réhydratation rapide. Pour les coups de chaleur plus graves, un refroidissement rapide et agressif est essentiel pour réduire l’incidence de mortalité. Le meilleur moyen prouvé de traiter les coups de soleil est le soulagement symptomatique à l’aide d’émollients et le contrôle de la douleur par les médicaments.
Keywords: coup de chaleur, coup de soleil, diagnostic, chiropraticien
Introduction
Heat related illnesses and sunburn are extremely common but dramatically under reported.1 Heat illness, including heat edema, heat cramps, heat syncope, heat exhaustion, and heatstroke, contribute to significant morbidity as well as occasional mortality in athletic, elderly, paediatric and disabled populations.1,2 The incidence of heatstroke alone, in urban areas of the United States during times of high ambient temperature, is upwards of 20 cases per 100,000 people, and accounts for at least 240 deaths annually.2 Among US high school athletes, “heat illness is the third leading cause of death.”1 Although often associated, sunburn is not considered a true heat illness since it is a direct result of excessive sunlight exposure, whereas heat illness is a result of an increase in body temperature.1–3 The data from 4,023 respondents of the 1996 Canadian National Survey on Sun Exposure & Protective Behaviours (NSSE&PB) indicated that; 53% of Canadians of age 15 years or older experience one or more sunburns during a summer, 68% of those being between the ages of 15 and 24, and a higher proportion of males reported sunburn than females.3 Evidence suggests that sun exposure leading to sunburn, including a history of sunburn at young ages, increases the risk of melanoma, basal cell carcinoma, and possibly squamous cell carcinomas.4 In addition to the risks of cancer, sunburn is commonly associated with heat exhaustion and heatstroke.5 These are alarming statistics, considering that heat illnesses and sunburns are almost completely preventable, especially in a sporting situation.1,2
This report will describe the on-field diagnosis and immediate treatment of four teenaged female athletes with various presentations of heat related illness and/or sunburn. The report will provide an overview of the etiology, symptomatology, risk identification, prevention, and the treatment for heat related illnesses and sunburn. The illustrative cases and discussion are of interest to chiropractors due to the high occurrence rate in athletes and people who enjoy physically active lifestyles, the risk of serious illness or death, and the fact that such situations are almost completely preventable. Chiropractors, as primary contact health care providers, are ideally suited to provide evidence based information and patient education regarding the prevention and treatment of heat related illness and sunburn.
Case Presentations
A female under-17, Canadian representative soccer team was competing in multiple games on a hot, sunny day with clear skies and minimal wind, in Central America during March break. The team flew in from Canada the evening previous, slept in a hotel, and woke-up early to arrive at the soccer fields on time. The ambient temperature was approximately 38°C (100.4°F), and no sun shelter was available. Midway through the 2nd half of the second game, several players reported various symptoms.
Case 1
A 14-year-old female, 5′6″ in height and 135 lbs., reports extreme thirst, feeling abnormally tired, and slightly dizzy. She states that she is too tired to continue playing without taking a break. Upon questioning, she states that she only had a little water in between this game and the previous game. She feels quite hot. Physical examination reveals normal vital statistics; blood pressure (BP), pulse rate (PR), respiration rate (RR), and tympanic membrane body temperature (BT).
Case 2
A 14-year-old female, 5′8″ in height and 145 lbs., with a self-reported history of “hypoglycemia,” removes herself from the game and describes symptoms of “light headedness” and “wooziness.” She also claims an abnormally high level of fatigue, and she appears very flushed with rosy cheeks, and sweaty. She reports that she has been drinking Gatorade™ fairly regularly during the day, and states that she has almost finished a 1-litre bottle. Physical examination reveals normal vital statistics (BP, PR, RR, and BT).
Case 3
A 14-year-old female, 5′6″ in height and 130 lbs., withdraws from the game and describes symptoms of headache, extreme fatigue, dizziness, weakness, and exhibits a very flushed, rosy cheeked, sweaty appearance. She also shows mild swelling in her fingers and feet. She reports a previous history of “mild heat problems” which have included episodes of “fatigue, headaches, and dizziness” occurring during and after strenuous exercise in the heat. She uses an inhaler as required for exercise induced asthma, and she had just recently experienced the onset of menses. She has been trying to drink lots of water during the day, but is unsure of how much she may have consumed. Physical examination reveals strong and regular peripheral pulses, normal respiration, a BP of 110/74, PR of 110 beats/min, and a BT of 38.9°C (102°F).
Case 4
Later that evening a 16-year-old female, 5′6″ in height and 117 lbs., presented with severely sunburned forehead and arms. The skin on both her forehead and arms is very red and painful to touch. Her forehead exhibits significant swelling and is starting to blister. She reports the additional symptoms of feeling hot and dizzy. She does not feel like eating. Previous medical history reveals that she takes oral acne medication and has a history of menstrual irregularity and dysmenorrhoea. Physical examination reveals normal vital statistics (BP, PR, RR, and BT).
The first three athletes were diagnosed with various severities of heat exhaustion and dehydration, from a mild to a more moderate presentation, respectively. They were removed from play for the remainder of the day, superfluous clothing was removed, cool water was splashed over their heads and upper torsos, and cool, wet towels were placed on their foreheads and necks. The third athlete presented, also had ice packs applied to both armpits and her neck. Shade was provided as best as possible using clothing and umbrellas as available. They were given easily digestible food, and instructed to slowly consume cool water until dinner time. All three of the athletes recovered rapidly and within approximately 30 to 60 minutes, reported little to no residual symptoms, with the exception of mild thirst. Upon follow-up that evening all three of the athletes had completely recovered and were continuing to slowly re-hydrate with water and electrolyte sport drinks.
The fourth athlete presented, was diagnosed with multiple, moderate to severe sunburns, and the associated symptoms of excessive sun exposure. The burst blisters on her forehead were cleaned with a mild anti-bacterial wound cleanser, and a clean dressing was applied. She was given a cool compress to apply to both her arms and forehead, and a moisturizing lotion was repeatedly applied to the burned areas on her arms. She was instructed to slowly re-hydrate with cool water, consume food when she felt better, and to maintain bed rest for the remainder of the evening and the next morning.
All four athletes were withheld from competition the next day and were continually monitored. After sunburns were covered with opaque clothing, and each athlete was instructed on, and monitored for, proper hydration and sun protection practices, all four athletes were cleared for return to play on the third day. None of the athletes experienced a recurrence of symptoms for the remainder of the trip, despite competing in five additional games under the same environmental conditions.
Discussion
Heat Related Illness
Humans are homeothermic organisms, meaning that humans regulate their own warm-blooded body temperature.6 Typically speaking, humans are successful in maintaining their body temperature within a normal range of 35.8°C to 37.3°C (96.4°F to 99.1°F).1,6 However, exercising in the heat places demands on the body’s ability to thermoregulate.1 Heat production during exercise is 15 to 20 times greater than at rest, and is sufficient to raise a persons core body temperature 1°C every five minutes, if there were no inherent regulatory mechanisms.1 The heat generated by the body and the heat absorbed from the ambient environment must be offset by multiple mechanisms for heat dissipation.1 These cooling mechanisms which work simultaneously to varying degrees depending on the situation include conduction, convection, radiation, and evaporation.1,2,7 Conduction refers to heat loss through direct contact with a cooler object.2,7 Convection is the dissipation of heat when relatively cool air passes over exposed skin.2,7 Radiation is the release of heat from the body directly into the environment, and evaporation through sweating, is a process that incorporates the processes of both convection and radiation by the secretion of body water through to the skins surface.2,7
Assuming a healthy body, heat exchange using the aforementioned mechanisms is dependent on gradients of temperature and moisture.6 As the ambient temperature and humidity increases, the thermal transfer from the body to the environment becomes less efficient.1,2,6 When the ambient temperature rises above 20°C (68°F), the processes of conduction, convection, and particularly radiation, become less and less efficient.1 In such situations the bulk of heat dissipation, especially in an exercising individual, results from evaporation through the process of sweating.1,7 In hot, dry conditions, evaporation from sweating can account for as much as “98% of dissipated heat.”1 Thus, any factor that limits the body’s ability to utilize evaporative sweating processes, such as high humidity, dehydration, or restrictive non-breathable clothing, will have a profound effect on physiological function, athletic performance, and the risk for heat illness in exercising individuals.1,7
Body temperature homeostasis is about balance.8 Heat dissipation must equal heat accumulation. When heat accumulation surpasses heat dissipation, homeostasis is lost and hyperthermia is the result.8 Marsh and Jenkins (2002) state that the “continuum of hyperthermia symptom progression results in the clinical subcategories of heat illness,” meaning that the various subcategories of heat illness (heat edema, heat cramps, heat syncope, heat exhaustion, and heatstroke) are the attendant clinical symptoms of various stages of hyperthermia.8 Although traditionally heat edema, heat cramps, heat syncope, heat exhaustion, and heatstroke are the five common types of heat illness typically associated with strenuous activity in hot, humid weather, there is disagreement as to whether heat edema and heat cramps are distinct conditions.1,7–9 Additionally, heat syncope is often used interchangeably with heat exhaustion.1,7,8,10 In fact, recent observations contend the idea that heat edema, heat cramps, heat syncope, and heat exhaustion are “heat illnesses” at all.7,9 A narrative review by Noakes (2008) contends that “heat stroke is the only condition that can be truly described as a heat illness, since it is the only condition in which there is clear evidence for a pathological elevation of body core temperature.”9
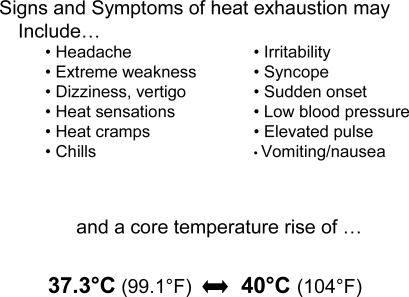
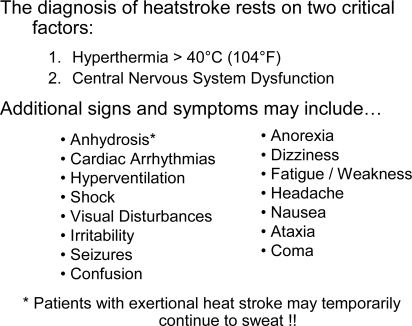
Heat edema is the mildest form of exercise related heat illness, and most commonly affects unacclimatised individuals in extreme heat.1,8 It is characterised by transient peripheral vasodilation complicated by orthostatic pooling of venous blood return, and it is generally considered to be a warning sign for heat exhaustion.1 Symptoms include; mild dependant edema in the hands and feet, normal vital signs, and concurrent symptoms of heat exhaustion may be present.1 Heat cramps can occur during or after strenuous activity in unacclimatised individuals in extreme heat.1,8 Cramping is attributed to excessive fluid and sodium loss via sweat, and the negative sodium balance which results from replacing lost water only.1,8 Like heat edema, heat cramps are considered a warning sign for the onset of heat exhaustion.1 Symptoms include; acute muscle spasms, normal vital signs, and concurrent symptoms of heat exhaustion.1 Heat syncope (fainting) is typically associated with prolonged standing or with a sudden rise from a seated or lying position in the heat.1 The condition is thought to result from inadequate cardiac output and postural hypotension from prolonged dehydration.1 Symptoms of heat syncope include acute/sudden temporary loss of consciousness and typically normal vital signs, however blood pressure may be abnormally low temporarily.1 Heat exhaustion is the most common form of exercise related heat illness, and realistically, likely encompasses the first three subcategories of heat illness.1,2,8–10 It represents a failure of the cardiovascular response to workload, typically under conditions of high external temperature and dehydration, and results in the inability to continue exercise or strenuous activity in the heat.1,2,8,10 Onset is usually sudden and the duration is typically brief.1 Symptoms include a core body temperature rise within the range of 37.3°C to 40°C (99.1°F to 104°F), and any combination of the signs and symptoms listed in Figure 1.1,2,8,10 However, recent studies have shown that the range of rectal temperatures in collapsed ultra-marathon runners is no different from those measured in asymptomatic runners, and that temperatures in some asymptomatic runners exercising in the heat can be above 40°C.7,10,11 Researchers point to the observation that “approximately 75% of subjects seen in the medical tent at the finish of an ultra-marathon race had collapsed after they had finished the race, not during.”7,9 This observation seems to contradict the notion that athletes collapsing at the end of an endurance event are experiencing “heat exhaustion.”7,9 If such athletes were experiencing significant dehydration combined with excess body heat, then it seems intuitive that they should have collapsed during the race, when demands on the cardiovascular and heat dissipation systems are maximally stressed, not at the end when the stress has been reduced.7,9 Evidence suggests that the fainting mechanism is actually a result of postural hypotension that develops after prolonged exercise due to “exercise-induced changes in blood pressure regulation and a state of low peripheral vascular resistance.”9 Hence, Noakes (2008) suggests that athletes presenting with signs and symptoms consistent with a diagnosis of heat exhaustion would better be diagnosed with “exercise-associated postural hypotension.”9 An interesting and likely accurate argument, however for the purposes of this paper the classical diagnostic term of “heat exhaustion” is utilized. Heatstroke is defined by the American College of Sports Medicine as “a condition in which body temperature is elevated to a level that causes damage to the body’s tissues, giving rise to a characteristic clinical and pathological syndrome affecting multiple organs.”10 It is a medical emergency involving total thermoregulatory failure that will not spontaneously reverse without external cooling measures.1,2,10 Heatstroke is subdivided into classical and exertional forms.8,10 Classical heatstroke is caused by environmental exposure and results in core body hyperthermia in excess of 40°C (104°F), central nervous system dysfunction, and the inability to sweat, a sign called anhydrosis.1,2,8,10 It primarily occurs in the elderly and those with chronic illness, and may develop slowly over several days.2 Exertional induced heatstroke is associated with hard exertion or exercise in a hot, humid environment resulting in core hyperthermia above 40°C (104°F) and central nervous system dysfunction.1,8–10 In contrast to the classical form, patients with exertional heatstroke may continue to sweat temporarily.8,10 It primarily affects younger, active persons, and has a relatively rapid onset, developing in hours, not days.1,8,10 It is important to note that the diagnosis of heatstroke, either classical or exertional, rests on two critical factors; hyperthermia in excess of 40°C (104°F), and central nervous system dysfunction.1,2,8–10 Additional signs and symptoms that may accompany a diagnosis of heatstroke are listed in Figure 2.
Figure 1.
Signs and Symptoms of heat exhaustion.
Figure 2.
Diagnostic criteria and additional signs and symptoms associated with heatstroke.
Sunburn
Sunburn is the acute reaction of the skin to damage by ultraviolet (UV) light exposure.5,12–14 It is estimated that 90% of UV light reaching the earth is UV light type “A” (UVA), which has been shown to penetrate into the dermis and contributes to the visible signs of aging and skin degeneration.12 The remaining 10% of UV light is UV light type “B” (UVB), the light responsible for sunburn erythema.12 The pathogenesis of sunburn is most likely due to vasodilation and increased vascular permeability of blood vessels in the upper dermis leading to erythema, edema, inflammatory response, and irreversible DNA damage.12 It is DNA damage that leads to the increased risk of skin cancer.3,12 The signs and symptoms of sunburn include; erythema, edema, blisters, ulcerations, and pain.5,12 Signs and symptoms typically become evident 3 to 5 hours after exposure, peaking in 12 to 24 hours, and generally start to dissipate by 72 hours post exposure.5,12 Although not common practice, sunburns can be graded in terms of severity.5 First-degree sunburn involves only erythema, second-degree burns have erythema and blistering, and third-degree burns have erythema, blisters, and ulcerations.5
Risk Factors for Exercise Related Heat Illnesses and Sunburn
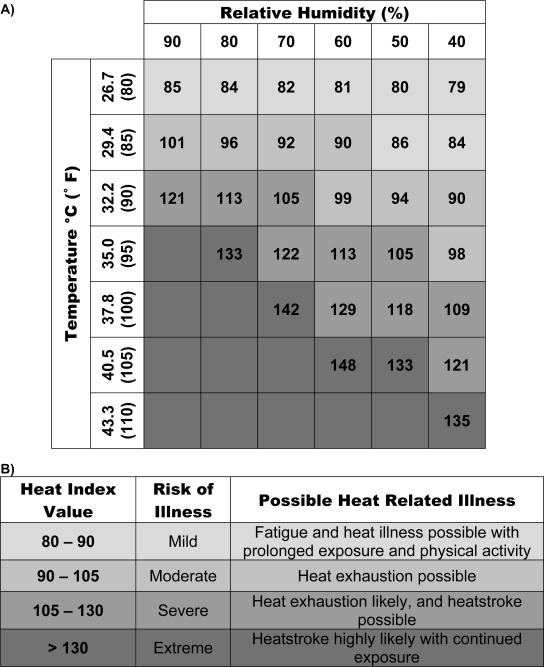
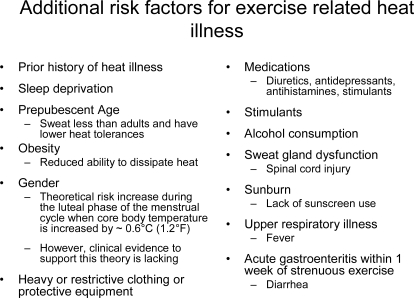
The major risk factor for exercise related heat illness is high ambient heat combined with a high level of humidity.1,8,15 Determination of the wet bulb globe temperature (WBGT) is used to assess environmental conditions and the associated risk of heat illness.1 WBGT is a standardized index of environmental heat stress that can be obtained using commercially available devices.1 It takes into account the contributions of ambient temperature, radiant heat, and humidity.1 WBGT above 27.8°C (82°F) is considered ‘very high risk.’1 WBGT between 22.8°C (73°F) and 27.8°C (82°F) is considered ‘high risk.’1 WBGT between 18.3°C (65°F) and 22.8°C (73°F) is considered ‘moderate risk,’ and WBGT below 18.3°C (65°F) is considered ‘low risk.’1 The risk associated with high environmental heat and humidity can also be assessed by utilizing a heat illness risk assessment chart (see Figure 3) in combination with readings for temperature and humidity available from local news stations or internet weather sites. Another major risk factor for exercise related heat illness is hydration status.1,15–17 Athletes typically dehydrate during exercise in the heat because of the unavailability of fluids or a mismatch between thirst and water requirements.15 A 1% reduction in body weight due to water loss can induce stress on the cardiovascular system in addition to increases in heart rate and an inhibition in heat transfer to the skin and the environment, thus contributing to an increase in core body temperature.17 When exercising in the heat, water intake equalling sweat loss results in the slowest core temperature rise compared with ‘at will’ drinking and no water consumption.1,15,17 Lack of acclimatisation is the third major risk factor for exercise related heat illness.16 People who are adjusted to activity in heat show a significantly increased ability to resist heat illness due to an increased sweating response, decreased heart rate, and a reduction in the level of perceived exertion during exercise in the heat.16 Compared to non-acclimated persons, acclimated persons demonstrate a comparatively lower core and skin temperature during exercise in the heat.16 The fourth major risk factor for heat illness in athletes is poor relative fitness leve1.16 Studies have shown that persons with high cardiovascular fitness, compared to untrained individuals, have an increased ability to dissipate heat, increased heat tolerance, and an increased glycogen storage ability which increases a body’s ability to store water.16 In addition to the major risk factors for exercise related heat illness, there are a variety of other factors that have been theoretically linked to an increased risk of heat injury.1,8,10 The associated risk factors are listed in Figure 4.
Figure 3.
Example of heat illness risk assessment charts. A) Heat index value is determined from temperature (°C) versus relative humidity (%). B) The risk of heat illness is estimated from the heat index value.
Note: The values for heat index are based upon shady, light wind conditions. Exposure to direct sunlight can increase the heat index by up to 9°C (15°F). Information adapted from http://www.crh.noaa.gov/pub/heat.php.
Figure 4.
Additional risk factors for exercise related heat illness.1,8,10
Purdue et al., (2001) utilizing information collected from the 1996 National Survey on Sun Exposure & Protective Behaviours (4,023 respondents) determined that the following factors are related to an increased risk of sunburn for persons in Canada; Ontario resident, younger age, male sex, upper middle to high income status, birthplace in North America, lighter skin colour, lighter hair colour, no personal history of skin cancer, family history of skin cancer, high awareness of the UV index, having worked outdoors over the previous summer, and increased leisure-time sun exposure.3
Prevention
Heat illness prevention depends on removing and/or minimizing risk factors.1 Thus, education is the first stage of prevention. Coaches, trainers, and the athletes themselves must be exposed to current and accurate information regarding the risks of exercise induced heat illness.16 It is of utmost importance that the athletes understand the various risks and predisposing factors, and that they are educated on how to minimize them.1,16 Proper hydration is an excellent example. Athletes are often poorly educated regarding hydration practices.1 In some athletic cultures, an ‘old school’ mentality persists where fluid restriction during athletic training is practiced and deemed necessary to ‘toughen up’ the athletes.1 Additionally, it is not uncommon for athletes to receive much of their hydration information from well intentioned but under-informed coaches, team-mates, or parents.1,16 This may impart from the fact that there remains some variability within the literature regarding the best hydration and re-hydration protocol.11,15–17 However, most sources recommend that athletes should consume 500 ml of fluid (water or electrolyte sports drink) one to two hours prior to an athletic event, and then consume approximately 250 ml of fluid every 20 minutes during exercise in activities lasting greater than one hour.1,15–17 Following exercise, an athlete should replace sweat water loss with 1.2 L of water containing 4% to 8% of carbohydrate (CHO) for every kilogram of body weight lost.1,15–17 However athletes should be careful not to consume greater than 1.5 L of fluids each hour to avoid gastric discomfort.1,15–18
Another area where an athlete can practice prevention is by becoming acclimated or acclimatized to exercise in the heat. This is more of an art than a science, as proper adaptation depends on the intensity and duration of exercise, on the environmental conditions, and the individual athlete.16,18 However, adaptation generally requires 7 to 10 days of 60 to 100 minutes of moderately strenuous exercise carried out in hot conditions, with the objective of raising body temperature and stimulating a significant sweating response.16
In addition to the above, exercise related heat illness can be prevented by athletes having heat exercise experience, and a self-awareness of how their body is responding to activity in the heat.1,15–17 Events can be timed to take place around the cooler times of the day, as opposed to occurring during or through high heat daytime hours.15–17 Athletes should wear light coloured, low weight, loose breathable clothing which does not interfere with the body’s cooling processes of conduction, convection, radiation, and evaporation.1,2,11,15–17 Athletes can maintain good lifestyle practices of eating a well balanced diet, maintaining regular hydration, and keeping cardiovascular fitness levels high.1,15–17 In addition to actively minimizing risk and predisposing factors, it is the responsibility of the athlete, team-mates, parents, coaches, trainers, and team doctors to monitor how someone is responding to exercising in the heat, and to obtain help and/or implement prevention/treatment strategies should any signs or symptoms of heat illness arise.
As with heat illness, the prevention of sunburn starts with education. Simple behavioural measures have been proven to minimize the risk of experiencing sunburn.13 Minimizing sun exposure, wearing protective clothing, and using topical sunscreens, are simple measures to undertake, which will significantly reduced a persons risk of incurring sunburn.3,13 It is generally recommended that the minimum level of sunscreen protection utilized when exercising in the heat is sun protection factor (SPF) 15, however longer sun exposure times will necessitate higher levels of protection and repeated applications.3,13
Treatment
When signs and symptoms of exercise induced heat illness present in an athlete prompt recognition is essential. Once symptoms have been recognized and the athlete assessed, treatment can be initiated.2,10,19,20 For the milder presentations of heat illness treatment is fairly straightforward and typically involves removal of the athlete from the hot environment, resting the patient in the side lying recovery position, then a gradual cooling of the patient by utilizing cool, wet towels or ice packs placed in the athletes underarms (axillae), groin, base of neck, or forehead.19 It is hypothesized that the application of cool compresses to areas were large arteries are relatively superficial in addition to the head and neck help to maximize the heat dissipation mechanism of conduction. However, to this author’s knowledge no study has been conducted to confirm the benefits of one area of cool compress application over another. Once cooling has been initiated, the athlete can slowly begin to consume cool carbohydrate/electrolyte fluids, while recovery and vitals are further monitored.2,19 It is recommended that following a mild heat related illness, athletes should be protected from heat exposure for 24 to 48 hours.2
The initial treatment of athletes presenting with heat exhaustion involves prompt recognition and stabilization in a cool area.2 If the patient is not stabilized, and the factors leading to the patient’s condition are not corrected swiftly, a progression to heatstroke may occur.2 The patient’s vital statistics, including blood pressure, heart rate, body temperature, and cognitive/central nervous system (CNS) functioning, should be determined and monitored.2,10 The patient should be placed in the recovery position and cooling should be immediately initiated.2,10 The skin can be wetted to start evaporative cooling in combination with cool, wet towel application and ice packs applied to the aforementioned areas.2 Once cooling has begun, hydration can also be initialized.2,19 Should symptoms fail to abate within 20–30 minutes, or if the patient’s vitals deteriorate, advanced medical care should be obtained and added cooling methods undertaken.2,10,19,20 Athletes diagnosed with heat exhaustion must be protected from heat exposure for a minimum of 48 hours after injury.2
Heatstroke is an emergency situation. Therefore prompt and accurate recognition is imperative. As mentioned previously, the diagnosis of heatstroke, either classical or exertional, rests on two critical factors, hyperthermia in excess of 40°C (104°F), and central nervous system dysfunction.1,2,8,10 The American College of Sports Medicine states that “mortality rate and organ damage due to heatstroke are proportional to the length of time between core temperature elevation and initiation of cooling therapy.”10 Consequently the initial stage of treatment for someone suspected of having heatstroke should be rapid and aggressive body cooling.10 Because rapid, aggressive cooling is the key to preventing mortality in patients diagnosed with heatstroke, several different cooling methods have been investigated and studied.2,10,19,20 Methods include; body immersion in iced water, evaporative cooling water spray and fans, immersing the hands and forearms in cold water, the use of ice or cold packs in the neck, groin, and axillae, invasive methods of iced gastric, bladder, or peritoneal lavage, and chemically assisted cooling.2,10,19,20 Evidence for and against these methods comes in the form of controlled trials, several case series, and experimental cooling method protocols. However, conclusive recommendations are generally lacking.2,10,19,20 A review of cooling methods for heatstroke by Hadad et al., in 2004, concluded that the majority of data, based on experimental models or healthy subjects, suggests that evaporative cooling is the best method to rapidly and safely lower core body temperature.20 However, in cases of actual heatstroke, cold water immersion was found to be the best for rapid cooling and a reduction in mortality.20 Yet, Haddad et al., (2004) also state that for field use, both methods were determined to be impractical, and that where immediate cooling is imperative, splashing copious amounts of cool water (1°C–16°C, 33.8°F–60.8°F) over the patient together with air fanning is strongly recommended.20 In 2005, a review by Smith concluded that the main predictor of outcome in exercise induced heatstroke is the duration and degree of hyperthermia, and that patients should be cooled using iced water immersion, or a combination of other techniques where iced water is not possible.19 Smith (2005) further stated that there was no evidence to support chemically induced cooling, and that further controlled trials are necessary to strengthen the overall recommendations.19 The consensus for practical emergency field care cooling methods at athletic events, are a combination of cool water spraying, fanning, cool wet towel application, and ice pack application to the neck, groin, and axillae.2,10,19,20 Regardless of the cooling method utilized, vital signs must be monitored during cooling, aggressive cooling should be stopped once core rectal temperature reaches 38°C (100.5°F), and the athlete should be transported for continued monitoring and/or advanced medical care as soon as possible.2,10,19,20
Many sunburn treatment methods have been proposed and investigated.12 However, conclusive evidence for any single treatment is lacking.12,14 A review of the management of acute sunburn by Han and Maibach in 2004, concluded that regardless of the treatment modality, the damage to epidermal cells after sunburn is the same and cannot be reversed.12 They further concluded that corticosteroids have minimal effect on the pain and tissue injury associated with sunburn, and that non-steroidal-anti-inflammatory drugs (NSAIDs) may have an effect on pain and erythema, but the effect tends to diminish after 24–36 hours.12,14 Antihistamines have been proven to be ineffective.12 Emollients (aloe vera, etc.) may be helpful for controlling pain and decreasing sunburn associated symptoms, but studies do not support the idea that emollients decrease the recovery time from sunburn.12 Han and Maibach (2004), state that based on published evidence, the most logical treatment of sunburn is symptomatic relief with emollients, and pain control via medications if needed.12 Included in this regimen would be cool compresses and oatmeal soaks in cool water for relief.12
Conclusions
Exercise related heat illness and sunburns, particularly the milder forms, are very common problems for athletes training or competing in hot climates or during the hotter seasons of the year. The best treatment approach, as with all injuries, is prevention. The major modifiable risk factors for heat illness are exercising in high heat and humidity, dehydration, and acclimatization, while the modifiable risk factor for sunburn is sun exposure. For the mild to moderate forms of heat illness, quick identification of signs and symptoms, followed by rapid cooling and proper re-hydration comprises the basic principle for emergency treatment. For the emergency situation of heat stroke, rapid and aggressive cooling is essential to reduce mortality. Best evidence treatment of sunburn seems to be symptomatic relief with emollients and pain control via medications. Ultimately, both exercise related heat illness and sunburn are preventable injuries. Consequently, it is the responsibility of those caring for athletes, the parents, coaches, trainers, and team doctors, to ensure that athletes are educated in preventative strategies and are properly monitored during training or competition in the heat. Chiropractors, as primary contact health care providers, are ideally suited to provide this type of education and care to athletes, physically active patients, and to the general population.
Acknowledgments
The author would like to thank Dr. Robert Gringmuth for the opportunity to travel with the team referenced in this article, and Dr. Brian Gleberzon and Christine Miners for editing the manuscript prior to publication.
Footnotes
Disclaimer: No funding was received for this report. The author has no commercial associations that might pose a conflict of interest in connection with the submitted article.
References
- 1.Coris EE, Ramirez AM, Van Durme DJ. Heat illness in athletes: the dangerous combination of heat, humidity and exercise. Sports Medicine. 2004;34(1):9–16. doi: 10.2165/00007256-200434010-00002. [DOI] [PubMed] [Google Scholar]
- 2.Glazer JL. Management of heatstroke and heat exhaustion. American Family Physician. 2005;71(11):2133–2140. [PubMed] [Google Scholar]
- 3.Purdue MP, Marrett LD, Peters L, Rivers JK. Predictors of sunburn among Canadian adults. Preventive Medicine. 2001;33:305–312. doi: 10.1006/pmed.2001.0888. [DOI] [PubMed] [Google Scholar]
- 4.Hall HI, McDavid K, Jorgensen CM, Kraft JM. Factors associated with sunburn in white children aged 6 months to 11 years. Am J Preventive Medicine. 2001;20(1):9–14. doi: 10.1016/s0749-3797(00)00265-8. [DOI] [PubMed] [Google Scholar]
- 5.Snowise M, Dexter WW. Cold, wind, and sun exposure: managing and preventing skin damage. The Physician and Sportsmedicine. 2004;32(12) doi: 10.3810/psm.2004.12.676. [DOI] [PubMed] [Google Scholar]
- 6.Cheung SS, McLellan TM, Tenaglia S. The thermophysiology of uncompensable heat stress. Sports Medicine. 2000;29(5):329–359. doi: 10.2165/00007256-200029050-00004. [DOI] [PubMed] [Google Scholar]
- 7.Wendt D, van Loon LJC, van Marken Lichtenbelt WD. Thermoregulation during exercise in the heat: strategies for maintaining health and performance. Sports Medicine. 2007;37(8):669–682. doi: 10.2165/00007256-200737080-00002. [DOI] [PubMed] [Google Scholar]
- 8.Marsh SA, Jenkins DG. Physiological responses to the menstrual cycle: implications for the development of heat illness in female athletes. Sports. 2002;32(10):601–614. doi: 10.2165/00007256-200232100-00001. [DOI] [PubMed] [Google Scholar]
- 9.Noakes TD. A modern classification of the exercise-related heat illnesses. J Science and Medicine in Sport. 2008;11:33–39. doi: 10.1016/j.jsams.2007.02.009. [DOI] [PubMed] [Google Scholar]
- 10.Armstrong LE, Epstein Y, Greenleaf JE, Haymes EM, Hubbard RW, Roberts WO, Thompson PD. Heat and cold illnesses during distance running. Medicine & Science in Sports & Exercises. 1996;28(10):139–148. [PubMed] [Google Scholar]
- 11.Naughton GA, Carlson JS. Reducing the risk of heat-related decrements to physical activity in young people. J Science and Medicine in Sport. 2008;11:58–65. doi: 10.1016/j.jsams.2006.07.009. [DOI] [PubMed] [Google Scholar]
- 12.Han A, Maibach HI. Management of acute sunburn. Am J Clinical Dermatology. 2004;5(1):39–47. doi: 10.2165/00128071-200405010-00006. [DOI] [PubMed] [Google Scholar]
- 13.Dupuy A, Dunant A, Grob JJ. Randomized controlled trial testing the impact of high-protection sunscreens on sun-exposure behaviour. Arch Dermatology. 2005;141:950–956. doi: 10.1001/archderm.141.8.950. [DOI] [PubMed] [Google Scholar]
- 14.Duteil L, Queille-Roussel C, Lorenz B, Thieroff-Ekerdt R, Ortonne JP. A randomized, controlled study of the safety and efficacy of topical corticosteroid treatments of sunburn in healthy volunteers. Clinical and Experimental Dermatology. 2002;27:314–318. doi: 10.1046/j.1365-2230.2002.01033.x. [DOI] [PubMed] [Google Scholar]
- 15.Sawka MN, Montain SJ. Fluid and electrolyte supplementation for exercise heat stress. Clinical Nutrition. 2000;72(suppl):564S–572S. doi: 10.1093/ajcn/72.2.564S. [DOI] [PubMed] [Google Scholar]
- 16.Maughan R, Shirreffs S. Exercise in the heat: challenges and opportunities. J Sports Sciences. 2004;22:917–927. doi: 10.1080/02640410400005909. [DOI] [PubMed] [Google Scholar]
- 17.Von Duvillard SP, Braun WA, Markofski M, Beneke R, Leithäuser R. Fluids and hydration in prolonged endurance performance. Nutrition. 2004;20(7/8):651–656. doi: 10.1016/j.nut.2004.04.011. [DOI] [PubMed] [Google Scholar]
- 18.Hargreaves M. Physiological limits to exercise performance in the heat. J Science and Medicine in Sport. 2008;11:66–71. doi: 10.1016/j.jsams.2007.07.002. [DOI] [PubMed] [Google Scholar]
- 19.Smith JE. Cooling methods used in the treatment of exertional heat illness. Br J Sports Medicine. 2005;39:503–507. doi: 10.1136/bjsm.2004.013466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hadad E, Rav-Acha M, Heled Y, Epstein Y, Moran DS. Heat stroke: a review of cooling methods. Sports Medicine. 2004;34(8):501–511. doi: 10.2165/00007256-200434080-00002. [DOI] [PubMed] [Google Scholar]