Abstract
Background
Aspiration of gastric contents is a serious problem in critically ill, mechanically ventilated patients receiving tube feedings.
Objectives
To evaluate the effectiveness of a three-pronged intervention to reduce aspiration risk in a group of critically ill, mechanically ventilated patients receiving tube feedings.
Method
A two-group quasi-experimental design was used to compare outcomes of a usual care group (December 2002–September 2004) with those of an Aspiration Risk Reduction Protocol (ARRP) group (January 2007–April 2008). The incidence of aspiration and pneumonia were compared between the usual care group (n = 329) and the ARRP Group (n = 145). The ARRP had three components: maintaining head-of-bed elevation at 30 degrees or higher, unless contraindicated; inserting feeding tubes into distal small bowel, when indicated; and using an algorithmic approach for high gastric residual volumes.
Results
Two of the three ARRP components were implemented successfully. Almost 90% of the ARRP group had mean head-of-bed elevations of 30 degrees or higher as compared to 38% in the usual care group. Almost three-fourths of the ARRP group had feeding tubes placed in the small bowel, as compared to less than 50% in the usual care group. Only three patients met the criteria for the high gastric residual volume algorithm. Aspiration was much lower in the ARRP group than in the usual care group (39% versus 88%, respectively). Similarly, pneumonia was much lower in the ARRP group than in the usual care group (19% versus 48%, respectively).
Discussion
Findings from this study suggest that a combination of a head-of-bed position elevated to at least 30 degrees and use of a small-bowel feeding site can reduce the incidence of aspiration and aspiration-related pneumonia dramatically in critically ill, tube-fed patients.
Keywords: enteral nutrition, respiratory aspiration, preventive measures
Frequent aspiration of gastric contents predisposes tube-fed patients to pneumonia, especially those who are critically ill and mechanically ventilated. Airway protection from regurgitated gastric contents often is impaired in these patients by underlying illness, sedation, or both. A number of interventions have been proposed to minimize aspiration. For example, a research-based guideline issued by the Centers for Disease Control and Prevention recommends a head-of-bed position elevated to at least 30 degrees to reduce risk for aspiration-related pneumonia (Tablan et al., 2004). Further, a frequently cited study of aspiration in mechanically ventilated patients found that aspiration was significantly more likely when patients were supine; however, it also occurred when they were semirecumbent (Torres et al., 1992). Findings from the Torres et al. study are convincing in that the methods used to detect aspiration were scientifically sound (radiolabeled enteral formula and comparisons between organisms found in the subjects’ stomachs and lungs). Other investigators have found that risk for pneumonia is increased by a low backrest elevated position (Grap et al., 2005). Investigators have shown that written medical orders for head-of-bed elevation are helpful in encouraging staff to maintain the appropriate backrest elevation (Helman, Sherner, Fitzpatrick, Callender, & Shorr, 2003). There is widespread agreement that an elevated head-of-bed position is helpful in reducing aspiration and pneumonia (Torres et al, 1992, Tablan et al, 2004; Grap et al., 2005).
A distal small-bowel feeding site has been also recommended to reduce aspiration risk, though it is less well-substantiated by research; presumably a small bowel feeding site reduces the likelihood of gastroesophageal reflux (Heyland, Drover, Dhaliwal, & Greenwood, 2002). Studies of the relationship between small-bowel feedings and aspiration have produced conflicting results. For example, in a study of 33 critically ill patients, Heyland et al. used radio-labeled formula to assess the extent of aspiration when feeding tubes were situated in various segments of the gastrointestinal tract (Heyland, Drover, MacDonald, Novak, & Lam, 2001). The rate of aspiration was 5.8% in the stomach (n = 21); 4.1% in the first portion of the duodenum (n = 8), 1.8% in the second portion of the duodenum (n = 3); and 0% in the fourth portion of the duodenum (n = 1). Overall, patients fed in the stomach tended to have more microaspiration than patients fed beyond the pylorus (7.5% vs. 3.9%, p = .22). When the logarithmic mean of the radioactivity count was compared across groups, there was also a trend toward increased microaspiration (1.9 vs.1.4 counts/g, p =.09) in patients fed into the stomach (Heyland et al., 2001). However, also using radio-labeled enteral formula, other investigators found no significant difference in aspiration in 27 patients fed in the stomach and 24 fed transpylorically (7% versus 13%, respectively; Esparza, Boivin, Hartshorne, & Levy, 2001). Although Heyland et al. (2001) and Esparza et al. (2001) used a reliable test for aspiration, both studies had relatively small sample sizes. Another problem with the Esparza et al. (2001) study was failure to provide information about the degree of aspiration encountered in patients fed in different portions of the small bowel. Despite the conflicting research findings regarding feeding tube location, many physicians prefer small-bowel feedings in patients at high risk for aspiration, provided the procedure can be performed at the bedside by bedside nurses (Heyland, Cook, & Dodek, 2002). There is evidence that bedside nurses can be taught how to successfully place feeding tubes into the distal small bowel (Welch, 1996).
Finally, an algorithmic approach to deal with high gastric residual volumes (GRV) has been proposed (Bourgault, Ipe, Weaver, Swartz, & O’dea, 2007; Kattelmann et al., 2006). For example, it has been recommended that gastric feedings be interrupted when a residual volume of 500 ml or more is identified (McClave et al., 2002) and it has been suggested that prokinetic drugs be initiated when GRVs of 250 ml or greater are identified (Booth, Heyland, & Paterson, 2002; Nguyen et al., 2007). A drawback to the use of prokinetics is their potential to produce undesirable side effects, such as dystonic reactions (Dubow, Leikin, & Rezak, 2006; Kenney, Hunter, Davidson, & Jankovic, 2008; Pasricha, Pehlivanov, Sugumar, & Jankovic, 2006; van der Padt, van Schalk, & Sonneveld, 2006).
Although the effects of single risk factors for aspiration have been studied previously, no studies were identified in which the combined effect of postpyloric tube site, head-of-bed elevation, and gastric residual volume were evaluated. Because it is likely that a combination of aspiration-risk-reducing interventions will be more beneficial than a single intervention, the study reported here was used to evaluate the effectiveness of a three-pronged intervention to reduce aspiration risk in a group of critically ill, mechanically ventilated tube-fed patients.
Method
Design
A two-group quasi-experimental design was used to compare outcomes of a usual care group with those of an Aspiration Risk Reduction Protocol (ARRP) group. Both groups included critically ill, mechanically ventilated tube-fed patients cared for in the same intensive care units (ICUs). The primary outcomes of interest were the frequency of aspiration and the incidence of pneumonia. A secondary outcome was the use of hospital resources (length of hospitalization, length of intensive care stay, and number of days of mechanical ventilation). The study was approved by the appropriate institutional review boards. A secondary data analysis was performed on the usual care group. Patients in the usual care group who had surgically or endoscopically placed tubes were eliminated from the analysis for the work reported here.
Setting
Both phases of the study took place in the same five ICUs at a Level I trauma center in the Midwest. Major services provided in the ICUs included neuromedicine/neurosurgery, trauma/surgery, and general medicine/pulmonary medicine.
Subjects
The usual care group (n = 329) was studied prospectively between December 2002 and September 2004 (Metheny et al., 2006). The ARRP Group (n = 145) was studied prospectively between January 2007 and April 2008. Inclusion criteria for the ARRP group were the same as for the usual care group: a) admitted to one of the five ICUs at the study site, (b) age ≥ 18 years; (c) informed consent of patient or legal guardian; (d) mechanical ventilation; and (e) medical order for blind insertion of feeding tube at bedside. Exclusion criteria were: (a) pneumonia present before tube feeding started; and (b) medical order for surgically or endoscopically placed feeding tube.
All patients who met the criteria were invited to participate for a 3-day period. While the ARRP was implemented for all tube-fed patients in the ICUs, data were collected only on those who gave informed consent. Registered nurse research assistants were present 16 hours a day, 7 days a week, to recruit patients, obtain informed consents, and collect data. The same measurements were made on the usual care group and ARRP group.
Independent Variable
The independent variable consisted of the two treatment conditions (usual care and the ARRP).
Usual care was defined as the absence of a systematic approach to minimize risk for aspiration. In 2002–2004, standing medical orders on the ICUs did not routinely include information about head-of-bed elevation and nurses did not chart head-of-bed angles on the patients’ flow sheets. Further, no formal program was in place to teach ICU nurses how to place small-bowel feeding tubes. Finally, there was no standardized approach for dealing with high gastric residual volumes.
The ARRP had three components: (a) maintain head-of-bed elevation at 30 degrees or higher, unless medically contraindicated; (b) insert feeding tube into distal small bowel, when requested by the attending physician; and (c) initiate an algorithmic approach for high gastric residual volumes.
Prior to initiation of the study in 2007, the hospital nursing practice committee and the ICU medical directors approved the ARRP for use in the ICUs, and 2 months prior to data collection, an advanced practice nurse skilled in critical care and nasoenteral tube placement initiated an educational program to introduce the protocol to the ICU staff. This nurse was present 40 hours a week during the ARRP phase of the study to encourage adoption of the protocol in the ICUs involved. Coaching by the advanced practice nurse consisted of a combination of teaching, training, and counseling designed to promote diffusion of the ARRP components. The advanced practice nurse also provided monthly feedback about implementation of the interventions and reinforced desired behaviors by emphasizing successful aspects of the protocol delivery.
Maintain head-of-bed elevation at 30 degrees or higher, unless medically contraindicated
Attending physicians were encouraged to write orders for the desired head-of-bed elevation and this action promoted appropriate patient positioning. Also, bedside nurses were encouraged to record head-of-bed angles at hourly intervals on the patients’ ICU flow sheets; this action reminded the nurses to check the bed position frequently and make corrections as necessary.
Insert feeding tube into distal small bowel, when requested by attending physician
Physicians were informed that the advanced practice nurse would assist ICU nurses with small-bowel tube insertions at the bedside. Thus, physicians were able to write orders more freely for bedside small-bowel tube insertions when they were deemed important for high-risk patients. The advanced practice nurse demonstrated small-bowel tube insertion to bedside nurses who were unskilled in this procedure and coached these nurses during small-bowel tube insertions until they gained proficiency in the procedure. To facilitate learning further, a videotape of a successful tube insertion was made available in all of the ICUs for nurses to view at their discretion.
The tube insertion procedure consisted of several steps. First, the patient’s attending physician was contacted to obtain permission to administer metoclopramide, 10 mg, intravenously. If permission was obtained, the medication was administered 10 minutes prior to introduction of the feeding tube through the patient’s mouth or right or left naris (whichever was most appropriate). Metoclopramide increases gastric and small intestinal motility and thus facilitates placement of a feeding tube into the small bowel (Rohm, Boldt, & Piper, 2009). The feeding tube was advanced to the 55 to 60 cm mark and an attempt was made to aspirate gastric contents. If an aspirate was obtained, its pH was measured with a pH test-strip and the appearance of the aspirate was observed. If the pH was 6 or higher, and the aspirate had the appearance of sputum, the tube was removed and a second attempt was made to insert the tube via the esophagus into the stomach. A pH less than 6 and as aspirate with a gastric appearance was used as an indication of tube placement in the stomach. The feeding tube was advanced gently with a rotating motion. When the 90 to 100 cm mark was reached, another attempt to aspirate fluid was made. This attempt was facilitated by injecting 30 ml of air through the tube to force the tube’s ports away from the intestinal mucosa. An aspirate pH ≥ 6 with bile staining was used as an indication of tube placement past the pylorus. A confirmatory radiograph was obtained to determine actual tube location.
Detect and manage high gastric residual volumes
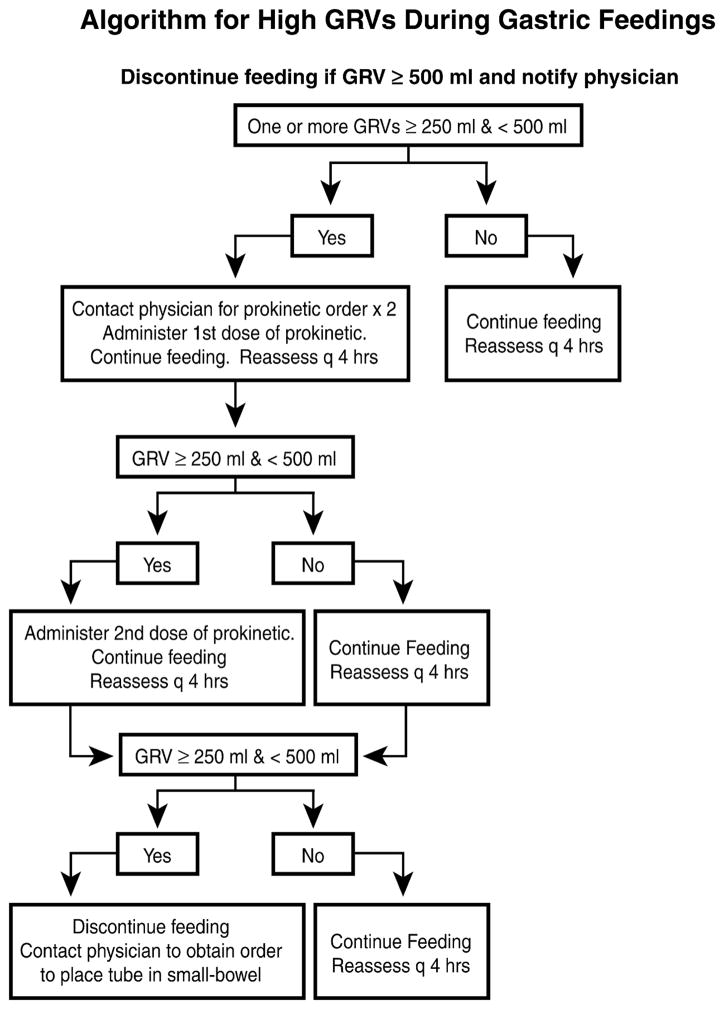
The algorithmic approach used to manage high GRVs during gastric feedings is depicted in Figure 1.
Figure 1.
Algorithm outlining actions for high gastric residual volumes observed during gastric feedings.
Measurements
Measurements performed on the usual care and ARRP groups are summarized in Table 2 and described below. All of the registered nurse data collectors were trained by the principal investigator and the project director on scoring of the measurements prior to data collection.
Table 2.
Patient Measurements, Scoring, and Frequency
| Measurements | Scoring | Frequency |
|---|---|---|
| Aspiration of Gastric Contents (Pepsin immunoassay performed on tracheal secretions) | 1 = present, 0 = absent | Each time patient is suctioned |
| Pneumonia (Simplified Clinical Pulmonary Infection Score; CPIS) | Range 0–10 | Every 24 hours |
| ≥ 6 positive for pneumonia | Days 1, 2, 3, 4 | |
| Use of Hospital Resources | ||
| Hospital length of stay | Time of discharge or death | |
| ICU length of stay | Days | |
| Ventilator use | ||
| Head-of-bed angle | Degrees (0–90) | Every hour |
| Feeding site | ||
| Stomach | Time of initial x-ray and every 4 hours thereafter | |
| First portion of duodenum | ||
| Second & third portion duodenum | ||
| Fourth portion of duodenum | ||
| Proximal jejunum | ||
| Level of consciousness (Glasgow Coma Scale) | Range 3–15 | Every 4 hours |
| Level of sedation (Vancouver Interaction and Calmness Score) | Range 10–60 | Every 4 hours |
| Gastric Residual Volume | Number ≥ 250 ml | Every 4 hours |
| APACHE II Score | 0–71 | At time of admission to ICU |
Note. APACHE II = Acute Physiology and Chronic Health Evaluation II
Pepsin assay to detect aspiration of gastric contents
Bedside nurses collected tracheal secretions in sputum traps during routine suctioning (between 0800 and 2400 hours) on Days 1, 2, and 3. The specimens were treated and frozen at minus 20 degrees Centigrade in a hospital laboratory prior to being transported to a research laboratory for pepsin analysis. The immunoassay used for pepsin analysis has been described previously (Metheny et al., 2006). In an animal model study, the assay was shown to have a sensitivity of 92.5% and a specificity of 100% (Metheny et al., 2004). The same biochemist, blinded to patients’ clinical status, interpreted all of the assays and recorded the results as either positive or negative. A positive reading indicated that the specimen contained pepsin in a concentration ≥ 1 μg/ml. The percentage of pepsin-positive tracheal secretions was calculated for each patient. The mean number of tracheal secretions assayed per patient was 15.9 ± 4.7 in the usual care group and 13.1 ± 4.2 in the ARRP group.
Clinical pulmonary infection score
The Clinical Pulmonary Infection Score (CPIS) described in Table 3 was used to assess for pneumonia at the end of Days 1, 2, 3, and 4 (Luna et al., 2006). Data on infiltrates were obtained from radiographic reports. The first blood gas of the day was used to calculate the oxygenation PaO2/FiO2 ratio. Bedside nurses estimated the volume and appearance of tracheal secretions at the time of routine suctioning. Blood leukocyte data were obtained from laboratory reports, and temperature data were obtained from the medical records. When an infiltrate was present, a CPIS score ≥ 6 was used as a proxy for pneumonia. The same individual, blinded to the pepsin assay results, calculated all of the CPIS scores. In an earlier study, investigators found significant agreement (r = .96) between the simplified CPIS results and 34 bronchoalveolar lavages (p < .001; Metheny et al., 2006). Another group of investigators compared postmortem examinations of 38 patients who had died after at least 72 hours of mechanical ventilation and compared their CPIS scores with bronchoscopic and histological techniques; according to their findings, the CPIS had a sensitivity of 72% and a specificity of 85% for pneumonia (Papazian et al., 1995).
Table 3.
Simplified Clinical Pulmonary Infection Score (CPIS)
| Component | Value | Points |
|---|---|---|
| Temperature (Centigrade, degrees) | ≥ 36.5 and ≤ 38.4 | 0 |
| ≥ 38.5 and ≤ 38.9 | 1 | |
| ≥ 39.9 and ≤ 36.0 | 2 | |
| Blood leukocytes per mm3 | ≥ 4,000 and ≤ 11,000 | 0 |
| < 4,000 or > 11,000 | 1 | |
| Tracheal secretions | Few | 0 |
| Moderate | 1 | |
| Large | 2 | |
| Purulent | +1 | |
| Oxygenation (PaO2/FiO2 mm Hg) | > 240 or presence of ARDS | 0 |
| ≤ 240 and absence of ARDS | 2 | |
| Chest radiograph | No infiltrate | 0 |
| Patchy or diffuse infiltrate | 1 | |
| Localized infiltrate | 2 |
Note. ARDS = Acute respiratory distress syndrome; CPIS = Clinical Pulmonary Infection Score
Use of hospital resources
Information needed to calculate hospital length of stay, ICU length of stay and ventilator days was obtained through chart review.
Angle of head-of-bed
During both phases of the study, registered nurse data collectors determined hourly backrest angles from digital readouts available on the patients’ beds (Stryker Medical, Kalamazoo, MI). During the ARRP phase of the study, the bedside nurses were encouraged to use the beds’ digital readouts to determine hourly backrest elevations and to record their findings on the patients’ flow sheets. The same beds were in use during both phases of the study. In a previous study, investigators compared 1,002 readings made between digital readouts on the Stryker Apex or Stryker EPIC II Critical Care beds and those obtained from a handheld angle reader; the Pearson correlation was .87, p < .001. However, the mean bed readouts tended to be higher than the mean readings obtained from the handheld device (21.3 ± 13.3 vs. 18.9 ± 11.7; Metheny et al., 2006).
Feeding tube site
Radiographic confirmation of tube location was obtained immediately after tube insertion; also at this time, the length of tubing extending from the exit site was measured with a centimeter tape. This measure was repeated at 4-hour intervals between 0800 and 2400 on Days 1, 2, and 3; also assessed at these times were the pH and appearance of fluid aspirated from the feeding tubes. The efficacy of these measures in detecting tube dislocation has been described previously (Metheny et al., 2005).
When there was concern about possible tube dislocation, the need for a radiograph was discussed with the patient’s attending physician. In addition, reports of radiographic studies performed on Days 1, 2, and 3 were reviewed to observe for radiographic evidence of tube movement. Most patients had at least one treatment-related x-ray during the study period that included information about the feeding tube’s location.
Residual volumes from feeding tubes
Research nurses used 60 ml syringes to measure volumes from feeding tubes every 4 hours. Approximately 30 ml of air was injected into the feeding tube prior to each attempt to withdraw fluid from the tube; then slow and steady negative pressure was applied with the plunger. The procedure was repeated until no more fluid could be withdrawn. The total volume of fluid removed from the feeding tube was reported in milliliters. Policy at the data collection site called for returning a gastric residual volume of 200 ml or less to the patient and discarding of any amount greater than 200 ml.
Level of consciousness
The Glasgow Coma Scale (GCS), adjusted for use with intubated patients, was used by the research nurses to assess patients’ level of consciousness at 4-hour intervals from 0800 through 2400. Scoring of the GCS is based on three components (best eye response, best motor response, and best verbal response). The worst possible total score is 3 and the best possible total score is 15. Because all of the patients were intubated tracheally, the verbal response was scored as generally unresponsive, ability to converse is in question, or appears able to converse. In a prospective, observational study, two observers determined the GCS of 39 poisoned patients; the weighted kappa score for the total GCS was .85; weighted kappa scores for individual components of the GCS ranged between .63 and .78 (Heard & Bebarta, 2004). In a review of published studies in which GCS was used, the tool was found to have good reliability (intraclass correlation coefficient, .8 to 1.0 for trained users); further, it was found to have well-established cross-sectional construct validity (Prasad, 1996).
Level of sedation
The Vancouver Interaction and Calmness Scale (VICS) was used to assess patients’ level of sedation (de Lemos, Tweeddale, & Chittock, 2000). This scale was developed for use with adult, critically ill, mechanically ventilated patients and it consists of two 5-item subscales quantifying interaction along a continuum from 5 to 30 points; the scores may range from 10 to 60. A low score indicates a high level of sedation. The tool’s developers report interrater reliability for the two scales as .89 and .90, and internal consistency as .95 for both subscales (de Lemos et al., 2000).
Severity of disease
The Acute Physiology and Chronic Health Evaluation II (APACHE II) score was calculated at the time of the patient’s admission to the ICU. This tool is designed to measure the severity of disease for adult patients admitted to ICUs. The tool has three components: the acute physiology score (APS), age, and chronic health. Overall, an integer score from 0 to 71 is computed on the basis of temperature, mean arterial pressure, heart rate, respiration rate, oxygenation, serum sodium, serum potassium, serum creatinine, hematocrit, white blood count, Glasgow Coma Score, age, and chronic health points (Knaus, Draper, Wagner & Zimmerman, 1985). Higher scores imply more severe disease state and greater risk for death. The APS component of the APACHE II instrument is highly reproducible (intraclass correlation coefficient = .90), and the age component of the instrument has an even higher reproducibility (intraclass correlation coefficient = .998). The chronic health component of the instrument does not fare as well (kappa = .66; Damiano, Bergner, Draper, Knaus, & Wagner, 1992).
Other observations
Demographic information was obtained by chart review. The number of vomiting episodes was determined by interviewing bedside nurses and by chart review.
Data Analysis
Simple descriptive statistics were used to describe the sample. To determine the effect of the ARRP on frequency of aspiration, a t-test for independent groups was used to compare patients in the usual care and ARRP groups on the mean percentage of pepsin-positive tracheal secretions. To determine the effect of the ARRP on the incidence of pneumonia, a z-test for comparing proportions in independent groups was used to compare the proportion of usual care patients with the proportion of ARRP patients with a positive CPIS for pneumonia on Day 4. Significant baseline differences between the two groups were controlled for in the analyses. To evaluate the effect of the ARRP on hospital resources, usual care and ARRP groups were compared using a z-test from the Mann Whitney U procedure, because the secondary outcomes of hospital length of stay, ICU length of stay, and days of ventilator use had skewed distributions.
Results
Descriptive Data
Descriptive data on both groups are provided in Table 1. As shown in Table 1, the ARRP and usual care groups did not differ in gender, level of consciousness, and the service that provided care. However, the ARRP group was younger, had a lower mean APACHE II score, and was less sedated than the usual care group.
Table 1.
Description of Usual Care and Aspiration Risk Reduction Protocol Groups
| Variable | Usual Care (n = 329) | ARRP Group (n = 145) |
|---|---|---|
| Age (in years) | 52.5 ± 18.1 | 48.8 ± 17.8* |
| Gender | ||
| Female | 42.9% | 35.2% |
| Male | 57.1% | 64.8% |
| APACHE II | 22.7 ± 6.4 | 19.5 ± 5.7** |
| Service | ||
| Neuromedicine/Neurosurgery | 30.4% | 33.2% |
| Trauma/Surgery | 39.8% | 44.8% |
| General Medicine/Pulmonary Medicine | 29.8% | 22.1% |
| Level of consciousness (Mean Glasgow Coma Scale Score) | 7.0 ± 2.8 | 6.9 ± 2.2 |
| Level of sedation (Mean Vancouver Interaction & Calmness Score) | 35.7 ± 4.1 | 36.5 ± 4.1* |
| Feeding site | ||
| Stomach throughout study | 47.7% | 27.6%** |
| Small bowel throughout study | 40.7% | 69.7% |
| Switch from stomach to small bowel | 4.0% | 0.0% |
| Switch from small bowel to stomach | 7.6% | 2.8% |
| Type of device during gastric feedings | ||
| 10 Fr polyurethane tube | 47.1% | 75.0%** |
| 14–18 Fr polyvinyl chloride tube | 52.9% | 25.0% |
| Type of device during small bowel feedings | ||
| 10 Fr polyurethane tube | 100% | 100% |
| One or more gastric residual volumes ≥ 250 ml in gastric-fed patients | 15.9% | 7.5% |
| Vomited at least once | 5.8% | 5.5% |
| Mean backrest elevation (degrees) | 23.7 ± 12.4 | 37.8 ± 9.1** |
| Mean percent backrest elevation ≥ 30 degrees | 37.7% | 88.4%** |
| Died during hospitalization | 19% | 14% |
Note. ARRP = Aspiration Risk Reduction Protocol Group; APACHE II = Acute Physiology and Chronic Health Evaluation II
p = < .05;
p = < .001
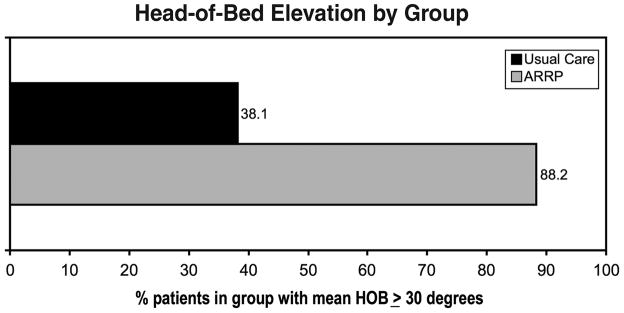
The mean head-of-bed elevation was significantly higher in the ARRP group than in the usual care group (37.8 ± 9.1 versus 23.7 ± 12.4 degrees, respectively, p < .001). Further, a mean head-of-bed elevation ≥ 30 degrees was achieved in 88% of the ARRP group as opposed to 38% of the usual care group (p < .001; Figure 2). Physicians included orders for the desired head-of-bed angle in 90% (n = 130) of the 145 ARRP patients. Bedside nurses charted the head-of-bed angle in 44% of the possible observations.
Figure 2.
Comparison of percentages of mean head-of-bed elevations equal to or greater than 30 degrees in the usual care and ARRP groups.
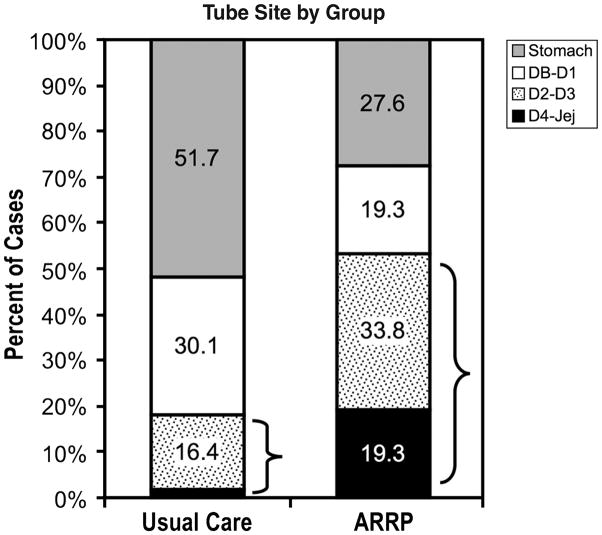
As shown in Figure 3, a small-bowel feeding site was achieved in 72.4% of the ARRP group, compared to 48.3% of the usual care group (p < .001). Further, tube placement past the proximal duodenum was achieved in 53.1% of the ARRP group, compared to 18.2%, of the usual care group (p < .001).
Figure 3.
Comparison of feeding tube sites in the usual care and ARRP groups.
Three patients in the ARRP group met the criteria for implementation of the high GRV algorithm depicted in Figure 1. One patient had nine high GRVs (ranging between 300 ml and 700 ml), a second had two high GRVs (both 350 ml), and a third had one GRV of 325 ml. However, physicians chose not to implement the algorithm in any of the cases.
Effect of the ARRP on Aspiration, Pneumonia, and Use of Hospital Resources
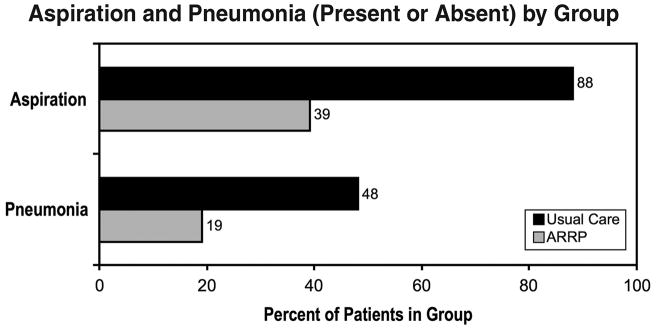
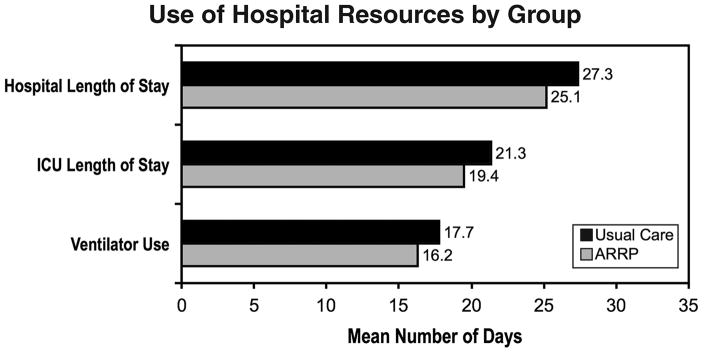
Aspiration was significantly lower in patients in the ARRP group than in usual care group, as evidenced by a lower mean percentage of pepsin-positive tracheal secretions (12.4 ± 21.8% versus 30.9 ± 24.2%, p < .001). Aspirating at least once was half as likely in the ARRP group as in the usual care group (39.3% versus 88.4%, p < .001). Further, pneumonia occurred in less than one-fifth of the ARRP group but in nearly half of the usual care group (19.3% versus 48.2%, p < .001; Figure 4). The ARRP patients were hospitalized on average 2.2 fewer days than usual care patients (25.1 ± 14.9 versus 27.3 ± 13.4, z from Mann Whitney U = −2.39, p = .017), and the average ICU length of stay for ARRP patients was 1.9 fewer days than for usual care patients (21.3 ± 10.5 versus 19.4 ± 12.1, z from Mann Whitney U = −2.46, p = .014). Finally, ARRP patients averaged 1.5 fewer days of mechanical ventilation than the usual care patients (16.2 ± 9.7 versus 17.7 ± 9.8, respectively, z from Mann Whitney U = −1.46, p = .14; Figure 5). When the usual care and ARRP groups were compared on the outcome variables using age, APACHE II, and sedation as covariates, the results were nearly identical.
Figure 4.
Comparison of aspiration and pneumonia (present or absent) in the usual care and ARRP groups.
Figure 5.
Comparison of use of hospital resources by the usual care and ARRP groups.
Discussion
Success in Delivery of the ARRP
Two of the three components of the ARRP were implemented successfully. That is, almost 90% of the ARRP group had mean head-of-bed elevations of 30 degrees or higher and almost three-fourths had feeding tubes placed in the small bowel (most beyond the proximal duodenum).
Successful implementation of a head-of-bed elevated position probably was influenced by a number of factors. Written medical orders regarding the desired backrest angle eliminated the possibility of elevating the backrest inappropriately and reminded staff of the importance of proper positioning. Frequent documentation of the backrest angle ensured corrections as needed. Also, the documentation probably enhanced the nurses’ sense of responsibility for appropriate patient positioning. A factor that also may have had a significant effect on the greater use of an elevated head-of-bed position in the ARRP group, as compared to the usual care group, was the growing number of publications emphasizing the need for an elevated head-of-bed position to prevent pneumonia (Tablan et al, 2004; Grap et al., 2005).
Successful implementation of small-bowel feeding tube insertions also probably was influenced by several factors. Many physicians prefer small-bowel feedings in patients at high risk for aspiration, provided the procedure can be performed at the bedside by bedside nurses; and in this study the educational program provided by the advanced practice nurse allowed a cadre of bedside nurses in the five ICUs to significantly improve their success in placing small-bowel feeding tubes.
Poor use of the algorithm was due to reluctance of the attending physicians to prescribe prokinetic agents for the three patients who met the criteria in the algorithm depicted in Figure 1. In all three cases, the physicians expressed concern about recent published reports of possible undesirable effects associated with prokinetic agents (Dubow et al, 2006; Kenney et al, 2008; Pasricha et al, 2006; van der Padt et al, 2006).
Improvement in Outcomes
To determine if younger age, better APACHE II score, and lower level of sedation had a significant effect on outcomes (aspiration and pneumonia), these factors were entered as covariates in the analyses. These factors had no significant effect on outcomes when the two groups were compared.
The combination of an elevated head-of-bed position and a mid-to-distal small-bowel feeding site probably contributed to the significantly less aspiration and pneumonia in the ARRP group than in the usual care group. The shorter hospital and ICU lengths of stay in the ARRP group were modest and doubtless influenced by the lower incidence of pneumonia.
Head-of-bed elevation
The supine position is a well-recognized risk factor for aspiration. As indicated earlier, there is widespread agreement that an elevated head-of-bed position is helpful in reducing aspiration and pneumonia (Torres et al, 1992, Tablan et al, 2004; Grap et al., 2005).
Small-bowel feeding site
Findings from the study reported here support those of other investigators who used a sensitive and specific test for aspiration of gastric contents (Heyland et al, 2001).
Gastric residual volume
Because the algorithm for high GRVs during gastric feedings was not implemented in the three ARRP patients with one or more GRVs ≥ 250 ml, it was not possible to determine what effect it might have had on their rates of aspiration (which ranged between 50% and 100%).
The study reported here adds to the evidence that an elevated head-of-bed position is helpful in preventing aspiration and pneumonia; further, it adds to the evidence that a distal small-bowel feeding site is associated with less aspiration than is the gastric feeding site. It is regrettable that the GRV component of the protocol could not be implemented and evaluated.
Strengths of the Study
The highly sensitive and specific pepsin assay allowed an accurate comparison of the two groups on aspiration and the large sample size provided adequate power to compare the usual care and ARRP groups on the major outcome variables (aspiration and pneumonia). The presence of skilled registered nurse research assistants for 16 hours a day, 7 days a week throughout both phases of the study allowed for uniformity in data collection procedures.
Limitations
A limitation of the study was the 28-month time lapse between the end of the usual care phase of the study and the beginning of the ARRP phase. It is conceivable that changes that occurred in the clinical site during that period could have accounted for some of the differences in outcomes.
Conclusions
Findings from this study suggest that a combination of a head-of-bed position elevated to at least 30 degrees and use of a small-bowel feeding site (especially beyond the first portion of the duodenum) can reduce the incidence of aspiration and aspiration-related pneumonia dramatically in critically ill, mechanically ventilated patients. It is highly probable that the presence of a skilled critical care nurse with special training in the placement of small-bowel feeding tubes played a significant role in encouraging ICU personnel at the study site to adopt the aspiration-reducing interventions and bring about the desired outcomes shown in this study.
Acknowledgments
This study was funded by the National Institute of Nursing Research, R01NR05007.
Contributor Information
Norma A. Metheny, School of Nursing, Saint Louis University, St. Louis, Missouri.
Jami Davis-Jackson, Department of Heart Services, Barnes-Jewish Hospital, St. Louis, Missouri.
Barbara J. Stewart, Oregon Health & Science University, Portland, Oregon.
References
- Booth CM, Heyland DK, Paterson WG. Gastrointestinal promotility drugs in the critical care setting: A systematic review of the evidence. Critical Care Medicine. 2002;30(7):1429–1435. doi: 10.1097/00003246-200207000-00005. [DOI] [PubMed] [Google Scholar]
- Bourgault AM, Ipe L, Weaver J, Swartz S, O’dea PJ. Development of evidence-based guidelines and critical care nurses’ knowledge of enteral feeding. Critical Care Nurse. 2007;27(4):17–22. 25–29. [PubMed] [Google Scholar]
- Damiano AM, Bergner M, Draper EA, Knaus WA, Wagner DP. Reliability of a measure of severity of illness: Acute physiology of chronic health evaluation--II. Journal of Clinical Epidemiology. 1992;45(2):93–101. doi: 10.1016/0895-4356(92)90001-4. [DOI] [PubMed] [Google Scholar]
- de Lemos J, Tweeddale M, Chittock D. Measuring quality of sedation in adult mechanically ventilated critically ill patients. The Vancouver Interaction and Calmness Scale. Sedation Focus Group. Journal of Clinical Epidemiology. 2000;53(9):908–919. doi: 10.1016/s0895-4356(00)00208-0. [DOI] [PubMed] [Google Scholar]
- Dubow JS, Leikin J, Rezak M. Acute chorea associated with metoclopramide use. American Journal of Therapeutics. 2006;13(6):543–544. doi: 10.1097/01.mjt.0000208271.34755.5b. [DOI] [PubMed] [Google Scholar]
- Esparza J, Boivin MA, Hartshorne MF, Levy H. Equal aspiration rates in gastrically and transpylorically fed critically ill patients. Intensive Care Medicine. 2001;27(4):660–664. doi: 10.1007/s001340100880. [DOI] [PubMed] [Google Scholar]
- Grap MJ, Munro CL, Hummel RS, 3rd, Elswick RK, Jr, McKinney JL, Sessler CN. Effect of backrest elevation on the development of ventilator-associated pneumonia. American Journal of Critical Care. 2005;14(4):325–332. [PubMed] [Google Scholar]
- Heard K, Bebarta VS. Reliability of the Glasgow Coma Scale for the emergency department evaluation of poisoned patients. Human & Experimental Toxicology. 2004;23(4):197–200. doi: 10.1191/0960327104ht436oa. [DOI] [PubMed] [Google Scholar]
- Helman DL, Jr, Sherner JH, 3rd, Fitzpatrick TM, Callender ME, Shorr AF. Effect of standardized orders and provider education on head-of-bed positioning in mechanically ventilated patients. Critical Care Medicine. 2003;31(9):2285–2290. doi: 10.1097/01.CCM.0000079609.81180.15. [DOI] [PubMed] [Google Scholar]
- Heyland DK, Cook DJ, Dodek PM. Prevention of ventilator-associated pneumonia: Current practice in Canadian intensive care units. Journal of Critical Care. 2002;17(3):161–167. doi: 10.1053/jcrc.2002.35814. [DOI] [PubMed] [Google Scholar]
- Heyland DK, Drover JW, Dhaliwal R, Greenwood J. Optimizing the benefits and minimizing the risks of enteral nutrition in the critically ill: Role of small bowel feeding. Journal of Parenteral and Enteral Nutrition. 2002;26(6 Suppl):S51–S55. doi: 10.1177/014860710202600608. [DOI] [PubMed] [Google Scholar]
- Heyland DK, Drover JW, MacDonald S, Novak F, Lam M. Effect of postpyloric feeding on gastroesophageal regurgitation and pulmonary microaspiration: Results of a randomized controlled trial. Critical Care Medicine. 2001;29(8):1495–1501. doi: 10.1097/00003246-200108000-00001. [DOI] [PubMed] [Google Scholar]
- Kattelmann KK, Hise M, Russell M, Charney P, Stokes M, Compher C. Preliminary evidence for a medical nutrition therapy protocol: Enteral feedings for critically ill patients. Journal of the American Dietetic Association. 2006;106(8):1226–1241. doi: 10.1016/j.jada.2006.05.320. [DOI] [PubMed] [Google Scholar]
- Kenney C, Hunter C, Davidson A, Jankovic J. Metoclopramide, an increasingly recognized cause of tardive dyskinesia. Journal of Clinical Pharmacology. 2008;48(3):379–384. doi: 10.1177/0091270007312258. [DOI] [PubMed] [Google Scholar]
- Knaus WA, Draper EA, Wagner DP, Zimmerman JE. APACHE II: A severity of disease classification system. Critical Care Medicine. 1985;13(10):818–829. [PubMed] [Google Scholar]
- Luna CM, Aruj P, Niederman MS, Garzon J, Violi D, Prignoni A, et al. Appropriateness and delay to initiate therapy in ventilator-associated pneumonia. The European Respiratory Journal. 2006;27(1):158–164. doi: 10.1183/09031936.06.00049105. [DOI] [PubMed] [Google Scholar]
- McClave SA, DeMeo MT, DeLegge MH, DiSario JA, Heyland DK, Maloney JP, et al. North American Summit on Aspiration in the Critically Ill Patient: Consensus statement. Journal of Parenteral and Enteral Nutrition. 2002;26(6 Suppl):S80–S85. doi: 10.1177/014860710202600613. [DOI] [PubMed] [Google Scholar]
- Metheny NA, Clouse RE, Chang YH, Stewart BJ, Oliver DA, Kollef MH. Tracheobronchial aspiration of gastric contents in critically ill tube-fed patients: Frequency, outcomes, and risk factors. Critical Care Medicine. 2006;34(4):1007–1015. doi: 10.1097/01.CCM.0000206106.65220.59. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metheny NA, Dahms TE, Chang YH, Stewart BJ, Frank PA, Clouse RE. Detection of pepsin in tracheal secretions after forced small-volume aspirations of gastric juice. Journal of Parenteral and Enteral Nutrition. 2004;28(2):79–84. doi: 10.1177/014860710402800279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Metheny NA, Schnelker R, McGinnis J, Zimmerman G, Duke C, Merrit B, et al. Indicators of tubesite during feedings. The Journal of Neuroscience Nursing. 2005;37(6):320–325. doi: 10.1097/01376517-200512000-00004. [DOI] [PubMed] [Google Scholar]
- Nguyen NQ, Chapman M, Fraser RJ, Bryant LK, Burgstad C, Holloway R. Prokinetic therapy for feed intolerance in critical illness: One drug or two? Critical Care Medicine. 2007;35(11):2561–2567. doi: 10.1097/01.CCM.0000286397.04815.B1. [DOI] [PubMed] [Google Scholar]
- Papazian L, Thomas P, Garbe L, Guignon I, Thirion X, Charrel J, et al. Bronchoscopic or blind sampling techniques for the diagnosis of ventilator-associated pneumonia. American Journal of Respiratory and Critical Care Medicine. 1995;152(6 Pt 1):1982–1991. doi: 10.1164/ajrccm.152.6.8520766. [DOI] [PubMed] [Google Scholar]
- Pasricha PJ, Pehlivanov N, Sugumar A, Jankovic J. Drug insight: From disturbed motility to disordered movement--A review of the clinical benefits and medicolegal risks of metoclopramide. Nature Clinical Practice. Gastroenterology & Hepatology. 2006;3(3):138–148. doi: 10.1038/ncpgasthep0442. [DOI] [PubMed] [Google Scholar]
- Prasad K. The Glasgow Coma Scale: A critical appraisal of its clinimetric properties. Journal of Clinical Epidemiology. 1996;49(7):755–763. doi: 10.1016/0895-4356(96)00013-3. [DOI] [PubMed] [Google Scholar]
- Rohm KD, Boldt J, Piper SN. Motility disorders in the ICU: Recent therapeutic options and clinical practice. Current Opinion in Clinical Nutrition and Metabolic Care. 2009;12(2):161–167. doi: 10.1097/MCO.0b013e32832182c4. [DOI] [PubMed] [Google Scholar]
- Tablan OC, Anderson LJ, Besser R, Bridges C, Hajjeh R Centers for Disease Control & the Healthcare Infection Control Practices Advisory Committee. Guidelines for preventing health-care-associated pneumonia, 2003: Recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee. Morbidity and Mortality Weekly Report. Recommendations & Reports. 2004;53(RR-3):1–36. [PubMed] [Google Scholar]
- Torres A, Serra-Batlles J, Ros E, Piera C, Puig de la Bellacasa J, Cobos A, et al. Pulmonary aspiration of gastric contents in patients receiving mechanical ventilation: The effect of body position. Annals of Internal Medicine. 1992;116(7):540–543. doi: 10.7326/0003-4819-116-7-540. [DOI] [PubMed] [Google Scholar]
- van der Padt A, van Schalk RH, Sonneveld P. Acute dystonic reaction to metoclopramide in patients carrying homozygous cytochrome P450 2D6 genetic polymorphisms. The Netherlands Journal of Medicine. 2006;64(5):160–162. [PubMed] [Google Scholar]
- Welch SK. Certification of staff nurses to insert enteral feeding tubes using a research-based procedure. Nutrition in Clinical Practice. 1996;11(1):21–27. doi: 10.1177/011542659601100121. [DOI] [PubMed] [Google Scholar]