Abstract
Background
Low social support has been associated with several disorders. We test the relationship between perceived interpersonal social support (ISS) and aspects of mental and physical health.
Methods
We used data from National Epidemiological Survey on Alcohol and Related Conditions in which 34 653 individuals aged 20–99 years were interviewed twice (2001–02 and 2004–05), with the second interview including the interpersonal support evaluation list. The association of perceived ISS with lifetime DSM-IV psychopathology and physical health from the past 12 months was investigated. We also tested whether this association changes as a function of number of traumatic events in accordance with the buffering hypothesis.
Results
Low perceived ISS correlated with increased prevalence of major depressive disorder, generalized anxiety, social phobia and several physical health problems. There was a strong association between excellent self-perceived physical health and high social support.
Conclusions
There was evidence for both the main, beneficial effects of high perceived ISS and buffering, whereby increased perceived ISS ameliorated the pathogenic influence of exposure to traumatic life events on psychopathology. Current findings highlight the importance of perceived ISS in individuals' general mental and physical well-being, both in daily life and upon exposure to negative life events.
Keywords: epidemiology
Introduction
Social support refers to resources, material and emotional, available to a person via interpersonal contacts. It has historically been defined using both community-centric and person-centric instruments. For the former, the term ‘social capital’ referring to civic architecture, neighborhood characteristics and societal ties has been widely popular.1,2 Here, we focus on the latter construct of person-centric social support which relates to an individual's experience of obtaining support from their friends and family. Specifically, this study focuses on perceived interpersonal social support (ISS),3–5 which refers to an individual's report of interpersonal support available to them, is considered by some to be a more sensitive measure of the ability to cope with mental and physical health challenges.
Several studies have investigated the association between perceived ISS and health outcomes. Importantly, individuals with higher perceived ISS are less likely to be depressed6–9 and have fewer physical symptoms and reduced risk for cardiovascular illness.10–18 According to the buffering hypothesis,3,4 increased perceived ISS, particularly in those experiencing high levels of stress, acts as a protective influence against physical and mental health problems.
There are several mechanisms that potentially link perceived ISS and health. First, high perceived ISS may lead to lower likelihood of mental health problems via enhanced social adjustment and reduction of stress. This may directly and indirectly influence physical health outcomes as well. Second, poor health, whether mental or physical, may lead to a reduction in affiliations with givers of social support further exacerbating the decline in health. Third, common factors, such as personality traits or socio-economic status, may jointly influence both perceived ISS and the likelihood of mental and physical illness.19–22
Another level of complexity in the relationship between perceived ISS and health is the intricate cross-talk between the domains of mental and physical health (e.g. depression itself is associated with poorer cardiovascular outcomes and vice versa). Thus, there is a need to comprehensively and jointly examine the association between perceived ISS and multiple measures of physical and mental health outcomes. Using a large data set (n = 34 653) of adults aged 20–99 years and representative of the US population, we examined the association between perceived ISS, as measured by the Interpersonal Support Evaluation List (ISEL),3,5 and 18 and 16 measures of mental and physical health, respectively. The goals of the present study were to investigate:
the factor structure underlying 12 items assessing perceived ISS;
the association between lifetime DSM-IV psychopathology and perceived ISS;
the association between physical health outcomes from the past 12 months and perceived ISS;
to test whether the association between perceived ISS and mental and physical health outcomes changes with varying exposure to traumatic events.
Materials and methods
Sample
Data on 34 653 individuals (aged 21–99 years) for this study were taken from the second wave of interviews conducted by the US Census Bureau under the supervision of the National Institutes of Alcohol Abuse and Alcoholism for the National Epidemiological Survey on Alcohol and Related Conditions (NESARC).23 Interviews were conducted during 2004–05,24 with data available on all participants from the Wave 1 interview conducted in 2001–02. Efforts to conduct face-to-face re-interviews with all 43 093 respondents from who had completed the Wave 1 interview were made, yielding a response rate of 86.7%25 or an effective sample size of 34 653, with exclusions due to death, deportation and mental or physical impairment. The cumulative response rate at Wave 2 was the product of this Wave 2 response rate and the response rate from Wave 1 (81.0%), or 70.2% and compare favorably with many cross-sectional studies. Non-response to items on age, sex, region, ethnicity and a history of psychiatric or substance use disorders were adjusted for, in addition to the complexity of the survey design using weights at the household and person levels. The final Wave 2 data are representative of the civilian population of the USA on a variety of socio-economic variables including region, age, race-ethnicity and sex, based on the 2000 Decennial Census. In addition to the diagnostic measures that comprised the Wave 1 interview, several additional scales and measures were incorporated into Wave 2, including (but not limited to) multiple items assessing perceived ISS. These measures have been demonstrated to have good reliability and internal consistency.25 Further details regarding study design and generalizability may be found elsewhere.25,26
Measures
The NESARC utilized the Alcohol Use Disorders and Associated Disabilities Interview (AUDADIS). The reliability and consistency of measures assessed using the AUDADIS are good.25,26
Perceived interpersonal social support
Twelve items assessing perceived ISS were assessed. Items were drawn from a larger pool of questions that comprise the ISEL for General Populations.3–5 Responses to each item were rated, by the respondent, on a 1–4 scale ranging from 1, definitely true, to 4, definitely false. All items (Table 1) were coded to represent decreasing perceived ISS—for example, for the item ‘If I wanted to go on a trip for a day (e.g., to the mountains, beach, or country), I would have a hard time finding someone to go with me’, 1, definitely false (i.e. high perceived ISS), and 4, definitely true (i.e. low perceived ISS). The ISEL includes items that are phrased in both directions (i.e. increasing and decreasing perceived ISS)—we reverse coded these items to represent decreasing perceived ISS. A composite measure of perceived ISS was constructed by summing across all 12 items—quartiles on this distribution were used for further analyses.
Table 1.
Association between a composite measure of perceived ISS and aspects of mental and physical health in 34 653 individuals from the NESARC
| High social support (n = 9612) | Intermediate high social support (n = 8155) | Intermediate low social support (n = 8500) | Low social support (n = 7720) | χ2a | |
|---|---|---|---|---|---|
| Mental health | |||||
| Major depressive disorder | 17.90 | 21.61 | 23.53 | 30.41 | 390.31*** |
| Generalized anxiety disorder | 4.88 | 6.88 | 8.15 | 12.46 | 353.72*** |
| Panic disorder (with or without agoraphobia) | 6.08 | 7.12 | 7.69 | 10.83 | 143.36*** |
| Social phobia | 3.71 | 5.84 | 7.55 | 12.14 | 486.64*** |
| Specific phobias | 13.72 | 15.89 | 16.27 | 18.38 | 70.32*** |
| Manic disorder | 3.64 | 4.34 | 5.30 | 8.67 | 238.79*** |
| Schizophrenia or other psychotic illness | 0.22 | 0.42 | 0.54 | 1.73 | 163.95*** |
| Attempted suicide | 2.37 | 2.91 | 3.25 | 6.63 | 253.46*** |
| Conduct disorder | 3.19 | 3.26 | 3.33 | 4.70 | 36.21*** |
| Alcohol abuse/dependence | 31.39 | 34.22 | 33.46 | 32.47 | 18.24*** |
| Nicotine dependence | 19.57 | 21.58 | 22.92 | 24.37 | 63.29*** |
| Cannabis abuse dependence | 8.29 | 9.50 | 9.17 | 9.26 | 9.32* |
| Sedative abuse/dependence | 1.02 | 1.16 | 1.25 | 1.52 | 9.02* |
| Tranquilizer abuse/dependence | 0.84 | 1.07 | 1.23 | 1.58 | 21.33*** |
| Opioid abuse/dependence | 1.50 | 1.73 | 1.65 | 2.50 | 27.40*** |
| Amphetamine abuse/dependence | 1.70 | 2.13 | 2.09 | 2.27 | 8.19* |
| Hallucinogen abuse/dependence | 1.36 | 1.73 | 1.59 | 1.90 | 8.49* |
| Cocaine abuse dependence | 2.76 | 3.36 | 3.00 | 3.46 | 9.08* |
| Physical health | |||||
| Good self-perceived current health | 65.31 | 61.79 | 52.91 | 40.17 | 1263.01*** |
| Hardening of arteries | 1.49 | 1.58 | 2.15 | 3.35 | 86.06*** |
| Hypertension | 22.82 | 25.38 | 28.03 | 31.54 | 180.72*** |
| Diabetes | 7.46 | 8.06 | 10.01 | 11.55 | 105.24*** |
| Cirrhosis of the liver | 0.12 | 0.20 | 0.32 | 0.39 | 14.57** |
| Other liver disease | 0.55 | 0.59 | 0.81 | 1.02 | 15.81** |
| Chest pain/angina pectoris | 3.07 | 3.79 | 4.23 | 6.34 | 118.57*** |
| Rapid heart beat/tachycardia | 4.06 | 4.29 | 5.21 | 7.03 | 91.90*** |
| Myocardial infarction | 0.56 | 0.73 | 1.08 | 1.46 | 42.90*** |
| High cholesterol | 18.39 | 19.71 | 21.90 | 24.25 | 99.99*** |
| Other heart disease | 2.06 | 2.50 | 2.81 | 4.21 | 76.57*** |
| Stomach ulcer | 1.88 | 2.18 | 2.65 | 3.97 | 82.21*** |
| HIV/AIDS/other STDs | 0.56 | 0.79 | 0.98 | 1.29 | 27.43*** |
| Gastritis | 4.30 | 4.60 | 5.52 | 6.76 | 61.13*** |
| Arthritis | 18.99 | 20.58 | 23.50 | 27.91 | 218.36*** |
| Stroke | 0.58 | 0.37 | 1.03 | 1.29 | 53.11*** |
Estimates reported are prevalences (%).
aThree degree of freedom test.
*P < 0.05.
**P < 0.01.
***P < 0.001.
Mental health
A majority of the mental health correlates were DSM-IV27 diagnoses—these included lifetime (both at Wave 1 and at Wave 2) histories of major depressive disorder, generalized anxiety disorder, social phobia, specific phobias, panic disorder (with/without agoraphobia), manic disorder, conduct disorder, alcohol abuse/dependence, nicotine dependence, as well as abuse/dependence of cannabis, cocaine, sedatives, amphetamines and opioids. Two additional items assessing a lifetime history of attempted suicide and a self-report of whether the participant had ever been diagnosed with schizophrenia or another psychotic illness by a health professional were also included.
Physical health
The NESARC queried participants about experiencing certain health problems in the past year (lifetime assessments not available) at their Wave 2 interview. For each health problem, participants were asked whether (a) they had experienced the problem and (b) the diagnosis had been confirmed by a doctor/health professional. For the present analyses, we only coded participants as having experienced a health problem if it had been confirmed by a physician—these problems included hardening of arteries, hypertension, diabetes, liver disease, chest pain/angina, tachycardia, myocardial infarction, other heart disease, high cholesterol, stomach ulcers, gastritis, arthritis, stroke and HIV/AIDS/other sexually transmitted diseases (STDs). Participants were also asked to rate their current health as excellent, very good, good, fair or poor—a measure representing excellent to very good self-perceived current health was also included.
Traumatic events
During an assessment of post-traumatic stress disorder, a series of questions regarding lifetime exposure to traumatic events were asked. These included four items on military/combat exposure and refugee status, which we excluded (to avoid any potential confounds with period/cohort effects) as well as 23 general items assessing traumatic events (based on the WMH-CIDI-A inventory). A variable was created by summing across the 23 events and classifying individuals based on whether they had experienced 0, 1, 2–3 or 4 or more traumatic events.
Socio-demographic control measures
Sex (males coded as ‘1’), age (three dummies representing those aged 21–31, 32–43 and 44–59 years), self-reported Caucasian ethnicity and living below the poverty line (based on US Census Bureau thresholds for 2005) were included as controls.
Statistical analysis
In order to examine the factorial structure underlying the 12 perceived ISS items, a factor analysis was conducted in SAS, using a maximum likelihood estimator. Eigenvalues and visual inspection of the scree plot were used to determine the factor structure.
All other statistical analyses were conducted in STATA28 adjusting for the complex survey design underlying NESARC. The svy (survey)29 suite of options was used and the STATA module idonepsu was used to account for strata with singleton primary sampling units (PSUs). Logistic regression was used to examine the uni- and multivariate relationship between perceived ISS and mental and physical health. The mental/physical health measure was the outcome and three dummy measures representing intermediate high, intermediate low and low perceived ISS (high perceived ISS was the reference group) were the predictor. All analyses were adjusted for socio-demographic control measures—in the first series of analyses, association between individual mental/physical health outcomes and perceived ISS was examined while adjusting only for the socio-demographic correlates. In the second series of analyses, for each mental health outcome, in addition to perceived ISS and socio-demographic controls, all other measures of mental health were included as covariates to adjust for inter-variable correlations. A similar set of analyses were conducted for the physical health outcomes by adjusting for other physical health measures.
Results
Factor analysis of perceived ISS
Factor analyses revealed that all 12 perceived ISS items loaded well on a single factor, with loadings ranging from 0.44 to 0.66 (see Supplementary material, Table S1)—hence, we used a composite measure representing perceived ISS, which was created by summation across all 12 items. The top quartile on this score represented high perceived ISS and the bottom quartile represented low perceived ISS.
Perceived ISS and demographics
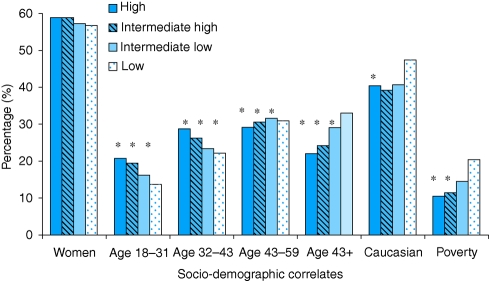
As shown in Fig. 1, women were significantly (P < 0.05) more likely to report high perceived ISS. Across all age groups, compared with older individuals, younger individuals reported greater levels of perceived ISS. Those endorsing Caucasian ethnicity and also those living below the poverty line were more likely to report statistically (P < 0.05) lower perceived ISS.
Fig. 1.
Socio-demographic characteristics of 34 653 individuals from the NESARC, categorized by levels of perceived ISS. *This prevalence is statistically different (P< 0.05) from that reported for those with low perceived ISS.
Perceived ISS and mental health
The association between mental health and perceived ISS is presented in Tables 1 and 2. Unadjusted χ2 tests revealed significant associations between mental health and changing level of perceived ISS (Table 1). For instance, when compared with those with high perceived ISS (i.e. top quartile), those with low perceived ISS (i.e. bottom quartile) were considerably more likely to report a lifetime history of major depressive disorder (17.9% versus 30.4%), generalized anxiety disorder (4.9% versus 12.46%) and social phobia (3.7% versus 12.14%). Such a linear increase in the likelihood of self-reported psychopathology with decreasing perceived ISS was seen for all measures. This was also reflected by the odds ratios (Table 2) which were adjusted for sex, age, ethnicity and poverty—for instance, when compared with those with low perceived ISS, those with intermediate low, intermediate high and high perceived ISS were 1.32, 1.57 and 2.32 times, respectively, more likely to meet criteria for a lifetime history of major depressive disorder and each of these odds ratios were statistically different from each other, clearly demonstrating increasing risk of mental health problems with decreasing perceived ISS. Similar trends were seen across multiple measures of psychopathology as well as for self-reported diagnosis of psychotic illness and attempted suicide—for the latter, compared with those with high perceived ISS, those with low perceived ISS were 3.28 times more likely to report attempting suicide.
Table 2.
Odds ratios (ORs) and 95% confidence intervals (95% CIs) depicting the association between levels of social support and mental and physical health using the top quartile (highest social support) as a reference group
|
Intermediate high social support (n = 8155) |
Intermediate low social support (n = 8500) |
Low social support (n = 7720) |
||||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Mental health | ||||||
| Major depressive disorder | 1.32*** | 1.21, 1.43 | 1.57*** | 1.44, 1.70 | 2.32*** | 2.11, 2.54 |
| Generalized anxiety disorder | 1.44*** | 1.24, 1.68 | 1.94*** | 1.66, 2.26 | 3.13*** | 2.71, 3.62 |
| Panic disorder (with or without agoraphobia) | 1.22a,** | 1.06, 1.41 | 1.39a,*** | 1.20, 1.62 | 2.16*** | 1.86, 2.50 |
| Social phobia | 1.72*** | 1.46, 2.04 | 2.36*** | 2.02, 2.75 | 4.24*** | 3.61, 4.98 |
| Specific phobias | 1.21***a | 1.09, 1.34 | 1.30***a | 1.16, 1.45 | 1.58*** | 1.42, 1.75 |
| Manic disorder | 1.28* | 1.06, 1.54 | 1.69*** | 1.43, 2.02 | 3.09*** | 2.60, 3.66 |
| Schizophrenia or other psychotic illness | 2.03 | 0.97, 4.27 | 2.81*** | 1.52, 5.20 | 10.09*** | 5.66, 17.99 |
| Attempted suicide | 1.29a,* | 1.02, 1.62 | 1.59a,*** | 1.27, 1.98 | 3.28*** | 2.70, 4.00 |
| Conduct disorder | 1.05 | 0.85, 1.28 | 1.09 | 0.89, 1.34 | 1.79*** | 1.45, 2.22 |
| Alcohol abuse/dependence | 1.18a,*** | 1.09, 1.28 | 1.16a,** | 1.07, 1.27 | 1.24a,*** | 1.13, 1.36 |
| Nicotine dependence | 1.20a,*** | 1.10, 1.31 | 1.31a,*** | 1.20, 1.43 | 1.50*** | 1.37, 1.65 |
| Cannabis abuse dependence | 1.17a,* | 1.02, 1.34 | 1.27a,*** | 1.11, 1.45 | 1.47*** | 1.28, 1.68 |
| Sedative abuse/dependence | 1.24 | 0.88, 1.76 | 1.40 | 0.97, 2.02 | 1.81*** | 1.33, 2.46 |
| Tranquilizer abuse/dependence | 1.34 | 0.97, 1.85 | 1.74a,*** | 1.24, 2.44 | 2.32a,*** | 1.66,3.25 |
| Opioid abuse/dependence | 1.19 | 0.89, 1.59 | 1.29 | 0.97, 1.70 | 1.98*** | 1.52, 2.57 |
| Amphetamine abuse/dependence | 1.27 | 0.98, 1.64 | 1.45a,** | 1.11, 1.91 | 1.47a,** | 1.12, 1.92 |
| Hallucinogen abuse/dependence | 1.49a,b,** | 1.13, 1.96 | 1.36a,* | 1.03, 1.81 | 1.88b,*** | 1.44, 2.47 |
| Cocaine abuse dependence | 1.32a,b,** | 1.08, 1.62 | 1.22a,* | 1.00, 1.49 | 1.52b,*** | 1.24, 1.85 |
| Physical health | ||||||
| Good self-perceived current health | 0.90** | 0.83, 0.97 | 0.65*** | 0.60, 0.70 | 0.43*** | 0.39, 0.47 |
| Hardening of arteries | 1.00 | 0.75, 1.33 | 1.22 | 0.92, 1.60 | 1.63*** | 1.24, 2.16 |
| Hypertension | 1.09 | 0.99, 1.19 | 1.15**a | 1.04, 1.26 | 1.18a,*** | 1.08, 1.30 |
| Diabetes | 1.03 | 0.89, 1.19 | 1.17a,* | 1.00, 1.36 | 1.22a,** | 1.05, 1.42 |
| Cirrhosis of the liver | 1.90 | 0.75, 4.82 | 2.10* | 1.00, 4.40 | 2.30 | 0.92, 5.76 |
| Other liver disease | 0.92 | 0.56, 1.50 | 1.04 | 0.68, 1.59 | 1.49 | 0.97, 2.29 |
| Chest pain/angina pectoris | 1.14 | 0.91, 1.43 | 1.16 | 0.96, 1.41 | 1.63*** | 1.33, 1.99 |
| Rapid heart beat/tachycardia | 0.94 | 0.78, 1.13 | 1.10 | 0.91, 1.32 | 1.37*** | 1.15, 1.64 |
| Myocardial infarction | 1.12 | 0.72, 1.74 | 1.70a,** | 1.14, 2.54 | 2.07a,*** | 1.38, 3.12 |
| High cholesterol | 1.01 | 0.91, 1.11 | 1.08 | 0.97, 1.20 | 1.15** | 1.04, 1.28 |
| Other heart disease | 1.19 | 0.95, 1.49 | 1.20 | 0.96, 1.51 | 1.64*** | 1.31, 2.05 |
| Stomach Ulcer | 1.07 | 0.84, 1.36 | 1.48** | 1.16, 1.88 | 2.18*** | 1.71, 2.79 |
| HIV/AIDS/other STDs | 1.36 | 0.90, 2.04 | 1.63a,* | 1.03, 2.56 | 2.34a,*** | 1.59, 3.50 |
| Gastritis | 1.04 | 0.86, 1.26 | 1.18 | 0.98, 1.41 | 1.34** | 1.12, 1.60 |
| Arthritis | 1.07 | 0.97, 1.19 | 1.09 | 0.98, 1.21 | 1.30*** | 1.18, 1.43 |
| Stroke | 0.85 | 0.50, 1.43 | 1.85a,** | 1.21, 2.82 | 2.07a,*** | 1.38, 3.09 |
Analyses control for gender, age, ethnicity and living below the poverty line according to the US Census.
a,b,cOdds ratios with the same alphabetical superscript are statistically equal to each other.
*P < 0.05.
**P < 0.01.
***P < 0.001.
Perceived ISS and physical health
Those reporting low perceived ISS were also less likely to report poorer self-perceived current health (40.17% compared with 65.3% in those with high perceived ISS; Table 1). These individuals were also considerably more likely to report that a health-care professional had diagnosed them (in the past year) with a host of other physical health problems—for instance, compared with those who reported high perceived ISS, those with low perceived ISS reported higher rates of arthritis (19% vs. 27.9%), hypertension (22.8% versus 31.5%) and chest pain/angina pectoris (3.1% versus 6.3%) (Table 1). However, the increased likelihood of poorer physical health as a function of decreasing perceived ISS was only statistically significant in those with the lowest perceived ISS (Table 2). Even though statistical differences were restricted to those with low perceived ISS (and only when they were compared with those with high perceived ISS), in a number of instances, there was greater than a two-fold increase in likelihood of physical health outcomes—for instance, those with low perceived ISS were twice as likely to report being diagnosed in the past year with myocardial infarctions, stomach ulcers, HIV/AIDS/other STDs and stroke.
Multivariate analyses
We conducted three series of multivariate analyses. The first jointly modeled the effects of all mental health correlates—only major depressive disorder, generalized anxiety disorder, social phobia and DSM-IV nicotine dependence were significantly associated with perceived ISS when other mental health covariates were adjusted for (Table 3). In the second, all physical health correlates were modeled together—when self-perceived current health was included in this model, no other physical problems were significant (although stomach ulcers and HIV/AIDS/STDs were significant in the low perceived ISS group only; Table 3). In a final series of models, we examined whether the association between physical health, as measured by self-perceived current health, and perceived ISS was mediated by mental health correlates (major depression, generalized anxiety disorder, social phobia and nicotine dependent) and vice versa. Odds ratios remained largely unchanged, suggesting that the relationship between mental and physical health correlates and perceived ISS were not mediated by each other.
Table 3.
Multivariate OR and 95% CI depicting the association between levels of social support and mental and physical health using the top quartile (highest social support) as a reference group
|
Intermediate high social support (n = 8155) |
Intermediate low social support (n = 8500) |
Low social support (n = 7720) |
||||
|---|---|---|---|---|---|---|
| OR | 95% CI | OR | 95% CI | OR | 95% CI | |
| Mental health | ||||||
| Major depressive disorder | 1.19a,*** | 1.09, 1.39 | 1.30a,*** | 1.19, 1.42 | 1.55*** | 1.41, 1.71 |
| Generalized anxiety disorder | 1.19a,* | 1.02, 1.39 | 1.42a,b,*** | 1.20, 1.67 | 1.65b,*** | 1.43, 1.91 |
| Panic disorder (with or without agoraphobia) | 1.02 | 0.87, 1.20 | 1.01 | 0.86, 1.18 | 1.12 | 0.96, 1.31 |
| Social phobia | 1.55*** | 1.31, 1.84 | 1.93*** | 1.64, 2.26 | 2.83*** | 2.43, 3.30 |
| Specific phobias | 1.07 | 0.97, 1.19 | 1.05 | 0.94, 1.17 | 1.01 | 0.90, 1.13 |
| Manic disorder | 1.06 | 0.87, 1.31 | 1.20 | 0.99, 1.44 | 1.55*** | 1.30, 1.86 |
| Schizophrenia or other psychotic illness | 1.12 | 0.56, 2.22 | 1.29 | 0.72, 2.31 | 2.89*** | 1.64, 5.07 |
| Attempted suicide | 1.06 | 0.84, 1.34 | 1.14 | 0.90, 1.45 | 1.69*** | 1.37, 2.08 |
| Conduct disorder | 0.95 | 0.76, 1.18 | 0.85 | 0.68, 1.05 | 1.13 | 0.91, 1.41 |
| Alcohol abuse/dependence | 1.10* | 1.01, 1.20 | 1.03 | 0.93, 1.13 | 0.97 | 0.88, 1.06 |
| Nicotine dependence | 1.12a,** | 1.02, 1.22 | 1.19a,*** | 1.09, 1.30 | 1.20a,*** | 1.10, 1.32 |
| Cannabis abuse dependence | 1.00 | 0.84, 1.19 | 1.06 | 0.89, 1.25 | 0.99 | 0.84, 1.17 |
| Sedative abuse/dependence | 0.93 | 0.59, 1.47 | 0.92 | 0.54, 1.58 | 1.05 | 0.66, 1.68 |
| Tranquilizer abuse/dependence | 1.18 | 0.75, 1.84 | 1.70a,* | 1.08, 2.68 | 1.79a,* | 1.05, 3.04 |
| Opioid abuse/dependence | 0.98 | 0.67, 1.42 | 0.91 | 0.63, 1.31 | 1.34 | 0.95, 1.88 |
| Amphetamine abuse/dependence | 0.98 | 0.70, 1.39 | 1.18 | 0.84, 1.65 | 0.90 | 0.61, 1.33 |
| Hallucinogen abuse/dependence | 1.40a,* | 1.00, 1.95 | 1.05 | 0.75, 1.48 | 1.42a,* | 1.03, 1.96 |
| Cocaine abuse dependence | 1.17 | 0.90, 1.53 | 0.95 | 0.73, 1.22 | 1.05 | 0.81, 1.37 |
| Physical health | ||||||
| Good self-perceived current health | 0.93 | 0.86, 1.01 | 0.67*** | 0.61, 0.73 | 0.46*** | 0.42, 0.50 |
| Hardening of arteries | 0.96 | 0.72, 1.27 | 1.10 | 0.84, 1.43 | 1.31 | 0.99, 1;73 |
| Hypertension | 1.07 | 0.97, 1.18 | 1.02 | 0.93, 1.13 | 0.95 | 0.86, 1.05 |
| Diabetes | 0.95 | 0.82, 1.10 | 0.98 | 0.84, 1.14 | 0.97 | 0.84, 1.12 |
| Cirrhosis of the liver | 1.90 | 0.72, 5.04 | 1.68 | 0.74, 3.78 | 1.25 | 0.51, 3.11 |
| Other liver disease | 0.85 | 0.52, 1.40 | 0.85 | 0.54, 1.33 | 0.96 | 0.62, 1.51 |
| Chest pain/angina pectoris | 1.08 | 0.85, 1.37 | 0.93 | 0.75, 1.14 | 1.13 | 0.89, 1.43 |
| Rapid heart beat/tachycardia | 0.90 | 0.74, 1.10 | 0.95 | 0.78, 1.16 | 0.97 | 0.79, 1.19 |
| Myocardial infarction | 0.93 | 0.56, 1.55 | 1.49 | 0.97, 2.31 | 1.43 | 0.91, 2.24 |
| High cholesterol | 0.98 | 0.89, 1.08 | 1.00 | 0.90, 1.12 | 1.01 | 0.92, 1.12 |
| Other heart disease | 1.10 | 0.87, 1.40 | 1.02 | 0.81, 1.29 | 1.23 | 0.98, 1.55 |
| Stomach ulcer | 0.99 | 0.78, 1.28 | 1.20 | 0.93, 1.56 | 1.55** | 1.18, 2.01 |
| HIV/AIDS/other STDs | 1.30 | 0.87, 1.94 | 1.47 | 0.95, 2.27 | 1.80* | 1.20, 2.72 |
| Gastritis | 0.99 | 0.82, 1.21 | 1.02 | 0.85, 1.23 | 0.98 | 0.81, 1.18 |
| Arthritis | 1.05 | 0.94, 1.17 | 0.97 | 0.87, 1.08 | 1.05 | 0.95, 1.16 |
| Stroke | 0.68 | 0.41, 1.13 | 1.23 | 0.82, 1.85 | 1.27 | 0.89, 1.82 |
Each mental and physical health outcome is adjusted for other mental and physical health measures, respectively. Analyses control for gender, age, ethnicity and living below the poverty line according to the US Census.
a,b,cOdds ratios with the same alphabetical superscript are statistically equal to each other.
*P < 0.05.
**P < 0.01.
***P < 0.001.
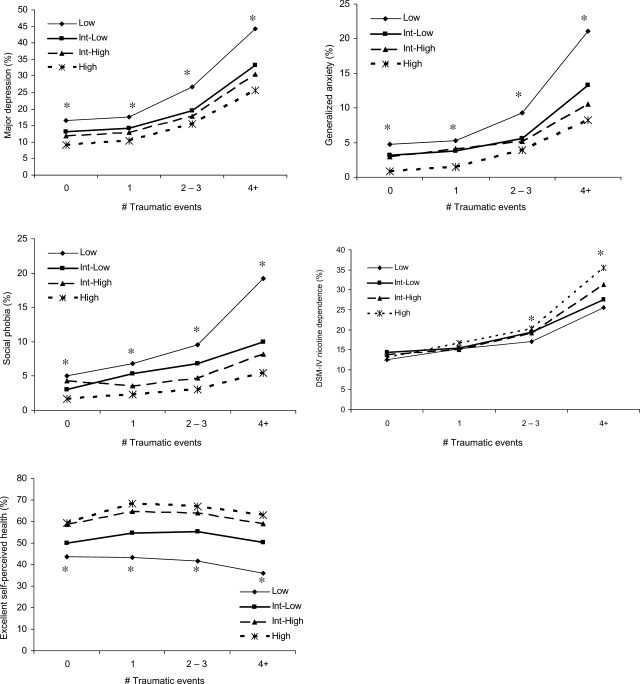
Traumatic events, perceived ISS and health outcomes
Decreasing perceived ISS and increasing exposure to traumatic events were modestly correlated with each other (r = −0.12). Figure 2 represents the joint effects of trauma exposure and perceived ISS on likelihood of experiencing major depressive disorder, generalized anxiety disorder, social phobia, alcohol abuse/dependence and self-perceived current health. In general, increasing exposure to traumatic events was associated with increased likelihood of disorder (i.e. main effect of trauma experience on likelihood of disorder). As shown by the asterisks in Fig. 2, for all mental and physical health outcomes, for each level of trauma experience (0, 1, 2–3, 4+ experiences) those at the lowest level of perceived ISS reported statistically (P < 0.05) higher rates of mental health problems (and lower perceived good health) than those experiencing the same number of traumatic events but reporting intermediate high and high perceived ISS. Consistent with the buffering hypothesis, those reporting the lowest level of perceived ISS were most likely to also report higher rates of major depressive disorder, generalized anxiety disorder, social phobia and poor self-perceived current health with increasing exposure to traumatic events. This interaction was significant in differentiating between those at the lowest level of perceived support and experiencing two or more traumatic events from others in the study. In our data, high perceived ISS did not appear to buffer the pathogenic effects of traumatic events on alcohol abuse/dependence.
Fig. 2.
Perceived social support and exposure to traumatic events have main and interactive effects on physical and mental health outcomes in 34 653 individuals from the NESARC. *Significance at P < 0.05 between low perceived ISS and other levels for given number of traumatic events.
Discussion
Main findings of this study
We sought to examine the association between perceived ISS and a series of physical and mental health outcomes in the National Epidemiological Survey on Alcohol and Related Conditions (Wave II). Increased perceived ISS was associated with decreased likelihood of major depressive disorder, generalized anxiety disorder, social phobia and alcohol abuse/dependence. Those reporting high perceived ISS also were more likely to report better perceived health.
What is known
Perceived ISS and health outcomes
While there is some heterogeneity within the literature for physical health, multiple studies show a strong link between depression and low perceived ISS. For instance, Cohen and Hoberman4 previously reported that the domains of the ISEL were strongly related to depressive symptoms but not of physical symptoms. These associations between the ISEL domains and psychological well-being, particularly depressive and anxiety disorders, have also been noted in population-based studies.7,30 George et al.6 also report lower rates of recovery from depression in those with impaired subjective perceived ISS particularly for middle-aged males. Stice et al.8 reported that deficits in parental (but not peer support) were associated with onset of major depression in young girls, with a reciprocal influence of depression on temporal changes in perceived ISS. With physical health outcomes, low perceived ISS has been associated with cardiovascular health, including myocardial infarctions and stroke;10–15,31,32 however, it is posited that the effects of low perceived ISS on physical health are largely mediated by intervening episodes of depression.
Can poor health modify perceived ISS?
Pathways between poor mental and physical health and perceived ISS may be reciprocal. Stice et al.8 demonstrated that while low parental support increased likelihood of major depression in girls, depression was significantly associated with subsequent erosion of peer support. Research into recovery from HIV/AIDS, for instance, has shown that low perceived ISS may be a consequence of stigma associated with diagnosis (particularly in vulnerable populations) and that low perceived ISS, in turn, can hinder medication adherence and led to poor prognosis.16–18,33
The buffering hypothesis
Cohen and Willis3 suggest that social support may act upon health in multiple ways—perceived ISS may be particularly relevant in situations of high stress when interpersonal ties are required to ‘buffer’ the pathogenic effects of stress. Their alternate hypothesis implies that low social support may be toxic regardless of stress exposure, and that this latter form of support relates to an individual's feeling of integration in their support system. It is likely that the process underlying the relationship between stress due to exposure to trauma, perceived social support and health is related via multiple feedback loops (e.g. increased social support might reduce likelihood of exposure to stress, or increased stress may induce a reduction in perceived social support).
What this study adds
Perceived ISS and health outcomes
Our findings are largely in keeping with a number of epidemiological and clinical investigations that have revealed a potent relationship between low perceived ISS and poorer mental and physical health outcomes. The strength of this particular study lies in its ability to jointly examine several mental and physical health outcomes in a large population-representative data set, and demonstrate the association between perceived ISS and both mental and physical well-being.
Can poor health modify perceived ISS?
Cause and effect cannot be disentangled in our study which is cross-sectional with respect to the assessments of perceived ISS. While it is likely that individuals with reduced perceived ISS are at increased likelihood of developing and sustaining poor physical and mental health outcomes, it is also plausible that negative physical and mental health outcomes lead to decreased levels of perceived ISS. The study of these complex feedback loops warrants detailed study; however, longitudinal data, across the lifespan will be necessary.
The buffering hypothesis
In our study, low perceived ISS and exposure to traumatic events were independently and interactively associated with poor mental and physical health outcomes. Therefore, we do find support for the buffering hypothesis whereby, even in individuals experiencing multiple negative life events, high perceived ISS was correlated with a reduction in rates of depression, anxiety and poor health when compared with individuals at low levels of perceived ISS, even when they experienced fewer traumatic events. However, high perceived ISS was beneficial, irrespective of stress exposure, also validating the alternate model posited by Cohen and Willis.
Public health relevance
Empirical evidence suggests that increased social support is associated with decreased likelihood of onset of illness and increased rates of recovery from illness.34–36 Increasing social support in the lives of patients recovering from myocardial infarction or stroke has helped ameliorate the effects of psychological problems, such as depression, on recovery.10,31 Likewise, enhanced social support is often a vital component of recovery from a variety of mental health problems. The current work highlights the two-fold benefit of increased social support (directly and as a buffer from trauma).
Limitations
Some limitations of this study are noteworthy:
Information of physical health outcomes was restricted to the past 12 months whereas measures of perceived ISS and of mental health were assessed for the lifetime. However, as the goal of this study is to examine associations (and not to ascribe causation), this is less of a concern.
Perceived ISS was not assessed at the first wave 1 and hence, we could not model causal pathways or mechanisms via which change in perceived ISS was correlated with moderation of physical and mental health outcomes. Likewise, it may be argued that our test of the buffering hypothesis is limited by our lack of knowledge of the temporal spacing of the negative life events with respect to perceived ISS.
A reduced list of ISEL items was used and hence data on some aspects of perceived ISS are unavailable.
Although our study does not examine causation, it aimed to explore correlations between perceived ISS was associated with lower rates of self-reported mental and physical health problems and also whether, globally, perceived ISS reduced the extent to which negative life events were associated with mental and physical health problems. Therefore, despite limitations associated with drawing causal inference, we underscore the beneficial role that perceived ISS plays in the well-being of an individual and demonstrate its important connections with life events and their links to well-being.
Supplementary data
Supplementary data are available at the Journal of Public Health online.
Funding
This work was supported by the National Institute on Drug Abuse [DA23668 and DA25886 to A.A.].
Supplementary Material
References
- 1.Putnam R. Bowling Alone: The Collapse and Revival of the American Community. New York: Simon & Schuster; 2000. [Google Scholar]
- 2.Hanifan LJ. The rural school community center. Ann Am Acad Polit Soc Sci. 1916;67:130–8. [Google Scholar]
- 3.Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull. 1985;98(2):310–57. [PubMed] [Google Scholar]
- 4.Cohen S, Hoberman HM. Positive events and social supports as buffers of life change stress. J Appl Soc Psychol. 1983;13(2):99–125. [Google Scholar]
- 5.Cohen S, Mermelstein R, Kamarck TW, et al. Measuring the functional components of social support. In: Sarason IG, Sarason BR, editors. Social Support: Theory, Research and Applications. 1985. pp. 73–94. [Google Scholar]
- 6.George LK, Blazer DG, Hughes DC, et al. Social support and the outcome of major depression. Br J Psychiatry. 1989;154:478–85. doi: 10.1192/bjp.154.4.478. [DOI] [PubMed] [Google Scholar]
- 7.Paykel ES. Life events, social support and depression. Acta Psychiatr Scand Suppl. 1994;377:50–8. doi: 10.1111/j.1600-0447.1994.tb05803.x. [DOI] [PubMed] [Google Scholar]
- 8.Stice E, Ragan J, Randall P. Prospective relations between social support and depression: differential direction of effects for parent and peer support? J Abnorm Psychol. 2004;113(1):155–9. doi: 10.1037/0021-843X.113.1.155. [DOI] [PubMed] [Google Scholar]
- 9.Stansfeld SA, Rael EG, Head J, et al. Social support and psychiatric sickness absence: a prospective study of British civil servants. Psychol Med. 1997;27(1):35–48. doi: 10.1017/s0033291796004254. [DOI] [PubMed] [Google Scholar]
- 10.Carod-Artal FJ, Egido JA. Quality of life after stroke: the importance of a good recovery. Cerebrovasc Dis. 2009;27(Suppl 1):204–14. doi: 10.1159/000200461. [DOI] [PubMed] [Google Scholar]
- 11.Glass TA, Maddox GL. The quality and quantity of social support: stroke recovery as psycho-social transition. Soc Sci Med. 1992;34(11):1249–61. doi: 10.1016/0277-9536(92)90317-j. [DOI] [PubMed] [Google Scholar]
- 12.Western H. Altered living: coping, hope and quality of life after stroke. Br J Nurs. 2007;16(20):1266–70. doi: 10.12968/bjon.2007.16.20.27573. [DOI] [PubMed] [Google Scholar]
- 13.Berkman LF, Leo-Summers L, Horwitz RI. Emotional support and survival after myocardial infarction. A prospective, population-based study of the elderly. Ann Intern Med. 1992;117(12):1003–9. doi: 10.7326/0003-4819-117-12-1003. [DOI] [PubMed] [Google Scholar]
- 14.Frasure-Smith N, Lesperance F, Gravel G, et al. Social support, depression, and mortality during the first year after myocardial infarction. Circulation. 2000;101(16):1919–24. doi: 10.1161/01.cir.101.16.1919. [DOI] [PubMed] [Google Scholar]
- 15.Lett HS, Blumenthal JA, Babyak MA, et al. Dimensions of social support and depression in patients at increased psychosocial risk recovering from myocardial infarction. Int J Behav Med. 2009;16(3):248–58. doi: 10.1007/s12529-009-9040-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Sun YH, Sun L, Wu HY, et al. Loneliness, social support and family function of people living with HIV/AIDS in Anhui rural area, China. Int J STD AIDS. 2009;20(4):255–8. doi: 10.1258/ijsa.2008.008348. [DOI] [PubMed] [Google Scholar]
- 17.Cote J, Godin G, Garcia PR, et al. Program development for enhancing adherence to antiretroviral therapy among persons living with HIV. AIDS Patient Care STDS. 2008;22(12):965–75. doi: 10.1089/apc.2008.0124. [DOI] [PubMed] [Google Scholar]
- 18.Hansen NB, Vaughan EL, Cavanaugh CE, et al. Health-related quality of life in bereaved HIV-positive adults: relationships between HIV symptoms, grief, social support, and Axis II indication. Health Psychol. 2009;28(2):249–57. doi: 10.1037/a0013168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kessler RC, Price RH, Wortman CB. Social factors in psychopathology: stress, social support, and coping processes. Annu Rev Psychol. 1985;36:531–72. doi: 10.1146/annurev.ps.36.020185.002531. [DOI] [PubMed] [Google Scholar]
- 20.Bergen SE, Gardner CO, Aggen SH, et al. Socioeconomic status and social support following illicit drug use: causal pathways or common liability? Twin Res Hum Genet. 2008;11(3):266–74. doi: 10.1375/twin.11.3.266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Den Oudsten BL, Van Heck GL, Van der Steeg AF, et al. Personality predicts perceived availability of social support and satisfaction with social support in women with early stage breast cancer. Support Care Cancer. 2009 doi: 10.1007/s00520-009-0714-3. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 22.Wilkinson R. Unhealthy Societies: The Afflictions of Inequality. New York: Routledge; 1996. [Google Scholar]
- 23.Grant BF, Kaplan K, Shepard J, et al. Source and Accuracy Statement for Wave 1 of the 2001–2002 of the National Epidemiologic Survey on Alcohol and Related Conditions. Bethesda, MD: National Institute on Alcohol Abuse and Alcoholism; 2003. [Google Scholar]
- 24.Grant BF, Goldstein RB, Chou SP, et al. Sociodemographic and psychopathologic predictors of first incidence of DSM-IV substance use, mood and anxiety disorders: results from the Wave 2 National Epidemiologic Survey on Alcohol and Related Conditions. Mol Psychiatry. 2008 doi: 10.1038/mp.2008.41. [Epub ahead of print] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ruan WJ, Goldstein RB, Chou SP, et al. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of new psychiatric diagnostic modules and risk factors in a general population sample 5. Drug Alcohol Depend. 2008;92(1–3):27–36. doi: 10.1016/j.drugalcdep.2007.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Grant BF, Dawson DA, Stinson FS, et al. The Alcohol Use Disorder and Associated Disabilities Interview Schedule-IV (AUDADIS-IV): reliability of alcohol consumption, tobacco use, family history of depression and psychiatric diagnostic modules in a general population sample. Drug Alcohol Depend. 2003;71(1):7–16. doi: 10.1016/s0376-8716(03)00070-x. [DOI] [PubMed] [Google Scholar]
- 27.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4th edn. Washington, DC: American Psychiatric Association; 1994. Revised edn. [Google Scholar]
- 28.Stata Corp. STATA. College Station, TX: 2003. [Google Scholar]
- 29.Sarver JH. IDONEPSU: stata module for dealing with strata that have singleton PSUs. 2001 [Google Scholar]
- 30.Kendler KS, Gardner CO, Prescott CA. Toward a comprehensive developmental model for major depression in women. Am J Psychiatry. 2002;159(7):1133–45. doi: 10.1176/appi.ajp.159.7.1133. [DOI] [PubMed] [Google Scholar]
- 31.Dafer RM, Rao M, Shareef A, et al. Poststroke depression. Top Stroke Rehabil. 2008;15(1):13–21. doi: 10.1310/tsr1501-13. [DOI] [PubMed] [Google Scholar]
- 32.Salter KL, Moses MB, Foley NC, et al. Health-related quality of life after stroke: what are we measuring? Int J Rehabil Res. 2008;31(2):111–7. doi: 10.1097/MRR.0b013e3282fc0f33. [DOI] [PubMed] [Google Scholar]
- 33.Gwadz MV, Cylar K, Leonard NR, et al. An exploratory behavioral intervention trial to improve rates of screening for AIDS clinical trials among racial/ethnic minority and female persons living with HIV/AIDS. AIDS Behav. 2009 doi: 10.1007/s10461-009-9539-9. [Epub ahead of print] [DOI] [PubMed] [Google Scholar]
- 34.Reblin M, Uchino BN. Social and emotional support and its implication for health. Curr Opin Psychiatry. 2008;21(2):201–5. doi: 10.1097/YCO.0b013e3282f3ad89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Uchino BN. Social support and health: a review of physiological processes potentially underlying links to disease outcomes. J Behav Med. 2006;29(4):377–87. doi: 10.1007/s10865-006-9056-5. [DOI] [PubMed] [Google Scholar]
- 36.Uchino BN, Cacioppo JT, Kiecolt-Glaser JK. The relationship between social support and physiological processes: a review with emphasis on underlying mechanisms and implications for health. Psychol Bull. 1996;119(3):488–531. doi: 10.1037/0033-2909.119.3.488. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.