Abstract
Previous studies have not compared Health-related Quality of Life (HR-QoL) across all DSM-IV anxiety disorders and comorbid conditions. We compared the effects of each anxiety disorder on HR-QoL, controlling for demographic variables, medical conditions, and comorbid Axis I disorders. Data are obtained from the Primary Care Anxiety Project (PCAP), a naturalistic, longitudinal study of anxiety disorders in 539 primary care patients. Each of the anxiety disorders was associated with worse self-reported physical and mental functioning compared to general population means. While all of the anxiety disorders were univariate predictors of specific domains of HR-QoL, only presence of Posttraumatic Stress and Disorder (PTSD) and comorbid Depressive Disorder (MDD) uniquely predicted worse functioning on both self-report and interview measures. The current study extends previous research by showing that different anxiety disorders and comorbid conditions may be associated with impairment in specific domains of HR-QoL.
Keywords: Anxiety, Quality of Life, Primary Care, SF-36
1. Introduction
The anxiety disorders are the most prevalent class of mental disorders, with over 28% of the population meeting criteria for an anxiety disorder at some point in their lifetime (Kessler, Chia, Demler, & Walters, 2005). Patients with anxiety disorders present with a range of symptoms that may negatively impact quality of life in multiple domains. Health Related Quality of Life (HR-QoL) comprises an individual’s subjective level of functioning and well-being in physical, mental, and social domains of life (Hays & Morales, 2001). Recent studies suggest that HR-QoL is a distinct construct from symptom severity. For example, studies have found that symptom severity does not account for a large proportion of variance in HR-QoL in participants with a range of anxiety and depressive disorders (Barrera & Norton, 2009; Rapaport, Clary, Fayyad, & Endicott, 2005). Supporting this distinction, a naturalistic, longitudinal study found that impairment in HR-QoL continued following recovery from an anxiety disorder (Stout, Dolan, Dyck, Eisen, & Keller, 2001). Although a distinct construct, HR-QoL may still affect the course of anxiety disorders. For example, worsening psychosocial functioning has been found to predict recurrence of some anxiety disorders (Rodriguez, Bruce, Pagano, & Keller, 2005).
The relationship between individual anxiety disorders and impaired HR-QoL is now well established (Olatunji, Cisler, & Tolin, 2007). A recent meta-analysis including studies of the general population, clinical samples, and primary care samples suggested that PTSD may be associated with relatively poorer HR-QoL and SP with relatively better HR-QoL among the anxiety disorders (Olatunji et al., 2007). However, there were no significant differences in HR-QoL among the anxiety disorders. Accurate comparisons across the anxiety disorders have been limited because few researchers have examined more than one anxiety disorder simultaneously within the same study (Olatunji et al., 2007).
Recently, a few studies have compared HR-QoL among multiple anxiety disorders simultaneously to determine the relative impact of specific disorders. For example, Rapaport et al., (2005) found that Panic Disorder (PD), Social Phobia (SP), Obsessive Compulsive Disorder (OCD), and Post-traumatic Stress Disorder (PTSD) were each associated with impairment compared to community norms. The most severe impairment was observed in PTSD. Quilty et al. (2003) compared SP, Panic Disorder (PD), OCD, and comorbid MDD and found that SP and comorbid MDD uniquely predicted impaired HR-QoL. In contrast with these studies but consistent with the Olatunji et al. (2007) meta-analysis, Barrera and Norton (2009) found no differences in quality of life among Generalized Anxiety Disorder (GAD), SP, and PD.
Although the above studies begin to extend our understanding of potential relative differences in HR-QoL among the anxiety disorders, the findings are inconsistent and further study is warranted. First, none of these studies included all of the anxiety disorders. Second, they all relied on self-report measures of HR-QoL. Finally, the above findings are specific treatment seeking samples, and further studies are needed in more generalizable samples.
Samples of primary care patients may be more heterogeneous than clinical samples (e.g., more comorbidity, include individuals who are not receiving treatment). Primary care samples are also particularly relevant to the study of anxiety disorders. Anxiety disorder patients are more likely to seek treatment from primary care physicians than mental health specialists (Harman, Rollman, Hanusa, Lenze, & Shear, 2002). One study estimated that as many as 47% of office visits to general medical physicians were due to anxiety symptoms (Skaer, Sclar, & Robison, 2008). Similar to other types of settings, few primary care studies have examined HR-QoL in more than one anxiety disorder. One primary care study that did examine multiple anxiety disorders found that PTSD predicted worse functioning compared to the other anxiety disorders (Schonfeld et al., 1997). However, that study utilized DSM-III-R criteria and excluded any patients who were receiving treatment for anxiety or depression. Thus, results may be an underestimate of impairment for some disorders, as treatment seeking is frequently associated with poorer functioning and worse course, presumably because patients with more severe symptoms seek treatment (DeWit, Ogborne, Offord, & MacDonald, 1999).
In sum, further studies are needed to advance our understanding of which anxiety disorders and comorbid conditions affect HR-QoL, as well as to identify specific associations with domains of functioning. Such information may lead to improved assessment, treatment, recovery, and relapse prevention after recovery. To this end, we examined HR-QoL in a large sample of primary care patients with a range of anxiety and comorbid disorders. Most previous studies utilized only one measure of HR-QoL (Olatunji et al., 2007), and researchers have recommended that future work include multiple measures (Rapaport et al., 2005). Furthermore, it is important to assess HR-QoL with both self-report and interview measures because they assess different perspectives of HR-QoL. For example, a clinician may rate an individual with SP as more impaired compared to a self-report rating because the individual may have lost perspective on “normalcy” due to a young age of onset and chronic course (Rapaport et al., 2005). Thus, in the current study, we assessed HR-QoL with a widely used self-report measure (The Medical Outcomes Survey Short Form-36; (Ware & Kosinski, 2001)) and an interviewer rated measure of overall psychosocial functioning (Global Social Adjustment Scale; (Keller, Lavori, Friedman, & Nielsen, 1987).
Data are obtained from the Primary Care Anxiety Project (PCAP), a prospective, naturalistic study of anxiety disorders in primary care patients. Consistent with previous findings, we expected that all of the anxiety disorders would be associated with poor HR-QoL compared to the general population. We also expected that among the anxiety disorders, poorer HR-QoL would be associated with the presence of PTSD after controlling for demographic variables, other anxiety disorders, and comorbid conditions. We also expected comorbid MDD to be a strong predictor of worse functioning. Finally, we anticipated observing additional differences among the disorders not previously reported, given the current study’s inclusion of all anxiety disorders, numerous comorobid conditions, and use of a self-report and interview measure of HR-QoL.
2. Methods
2.1 Study Design
Participants in this study are part of the Primary Care Anxiety Project (PCAP), a prospective, naturalistic, short interval interview, longitudinal study of anxiety disorders in primary care settings. The PCAP study was conducted in five rural and 10 urban/suburban internal medicine and family medicine practices in New Hampshire, Massachusetts, Rhode Island, and Vermont. Four of the sites were small, private practices, four were free-standing clinics with a university affiliation, and seven were large university teaching hospital-based clinics. Descriptions of participant recruitment and screening procedures can be found in other published reports (Rodriguez et al., 2004; Weisberg et al., 2002). PCAP was approved by the institutional review board of Brown University and participating hospitals. All participants provided written informed consent prior to enrollment in the study. Once enrolled, participants were contacted for an in-person or telephone follow-up interview at 6 and 12 months, and annually thereafter. This report focuses on intake data only.
Participants
Criteria to be enrolled in PCAP included being diagnosed with at least one of the following anxiety disorders, according to the Structured Clinical Interview for the DSM-IV (SCID-IV): PTSD, SP, Panic Disorder (PD), Panic Disorder with Agoraphobia (PDA), and Generalized Anxiety Disorder (GAD). There was also a small sample of patients with GAD features occurring solely during the course of a mood disorder, mixed anxiety-depressive disorder, or Agoraphobia with out history of PD. A total of 539 patients who met DSM-IV criteria for one or more index anxiety disorders were included in the full PCAP sample. To be eligible for the study, participants needed to be at least 18 years of age, English-speaking, and scheduled for a general medical appointment on the day of recruitment. Participants were excluded from the study if they were suffering from active psychosis, had no current address and phone number, or were pregnant.
2.3 Measures
Diagnostic Clinical Interview
For the PCAP study, all clinical diagnoses were established by means of in-person diagnostic interviews that employed the SCID-IV (First, Spitzer, Gibbon, & Williams, 1996). The psychotic screen, mood, anxiety, substance use, and eating disorders modules of the SCID-IV were administered. Interviewers completed a rigorous training program, and PCAP clinical staff reviewed each diagnosis. Training and diagnostic review procedures are detailed in previous published reports (Rodriguez et al., 2004).
HR-QoL Measures
We utilized a multi-modal assessment of HR-QoL including a self-report and interviewer rated measure: The Medical Outcomes Study (MOS) 36-Item Short-Form Health Survey (SF-36)(Ware & Kosinski, 2001) is a widely used self-report measure of HR-QoL. The 36 item measure yields two summary scores: Physical Component Score (PCS) and Mental Component Score (MCS).1 Higher scores indicate better functioning. The SF-36 has demonstrated excellent internal consistency (McHorney, Ware, Lu, & Sherbourne, 1994) and construct validity (McHorney, Ware, & Raczek, 1993).
The Global Social Adjustment Scale (GSA) is part of the Longitudinal Interval Follow-up Evaluation for the DSM-IV (LIFE) (Keller et al., 1987). The interrater reliability for items on the LIFE has been found to be good, with the intraclass correlation coefficients (ICC) ranging from .58 to .91(Keller et al., 1987; Warshaw, Keller, & Stout, 1994). In the LIFE, the GSA is an interviewer’s rating of an individual’s current level of overall psychosocial functioning. After assessing an individual’s functioning in specific domains, the interviewer rates the overall level of psychosocial adjustment during the past week, taking into consideration everything the interviewer knows about the individual’s education, social background, and the level of functioning in the areas of work, self-satisfaction, interpersonal relations, and sex. The interviewer makes a rating from 1 (no impairment) to 5 (marked impairment).
Non-Psychiatric Medical Problems
A Medical History Form designed for the study (Weisberg et al., 2002) was used to assess medical problems. Participants were asked whether or not they have ever had any of the following illnesses or medical problems: asthma, cancer, diabetes, epilepsy, heart disease, kidney disease, liver disease, lung or respiratory illness, stroke and/or thyroid disease. For the present study, medical illness was coded as a dichotomous yes/no response for the presence of at least one current non-psychiatric medical illness.
2.4 Statistical Analyses
Analyses were conducted using SAS software. We first examined whether each PCAP index anxiety disorder, comorbid condition, and number of disorders individually predicted each measure of HR-QoL after controlling for demographic variables (age, gender, race, marital status, education). We then included any significant predictors simultaneously in a multivariate regression model to examine unique predictors of HR-QoL. In total, we examined the following predictors: age, gender, race, education, marital status, presence of current medical illness, number of disorders, PCAP index anxiety disorders (PTSD, SP, GAD, PD, PDA), and comorbid disorders (OCD, Specific Phobia, MDD, Substance Use Disorders (SUD)). In the current study, OCD and Specific Phobia are considered comorbid conditions because these disorders were not PCAP index disorders, meaning that a patient had to have one of the other anxiety disorders to be included in the PCAP sample. We did not include mixed anxiety-depressive disorder, GAD within a mood disorder, or Agoraphobia without history of PD as predictors because these disorders had too few cases. Statistical significance was set at .05, and a Bonferroni correction was applied for each model to account for multiple statistical comparisons.
3. Results
3.1 Characteristics of Sample
Sociodemographic characteristics of the participants are presented in Table 1. The 539 participants ranged in age from 18 to 78 years (M = 39 years). The majority of participants were female and white. Half of participants were currently married or living together with partners. Less than half of patients had completed some college; less than 40% of patients were employed full-time; and more than half of patients earned less than $19,999 annually.
Table 1.
Sociodemographic Characteristics
| Characteristic | N | % |
|---|---|---|
| Sex | ||
| Female | 412 | 76.4 |
| Male | 127 | 23.6 |
| Age in years (M, SD) | 39 | 11.6 |
| Race/ethnicity | ||
| White | 447 | 82.9 |
| Black | 41 | 7.6 |
| Asian | 7 | 1.3 |
| Hispanic | 19 | 3.5 |
| Native American | 9 | 1.7 |
| Other | 16 | 3.0 |
| Marital Status | ||
| Never Married | 147 | 27.3 |
| Marrieda | 267 | 49.5 |
| Divorced/separated/widowed | 104 | 23.2 |
| Education | ||
| < High school graduate | 52 | 9.7 |
| High school graduate | 134 | 24.9 |
| Some college | 229 | 42.5 |
| College graduate | 124 | 23.0 |
| Income ($ per year) | ||
| < 5,000 | 95 | 18.5 |
| 5,000 – 19,999 | 196 | 38.1 |
| 20,000 – 34,999 | 104 | 20.2 |
| 35,000 – 49,999 | 67 | 13.0 |
| > 50,000 | 53 | 10.3 |
| Fulltime Employment | ||
| No | 330 | 61.2 |
| Yes | 209 | 38.8 |
| Health Insurance b | ||
| None | 48 | 9.1 |
| Medicare or public assistance | 173 | 32.6 |
| Private | 330 | 62.3 |
| Military | 7 | 1.3 |
Includes persons living with someone as though married.
Percentages do not add up to 100 due to some patients having multiple types of insurance.
Table 2 displays the number of participants meeting DSM-IV criteria for several Axis I disorders at intake. PTSD was the most common anxiety disorder, and MDD was the most common disorder overall. Patterns of comorbidity in the PCAP sample are described in detail elsewhere (Rodriguez et al., 2004). Briefly, more than 70% of the PCAP sample was diagnosed with multiple current Axis I disorders at the time of study intake, with 29% having two, 23% having three, and 19% having four or more current Axis I conditions.
Table 2.
Current Disorders and HR-QoL Measures
| DSM-IV Mental Disorder | N | % |
|---|---|---|
| PCAP Index Anxiety Disorders | ||
| Posttraumatic Stress Disorder | 199 | 36.9 |
| Social Phobia | 182 | 33.8 |
| Panic Disorder | 85 | 15.8 |
| Panic Disorder with Agoraphobia | 150 | 27.8 |
| Generalized Anxiety Disorder | 135 | 25.1 |
| Comorbid Disorders | ||
| Obsessive-compulsive Disorder | 39 | 7.2 |
| Specific Phobia | 92 | 17.1 |
| Major Depressive Disorder | 220 | 40.8 |
| Alcohol/Substance Use Disorder | 55 | 10.2 |
| Current Medical Condition | 269 | 49.9 |
| M | SD | |
|
| ||
| Total Number of Index Disorders at Intake | 1.5 | 0.73 |
| SF-36 Physical Component Score | 43.7 | 12.34 |
| SF-36 Mental Component Score | 36.9 | 12.14 |
| Global Social Adjustment Scale | 3.2 | 0.93 |
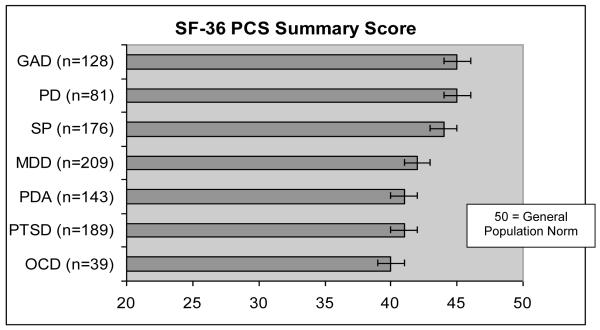
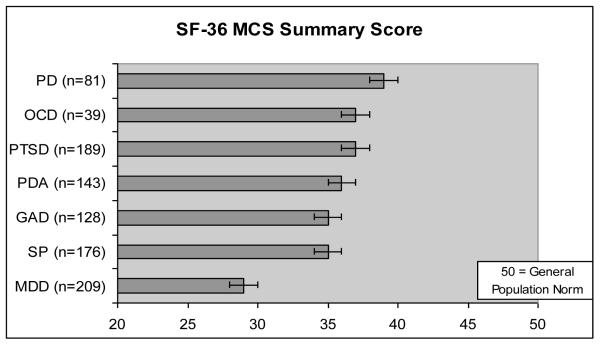
Table 2 presents descriptive statistics for the SF-36 composite scores and GSA scores. The mean (SD) GSA score was 3.2 (0.9), reflecting a moderate level of impairment in the total sample. The overall mean (SD) PCS and MCS scores were 43.7 (12.3) and 36.9 (12.1) respectively. The mean summary scores for each index disorder, and for MDD and the presence of a medical condition, are presented in Figure 1 (physical functioning) and Figure 2 (mental functioning). As expected, the means for all of the anxiety disorders were lower (indicating worse HR-QoL) compared to the general population (M = 50) for both physical and mental functioning.
Figure 1.
Physical Component Score
Note: Due to comorbidity, the disorder categories are NOT mutually exclusive. For example, ALL participants in the MDD group also had at least one anxiety disorder.
Figure 2.
Mental Component Score
3.2 Predictors of HR-QoL
3.2.1 Physical Functioning
Presence of PTSD, a current non-psychiatric medical condition, comorbid OCD, and number of disorders each individually significantly predicted worse PCS scores after controlling for demographic variables. When these significant predictors and demographic variables were included in a multivariate regression model, the following variables remained significant (ps < .006) predictors of worse physical functioning: older age, less education, and current non-psychiatric medical condition. PTSD was a marginal predictor in the model (p = .009), and comorbid OCD was not a significant predictor (p = .086). Test statistics for the PCS are presented in Table 3.
Table 3.
Multivariate Regression Model Predicting PCS scores
| Predictor (N = 516) | β | SE | t | p |
|---|---|---|---|---|
| Age | −.2518 | .0506 | −4.98 | <.0001 |
| Female | −.2381 | 1.1599 | −.21 | .8375 |
| Caucasian | 2.1837 | 1.3460 | 1.62 | .1054 |
| Marital status | ||||
| Never married | .8344 | 1.3059 | .64 | .5231 |
| Separated, Divorced, Widowed | 1.6496 | 1.2560 | 1.31 | .1897 |
| Education | ||||
| Never graduated HS | −9.6385 | 1.904 | −5.02 | <.0001 |
| Never attended college (HS degree) | −6.1761 | 1.4329 | −4.31 | <.0001 |
| Never graduated from a 4-year college | −5.4775 | 1.2856 | −4.26 | <.0001 |
| Any comorbid medical conditions | −5.9598 | 1.0251 | −5.81 | <.0001 |
| Number of disorders | −.2150 | .4592 | −.47 | .6398 |
| Post Traumatic Stress Disorder | −2.8026 | 1.0753 | −2.61 | .0094 |
| Obsessive Compulsive Disorder | −3.3688 | 1.9573 | −1.72 | .0858 |
3.2.2 Mental Functioning
Presence of SP, GAD, comorbid MDD and Substance Use Disorders (SUD), and number of disorders each individually significantly predicted worse MCS scores after controlling for demographic variables. When these significant predictors and demographic variables were included in a multivariate regression model, the following variables remained significant (ps < .005) predictors of worse mental functioning: current marital status of separated / divorced / widowed and comorbid MDD. Younger age and the presence of SP, GAD, and comorbid SUD were marginal predictors of mental functioning (ps < .058) in the multivariate analysis. Number of disorders was not a unique predictor in this model. Test statistics for the MCS are presented in Table 4.
Table 4.
Multivariate Regression Model Predicting MCS scores
| Predictor (N = 516) | β | SE | t | p |
|---|---|---|---|---|
| Age | .1098 | .0453 | 2.43 | .0156 |
| Female | −.6212 | 1.0933 | −.57 | .5701 |
| Caucasian | −.6396 | 1.2492 | −.51 | .6089 |
| Marital status | ||||
| Never married | −1.1726 | 1.2364 | −.95 | .3434 |
| Separated, Divorced, Widowed | −4.0674 | 1.1614 | −3.50 | .0005 |
| Education | ||||
| Never graduated HS | −.2740 | 1.7913 | −.15 | .8785 |
| Never attended college (HS degree) | −.3976 | 1.3264 | −.30 | .7645 |
| Never graduated from a 4 year college | 1.8554 | 1.1967 | 1.55 | .1217 |
| Number of disorders | .2595 | .5400 | .48 | .6310 |
| Social Phobia | −2.6702 | 1.0693 | −2.50 | .0128 |
| Generalized Anxiety Disorder | −2.5887 | 1.1078 | −2.34 | .0198 |
| Major Depressive Disorder | −12.6141 | 1.1046 | −11.42 | <.0001 |
| Substance Use Disorders | −3.1388 | 1.6497 | −1.90 | .0577 |
3.2.3 Global Social Adjustment Scale (GSA)
Finally, we examined the same set of predictors for the interviewer rated measure of overall psychosocial functioning. Presence of PTSD, SP, PDA, comorbid MDD, comorbid medical condition, and number of disorders each individually significantly predicted worse GSA scores after controlling for demographic variables. When these significant predictors and demographic variables were included in the multivariate regression model, the following variables remained significant (ps < .005) predictors of worse psychosocial functioning: current marital status of never married, the presence of PTSD and comorbid MDD. There was a trend for educational status of never graduating from high school and never attending college, and the presence of SP and PDA to predict worse GSA scores (ps < .05) in the multivariate analysis. Number of disorders was not a unique predictor in this model. Test statistics for the GSA are presented in Table 5.
Table 5.
Multivariate Regression Model Predicting GSA scores
| Predictor (N = 539) | β | SE | t | p |
|---|---|---|---|---|
| Age | .0065 | .0035 | 1.87 | .0617 |
| Female | .1176 | .0801 | 1.47 | .1430 |
| Caucasian | −.2401 | .0929 | −2.58 | .0101 |
| Marital status | ||||
| Never married | .3522 | .0900 | 3.91 | .0001 |
| Separated, Divorced, Widowed | .2308 | .0881 | 2.62 | .0091 |
| Education | ||||
| Never graduated HS | .2668 | .1349 | 1.98 | .0484 |
| Never attended college (HS degree) | .2444 | .1004 | 2.43 | .0152 |
| Never graduated from a 4 year college | .0749 | .0895 | 0.84 | .4030 |
| Post Traumatic Stress Disorder | .2629 | .0779 | 3.37 | .0008 |
| Social Phobia | .1546 | .0786 | 1.97 | .0497 |
| Panic Disorder with Agoraphobia | .2309 | .0844 | 2.74 | .0064 |
| Major Depressive Disorder | .7236 | .0854 | 8.47 | <.0001 |
| Any Comorbid Medical Conditions | .0529 | .0712 | 0.74 | .4582 |
| Number of disorders | .0202 | .0424 | 0.48 | .6337 |
4. Discussion
Although each of the anxiety disorders has been associated with impaired HR-QoL, this is the first study to examine the relative differences in HR-QoL across all of DSM-IV anxiety disorders and comorbid conditions using both self-report and interview HR-QoL measures. As expected, all of the anxiety disorders were associated with worse mental and physical functioning compared to the general population. This finding replicates many previous studies and underscores the importance of addressing HR-QoL in the assessment and treatment of anxiety disorders. The value of targeting HR-QoL in anxiety disorders may be especially relevant to primary care physicians because most individuals initially seek treatment from primary care providers (Harman et al., 2002).
A recent meta-analysis did not find significant differences in HR-QoL among the anxiety disorders, but noted that few studies had examined multiple anxiety disorders simultaneously (Olatunji et al., 2007). The current study, which did examine multiple disorders, partially supports the conclusion in the meta-analysis, as each of the PCAP index anxiety disorders predicted at least one domain of HR-QoL (with the exception of PD without Agoraphobia). However, as expected, only PTSD and comorbid MDD remained significant in the multivariate models and were associated with two domains of impairment (whereas the other disorders were associated with only one domain).
The current results do not suggest that all of the anxiety disorders are associated with the same type of impairment in HR-QoL. Rather, different anxiety disorders were associated with different domains of HR-QoL. Presence of PTSD, comorbid OCD, and a current medical condition predicted worse self-reported physical functioning. Presence of SP, GAD, and comorbid MDD predicted worse self-reported mental functioning, although only MDD was a unique predictor. Finally, the presence of PTSD, PDA, SP, and comorbid MDD predicted worse interviewer-rated, overall psychosocial functioning, with PTSD and MDD remaining unique predictors.
Previous research has generally relied on a single, self-report measure of HR-QoL. The current study used both a self-report and interviewer rated measure and found that impairment in some disorders may not be evident on all measures of HR-QoL. For example, in the current study, PDA’s association with impairment was only revealed in the interviewer-rated measure. Future research may also benefit from including an interviewer based measure, as an interviewer, unbiased by having a chronic disorder, may have a different perspective of an individual’s impairment level.
Consistent with previous findings, PTSD and comorbid MDD were more robustly associated with impairment than the other disorders. Only PTSD and MDD showed impairment on both self-report and interviewer rated measures. Previous studies examining clinical (Rapaport et al., 2005) and primary care samples (Schonfeld et al., 1997) have also suggested that PTSD is associated with relatively worse functioning compared to other anxiety disorders. It is important to note that in the current study, all participants had at least one anxiety disorder to qualify for study entry. Thus, all MDD was comorbid with an anxiety disorder, whereas not all cases of any of the anxiety disorders were comorbid. Thus, findings indicate that, among anxiety disorder patients, having comorbid MDD predicts worse HR-QoL than not having MDD. With that noted, these findings strongly suggest that clinicians should address HR-QoL issues in their assessment and treatment of PTSD, as well as comorbid MDD in anxiety disorder patients.
Presence of SP and GAD predicted worse self-reported mental functioning, although this association fell to a trend level in the multivariate model. Individuals with GAD have at times been viewed as the “worried well.” Similarly, previous studies have suggested that SP may be associated with relatively better functioning compared to other anxiety disorders (Olatunji et al., 2007). Current findings, as well as other recent studies contrast these views. Using a different self-report measure of HR-QoL (i.e., EuroQoL-5D), Saarni et al. (2007) also found that SP and GAD had a greater impact on HR-QoL compared to panic and agoraphobia. Additionally, Quilty et al. (2003) found that SP was associated with poorer HR-QoL than PD or OCD. A recent review of 31 studies suggests that GAD is associated with significant impairment in HR-QoL that is similar to MDD in magnitude (Hoffman, Dukes, & Wittchen, 2008). One explanation for these different conclusions may be differences in samples. For example, it is unlikely that clinical trial samples represent the HR-QoL of most individuals with SP. Indeed, only 4% of people with SP sought treatment in the National Comorbidity Survey (Magee, Eaton, Wittchen, McGonagle, & Kessler, 1996).
As an index of the overall effect of comorbidity on HR-QoL, we entered participants’ number of disorders as a predictor. The number of comorbid disorders did not uniquely predict any domains of HR-QoL. Thus, comorbidity alone may not affect HR-QoL. Additionally, presence of a comorbid substance use disorder did not uniquely predict any of the HR-QoL measures. This finding converges with a previous study that found smaller effects on HR-QoL due to alcohol dependence compared to anxiety disorders (Saarni et al., 2007). It is also possible that the failure to find a significant effect here was due to the low number of participants in this sample reporting a substance use disorder.
Other comorbid conditions did predict worse HR-QoL. For example, comorbid OCD predicted worse physical functioning, although this relationship fell to a trend level in the multivariate model. A recent study also revealed impaired HR-QoL in OCD, but in the domains of work, social life, and family life (Huppert, Simpson, Nissenson, Liebowitz, & Foa, 2009). That study did not examine physical functioning. OCD has received considerably less attention in studies of HR-QoL, and the current results suggest that future research should include this disorder in their examinations. However, it is important to recall that OCD was not an index anxiety disorder in this study. Thus, similar caution applies to interpretation of our OCD findings, as does to the findings discussed earlier, regarding comorbid MDD. Specifically, results only detail the increase in impairment that individuals, already suffering from an anxiety disorder, experience when they also have a diagnosis of OCD.
The finding that PTSD predicted worse physical functioning, whereas comorbid MDD did not, converges with previous studies that found a unique association between anxiety and physical disorders (Sareen, Cox, Clara, & Asmundson, 2005) and a stronger association with pain compared to depression (McWilliams, Cox, & Enns, 2003). Additionally, presence of a comorbid medical condition predicted worse HR-QoL. Together, these results highlight the need for researchers and clinicians to attend to physical functioning and medical conditions in individuals with anxiety disorders, as well as mechanisms underlying this relationship.
Strengths of the current study include use of a multi-modal assessment of HR-QoL in a large sample of primary care patients with a range of anxiety and comorbid disorders. The current study also has several limitations. First, we did not include a reference group (e.g., primary care patients without any Axis I disorder). Although we compared our means with general population norms, our results only speak to the relative differences in HR-QoL among the anxiety disorders. Additionally, some comorbid conditions, such as OCD and SUD, had relatively smaller samples sizes compared to the PCAP index disorders. Thus, findings regarding these disorders should be interpreted tentatively until replication with larger samples occurs.
Finally, the current study is not an epidemiological study, as we did not systematically interview all members of the available population. Our results are specific to primary care patients from the New England region who are mostly female, Caucasian, and already receiving care for medical conditions and may not generalize to all primary care populations, the general population, or more diverse samples. The most common anxiety disorder in the PCAP sample was PTSD, which does not parallel previous studies. Relatively higher rates of PTSD and lower rates of GAD may be due to the careful assessment of GAD that involved stringent enforcement of exclusion criteria (e.g., cannot occur during PTSD or MDD) and inclusion criteria (e.g., worry needed to be excessive). However, despite differences in sample composition, findings obtained from the PCAP sample do parallel those obtained from general population and clinical samples.
The current study cannot determine the causal direction of the relationship between anxiety disorders and impaired HR-QoL. Participants were only eligible for the study if they met criteria for an anxiety disorder at intake. Thus, we do not know if onset of an anxiety disorder preceded the impairment or vice versa. Finally, the current study did not examine clinical correlates of HR-QoL other than the presence of a disorder. Future studies might extend the current findings by identifying specific symptoms that impact HR-QoL (e.g., sleep difficulty in GAD). A related suggestion is for future studies to examine disorder effects on more specific domains of HR-QoL (e.g., pain, social relationships).
5. Conclusions
Most of the anxiety disorders predicted at least one domain of HR-QoL. However, after controlling for demographic variables and presence of other disorders only PTSD and comorbid MDD predicted indices of HR-QoL. Our results may alert researchers and clinicians to the importance of assessing impairment in multiple domains of HR-QoL in all of the anxiety disorders. Current findings support continued efforts directed toward identification and treatment of anxiety disorders, particularly in the primary care setting.
Acknowledgements
We thank Fengjuan Liu and Ingrid Dyck for assisting with the statistical analyses.
Role of Funding Source The Primary Care Anxiety Project is supported by an unrestricted grant from Pfizer Inc awarded to Dr. Keller. Pfizer, Inc. had no further role in study design; in the collection, analysis and interpretation of data; in the writing of the report; and in the decision to submit the paper for publication.
Disclosures Dr. Beard’s time and effort is supported in full by F32 MH083330. A portion of Dr. Weisberg’s salary at Brown is supported by the unrestricted grant from Pfizer, Inc. The majority of Dr. Weisberg’s time and effort is supported by K23 MH069595. Additionally, Dr. Weisberg has received honorarium from Astra Zeneca within the past 12 months. In the past two years, Dr. Keller has been a consultant/received honoraria from: Abbott, CENEREX, Cephalon, Cypress Bioscience, Cyberonics, Forest Laboratories, Janssen, JDS, Medtronic, Organon, Novartis, Pfizer, Roche, Solvay, Wyeth. During this time Dr. Keller was on advisory boards of Abbott Laboratories, Bristol-Myers Squibb, CENEREX, Cypress Bioscience, Cyberonics, Forest Laboratories, Janssen, Neuonetics, Novartis, Organon, and Pfizer; but is no longer on any such boards.
Footnotes
The SF-36 also yields eight subscales. However, to avoid an excessive number of comparisons and to simplify interpretation for multiple anxiety disorders, we chose to analyze the PCS and MCS summary scores, rather than the subscales.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Barrera TL, Norton PJ. Quality of life impairment in generalized anxiety disorder, social phobia, and panic disorder. Journal of Anxiety Disorders. 2009;23:1086–1090. doi: 10.1016/j.janxdis.2009.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DeWit DJ, Ogborne A, Offord DR, MacDonald K. Antecedents of the risk of recovery from DSM-III-R social phobia. Psychological Medicine. 1999;29:569–582. doi: 10.1017/s0033291799008399. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV axis I disorders - patient edition (SCID-I/PI, version 2.0) Biometrics Research Department; New York: 1996. [Google Scholar]
- Harman JS, Rollman BL, Hanusa BH, Lenze EJ, Shear MK. Physician Office Visits of Adults for Anxiety Disorders in the United States, 1985 to1998. Journal of Gen Intern Med. 2002;17:165–172. doi: 10.1046/j.1525-1497.2002.10409.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hays RD, Morales LS. The RAND-36 measure of health-related quality of life. Annals of Medicine. 2001;33:350–357. doi: 10.3109/07853890109002089. [DOI] [PubMed] [Google Scholar]
- Hoffman DL, Dukes EM, Wittchen H-U. Human and economic burden of generalized anxiety disorder. Depression and Anxiety. 2008;25:72–90. doi: 10.1002/da.20257. [DOI] [PubMed] [Google Scholar]
- Huppert JD, Simpson HB, Nissenson KJ, Liebowitz MR, Foa EB. Quality of life and functional impairment in obsessive-compulsive disorder: A comparison of patients with and without comorbidity, patients in remission, and healthy controls. Depression and Anxiety. 2009;26:39–45. doi: 10.1002/da.20506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Keller MB, Lavori PW, Friedman B, Nielsen E. The longitudinal interval follow-up evaluation: A comprehensive method for assessing outcome in prospective longitudinal studies. Archives of General Psychiatry. 1987;44:540–548. doi: 10.1001/archpsyc.1987.01800180050009. [DOI] [PubMed] [Google Scholar]
- Kessler RC, Chia WT, Demler O, Walters EE. Prevalence, Severity, and Comorbidity of 12-month DSM-IV Disorders in the National Comorbidity Survery Replication. Archives of General Psychiatry. 2005;62:617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Magee WJ, Eaton WW, Wittchen H-U, McGonagle KA, Kessler RC. Agoraphobia, simple phobia, and social phobia in the national comorbidity survey. Archives of General Psychiatry. 1996;53:159–168. doi: 10.1001/archpsyc.1996.01830020077009. [DOI] [PubMed] [Google Scholar]
- McHorney CA, Ware JE, Lu JFR, Sherbourne CD. The MOS 36-item Short-Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Medical Care. 1994;32:40–66. doi: 10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- McHorney CA, Ware JE, Raczek AE. The MOS 36-Item Short-Form Health Survey (SF-36): II. Psychometric and clinical tests of validity in measuring physical and mental health constructs. Medical Care. 1993;31:247–263. doi: 10.1097/00005650-199303000-00006. [DOI] [PubMed] [Google Scholar]
- McWilliams LA, Cox BJ, Enns MW. Mood and anxiety disorders associated with chronic pain: An examination in a nationally representative sample. Pain. 2003;106:127–133. doi: 10.1016/s0304-3959(03)00301-4. [DOI] [PubMed] [Google Scholar]
- Olatunji BO, Cisler JM, Tolin DF. Quality of life in the anxiety disorders: A meta-analytic review. Clinical Psychology Review. 2007;27:572–581. doi: 10.1016/j.cpr.2007.01.015. [DOI] [PubMed] [Google Scholar]
- Quilty LC, Ameringen MV, Mancini C, Oakman J, Farvolden P. Quality of life and the anxiety disorders. Journal of Anxiety Disorders. 2003;17:405–426. doi: 10.1016/s0887-6185(02)00225-6. [DOI] [PubMed] [Google Scholar]
- Rapaport MH, Clary C, Fayyad R, Endicott J. Quality-of-Life Impairment in Depressive and Anxiety Disorders. American Journal of Psychiatry. 2005;162:1171–1178. doi: 10.1176/appi.ajp.162.6.1171. [DOI] [PubMed] [Google Scholar]
- Rodriguez BF, Bruce SE, Pagano ME, Keller MB. Relationships among psychosocial functioning, diagnostic comorbidity, and the recurrence of generalized anxiety disorder, panic disorder, and major depression. Journal of Anxiety Disorders. 2005;19:752–766. doi: 10.1016/j.janxdis.2004.10.002. [DOI] [PubMed] [Google Scholar]
- Rodriguez BF, Weisberg RB, Pagano ME, Culpepper L, Keller MB, Machan JT. Frequency and patterns of psychiatric comorbidity in a sample of primary care patients with anxiety disorders. Comprehensive Psychiatry. 2004;45:129–137. doi: 10.1016/j.comppsych.2003.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Saarni SI, Suvisaari J, Sintonen H, Pirkola S, Koskinen S, Aromaa A, Lonqvist J. Impact of psychiatric disorders on health-related quality of life: General population survey. British Journal of Psychiatry. 2007;190:326–332. doi: 10.1192/bjp.bp.106.025106. [DOI] [PubMed] [Google Scholar]
- Sareen J, Cox BJ, Clara I, Asmundson GJG. The Relationship Between Anxiety Disorders and Physical Disorders in The U.S. National Comorbidity Survey. Depression and Anxiety. 2005;21:193–202. doi: 10.1002/da.20072. [DOI] [PubMed] [Google Scholar]
- Schonfeld WH, Verboncoeur CJ, Fifer SK, Lipschutz RC, Lubeck DP, Buesching DP. The functioning and well-being of patients with unrecognized anxiety disorders and major depressive disorder. Journal of Affective Disorders. 1997;43:105–119. doi: 10.1016/s0165-0327(96)01416-4. [DOI] [PubMed] [Google Scholar]
- Skaer TL, Sclar DA, Robison LM. Trend in anxiety disorders in the USA 1990-2003. Primary Care & Community Psychiatry. 2008;13:1–7. [Google Scholar]
- Stout RL, Dolan R, Dyck I, Eisen J, Keller MB. Course of social functioning after remission from panic disorder. Comprehensive Psychiatry. 2001;42:441–447. doi: 10.1053/comp.2001.27894. [DOI] [PubMed] [Google Scholar]
- Ware J, Kosinski M. SF-36 Physical and Mental Health Summary Scales: A Manual for Users of Version 1. Second ed QualityMetric Incorporated; Lincoln: 2001. [Google Scholar]
- Warshaw MG, Keller MB, Stout RL. Reliability and validity of the longitudinal interval follow-up evaluation for assessing outcome of anxiety disorders. Journal of Psychiatric Research. 1994;28:531–545. doi: 10.1016/0022-3956(94)90043-4. [DOI] [PubMed] [Google Scholar]
- Weisberg RB, Bruce SE, Machan JT, Culpepper L, Keller MB, Kessler RC. Nonpsychiatric illness among primary care patients with trauma histories and posttraumatic stress disorder. Psychiatric Services. 2002;53:848–854. doi: 10.1176/appi.ps.53.7.848. [DOI] [PubMed] [Google Scholar]