Abstract
Introduction and hypothesis
This study evaluates the relevance of the tape position and change in shape (tape functionality) under in vivo conditions for mid-term outcome.
Methods
Changes in the sonographic tension-free vaginal tape (TVT) position relative to the percentage urethral length and the tape–urethra distance were determined after 6 and 48 months in 41 women with stress urinary incontinence.
Results
At 48 months, 76% (31/41) of women were cured, 17% (7/41) were improved, and 7% (3/41) were failures. Disturbed bladder voiding was present in 12% (5/41), de novo urge incontinence in 7% (3/41). The median TVT position was at 63% of urethral length. Median tape–urethra distance was 2.7 mm, ranging from 2.9 mm in continent patients without complications to 1.1 mm in those with obstructive complications. Patients with postoperative urine loss had a median distance of 3.9 mm. The tape was stretched at rest and C-shaped during straining in 15 of 41 women (37%) at 48 months (all continent). Patients with this tape functionality at 6 months were also cured at 48 months in 86% of cases (19/22), and only 14% (3/22) showed recurrent incontinence.
Conclusions
Mid-term data suggest an optimal outcome if the tape is positioned at least 2 mm from the urethra at the junction of the middle and distal thirds. Patients with optimal tape functionality at 6 months are likely to show mid-term therapeutic success.
Keywords: Introital ultrasound, Mid-term outcome, Stress urinary incontinence, Tape position, Tape tension→tape functionality, Tension-free vaginal tape (TVT)
Introduction
Surgical insertion of tension-free vaginal tape (TVT) aims at stabilizing the mid-third of the urethra. This therapeutic option for women with urinary incontinence has been extensively studied, but there is one aspect that has so far not received any scientific attention, namely how the elastic sling behaves in vivo during straining. Ultrasound (US) is an easy to perform imaging modality that allows in vivo evaluation of the TVT. Sonographic evaluation of the lower urinary tract has become an established component of the urogynecologic diagnostic workup of women presenting with urinary incontinence. US is a straightforward, fast, and reproducible dynamic imaging tool [1–5].
The aim of the study presented here is to summarize mid-term data on the relevance of the sonographically determined tape position and changes in TVT shape for the outcome of surgery and the occurrence of complications. Another aim is to identify intra-individual tape changes in this patient population and discuss their potential implications.
Patients and methods
Our mid-term study is based on the data obtained in 41 women with clinically and urodynamically proven stress urinary incontinence (SUI) who underwent TVT insertion at the Dept. of Urogynecology of en-Süd-Klinikum Schwelm (Germany) between April 2000 and June 2002 using the standard technique [6, 7]. The patients underwent routine postoperative examinations. All factors considered to possibly affect outcome at the time of examination were carefully documented to be available for later evaluation of treatment success in the setting of quality assurance. In this sense, data were obtained in a prospective manner.
The patients had a median age of 58.8 years (range, 38–82) and a median weight of 71.3 kg (range, 55–100) with a median body mass index (BMI) of 26.2 kg/m2 (range, 20–35). The median number of spontaneous deliveries was 2.0 (range, 0–5). One patient had a history of vacuum extraction, while none of the patients had had a cesarean section.
Since all study patients underwent routine investigations and introital US was used for quality assurance purposes, the study was exempted from formal Ethics Committee approval by the Institutional Review Board of the University of Göttingen, Germany. Nevertheless, all patients were informed about the study and consented to participate.
The patients’ incontinence symptoms were verified preoperatively by clinical examinations and urodynamic testing. In addition, the patients underwent a 1-h pad test, documented their drinking and voiding habits in a voiding diary, and were administered a self-completion detailed urinary incontinence questionnaire according to Ulmsten et al. [7] The patients assessed their subjective degree of suffering on a ten-point visual analogue scale (VAS) ranging from 0 (no suffering due to incontinence) to 10 (unbearable suffering due to incontinence).
Standardized introital ultrasound was performed after 6 months using an Ultramark HDI C9-5 ICT system (ATL, Hamburg, Germany) and after 48 months using a Toshiba Aplio [3]. Both follow-up ultrasound examinations were performed by the same examiners, using comparable ultrasound equipment and parameter settings. In addition, parallel measurements were performed to preclude systematic errors. With the patient in the semi-sitting position and a standardized bladder filling volume of 300 ml, the ultrasound probe (3.6–8.3-MHz vaginal probe, 160° ultrasound beam angle) was positioned in the area of the vaginal opening at the level of the external urethral orifice exerting the slightest pressure possible and aligning the axis of the probe to the patient’s long body axis. Postoperative US examinations were performed with a sonographically verified bladder filling volume of about 300 ml. With the probe in this position, median sagittal US views comprise the urinary bladder, urethra, suburethral vagina, pubic symphysis, and the interpubic disk.
The following parameters were analyzed: the position of the TVT (center of the tape) relative to the percentage urethral length, L, on median sagittal views and the shortest distance, A, in millimeters (mm) between the hypoechoic urethra and the tape. Urethral length was measured on a median sagittal scan with 300-ml bladder filling from the bladder neck (anterior edge) to the distal end of the hypoechoic urethra. The distance was measured by drawing a perpendicular line from the border of the hypoechoic periurethral muscle and mucosa to the tape, which has high echogenicity on sonography.
Changes in tape shape (tape functionality) during Valsalva’s maneuver were documented by video. At rest, the hyperechoic TVT lies parallel to the hypoechoic urethra. This TVT shape is referred to as “stretched out”. A typical change in TVT shape is observed during Valsalva’s maneuver. The dorsocaudal movement of the bladder neck and urethra causes the latter to assume a C-shape and press against the TVT. The tape being elastic adjusts its shape to the bent urethra and briefly becomes what we refer to as “C-shaped” as well. The maximum change observed in this setting served to divide the patients into three groups:
-
Group I
The tape is “stretched out” at rest and becomes “C-shaped” during straining.
-
Group II
The tape lies parallel to the urethral lumen at rest and during straining.
-
Group III
The tape is already “C-shaped” at rest and does not change upon straining.
All TVT operations in the study population were performed by two urogynecologists following the manufacturer’s recommendations [6].
Postoperatively, the patients’ symptoms were followed up by history, clinical examination, and introital US between the second and fifth postoperative day, at 6 and at 48 months. Additional urodynamic testing was performed in patients with therapeutic failure. Voiding dysfunction was defined as symptoms of stranguria and a postmicturition residual volume of greater than 100 ml at 48-months follow-up (median, 15 ml; range, 0–150) [8].
The outcome of TVT treatment was evaluated using a combination of objective and subjective criteria modified from the suggestions made by Ulmsten et al. in 1999 [7]. Patients were classified as cured if the postoperative cough test was negative, the 1-h pad test was negative (<2 g difference), and the degree of subjective suffering improved to over 90% (VAS score of 0 or 1). Criteria for improvement were involuntary loss of only a few drops of urine during straining or a 1-h pad test with a weight difference of 2–10 g (or a reduction of over 50%), and an improvement of the degree of suffering to over 75% (VAS score of 2 or 3) . All other patients were classified as therapeutic failures (even if they showed marked improvement of one of the parameters compared with their preoperative status).
Statistical analysis was done using the Wilcoxon–Mann–Whitney (WMW) test for continuous parameters and Pearson’s chi2 test for categorical data. Statistical significance was assumed at a p-value <0.05. Statistical tests were performed and graphic representations were generated using STATISTICA 8.0.725 (StatSoft, Inc. 2008).
Results
Table 1 lists the cure rates at 6- and 48-month follow-ups. Comparison of outcome at 6 and 48 months reveals that 86% (30/35) of the women initially classified as cured were still continent at the 48-month follow-up, 9% (3/35) showed improvement, and secondary therapeutic failure was noted in 6% (2/35).
Table 1.
Changes in outcome between 6 and 48 months after surgery
| Cured (48 months) | Improved (48 months) | Failure (48 months) | Total | |
|---|---|---|---|---|
| Cured (6 months) | 30 | 3 | 2 | 35 |
| Improved (6 months) | 1 | 3 | 0 | 4 |
| Failure (6 months) | 0 | 1 | 1 | 2 |
| Total | 31 | 7 | 3 | 41 |
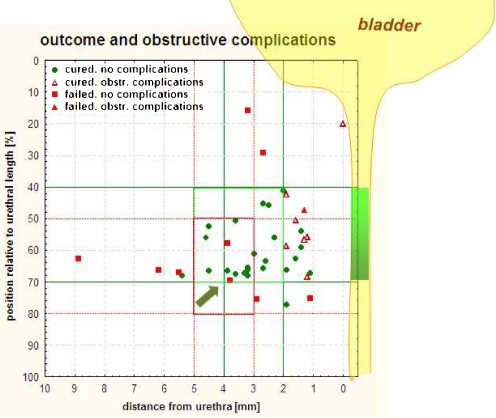
During the 48-month follow-up period, the median tape position (percentage relative to urethral length) changed from 65.0% (range, 22.0–87.0) to 62.5% (range, 15.7–77.0). The tape–urethra distance significantly decreased from 3.9 mm (range, 1.0–8.9) to 2.7 mm (range, 0.0–8.9) (p < 0.001). The optimal tape position determined at 6-month follow-up was at 50–80% of the urethral length with a tape–urethra distance of 3–5 mm. A significant ventrocranial shift of the tape was noted at 48 months as shown in Fig. 1. At 48 months, success rates were highest for tape positions between 40% and 70% of the urethral length and a tape distance of 2–5 mm. A tape position outside this range significantly decreased the likelihood of being cured (p < 0.001).
Fig. 1.
Outcome 48 months after TVT insertion according to tape position relative to the urethra and tape distance from the urethra. The optimal tape position, which was found to be at 50–80% of the urethral length with a tape–urethra distance of 3–5 mm at 6 months (indicated by red rectangle) [9], significantly shifts ventrocranially (p < 0.001). At 48 months, the highest success rates were found for tape position at 40–70 % of the urethral length and a tape–urethra distance of 2–5 mm (green square)
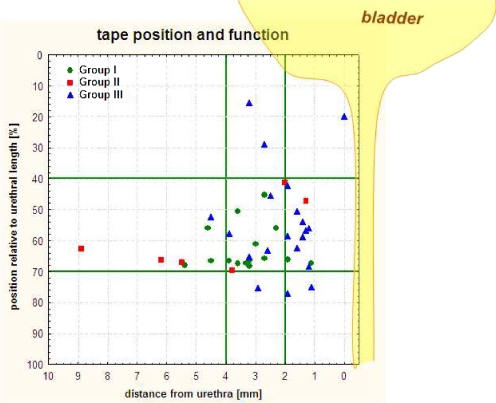
The data summarized in Table 2 demonstrate that ventrocranial shift of the tape affects tape function. An earlier study of our group revealed that tape functionality correlates with outcome at 6 months postoperatively [9]; the data of the present analysis show that a similar correlation also exists at 48-month follow-up. The cure rate was 100% (15/15) in women with a stretched tape at rest and a C-shape during straining (Group I). In contrast, 39% of the patients with tape shapes according to Groups II and III were incontinent (p < 0.001). Figure 2 shows the changes in tape shape in Groups I–III (tape functionality) by baseline tape position. Outcome was best in Group I, where most patients had a tape position between 40% and 70% of the urethral length. In Group II, the tape–urethra distance was typically 4 mm or more. Nevertheless, an unchanged tape (parallel to the urethra at rest and during straining) was observed in two women despite a small tape–urethra distance and was attributed to an immobile, rigid urethra. A change in tape shape according to Group III was seen when the tape distance was <2 mm and was significantly associated with obstructive complications.
Table 2.
Changes in tape functionality between 6 and 48 months after surgery
| Group I (48 months) | Group II (48 months) | Group III (48 months) | Total | |
|---|---|---|---|---|
| Group I (6 months) | 13 | 3 | 6 | 22 |
| Group II (6 months) | 2 | 3 | 0 | 5 |
| Group III (6 months) | 0 | 0 | 14 | 14 |
| Total | 15 | 6 | 20 | 41 |
Fig. 2.
Changes in tape shape in Groups I–III (tape functionality) by baseline tape position at 48-month follow-up. The groups are explained in the “Patients and methods” section
A multifactorial regression analysis taking into account all demographic and preoperative factors revealed no influence of any of these factors on the women’s outcome.
The rate of obstructive complications increased from 12% (5/41) to 19% (8/41) between the 6- and 48-month postoperative follow-ups. There was a change in the critical minimum distance of the tape from the urethra below which obstructive complications occurred. At the 6-month follow-up, a tape distance of less than 3 mm was associated with a significantly higher complication rate (p < 0.001). At the 48-month follow-up, all women with obstructive complications had a tape–urethra distance of less than 2 mm. The median tape distance in women with obstructive complications was 1.3 mm. Patients who were classified as cured had a significantly greater median tape–urethra distance of 2.9 mm (p < 0.001). Women with a less than 2 mm distance had a 2.8-fold higher risk of obstructive complications.
At the 6-month follow-up, a tape distance of less than 2 mm was measured in 14 patients; five of the patients (36%) had obstructive complications. The VAS scores these patients assigned to their degree of suffering were 6, 5, 0, 5, and 3. The scores assigned at the 48-month follow-up were 0, 3, 0, 1, and 9, respectively. These scores were assigned after conservative treatment and despite persistent symptoms. All patients in this subgroup had Group III tape functionality.
In two women with new-onset obstructive complications and proven tape displacement toward the urethra at the 48-month follow-up, splitting of the TVT had to be recommended after failure of medical treatment.
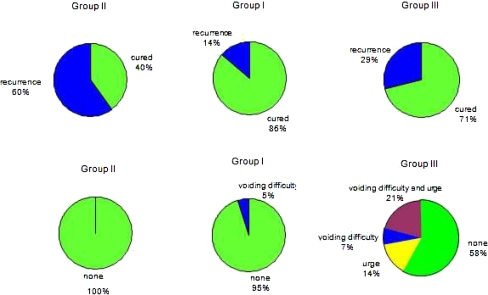
Figure 3 shows that a clear association exists between recurrence and complication rates at 48 months and tape functionality at the 6-month follow-up. Patients in whom tape functionality was rated to be optimal at the 6-month follow-up were found to have a 3.7-fold lower risk of recurrent SUI and a significantly lower risk of mid-term complications (p = 0.016) at 48 months.
Fig. 3.
Patients were assigned to the groups based on tape functionality at the 6-month postoperative follow-up. The figure shows cure and complication rates by group at 48 months
Discussion
Ultrasound is a simple and noninvasive imaging modality that provides detailed information on the position of the TVT relative to the urethra and changes in shape during straining [8–11].
Here, we, for the first time present mid-term data that show how these sonographically determined parameters affect the success of surgery and the complication rate. Note that the findings obtained with the TVT used in our patients may not be transferable to other suburethral slings made of different materials.
Our study has revealed specific ultrasound findings that can be obtained if the tape is either too close to the urethra or too far away and that these findings are associated with a lower cure rate and higher rate of complications. Outcome was best in women in whom US demonstrated the elastic sling to lie parallel to the urethra at rest and assume a transient C-shape during straining. We assume that this ultrasound finding suggests tension-free orthotopic positioning of the tape and that this position makes optimal use of the tape’s elasticity reserve, thereby ensuring sufficient compression of the urethra during Valsalva’s maneuver. Our data also indicate that if ultrasound shows this tape functionality at 6-month, the patient can expect mid-term cure and a low mid-term complication rate.
However, if the shape of the TVT remains unchanged during straining (Group II), women continue to experience involuntary loss of urine during stress. We attribute failure in these cases to the fact that the urethra is not sufficiently pressed into the prolene tape or not at all, which is not related to absolute tape–urethra distance alone but also to urethral mobility [10] (see Fig. 2). In these cases, the elasticity reserve of the tape is not fully exploited and tape position can be characterized as loose rather than tension-free.
Those cases where the sonographic findings show the tape to be C-shaped already at rest are associated with a higher rate of mid-term complications, confirming our earlier observations [9]. A permanent C-shape may suggest that the tape has been placed with too much tension intraoperatively, resulting in permanent folding at the midline. In this setting, the tape has no elasticity reserve and cannot change its shaping during straining.
Moreover, our results suggest that tape position significantly affects outcome, which is in disagreement with the results published by Dietz et al. in 2004 [12]. In their study, Dietz et al. used the symphysis pubis as reference and found the sonographically determined tape position to vary in a range from 30 mm above to 12.7 mm below the symphysis. However, the tape directly affects the urethra and we therefore think that the urethra is also the most suitable reference for determining the optimal TVT position. This may in part explain the different conclusions drawn by Dietz et al. Moreover, Dietz et al. do not take into account urethral length and its physiological variation. We think that urethral length is a central factor for optimal TVT placement since the procedure aims at supporting the mid-third of the urethra during straining [13]. Our findings suggest that optimal outcome is achieved if the TVT is placed at 40% to 70% of the urethral length. These results also support the pathophysiological insights of Ulmsten and Petros [14].
In another study published in 2003, Dietz et al. demonstrated gradual upward displacement of the TVT relative to the symphysis pubis over a 17-month period [15]. Our mid-term results show a significant change in the tape position relative to the length of the urethra toward the bladder neck as well as a significant shortening of the tape–urethra distance during the 48-month follow-up period. Both changes can be attributed to a gradual prolapse of the anterior compartment, resulting in a relative shift of the urethra. Concomitantly, the TVT is displaced ventrocranially.
Interestingly, the change in tape–urethra distance and tape position did not adversely affect patient satisfaction with outcome. The patients who were satisfied at the 6-month follow-up when the tape–urethra distance was 3 mm were also satisfied at 48 months despite a decrease in tape distance to 2 mm. The optimal tape–urethra distance decreased from 3–5 mm to 2.5 mm during the follow-up period of our study. In contrast, patients with a tape–urethra distance of 2 mm were already more dissatisfied at 6 months. These observations suggest that the range of optimal tape positions increases over time through habituation or adaptation of the urethral tissue to the TVT. Similar observations regarding complications were reported by Nilsson et al. in 2008, who did not find an increase in complications even after 11 years [16].
Predictors of mid-term outcome after suburethral sling procedures are still a matter of scientific debate [17–20]. The mid-term data we presented here suggest that sonographic evaluation of tape functionality at 6 months provides clues to mid-term outcome and complications. Optimal tape functionality at 6 months is a good predictor of mid-term therapeutic success. The pilot character of our study is a potential weakness, and our findings need to be confirmed in larger, prospective studies, which are already planned.
Summary
TVT insertion is a reliable and successful therapeutic option that ensures mid-term cure of stress urinary incontinence [16, 21]. The mid-term results presented here show that the position of the tape relative to the urethra as determined by introital ultrasound affects both outcome and the occurrence of complications. Ventrocranial displacement of the tape was observed to occur over time. Outcome was optimal in our study if the tape was position between 40% and 70% of the urethral length. Obstructive complications were significantly more common when the tape–urethra distance was <2 mm. The optimal range of the tape–urethra distance increased to 2–5 mm at the 48-month follow-up compared with the 6-month follow-up and is attributable to habituation. Tape functionality was identified as another crucial factor. Optimal tape functionality at 6-month follow-up was a good predictor of mid-term therapeutic success.
Acknowledgments
Conflicts of interest
None.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Footnotes
An erratum to this article can be found at http://dx.doi.org/10.1007/s00192-010-1256-4
References
- 1.Harms L, Emons G, Bader W, Lange R, Hilgers R, Viereck V. Funneling before and after anti-incontinence surgery—a prognostic indicator? Part 2: tension-free vaginal tape. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18:289–294. doi: 10.1007/s00192-006-0147-1. [DOI] [PubMed] [Google Scholar]
- 2.Masata J, Martan A, Svabik K, Drahoradova P, Pavlikova M. Ultrasound imaging of the lower urinary tract after successful tension-free vaginal tape (TVT) procedure. Ultrasound Obstet Gynecol. 2006;28:221–228. doi: 10.1002/uog.2692. [DOI] [PubMed] [Google Scholar]
- 3.Tunn R, Schaer G, Peschers U, Bader W, Gauruder A, Hanzal E, et al. Updated recommendations on ultrasonography in urogynecology. Int Urogynecol J Pelvic Floor Dysfunct. 2005;16:236–241. doi: 10.1007/s00192-004-1228-7. [DOI] [PubMed] [Google Scholar]
- 4.Viereck V, Bader W, Krauss T, Oppermann M, Gauruder-Burmester A, Hilgers R, et al. Intra-operative introital ultrasound in Burch colposuspension reduces post-operative complications. BJOG. 2005;112:791–796. doi: 10.1111/j.1471-0528.2005.00526.x. [DOI] [PubMed] [Google Scholar]
- 5.Skala C, Emons G, Krauss T, Hilgers R, Gauruder-Burmester A, Lange R, et al. Postoperative funneling after anti-incontinence surgery—a prognostic indicator? Part 1: colposuspension. Neurourol Urodyn. 2004;23:636–642. doi: 10.1002/nau.20056. [DOI] [PubMed] [Google Scholar]
- 6.Ulmsten U, Henriksson L, Johnson P, Varhos G. An ambulatory surgical procedure under local anesthesia for treatment of female urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 1996;7:81–85. doi: 10.1007/BF01902378. [DOI] [PubMed] [Google Scholar]
- 7.Ulmsten U, Johnson P, Rezapour M. A three-year follow up of tension free vaginal tape for surgical treatment of female stress urinary incontinence. Br J Obstet Gynaecol. 1999;106:345–350. doi: 10.1111/j.1471-0528.1999.tb08272.x. [DOI] [PubMed] [Google Scholar]
- 8.Viereck V, Pauer HU, Hesse O, Bader W, Tunn R, Lange R, et al. Urethral hypermobility after anti-incontinence surgery—a prognostic indicator? Int Urogynecol J Pelvic Floor Dysfunct. 2006;17:586–592. doi: 10.1007/s00192-006-0071-4. [DOI] [PubMed] [Google Scholar]
- 9.Kociszewski J, Rautenberg O, Perucchini D, Eberhard J, Geissbühler V, Hilgers R, et al. Tape functionality: sonographic tape characteristics and outcome after TVT incontinence surgery. Neurourol Urodyn. 2008;27:485–490. doi: 10.1002/nau.20556. [DOI] [PubMed] [Google Scholar]
- 10.Viereck V, Nebel M, Bader W, Harms L, Lange R, Hilgers R, et al. Role of bladder neck mobility and urethral closure pressure in predicting outcome of tension-free vaginal tape (TVT) procedure. Ultrasound Obstet Gynecol. 2006;28:214–220. doi: 10.1002/uog.2834. [DOI] [PubMed] [Google Scholar]
- 11.Sarnelli G, D’Urso L, Muto G. Tension-free vaginal tape (TVT) for the treatment of female stress urinary incontinence (SUI): evaluating perineal ultrasound (PU) findings in postoperative voiding obstructive complaints. Arch Ital Urol Androl. 2008;80:92–94. [PubMed] [Google Scholar]
- 12.Dietz HP, Mouritsen L, Ellis G, Wilson PD. How important is TVT location? Acta Obstet Gynecol Scand. 2004;83:904–908. doi: 10.1111/j.0001-6349.2004.00198.x. [DOI] [PubMed] [Google Scholar]
- 13.Ulmsten U. An introduction to tension-free vaginal tape (TVT)—a new surgical procedure for treatment of female urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2001;12:3–4. doi: 10.1007/s001920170086. [DOI] [PubMed] [Google Scholar]
- 14.Petros PE, Ulmsten UI. An integral theory of female urinary incontinence. Experimental and clinical considerations. Acta Obstet Gynecol Scand. 1990;153:7–31. doi: 10.1111/j.1600-0412.1990.tb08027.x. [DOI] [PubMed] [Google Scholar]
- 15.Dietz HP, Mouritsen L, Ellis G, Wilson PD. Does the tension-free vaginal tape stay where you put it? Am J Obstet Gynecol. 2003;188:950–953. doi: 10.1067/mob.2003.268. [DOI] [PubMed] [Google Scholar]
- 16.Nilsson CG, Palva K, Rezapour M, Falconer C. Eleven years prospective follow-up of the tension-free vaginal tape procedure for treatment of stress urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:1043–1047. doi: 10.1007/s00192-008-0666-z. [DOI] [PubMed] [Google Scholar]
- 17.Lee KS, Choo MS, Doo CK, Han DH, Lee YS, Kim JY, Kim WS, Jung HC. The long term (5-years) objective TVT success rate does not depend on predictive factors at multivariate analysis: a multicentre retrospective study. Eur Urol. 2008;53:176–182. doi: 10.1016/j.eururo.2007.08.033. [DOI] [PubMed] [Google Scholar]
- 18.Dawson T, Lawton V, Adams E, Richmond D. Factors predictive of post-TVT voiding dysfunction. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18:1297–1302. doi: 10.1007/s00192-007-0324-x. [DOI] [PubMed] [Google Scholar]
- 19.Takacs P, Medina CA. Tension-free vaginal tape: poor intraoperative cough test as a predictor of postoperative urinary retention. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18:1445–1447. doi: 10.1007/s00192-007-0364-2. [DOI] [PubMed] [Google Scholar]
- 20.Duckett J, Aggarwal I, Patil A, Vella M. Effect of tension-free vaginal tape position on the resolution of irritative bladder symptoms in women with mixed incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:237–239. doi: 10.1007/s00192-007-0409-6. [DOI] [PubMed] [Google Scholar]
- 21.Novara G, Ficarra V, Boscolo-Bento R, Secco S, Cavalleri S, Artibani W. Tension-free midurethral slings in the treatment of female stress urinary incontinence: a systematic review and meta-analysis of randomized controlled trials of effectiveness. Eur Urol. 2007;52:663–678. doi: 10.1016/j.eururo.2007.06.018. [DOI] [PubMed] [Google Scholar]