Abstract
Uterine fibroids are a very common finding in women of reproductive age. The majority of fibroids do not change their size during pregnancy, but one-third may grow in the first trimester. Although the data are conflicting and most women with fibroids have uneventful pregnancies, the weight of evidence in the literature suggests that uterine fibroids are associated with an increased rate of spontaneous miscarriage, preterm labor, placenta abruption, malpresentation, labor dystocia, cesarean delivery, and postpartum hemorrhage.
Key words: Fibroids, Miscarriage, Preterm labor, Placenta abruption, Fetal anomalies, Myomectomy, Uterine artery embolization
Fibroids (leiomyomas) are benign smooth muscle cell tumors of the uterus. Although they are extremely common, with an overall incidence of 40% to 60% by age 35 and 70% to 80% by age 50, the precise etiology of uterine fibroids remains unclear.1 The diagnosis of fibroids in pregnancy is neither simple nor straightforward. Only 42% of large fibroids (> 5 cm) and 12.5% of smaller fibroids (3–5 cm) can be diagnosed on physical examination.2 The ability of ultrasound to detect fibroids in pregnancy is even more limited (1.4%–2.7%) primarily due to the difficulty of differentiating fibroids from physiologic thickening of the myometrium.3–6 The prevalence of uterine fibroids during pregnancy is therefore likely underestimated. Reflecting the growing trend of delayed childbearing, the incidence of fibroids in older women undergoing treatment for infertility is reportedly 12% to 25%.7 Despite their growing prevalence, the relationship between uterine fibroids and adverse pregnancy outcome is not clearly understood.
Prospective studies using ultrasound to follow the size of uterine fibroids throughout pregnancy have shown that the majority of fibroids (60%–78%) do not demonstrate any significant change in volume during pregnancy.8,9 Of the 22% to 32% of fibroids that did increase in volume, the growth was limited almost exclusively to the first trimester, especially the first 10 weeks of gestation, with very little if any growth in the second and third trimesters. The mean increase in volume in this cohort was only 12% ± 6%, and the maximum growth was only 25% of the initial volume.8 Some studies have shown that small fibroids are just as likely to grow as large fibroids,8 whereas other studies have suggested that small and large fibroids (≥ 6 cm) have different growth patterns in the second trimester (small fibroids grow whereas large fibroids remain unchanged or decrease in size), but all decrease in size in the third trimester.9,10 The majority of fibroids show no change during the puerperium, although 7.8% will decrease in volume by up to 10%.8,9
Most fibroids are asymptomatic. However, severe localized abdominal pain can occur if a fibroid undergoes so-called “red degeneration,” torsion (seen most commonly with a pedunculated subserosal fibroid), or impaction (Figure 1). Pain is the most common complication of fibroids in pregnancy, and is seen most often in women with large fibroids (> 5 cm) during the second and third trimesters of pregnancy.3,11 In a study of 113 pregnant women, 9% of fibroids showed a heterogeneous echogenic pattern or cystic changes on ultrasound indicating the development of red degeneration. Of these women, 70% (7 of 10) had severe abdominal pain compared with 11.7% (12 of 103) of women with fibroids that showed no echogenic changes on ultrasound.10 Three main theories have been proposed to explain the severe pain associated with red degeneration. First, that rapid fibroid growth results in the tissue outgrowing its blood supply leading to tissue anoxia, necrosis, and infarction.11,12 Second, that the growing uterus results in a change in the architecture (kinking) of the blood supply to the fibroid leading to ischemia and necrosis even in the absence of fibroid growth.13 Third, that the pain results from the release of prostaglandins from cellular damage within the fibroid. This is supported by the observation that ibuprofen and other prostaglandin synthetase inhibitors effectively and rapidly control fibroid pain.11
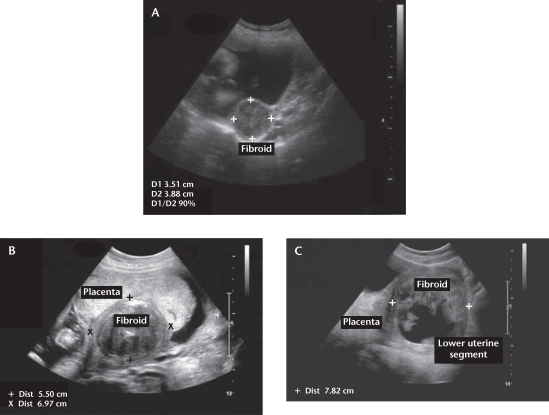
Figure 1.
Representative images of fibroids in pregnancy. (A) A 3.5 × 3.8 cm fibroid is evident in the posterior uterine wall. This small fibroid is unlikely to cause any pregnancy-related complications. (B) A 5.5 × 6.9 cm retroplacental fibroid is shown. This large fibroid is likely to interfere with placentation and uteroplacental blood flow due both to its size and location, which may present clinically as intrauterine growth restriction, placental abruption, or preeclampsia. (C) A 7.8 cm fibroid is evident in the lower uterine segment. Given its size and location, this large fibroid may interfere with engagement of the fetal head near term and the normal progress of labor. Moreover, the internal echogenic changes are consistent with “red degeneration,” and would likely account for the patient’s lower abdominal pain.
Effect of Fibroids on Pregnancy Outcome
Approximately 10% to 30% of women with uterine fibroids develop complications during pregnancy.11 However, these adverse pregnancy outcomes have been reported in incomplete settings with selection bias, small and differing populations, varying inclusion criteria, low occurrence of adverse outcomes, and inadequate confounding variables. As a result, these studies have reported inconsistent relationships between fibroids and adverse obstetric outcomes. Although decreased uterine distensibility or mechanical obstruction may explain some adverse outcomes, the precise mechanism by which uterine fibroids induce obstetric complications is not clear.4
Early Pregnancy
Miscarriage. Spontaneous miscarriage rates are greatly increased in pregnant women with fibroids compared with control subjects without fibroids (14% vs 7.6%, respectively).14 The weight of evidence in the literature suggests that the size of the fibroid does not affect the rate of miscarriage, but multiple fibroids may increase the miscarriage rate compared with the presence of a single fibroid only (23.6% vs 8.0%).14 The location of the fibroid may also be important. Early miscarriage is more common in women with fibroids located in the uterine corpus (body) than in the lower uterine segment10 and in women with intramural or submucosal fibroids.7,15–17 The mechanism by which fibroids cause spontaneous abortion is unclear. Increased uterine irritability and contractility, the compressive effect of fibroids, and compromise to the blood supply of the developing placenta and fetus have all been implicated.18
Bleeding in early pregnancy. The location of the fibroid determines the risk for bleeding. Bleeding in early pregnancy is significantly more common if the placenta implants close to the fibroid compared with pregnancies in which there is no contact between the placenta and fibroid (60% vs 9%, respectively).2,19
Late Pregnancy
Preterm labor and preterm premature rupture of membranes. Pregnant women with fibroids are significantly more likely to develop preterm labor and to deliver preterm than women without fibroids (16.1% vs 8.7% and 16% vs 10.8%, respectively; Table 1).7 Multiple fibroids and fibroids contacting the placenta appear to be independent risk factors for preterm labor.10,19 In contrast, fibroids do not appear to be a risk factor for preterm premature rupture of membranes (PPROM). Indeed, a recent systematic review suggests that fibroids are associated with a decreased risk of PPROM (Table 1).7
Table 1.
Cumulative Risk of Adverse Obstetric Outcomes in Pregnant Women With Fibroids
| Fibroids | No Fibroids | P Value | Unadjusted OR (95% CI) | |
| Cesarean delivery | 48.8% (2098/4322) | 13.3% (22,989/173,052) | <.001 | 3.7 (3.5–3.9) |
| Malpresentation | 13.0% (466/3585) | 4.5% (5864/130,932) | <.001 | 2.9 (2.6–3.2) |
| Labor dystocia | 7.5% (260/3471) | 3.1% (4703/148,778) | <.001 | 2.4 (2.1–2.7) |
| Postpartum hemorrhage | 2.5% (87/3535) | 1.4% (2130/153,631) | <.001 | 1.8 (1.4–2.2) |
| Peripartum hysterectomy | 3.3% (18/554) | 0.2% (27/18,000) | <.001 | 13.4 (9.3–19.3) |
| Retained placenta | 1.4% (15/1069) | 0.6% (839/134,685) | .001 | 2.3 (1.3–3.7) |
| Chorio or endometriosis | 8.7% (78/893) | 8.2% (2149/26,090) | .63 | 1.06 (0.8–1.3) |
| IUGR | 11.2% (112/961) | 8.6% (3575/41,630) | <.001 | 1.4 (1.1–1.7) |
| Preterm labor | 16.1% (116/721) | 8.7% (1577/18,187) | <.001 | 1.9 (1.5–2.3) |
| Preterm delivery | 16.0% (183/1145) | 10.8% (3433/31,770) | <.001 | 1.5 (1.3–1.7) |
| Placenta previa | 1.4% (50/3608) | 0.6% (924/154,334) | <.001 | 2.3 (1.7–3.1) |
| First-trimester bleeding | 4.7% (120/2550) | 7.6% (1193/15,732) | <.001 | 0.6 (0.5–0.7) |
| Abruption | 3.0% (115/4159) | 0.9% (517/60,474) | <.001 | 3.2 (2.6–4.0) |
| PPROM | 9.9% (123/1247) | 13.0% (7319/56,418) | .003 | 0.8 (0.6–0.9) |
| PPROM or PROM | 6.2% (217/3512) | 12.2% (7425/60.661) | <.001 | 0.5 (0.4–0.6) |
OR, odds ratio; CI, confidence interval; IUGR, intrauterine growth restriction; PPROM, preterm premature rupture of membranes; PROM, premature rupture of membranes.
Reprinted from American Journal of Obstetrics & Gynecology, Vol. 198, PC Klatsky et al, “Fibroids and reproductive outcomes: a systematic literature review from conception to delivery,” pp. 357–366, Copyright 2008, with permission from Elsevier.7
Placental abruption. Although reports are conflicting, pooled cumulative data suggest that the risk of placental abruption is increased 3-fold in women with fibroids (Table 1).7 Submucosal fibroids, retroplacental fibroids, and fibroid volumes > 200 cm3 are independent risk factors for placental abruption.20 One retrospective study reported placental abruption in 57% of women with retroplacental fibroids in contrast with 2.5% of women with fibroids located in alternate sites.3 One possible mechanism of placental abruption may be diminished blood flow to the fibroid and the adjacent tissues which results in partial ischemia and decidual necrosis in the placental tissues overlaying the leiomyoma.3
Placenta previa. The relationship between fibroids and placenta previa has been examined in only 2 studies, both of which suggest that the presence of fibroids is associated with a 2-fold increased risk of placenta previa even after adjusting for prior surgeries such as cesarean section or myomectomy (Table 1).4,7,21
Fetal growth restriction and fetal anomalies. Fetal growth does not appear to be affected by the presence of uterine fibroids. Although cumulative data and a population-based study suggested that women with fibroids are at slightly increased risk of delivering a growth-restricted infant, these results were not adjusted for maternal age or gestational age (Table 1).7,22 Rarely, large fibroids can compress and distort the intrauterine cavity leading to fetal deformities. A number of fetal anomalies have been reported in women with large submucosal fibroids, including dolichocephaly (lateral compression of the fetal skull), torticollis (abnormal twisting of the neck), and limb reduction defects.23–25
Labor and Delivery
Malpresentation, labor dystocia, and cesarean delivery. The risk of fetal malpresentation increases in women with fibroids compared with control subjects (13% vs 4.5%, respectively; Table 1).7,22 Large fibroids, multiple fibroids, and fibroids in the lower uterine segment have all been reported as independent risk factors for malpresentation.4,10,21,26
Numerous studies have shown that uterine fibroids are a risk factor for cesarean delivery.3,7,10,21,22,27–29 In a systematic review, women with fibroids were at a 3.7-fold increased risk of cesarean delivery (48.8% vs 13.3%, respectively).7 This is due in part to an increase in labor dystocia, which is increased 2-fold in pregnant women with fibroids (Table 1).7,22 Malpresentation, large fibroids, multiple fibroids, submucosal fibroids, and fibroids in the lower uterine segment are considered predisposing factors for cesarean delivery.5,10,21,27–29 Despite the increased risk of cesarean, the presence of uterine fibroids-even large fibroids (> 5 cm)-should not be regarded as a contraindication to a trial of labor.4,21,22
Postpartum hemorrhage. Reports on the association between fibroids and postpartum hemorrhage are conflicting.2,10,27,30–32 Pooled cumulative data suggest that postpartum hemorrhage is significantly more likely in women with fibroids compared with control subjects (2.5% vs 1.4%, respectively; Table 1).7 Fibroids may distort the uterine architecture and interfere with myometrial contractions leading to uterine atony and postpartum hemorrhage.33 This same mechanism may also explain why women with fibroids are at increased risk of puerperal hysterectomy.3,7,20
Retained placenta. One study reported that retained placenta was more common in women with fibroids, but only if the fibroid was located in the lower uterine segment.10 However, pooled cumulative data suggest that retained placenta is more common in all women with fibroids compared with control subjects, regardless of the location of the fibroid (1.4% vs 0.6%, respectively; Table 1).7
Uterine rupture after myomectomy. Uterine rupture after abdominal myomectomy is extremely rare.34–36 In a retrospective study of 120 women delivering at term following abdominal myomectomy in which the uterine cavity was not entered, there were no cases of uterine rupture reported.36 Whether the same is true also of laparoscopic myomectomy is not known, because there are numerous case reports and case series describing intrapartum uterine rupture after laparoscopic myomectomy.37–45 Recent data suggest that such uterine ruptures occur prior to the onset of labor at the site of the prior laparoscopic myomectomy.37–39,44 Fortunately, the absolute risk of uterine rupture following laparoscopic myomectomy remains low at 0.5% to 1%.41
Effect of Uterine Fibroids on Pregnancy Management
Pain Management
Fibroid pain during pregnancy is usually managed conservatively by bed rest, hydration, and analgesics. Prostaglandin synthase inhibitors (eg, nonsteroidal anti-inflammatory drugs) should be used with caution, especially prolonged use (> 48 hours) in the third trimester where it has been associated with both fetal and neonatal adverse effects, including premature closure of the fetal ductus arteriosus, pulmonary hypertension, necrotizing enterocolitis, intracranial hemorrhage, or oligohydramnios.46 Rarely, severe pain may necessitate additional pain medication (narcotic analgesia), epidural analgesia, or surgical management (myomectomy).47,48
Myomectomy. Prior to pregnancy, myomectomy can be considered in women with unexplained infertility or recurrent pregnancy loss,49,50 although whether such surgical interventions actually improve fertility rates and perinatal outcome remains unclear.
It is rare for fibroids to be treated surgically in the first half of pregnancy. If necessary, however, several studies have reported that antepartum myomectomy can be safely performed in the first and second trimester of pregnancy.12,20,48,51–55 Acceptable indications include intractable pain from a degenerating fibroid especially if it is subserosal or pedunculated, a large or rapidly growing fibroid, or any large fibroid (> 5 cm) located in the lower uterine segment. Obstetric and neonatal outcomes in women undergoing myomectomy in pregnancy are comparable with that in conservatively managed women,20,53 although women who had a myomectomy during pregnancy were far more likely to be delivered by cesarean due to concerns about uterine rupture (Table 2).12,20,51–55
Table 2.
Obstetric and Neonatal Outcomes in Normal Pregnant Women and Women With/Without Antepartum Myomectomy
| Pregnancies With Uterine Fibroids | |||
| Normal Pregnancies (n = 2463) | With Myomectomy (n = 18) | Without Myomectomy (n = 88) | |
| Age (y) | 29 (26–40) | 33 (28–40) | 35 (29–40) |
| Nulliparous | 1639 (66.5%) | 16 (83.3%) | 40 (45.4%) |
| Multiparous | 824 (33.5%) | 2 (16.7%) | 48 (54.6%) |
| Gestational age at diagnosis (wk) | - | 11 (8–17) | 13 (6–22) |
| Gestational age at myomectomy (wk) | - | 12 (10–19) | - |
| Abortion | 228 (9.3%) | 0 | 12 (13.6%) |
| Premature membranes rupture | 134 (5.4%) | 1 (5.6%) | 20 (22.7%) |
| IUGR | 61 (2.5%) | 1 (5.6%) | 4 (4.5%) |
| Preterm labor | 141 (5.7%) | 1 (5.6%) | 19 (21.6%) |
| Cesarean delivery | (16.3%) | (93.7%) | (34%) |
| Postcesarean hysterectomy | 3 (0.12%) | 0 | 4 (4.5%) |
| Apgar score | |||
| > 7 | 2447 (99.3%) | 18 (100%) | 87 (98.9%) |
| ≤ 7 | 16 (0.7%) | 0 | 1 (1.1%) |
| Weight: | |||
| > 2500 g | 2283 (92.7%) | 17 (94.4%) | 80 (90.9%) |
| ≤ 2500 g | 180 (7.3%) | 1 (5.6%) | 8 (9.1%) |
| Fibroids | |||
| Small (< 5 cm) | 0 | 45 | |
| Medium (5–10 cm) | 9 | 42 | |
| Large (> 10 cm) | 9 | 1 | |
IUGR, intrauterine growth restriction.
Reprinted with permission from Mollica G et al.53
Although not supported by all studies,56,57 most authorities agree that every effort should be made to avoid performing a myomectomy at the time of cesarean delivery due to the well-substantiated risk of severe hemorrhage requiring blood transfusion, uterine artery ligation, and/or puerperal hysterectomy.20,31,58,59 Myomectomy at the time of cesarean delivery should only be performed if unavoidable to facilitate safe delivery of the fetus or closure of the hysterotomy. Pedunculated subserosal fibroids can also be safely removed at the time of cesarean delivery without increasing the risk of hemorrhage.31
Uterine artery embolization. Bilateral uterine artery embolization (UAE) has long been performed by interventional radiologists to control postpartum hemorrhage. More recently, UAE has been used as an alternative procedure for treating large symptomatic fibroids in women who are not pregnant and, most importantly, do not desire future fertility.7 A recent prospective study reported that UAE performed immediately after cesarean delivery in women with uterine fibroids may be effective in decreasing postpartum blood loss and minimizing the risk of myomectomy or hysterectomy by inducing shrinkage of the fibroids.60 Although not recommended, there are several reports of successful and uneventful pregnancies after UAE for uterine fibroids.60–63
Conclusions
Uterine fibroids are a very common finding in women of reproductive age. The majority of fibroids do not change their size during pregnancy, but one-third may grow in the first trimester. Although the data are conflicting and most women with fibroids have uneventful pregnancies, the weight of evidence in the literature suggests that uterine fibroids are associated with an increased rate of spontaneous miscarriage, preterm labor, placenta abruption, malpresentation, labor dystocia, cesarean delivery, and postpartum hemorrhage. Pain is the most common complication of fibroids during pregnancy. The symptoms can usually be controlled by conservative treatment, but may require definitive surgical resection in rare instances. Some women with a previous myomectomy may need to be delivered by elective cesarean delivery prior to the onset of labor, particularly if the uterine cavity was entered. Women with a previous myomectomy should probably be delivered by cesarean prior to the onset of labor, particularly if the uterine cavity was entered. UAE is an alternative procedure to operative intervention for the treatment of symptomatic fibroids, but is absolutely contraindicated in pregnancy and in women desiring future fertility.
Main Points.
Uterine fibroids are very common in women of reproductive age. Most are asymptomatic; however, severe localized abdominal pain can occur if a fibroid undergoes so-called “red degeneration,” torsion, or impaction. Pain is the most common complication of fibroids in pregnancy, and is seen most often in women with fibroids > 5 cm during the second and third trimesters of pregnancy.
Approximately 10% to 30% of women with fibroids develop complications during pregnancy, although these adverse pregnancy outcomes have been reported in incomplete settings with selection bias, small and differing populations, varying inclusion criteria, low occurrence of adverse outcomes, and inadequate confounding variables.
In early pregnancy, spontaneous miscarriage rates are greatly increased in pregnant women with fibroids compared with those without fibroids (14% vs 7.6%, respectively), and bleeding is significantly more common if the placenta implants close to the fibroid. In late pregnancy, such complications include preterm labor, placental abruption, placenta previa, and fetal anomalies.
Pain is the most common complication of fibroids during pregnancy. The symptoms can usually be controlled by conservative treatment (bed rest, hydration, and analgesics), but may require definitive surgical resection in rare instances.
Prior to pregnancy, myomectomy can be considered in women with unexplained infertility or recurrent pregnancy loss, although whether this intervention improves fertility rates and perinatal outcome remains unclear. Uterine artery embolization is an alternative procedure to operative intervention, but is contraindicated in pregnancy and in women desiring future fertility.
References
- 1.Day Baird D, Dunson DB, Hill MC, et al. High cumulative incidence of uterine leiomyoma in black and white women: ultrasound evidence. Am J Obstet Gynecol. 2003;188:100–107. doi: 10.1067/mob.2003.99. [DOI] [PubMed] [Google Scholar]
- 2.Muram D, Gillieson M, Walters JH. Myomas of the uterus in pregnancy: ultrasonographic follow-up. Am J Obstet Gynecol. 1980;138:16–19. doi: 10.1016/0002-9378(80)90005-8. [DOI] [PubMed] [Google Scholar]
- 3.Burton CA, Grimes DA, March CM. Surgical management of leiomyomata during pregnancy. Obstet Gynecol. 1989;74:707–709. [PubMed] [Google Scholar]
- 4.Rice JP, Kay HH, Mahony BS. The clinical significance of uterine leiomyomas in pregnancy. Am J Obstet Gynecol. 1989;160:1212–1216. doi: 10.1016/0002-9378(89)90194-4. [DOI] [PubMed] [Google Scholar]
- 5.Qidwai GI, Caughey AB, Jacoby AF. Obstetric outcomes in women with sonographically identified uterine leiomyomata. Obstet Gynecol. 2006;107:376–382. doi: 10.1097/01.AOG.0000196806.25897.7c. [DOI] [PubMed] [Google Scholar]
- 6.Cooper NP, Okolo S. Fibroids in pregnancycommon but poorly understood. Obstet Gynecol Surv. 2005;60:132–138. doi: 10.1097/01.ogx.0000154688.02423.68. [DOI] [PubMed] [Google Scholar]
- 7.Klatsky PC, Tran ND, Caughey AB, Fujimoto VY. Fibroids and reproductive outcomes: a systematic literature review from conception to delivery. Am J Obstet Gynecol. 2008;198:357–366. doi: 10.1016/j.ajog.2007.12.039. [DOI] [PubMed] [Google Scholar]
- 8.Aharoni A, Reiter A, Golan D, et al. Patterns of growth of uterine leiomyomas during pregnancy. A prospective longitudinal study. Br J Obstet Gynaecol. 1988;95:510–513. doi: 10.1111/j.1471-0528.1988.tb12807.x. [DOI] [PubMed] [Google Scholar]
- 9.Rosati P, Exacoustòs C, Mancuso S. Longitudinal evaluation of uterine myoma growth during pregnancy. A sonographic study. J Ultrasound Med. 1992;11:511–515. doi: 10.7863/jum.1992.11.10.511. [DOI] [PubMed] [Google Scholar]
- 10.Lev-Toaff AS, Coleman BG, Arger PH, et al. Leiomyomas in pregnancy: sonographic study. Radiology. 1987;164:375–380. doi: 10.1148/radiology.164.2.3299488. [DOI] [PubMed] [Google Scholar]
- 11.Katz VL, Dotters DJ, Droegemueller W. Complications of uterine leiomyomas in pregnancy. Obstet Gynecol. 1989;73:593–596. [PubMed] [Google Scholar]
- 12.De Carolis S, Fatigante G, Ferrazzani S, et al. Uterine myomectomy in pregnant women. Fetal Diagn Ther. 2001;16:116–119. doi: 10.1159/000053893. [DOI] [PubMed] [Google Scholar]
- 13.Parker WH. Etiology, symptomatology, and diagnosis of uterine myomas. Fertil Steril. 2007;87:725–736. doi: 10.1016/j.fertnstert.2007.01.093. [DOI] [PubMed] [Google Scholar]
- 14.Benson CB, Chow JS, Chang-Lee W, et al. Outcome of pregnancies in women with uterine leiomyomas identified by sonography in the first trimester. J Clin Ultrasound. 2001;29:261–264. doi: 10.1002/jcu.1031. [DOI] [PubMed] [Google Scholar]
- 15.Goldenberg M, Sivan E, Sharabi Z, et al. Outcome of hysteroscopic resection of submucous myomas for infertility. Fertil Steril. 1995;64:714–716. doi: 10.1016/s0015-0282(16)57844-3. [DOI] [PubMed] [Google Scholar]
- 16.Casini ML, Rossi F, Agostini R, Unfer V. Effects of the position of fibroids on fertility. Gynecol Endocrinol. 2006;22:106–109. doi: 10.1080/09513590600604673. [DOI] [PubMed] [Google Scholar]
- 17.Bernard G, Darai E, Poncelet C, et al. Fertility after hysteroscopic myomectomy: effect of intramural myomas associated. Eur J Obstet Gynecol Reprod Biol. 2000;88:85–90. doi: 10.1016/s0301-2115(99)00123-2. [DOI] [PubMed] [Google Scholar]
- 18.Wallach EE, Vu KK. Myomata uteri and infertility. Obstet Gynecol Clin North Am. 1995;22:791–799. [PubMed] [Google Scholar]
- 19.Winer-Muram HT, Muram D, Gillieson MS. Uterine myomas in pregnancy. J Can Assoc Radiol. 1984;35:168–170. [PubMed] [Google Scholar]
- 20.Exacoustòs C, Rosati P. Ultrasound diagnosis of uterine myomas and complications in pregnancy. Obstet Gynecol. 1993;82:97–101. [PubMed] [Google Scholar]
- 21.Vergani P, Locatelli A, Ghidini A, et al. Large uterine leiomyomata and risk of cesarean delivery. Obstet Gynecol. 2007;109:410–414. doi: 10.1097/01.AOG.0000250470.78700.f0. [DOI] [PubMed] [Google Scholar]
- 22.Coronado GD, Marshall LM, Schwartz SM. Complications in pregnancy, labor, and delivery with uterine leiomyomas: a population-based study. Obstet Gynecol. 2000;95:764–769. doi: 10.1016/s0029-7844(99)00605-5. [DOI] [PubMed] [Google Scholar]
- 23.Chuang J, Tsai HW, Hwang JL. Fetal compression syndrome caused by myoma in pregnancy: a case report. Acta Obstet Gynecol Scand. 2001;80:472–473. [PubMed] [Google Scholar]
- 24.Graham JM , Jr, Miller ME, Stephan MJ, Smith DW. Limb reduction anomalies and early in utero limb compression. J Pediatr. 1980;96:1052–1056. doi: 10.1016/s0022-3476(80)80640-8. [DOI] [PubMed] [Google Scholar]
- 25.Romero R, Chervenak FA, DeVore G, et al. Fetal head deformation and congenital torticollis associated with a uterine tumor. Am J Obstet Gynecol. 1981;141:839–840. doi: 10.1016/0002-9378(81)90715-8. [DOI] [PubMed] [Google Scholar]
- 26.Phelan JP. Myomas and pregnancy. Obstet Gynecol Clin North Am. 1995;22:801–805. [PubMed] [Google Scholar]
- 27.Vergani P, Ghidini A, Strobelt N, et al. Do uterine leiomyomas influence pregnancy outcome? Am J Perinatol. 1994;11:356–358. doi: 10.1055/s-2007-994554. [DOI] [PubMed] [Google Scholar]
- 28.Aydeniz B, Wallwiener D, Kocer C, et al. Significance of myoma-induced complications in pregnancy. A comparative analysis of pregnancy course with and without myoma involvement [Article in German] Z Geburtshilfe Neonatol. 1998;202:154–158. [PubMed] [Google Scholar]
- 29.Donnez J, Pirard C, Smets M, et al. Unusual growth of a myoma during pregnancy. Fertil Steril. 2002;78:632–633. doi: 10.1016/s0015-0282(02)03297-1. [DOI] [PubMed] [Google Scholar]
- 30.Roberts WE, Fulp KS, Morrison JC, Martin JN., Jr The impact of leiomyomas on pregnancy. Aust N Z J Obstet Gynaecol. 1999;39:43–47. doi: 10.1111/j.1479-828x.1999.tb03442.x. [DOI] [PubMed] [Google Scholar]
- 31.Hasan F, Arumugam K, Sivanesaratnam V. Uterine leiomyomata in pregnancy. Int J Gynaecol Obstet. 1991;34:45–48. doi: 10.1016/0020-7292(91)90537-f. [DOI] [PubMed] [Google Scholar]
- 32.Ohkuchi A, Onagawa T, Usui R, et al. Effect of maternal age on blood loss during parturition: a retrospective multivariate analysis of 10,053 cases. J Perinat Med. 2003;31:209–215. doi: 10.1515/JPM.2003.028. [DOI] [PubMed] [Google Scholar]
- 33.Szamatowicz J, Laudanski T, Bulkszas B, Akerlund M. Fibromyomas and uterine contractions. Acta Obstet Gynecol Scand. 1997;76:973–976. doi: 10.3109/00016349709034912. [DOI] [PubMed] [Google Scholar]
- 34.Palerme GR, Friedman EA. Rupture of the gravid uterus in the third trimester. Am J Obstet Gynecol. 1966;94:571–576. doi: 10.1016/0002-9378(66)90064-0. [DOI] [PubMed] [Google Scholar]
- 35.Miller CE. Myomectomy. Comparison of open and laparoscopic techniques. Obstet Gynecol Clin North Am. 2000;27:407–420. doi: 10.1016/s0889-8545(00)80031-5. [DOI] [PubMed] [Google Scholar]
- 36.Brown AB, Chamberlain R, Te Linde RW. Myomectomy. Am J Obstet Gynecol. 1956;71:759–763. doi: 10.1016/0002-9378(56)90570-1. [DOI] [PubMed] [Google Scholar]
- 37.Levine D, Hulka CA, Ludmir J, et al. Placenta accreta: evaluation with color Doppler US, power Doppler US, and MR imaging. Radiology. 1997;205:773–776. doi: 10.1148/radiology.205.3.9393534. [DOI] [PubMed] [Google Scholar]
- 38.Harris WJ. Uterine dehiscence following laparoscopic myomectomy. Obstet Gynecol. 1992;80:545–546. [PubMed] [Google Scholar]
- 39.Dubuisson JB, Chavet X, Chapron C, et al. Uterine rupture during pregnancy after laparoscopic myomectomy. Hum Reprod. 1995;10:1475–1477. [PubMed] [Google Scholar]
- 40.Dubuisson JB, Fauconnier A, Deffarges JV, et al. Pregnancy outcome and deliveries following laparoscopic myomectomy. Hum Reprod. 2000;15:869–873. doi: 10.1093/humrep/15.4.869. [DOI] [PubMed] [Google Scholar]
- 41.Dubuisson JB, Fauconnier A, Babaki-Fard K, Chapron C. Laparoscopic myomectomy: a current view. Hum Reprod Update. 2000;6:588–594. doi: 10.1093/humupd/6.6.588. [DOI] [PubMed] [Google Scholar]
- 42.Asakura H, Oda T, Tsunoda Y, et al. A case report: change in fetal heart rate pattern on spontaneous uterine rupture at 35 weeks gestation after laparoscopically assisted myomectomy. J Nippon Med Sch. 2004;71:69–72. doi: 10.1272/jnms.71.69. [DOI] [PubMed] [Google Scholar]
- 43.Lieng M, Istre O, Langebrekke A. Uterine rupture after laparoscopic myomectomy. J Am Assoc Gynecol Laparosc. 2004;11:92–93. doi: 10.1016/s1074-3804(05)60020-5. [DOI] [PubMed] [Google Scholar]
- 44.Banas T, Klimek M, Fugiel A, Skotniczny K. Spontaneous uterine rupture at 35 weeks’ gestation, 3 years after laparoscopic myomectomy, without signs of fetal distress. J Obstet Gynaecol Res. 2005;31:527–530. doi: 10.1111/j.1447-0756.2005.00331.x. [DOI] [PubMed] [Google Scholar]
- 45.Grande N, Catalano GF, Ferrari S, Marana R. Spontaneous uterine rupture at 27 weeks of pregnancy after laparoscopic myomectomy. J Minim Invasive Gynecol. 2005;12:301. doi: 10.1016/j.jmig.2005.05.009. [DOI] [PubMed] [Google Scholar]
- 46.Norton ME, Merril J, Cooper BA, et al. Neonatal complications after administration of indomethacin for preterm labor. N Engl J Med. 1993;329:1602–1607. doi: 10.1056/NEJM199311253292202. [DOI] [PubMed] [Google Scholar]
- 47.Seki H, Takizawa Y, Sodemoto T. Epidural analgesia for painful myomas refractory to medical therapy during pregnancy. Int J Gynaecol Obstet. 2003;83:303–304. doi: 10.1016/s0020-7292(03)00207-8. [DOI] [PubMed] [Google Scholar]
- 48.Wittich AC, Salminen ER, Yancey MK, Markenson GR. Myomectomy during early pregnancy. Mil Med. 2000;165:162–164. [PubMed] [Google Scholar]
- 49.Li TC, Mortimer R, Cooke ID. Myomectomy: a retrospective study to examine reproductive performance before and after surgery. Hum Reprod. 1999;14:1735–1740. doi: 10.1093/humrep/14.7.1735. [DOI] [PubMed] [Google Scholar]
- 50.Surrey ES, Minjarez DA, Stevens JM, Schoolcraft WB. Effect of myomectomy on the outcome of assisted reproductive technologies. Fertil Steril. 2005;83:1473–1479. doi: 10.1016/j.fertnstert.2004.11.045. [DOI] [PubMed] [Google Scholar]
- 51.Glavind K, Palvio DH, Lauritsen JG. Uterine myoma in pregnancy. Acta Obstet Gynecol Scand. 1990;69:617–619. doi: 10.3109/00016349009028706. [DOI] [PubMed] [Google Scholar]
- 52.Michalas SP, Oreopoulou FV, Papageorgiou JS. Myomectomy during pregnancy and caesarean section. Hum Reprod. 1995;10:1869–1870. doi: 10.1093/oxfordjournals.humrep.a136195. [DOI] [PubMed] [Google Scholar]
- 53.Mollica G, Pittini L, Minganti E, et al. Elective uterine myomectomy in pregnant women. Clin Exp Obstet Gynecol. 1996;23:168–172. [PubMed] [Google Scholar]
- 54.Febo G, Tessarolo M, Leo L, et al. Surgical management of leiomyomata in pregnancy. Clin Exp Obstet Gynecol. 1997;24:76–78. [PubMed] [Google Scholar]
- 55.Celik C, Acar A, Ciçek N, et al. Can myomectomy be performed during pregnancy? Gynecol Obstet Invest. 2002;53:79–83. doi: 10.1159/000052997. [DOI] [PubMed] [Google Scholar]
- 56.Brown D, Fletcher HM, Myrie MO, Reid M. Caesarean myomectomy-a safe procedure. A retrospective case controlled study. J Obstet Gynaecol. 1999;19:139–141. doi: 10.1080/01443619965435. [DOI] [PubMed] [Google Scholar]
- 57.Kwawukume EY. Caesarean myomectomy. Afr J Reprod Health. 2002;6:38–43. [PubMed] [Google Scholar]
- 58.Ehigiegba AE, Ande AB, Ojobo SI. Myomectomy during cesarean section. Int J Gynaecol Obstet. 2001;75:21–25. doi: 10.1016/s0020-7292(01)00452-0. [DOI] [PubMed] [Google Scholar]
- 59.Buttram VC , Jr, Reiter RC. Uterine leiomyomata: etiology, symptomatology, and management. Fertil Steril. 1981;36:433–445. doi: 10.1016/s0015-0282(16)45789-4. [DOI] [PubMed] [Google Scholar]
- 60.Liu WM, Wang PH, Tang WL, et al. Uterine artery ligation for treatment of pregnant women with uterine leiomyomas who are undergoing cesarean section. Fertil Steril. 2006;86:423–428. doi: 10.1016/j.fertnstert.2006.01.027. [DOI] [PubMed] [Google Scholar]
- 61.Pron G, Mocarski E, Bennett J, et al. Pregnancy after uterine artery embolization for leiomyomata: the Ontario multicenter trial. Obstet Gynecol. 2005;105:67–76. doi: 10.1097/01.AOG.0000149156.07061.1f. [DOI] [PubMed] [Google Scholar]
- 62.Walker WJ, McDowell SJ. Pregnancy after uterine artery embolization for leiomyomata: a series of 56 completed pregnancies. Am J Obstet Gynecol. 2006;195:1266–1271. doi: 10.1016/j.ajog.2006.04.011. [DOI] [PubMed] [Google Scholar]
- 63.Goldberg J, Pereira L, Berghella V, et al. Pregnancy outcomes after treatment for fibromyomata: uterine artery embolization versus laparoscopic myomectomy. Am J Obstet Gynecol. 2004;191:18–21. doi: 10.1016/j.ajog.2004.01.046. [DOI] [PubMed] [Google Scholar]