Abstract
With the aging population in the United States, there has been a renewed interest in pessaries as a conservative alternative to surgical repair for pelvic organ prolapse (POP). They present a good option for patients who have not completed childbearing, do not desire surgery, or are poor surgical candidates. Long-term pessary use is a safe and effective option for patients with POP and stress urinary incontinence. Although serious side effects are infrequent, insertion and removal of most pessary types still pose a challenge for many patients. Pessary design should continue to improve, making its use a more attractive option.
Key words: Pessary, Pelvic organ prolapse, Incontinence
Pelvic organ prolapse (POP) is an important and common medical condition. By age 80, women in the United States have an 11% lifetime risk of undergoing surgery for prolapse or incontinence,1 with a 30% risk of reoperation over a period of 4 years.2 The United States Census Bureau projects that the number of women in America aged ≥ 65 years will double to over 40 million by the year 2030.3 With the aging United States population, there has been a renewed interest in the use of pessaries. A survey distributed to members of the American Urogynecologic Society indicated that 77% of respondents used pessaries as their first-line therapy for POP.4 As treatment options for prolapse and incontinence continue to evolve, the pessary remains a practical alternative.
The use of pessaries dates back as early as the 5th century BCE, during the time of Hippocrates, when hot oil stimulants, astringent-soaked plugs, and pomegranates were used to treat prolapse.5 There has been some advancement in pessaries over the centuries, which are now generally composed of silicone. Despite numerous technological breakthroughs in the medical field over recent decades, pessaries have remained essentially unchanged throughout the 20th century.6
Indications and Contraindications for Pessary Use
POP remains the most common indication for pessary use. Physicians generally offer pessaries as a first-line option for women with POP who desire nonsurgical management, future pregnancy, have early-stage prolapse, or are too frail for surgery. Additionally, pessaries are a valid option for patients with stress incontinence worsened by strenuous physical activity. In women presenting with pelvic pain, back pain, and pressure thought to be due to POP, pessaries offer an opportunity to simulate postsurgical conditions and aid in patient expectations regarding symptom reduction.
There are very few contraindications to pessary use, which allows clinicians to offer pessaries to almost all patients presenting with prolapse and incontinence. Pessaries should not be placed in patients with evidence of an active pelvic infection or severe ulceration, allergy to both silicone and latex, or those patients who are noncompliant and unlikely to follow up.
Types of Pessaries
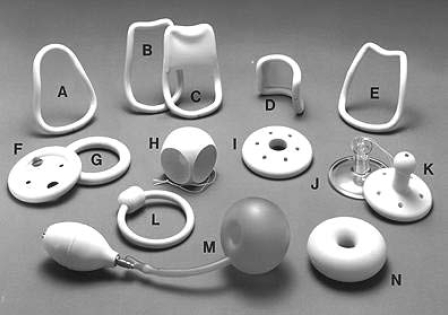
Pessaries are now generally made of an inert plastic or silicone to prevent odors and absorption of vaginal secretions. Silicone pessaries can be autoclaved. 7 There are currently many shapes and sizes of pessaries available to suit individual needs: supportive or space-occupying in nature, some designed to address urinary incontinence, all with their own advantages and disadvantages (Table 1). Support pessaries include the ring; the lever pessaries include the Smith, Hodge, Risser, and Gehrung. Spaceoccupying pessaries for more advanced prolapse consist of the Gellhorn, donut, and the cube. Sexual intercourse is not possible with a space-occupying pessary in place (Figure 1).
Table 1.
Pessary Types
| Support Pessaries | Stage I and II POP | Stage III and IV POP | Removal for Intercourse | In the Treatment of Incontinence | Advantages/Disadvantages |
| Ring | +++ | ++ | Not necessary | No | Easy insertion and removal |
| Lever (Smith, Hodge, Risser) | ++ | + | Not necessary | No | Historically used for retroverted uterus especially during pregnancy |
| Gehrung | ++ | + | Not necessary | No | Can mold to custom shape |
| Changes its position in the vagina | |||||
| Incontinence Ring | +++ | + | Not necessary | ++ | Migrates in vagina |
| Mar-land | ++ | + | Not necessary | ++ | |
| Space-Occupying Pessaries | |||||
| Gellhorn | + | +++ | Not possible | No | Difficult to remove |
| Donut | + | ++ | Not possible | No | Difficult to remove |
| Cube | + | ++ | +++ | No | Associated with malodorous discharge, vaginal erosions |
+++, highly recommended; ++, recommended; +, least recommended; POP, pelvic organ prolapse.
Figure 1.
Commonly used pessaries: (A) Smith; (B) Hodge; (C) Hodge with support; (D) Gehrung; (E) Risser; (F) Ring with diaphragm; (G) Ring; (H) Cube; (I) Shaatz; (J) Rigid Gellhorn; (K) Flexible Gellhorn; (L) Incontinence ring; (M) Inflatoball; (N) Donut. Image courtesy of CooperSurgical, Inc., Trumbull, CT.
Support Pessaries
Ring pessary. There are a few types of ring pessaries—those with and without support, and those with a knob for concomitant stress urinary incontinence. Ring pessaries are generally the first-line pessary for clinicians, due to ease of insertion and removal. These are generally chosen for earlier stage prolapse—stage I and II, but can be successful for all stages of POP. The ring is easy to insert by folding the ring in half and placing a small amount of lubricant on the tip of the pessary to aide in insertion. It is then placed into the vagina where it unfolds once above the pubic symphysis. For removal, the pessary is gently pulled and folded in half. A string can be attached to the ring to aid in insertion and removal. Patients can easily be taught to do this by themselves.
Gehrung. If a cystocele or rectocele accompanies the third-degree uterine prolapse, a Gehrung pessary—which rests along the anterior vaginal wall like a bridge—may be the most helpful. The Gehrung can be manually molded to fit each patient. The Gehrung can be difficult to insert.7
Mar-land. The flexible silicone Mar-land pessary and the Incontinence Dish can be used for minor degrees of prolapse and for the relief of stress incontinence. These pessaries decrease urethral hypermobility by compressing the urethra against the upper posterior portion of the symphysis pubis and elevating the bladder neck.
Space-Occupying Pessaries
Gellhorn. The Gellhorn is generally the pessary of choice for more advanced-stage prolapse, or in a patient who is no longer sexually active. Removal and insertion of this pessary is more difficult and therefore cannot be done by the patient. Most patients can be successfully managed with the 2.5-, 2.75-, and 3-inch size. This pessary has a concave portion attached to a stem that faces into the vagina. To insert the Gellhorn, the pessary is folded in half with the use of lubricant on the leading edge to ease insertion. Once the pessary is behind the pubic symphysis, it will expand and rest against the leading edge of prolapse, forming suction. To remove the Gellhorn, the knob is grasped, generally with the help of a ring forceps, while the concave end of the pessary is rotated to release the suction and the pessary is pulled downward, folded, and removed.
Donut. The donut pessary may be used to relieve the symptoms of a cystocele or rectocele as well as a secondor third-degree uterine prolapse. As it is not compressed easily, it is one of the hardest to insert and, in particular, to remove.
Cube. The cube pessary is flexible silicone7 and is an option in the case of stage III and IV prolapse. The pessary has a string on one end for ease of removal. To insert, the cube pessary is compressed and inserted into the vagina. The cube forms suction with the leading edge of prolapse and oftentimes vaginal secretions are trapped in the crevices of the pessary, leading to malodorous discharge; it is usually the pessary of last resort. This pessary should be removed on a nightly basis when possible.
Patient Evaluation and Pessary Placement
When a patient presents for treatment of POP or urinary incontinence, a thorough evaluation including a comprehensive history and symptoms assessment, expectations for treatment, obstetrical history, and surgical history must be performed. After a thorough examination, treatment options should be discussed. Once the decision to use a pessary is made, the clinician will choose the type of pessary based on severity of prolapse, presence or absence of a uterus, sexual activity, and concomitant stress urinary incontinence.
The patient should empty her bladder before pessary fitting. To begin fitting, the clinician can estimate the width of the mid-vagina and use this information to select the appropriate size pessary. The patient should be fitted with the largest size pessary that fits comfortably. The patient is examined in supine and standing position with and without Valsalva. The examiner should be able to comfortably fit a finger on either side of the pessary. If atrophy is present estrogen should also be prescribed, generally in cream, ring, or tablet form. The patient is then instructed to ambulate, sit on the toilet, and Valsalva to further assess comfort and appropriate pessary fit. Once the correct pessary type and size are chosen and successfully fitted in place, the patient should attempt to remove and reinsert the pessary on her own. This is commonly possible with the ring type. It is always reassuring if the patient can void with the pessary in place before she leaves the office. Patients should be advised that urine leakage may increase with prolapse reduction. Follow-up in 2 to 4 weeks is routine.
Although complications at the time of pessary fitting are extremely rare, a case of enterocele rupture and vaginal evisceration during pessary fitting was referred to our practice. The patient was successfully managed with transvaginal closure and concomitant colpocleisis.8
Factors Affecting Successful Fitting
Several studies have evaluated the success of pessary fitting, with success rates ranging from 41% to 74%.9–14 Success rates of up to 62% have been reported in patients with stage III and IV prolapse, indicating that pessaries are an excellent option even in a population with advanced POP.15 Studies varied considerably in the definition of successful fitting with variable lengths of follow-up—from 1 week to 36 months.10–14 In one study, up to 53% of women continued pessary use 3 years after successful pessary fitting. 10 Most protocols for pessary fitting were similar, with initial fitting using a ring pessary and transition to a space-occupying pessary if the ring pessary failed.9,10,13 On average, 2 to 3 fittings were required until the appropriate pessary was found.13,14,16,17
Factors associated with unsuccessful fitting include shortened vaginal length (< 6 cm), wide vaginal introitus (4 fingerbreadth or more),13 history of previous pelvic surgery,12,16 hysterectomy,17 or coexistence of stress urinary incontinence.14,18 Other factors associated with unsuccessful pessary fitting are obesity12 and younger age.10 Successful retention of a pessary is associated with hormone use16 and sexual activity.17 Anatomically, successful pessary fitting has been associated with a shorter perineal body at rest and a larger (more positive) point Aa measurement.14 In a study by Handa and Jones, continued pessary use was thought to improve and perhaps slow progression of prolapse.9
Pessary Maintenance and Follow-Up
Women who are able to remove and reinsert the pessary on their own will have the choice to remove it weekly, possibly even nightly, for cleaning. Patients who are sexually active may prefer to remove the pessary prior to intercourse. However, this is not mandatory for those using a support pessary. Follow-up visits for these patients may be every 6 months. There is, however, no consensus on the follow-up regimen for patients using pessaries. This strategy is likely to be different depending on the patient’s ability to remove and insert the pessary, the extent of prolapse, and the health of the vaginal epithelium. When the pessary cannot be removed regularly by the patient, visits at 2- to 3-month intervals have been widely adopted.
At each visit, the pessary is removed and cleaned. It is reinserted after an examination of the vagina for evidence of ulceration, bruising, and granulation tissue. The pessary is examined for discoloration, cracking, and deformation, and replaced as needed.
Complications Associated With Pessaries
Modern pessaries are composed of inert substances that require minimal care, regular removal, and inspection of vaginal epithelium.7 Common side effects include vaginal discharge and odor. Serious complications from pessaries are rare; however, vesicovaginal fistula,19,20 rectovaginal fistula,21 erosion, and subsequent impaction22 have all been reported. Neglected pessaries can be removed safely and resultant defects—including vesicovaginal fistulas and vaginal strictures—repaired.22 Interestingly, fibrosis due to neglected pessaries has been associated with prolapse regression.22 Serious complications can be thwarted with appropriate fitting, local estrogen, and regular, careful follow-up.
Symptom Improvement and Satisfaction
In a multicenter, randomized, controlled trial of 106 women with stage II or greater POP, there was significant symptom improvement as measured by the Prolapse and Urinary Scales of the Pelvic Floor Distress Inventory (PFDI).23 In a prospective cohort study of 64 women fitted with a pessary, subjects choosing to continue pessary use were found to have significantly lower PFDI scores and a greater decline in their scores than women who discontinued pessary use. The greatest difference was seen in the prolapse scale of the PFDI. In this study, a 50% improvement in PFDI score was associated with continued pessary use.24
Novel Ideas
In contrast to the pelvic reconstructive surgical arena, which is generating exciting innovative techniques every day, there has not been any major improvement in pessary design for decades. Ideally, a pessary should be inert, compact, and relatively inexpensive; its design should allow easy removal and insertion by the patient.
A prospective trial of the Colpexin™ sphere (Marina Medical, Sunrise, FL), a sphere-shaped intravaginal device for prolapse that was designed to simultaneously strengthen the pelvic floor, was conducted. The device, developed in Europe and used for over 10 years, offers ease of insertion and removal, less vaginal epithelial irritation, and the ability to perform concomitant pelvic floor strengthening. Eighty-one percent of subjects had improvement in at least 1 prolapsed vaginal compartment and a statistically significant improvement in pelvic floor strength at 16 weeks. However, possibly because the Colpexin sphere fell out during defecation in 72% of women, it has not been widely adopted by the practitioners and the patients.25
The uresta® (EastMed Inc., Halifax, Nova Scotia), a bell-shaped pessary with a handle at its base, was introduced and marketed for urinary incontinence. At 2 weeks, 66% of women were satisfied with the pessary. Subjects were followed for 12 months, and at completion of the study, 50% of subjects continued pessary use with statistically significant differences in scores on Urinary Distress Inventory and Incontinence Impact Questionnaire, pad weight, and number of leakage episodes.26
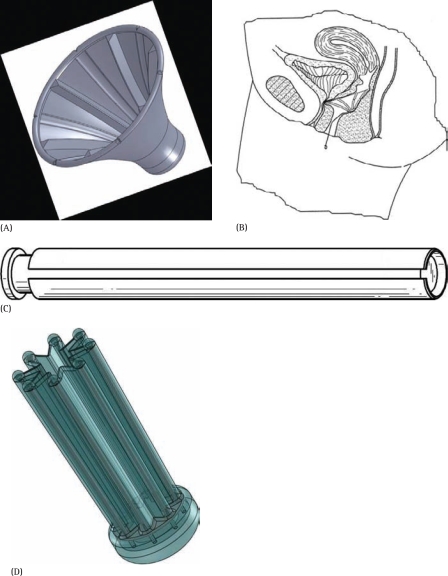
The difficulty with self-removal and insertion may be limiting more widespread use of the currently available pessaries. For the great majority of women with prolapse, pessaries equate to a commitment to lifelong office visits every 2 to 3 months. Even in the most experienced hands, pessary removal in the office may be difficult and painful. Many patients leave the office with small but painful abrasions of the vaginal introitus. This stressful experience, which has to be repeated a few times a year, may be the leading cause of pessary discontinuation and ultimate surgery. This urged the authors to reexamine the structure of the pessary, with the goal of developing a manually expandable pessary. This pessary would be designed to remain in a compact state during insertion and removal, with expansion inside the vagina only after insertion. If successfully developed, it will change how physicians approach conservative care of women with prolapse, and perhaps provide a more appealing alternative to surgery (Figure 2).
Figure 2.
A novel pessary idea: (A) Resembles an inverted umbrella with a string attached. Biased to stay open, it expands to support the vaginal walls (B). For removal, the patient inserts the string into a tubular introducer (C) and pulls gently to collapse the pessary (D) into the introducer. For insertion, the introducer loaded with the pessary is placed at the vaginal opening and the pessary is released by a plunger.
Conclusions
Pessaries offer a good noninvasive option in POP management for women unfit for surgery, those who have not yet completed childbearing, or those who do not desire surgical repair. There are few side effects associated with pessaries and only rare complications when patients are followed appropriately. Continued advancement in pessary composition and structure will allow improved satisfaction and utilization of pessaries. As the United States population continues to age, pessary use will likely increase.
Main Points.
Pelvic organ prolapse (POP) remains the most common indication for pessary use with few contraindications. Physicians utilize pessaries as a first-line treatment option for women who desire nonsurgical management or future pregnancy, have early-stage prolapse, or are too frail for surgery. They are also a valid option for those with stress incontinence worsened by strenuous physical activity.
There are many shapes and sizes of pessaries available to suit individual needs: supportive or space-occupying in nature, some designed to address urinary incontinence, all with their own advantages and disadvantages. Clinicians choose the type of pessary based on severity of prolapse, presence or absence of a uterus, sexual activity, and concomitant stress urinary incontinence.
Modern pessaries are composed of inert substances that require minimal care, regular removal, and inspection of vaginal epithelium. Common side effects include vaginal discharge and odor. Serious complications from pessaries are rare; however, vesicovaginal fistula, rectovaginal fistula, erosion, and subsequent impaction have all been reported.
Difficulty with self-removal and insertion may be limiting more widespread use of currently available pessaries.
Footnotes
Oz Harmanli, MD, is a partial owner of Oz Technologies, LLC (Springfield, MA), which is developing a new pessary.
References
- 1.Olsen AL, Smith VJ, Bergstrom JO, et al. Epidemiology of surgically managed pelvic organ prolapse and urinary incontinence. Obstet Gynecol. 1997;89:501–506. doi: 10.1016/S0029-7844(97)00058-6. [DOI] [PubMed] [Google Scholar]
- 2.Boyles SH, Weber AM, Meyn L. Procedures for pelvic organ prolapse and urinary incontinence in the United States, 1979–1997. Am J Obstet Gynecol. 2003;188:108–115. doi: 10.1067/mob.2003.101. [DOI] [PubMed] [Google Scholar]
- 3.US Census Bureau, authors. U.S. interim projections by age, sex, race, and Hispanic origin: 2000–2050. [Accessed October 2009]. http://www.census.gov/ipc/www/usinterimproj.
- 4.Cundiff GW, Weidner AC, Visco AC, et al. A survey of pessary use by members of the American Urogynecologic Society. Obstet Gynecol. 2000;95:931–935. doi: 10.1016/s0029-7844(00)00788-2. [DOI] [PubMed] [Google Scholar]
- 5.Shah SM, Sultan AH, Thakar R. The history and evolution of pessaries for pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17:170–175. doi: 10.1007/s00192-005-1313-6. [DOI] [PubMed] [Google Scholar]
- 6.Deger RD, Menzin AW, Mikuta JJ. The vaginal pessary: past and present. Postgraduate Obstet Gynecol. 1993;13:1–7. [Google Scholar]
- 7.Bash KL. Review of vaginal pessaries. Obstet Gynecol Surv. 2000;55:455–460. doi: 10.1097/00006254-200007000-00025. [DOI] [PubMed] [Google Scholar]
- 8.Rubin R, Jones KA, Harmanli OH. Vaginal evisceration during pessary fitting and its treatment with immediate colpocleisis. Obstet Gynecol. doi: 10.1097/AOG.0b013e3181da371d. In press. [DOI] [PubMed] [Google Scholar]
- 9.Handa VL, Jones M. Do pessaries prevent the progression of pelvic organ prolapse? Int Urogynecol J Pelvic Floor Dysfunct. 2002;13:349–351. doi: 10.1007/s001920200078. discussion 352. [DOI] [PubMed] [Google Scholar]
- 10.Wu V, Farrell SA, Basket TF, Flowerdew G. A simplified protocol for pessary management. Obstet Gynecol. 1997;90:990–994. doi: 10.1016/s0029-7844(97)00481-x. [DOI] [PubMed] [Google Scholar]
- 11.Cundiff GW, Amundsen CL, Bent AE, et al. The PESSRI study: symptom relief outcomes of a randomized crossover trial of the ring and Gellhorn pessaries. Am J Obstet Gynecol. 2007;196:e1–8. 405. doi: 10.1016/j.ajog.2007.02.018. [DOI] [PubMed] [Google Scholar]
- 12.Mutone MF, Terry C, Hale DS, Benson JT. Factors which influence the short-term success of pessary management of pelvic organ prolapse. Am J Obstet Gynecol. 2005;193:89–94. doi: 10.1016/j.ajog.2004.12.012. [DOI] [PubMed] [Google Scholar]
- 13.Clemons JL, Aguilar VC, Sokol ER, et al. Patient characteristics that are associated with continued pessary use versus surgery after 1 year. Am J Obstet Gynecol. 2004;191:159–164. doi: 10.1016/j.ajog.2004.04.048. [DOI] [PubMed] [Google Scholar]
- 14.Jones K, Yang L, Lowder JL, et al. Effect of pessary use on genital hiatus measurements in women with pelvic organ prolapse. Obstet Gynecol. 2008;112:630–636. doi: 10.1097/AOG.0b013e318181879f. [DOI] [PubMed] [Google Scholar]
- 15.Powers K, Lazarou G, Wang A, et al. Pessary use in advanced pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17:160–164. doi: 10.1007/s00192-005-1311-8. [DOI] [PubMed] [Google Scholar]
- 16.Donnelly MJ, Powell-Morgan S, Olsen AL, Nygaard IE. Vaginal pessaries for the management of stress and mixed urinary incontinence. Int Urogynecol J Pelvic Floor Dysfunct. 2004;15:302–307. doi: 10.1007/s00192-004-1163-7. [DOI] [PubMed] [Google Scholar]
- 17.Hanson LA, Schulz JA, Flood CG, et al. Vaginal pessaries in managing women with pelvic organ prolapse and urinary incontinence: patient characteristics and factors contributing to success. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17:155–159. doi: 10.1007/s00192-005-1362-x. [DOI] [PubMed] [Google Scholar]
- 18.Brincat C, Kenton K, Pat Fitzgerald M, Brubaker L. Sexual activity predicts continued pessary use. Am J Obstet Gynecol. 2004;191:198–200. doi: 10.1016/j.ajog.2004.03.083. [DOI] [PubMed] [Google Scholar]
- 19.Grody MH, Nyirjesy P, Chatwani A. Intravesical foreign body and vesicovaginal fistula: a rare complication of neglected pessary. Int Urogynecol J Pelvic Floor Dysfunct. 1999;10:407–408. doi: 10.1007/s001920050070. [DOI] [PubMed] [Google Scholar]
- 20.Esin S, Harmanli OH. Large vesicovaginal fistula in women with pelvic organ prolapse: the role of colpocleisis revisited. Int Urogynecol J Pelvic Floor Dysfunct. 2008;19:1711–1713. doi: 10.1007/s00192-008-0636-5. [DOI] [PubMed] [Google Scholar]
- 21.Russell JK. The dangerous vaginal pessary. BMJ. 1961;2:1595–1597. doi: 10.1136/bmj.2.5267.1595. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fernando RJ, Sultan AH, Thakar R, Jeyanthan K. Management of the neglected vaginal ring pessary. Int Urogynecol J Pelvic Floor Dysfunct. 2007;18:117–119. doi: 10.1007/s00192-006-0089-7. [DOI] [PubMed] [Google Scholar]
- 23.Barber MD, Walters MD, Cundiff GW PESSRI Trial Group, authors. Responsiveness of the Pelvic Floor Distress Inventory (PFDI) and Pelvic Floor Impact Questionnaire in women undergoing vaginal surgery and pessary treatment for pelvic organ prolapse. Am J Obstet Gynecol. 2006;194:1492–1498. doi: 10.1016/j.ajog.2006.01.076. [DOI] [PubMed] [Google Scholar]
- 24.Clemons JL, Aguilar VC, Tillinghast TA, et al. Patient satisfaction and changes in prolapse and urinary symptoms in women who were fitted successfully with a pessary for symptomatic pelvic organ prolapse. Am J Obstet Gynecol. 2004;190:1025–1029. doi: 10.1016/j.ajog.2003.10.711. [DOI] [PubMed] [Google Scholar]
- 25.Lukban JC, Aguirre OA, Davila GW, Sand PK. Safety and effectiveness of Colpexin Sphere in treatment of pelvic organ prolapse. Int Urogynecol J Pelvic Floor Dysfunct. 2006;17:449–454. doi: 10.1007/s00192-005-0033-2. [DOI] [PubMed] [Google Scholar]
- 26.Farrell SA, Baydock S, Amir B, Fanning C. Effectiveness of new self-positioning pessary for the management of urinary incontinence in women. Am Journal Obstet Gynecol. 2007;196:e1–e8. 474. doi: 10.1016/j.ajog.2006.11.038. [DOI] [PubMed] [Google Scholar]