Overweight and hypertension are major risk factors for cardiovascular morbidity and mortality;1,2 both are associated with decline in cognitive performance.3,4 We know that exercise is associated with modest reductions in blood pressure (BP) and that weight loss results in even larger, clinically important reductions in BP.5 What we did not know, prior to a report6 in this issue of Hypertension, is whether reductions in BP in association with diet and exercise (or diet alone) are associated with improvement in cognitive functioning. With publication of this paper, we have evidence supporting an association of diet and exercise and diet alone with a concordant decline in BP and improvement in cognition.6 These are important findings given a recent meta analysis of clinical trials of antihypertensive medications that indicated no improvements in cognitive performance associated with decline in BP.7
Two important issues are raised in this editorial comment: (1) are the Smith et al.6 findings important clinically; (2) where should this line of research go from here?
Employing a sample of 124 overweight and prehypertensive or moderately (Stage I) hypertensive adults, Smith and colleagues6 examined the association between two interventions and a control on cognitive performance for three groups: (1) diet alone (DASH-A), n= 38; (2) diet and exercise (DASH + weight management), n= 43; (3) usual care control (UC), n= 43. The UC group maintained their usual lifestyles.
After four months of treatment, participants randomly assigned to DASH-A improved with respect to Psychomotor Speed as compared to persons assigned to the UC group. Persons randomly assigned to DASH + WM improved on a composite of cognitive tests reflecting Executive Performance (e.g., planning, organization, shifting set) and Learning-Memory and also improved on Psychomotor Speed as compared to persons in the UC group. Power limitations precluded a comparison of DASH-A and DASH + WM groups. Importantly, the improvement was not remedial as none of the groups exhibited clinically important deficits in cognition prior to the first assessment.
No reductions in weight or BP were seen for the controls; however, relative to the controls, impressive reductions in average systolic and diastolic BP were observed for the DASH + WM group (14 mmHg and 10 mmHg) and the DASH-A group (10 mmHg and 8 mmHg). Weight decreased and peak VO2 max improved in the DASH + WM group as compared to the UC group. DASH-A participants did not differ from the UC group in VO2 max or weight. Clearly diet plus weight management, including exercise, was effective with regard to lowering BP.
Improvements in cognitive performance with DASH + WM were modest, approximately .08 SD units for an Executive Functioning/Learning-Memory composite. Participants in the DASH-A diet showed essentially no change. Participants in the DASH + WM diet performed at an average level prior to diet and exercise, but modest improvement is an important finding for two reasons: (1) hypertension-related cognitive deficits are cumulative over the life span;4 (2) modest decrements in cognition in mid-life increase the risk for dementia in late life.8 Improvements in cognition for any reason lead to increased cognitive reserve and prolong cognitive performance across the life span.
Some members of the Seventh Joint National Committee on the Prevention, Detection, Evaluation and Treatment of Hypertension (JNC-7) were initially concerned over premature treatment with antihypertensive medication.1 The Smith et al. paper6 offers support for supervised diet and exercise as an alternative treatment for mild hypertension with a positive outcome with respect to cognitive functioning. Moreover, the Smith et al. paper and its companion publication5,6 clearly specify the protocol for a demonstrably effective diet and weight management program.
Smith’s group advocates further work with elderly adults, patients on antihypertensive drugs, more severely hypertensive individuals, individuals with more severe cognitive impairment and in the preclinical phase of dementia. These are admirable and appropriate goals, but the number of exclusions required to select a sample with young, prehypertensive and stage I individuals in their initial investigation6 forewarns of many methodological challenges to the work proposed. We see the most practicable and useful next step as larger trial or trials, ideally including an exercise-only-group and specifically targeted at individuals diagnosed with prehypertension. With the exception of secondary hypertension and hypertension-related complications requiring prescribed medication or surgical intervention, it seems logical to argue that prehypertensive patients, especially those who are overweight, are most likely to profit from diet and exercise intervention as early in life as possible. Prehypertension begets hypertension at an alarming rate and heralds cardiovascular disease events many years later;1 therefore, an ounce of prevention is worth a pound of cure in terms of hypertension-related mortality and morbidity and preservation of cognitive ability over the lifespan. A search of PubMed for the years 2000–2010, using diet + exercise + prehypertension as descriptors, revealed only five studies of diet and exercise in preypertensive individuals; none involved cognition.
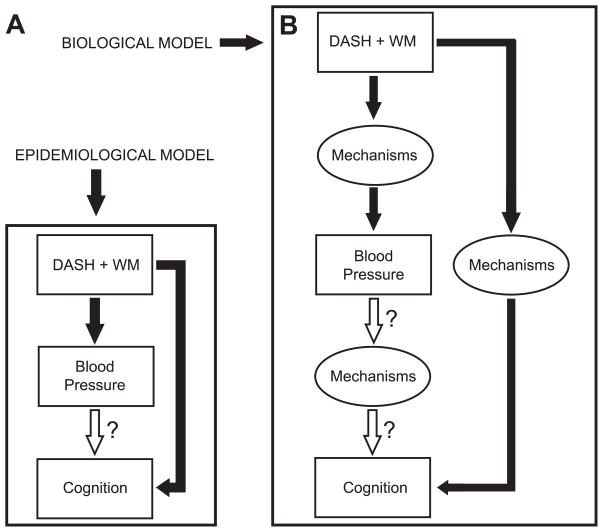
The unanswered question in the Smith et al. study6 is: what mechanisms, aside from VO2 max, intervene between diet and exercise, BP and cognition? Figure 1 illustrates models for the studies addressing this question using path analysis as the statistical approach. We have observable variables (rectangles) in Figure 1-a (epidemiological model), and observable and latent variables or unspecified mechanisms (ovals) in Figure 1-b (biological model). Arrows represent paths from one variable to another variable. As research progresses, the latent variables (labeled mechanisms) will be filled in with observable variables. VO2 max is a candidate variable based on the Smith et al. study.6 A review of the expanding literature9,10 on changes in brain structure and function triggered by chronic exercise in humans and animals is beyond this commentary, but it is noteworthy that many of these alterations occur in the hippocampus and other structures involved in executive performance, learning and memory. Insulin resistance, changes in cerebral blood flow, and lowered levels of noradrenalin in central and peripheral nervous system tissue, are just some among the important candidate mechanisms9,10 that may explain not only how diet and exercise may influence cognition, but also how blood pressure modulates their relationships as well as how BP directly affects cognition.
Figure 1.
Models for further research of the paths among observable (Figure 1-a) and observable and latent (Figure 1-b) variables.
Mediation regression analysis by Smith et al.6 indicated that adjustment for BP does attenuate the relations between Diet + Exercise and Cognition. Our personal view, reinforced by the Smith et al.6 and McGuinness et al.7 studies is as follows. Treatment does not directly mitigate the effects of hypertension on cognition, but affords protection against rise in BP over time and further brain injury. This is an arguable point subject to further investigation. Regardless of whether lowering of BP and improvement in cognition are simply coincidental phenomena, the Smith et al.6 data strongly encourage consideration of diet combined with exercise as means to protect and better serve our patients.
Acknowledgments
We acknowledge Penelope K. Elias, PhD (University of Maine) for editorial suggestions and Gregory A. Dore, BA (University of Maine) for technical work on the figures.
Sources of Funding
Preparation of this editorial was supported by grants R01-HL067358 and R01-HL081290 from the National Heart, Lung and Blood Institute and 1P01-AG17553. National Institutes of Health (NIH), USA. The opinions and conclusions reached are the opinions of the authors and have not been approved by the NIH.
Footnotes
Disclosures
Merrill F. Elias is a salaried principal investigator on research grant R01-HL081290 from the National Heart Lung and Blood Institute, National Institutes of Health (NIH), USA, and has received compensation from NIH for research grant reviews, and royalties from Taylor and Francis publishing company for book chapter and editorial responsibilities.
Amanda L. Goodell has no conflicts of interest or disclosures.
Contributor Information
Merrill F. Elias, Email: MFElias@aol.com.
Amanda L. Goodell, Email: amanda.goodell@umit.maine.edu.
References
- 1.Chobanian AV. Prehypertension revisited. Hypertension. 2006;48:812–814. doi: 10.1161/01.HYP.0000241684.29799.14. [DOI] [PubMed] [Google Scholar]
- 2.Franks PW, Hanson RL, Knowler WC, Sievers ML, Bennett PH, Looker HC. Childhood obesity, other cardiovascular risk factors, and premature death. N Engl J Med. 2010;362:485–493. doi: 10.1056/NEJMoa0904130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Dore GA, Elias MF, Robbins MA, Budge MM, Elias PK. Relation between central adiposity and cognitive function in the Maine-Syracuse Study: Attenuation by physical activity. Ann Behav Med. 2008;35:341–350. doi: 10.1007/s12160-008-9038-7. [DOI] [PubMed] [Google Scholar]
- 4.Elias PK, Elias MF, Robbins MA, Budge MM. Blood pressure-related cognitive decline: Does age make a difference? Hypertension. 2004;44:631–636. doi: 10.1161/01.HYP.0000145858.07252.99. [DOI] [PubMed] [Google Scholar]
- 5.Blumenthal JA, Babyak MA, Hinderliter A, Watkins LL, Craighead L, Lin PH, Caccia C, Johnson J, Waugh R, Sherwood A. Effects of the DASH diet alone and in combination with exercise and weight loss on blood pressure and cardiovascular biomarkers in men and women with high blood pressure: The ENCORE Study. Arch Int Med. 2010;170:126–135. doi: 10.1001/archinternmed.2009.470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Smith PJ, Blumenthal JA, Babyak MA, Craighead L, Welsh-Bohmer KA, Browndyke JN, Strauman TA, Sherwood A. The effects of DASH diet, exercise, and caloric restriction on neurocognition in overweight adults with high blood pressure. Hypertension. 2010 doi: 10.1161/HYPERTENSIONAHA.109.146795. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.McGuinness B, Todd S, Passmore AP, Bullock R. Systematic review: blood pressure lowering in patients without prior cerebrovascular disease for prevention of cognitive impairment and dementia. J Neurol Neurosurg Psychiatry. 2008;79:4–5. doi: 10.1136/jnnp.2007.118505. [DOI] [PubMed] [Google Scholar]
- 8.Elias MF, Beiser A, Wolf PA, Au R, White RF, D’Agostino RB. The preclinical phase of Alzheimer’s disease: A 22-year prospective study of the Framingham cohort. Arch Neurol. 2000;57:808–813. doi: 10.1001/archneur.57.6.808. [DOI] [PubMed] [Google Scholar]
- 9.Hillman CH, Erickson KI, Kramer AF. Be smart, exercise your heart: exercise effects on brain and cognition. Nat Rev Neurosci. 2008;9:58–65. doi: 10.1038/nrn2298. [DOI] [PubMed] [Google Scholar]
- 10.Dishman RK, Berthoud HR, Booth FW, Cotman CW, Edgerton VR, Fleshner MR, Gandevia SC, Gomez-Pinilla F, Greenwood BN, Hillman CH, Kramer AF, Levin BE, Moran TH, Russo-Neustadt AA, Salamone JD, Van Hoomissen JD, Wade CE, York DA, Zigmond MJ. Neurobioloy of exercise. Obesity. 2006;14:345–356. doi: 10.1038/oby.2006.46. [DOI] [PubMed] [Google Scholar]