Abstract
Previous pharmacodynamic studies using in vivo candidiasis models have demonstrated that the 24-h area under the concentration-time curve (AUC)/MIC is a good descriptor of the echinocandin exposure-response relationship. Further studies investigating the 24-h AUC/MIC target for a stasis endpoint identified free-drug 24-h AUC/MIC against Candida albicans and were similar for two echinocandins, anidulafungin and micafungin. The current studies expand investigation of a third echinocandin (caspofungin) and compare the pharmacodynamic target among C. albicans, Candida glabrata, and Candida parapsilosis. Treatment studies were conducted with six C. albicans, nine C. glabrata, and 15 C. parapsilosis strains with various MICs (anidulafungin, 0.015 to 4.0 μg/ml; caspofungin, 0.03 to 4.0 μg/ml; and micafungin, 0.008 to 1.0 μg/ml). Efficacy was closely tied to MIC and the 24-h AUC/MIC. Therapy against C. parapsilosis required more of each echinocandin on a mg/kg basis. Caspofungin required less drug on a mg/kg basis for efficacy against all of the organisms than did the other two drugs. However, the 24-h AUC/MIC targets were similar among the echinocandins when free drug concentrations were considered, suggesting the relevance of protein binding. The targets for C. parapsilosis (mean, 7) and C. glabrata (mean, 7) were significantly lower than those for C. albicans (mean, 20) for each echinocandin. The results suggest that current susceptibility breakpoints and the consideration of organism species in these determinations should be reexplored.
Experimental antifungal pharmacodynamic investigations have been important for the design of optimal dosing strategies and the development of susceptibility breakpoints (1, 2, 5, 17). Several studies have begun to focus on the most recently approved antifungal drug class, the echinocandins (9, 11, 14, 21, 22, 34, 57). Results of these pharmacodynamic experiments have demonstrated concentration-dependent killing and have shown prolonged postantifungal effects. Both concentration-associated pharmacodynamic indices, the 24-h area under the concentration-time curve (AUC)/MIC and the Cmax/MIC, have been linked to treatment efficacy. More recently, investigations have attempted to identify the pharmacodynamic target or the drug exposure relative to the MIC needed for treatment efficacy (9, 14). Several observations were made in studies with two echinocandins in experimental models of disseminated Candida albicans. The pharmacodynamic targets were similar between the two echinocandins as long as free drug concentrations were considered, suggesting the relevance of protein binding. However, only a few “high” MIC organisms were available for investigation at the time, and the studies did not include the species demonstrating the least susceptibility in vitro, Candida parapsilosis. The present studies expand evaluation to include all three FDA-approved echinocandins as well as in depth exploration of the pharmacodynamic target for C. parapsilosis. The results from these experiments provide pharmacodynamic support for current clinical dosing regimens and suggest that current susceptibility breakpoints based upon Candida species should be reconsidered.
MATERIALS AND METHODS
Organisms.
Thirty clinical Candida isolates were used for the in vivo treatment studies, including six C. albicans, nine Candida glabrata, and 15 C. parapsilosis strains (Table 1). The C. parapsilosis group was further characterized into C. parapsilosis, Candida metapsilosis, and Candida orthopsilosis, as previously described (33, 55). The organisms were chosen to include isolates with relatively similar degrees of fitness in the animal model, as determined by the amount of growth in the kidneys of untreated animals over 96 h. We also attempted to choose strains with various echinocandin susceptibilities.
TABLE 1.
In vitro susceptibility of study organisms (C. albicans, C. glabrata, and C. parapsilosis) against anidulafungin, caspofungin, and micafungin
| Organisma | MIC (μg/ml) |
||
|---|---|---|---|
| Anidulafungin | Caspofungin | Micafungin | |
| CA 98-17 | 0.03 | 0.12 | 0.03 |
| CA 98-210 | 0.015 | 0.02 | 0.016 |
| CA 580 | 0.015 | 0.03 | 0.008 |
| CA 98-234 | 0.015 | 0.03 | ND |
| CA K1 | 0.015 | 0.03 | 0.016 |
| CA 570 | 0.03 | 0.12 | 0.02 |
| CG 5592 | 0.06 | 0.03 | 0.016 |
| CG 513 | 0.06 | 0.03 | 0.016 |
| CG 33609 | 0.03 | 0.03 | 0.016 |
| CG 32930 | 0.06 | 0.03 | 0.008 |
| CG 33616 | 1 | 0.25 | 0.25 |
| CG 35315 | 0.25 | 0.12 | 0.06 |
| CG 5376 | 0.03 | 0.03 | 0.008 |
| CG 34341 | 0.12 | 0.25 | 0.06 |
| CG 37661 | 2 | ND | 0.25 |
| CP-M 20463.02 | 0.25 | 0.06 | 0.12 |
| CP 20450.096 | 1 | 0.50 | 0.25 |
| CP 20477.078 | 2 | 0.50 | 0.50 |
| CP 20385.079 | 1 | 0.50 | 0.50 |
| CP 20477.048 | 2 | 4.00 | 0.50 |
| CP 20423.072 | 1 | 0.12 | 0.25 |
| CP 20423.078 | 1 | 0.25 | 0.50 |
| CP 20562.03 | 1 | 0.25 | 0.50 |
| CP 20553.009 | 2 | 1.00 | 1.00 |
| CP 20489.085 | 1 | 0.25 | 0.12 |
| CP 20511.092 | 1 | 0.06 | 0.25 |
| CP 20557.012 | 0.5 | 0.12 | 0.25 |
| CP-O 20577.055 | 0.5 | 0.06 | 0.25 |
| CP 20519.069 | 4 | 1.00 | 1.00 |
| CP 20435.057 | 1 | 0.06 | 0.50 |
CA, C. albicans; CG, C. glabrata; CP, C. parapsilosis; CP-M, C. metapsilosis; CP-O, C. orthopsilosis.
Antifungal agents.
Anidulafungin, caspofungin, and micafungin were obtained from Pfizer, Merck, and Astellas, respectively, for in vitro susceptibility testing. Stock solutions were prepared for susceptibility testing as described in the Clinical Laboratory Standards Institute (CLSI) standard M27-A3 (37). The same drugs were obtained from the University of Wisconsin Pharmacy for in vivo treatment studies and prepared according to the manufacturers’ instructions.
In vitro susceptibility testing.
All isolates were tested in accordance with the standards in the CLSI document M27-A3, using RPMI 1640 medium, an inoculum of from 0.5 × 103 to 2.5 × 103 cells/ml, and incubation at 35°C (37). MICs were determined visually after 24 h of incubation as the lowest concentration of drug that caused a significant diminution (≥50%) of growth of control levels. Studies were performed on three separate occasions in duplicate. Final results were expressed as the mean of these results. Quality control was performed on each day of testing by using CLSI-recommended reference strains Candida krusei ATCC 6258 and C. parapsilosis ATCC 22019.
Animals.
Six-week-old ICR Swiss specific-pathogen-free female mice weighing 23 to 27 g purchased from Harlan Sprague-Dawley were used for all studies. Animals were maintained in accordance with the American Association for Accreditation of Laboratory Care criteria. Animal studies were approved by the University of Wisconsin Animal Care Committee.
Infection model.
A neutropenic, murine, disseminated candidiasis model was used for the treatment studies. Mice were made neutropenic (polymorphonuclear cells, <100 mm3) by injecting cyclophosphamide subcutaneously 4 days before infection (150 mg/kg of body weight), 1 day before infection (100 mg/kg), and 2 days after infection (100 mg/kg). Previous investigations have demonstrated that this regimen produces neutropenia throughout the 96-h study period (4). Organisms were subcultured on Sabouraud dextrose agar (SDA) 24 h prior to infection. The inoculum was prepared by placing three to five colonies into 5 ml of sterile 0.15 M NaCl warmed to 35°C. The final inoculum was adjusted to a 0.6 transmittance at 530 nm. Fungal counts of the inoculum determined by viable counts on SDA were 6.25 ± 0.33 log10 CFU/ml.
Disseminated infection with the Candida organisms was produced by injection of 0.1 ml of the inoculum via the lateral tail vein 2 h prior to the start of antifungal therapy. At the end of the study period, animals were sacrificed by CO2 asphyxiation. After sacrifice, the kidneys of each mouse were immediately removed and placed in 0.15 M NaCl at 4°C. The organs were homogenized and then serially diluted 1:10. Aliquots were plated onto SDA for viable fungal colony counts after incubation for 24 h at 35°C. The lower limit of detection was 100 CFU/ml. The results were expressed as the mean number of CFU/kidneys for three mice.
Pharmacokinetic studies and analysis.
The single-dose pharmacokinetics of anidulafungin and micafungin used for these studies were previously performed, analyzed, and published in this journal (9, 14). Identical experiments were undertaken using this animal model with caspofungin. Briefly, studies were performed in infected neutropenic mice by using the infection model described above. Mice were administered single doses of the echinocandin drugs by the intraperitoneal route at doses of 80, 20, and 5 mg/kg in a 0.2-ml volume. Blood samples were collected from groups of three mice per time point at each of eight time points. Serum was stored at −80°C until drug assay. Anidulafungin and micafungin concentrations were analyzed by gas chromatography-mass spectrometry (GC/MS) and microbiologic assay as previously described (8, 9). Caspofungin was analyzed using the same assay as that used for micafungin. C. albicans K1 was used as the assay organism. The lower limit of detection of the caspofungin in the microbiologic assay was 0.10 μg/ml. The lower limit of quantitation was 0.4 μg/ml. The mean intraday variation for the caspofungin assay was <5%. The assay performances for anidulafungin and micafungin were previously reported (8, 9).
A noncompartmental model was used in the pharmacokinetic analysis (WinNonlin, Pharsight Corporation, Cary, NC). Pharmacokinetic parameters, including elimination half-life and concentration at time zero (C0) were calculated via nonlinear least-squares techniques. The AUC was calculated by the trapezoidal rule. For treatment doses in which no kinetics were determined, the pharmacokinetic index was estimated by extrapolation from higher and lower dose levels and interpolation for dose levels within the dose range studied. Protein binding for each echinocandin was based upon previous reports of binding in mice and humans (anidulafungin, 99%; caspofungin, 97%; and micafungin, 99.75%) (9, 14, 24, 26).
Pharmacodynamic target determination.
The thirty Candida strains described above were used for in vivo treatment studies with each of the three echinocandins. Infection in neutropenic mice was produced as described above. Dosing regimens were chosen to vary the magnitude of the 24-h AUC/MIC index and to attempt to produce a range of efficacy that included no effect to maximal effect. Four to six (all but four treatment studies used six) dose levels that varied from 0.078 to 160 mg/kg were administered in a 0.2-ml volume by the intraperitoneal route. The antifungals were given every 24 h for a 4-day period. Groups of three mice were used for each dosing regimen. At the end of the treatment period, mice were euthanized, and the kidneys were immediately processed for determination of the number of CFU as described above.
The dose response results were analyzed using a sigmoid dose-effect model. To compare the in vivo potencies of each drug against the various Candida strains and species, we utilized the dose level required to produce a net static effect (no change in organism burden compared to the start of therapy) and a 1 log kill (relative to burden at the start of therapy) as previously described (9). The echinocandin exposure associated with each treatment endpoint was calculated from the following equation: log10 D = log10 (E/Emax − E)/N + log10 ED50, where D is the drug dose, E is the control growth in untreated animals, Emax is the maximal effect, N is the slope of the dose-response relationship, and ED50 is the dose needed to achieve 50% of the maximal effect. Emax was constrained when the true Emax was not achieved. The significance of differences among for the dose levels (static dose and 1 log kill) among echinocandins and Candida species was determined by using analysis of variance (ANOVA) and pairwise comparisons. One-way ANOVA and the Holm-Sidak method were used for normally distributed data. ANOVA on ranks and Dunn's method were used for nonparametric analysis when the data were not normally distributed.
RESULTS
In vitro susceptibility testing.
The MICs of anidulafungin, caspofungin, and micafungin for the Candida strains are shown in Table 1. The MICs for the entire group varied 500-fold (range, 0.008 to 4.0 μg/ml). The ranges were relatively similar among the three echinocandins (anidulafungin, 0.015 to 4.0 μg/ml; caspofungin, 0.03 to 4.0 μg/ml; micafungin, 0.008 to 1.0 μg/ml). The C. parapsilosis group exhibited the highest MICs among the Candida species. For the group of C. parapsilosis, the anidulafungin MICs were 2- to 3-fold higher than for caspofungin or micafungin (mean MICs, anidulafungin, 1.28 μg/ml; caspofungin, 0.58 μg/ml; micafungin, 0.43 μg/ml; P = 0.01). The MICs were lower, and the range was smallest for the C. albicans group (0.008 to 0.12 μg/ml). This pattern of MIC results is similar to that reported in larger surveillance studies.
Pharmacokinetics.
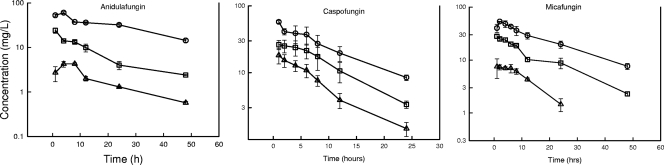
The pharmacokinetics of anidulafungin and micafungin in this in vivo model have been previously published (9, 14). The pharmacokinetic parameters following single intraperitoneal doses of 5, 20, and 80 mg/kg are reported in Table 2. The serum concentrations for each compound are shown in Fig. 1. Peak levels were observed by 1 to 4 h with each of the drugs. The elimination half-lives in mouse serum ranged from 7.9 to 24 h and were relatively similar for caspofungin and micafungin and slightly longer for anidulafungin. The AUC0-∞ values ranged from 96 to 1,975 μg·h/ml for anidulafungin, 164 to 667 μg·h/ml for caspofungin, and 135 to 1,400 μg·h/ml for micafungin. The AUC values were linear (R2 = 0.98 to 0.99) over the dose range studied.
TABLE 2.
Serum pharmacokinetic parameters for anidulafungin, caspofungin, and micafungin in mice
| Drug | Dose (mg/kg) | Cmax (μg/ml) | AUC (mg·h/liter) | t1/2 (h) | Protein binding (%) |
|---|---|---|---|---|---|
| Anidulafungin | 80 | 60 | 1975 | 24 | 99 |
| 20 | 24 | 382 | 14.7 | ||
| 5 | 4.3 | 96 | 14.8 | ||
| Caspofungin | 80 | 58 | 667 | 8.75 | 97 |
| 20 | 26 | 345 | 6.87 | ||
| 5 | 18 | 164 | 6.18 | ||
| Micafungin | 80 | 53 | 1400 | 16 | 99.75 |
| 20 | 28 | 520 | 13 | ||
| 5 | 7 | 138 | 7.50 |
FIG. 1.
Single-dose serum pharmacokinetics of anidulafungin, caspofungin, and micafungin following intraperitoneal doses of 5, 20, and 80 mg/kg. Each symbol represents the mean concentration from three mice. The error bars represent the standard deviation.
Pharmacodynamic target determination.
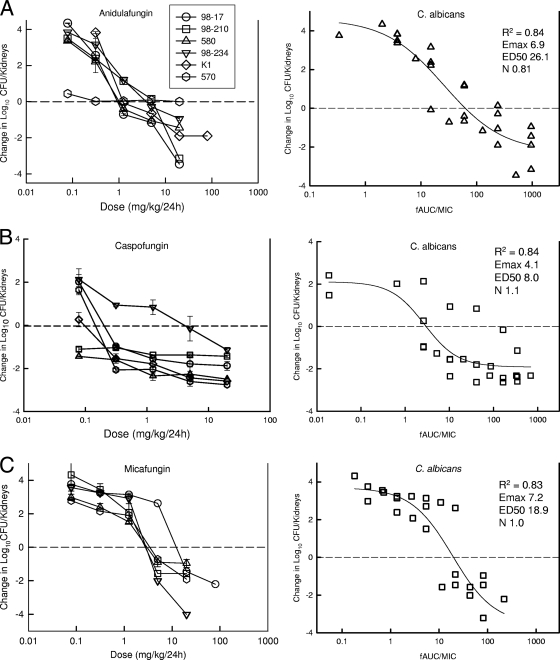
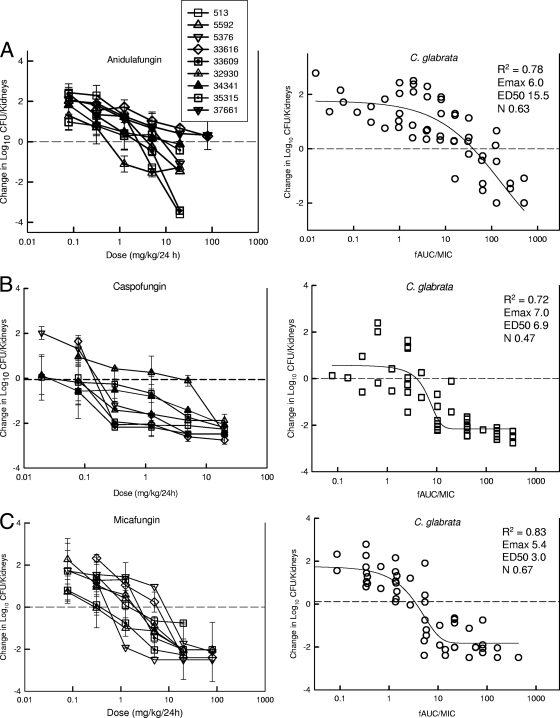
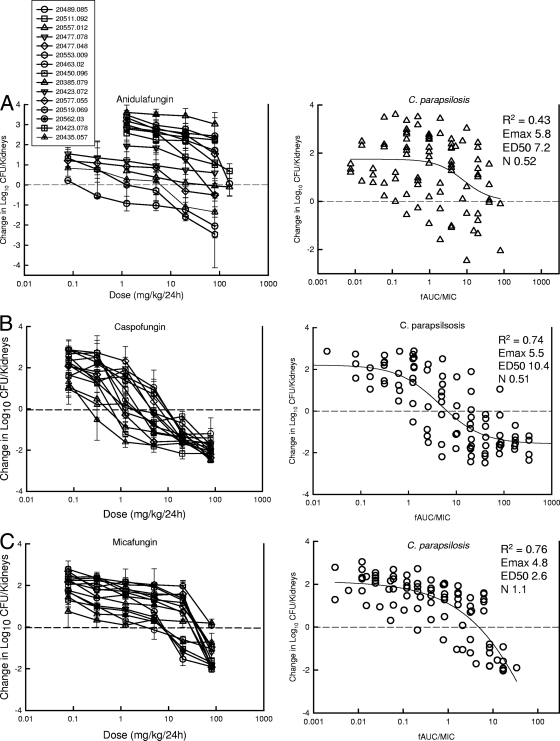
To determine if the index magnitudes among Candida strains and echinocandins were similar, we studied the in vivo activities of anidulafungin, caspofungin, and micafungin by using a 24-hour dosing regimen against up to 30 isolates. At the start of therapy, mice had 4.16 ± 0.39 log10 CFU/kidneys. The organisms grew 2.47 ± 0.86 log10 CFU/kidneys after 96 h in untreated control mice, and the growth values were similar among Candida species. There was also no significant difference in the burden at the start of therapy among the three Candida species. Escalating doses of each echinocandin resulted in concentration-dependent killing of all three Candida species (Fig. 2A to C, 3A to C, and 4A to C). We did not observe a paradoxical effect over the dose range with the organisms utilized in this study (54).
FIG. 2.
Relationship between anidulafungin (A), caspofungin (B), and micafungin (C) exposure (left panel, dose [mg/kg]; right panel, fAUC/MIC) and the burden of organisms in the kidneys of mice after 96 h of therapy against C. albicans. Each symbol represents the mean log10 CFU/kidneys of three mice. Efficacy on the y axis is expressed as the change in log10 CFU/kidneys compared to organism burden at the start of therapy. The horizontal dashed line represented the burden of organisms at the start of therapy. The solid line drawn through the data points represents the best fit line. The R2 is the coefficient of determination from regression using a sigmoid Emax model. The Emax is the maximal effect, the ED50 is the exposure value associated with 50% of Emax, and N is the slope of the regression.
FIG. 3.
Relationship between anidulafungin (A), caspofungin (B), and micafungin (C) exposure (left panel, dose [mg/kg]; right panel, fAUC/MIC) and the burden of organisms in the kidneys of mice after 96 h of therapy against C. glabrata. Each symbol represents the mean log10 CFU/kidneys of three mice. Efficacy on the y axis is expressed as the change in log10 CFU/kidneys compared to organism burden at the start of therapy. The horizontal dashed line represented the burden of organisms at the start of therapy. The solid line drawn through the data points represents the best fit line. The R2 is the coefficient of determination from regression using a sigmoid Emax model. The Emax is the maximal effect, the ED50 is the exposure value associated with 50% of Emax, and N is the slope of the regression.
FIG. 4.
Relationship between anidulafungin (A), caspofungin (B), and micafungin (C) exposure (left panel, dose [mg/kg]; right panel, fAUC/MIC) and the burden of organisms in the kidneys of mice after 96 h of therapy against C. parapsilosis. Each symbol represents the mean log10 CFU/kidneys of three mice. Efficacy on the y axis is expressed as the change in log10 CFU/kidneys compared to organism burden at the start of therapy. The horizontal dashed line represented the burden of organisms at the start of therapy. The solid line drawn through the data points represents the best fit line. The R2 is the coefficient of determination from regression using a sigmoid Emax model. The Emax is the maximal effect, the ED50 is the exposure value associated with 50% of Emax, and N is the slope of the regression.
In general, the shapes of the exposure-response curves were similar for all strains, with the exception of the anidulafungin-treated C. parapsilosis group. The location of the exposure-response curve in most cases was related to the MIC for the organism. The higher MIC values likely explain the lower anidulafungin C. parapsilosis response. The relationship between efficacy and both echinocandin dose and 24-h AUC/MIC was strong for each of the drug-organism groups (as reflected in the relatively high R2 values), with the exception of the anidulafungin data with C. parapsilosis, for which the data variability was quite large.
Caspofungin dosing regimens produced a static effect and 1 log kill for all of the study organisms (Fig. 2B, 3B, and 4B). The micafungin regimens similarly achieved the stasis endpoint for all organisms and the 1 log killing endpoint for all but two C. parapsilosis isolates and one C. glabrata isolate (Fig. 2C, 3C, and 4C). The treatment regimens for anidulafungin were similarly effective against C. albicans. However, the regimens were somewhat less effective against C. glabrata (1 log kill for five of nine strains) and exhibited reduced in vivo efficacy against the C. parapsilosis group (stasis endpoint for 7 of 15 organisms and 1 log kill for 3 of 15 organisms) (Fig. 2A, 3A, and 4A).
When one considers the dose levels (mg/kg) needed to achieve the treatment endpoints, two patterns were observed across the treatment results. First, therapy with caspofungin required less drug on a mg/kg basis (3- to 63-fold) than did that of either anidulafungin or micafungin to achieve the study endpoints. These differences were statistically significant (P value range of <0.001 to 0.01) for the stasis endpoint with each Candida species. The differences were also significant for the 1 log kill against the C. glabrata and C. parapsilosis species. The dose levels associated with these treatment goals were similar for both anidulafungin and micafungin (with the exception of the 1 log kill endpoint for C. glabrata, which was higher for anidulafungin). A second pattern observed throughout the study was the need for higher doses of each of the echinocandins for efficacy against C. parapsilosis (2.4- to 22-fold more drug on a mg/kg basis; P value range of <0.001 to 0.03) than those needed against either C. albicans or C. glabrata, which were relatively similar.
The 24-h AUC/MIC was used for pharmacodynamic index exploration of the exposure-response relationship (Fig. 2A to C, 3A to C, 4A to C, and 5; Table 3). Both total and free drug concentrations were considered, but only the free drug values are shown in the figures. When total drug concentrations were considered, exposures for each of the echinocandins were similar to those observed with dose alone. The total-drug 24-h AUC/MIC (tAUC/MIC) for caspofungin to achieve stasis or killing was 2- to nearly 16-fold lower than that for anidulafungin or micafungin against C. albicans and C. glabrata (P value range of 0.001 to 0.01). These differences were smaller and not statistically significant against C. parapsilosis where the data variability was greater. Although the tAUC/MIC values for anidulafungin and micafungin were similar, the anidulafungin tAUC/MIC values were slightly (but not statistically) smaller than those for micafungin (<2-fold) across the three Candida species. We theorize that this discrepancy is due to small differences in protein binding.
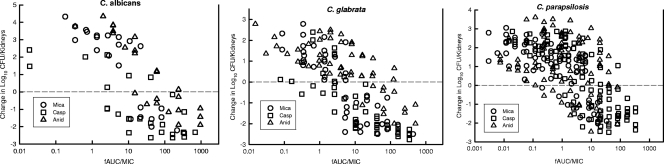
FIG. 5.
Relationship between anidulafungin (Anid), caspofungin (Casp), and micafungin (Mica) exposure (24-h fAUC/MIC and effect on the burden of organisms in the kidneys of mice after 96 h of therapy against C. albicans [left panel], C. glabrata [middle panel], and C. parapsilosis [right panel]). Each symbol represents the mean log10 CFU/kidneys of three mice. Efficacy on the y axis is expressed as the change in log10 CFU/kidneys compared to organism burden at the start of therapy. The horizontal dashed line represented the burden of organisms at the start of therapy.
TABLE 3.
In vivo pharmacodynamic target identification of anidulafungin, caspofungin, and micafungin against C. albicans, C. glabrata, and C. parapsilosis in a neutropenic murine disseminated candidiasis model
| Drug | Organism | Mean ± SDa |
|||||
|---|---|---|---|---|---|---|---|
| Static dose (mg/kg/24 h) | Static dose 24-h AUC/MIC | Static dose 24-h fAUC/MIC | 1 log kill (mg/kg/24 h) | 1 log kill 24-h AUC/MIC | 1 log kill 24-h fAUC/MIC | ||
| Anidulafungin | C. albicans | 2.32 ± 1.48 | 2,782 ± 2116 | 27.8 ± 21.1 | 4.25 ± 8.17 | 9,125 ± 8,144 | 91 ± 81 |
| C. glabrata | 21.1 ± 33.5 | 1,366 ± 1100 | 13.7 ± 11.0 | 39 ± 39 | 3,188 ± 2,256 | 32 ± 23 | |
| C. parapsilosis | 51.0 ± 35 | 1,154 ± 1091 | 11.5 ± 10.9 | 47 ± 46 | 2,244 ± 2,384 | 22 ± 24 | |
| Caspofungin | C. albicans | 0.72 ± 1.51 | 748 ± 1,675 | 22.4 ± 50.2 | 2.91 ± 6.66 | 865 ± 1,831 | 25.9 ± 54.9 |
| C. glabrata | 0.33 ± 0.71 | 96.2 ± 96 | 2.9 ± 2.8 | 1.16 ± 2.15 | 450 ± 448 | 13.5 ± 13.4 | |
| C. parapsilosis | 3.56 ± 3.08 | 559 ± 879 | 16.8 ± 26.4 | 9.84 ± 7.40 | 1,185 ± 1,385 | 35.5 ± 41.5 | |
| Micafungin | C. albicans | 2.79 ± 0.65 | 5,299 ± 1,860 | 12.7 ± 4.8 | 5.63 ± 3.08 | 10,088 ± 5,416 | 25.2 ± 13.5 |
| C. glabrata | 2.47 ± 2.79 | 1,542 ± 1,252 | 3.90 ± 3.1 | 5.88 ± 6.33 | 3,778 ± 3,003 | 9.45 ± 8.24 | |
| C. parapsilosis | 32.3 ± 24.0 | 1,981 ± 1,439 | 4.95 ± 3.6 | 55.8 ± 23.9 | 3,090 ± 1,781 | 7.73 ± 4.45 | |
Comparisons were statistically significant as follows. Static dose C. albicans caspofungin versus micafungin and anidulafungin, P = 0.01 and 0.04, respectively. Static dose C. glabrata caspofungin versus micafungin and anidulafungin, P < 0.001 and P = 0.05, respectively. Static dose C. parapsilosis caspofungin versus micafungin and anidulafungin, P = 0.0001 and P = 0.04, respectively. 1 Log kill dose C. glabrata caspofungin versus micafungin and anidulafungin, P = 0.001 and 0.005, respectively. 1 Log kill dose C. parapsilosis caspofungin versus micafungin and anidulafungin, P = 0.0001 and 0.001, respectively. Caspofungin static dose C. parapsilosis versus C. albicans and C. glabrata, P = 0.01 and 0.003, respectively. Caspofungin 1 log kill dose C. parapsilosis versus C. albicans and C. glabrata, P = 0.03 and 0.002, respectively. Anidulafungin static dose C. parapsilosis versus C. albicans and C. glabrata, P = 0.002 and 0.03, respectively. Micafungin static dose C. albicans versus C. parapsilosis and C. glabrata, P = 0.001 and P < 0.001, respectively. Micafungin 1 log kill dose C. albicans versus C. parapsilosis and C. glabrata, P < 0.001 and P < 0.001, respectively. tAUC/MIC static dose C. albicans anidulafungin versus caspofungin, P = 0.03; micafungin versus caspofungin, P < 0.001. tAUC/MIC static dose C glabrata anidulafungin versus caspofungin, P = 0.01; micafungin versus caspofungin, P = 0.001. tAUC/MIC static dose C parapsilosis micafungin versus caspofungin, P = 0.001. tAUC/MIC anidulafungin C. albicans versus C. parapsilosis, P = 0.01. tAUC/MIC 1 log kill anidulafungin C. albicans versus C. glabrata and C. parapsilosis, P = 0.01 and 0.001, respectively. fAUC static dose C. glabrata anidulafungin versus caspofungin and micafungin, P = 0.002 and 0.005, respectively. fAUC/MIC 1 log kill dose C. glabrata anidulafungin versus caspofungin and micafungin, P = 0.007 and 0.02, respectively. fAUC/MIC 1 log kill dose C. parapsilosis caspofungin versus micafungin, P = 0.009. fAUC/MIC static dose micafungin C. albicans versus C. glabrata and C. parapsilosis, P < 0.001 and P < 0.001, respectively. fAUC/MIC 1 log kill micafungin C. albicans versus C. glabrata and C. parapsilosis, P < 0.001 and P < 0.001, respectively.
Several interesting observations were seen in evaluation of the impact of the infecting Candida species. For micafungin, the tAUC/MIC values for C. parapsilosis and C. glabrata were roughly 3-fold lower than for C. albicans. For anidulafungin, the exposures for C. albicans and C. glabrata were similar. The anidulafungin values for C. parapsilosis are more difficult to interpret due to the small number of strains for which the endpoints were achieved and the wide variability in the available results; however, for the few strains the target was lower than for C. albicans and C. glabrata. For caspofungin, the tAUC/MIC exposure associated with stasis was a bit higher for C. parapsilosis. However, there were three strain outliers among the 15 strains studied. In each of the three cases, the MICs were low (0.06 μg/ml). Mean pharmacodynamic target calculations for caspofungin in the absence of these data three points result in a C. parapsilosis pharmacodynamic target (free-drug AUC/MIC [fAUC/MIC], 6.0) that is nearly identical to that observed with the other two echinocandins.
Consideration of free drug exposure markedly reduced the differences among the echinocandins (differences were less than 2-fold and not statistically significant) (Table 3). The 24-h fAUC/MICs associated with the stasis endpoint for the echinocandin group against C. albicans was 20.6 ± 32 (mean ± standard deviation). Similar values for C. glabrata and C. parapsilosis were 7.0 ± 8.3 and 7.6 ± 7.1, respectively. The values for C. glabrata and C. parapsilosis were statistically lower than those for C. albicans (P < 0.001). The dose-response relationships were fairly steep for each organism group, and the exposures needed for a 1 log10 kill were only 1.2- to 4.5-fold higher (mean ± standard deviation, 2.3 ± 0.92) than that needed for the stasis endpoint.
DISCUSSION
Candida species are the most common systemic fungal pathogens in humans and exhibit a disease spectrum ranging from mucosal to systemic infections. Invasive candidiasis has high attributable mortality, especially in immunosuppressed patients (41, 42). The addition of the echinocandin class of antifungals marks a significant advance in therapy of these diseases, with enhanced safety and efficacy compared to previously available antifungal therapies (31, 36, 43, 52). However, as with the other available antifungal therapies, the echinocandins exhibit variable potencies against different fungal species, and accumulating case reports have illustrated the potential for resistance development (18-20, 25, 27, 28, 30, 32, 35, 44, 45, 49). Thus, it is clear that there are Candida infections for which echinocandin potency is insufficient for effective therapy. Understanding the limits of echinocandin therapy in relation to the MIC should aid in development of susceptibility breakpoints and guide optimal antifungal treatment strategies.
The MIC distributions of the echinocandin class are relatively similar against most Candida species (33, 45-48). The species for which potency is reduced in vitro is C. parapsilosis. Most isolates are 50- to 100-fold less susceptible to the echinocandins than other common Candida species. However, clinical trials have demonstrated effectiveness for management of both mucosal and systemic candidiasis against each of the common Candida species, including C. parapsilosis (36, 43, 52). Reports from these large trials do not detect a relationship between in vitro susceptibility and treatment efficacy (29). However, the ability of these trials to discern this relationship has been limited due to the narrow range of MICs for study isolates and there being very few isolates with higher MIC values and the complexity of the disease state.
Recent suggestions have been made by the CLSI to define susceptibility breakpoints for the echinocandins and Candida species (50). The rationale for these recommendations is based upon a “blueprint” procedure which has been effective for other antifungal compounds (50, 51, 53). The process evaluates clinical outcome relative to MIC, considers pharmacodynamic analyses from experimental and clinical data sets, and assesses the MIC distribution with a preference to avoid setting a breakpoint that would split a wild-type MIC range (51, 53).
The pharmacodynamic analysis component of this process is the focus of the current investigation. The study of antimicrobial pharmacodynamics explores the relationships among pharmacokinetics, MIC, and treatment outcome (1, 17). Application of these tools has been utilized to define the limits of treatment relative to the MIC and to subsequently guide susceptibility breakpoints. The goal of the present study was to determine the amount of drug relative to the MIC required for efficacy of three echinocandins against the three most common Candida species, including the species with higher MICs, C. parapsilosis. With this information, we then extrapolated the experimental findings to patients and asked, with clinically relevant echinocandin pharmacokinetics, what is the highest Candida MIC for which treatment would be expected to remain effective?
Previous studies using this model and analyses have explored the pharmacodynamic target for select echinocandins against C. albicans and C. glabrata (9, 14). Prior attempts to examine the target for the high-MIC C. parapsilosis group have been difficult due to the reduced fitness of this species in the mouse infection model (15). In designing the current experiments, we strove to include organisms with similar fitness levels in the infection to avoid potentially confounding differences in outcome associated with differences in organism virulence. The organisms used in the present study, were screened for fitness in the model, and all were shown to grow well in the kidneys of mice over the treatment period. The C. parapsilosis collection of organisms was identified through a laborious screening process in which nearly 80 individual isolates were tested in the animal model to find the group of 15 organisms sufficient for the goals of this study (data not shown).
In general, the amount of drug required to produce these treatment endpoints in the current study was related to the organism MIC. The organism group for which each of the echinocandins demonstrated the least in vivo activity was C. parapsilosis. This discrepancy was most evident for anidulafungin. These study findings are not surprising, given the higher MICs for this collection of strains.
In the pharmacodynamic analyses, we considered both protein-bound and unbound drug concentrations, since numerous antibacterial and antifungal pharmacodynamic experiments have suggested the relevance of protein binding (2, 10, 12, 13, 38, 40). The majority of these investigations have shown that free drug concentrations are most relevant. Findings from the current studies suggest the relevance of this pharmacokinetic phenomenon as well. If one considers only total drug concentrations, it would appear that caspofungin requires much less drug than does either anidulafungin or micafungin. However, the degree of binding of caspofungin is lower (97%) than that of these echinocandins (anidulafungin, 99%, and micafungin, 99.75%). When unbound concentrations are considered, the amounts of drug needed for efficacy are very similar among the three compounds. Interestingly, even though the differences in binding between anidulafungin and micafungin are small, across the majority of study isolates, anidulafungin required lower total drug exposures than did micafungin, suggesting the relevance of even small differences in protein binding.
One unexpected finding from these studies was the apparent difference in the pharmacodynamic target for echinocandins among Candida species. The target for C. albicans was larger than that for either C. glabrata or C. parapsilosis. Perhaps these observations should not be surprising given the demonstrated relevance of species-specific susceptibility breakpoints for antibacterial agents (1, 3, 6, 7). For example, the 24-h AUC/MIC quinolone target for Streptococcus pneumoniae is near 25, while the target for Gram-negative bacilli is nearly 4-fold higher. Clinical pharmacodynamic analyses with large case numbers from each of the Candida species should be undertaken to further explore this phenomenon for the echinocandins.
The ability to translate these mouse pharmacodynamic results to patients lies with the premise that the drug target is in the organism and thus the host handling of the drug is of minimal consequence. The pharmacodynamic targets or amounts of drug relative to the MIC needed for effect should be similar for mice and men. Human pharmacokinetics with each of these echinocandins demonstrates protein binding values that are essentially the same as those observed in mice. The approved steady-state regimens for treatment of invasive candidiasis with these drugs include 100 mg/day of both anidulafungin and micafungin and 50 mg/day of caspofungin. These regimens produce total- and free-drug 24-h AUC values in healthy volunteers of 112 mg·h/ml and 1.12 mg·h/ml for anidulafungin, 98 mg·h/ml and 2.94 mg·h/ml for caspofungin, and 126 mg·h/ml and 0.38 mg·h/ml for micafungin (16, 23, 26, 56). If one considers these pharmacokinetics with these echinocandins and the presented pharmacodynamic targets, one can then estimate the highest MICs for the three Candida species that would allow the pharmacodynamic 24-h fAUC/MIC to be met. The MIC ceiling based on fAUC/MIC ranging from 5 to 20 would place the susceptibility breakpoint lower than the current CLSI value of 2 μg/ml for each of the drugs. However, the MICs for nearly all of the wild-type strains from surveillance studies would be expected to fall within the “pharmacodynamically susceptible” category based upon the fAUC/MIC targets reported in this study, with the exception of a subset of C. parapsilosis isolates (39, 45).
Previous animal model and clinical epidemiologic studies have suggested that C. parapsilosis is a less fit or virulent species than are other commonly encountered Candida species. A limitation of the current study was the inability to include C. parapsilosis with various levels of and specifically reduced in vivo fitness. One may speculate that the pharmacodynamic target may be lower in organisms that are “less fit.” Thus, it is possible that the echinocandin exposure target for the C. parapsilosis group may be artificially elevated in the current study, as the organisms we were able to study represent a highly fit subset of the wild-type population. The impact of organism fitness on pharmacodynamic relationships is difficult but an important area for future investigation.
In summary, these studies demonstrate a relationship between echinocandin dose, MIC, and efficacy. More specifically, the results identify the pharmacodynamic target for clinically available echinocandins against the three most commonly encountered Candida species and suggest differences among species. Future studies should examine the impact of even higher MICs and explore the mechanistic basis for the subtle differences in echinocandin-Candida species targets identified in this study.
Acknowledgments
This research was funded by grants from Merck, Astellas, and Pfizer.
Footnotes
Published ahead of print on 12 April 2010.
REFERENCES
- 1.Ambrose, P. G., S. M. Bhavnani, C. M. Rubino, A. Louie, T. Gumbo, A. Forrest, and G. L. Drusano. 2007. Pharmacokinetics-pharmacodynamics of antimicrobial therapy: it's not just for mice anymore. Clin. Infect. Dis. 44:79-86. [DOI] [PubMed] [Google Scholar]
- 2.Andes, D. 2003. In vivo pharmacodynamics of antifungal drugs in treatment of candidiasis. Antimicrob. Agents Chemother. 47:1179-1186. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Andes, D. 2001. Pharmacokinetic and pharmacodynamic properties of antimicrobials in the therapy of respiratory tract infections. Curr. Opin. Infect. Dis. 14:165-172. [DOI] [PubMed] [Google Scholar]
- 4.Andes, D. 2005. Use of an animal model of disseminated candidiasis in the evaluation of antifungal therapy. Methods Mol. Med. 118:111-128. [DOI] [PubMed] [Google Scholar]
- 5.Andes, D., and W. A. Craig. 2002. Animal model pharmacokinetics and pharmacodynamics: a critical review. Int. J. Antimicrob. Agents 19:261-268. [DOI] [PubMed] [Google Scholar]
- 6.Andes, D., and W. A. Craig. 2003. Pharmacodynamics of the new des-f(6)-quinolone garenoxacin in a murine thigh infection model. Antimicrob. Agents Chemother. 47:3935-3941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Andes, D., and W. A. Craig. 2002. Pharmacodynamics of the new fluoroquinolone gatifloxacin in murine thigh and lung infection models. Antimicrob. Agents Chemother. 46:1665-1670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reference deleted.
- 9.Andes, D., D. J. Diekema, M. A. Pfaller, R. A. Prince, K. Marchillo, J. Ashbeck, and J. Hou. 2008. In vivo pharmacodynamic characterization of anidulafungin in a neutropenic murine candidiasis model. Antimicrob. Agents Chemother. 52:539-550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Andes, D., K. Marchillo, R. Conklin, G. Krishna, F. Ezzet, A. Cacciapuoti, and D. Loebenberg. 2004. Pharmacodynamics of a new triazole, posaconazole, in a murine model of disseminated candidiasis. Antimicrob. Agents Chemother. 48:137-142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Andes, D., K. Marchillo, J. Lowther, A. Bryskier, T. Stamstad, and R. Conklin. 2003. In vivo pharmacodynamics of HMR 3270, a glucan synthase inhibitor, in a murine candidiasis model. Antimicrob. Agents Chemother. 47:1187-1192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Andes, D., K. Marchillo, T. Stamstad, and R. Conklin. 2003. In vivo pharmacodynamics of a new triazole, ravuconazole, in a murine candidiasis model. Antimicrob. Agents Chemother. 47:1193-1199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Andes, D., K. Marchillo, T. Stamstad, and R. Conklin. 2003. In vivo pharmacokinetics and pharmacodynamics of a new triazole, voriconazole, in a murine candidiasis model. Antimicrob. Agents Chemother. 47:3165-3169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Andes, D. R., D. J. Diekema, M. A. Pfaller, K. Marchillo, and J. Bohrmueller. 2008. In vivo pharmacodynamic target investigation for micafungin against Candida albicans and C. glabrata in a neutropenic murine candidiasis model. Antimicrob. Agents Chemother. 52:3497-3503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Arendrup, M., T. Horn, and N. Frimodt-Moller. 2002. In vivo pathogenicity of eight medically relevant Candida species in an animal model. Infection 30:286-291. [DOI] [PubMed] [Google Scholar]
- 16.Chandrasekar, P. H., and J. D. Sobel. 2006. Micafungin: a new echinocandin. Clin. Infect. Dis. 42:1171-1178. [DOI] [PubMed] [Google Scholar]
- 17.Craig, W. A. 1998. Pharmacokinetic/pharmacodynamic parameters: rationale for antibacterial dosing of mice and men. Clin. Infect. Dis. 26:1-10. (Quiz 11-2.) [DOI] [PubMed] [Google Scholar]
- 18.Forrest, G. N., E. Weekes, and J. K. Johnson. 2008. Increasing incidence of Candida parapsilosis candidemia with caspofungin usage. J. Infect. 56:126-129. [DOI] [PubMed] [Google Scholar]
- 19.Garcia-Effron, G., D. P. Kontoyiannis, R. E. Lewis, and D. S. Perlin. 2008. Caspofungin-resistant Candida tropicalis strains causing breakthrough fungemia in patients at high risk for hematologic malignancies. Antimicrob. Agents Chemother. 52:4181-4183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Garcia-Effron, G., S. Park, and D. S. Perlin. 2009. Correlating echinocandin MIC and kinetic inhibition of fks1 mutant glucan synthases for Candida albicans: implications for interpretive breakpoints. Antimicrob. Agents Chemother. 53:112-122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gumbo, T., G. L. Drusano, W. Liu, R. W. Kulawy, C. Fregeau, V. Hsu, and A. Louie. 2007. Once-weekly micafungin therapy is as effective as daily therapy for disseminated candidiasis in mice with persistent neutropenia. Antimicrob. Agents Chemother. 51:968-974. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gumbo, T., G. L. Drusano, W. Liu, L. Ma, M. R. Deziel, M. F. Drusano, and A. Louie. 2006. Anidulafungin pharmacokinetics and microbial response in neutropenic mice with disseminated candidiasis. Antimicrob. Agents Chemother. 50:3695-3700. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Gumbo, T., J. Hiemenz, L. Ma, J. J. Keirns, D. N. Buell, and G. L. Drusano. 2008. Population pharmacokinetics of micafungin in adult patients. Diagn. Microbiol. Infect. Dis. 60:329-331. [DOI] [PubMed] [Google Scholar]
- 24.Hajdu, R., R. Thompson, J. G. Sundelof, B. A. Pelak, F. A. Bouffard, J. F. Dropinski, and H. Kropp. 1997. Preliminary animal pharmacokinetics of the parenteral antifungal agent MK-0991 (L-743,872). Antimicrob. Agents Chemother. 41:2339-2344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Hakki, M., J. F. Staab, and K. A. Marr. 2006. Emergence of a Candida krusei isolate with reduced susceptibility to caspofungin during therapy. Antimicrob. Agents Chemother. 50:2522-2524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hebert, M. F., H. E. Smith, T. C. Marbury, S. K. Swan, W. B. Smith, R. W. Townsend, D. Buell, J. Keirns, and I. Bekersky. 2005. Pharmacokinetics of micafungin in healthy volunteers, volunteers with moderate liver disease, and volunteers with renal dysfunction. J. Clin. Pharmacol. 45:1145-1152. [DOI] [PubMed] [Google Scholar]
- 27.Hernandez, S., J. L. Lopez-Ribot, L. K. Najvar, D. I. McCarthy, R. Bocanegra, and J. R. Graybill. 2004. Caspofungin resistance in Candida albicans: correlating clinical outcome with laboratory susceptibility testing of three isogenic isolates serially obtained from a patient with progressive Candida esophagitis. Antimicrob. Agents Chemother. 48:1382-1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Kabbara, N., C. Lacroix, R. Peffault de Latour, G. Socie, M. Ghannoum, and P. Ribaud. 2008. Breakthrough C. parapsilosis and C. guilliermondii blood stream infections in allogeneic hematopoietic stem cell transplant recipients receiving long-term caspofungin therapy. Haematologica 93:639-640. [DOI] [PubMed] [Google Scholar]
- 29.Kartsonis, N., J. Killar, L. Mixson, C. M. Hoe, C. Sable, K. Bartizal, and M. Motyl. 2005. Caspofungin susceptibility testing of isolates from patients with esophageal candidiasis or invasive candidiasis: relationship of MIC to treatment outcome. Antimicrob. Agents Chemother. 49:3616-3623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Krogh-Madsen, M., M. C. Arendrup, L. Heslet, and J. D. Knudsen. 2006. Amphotericin B and caspofungin resistance in Candida glabrata isolates recovered from a critically ill patient. Clin. Infect. Dis. 42:938-944. [DOI] [PubMed] [Google Scholar]
- 31.Kuse, E. R., P. Chetchotisakd, C. A. da Cunha, M. Ruhnke, C. Barrios, D. Raghunadharao, J. S. Sekhon, A. Freire, V. Ramasubramanian, I. Demeyer, M. Nucci, A. Leelarasamee, F. Jacobs, J. Decruyenaere, D. Pittet, A. J. Ullmann, L. Ostrosky-Zeichner, O. Lortholary, S. Koblinger, H. Diekmann-Berndt, and O. A. Cornely. 2007. Micafungin versus liposomal amphotericin B for candidaemia and invasive candidosis: a phase III randomised double-blind trial. Lancet 369:1519-1527. [DOI] [PubMed] [Google Scholar]
- 32.Laverdière, M., R. G. Lalonde, J. G. Baril, D. C. Sheppard, S. Park, and D. S. Perlin. 2006. Progressive loss of echinocandin activity following prolonged use for treatment of Candida albicans oesophagitis. J. Antimicrob. Chemother. 57:705-708. [DOI] [PubMed] [Google Scholar]
- 33.Lockhart, S. R., S. A. Messer, M. A. Pfaller, and D. J. Diekema. 2008. Geographic distribution and antifungal susceptibility of the newly described species Candida orthopsilosis and Candida metapsilosis in comparison to the closely related species Candida parapsilosis. J. Clin. Microbiol. 46:2659-2664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Louie, A., M. Deziel, W. Liu, M. F. Drusano, T. Gumbo, and G. L. Drusano. 2005. Pharmacodynamics of caspofungin in a murine model of systemic candidiasis: importance of persistence of caspofungin in tissues to understanding drug activity. Antimicrob. Agents Chemother. 49:5058-5068. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Miller, C. D., B. W. Lomaestro, S. Park, and D. S. Perlin. 2006. Progressive esophagitis caused by Candida albicans with reduced susceptibility to caspofungin. Pharmacotherapy 26:877-880. [DOI] [PubMed] [Google Scholar]
- 36.Mora-Duarte, J., R. Betts, C. Rotstein, A. L. Colombo, L. Thompson-Moya, J. Smietana, R. Lupinacci, C. Sable, N. Kartsonis, and J. Perfect. 2002. Comparison of caspofungin and amphotericin B for invasive candidiasis. N. Engl. J. Med. 347:2020-2029. [DOI] [PubMed] [Google Scholar]
- 37.NCCLS. 2002. Clinical Laboratory Standards Institute, reference method for broth dilution antifungal susceptibility testing. Document M27-A2, 2nd ed. National Committee for Clinical Laboratory Standards, Wayne, PA.
- 38.Odabasi, Z., V. Paetznick, J. H. Rex, and L. Ostrosky-Zeichner. 2007. Effects of serum on in vitro susceptibility testing of echinocandins. Antimicrob. Agents Chemother. 51:4214-4216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Ostrosky-Zeichner, L., J. H. Rex, P. G. Pappas, R. J. Hamill, R. A. Larsen, H. W. Horowitz, W. G. Powderly, N. Hyslop, C. A. Kauffman, J. Cleary, J. E. Mangino, and J. Lee. 2003. Antifungal susceptibility survey of 2,000 bloodstream Candida isolates in the United States. Antimicrob. Agents Chemother. 47:3149-3154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Paderu, P., G. Garcia-Effron, S. Balashov, G. Delmas, S. Park, and D. S. Perlin. 2007. Serum differentially alters the antifungal properties of echinocandin drugs. Antimicrob. Agents Chemother. 51:2253-2256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Pappas, P. G., C. A. Kauffman, D. Andes, D. K. Benjamin, Jr., T. F. Calandra, J. E. Edwards, Jr., S. G. Filler, J. F. Fisher, B. J. Kullberg, L. Ostrosky-Zeichner, A. C. Reboli, J. H. Rex, T. J. Walsh, and J. D. Sobel. 2009. Clinical practice guidelines for the management of candidiasis: 2009 update by the Infectious Diseases Society of America. Clin. Infect. Dis. 48:503-535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Pappas, P. G., J. H. Rex, J. Lee, R. J. Hamill, R. A. Larsen, W. Powderly, C. A. Kauffman, N. Hyslop, J. E. Mangino, S. Chapman, H. W. Horowitz, J. E. Edwards, and W. E. Dismukes. 2003. A prospective observational study of candidemia: epidemiology, therapy, and influences on mortality in hospitalized adult and pediatric patients. Clin. Infect. Dis. 37:634-643. [DOI] [PubMed] [Google Scholar]
- 43.Pappas, P. G., C. M. Rotstein, R. F. Betts, M. Nucci, D. Talwar, J. J. De Waele, J. A. Vazquez, B. F. Dupont, D. L. Horn, L. Ostrosky-Zeichner, A. C. Reboli, B. Suh, R. Digumarti, C. Wu, L. L. Kovanda, L. J. Arnold, and D. N. Buell. 2007. Micafungin versus caspofungin for treatment of candidemia and other forms of invasive candidiasis. Clin. Infect. Dis. 45:883-893. [DOI] [PubMed] [Google Scholar]
- 44.Park, S., R. Kelly, J. N. Kahn, J. Robles, M. J. Hsu, E. Register, W. Li, V. Vyas, H. Fan, G. Abruzzo, A. Flattery, C. Gill, G. Chrebet, S. A. Parent, M. Kurtz, H. Teppler, C. M. Douglas, and D. S. Perlin. 2005. Specific substitutions in the echinocandin target Fks1p account for reduced susceptibility of rare laboratory and clinical Candida sp. isolates. Antimicrob. Agents Chemother. 49:3264-3273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Pfaller, M. A., L. Boyken, R. J. Hollis, J. Kroeger, S. A. Messer, S. Tendolkar, and D. J. Diekema. 2008. In vitro susceptibility of invasive isolates of Candida spp. to anidulafungin, caspofungin, and micafungin: six years of global surveillance. J. Clin. Microbiol. 46:150-156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Pfaller, M. A., L. Boyken, R. J. Hollis, S. A. Messer, S. Tendolkar, and D. J. Diekema. 2006. Global surveillance of in vitro activity of micafungin against Candida: a comparison with caspofungin by CLSI-recommended methods. J. Clin. Microbiol. 44:3533-3538. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Pfaller, M. A., L. Boyken, R. J. Hollis, S. A. Messer, S. Tendolkar, and D. J. Diekema. 2005. In vitro activities of anidulafungin against more than 2,500 clinical isolates of Candida spp., including 315 isolates resistant to fluconazole. J. Clin. Microbiol. 43:5425-5427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pfaller, M. A., L. Boyken, R. J. Hollis, S. A. Messer, S. Tendolkar, and D. J. Diekema. 2006. In vitro susceptibilities of Candida spp. to caspofungin: four years of global surveillance. J. Clin. Microbiol. 44:760-763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Pfaller, M. A., D. J. Diekema, D. L. Gibbs, V. A. Newell, K. P. Ng, A. Colombo, J. Finquelievich, R. Barnes, and J. Wadula. 2008. Geographic and temporal trends in isolation and antifungal susceptibility of Candida parapsilosis: a global assessment from the ARTEMIS DISK Antifungal Surveillance Program, 2001 to 2005. J. Clin. Microbiol. 46:842-849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pfaller, M. A., D. J. Diekema, L. Ostrosky-Zeichner, J. H. Rex, B. D. Alexander, D. Andes, S. D. Brown, V. Chaturvedi, M. A. Ghannoum, C. C. Knapp, D. J. Sheehan, and T. J. Walsh. 2008. Correlation of MIC with outcome for Candida species tested against caspofungin, anidulafungin, and micafungin: analysis and proposal for interpretive MIC breakpoints. J. Clin. Microbiol. 46:2620-2629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pfaller, M. A., D. J. Diekema, J. H. Rex, A. Espinel-Ingroff, E. M. Johnson, D. Andes, V. Chaturvedi, M. A. Ghannoum, F. C. Odds, M. G. Rinaldi, D. J. Sheehan, P. Troke, T. J. Walsh, and D. W. Warnock. 2006. Correlation of MIC with outcome for Candida species tested against voriconazole: analysis and proposal for interpretive breakpoints. J. Clin. Microbiol. 44:819-826. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Reboli, A. C., C. Rotstein, P. G. Pappas, S. W. Chapman, D. H. Kett, D. Kumar, R. Betts, M. Wible, B. P. Goldstein, J. Schranz, D. S. Krause, and T. J. Walsh. 2007. Anidulafungin versus fluconazole for invasive candidiasis. N. Engl. J. Med. 356:2472-2482. [DOI] [PubMed] [Google Scholar]
- 53.Rex, J. H., M. A. Pfaller, J. N. Galgiani, M. S. Bartlett, A. Espinel-Ingroff, M. A. Ghannoum, M. Lancaster, F. C. Odds, M. G. Rinaldi, T. J. Walsh, A. L. Barry, and the Subcommittee on Antifungal Susceptibility Testing of the National Committee for Clinical Laboratory Standards. 1997. Development of interpretive breakpoints for antifungal susceptibility testing: conceptual framework and analysis of in vitro-in vivo correlation data for fluconazole, itraconazole, and Candida infections. Clin. Infect. Dis. 24:235-247. [DOI] [PubMed] [Google Scholar]
- 54.Stevens, D. A., M. Ichinomiya, Y. Koshi, and H. Horiuchi. 2006. Escape of Candida from caspofungin inhibition at concentrations above the MIC (paradoxical effect) accomplished by increased cell wall chitin; evidence for β-1,6-glucan synthesis inhibition by caspofungin. Antimicrob. Agents Chemother. 50:3160-3161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.van Asbeck, E. C., K. V. Clemons, A. N. Markham, and D. A. Stevens. 2009. Correlation of restriction fragment length polymorphism genotyping with internal transcribed spacer sequence, randomly amplified polymorphic DNA and multilocus sequence groupings for Candida parapsilosis. Mycoses 52:493-498. [DOI] [PubMed] [Google Scholar]
- 56.Vazquez, J. A., and J. D. Sobel. 2006. Anidulafungin: a novel echinocandin. Clin. Infect. Dis. 43:215-222. [DOI] [PubMed] [Google Scholar]
- 57.Wiederhold, N. P., D. P. Kontoyiannis, J. Chi, R. A. Prince, V. H. Tam, and R. E. Lewis. 2004. Pharmacodynamics of caspofungin in a murine model of invasive pulmonary aspergillosis: evidence of concentration-dependent activity. J. Infect. Dis. 190:1464-1471. [DOI] [PubMed] [Google Scholar]