Abstract
To evaluate the tolerability and liver safety profiles of the systemic antifungal agents commonly used for the treatment of invasive fungal infection, we conducted a systematic review and meta-analysis of randomized controlled trials published before 31 August 2009. Two reviewers independently applied selection criteria, performed quality assessment, and extracted data. We used the beta-binomial model to account for variation across studies and the maximum likelihood method to estimate the pooled risks. We identified 39 studies with more than 8,000 enrolled patients for planned comparisons. The incidence rates of treatment discontinuation due to adverse reactions and liver injury associated with antifungal therapy ranged widely. The pooled risks of treatment discontinuation due to adverse reactions were above 10% for amphotericin B formulations and itraconazole, whereas they were 2.5% to 3.8% for fluconazole, caspofungin, and micafungin. We found that 1.5% of the patients stopped itraconazole treatment due to hepatotoxicity. Furthermore, 19.7% of voriconazole users and 17.4% of itraconazole users had elevated serum liver enzyme levels, although they did not require treatment discontinuation, whereas 2.0% or 9.3% of fluconazole and echinocandin users had elevated serum liver enzyme levels but did not require treatment discontinuation. The results were similar when we stratified the data by empirical or definitive antifungal therapy. Possible explanations for antifungal agent-related hepatotoxicity were confounded by antifungal prescription to patients with a high risk of liver injury, the increased chance of detection of hepatotoxicity due to prolonged treatment, or the pharmacological entity.
Invasive fungal infection is a leading cause of morbidity and mortality among immunocompromised and debilitated patients, including those with hematological malignancy, solid organ or bone marrow transplantation, and neutropenia and those receiving systemic corticosteroid therapy. Candida species and Aspergillus species are the two predominant causative fungi, with the case fatality rates being 30% and 50% among those infected with members of these two fungal genera, respectively (19, 53). Over the past few decades, amphotericin B has been the mainstay treatment of candidiasis and aspergillosis, whereas fluconazole has been extensively used among patients with Candida albicans infection. After randomized controlled trials showed that extended-spectrum azoles (itraconazole, voriconazole, posaconazole) and echinocandins (anidulafungin, caspofungin, micafungin) had efficacies similar to those of amphotericin B and fluconazole, these newer antifungal agents have been used more frequently for the treatment of patients with probable or proven invasive fungal infection (18, 32, 56, 59, 81). Current practice guidelines recommend amphotericin B formulations, fluconazole, and echinocandins as first-line therapy for patients with candidemia; and amphotericin B formulations or voriconazole are the drugs of choice for the primary therapy of invasive aspergillosis (32, 56, 59, 81). For patients who fail the primary therapy or who have intolerable adverse reactions, the common practice is to switch to a different class of antifungal agents (60, 73).
With regard to the safety of antifungal therapies, amphotericin B desoxycholate is known for its infusion-related adverse effects and nephrotoxicity; approximately 30% of patients developed abnormal renal function during treatment, and treatment was discontinued in 5% of patients because of toxicity (4, 28). Other amphotericin B formulations, including amphotericin B colloidal dispersion, amphotericin B lipid complex, liposomal amphotericin B (Ambisome), and other, newer antifungal agents, are associated with substantially fewer infusion-related and nephrotoxic events. However, hepatotoxic reactions to antifungal agents were increasingly reported and ranged from mild and asymptomatic abnormalities in liver function test results to potentially fatal fulminant hepatic failure (17, 20, 25, 35, 74, 88). While individual reviews of new antifungal agents have been published (7, 16, 24, 27, 28, 29, 34, 41, 47, 50, 67, 68, 71), there has been no systematic evaluation of the liver toxicity associated with these treatments. We conducted a systematic review and meta-analysis to evaluate the safety information from published studies of definitive therapy for invasive fungal infection and empirical antifungal use for prolonged febrile neutropenia and calculated the absolute risk estimates associated with these treatment regimens.
MATERIALS AND METHODS
We followed the recommendations of the Quality of Reporting of Meta-Analyses (QUOROM) conference in conducting this systematic review (51).
Literature search strategy.
We searched Medline, Embase, the Cochrane Library (which includes the Cochrane Database of Systematic Reviews, the Database of Abstracts of Reviews of Effects, and the Cochrane Register of Controlled Trials), and the ClinicalTrials.gov website for relevant articles. The Medical Subjects Heading (MeSH) terms used for keyword and text word searches included antifungals, amphotericin, Ambisome, itraconazole, fluconazole, voriconazole, posaconazole, caspofungin, micafungin, anidulafungin, fungemia, aspergillosis, and candidiasis. The references of 13 review articles on treatments for invasive fungal infection and empirical antifungal treatments for febrile neutropenia were examined to identify additional studies that were not found in the computerized databases (7, 16, 24, 27, 28, 29, 47, 34, 41, 50, 67, 68, 71). Additional reports were identified from the reference lists of those articles.
Selection criteria for studies.
We included trials that mainly enrolled adult patients who had suspected or documented invasive fungal (Aspergillus, Candida) infections or persistent febrile neutropenia and who were receiving empirical, preemptive, or definitive antifungal therapy. Only articles in the English language published before 31 August 2009 were included. We excluded trials that enrolled only neonatal or pediatric patients, pharmacokinetic studies, mycology studies, and studies focusing on drug-drug interactions. We also excluded studies of asymptomatic patients received antifungal therapy as prophylaxis or prevention, studies enrolling patients with superficial (dermatomycosis, onychomycosis) and mucocutaneous (mucositis, gingivitis, esophagitis, vaginitis) fungal infections, studies focusing on infusion-related or renal toxicity, and studies of combination antifungal treatments. The main analytical results were obtained by combining data only from randomized controlled trials. In the auxiliary analysis, we added data from nonrandomized controlled trials and case series and cohort studies to increase the generalizability of our study results.
Trials of systemic amphotericin B formulations (amphotericin B desoxycholate, amphotericin B colloidal dispersion, amphotericin B lipid complex, liposomal amphotericin B), itraconazole, fluconazole, voriconazole, caspofungin, micafungin, and anidulafungin, with or without subsequent oral therapy, as one of the treatment arms were included, regardless of the antifungal dosage or the length of therapy. We did not evaluate studies of miconazole, ketoconazole, oral amphotericin B, or amphotericin B intralipid mixture, as they are no longer considered standard treatments for invasive fungal infection. Treatment arms involving sequential or salvage antifungal therapy were included only if clear safety endpoints were reported for each treatment phase of the trials.
Safety outcomes.
The primary outcome of interest was the cumulative incidence of patients who withdrew from the study due to adverse reactions. Secondary outcomes of interest were the cumulative incidence of patients stopping treatment due to abnormal liver function test results (abnormal serum transaminase, alkaline phosphatase, or bilirubin levels) and the cumulative incidence of patients developing abnormal liver function test results during treatment but not requiring discontinuation. We did not define the specific cutoff values for the liver enzyme levels that warranted treatment termination because different criteria were used in different studies.
Data extraction and quality assessment.
Two physician reviewers (J.-L.W. and C.-H.C.) independently evaluated each study and abstracted the relevant information. Disagreement on the specific studies to be included in the analysis between the two reviewers was resolved through discussion. The data abstracted included study characteristics (author, year in which the results of the study were published, study design, treatment regimen, dose, and duration), patient characteristics (percentage of patients who were male; percentages of patients with leukemia, neutropenia, and transplantation; and mean age), treatment indication (empirical, definitive), the causative fungi (yeast, mold), sample size, efficacy outcomes, and the proportions of patients who withdrew due to adverse events and, more specifically, due to abnormal liver function test results, as well as the proportion of patients developing abnormal liver function test results but not requiring treatment discontinuation. Empirical therapy was defined as antifungal use for patients with persistent febrile neutropenia, despite ≥3 days of treatment with broad-spectrum antibiotics; definitive treatment was defined as antifungal use for proven or probable invasive aspergillosis/candidiasis on the basis of clinical, microbiological, radiological, and histopathological evidence. For each treatment arm, the number of patients who received at least one dose of an antifungal agent was used as the denominator of the cumulative incidence. Studies that did not report these safety outcome data were excluded from the analysis. Two reviewers independently evaluated the methodological quality of each study. The quality of each study was assessed for the adequacy of allocation sequence generation and concealment, the blinding of subjects and investigators to treatment assignment, and the availability of data for intention-to-treat analysis.
Statistical analysis.
Instead of evaluating relative-effect measures such as risk difference, relative risk, or odds ratio, which required the same contrast of comparison in all studies, we used absolute risk (cumulative incidence) as our outcome of interest because it was not restricted by the comparative arms and its interpretation has direct clinical meaning. As the trial designs varied considerably in terms of the dosage, treatment duration, regimen, and adherence to oral therapy, we used the beta-binomial model to account for the heterogeneity across studies and the maximum likelihood method to estimate the pooled event risks (12). From every eligible trial, we combined all treatment arms with the same antifungal agent regardless of the dosage and duration and obtained the summary estimates of cumulative incidence and their 95% confidence intervals (CIs). In the situation in which few adverse events occurred, there were only one or two studies of the treatment regimen group, or there was no significant heterogeneity, the beta-binomial distribution was collapsed to a simple binomial distribution and Wald confidence intervals were calculated (14). We used the adjusted Wald method to calculate the point estimates and 95% CIs for those risk estimates corresponding to no event (2). For rare outcomes, the lower bounds of the CIs were set to be no smaller than zero.
In every case in which we used the beta-binomial model, we used the likelihood ratio test to assess heterogeneity (30). The null hypothesis was that the distribution is binomial, while the alternative hypothesis was that the distribution is beta-binomial as a result of heterogeneity. In addition, we used Tarone's Z statistic to test for heterogeneity to corroborate the results from the likelihood ratio tests (76). This Z statistic has an asymptotic standard normal distribution under the null hypothesis of a binomial distribution.
Due to the heterogeneity among trials of antifungal therapy in terms of patient characteristics, the dosage and duration of antifungal treatment, and the concomitant use of other medications, we stratified the results by treatment indication (empirical versus definitive treatment and yeast infection versus mold infection) and calculated the pooled risks of three safety outcomes for the following treatment categories: amphotericin B formulations, amphotericin B desoxycholate and the lipid form of amphotericin B (including amphotericin B colloidal dispersion, amphotericin B lipid complex, and liposomal amphotericin B), fluconazole, itraconazole, voriconazole, and echinocandins (anidulafungin, caspofungin, micafungin).
RESULTS AND DISCUSSION
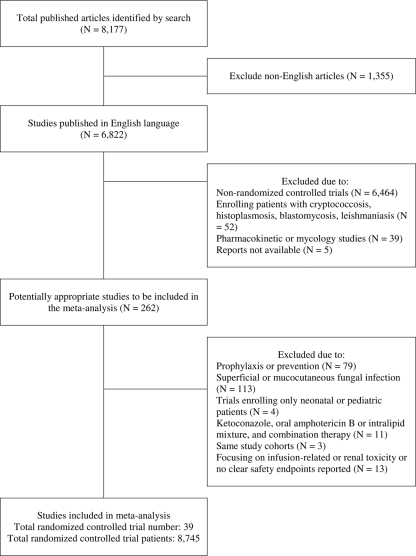
We identified 8,177 studies that reported on definitive treatment for invasive fungal infection or empirical therapy for persistent febrile neutropenia from computerized literature databases and reference lists of systematic reviews and identified articles (Fig. 1); 6,822 of them were reported in English and were retrievable for review. A total of 262 randomized trials were provisionally included for further review, after the exclusion of studies focusing on cryptococcosis, histoplasmosis, blastomycosis, and leishmaniasis; pharmacokinetic or mycology studies; pharmacological studies; and reports not available. Two internists independently reviewed all reports. The relevant safety information was reported in 39 studies that met the eligibility criteria, and those studies were included in the meta-analysis. The 39 studies were published from 1989 through 2009 and had a total of 8,745 enrolled patients, and the number of patients per study ranged from 28 to 1,111.
FIG. 1.
Literature search and selection of published reports.
These 39 randomized controlled trials were head-to-head comparisons of a variety of antifungal agents or different dosages of the same agent, and 21 studies included amphotericin B formulations as a comparative arm. The characteristics of the study regimen arms are summarized in Tables 1 and 2. Most trial reports were based on intention-to-treat analysis. Thirteen of them were double-blinded trials. The mean ages of the enrolled patients ranged from 18 to 61 years. For trials of empirical antifungal treatment and definitive therapy against invasive mold infection, substantially higher proportions of enrolled patients had neutropenia, leukemia, or transplantation compared with the proportion enrolled in trials of invasive yeast infection. The common criterion of abnormal liver function was any liver enzyme level abnormality or a liver enzyme level higher than two times the upper normal limit (UNL) after treatment, and the common criterion for the discontinuation of antifungal treatment was a liver enzyme level higher than five times the UNL.
TABLE 1.
Characteristics, study quality, and safety results of randomized controlled trials of empirical therapy for invasive antifungal infection included in the analysis
| Treatment and author, yr (reference) | Patients |
Study quality |
Regimen | Treatment duration (days) | No. of patients | % of patients with: |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Mean age (yr) | % male | % of patients with: |
Allocation generation | Allocation concealment | Double blinding | Intention to treat | Discontinuation due to adverse reaction | Discontinuation due to elevated serum transaminase level | Transaminase level elevation not requiring stopping of treatment | ||||||
| Neutropenia | Leukemia | Transplantation | |||||||||||||
| Amphotericin B formulations | |||||||||||||||
| EORTC | 39.3 | 61 | 100 | 75 | 0 | NAa | NA | No | No | Amphotericin B, 0.6 mg/kg of body weight/day | NA | 68 | 21 | 0 | 0 |
| International Antimicrobial Therapy Cooperative Group, 1989 (23) | |||||||||||||||
| No antifungal treatment | NA | 64 | 5 | 0 | 0 | ||||||||||
| Prentice et al., 1997 (62) | 21.4 | 59 | 98 | 59 | NA | NA | Adequate | No | Yes | Ambisome, 1 mg/kg/day | NA | 118 | NA | NA | 11 |
| Ambisome, 3 mg/kg/day | NA | 118 | NA | NA | 22 | ||||||||||
| Amphotericin B, 1 mg/kg/day | NA | 102 | NA | NA | 20 | ||||||||||
| Schoffski et al., 1998 (69) | 43.4 | 69 | 100 | 69 | NA | NA | NA | No | Yes | Amphotericin B, 0.75 mg/kg/day in 5% glucose | 11.3 | 24 | 0 | 0 | 21 |
| Amphotericin B, 0.75 mg/kg/day in 20% intralipid | 9.9 | 27 | 0 | 0 | 17 | ||||||||||
| Subira et al., 2004 (75) | 45.5 | 53 | 100 | 70 | 39 | NA | Adequate | No | Yes | Amphotericin B lipid complex, 1 mg/kg/day | 8 | 49 | 4 | 2 | 22 |
| Amphotericin B, 0.6 mg/kg/day | 6 | 56 | 20 | 0 | 25 | ||||||||||
| Walsh et al. 1999 (82) | 41.5 | 54 | 100 | 54 | 46 | Adequate | Adequate | Yes | Yes | Ambisome 3 mg/kg/day | 10.8 | 343 | 0 | 0 | 18 |
| Amphotericin B, 0.6 mg/kg/day | 10.3 | 344 | 0 | 0 | 20 | ||||||||||
| White et al., 1998 (87) | 36 | 62 | 100 | 27 | 69 | NA | Adequate | Yes | Yes | Amphotericin B colloidal dispersion, 4 mg/kg/day | 8 | 101 | 18 | NA | NA |
| Amphotericin B, 0.8 mg/kg/day | 7.5 | 95 | 21 | NA | NA | ||||||||||
| Wingard et al., 2000 (89) | 45 | 53 | 100 | 33 | 49 | NA | NA | Yes | Yes | Ambisome, 3 mg/kg/day | 8.6 | 85 | 13 | NA | 12 |
| Ambisome, 5 mg/kg/day | 8.3 | 81 | 12 | NA | 12 | ||||||||||
| Amphotericin B lipid complex, 5 mg/kg/day | 7.5 | 78 | 32 | NA | 12 | ||||||||||
| Azoles vs amphotericin B | |||||||||||||||
| Boogaerts et al., 2001 (6) | 48.3 | 60 | 100 | 63 | 38 | Adequate | NA | No | Yes | Itraconazole, 200 mg/day | 8.5 | 192 | 19 | 3 | 11 |
| Amphotericin B, 1 mg/kg/day | 7 | 192 | 38 | 0 | 8 | ||||||||||
| Ellis et al., 1995 (22) | 24.6 | 56 | 100 | 85 | 20 | NA | NA | Single | No | Fluconazole, 4 mg/kg/day (maximum, 400 mg/day) | NA | 16 | 0 | 0 | 6 |
| Amphotericin B, 0.5 mg/kg/day | NA | 25 | 0 | 0 | 4 | ||||||||||
| Malik et al., 1998 (46) | 33.5 | 65 | 100 | 59 | NA | NA | NA | No | Yes | Fluconazole, 400 mg/day | 7.9 | 52 | 0 | 0 | 10 |
| Amphotericin B, 0.5 mg/kg/day | 8.3 | 48 | 4 | 0 | 19 | ||||||||||
| Schuler et al., 2007 (70) | 52.5 | 69 | 100 | 73 | 42 | NA | NA | No | Yes | Itraconazole, 200 mg/day | NA | 81 | 22 | 0 | 9 |
| Amphotericin B, 0.7-1 mg/kg/day | NA | 81 | 57 | 0 | 7 | ||||||||||
| Silling et al., 1999 (72) | 46.1 | 58 | 100 | 85 | NA | NA | NA | No | Yes | Fluconazole, 5.7 mg/kg/day (maximum, 400 mg/day) | NA | 51 | 0 | 0 | NA |
| Amphotericin B, 0.75 mg/kg/day + flucytosine | NA | 47 | 0 | 0 | NA | ||||||||||
| Viscoli et al., 1996 (80) | 25.5 | 71 | 100 | 63 | 53 | Adequate | Adequate | No | Yes | Fluconazole, 6 mg/kg/day (maximum, 400 mg/day) | 13 | 56 | 0 | 0 | 18 |
| Amphotericin B, 0.8 mg/kg/day | 10 | 56 | 9 | 2 | 11 | ||||||||||
| Walsh et al., 1991 (85) | 26.5 | NA | 100 | 63 | NA | NA | NA | No | No | Ketoconazole, 800 mg/day | NA | 32 | 4 | 0 | 22 |
| Amphotericin B, 0.5 mg/kg/day | NA | 32 | 13 | 0 | 31 | ||||||||||
| Walsh et al., 2002 (84) | 45.6 | 54 | 100 | 52 | 50 | Adequate | NA | No | No | Fluconazole, 400 mg/day | 8 | 158 | 1 | 1 | 1 |
| Amphotericin B, 0.5 mg/kg/day | 10 | 159 | 7 | 1 | 1 | ||||||||||
| Winston et al., 2000 (90) | 47 | 49 | 100 | 50 | 38 | NA | NA | No | Yes | Voriconazole, 3 mg/kg every 12 h or 200 mg orally every 12 h after at least 3 days of intravenous therapy | 7 | 415 | 5 | NA | 18 |
| Ambisome, 3 mg/kg/day | 7 | 422 | 5 | NA | 23 | ||||||||||
| Echinocandins vs amphotericin B, Walsh et al., 2004 (86) | 50 | 56 | 100 | 74 | 7 | NA | NA | Yes | Yes | Caspofungin, 50 mg/day | 13.0 | 564 | 5 | NA | 9 |
| Ambisome, 3 mg/kg/day | 12.5 | 547 | 8 | NA | 12 | ||||||||||
NA, not available due to not being reported in the published literature.
TABLE 2.
Characteristics, study quality, and safety results of randomized controlled trials of definitive therapy for invasive antifungal infection included in the analysis
| Treatment and author, yr (reference) | Patients |
Study quality |
Regimen | Duration (days) | No. of patients | % of patients with: |
||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pathogena | Mean age (yr) | % male | % of patients with: |
Allocation generation | Allocation concealment | Double blinding | Intention to treat | Discontinuation due to adverse reaction | Discontinuation due to elevated serum transaminase level | Transaminase level elevation not requiring stopping of treatment | ||||||
| Neutropenia | Leukemia | Transplantation | ||||||||||||||
| Amphotericin B formulations | ||||||||||||||||
| Pachl et al., 2006 (55) | Y | 61.1 | 66 | 6 | NAb | NA | NA | NA | Yes | Yes | Ambisome, 3 mg/kg/day, or Abelcet,c 5 mg/kg/day | 10.5 | 69 | NA | NA | 4 |
| Ambisome or Abelcet plus Mycograbd | 10.0 | 68 | NA | NA | 3 | |||||||||||
| Bowden et al., 2002 (8) | M | 46 | 50 | 32 | 70 | 47 | NA | NA | Yes | Yes | Amphotericin B colloidal dispersion, 6.0 mg/kg/day | 13.0 | 88 | 23 | NA | NA |
| Amphotericin B, 1-1.5 mg/kg/day | 14.5 | 86 | 23 | NA | NA | |||||||||||
| Cornely et al., 2007 (13) | M | 50.7 | 62 | 73 | 93 | 20 | NA | NA | Yes | Yes | Ambisome, 3 mg/kg/day for 14 days and then 3 mg/kg/day | 15 | 115 | 20 | NA | 16 |
| Ambisome, 10 mg/kg/day for 14 days and then 3 mg/kg/day | 14 | 111 | 32 | NA | 14 | |||||||||||
| Ellis et al., 1998 (21) | M | 48.4 | 72 | 84 | 77 | 20 | NA | NA | No | No | Ambisome, 1 mg/kg/day | 18 | 41 | 0 | 0 | 0 |
| Ambisome, 4 mg/kg/day | 19 | 46 | 2 | 2 | 0 | |||||||||||
| Leenders et al., 1998 (42) | Y, M | 50.2 | 24 | 91 | 77 | 15 | Adequate | Adequate | No | Yes | Ambisome, 5 mg/kg/day | 13 | 52 | 6 | 2 | 17 |
| Amphotericin B, 1 mg/kg/day | 14 | 54 | 13 | 0 | 15 | |||||||||||
| Fleming et al., 2001 (26) | E, Y, M | 58 | NA | 87 | 100 | NA | Adequate | NA | No | Yes | Amphotericin B lipid complex, 3-5 mg/kg/day | 10 | 43 | 21 | NA | 37 |
| Ambisome, 3-5 mg/kg/day | 15 | 39 | 21 | NA | 56 | |||||||||||
| Nucci et al., 1999 (54) | E, Y, M | 18.1 | 75 | 82 | 74 | 10 | NA | NA | No | No | Amphotericin B, 1-1.5 mg/kg/day in 5% dextrose | NA | 33 | 0 | 0 | 0 |
| Amphotericin B, 1-1.5 mg/kg/day in intralipid | NA | 28 | 0 | 0 | 0 | |||||||||||
| Verweij et al., 1994 (79) | Y, M | 41.7 | 61 | 100 | 100 | NA | NA | NA | No | Yes | Amphotericin B, 0.5-1 mg/kg/day | 10 | 14 | 0 | 0 | 0 |
| Amphotericin B, 0.5-1 mg/kg/day, + flucytosine | 10 | 14 | 0 | 0 | 0 | |||||||||||
| Azoles vs amphotericin | ||||||||||||||||
| Abele-Horn et al., 1996 (1) | Y | 59 | 71 | 0 | NA | NA | Adequate | NA | No | Yes | Fluconazole, 200 mg/day | 14.9 | 36 | NA | NA | 25 |
| Amphotericin B, 1-1.5 mg/kg/every 2 days, + flucytosine | 15.4 | 36 | NA | NA | 19 | |||||||||||
| Anaissie et al., 1996 (3) | Y | 60.1 | 62 | 25 | 18* | 18* | Adequate | Adequate | No | Yes | Fluconazole, 400 mg/day | 9 | 80 | 1 | 1 | 3 |
| Amphotericin B, 0.67 mg/kg/day (25-50 mg/day) | 9 | 80 | 4 | 0 | 4 | |||||||||||
| Kullberg et al., 2005 (38) | Y | 53.5 | 58 | 0 | NA | NA | Adequate | Adequate | No | Yes | Voriconazole, 400 mg/day | 15 | 272 | 15 | NA | 23 |
| Amphotericin B, 0.7-1 mg/kg/day for 4 days, and then fluconazole, 400 mg/day | 15 | 131 | 7 | NA | 24 | |||||||||||
| Kujath et al., 1993 (37) | Y | 54 | 53 | 0 | NA | NA | NA | NA | No | Yes | Fluconazole, 300 mg/day | NA | 20 | 0 | 0 | 0 |
| Amphotericin B, 0.5 mg/kg/day, + flucytosine | NA | 20 | 0 | 0 | 0 | |||||||||||
| Rex et al., 1994 (64) | Y | 59 | 51 | 0 | 0 | 0 | NA | Adequate | No | No | Fluconazole, 400 mg/day | 18 | 103 | 2 | NA | 14 |
| Amphotericin B, 0.5-0.6 mg/kg/day | 17 | 103 | 3 | NA | 10 | |||||||||||
| Rex et al., 2003 (65) | Y | 56 | 51 | 0 | NA | 2 | NA | Adequate | Yes | No | Fluconazole, 800 mg/day, + placebo | 16.7 | 107 | 5 | 5 | 9 |
| Fluconazole, 800 mg/day, + amphotericin B, 0.6-0.7 mg/kg/day | 15 | 112 | 6 | 5 | 8 | |||||||||||
| van't Wout et al., 1991 (77) | Y, M | 41.5 | 50 | 100 | 85 | NA | NA | NA | No | Yes | Itraconazole, 400 mg/day | 20 | 20 | 5 | 0 | 40 |
| Amphotericin B, 0.6 mg/kg/day or 0.3 mg/kg/day, + flucytosine | 13 | 20 | 10 | 0 | 55 | |||||||||||
| Herbrecht et al., 2002 (31) | M | 49.5 | 68 | 45 | 43 | 34 | NA | NA | No | Yes | Voriconazole, 400 mg/day | 77 | 194 | NA | NA | 4 |
| Amphotericin B, 1-1.5 mg/kg/day | 10 | 185 | NA | NA | 2 | |||||||||||
| Echinocandins vs amphotericin | ||||||||||||||||
| Kuse et al., 2007 (39) | Y | 55.3 | 61 | 12 | 8 | 6 | Adequate | Adequate | Yes | Yes | Micafungin, 100 mg/day | 15 | 264 | 5 | 3 | 3 |
| Ambisome, 3 mg/kg/day | 15 | 267 | 9 | 1 | 1 | |||||||||||
| Mora-Duarte et al., 2002 (52) | Y | 55.5 | 56 | 11 | 13 | 3 | Adequate | Adequate | Yes | Yes | Caspofungin, 50 mg/day | 12.1 | 114 | 3 | NA | 8 |
| Amphotericin B, 0.6-1.0 mg/kg/day | 11.7 | 125 | 23 | NA | 15 | |||||||||||
| Echinocandins vs azoles, Reboli et al., 2007 (63) | Y | 58.1 | 51 | 3 | NA | 5 | NA | NA | Yes | Yes | Anidulafungin, 100 mg/day | 15.9 | 131 | 8 | 1 | 2 |
| Fluconazole, 400 mg/day | 14.4 | 125 | 13 | 2 | 7 | |||||||||||
| Echinocandins | ||||||||||||||||
| Krause et al., 2004 (36) | Y | 55 | 43 | 13 | NA | NA | NA | NA | No | Yes | Anidulafungin, 50 mg/day | NA | 40 | NA | NA | 3 |
| Anidulafungin, 75 mg/day | NA | 40 | NA | NA | 0 | |||||||||||
| Anidulafungin, 100 mg/day | NA | 40 | NA | NA | 5 | |||||||||||
| Pappas et al., 2007 (57) | Y | 55.9 | 58 | 9 | NA | 7 | NA | NA | Yes | Yes | Micafungin, 100 mg/day | 14 | 200 | 3 | NA | NA |
| Micafungin, 150 mg/day | 14 | 202 | 3 | NA | NA | |||||||||||
| Caspofungin, 50 mg/day | 14 | 193 | 4 | NA | NA | |||||||||||
| Betts et al., 2009 (5) | Y | 56.9 | 56 | 7 | NA | 5 | Adequate | Adequate | Yes | Yes | Caspofungin, 50 mg/day | 14.5 | 104 | 2 | 0 | 7 |
| Caspofungin, 150 mg/day | 14.2 | 100 | 2 | 0 | 2 | |||||||||||
Y, yeast; M, mold; E, empirical.
NA, not available due to not being reported in the published literature.
Abelcet is a lipid-amphotericin B complex.
Mycograb is a recombinant antibody against fungal heat shock protein 90.
There was substantial variability in the reported risk of safety outcomes among study arms receiving the same antifungal agent (Tables 1 and 2). On the basis of the beta-binomial model, the pooled risks of treatment discontinuation due to adverse reactions were above 10% for the amphotericin B formulations and itraconazole, whereas they were 2.2% to 3.8% for fluconazole, caspofungin, and micafungin (Table 3). For itraconazole and micafungin, the pooled risks of developing abnormal liver function test results requiring treatment termination were 1.5% to 2.7%, whereas they were 0.2% to 0.8% for the other antifungal agents. In addition, itraconazole and voriconazole were also associated with a higher risk of elevated serum liver enzyme levels that did not require treatment discontinuation; for those two antifungals, the pooled risks were 17.4% to 19.7%, whereas they were 2.0% to 9.3% for fluconazole and the echinocandins. Micafungin had a low pooled risk of elevated liver enzyme levels not requiring treatment discontinuation. Anidulafungin, instead, had the lowest risk of elevated serum liver enzyme levels not requiring the cessation of treatment (pooled estimated risk, 2.0%).
TABLE 3.
Pooled risk estimates of safety outcomes from randomized controlled trials of therapy against invasive fungal infection
| Drug(s) | No. of trial arms included | Total no. of patients included | % of patients with: |
|||||
|---|---|---|---|---|---|---|---|---|
| Treatment discontinuation due to adverse effects |
Elevation of liver enzyme levels requiring stopping of treatment |
Elevation of liver enzyme levels not requiring stopping of treatment |
||||||
| Pooled estimate | 95% CI | Pooled estimate | 95% CI | Pooled estimate | 95% CI | |||
| Amphotericin B formulationsa | 41 | 4,775 | 13.4 | 8.9-17.8 | 0.4 | 0.1-0.8 | 14.1 | 10.3-18.0 |
| Itraconazole | 3 | 293 | 18.8 | 14.3-23.2 | 1.5 | 0-4.0 | 17.4 | 3.9-31.0 |
| Fluconazole | 10 | 697 | 2.2 | 0-4.6 | 0.7 | 0-1.4 | 9.3 | 4.0-14.5 |
| Voriconazole | 3 | 881 | 9.5 | 2.3-16.8 | NAb | NA | 19.7 | 16.8-22.6 |
| Anidulafungin | 4 | 251 | 8.4 | 3.6-13.1 | 0.8 | 0-2.3 | 2.0 | 0.3-3.7 |
| Caspofungin | 5 | 1,075 | 3.8 | 2.7-5.0 | 0.2c | 0.1-0.4c | 7.0 | 4.1-9.9 |
| Micafungin | 3 | 666 | 3.6 | 2.2-5.0 | 2.7 | 0.7-4.6 | 3.0 | 1.0-5.1 |
Including amphotericin B desoxycholate, amphotericin B colloidal dispersion, amphotericin B lipid complex, and liposomal amphotericin B.
NA, not available.
Adjusted Wald method for point estimate and confidence interval.
Stratification of the analysis on different indications for antifungal use showed that definitive treatment was associated with a significantly higher risk of treatment discontinuation due to abnormal liver function (likelihood ratio test, P = 0.048) than empirical treatment. The pooled risk of this safety outcome was 1.3% (95% CI, 0.6%, 2.0%) for definitive treatment, whereas it was 0.5% (95% CI, 0, 0.9%) for empirical treatment (Table 4). For the other two safety outcomes, treatment discontinuation due to adverse effects and elevation of liver enzyme levels not requiring treatment termination, the definitive and empirical treatments were similar and had largely overlapping confidence intervals (P = 0.71 and P = 0.098, respectively). We also conducted an analysis stratified on the basis of different fungal infections (candidiasis versus aspergillosis). The pooled risk of treatment discontinuation due to all adverse effects was 16.5% (95% CI, 5.0%, 27.9%) for aspergillosis, which was higher than the pooled risk of 6.1% (95% CI, 3.7%, 8.5%) for candidiasis. Similarly, the risks of achieving elevated liver enzyme levels not requiring treatment termination were also higher for aspergillosis (Table 5).
TABLE 4.
Pooled risk estimates of safety outcomes from randomized controlled trials of therapy against invasive fungal infection
| Type of therapy and drug(s) | No. of trial arms included | No. of total patients included | % of patients with: |
|||||
|---|---|---|---|---|---|---|---|---|
| Treatment discontinuation due to adverse effects |
Elevation of liver enzyme levels requiring stopping of treatment |
Elevation of liver enzyme levels not requiring stopping of treatment |
||||||
| Pooled estimate | 95% CI | Pooled estimate | 95% CI | Pooled estimate | 95% CI | |||
| Empirical therapy | ||||||||
| Amphotericin B formulationsa | 23 | 3,224 | 13.9 | 7.3-20.5 | 0.2 | 0-0.6 | 14.5 | 10.5-18.5 |
| Amphotericin B deoxycholate | 13 | 1,282 | 15.4 | 5.6-25.3 | 0.2 | 0-0.4 | 13.3 | 6.8-19.9 |
| Lipid form amphotericin Bb | 10 | 1,942 | 11.2 | 3.5-18.9 | 0.7 | 0-3.2 | 16.2 | 12.9-19.4 |
| Fluconazole | 5 | 333 | 0.3 | 0-0.9 | 0.3 | 0-0.9 | 8.6 | 1.0-16.1 |
| Itraconazole | 2 | 273 | 19.8 | 15.1-24.5 | 1.9 | 0-4.5 | 10.3 | 6.7-13.9 |
| Echinocandins | 1 | 564 | 4.8 | 3.0-6.5 | NAc | NA | 8.7 | 6.4-11.0 |
| All antifungal agents | 32 | 4,809 | 11.4 | 6.3-16.5 | 0.5 | 0-0.9 | 13.3 | 10.2-16.5 |
| Definitive therapy | ||||||||
| Amphotericin B formulationsa | 18 | 1,551 | 12.7 | 7.2-18.3 | 0.9 | 0.1-1.6 | 13.5 | 6.2-20.9 |
| Amphotericin B deoxycholate | 8 | 680 | 10.0 | 2.5-17.5 | 0.3d | 0.1-0.7d | 11.0 | 3.9-18.1 |
| Lipid form amphotericin Bb | 10 | 871 | 14.9 | 7.3-22.4 | 1.2 | 0.2-2.3 | 15.7 | 3.9-27.5 |
| Fluconazole | 5 | 364 | 4.6 | 0-9.5 | 1.3 | 0-2.8 | 9.8 | 2.5-17.0 |
| Voriconazole | 2 | 466 | 14.7 | 10.5-18.9 | NA | NA | 21.5 | 17.7-25.2 |
| Echinocandins | 11 | 1,428 | 3.7 | 2.5-4.9 | 1.0 | 0-2.3 | 3.8 | 2.0-5.5 |
| All antifungal agents | 38 | 3,936 | 8.9 | 5.9-11.9 | 1.3 | 0.6-2.0 | 11.7 | 7.5-15.9 |
Including amphotericin B desoxycholate, amphotericin B colloidal dispersion, amphotericin B lipid complex, and liposomal amphotericin B.
Including amphotericin B colloidal dispersion, amphotericin B lipid complex, and liposomal amphotericin B.
NA, not available.
Adjusted Wald method for point estimate and confidence interval.
TABLE 5.
Pooled risk estimates of safety outcomes from randomized controlled trials of therapy against invasive fungal infection (aspergillosis versus candidiasis)
| Infection | Total no. of patients included | % of patients with: |
|||||
|---|---|---|---|---|---|---|---|
| Treatment discontinuation due to adverse effects |
Elevation of liver enzyme levels requiring of stopping treatment |
Elevation of liver enzyme levels not requiring stopping of treatment |
|||||
| Pooled estimate | 95% CI | Pooled estimate | 95% CI | Pooled estimate | 95% CI | ||
| Aspergillosis | 866 | 16.5 | 5.0-27.9 | 1.1 | 0-3.4 | 12.4 | 2.1-22.8 |
| Candidiasis | 2,708 | 6.1 | 3.7-8.5 | 1.1 | 0.4-1.8 | 7.2 | 4.3-10.2 |
In the auxiliary analysis, we added data from nonrandomized controlled trials and case series and cohort studies to increase the generalizability of our study results. An additional 37 reports with a total of 3,191 patients were identified and included in the planned comparison (see the references in the supplemental material). In the auxiliary analysis that added data from those studies, the safety profiles of the different antifungal regimens generally followed the same order as the results from the randomized trials (see Tables S1 and S2 in the supplemental material).
In this meta-analysis, we found, in general, that fluconazole had better hepatic safety profiles than the other antifungal agents, with the risk of abnormal liver function test results requiring or not requiring treatment termination being 0.7% and 9.3%, respectively. These findings, which are in accordance with the results from previous meta-analyses and population-based studies, suggest that fluconazole is well-tolerated and safe (9, 28). We also observed that the use of echinocandins is associated with a lower risk of liver injury. Since echinocandins and fluconazole are mostly used for the treatment of candidiasis and not aspergillosis, this may partially contribute to the low incidence of hepatic dysfunction associated with these drugs.
We found that while up to 12 to 20% of patients who received amphotericin B formulations in clinical trials stopped treatment due to all adverse reactions, less than 1% stopped treatment due to liver injury. In addition, 12 to 23% of patients who received therapy with amphotericin B formulations developed abnormal liver function test results but continued with treatment. This result was comparable to that in a prior meta-analysis, which reported that 14 to 19% of patients developed abnormal liver function test results during treatment with an amphotericin B formulation, but only less than 1% discontinued treatment due to hepatotoxicity (28). Previous studies revealed that the abnormal liver function observed during amphotericin B treatment was mild and reversible (33, 49, 83). A recent autopsy study of patients with hematological malignancies did not find direct histopathological evidence of hepatotoxicity related to amphotericin B treatment, while many cases of abnormal liver function test results during treatment were thought to be caused by underlying disease, such as tumor infiltration, fungal infection in the liver, and graft-versus-host disease (10). The pooled estimate that 12 to 23% of patients receiving amphotericin B formulations developed elevated liver enzyme levels might be interpreted as the background rate of liver injury among patients with suspected or documented invasive fungal infection.
In this study, we found that 19% of patients terminated itraconazole treatment due to an adverse reaction and 1.5% stopped due to hepatotoxicity, similar to the proportions of the high incidence of liver injury reported previously (9, 28). Furthermore, voriconazole seemed to present a higher risk of liver injury, even though voriconazole use may not lead to treatment discontinuation. The pooled risk was as high as 20% for voriconazole, whereas the pooled risks were 2 to 9% for fluconazole and the echinocandins and 12% for amphotericin B desoxycholate. In the auxiliary analysis of nonrandomized studies, voriconazole also showed a safety profile similar to that described above. The pooled risk of an elevation of liver enzyme levels requiring the cessation of treatment was as high as 11.6% for voriconazole, whereas the pooled risks ranged from 0 to 2.6% for the other antifungals. There are possible explanations for this apparent liver injury among voriconazole users. First, compared with the patients enrolled in trials of echinocandins, more of the patients enrolled in studies of voriconazole were bone marrow transplant recipients having a documented invasive fungal infection, especially aspergillosis, who were at high risk of graft-versus-host disease and who may also have been receiving concomitantly medications that were hepatotoxic. Second, compared with empirical antifungal use, studies of the activity of voriconazole against definitive mold infection had longer treatment durations and may have had more opportunities to detect liver injury. However, this increased risk of liver injury in association with voriconazole/itraconazole use still persisted even after we stratified the results according to treatment indication and especially when the risk was compared with the risk for those who received amphotericin B formulations for the same treatment indication. This finding was compatible with that of a study of Riedel and colleagues of antifungal prophylaxis in patients with neutropenia, which suggested that voriconazole had a greater risk of causing severe hepatic toxicity than either amphotericin B or fluconazole (66). Nevertheless, a comparison of the data in the literature led an FDA advisory committee to conclude that in severely ill populations, the risk of hepatotoxic reactions associated with voriconazole use is not greater than that associated with the use of other antifungal agents (61). The liver toxicity caused by voriconazole may be attributed to the dosing regimens used, the serum drug concentration, or cytochrome P450 polymorphisms (15, 17, 43, 45). Several researchers suggested that voriconazole therapeutic drug monitoring may improve treatment efficacy and safety among those with a higher risk of liver toxicity (40, 45, 48, 58). Further studies examining the association between genetic factors and plasma voriconazole concentrations are needed to identify patients at high risk of voriconazole-induced hepatotoxicity (44, 45, 48, 58).
In this study we assumed that the risks of adverse events reported in different studies varied as a function of the study attributes and that they followed a beta distribution. This assumption, plus the binomial assumption for the risk of adverse events within each study, led us to use a beta-binomial model. This parametric model captures the variation across studies but does not require the strong assumption of fixed-effect models. The beta-binomial model has been widely used to evaluate drug safety profiles, including in our prior research on oral antifungal treatments for superficial dermatophytosis and onychomycosis (11). Several limitations of our study should be considered. First, in this study we tried to combine individual study results and compare the average risks of three important safety outcomes across the trials. The treatment groups were heterogeneous in terms of the baseline risks of liver injury, despite our stratified analysis comparing homogeneous subgroups of patients with similar indications. Furthermore, monitoring of patients and the quality of reporting of the safety outcomes varied across the studies. We did not define specific cutoff values for liver enzyme levels that warranted treatment termination because different criteria were used in the different studies, and such a discrepancy reflects clinical practice. Second, studies of empirical antifungal use and the use of antifungals against definitive mold or yeast infection had different treatment durations and may have had different opportunities to detect liver injury. In the stratified analysis based on the treatment indication, we found that in comparison with empirical treatment, definitive treatment was associated with a significantly higher risk of treatment discontinuation due to an abnormal liver function but not due to the other two safety outcomes. Third, for amphotericin B-related formulations, discontinuation due to infusion-related or renal toxicity before the onset of liver toxicity may lead to underestimation of the risk of liver toxicity. Fourth, the limited data for echinocandins preclude precise estimates of the cumulative incidence of adverse events from being made.
In the auxiliary analysis we included nonrandomized trials and observational studies to evaluate antifungal safety in real clinical practice and found that the results were similar to those from randomized trials. In conclusion, in this meta-analysis of 39 randomized control trials with almost 9,000 enrolled patients with probable or documented invasive fungal infection, we found that fluconazole and echinocandins were generally associated with a lower risk of treatment termination and adverse liver events. The use of itraconazole and voriconazole was associated with a higher risk of liver injury, and users of those agents, especially those at high risk for hepatic dysfunction, need to be closely monitored during antifungal therapy.
Supplementary Material
Acknowledgments
This study was supported in part by National Institutes of Health grant RO-1 DK62322 and by the Harvard Pharmacoepidemiology Program.
Footnotes
Published ahead of print on 22 March 2010.
Supplemental material for this article may be found at http://aac.asm.org/.
REFERENCES
- 1.Abele-Horn, M., A. Kopp, U. Sternberg, A. Ohly, A. Dauber, W. Russwurm, W. Buchinger, O. Nagengast, and P. Emmerling. 1996. A randomized study comparing fluconazole with amphotericin B/5-flucytosine for the treatment of systemic Candida infections in intensive care patients. Infection 24:426-432. [DOI] [PubMed] [Google Scholar]
- 2.Agresti, A., and B. Coull. 1998. Approximate is better than ‘exact’ for interval estimation of binomial proportions. Am. Stat. 52:119-126. [Google Scholar]
- 3.Anaissie, E. J., R. O. Darouiche, D. Abi-Said, O. Uzun, J. Mera, L. O. Gentry, T. Williams, D. P. Kontoyiannis, C. L. Karl, and G. P. Bodey. 1996. Management of invasive candidal infections: results of a prospective, randomized, multicenter study of fluconazole versus amphotericin B and review of the literature. Clin. Infect. Dis. 23:964-972. [DOI] [PubMed] [Google Scholar]
- 4.Bates, D. W., L. Su, D. T. Yu, G. M. Chertow, D. L. Seger, D. R. Gomes, E. J. Dasbach, and R. Platt. 2001. Mortality and costs of acute renal failure associated with amphotericin B therapy. Clin. Infect. Dis. 32:686-693. [DOI] [PubMed] [Google Scholar]
- 5.Betts, R. F., M. Nucci, D. Talwar, M. Gareca, F. Queiroz-Telles, R. J. Bedimo, R. Herbrecht, G. Ruiz-Palacios, J. A. Young, J. W. Baddley, K. M. Strohmaier, K. A. Tucker, A. F. Taylor, and N. A. Kartsonis. 2009. A multicenter, double-blind trial of a high-dose caspofungin treatment regimen versus a standard caspofungin treatment regimen for adult patients with invasive candidiasis. Clin. Infect. Dis. 48:1676-1684. [DOI] [PubMed] [Google Scholar]
- 6.Boogaerts, M., D. J. Winston, E. J. Bow, G. Garber, A. C. Reboli, A. P. Schwarer, N. Novitzky, A. Boehme, E. Chwetzoff, and K. De Beule. 2001. Intravenous and oral itraconazole versus intravenous amphotericin B deoxycholate as empirical antifungal therapy for persistent fever in neutropenic patients with cancer who are receiving broad-spectrum antibacterial therapy. A randomized, controlled trial. Ann. Intern. Med. 135:412-422. [DOI] [PubMed] [Google Scholar]
- 7.Bow, E. J. 2008. Considerations in the approach to invasive fungal infection in patients with haematological malignancies. Br. J. Haematol. 140:133-152. [DOI] [PubMed] [Google Scholar]
- 8.Bowden, R., P. Chandrasekar, M. H. White, X. Li, L. Pietrelli, M. Gurwith, J. A. van Burik, M. Laverdiere, S. Safrin, and J. R. Wingard. 2002. A double-blind, randomized, controlled trial of amphotericin B colloidal dispersion versus amphotericin B for treatment of invasive aspergillosis in immunocompromised patients. Clin. Infect. Dis. 35:359-366. [DOI] [PubMed] [Google Scholar]
- 9.Bradbury, B. D., and S. S. Jick. 2002. Itraconazole and fluconazole and certain rare, serious adverse events. Pharmacotherapy 22:697-700. [DOI] [PubMed] [Google Scholar]
- 10.Chamilos, G., M. Luna, R. E. Lewis, R. Chemaly, I. I. Raad, and D. P. Kontoyiannis. 2007. Effects of liposomal amphotericin B versus an amphotericin B lipid complex on liver histopathology in patients with hematologic malignancies and invasive fungal infections: a retrospective, nonrandomized autopsy study. Clin. Ther. 29:1980-1986. [DOI] [PubMed] [Google Scholar]
- 11.Chang, C. H., Y. Young-Xu, T. Kurth, J. E. Orav, and A. K. Chan. 2007. The safety of oral antifungal treatments for superficial dermatophytosis and onychomycosis: a meta-analysis. Am. J. Med. 120:791-798. [DOI] [PubMed] [Google Scholar]
- 12.Chuang-Stein, C. 1993. An application of the beta-binomial model to combine and monitor medical event rates in clinical trials. Drug Infect. J. 27:515-523. [Google Scholar]
- 13.Cornely, O. A., J. Maertens, M. Bresnik, R. Ebrahimi, A. J. Ullmann, E. Bouza, C. P. Heussel, O. Lortholary, C. Rieger, A. Boehme, M. Aoun, H. A. Horst, A. Thiebaut, M. Ruhnke, D. Reichert, N. Vianelli, S. W. Krause, E. Olavarria, and R. Herbrecht. 2007. Liposomal amphotericin B as initial therapy for invasive mold infection: a randomized trial comparing a high-loading dose regimen with standard dosing (AmBiLoad trial). Clin. Infect. Dis. 44:1289-1297. [DOI] [PubMed] [Google Scholar]
- 14.Daniel, W. 1997. Probability distribution. In Biostatistics: a foundation for analysis in the health sciences, 7th ed. John Wiley & Sons, Inc., New York, NY.
- 15.den Hollander, J. G., C. van Arkel, B. J. Rijnders, P. J. Lugtenburg, S. de Marie, and M. D. Levin. 2006. Incidence of voriconazole hepatotoxicity during intravenous and oral treatment for invasive fungal infections. J. Antimicrob. Chemother. 57:1248-1250. [DOI] [PubMed] [Google Scholar]
- 16.Denning, D. W. 2003. Echinocandin antifungal drugs. Lancet 362:1142-1151. [DOI] [PubMed] [Google Scholar]
- 17.Denning, D. W., P. Ribaud, N. Milpied, D. Caillot, R. Herbrecht, E. Thiel, A. Haas, M. Ruhnke, and H. Lode. 2002. Efficacy and safety of voriconazole in the treatment of acute invasive aspergillosis. Clin. Infect. Dis. 34:563-571. [DOI] [PubMed] [Google Scholar]
- 18.Dismukes, W. E. 2006. Antifungal therapy: lessons learned over the past 27 years. Clin. Infect. Dis. 42:1289-1296. [DOI] [PubMed] [Google Scholar]
- 19.Eggimann, P., J. Garbino, and D. Pittet. 2003. Epidemiology of Candida species infections in critically ill non-immunosuppressed patients. Lancet Infect. Dis. 3:685-702. [DOI] [PubMed] [Google Scholar]
- 20.Ellis, M., A. Shamoon, W. Gorka, F. Zwaan, and B. al-Ramadi. 2001. Severe hepatic injury associated with lipid formulations of amphotericin B. Clin. Infect. Dis. 32:E87-E89. [DOI] [PubMed] [Google Scholar]
- 21.Ellis, M., D. Spence, B. de Pauw, F. Meunier, A. Marinus, L. Collette, R. Sylvester, J. Meis, M. Boogaerts, D. Selleslag, V. Krcmery, W. von Sinner, P. MacDonald, C. Doyen, and B. Vandercam. 1998. An EORTC international multicenter randomized trial (EORTC number 19923) comparing two dosages of liposomal amphotericin B for treatment of invasive aspergillosis. Clin. Infect. Dis. 27:1406-1412. [DOI] [PubMed] [Google Scholar]
- 22.Ellis, M. E., M. A. Halim, D. Spence, P. Ernst, H. Clink, M. Kalin, F. Baillie, and W. Greer. 1995. Systemic amphotericin B versus fluconazole in the management of antibiotic resistant neutropenic fever—preliminary observations from a pilot, exploratory study. J. Infect. 30:141-146. [DOI] [PubMed] [Google Scholar]
- 23.EORTC International Antimicrobial Therapy Cooperative Group. 1989. Empiric antifungal therapy in febrile granulocytopenic patients. Am. J. Med. 86:668-672. [DOI] [PubMed] [Google Scholar]
- 24.Falagas, M. E., F. Ntziora, G. I. Betsi, and G. Samonis. 2007. Caspofungin for the treatment of fungal infections: a systematic review of randomized controlled trials. Int. J. Antimicrob. Agents 29:136-143. [DOI] [PubMed] [Google Scholar]
- 25.Fischer, M. A., W. C. Winkelmayer, R. H. Rubin, and J. Avorn. 2005. The hepatotoxicity of antifungal medications in bone marrow transplant recipients. Clin. Infect. Dis. 41:301-307. [DOI] [PubMed] [Google Scholar]
- 26.Fleming, R. V., H. M. Kantarjian, R. Husni, K. Rolston, J. Lim, I. Raad, S. Pierce, J. Cortes, and E. Estey. 2001. Comparison of amphotericin B lipid complex (ABLC) vs. Ambisome in the treatment of suspected or documented fungal infections in patients with leukemia. Leuk. Lymphoma 40:511-520. [DOI] [PubMed] [Google Scholar]
- 27.Gafter-Gvili, A., L. Vidal, E. Goldberg, L. Leibovici, and M. Paul. 2008. Treatment of invasive candidal infections: systematic review and meta-analysis. Mayo Clin. Proc. 83:1011-1021. [DOI] [PubMed] [Google Scholar]
- 28.Girois, S. B., F. Chapuis, E. Decullier, and B. G. Revol. 2006. Adverse effects of antifungal therapies in invasive fungal infections: review and meta-analysis. Eur. J. Clin. Microbiol. Infect. Dis. 25:138-149. [DOI] [PubMed] [Google Scholar]
- 29.Goldberg, E., A. Gafter-Gvili, E. Robenshtok, L. Leibovici, and M. Paul. 2008. Empirical antifungal therapy for patients with neutropenia and persistent fever: systematic review and meta-analysis. Eur. J. Cancer 44:2192-2203. [DOI] [PubMed] [Google Scholar]
- 30.Guimarães, P. 2005. A simple approach to fit the beta-binomial model. Stata J. 5:385-394. [Google Scholar]
- 31.Herbrecht, R., D. W. Denning, T. F. Patterson, J. E. Bennett, R. E. Greene, J. W. Oestmann, W. V. Kern, K. A. Marr, P. Ribaud, O. Lortholary, R. Sylvester, R. H. Rubin, J. R. Wingard, P. Stark, C. Durand, D. Caillot, E. Thiel, P. H. Chandrasekar, M. R. Hodges, H. T. Schlamm, P. F. Troke, and B. de Pauw. 2002. Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N. Engl. J. Med. 347:408-415. [DOI] [PubMed] [Google Scholar]
- 32.Hughes, W. T., D. Armstrong, G. P. Bodey, E. J. Bow, A. E. Brown, T. Calandra, R. Feld, P. A. Pizzo, K. V. Rolston, J. L. Shenep, and L. S. Young. 2002. 2002 guidelines for the use of antimicrobial agents in neutropenic patients with cancer. Clin. Infect. Dis. 34:730-751. [DOI] [PubMed] [Google Scholar]
- 33.Imhof, A., R. B. Walter, and A. Schaffner. 2003. Continuous infusion of escalated doses of amphotericin B deoxycholate: an open-label observational study. Clin. Infect. Dis. 36:943-951. [DOI] [PubMed] [Google Scholar]
- 34.Jorgensen, K. J., P. C. Gotzsche, and H. K. Johansen. 2006. Voriconazole versus amphotericin B in cancer patients with neutropenia. Cochrane Database Systematic Review CD004707. [DOI] [PubMed]
- 35.Kim, H., and C. Bindslev-Jensen. 2004. Reported case of severe hepatotoxicity likely due to fluconazole and not desloratadine. Acta Haematol. 112:177-178. [DOI] [PubMed] [Google Scholar]
- 36.Krause, D. S., J. Reinhardt, J. A. Vazquez, A. Reboli, B. P. Goldstein, M. Wible, and T. Henkel. 2004. Phase 2, randomized, dose-ranging study evaluating the safety and efficacy of anidulafungin in invasive candidiasis and candidemia. Antimicrob. Agents Chemother. 48:2021-2024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kujath, P., K. Lerch, P. Kochendorfer, and C. Boos. 1993. Comparative study of the efficacy of fluconazole versus amphotericin B/flucytosine in surgical patients with systemic mycoses. Infection 21:376-382. [DOI] [PubMed] [Google Scholar]
- 38.Kullberg, B. J., J. D. Sobel, M. Ruhnke, P. G. Pappas, C. Viscoli, J. H. Rex, J. D. Cleary, E. Rubinstein, L. W. Church, J. M. Brown, H. T. Schlamm, I. T. Oborska, F. Hilton, and M. R. Hodges. 2005. Voriconazole versus a regimen of amphotericin B followed by fluconazole for candidaemia in non-neutropenic patients: a randomised non-inferiority trial. Lancet 366:1435-1442. [DOI] [PubMed] [Google Scholar]
- 39.Kuse, E. R., P. Chetchotisakd, C. A. da Cunha, M. Ruhnke, C. Barrios, D. Raghunadharao, J. S. Sekhon, A. Freire, V. Ramasubramanian, I. Demeyer, M. Nucci, A. Leelarasamee, F. Jacobs, J. Decruyenaere, D. Pittet, A. J. Ullmann, L. Ostrosky-Zeichner, O. Lortholary, S. Koblinger, H. Diekmann-Berndt, and O. A. Cornely. 2007. Micafungin versus liposomal amphotericin B for candidaemia and invasive candidosis: a phase III randomised double-blind trial. Lancet 369:1519-1527. [DOI] [PubMed] [Google Scholar]
- 40.Langman, L. J., and F. Boakye-Agyeman. 2007. Measurement of voriconazole in serum and plasma. Clin. Biochem. 40:1378-1385. [DOI] [PubMed] [Google Scholar]
- 41.Leather, H. L., and J. R. Wingard. 2002. Prophylaxis, empirical therapy, or pre-emptive therapy of fungal infections in immunocompromised patients: which is better for whom? Curr. Opin. Infect. Dis. 15:369-375. [DOI] [PubMed] [Google Scholar]
- 42.Leenders, A. C., S. Daenen, R. L. Jansen, W. C. Hop, B. Lowenberg, P. W. Wijermans, J. Cornelissen, R. Herbrecht, H. van der Lelie, H. C. Hoogsteden, H. A. Verbrugh, and S. de Marie. 1998. Liposomal amphotericin B compared with amphotericin B deoxycholate in the treatment of documented and suspected neutropenia-associated invasive fungal infections. Br. J. Haematol. 103:205-212. [DOI] [PubMed] [Google Scholar]
- 43.Levin, M. D., J. G. den Hollander, B. van der Holt, B. J. Rijnders, M. van Vliet, P. Sonneveld, and R. H. van Schaik. 2007. Hepatotoxicity of oral and intravenous voriconazole in relation to cytochrome P450 polymorphisms. J. Antimicrob. Chemother. 60:1104-1107. [DOI] [PubMed] [Google Scholar]
- 44.Lewis, R. E. 2008. What is the “therapeutic range” for voriconazole? Clin. Infect. Dis. 46:212-214. [DOI] [PubMed] [Google Scholar]
- 45.Lutsar, I., M. R. Hodges, K. Tomaszewski, P. F. Troke, and N. D. Wood. 2003. Safety of voriconazole and dose individualization. Clin. Infect. Dis. 36:1087-1088. [DOI] [PubMed] [Google Scholar]
- 46.Malik, I. A., I. Moid, Z. Aziz, S. Khan, and M. Suleman. 1998. A randomized comparison of fluconazole with amphotericin B as empiric anti-fungal agents in cancer patients with prolonged fever and neutropenia. Am. J. Med. 105:478-483. [DOI] [PubMed] [Google Scholar]
- 47.McCormack, P. L., and C. M. Perry. 2005. Caspofungin: a review of its use in the treatment of fungal infections. Drugs 65:2049-2068. [DOI] [PubMed] [Google Scholar]
- 48.Mikus, G., V. Schowel, M. Drzewinska, J. Rengelshausen, R. Ding, K. D. Riedel, J. Burhenne, J. Weiss, T. Thomsen, and W. E. Haefeli. 2006. Potent cytochrome P450 2C19 genotype-related interaction between voriconazole and the cytochrome P450 3A4 inhibitor ritonavir. Clin. Pharmacol. Ther. 80:126-135. [DOI] [PubMed] [Google Scholar]
- 49.Miller, M. A. 1984. Reversible hepatotoxicity related to amphotericin B. Can. Med. Assoc. J. 131:1245-1247. [PMC free article] [PubMed] [Google Scholar]
- 50.Mills, E. J., D. Perri, C. Cooper, J. B. Nachega, P. Wu, I. Tleyjeh, and P. Phillips. 2009. Antifungal treatment for invasive Candida infections: a mixed treatment comparison meta-analysis. Ann. Clin. Microbiol. Antimicrob. 8:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Moher, D., D. J. Cook, S. Eastwood, I. Olkin, D. Rennie, and D. F. Stroup. 1999. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Quality of Reporting of Meta-Analyses. Lancet 354:1896-1900. [DOI] [PubMed] [Google Scholar]
- 52.Mora-Duarte, J., R. Betts, C. Rotstein, A. L. Colombo, L. Thompson-Moya, J. Smietana, R. Lupinacci, C. Sable, N. Kartsonis, and J. Perfect. 2002. Comparison of caspofungin and amphotericin B for invasive candidiasis. N. Engl. J. Med. 347:2020-2029. [DOI] [PubMed] [Google Scholar]
- 53.Nivoix, Y., M. Velten, V. Letscher-Bru, A. Moghaddam, S. Natarajan-Ame, C. Fohrer, B. Lioure, K. Bilger, P. Lutun, L. Marcellin, A. Launoy, G. Freys, J. P. Bergerat, and R. Herbrecht. 2008. Factors associated with overall and attributable mortality in invasive aspergillosis. Clin. Infect. Dis. 47:1176-1184. [DOI] [PubMed] [Google Scholar]
- 54.Nucci, M., M. Loureiro, F. Silveira, A. R. Casali, L. F. Bouzas, E. Velasco, N. Spector, and W. Pulcheri. 1999. Comparison of the toxicity of amphotericin B in 5% dextrose with that of amphotericin B in fat emulsion in a randomized trial with cancer patients. Antimicrob. Agents Chemother. 43:1445-1448. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Pachl, J., P. Svoboda, F. Jacobs, K. Vandewoude, B. van der Hoven, P. Spronk, G. Masterson, M. Malbrain, M. Aoun, J. Garbino, J. Takala, L. Drgona, J. Burnie, and R. Matthews. 2006. A randomized, blinded, multicenter trial of lipid-associated amphotericin B alone versus in combination with an antibody-based inhibitor of heat shock protein 90 in patients with invasive candidiasis. Clin. Infect. Dis. 42:1404-1413. [DOI] [PubMed] [Google Scholar]
- 56.Pappas, P. G., C. A. Kauffman, D. Andes, D. K. Benjamin, Jr., T. F. Calandra, J. E. Edwards, Jr., S. G. Filler, J. F. Fisher, B. J. Kullberg, L. Ostrosky-Zeichner, A. C. Reboli, J. H. Rex, T. J. Walsh, and J. D. Sobel. 2009. Clinical practice guidelines for the management of candidiasis: 2009 update by the Infectious Diseases Society of America. Clin. Infect. Dis. 48:503-535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Pappas, P. G., C. M. Rotstein, R. F. Betts, M. Nucci, D. Talwar, J. J. De Waele, J. A. Vazquez, B. F. Dupont, D. L. Horn, L. Ostrosky-Zeichner, A. C. Reboli, B. Suh, R. Digumarti, C. Wu, L. L. Kovanda, L. J. Arnold, and D. N. Buell. 2007. Micafungin versus caspofungin for treatment of candidemia and other forms of invasive candidiasis. Clin. Infect. Dis. 45:883-893. [DOI] [PubMed] [Google Scholar]
- 58.Pascual, A., T. Calandra, S. Bolay, T. Buclin, J. Bille, and O. Marchetti. 2008. Voriconazole therapeutic drug monitoring in patients with invasive mycoses improves efficacy and safety outcomes. Clin. Infect. Dis. 46:201-211. [DOI] [PubMed] [Google Scholar]
- 59.Patterson, T. F. 2005. Advances and challenges in management of invasive mycoses. Lancet 366:1013-1025. [DOI] [PubMed] [Google Scholar]
- 60.Patterson, T. F., H. W. Boucher, R. Herbrecht, D. W. Denning, O. Lortholary, P. Ribaud, R. H. Rubin, J. R. Wingard, B. DePauw, H. T. Schlamm, P. Troke, and J. E. Bennett. 2005. Strategy of following voriconazole versus amphotericin B therapy with other licensed antifungal therapy for primary treatment of invasive aspergillosis: impact of other therapies on outcome. Clin. Infect. Dis. 41:1448-1452. [DOI] [PubMed] [Google Scholar]
- 61.Potoski, B. A., and J. Brown. 2002. The safety of voriconazole. Clin. Infect. Dis. 35:1273-1275. [DOI] [PubMed] [Google Scholar]
- 62.Prentice, H. G., I. M. Hann, R. Herbrecht, M. Aoun, S. Kvaloy, D. Catovsky, C. R. Pinkerton, S. A. Schey, F. Jacobs, A. Oakhill, R. F. Stevens, P. J. Darbyshire, and B. E. Gibson. 1997. A randomized comparison of liposomal versus conventional amphotericin B for the treatment of pyrexia of unknown origin in neutropenic patients. Br. J. Haematol. 98:711-718. [DOI] [PubMed] [Google Scholar]
- 63.Reboli, A. C., C. Rotstein, P. G. Pappas, S. W. Chapman, D. H. Kett, D. Kumar, R. Betts, M. Wible, B. P. Goldstein, J. Schranz, D. S. Krause, and T. J. Walsh. 2007. Anidulafungin versus fluconazole for invasive candidiasis. N. Engl. J. Med. 356:2472-2482. [DOI] [PubMed] [Google Scholar]
- 64.Rex, J. H., J. E. Bennett, A. M. Sugar, P. G. Pappas, C. M. van der Horst, J. E. Edwards, R. G. Washburn, W. M. Scheld, A. W. Karchmer, A. P. Dine, et al. 1994. A randomized trial comparing fluconazole with amphotericin B for the treatment of candidemia in patients without neutropenia. Candidemia Study Group and the National Institute. N. Engl. J. Med. 331:1325-1330. [DOI] [PubMed] [Google Scholar]
- 65.Rex, J. H., P. G. Pappas, A. W. Karchmer, J. Sobel, J. E. Edwards, S. Hadley, C. Brass, J. A. Vazquez, S. W. Chapman, H. W. Horowitz, M. Zervos, D. McKinsey, J. Lee, T. Babinchak, R. W. Bradsher, J. D. Cleary, D. M. Cohen, L. Danziger, M. Goldman, J. Goodman, E. Hilton, N. E. Hyslop, D. H. Kett, J. Lutz, R. H. Rubin, W. M. Scheld, M. Schuster, B. Simmons, D. K. Stein, R. G. Washburn, L. Mautner, T. C. Chu, H. Panzer, R. B. Rosenstein, and J. Booth. 2003. A randomized and blinded multicenter trial of high-dose fluconazole plus placebo versus fluconazole plus amphotericin B as therapy for candidemia and its consequences in nonneutropenic subjects. Clin. Infect. Dis. 36:1221-1228. [DOI] [PubMed] [Google Scholar]
- 66.Riedel, A., L. Choe, J. Inciardi, C. Yuen, T. Martin, and B. J. Guglielmo. 2007. Antifungal prophylaxis in chemotherapy-associated neutropenia: a retrospective, observational study. BMC Infect. Dis. 7:70. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Robenshtok, E., A. Gafter-Gvili, E. Goldberg, M. Weinberger, M. Yeshurun, L. Leibovici, and M. Paul. 2007. Antifungal prophylaxis in cancer patients after chemotherapy or hematopoietic stem-cell transplantation: systematic review and meta-analysis. J. Clin. Oncol. 25:5471-5489. [DOI] [PubMed] [Google Scholar]
- 68.Sable, C. A., K. M. Strohmaier, and J. A. Chodakewitz. 2008. Advances in antifungal therapy. Annu. Rev. Med. 59:361-379. [DOI] [PubMed] [Google Scholar]
- 69.Schoffski, P., M. Freund, R. Wunder, D. Petersen, C. H. Kohne, H. Hecker, U. Schubert, and A. Ganser. 1998. Safety and toxicity of amphotericin B in glucose 5% or intralipid 20% in neutropenic patients with pneumonia or fever of unknown origin: randomised study. BMJ 317:379-384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Schuler, U., S. Bammer, W. E. Aulitzky, C. Binder, A. Bohme, G. Egerer, M. Sandherr, R. Schwerdtfeger, G. Silling, H. Wandt, A. Glasmacher, and G. Ehninger. 2007. Safety and efficacy of itraconazole compared to amphotericin B as empirical antifungal therapy for neutropenic fever in patients with haematological malignancy. Onkologie 30:185-191. [DOI] [PubMed] [Google Scholar]
- 71.Scott, L. J., and D. Simpson. 2007. Voriconazole: a review of its use in the management of invasive fungal infections. Drugs 67:269-298. [DOI] [PubMed] [Google Scholar]
- 72.Silling, G., W. Fegeler, N. Roos, M. Essink, and T. Buchner. 1999. Early empiric antifungal therapy of infections in neutropenic patients comparing fluconazole with amphotericin B/flucytosine. Mycoses 42(Suppl. 2):101-104. [DOI] [PubMed] [Google Scholar]
- 73.Sobel, J. D., and S. G. Revankar. 2007. Echinocandins—first-choice or first-line therapy for invasive candidiasis? N. Engl. J. Med. 356:2525-2526. [DOI] [PubMed] [Google Scholar]
- 74.Song, J. C., and S. Deresinski. 2005. Hepatotoxicity of antifungal agents. Curr. Opin. Invest. Drugs 6:170-177. [PubMed] [Google Scholar]
- 75.Subira, M., R. Martino, L. Gomez, J. M. Marti, C. Estany, and J. Sierra. 2004. Low-dose amphotericin B lipid complex vs. conventional amphotericin B for empirical antifungal therapy of neutropenic fever in patients with hematologic malignancies—a randomized, controlled trial. Eur. J. Haematol. 72:342-347. [DOI] [PubMed] [Google Scholar]
- 76.Tarone, R. E. 1979. Testing the goodness of fit of the binomial distribution. Biometrika 66:585-590. [Google Scholar]
- 77.van't Wout, J. W., I. Novakova, C. A. Verhagen, W. E. Fibbe, B. E. de Pauw, and J. W. van der Meer. 1991. The efficacy of itraconazole against systemic fungal infections in neutropenic patients: a randomised comparative study with amphotericin B. J. Infect. 22:45-52. [DOI] [PubMed] [Google Scholar]
- 78.Reference deleted.
- 79.Verweij, P. E., J. P. Donnelly, B. J. Kullberg, J. F. Meis, and B. E. De Pauw. 1994. Amphotericin B versus amphotericin B plus 5-flucytosine: poor results in the treatment of proven systemic mycoses in neutropenic patients. Infection 22:81-85. [DOI] [PubMed] [Google Scholar]
- 80.Viscoli, C., E. Castagnola, M. T. Van Lint, C. Moroni, A. Garaventa, M. R. Rossi, R. Fanci, F. Menichetti, D. Caselli, M. Giacchino, and M. Congiu. 1996. Fluconazole versus amphotericin B as empirical antifungal therapy of unexplained fever in granulocytopenic cancer patients: a pragmatic, multicentre, prospective and randomised clinical trial. Eur. J. Cancer 32A:814-820. [DOI] [PubMed] [Google Scholar]
- 81.Walsh, T. J., E. J. Anaissie, D. W. Denning, R. Herbrecht, D. P. Kontoyiannis, K. A. Marr, V. A. Morrison, B. H. Segal, W. J. Steinbach, D. A. Stevens, J. A. van Burik, J. R. Wingard, and T. F. Patterson. 2008. Treatment of aspergillosis: clinical practice guidelines of the Infectious Diseases Society of America. Clin. Infect. Dis. 46:327-360. [DOI] [PubMed] [Google Scholar]
- 82.Walsh, T. J., R. W. Finberg, C. Arndt, J. Hiemenz, C. Schwartz, D. Bodensteiner, P. Pappas, N. Seibel, R. N. Greenberg, S. Dummer, M. Schuster, and J. S. Holcenberg. 1999. Liposomal amphotericin B for empirical therapy in patients with persistent fever and neutropenia. National Institute of Allergy and Infectious Diseases Mycoses Study Group. N. Engl. J. Med. 340:764-771. [DOI] [PubMed] [Google Scholar]
- 83.Walsh, T. J., J. W. Hiemenz, N. L. Seibel, J. R. Perfect, G. Horwith, L. Lee, J. L. Silber, M. J. DiNubile, A. Reboli, E. Bow, J. Lister, and E. J. Anaissie. 1998. Amphotericin B lipid complex for invasive fungal infections: analysis of safety and efficacy in 556 cases. Clin. Infect. Dis. 26:1383-1396. [DOI] [PubMed] [Google Scholar]
- 84.Walsh, T. J., P. Pappas, D. J. Winston, H. M. Lazarus, F. Petersen, J. Raffalli, S. Yanovich, P. Stiff, R. Greenberg, G. Donowitz, M. Schuster, A. Reboli, J. Wingard, C. Arndt, J. Reinhardt, S. Hadley, R. Finberg, M. Laverdiere, J. Perfect, G. Garber, G. Fioritoni, E. Anaissie, and J. Lee. 2002. Voriconazole compared with liposomal amphotericin B for empirical antifungal therapy in patients with neutropenia and persistent fever. N. Engl. J. Med. 346:225-234. [DOI] [PubMed] [Google Scholar]
- 85.Walsh, T. J., M. Rubin, J. Hathorn, J. Gress, M. Thaler, J. Skelton, J. McKnight, M. Browne, D. Marshall, D. Cotton, et al. 1991. Amphotericin B vs high-dose ketoconazole for empirical antifungal therapy among febrile, granulocytopenic cancer patients. A prospective, randomized study. Arch. Intern. Med. 151:765-770. [PubMed] [Google Scholar]
- 86.Walsh, T. J., H. Teppler, G. R. Donowitz, J. A. Maertens, L. R. Baden, A. Dmoszynska, O. A. Cornely, M. R. Bourque, R. J. Lupinacci, C. A. Sable, and B. E. dePauw. 2004. Caspofungin versus liposomal amphotericin B for empirical antifungal therapy in patients with persistent fever and neutropenia. N. Engl. J. Med. 351:1391-1402. [DOI] [PubMed] [Google Scholar]
- 87.White, M. H., R. A. Bowden, E. S. Sandler, M. L. Graham, G. A. Noskin, J. R. Wingard, M. Goldman, J. A. van Burik, A. McCabe, J. S. Lin, M. Gurwith, and C. B. Miller. 1998. Randomized, double-blind clinical trial of amphotericin B colloidal dispersion vs. amphotericin B in the empirical treatment of fever and neutropenia. Clin. Infect. Dis. 27:296-302. [DOI] [PubMed] [Google Scholar]
- 88.Wingard, J. R., and H. Leather. 2005. Hepatotoxicity associated with antifungal therapy after bone marrow transplantation. Clin. Infect. Dis. 41:308-310. [DOI] [PubMed] [Google Scholar]
- 89.Wingard, J. R., M. H. White, E. Anaissie, J. Raffalli, J. Goodman, and A. Arrieta. 2000. A randomized, double-blind comparative trial evaluating the safety of liposomal amphotericin B versus amphotericin B lipid complex in the empirical treatment of febrile neutropenia. L Amph/ABLC Collaborative Study Group. Clin. Infect. Dis. 31:1155-1163. [DOI] [PubMed] [Google Scholar]
- 90.Winston, D. J., J. W. Hathorn, M. G. Schuster, G. J. Schiller, and M. C. Territo. 2000. A multicenter, randomized trial of fluconazole versus amphotericin B for empiric antifungal therapy of febrile neutropenic patients with cancer. Am. J. Med. 108:282-289. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.