Abstract
The pathogenesis of Francisella tularensis has been associated with this bacterium's ability to replicate within macrophages. F. tularensis can also invade and replicate in a variety of nonphagocytic host cells, including lung and kidney epithelial cells and hepatocytes. As uracil biosynthesis is a central metabolic pathway usually necessary for pathogens, we characterized ΔpyrF mutants of both F. tularensis LVS and Schu S4 to investigate the role of these mutants in intracellular growth. As expected, these mutant strains were deficient in de novo pyrimidine biosynthesis and were resistant to 5-fluoroorotic acid, which is converted to a toxic product by functional PyrF. The F. tularensis ΔpyrF mutants could not replicate in primary human macrophages. The inability to replicate in macrophages suggested that the F. tularensis ΔpyrF strains would be attenuated in animal infection models. Surprisingly, these mutants retained virulence during infection of chicken embryos and in the murine model of pneumonic tularemia. We hypothesized that the F. tularensis ΔpyrF strains may replicate in cells other than macrophages to account for their virulence. In support of this, F. tularensis ΔpyrF mutants replicated in HEK-293 cells and normal human fibroblasts in vitro. Moreover, immunofluorescence microscopy showed abundant staining of wild-type and mutant bacteria in nonmacrophage cells in the lungs of infected mice. These findings indicate that replication in nonmacrophages contributes to the pathogenesis of F. tularensis.
Francisella tularensis causes the acute illness known as tularemia and is classified by the Centers for Disease Control and Prevention as a category A biodefense agent. This organism is highly infectious, as a single bacterium can lead to disease that may be fatal if untreated (16, 39, 53). The virulence of F. tularensis has been associated with this organism's ability to replicate within phagocytic cells of the innate immune system, such as macrophages (4). In the murine model of respiratory tularemia, both airway macrophages and dendritic cells are infected within 1 h following inhalation of F. tularensis (7). As this disease progresses, macrophage numbers decline (26, 63), likely due to the induction of caspase-3-dependent apoptosis induced by the virulent type A F. tularensis strain (63). During interactions with host macrophages, F. tularensis can block the activation of these cells, as evidenced by the inhibition of proinflammatory cytokine production (9, 60, 61). In addition to macrophages and dendritic cells, F. tularensis can invade and replicate in nonphagocytic host cells, such as alveolar epithelial cells, kidney epithelial cells, hepatocytes, and fibroblasts (14, 21, 25-27, 47). Although there has been recent progress on understanding the bacterial molecules that contribute to intramacrophage growth, less has been done to investigate F. tularensis growth in other cell types. And in the current paradigm of tularemia pathogenesis, F. tularensis mutants deficient in intramacrophage replication should be attenuated for virulence during animal infection.
The de novo synthesis of pyrimidines is a central metabolic pathway, as these molecules are precursors of RNA, DNA, cell membranes, and glycosylation substrates (18, 57). This pathway comprises the activity of six enzymatic reactions that culminate in the decarboxylation of orotidine-5′-phosphate to uridine-5′-monophosphate, a step mediated by the protein product of pyrF (2). Prior reports have shown that F. tularensis genes encoding homologs to enzymes mediating initial steps of pyrimidine biosynthesis, such as carAB and pyrB, are essential for intramacrophage growth (47, 56). Although F. tularensis mutants of these genes did not replicate in primary macrophages in vitro, the in vivo virulence of these strains was not detailed fully (56).
The gene encoding the ultimate enzyme of pyrimidine biosynthesis, pyrF, has not been characterized for Francisella. pyrF mutations in other bacteria lead to uracil auxotrophy and resistance to 5-fluoroorotic acid (FOA), which provides a nonantibiotic counterselectable marker useful in applied bacterial genetics (30, 45, 54, 55). A counterselectable marker would be especially beneficial when working with a category A biodefense agent, such as F. tularensis, where the choice of antibiotic selection and the cognate resistance markers are limited. An F. tularensis strain containing a deletion of pyrF may be attenuated for virulence and would also be a potential vaccine candidate.
In this report, we characterize pyrF mutant strains of both F. tularensis LVS and the fully virulent F. tularensis strain Schu S4. Using a genetic approach, we show that this gene encodes a functional orotidine-5′-phosphate decarboxylase and that its activity is critical for replication in macrophages in vitro. Although ΔpyrF mutants of both LVS and Schu S4 had similar phenotypes, we present evidence suggesting that F. tularensis Schu S4 possesses more mechanisms than LVS for silencing macrophage activation. Surprisingly, the ΔpyrF mutants were not attenuated in vivo. Furthermore, we show that intramacrophage replication is expendable during F. tularensis infection, provided that this bacterium can still replicate in nonmacrophage cells. These findings delineate the contribution of F. tularensis replication in the host's nonmacrophage cells in vivo and provide novel insight into the pathogenesis of this bacterium.
MATERIALS AND METHODS
Bacterial strains and growth conditions.
The bacterial strains used in this study are listed in Table 1. All broth cultures were grown with agitation. All cloning was conducted using Escherichia coli strain XL10-Gold or DH5α. For general cultivation of E. coli, bacteria were grown at 37°C on LB agar plates or in LB broth. For routine cultivation of F. tularensis, frozen stock cultures were streaked on chocolate II agar plates and incubated at 37°C with 5% CO2 for 1 to 4 days. These bacteria were subsequently used to inoculate cultures grown in Trypticase soy broth supplemented with 0.1% cysteine HCl (TSBc). Chamberlain's chemically defined broth medium (11) was modified by adding 2% bacteriological agar to produce a solid growth substrate (CDM). For pyrimidine auxotrophy experiments, CDM was supplemented with 400 μg/ml uracil. To confirm that the pyrimidine auxotrophy was due to a nonfunctional PyrF protein, bacteria were plated on cysteine heart broth supplemented with 5% defibrinated rabbit blood and 2% bacteriological agar (CHAB), modified with 500 μg/ml 5-fluoroorotic acid (FOA) as specified. When required, antibiotics were added to the media at the following concentrations: ampicillin (Ap) at 150 μg/ml for E. coli, kanamycin (Km) at 35 μg/ml for E. coli and 10 μg/ml for F. tularensis, polymyxin at 100 μg/ml, and hygromycin at 200 μg/ml for E. coli and F. tularensis LVS but 400 μg/ml for Schu S4. All work with F. tularensis Schu S4 and derived strains was conducted under BSL-3 conditions at the University of Pittsburgh with approval from the Centers for Disease Control and Prevention Select Agent Program.
TABLE 1.
Strains, plasmids, and primers used in this study
| Strain, plasmid, or primer | Description | Source or reference |
|---|---|---|
| Strains | ||
| F. tularensis | ||
| LVS | F. tularensis subsp. holartica live vaccine strain; type B strain | Karen Elkins |
| Schu S4 | F. tularensis subsp. tularensis; type A strain | BEI Resources |
| LVS ΔpyrF | LVS with a deletion of FTL_0045 (pyrF) | This study |
| Schu S4 ΔpyrF | Schu S4 with a deletion of FTT_1648c (pyrF) | This study |
| LVS ΔdeoB | LVS with a deletion of FTL_1664 (deoB) | 28 |
| E. coli | ||
| XL10-Gold | Δ(mcrA)183 Δ(mcrCB-hsdSMR-mrr)173 endA1 supE44 thi-1 recA1 gyrA96 relA1 lac Hte [F′ proAB lacIqZΔM15 Tn10 (Tetr) Amy Camr] | Stratagene |
| DH5α | F− φ80lacZΔM15 Δ(lacZYA-argF) U169 recA1 endA1 hsdR17 (rK− mK+) phoA supE44 λ−thi-1 gyrA96 relA1 | Invitrogen |
| SKP10 | F−recA1 endA1 gyrA96 thi hsdR17 (rK− mK+) supE44 relA1 lac trp::Tn10 pyrF287 | 64 |
| Plasmids | ||
| pFNLTP8 | Francisella shuttle plasmid; Apr Kmr | 36 |
| pGUTS | pGRP with I-SceI under the control of FGRp | 28 |
| pJH1 | pMQ225 with the I-SceI restriction site | 28 |
| pJH1ΔpyrF | pJH1 with 1-kb DNA from both the up- and downstream adjacent regions flanking the pyrF chromosomal locus | This study |
| pF8pyrFpart | pFNLTP8 with F. tularensis LVS pyrF in addition to 574 bp upstream of this gene's start codon that comprise incomplete transcription initiation sites | This study |
| pF8pyrFfull2 | pFNLTP8 with F. tularensis LVS pyrF in addition to 1,000 bp upstream of this gene's start codon that comprise the full native promoter; pyrF complementing construct | This study |
| Primers | ||
| 1pyrFclean | 5′-CATGGGATCCCAGCCAGCACCAGGTA-3′ | IDT |
| 2pyrFclean | 5′-GTCGACGGTACCACCGGTTTATTATTAACCATCTGCTGAGAA CATTATTTTC-3′ | IDT |
| 3pyrFclean | 5′-TAATAATAAACCGGTGGTACCGTCGACGAGAAGCTAAAAGA GTTTGAGTGC-3′ | IDT |
| 4pyrFclean | 5′-CATGCTGCAGTTAGATATAGAAAGTAGTGCATTAGCAATTAG-3′ | IDT |
| 1.1pyrFclean | 5′-CATTAGGGATCCGCTCCCTCTTCAACAAAGAAATC-3′ | IDT |
| 4.1pyrFclean | 5′-CATTAGCTGCAGGCCGGCAGACTATACTTATGTAATGG-3′ | IDT |
Plasmid construction.
A list of the plasmids and primers used in this study can be found in Table 1. The pyrF deletion construct pJH1ΔpyrF was generated as follows. Amplicons containing 1 kb of DNA of loci flanking F. tularensis LVS pyrF were generated by PCR using either the primer pair comprising 1pyrFclean and 2pyrFclean or the primer pair comprising 3pyrFclean and 4pyrFclean. These amplicons were TA cloned into pGEM-T (Promega) and were subsequently subcloned adjacent to one another in a single pGEM-T vector by ligating AgeI/SacI fragments containing the LVS DNA. This construct (designated pGEM3+4) was digested with BamHI/PstI, and the fragment containing the F. tularensis DNA was ligated into pJH1, which had been digested with the same enzymes, to produce pJH1ΔpyrF. This construct was used to produce both the LVS and the Schu S4 ΔpyrF mutant strains.
The pyrF-complementing construct (pF8pyrFfull2) was constructed by PCR amplification of a region of the LVS chromosome consisting of pyrF with the full native promoter (∼1 kb of upstream sequence) and the predicted transcriptional terminating sequence by using the primers 1pyrFclean and 4.1pyrFclean. This amplicon was TA cloned into pGEM-T. The BamHI/EagI fragment containing LVS DNA was ligated into pFNLTP8, which had been treated with BamHI/NotI, to produce pF8pyrFfull2. The construct containing a partial pyrF promoter (∼0.5 kb of upstream sequence; pF8pyrFpart) was constructed similarly, except the primers used here were 1.1pyrFclean and 4.1pyrFclean.
Generation of F. tularensis ΔpyrF strains.
F. tularensis ΔpyrF strains were generated by homologous recombination using pJH1ΔpyrF (28). The first recombination event resulting in integration of pJH1ΔpyrF into a locus flanking pyrF was identified following mobilization of this plasmid into F. tularensis by triparental mating conjugation. Isolated F. tularensis merodiploids were electroporated with pGUTS to force merodiploid resolution (28). I-SceI, whose coding sequence is in pGUTS, is an endonuclease that recognizes an 18-bp restriction sequence (40) in pJH1ΔpyrF that is not found in the wild-type Francisella genome. Similar systems for generating markerless deletions have been adapted for use in various bacterial species, such as E. coli and Bacillus anthracis, in addition to higher organisms, including Drosophila (13, 31, 46, 51). After transformation with pGUTS, colonies resistant to kanamycin were screened by PCR for either resolution to pyrF deletion or the wild type, using the primers 1.1pyrFclean and 4.1pyrFclean (28). All colonies producing an amplicon reduced in size by ∼580 bp also showed uracil auxotrophy and FOA resistance, further confirming a deletion of pyrF (28). Finally, to cure pGUTS, the F. tularensis ΔpyrF strains were passaged in TSBc, diluted, and plated to a density of 100 to 500 colonies per chocolate II agar petri plate. Colonies were replica plated onto chocolate II agar plates with and without kanamycin, and colonies sensitive to kanamycin were isolated and again tested for sensitivity to this antibiotic. These strains are identified as F. tularensis LVS ΔpyrF and F. tularensis Schu S4 ΔpyrF. DNA sequencing (Agencourt) confirmed that the pyrF deletion mutants resolved to maintain the initial nine codons of pyrF, followed by three stop codons (ochre) and AgeI, KpnI, and SalI restriction sites, terminating with the coding sequence for the eight C-terminal residues and the stop codon of pyrF.
Macroscopic images.
Pictures of bacteria spread on agar plates were obtained with a standard digital camera. Images of colonies were acquired using an Olympus MVX microscope. All images in each figure were rendered in grayscale, and brightness and contrast were adjusted uniformly using Microsoft Power Point.
Tissue culture and in vitro infections.
Buffy coats from blood donations (Central Blood Bank, Pittsburgh, PA) served as the source of human monocytes that were differentiated into macrophages by in vitro culture as has been detailed previously (9, 10, 27, 29, 50). For in vitro infections, primary human macrophages were washed and resuspended in Dulbecco's modified Eagle's medium (DMEM) supplemented with 1% human serum AB (complement replete; GemCell Gemini Bio-Products), 25 mM HEPES, and 1% GlutaMAX and then plated onto Primaria-coated 96-well culture dishes (Becton, Dickinson and Company) at a density of 5.0 × 104 cells per well as we have described previously (27). Use of primary human macrophages was approved by the University of Pittsburgh's Institutional Review Board.
HEK-293 cells (ATCC CRL-1573), a nonphagocytic kidney epithelial cell line (59), were cultivated in DMEM supplemented with 10% fetal bovine serum (Gibco), 25 mM HEPES, and 1% GlutaMAX with 100 U/ml penicillin-streptomycin. HEK-293 cells were passed at least once without antibiotics and seeded in 96-well plates at a concentration of 5 × 104 cells per well. Infections were carried out in this same medium without penicillin-streptomycin. Normal human dermal fibroblasts (NHDF) (adult skin; Clonetics CC-2511) were cultivated similarly to the HEK-293 cells.
We used a gentamicin protection assay (58) for in vitro infection experiments measuring intracellular growth. Here, bacteria grown in TSBc or on chocolate II agar were adjusted to an optical density at 600 nm (OD600) of 0.3 (approximately 3 × 109 CFU/ml) and diluted to attain a multiplicity of infection (MOI) of 500, which typically yields an infection rate of >80% after a 2-h coincubation (9, 34). For intracellular CFU enumeration, mammalian cells (except the NHDF cells) were exposed to the initial bacterial load for 2 h at 37°C with 5% CO2 and then incubated with gentamicin (50 μg/ml) for 30 min to kill extracellular bacteria. The uptake of F. tularensis by NHDF cells was less than other cell types for the same MOI (data not shown). To enhance the uptake, NHDF cells were incubated with bacteria for 3.5 h at the MOI of 500 prior to gentamicin treatment. All mammalian cells were washed with warm Hanks’ balanced salt solution (HBSS) and then incubated at 37°C with 5% CO2 for another 22 h with fresh culture medium. At the indicated time points postinfection, mammalian cells were lysed with 0.02% sodium dodecyl sulfate. In vitro intracellular growth assays conducted here did not extend beyond 24 h postinfection. Serial dilutions of the lysates were plated on chocolate II agar plates for enumeration of viable bacteria. CFU counts were converted to log10 values and analyzed by Student's t test to determine statistical differences.
Cytokines were measured by infecting macrophages at an MOI of 10 for 24 h, and supernatants were assayed by an enzyme-linked immunosorbent assay (ELISA) (R&D Systems). Statistical differences in cytokine production were determined using a one-way analysis of variance (ANOVA) with Dunnett's multiple comparison post hoc test.
Mean generation time (or doubling time) was calculated by using the equation g = [(log10Nt − log10N0)/log102]/22, where g is mean generation time, Nt is the number of CFU at 24 h postinfection, and N0 is the number of CFU at 2 h postinfection.
Animal infections.
Chicken embryos were infected with F. tularensis LVS, LVS ΔpyrF, LVS ΔpyrF/pF8pyrFfull2, LVS ΔpyrF/pFNLTP8, or LVS ΔdeoB as previously detailed (15, 27, 42). Briefly, 1 week-old Whiteleghorn chicken eggs (viable, fertilized, and specific pathogen free; Charles River Laboratories) were infected beneath the chorioallantoic membrane with bacteria suspended in phosphate-buffered saline (PBS). Following mechanical repair of the egg shell, infected embryos were incubated with high humidity and gentle rocking at 37°C. Eggs were candled daily to monitor viability for 7 days. As previously reported (42), embryos that expired within the initial 24 h of the infection were thought to have suffered lethal trauma during inoculation and were removed from the experiment.
Female 6- to 8-week-old C57BL/6J mice (Jackson Laboratory) were housed under ABSL-3 conditions at the University of Pittsburgh. These mice were infected intratracheally (i.t.) via oropharyngeal instillation (41). Briefly, mice that had been anesthetized with ketamine and xylazine (80 mg/kg and 8 mg/kg of body weight, respectively) were suspended by their front incisors. The animal's tongue was withdrawn with forceps, and an inoculum of 50 μl was deposited at the base of the oropharynx and was aspirated by the mouse. A subset of mice was sacrificed at 2 h postinfection, and their lungs were homogenized and plated to confirm the efficacy of bacterial delivery to pulmonary tissue. This indicated comparable rates of delivery for all strains used in the current study (data not shown). Following infection, mice were monitored twice daily for morbidity and mortality. Morbidity was measured by a nominal scale that integrated the grooming, activity, posture, and overall appearance of the mice. Mice reaching a predetermined score were sacrificed humanely and counted as dead. Survival differences in the chicken embryo or mouse infections were calculated by the log rank test (GraphPad Prism 5). All animal experiments were approved by the University of Pittsburgh's Institutional Animal Care and Use Committee.
For the analysis of the bacterial burden from organs, mice infected i.t. with ∼102 CFU were sacrificed at the indicated time points and organs were removed and homogenized in TSBc. Blood was drawn using a needle and syringe by cardiac puncture or from the inferior vena cava and heparinized to prevent coagulation. Tibias were mechanically separated from connective tissue and muscle, and 1 ml of PBS or HBSS was pushed though the bone interior with a syringe to expel the marrow. The organ homogenates, blood, and suspended marrow were diluted and plated on chocolate II agar. Following incubation at 37°C with 5% CO2 for 3 days, colonies were counted to enumerate CFU. Following conversion of values to log10, the mean numbers of CFU from two separate experiments were analyzed by a two-way ANOVA with the Bonferroni posttest (GraphPad Prism 5).
Immunofluorescence microscopy.
Mice that had been infected i.t. were sacrificed, and lungs were either first inflated with 37% formalin for 8 min or directly placed in this fixative. The lungs were placed in histology cassettes, transferred to 10% formalin, and embedded in paraffin and sectioned by the University of Pittsburgh, School of Medicine Histology Core in the Department of Pathology Development Laboratory. Glass slides containing paraffin-embedded thin sections were deparaffinized by two immersions (each for 5 min) in xylene, 100% ethanol, and 95% ethanol and two 1-min changes in 80% ethanol. The slides were subsequently rinsed with deionized water and incubated in PBS. Sections were blocked with 2.5% bovine serum albumin with 0.2% sodium azide for 20 to 30 min. Subsequently, sections were probed with the primary antibodies (rat anti-mouse F4/80 [1:50; Santa Cruz or Serotec] and rabbit anti-F. tularensis [1:500; BD]) that had been diluted in the blocking solution for at least 1 h at 4°C. Although small subsets of dendritic cells and eosinophils have been reported to express this antigen (33, 37), F4/80 has been used as a pan-macrophage marker in many laboratories (24, 38), including those used by researchers in the F. tularensis field (6, 63). The antibody isotype controls that had been used were rat IgG2b (BD Pharmingen) and normal rabbit IgG (Calbiochem) (data not shown). Slides were washed three times in PBS with 0.2% Tween 20 and were probed with secondary antibodies (Alexa Fluor 555 anti-rat immunoglobulin [Invitrogen; 1:1,000] and Alexa Fluor 488 anti-rabbit immunoglobulin [Invitrogen; 1:1,000]) that had been diluted in the blocking solution. Following three washes in PBS, the sections were stained with 0.5 μg/ml 4′,6-diamidino-2-phenylindole dihydrochloride (DAPI) (Invitrogen). The slides were washed three times in PBS and mounted in ProLong Gold antifade reagent (Invitrogen). Fluorescence microscopy was carried out using a Zeiss Axiovert 200 microscope. When images were acquired, identical settings were used for all samples. AxioVision software was used to view the captured images, merge the three colors (green, red, and blue channels), and make modifications in brightness and contrast uniformly across all images. When the high-power 63× Neofluar oil immersion objective (Zeiss) was used, an ApoTome was used to enhance contrast and increase axial resolution.
For quantification of fluorescence, three-color images of randomly selected regions of the lung sections that showed F. tularensis staining were captured. MicroSuite Basic Edition software (Olympus America, Inc.) was used to quantify the fluorescence intensity of the infected cells within these regions. Cumulative F. tularensis antigen intensity was calculated as follows. Polygons were drawn around the perimeters of the infected host cells. The total green fluorescence for the infected F4/80+ and F4/80− cells in each field was determined. To normalize each field, the green fluorescence values for infected cells were divided by the total green fluorescence value for a 5,005-square-pixel quadrilateral in a blank section of each field. Values were obtained from two independent experiments that comprised at least three mice per time point. Three separate fields with F. tularensis colonization per section were quantified. The χ2 test was used to compare the percentages of green fluorescence intensity within macrophages {[F4/80+ value/(F4/80+ value + F4/80− value)]× 100} from mice infected with Schu S4 and mice infected with Schu S4 ΔpyrF. To calculate the proportion of F. tularensis antigen intensity per μm2 of the infected host cell, the total green fluorescence value for the infected cells was divided by the total area of the host cells. To normalize, these values were divided by the value for green fluorescence intensity per unit area of the 5,005-square-pixel blank quadrilateral in each field. The χ2 test was used for comparisons of the percentages of green fluorescence intensity per μm2 within F4/80+ host cells for Schu S4 (expected) and Schu S4 ΔpyrF (observed).
RESULTS
F. tularensis pyrF encodes a functional orotidine-5′-phosphate decarboxylase.
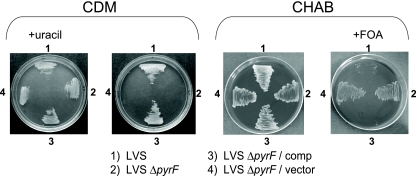
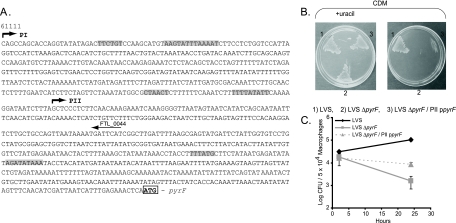
To investigate pyrimidine biosynthesis, pyrF, and intracellular growth, deletions of pyrF in both F. tularensis LVS and Schu S4 (FTL_0045 and FTT_1648c, respectively) were made using two-step allelic replacement. ΔpyrF strains should be pyrimidine auxotrophs and therefore fail to grow on a chemically defined medium lacking a pyrimidine source. To test this, we spread F. tularensis LVS and LVS ΔpyrF strains on CDM with or without uracil (Fig. 1). This clearly showed that the pyrF mutant was auxotrophic for uracil, indicating a deficiency in de novo pyrimidine biosynthesis (Fig. 1). To confirm that this uracil auxotrophy was specifically attributed to the absence of pyrF and not to any polar effects that may have occurred as a result of the mutagenesis, we introduced a trans-complementing construct (pF8pyrFfull2) into LVS ΔpyrF. This vector contained an intact copy of pyrFLVS under the control of this gene's native promoter. As a control, the empty Francisella shuttle vector (pFNLTP8) was transformed into LVS ΔpyrF, and these strains were cultivated on CDM with or without uracil (Fig. 1). Because introduction of pF8pyrFfull2, but not pFNLTP8, complemented the uracil auxotrophy, we conclude that the deficiency in de novo pyrimidine biosynthesis observed by LVS ΔpyrF can be directly attributed to the absence of pyrF. An alternative construct was generated as an added control. pF8pyrFpart contained all of pyrF but only one of the three predicted promoters upstream (Fig. 2A). This construct provided only partial uracil protrophy to LVS ΔpyrF relative to pF8pyrFfull2 (Fig. 1 and 2B). The identical phenotypes were observed with the cognate F. tularensis Schu S4 strains (data not shown), suggesting that uracil and pyrimidine biosynthesis is conserved with respect to pyrF among francisellae.
FIG. 1.
F. tularensis ΔpyrF mutants are uracil auxotrophs and resistant to FOA. LVS strains were spread onto CDM with or without uracil (left) or on CHAB with or without FOA (right). The abbreviation “comp” refers to the complementing construct, pF8pyrFfull2, and “vector” designates the empty shuttle plasmid, pFNLTP8. Similar results were observed with the cognate F. tularensis Schu S4 strains (not shown). Images shown are representative of at least four independent experiments.
FIG. 2.
Promoter characterization of F. tularensis pyrF. (A) Genomic arrangement of pyrF where the three predicted −10 and −35 promoter regions are shaded (BPROM; www.softberry.ru). The start codon of pyrF is boxed and in boldface type. (B) The indicated bacterial strains were spread onto CDM with or without uracil. The plasmid PII ppyrF refers to the construct pF8pyrFpart, and “vector” designates the empty shuttle plasmid, pFNLTP8. PII ppyrF contains sequence up to the site designated PII (A). The fully complementing vector (not shown in this figure) contains coding sequence up to the PI site. (C) Macrophages were infected with the designated strains (MOI, 500) using a gentamicin protection assay. Macrophages were lysed at the indicated time points, and lysates were diluted and plated to enumerate intracellular CFU. Data shown are means ± standard errors of the means (SEM) of results from triplicate wells within one experiment.
Wild-type organisms, or bacteria with a functional PyrF protein, are unable to be cultivated on medium containing the pyrimidine analog 5-fluoroorotic acid (FOA). Here, the orotidine-5′-phosphate decarboxylase activity of PyrF results in the conversion of FOA to a toxic product (5). Conversely, pyrF mutants grow normally in the presence of FOA on rich medium. As expected, wild-type LVS, and the trans-complemented LVS ΔpyrF strain could not grow on CHAB agar containing FOA (Fig. 1). In contrast, the LVS ΔpyrF strains and the ΔpyrF strain containing the empty shuttle vector grew on the medium containing FOA (Fig. 1). Again, identical phenotypes were observed with the corresponding Schu S4 strains (data not shown). This provides further evidence that pyrF of F. tularensis LVS and Schu S4 each encode a functional orotidine-5′-phosphate decarboxylase.
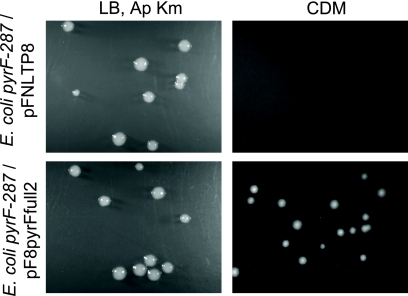
To confirm that the F. tularensis pyrF gene encodes a bona fide orotidine-5′-phosphate decarboxylase, we expressed this gene in an E. coli strain containing a mutated pyrF gene (strain SKP10, containing pyrF287 [64]). Here, E. coli pyrF287 was transformed with the pyrFLVS-complementing construct (pF8pyrFfull2) or the empty shuttle vector (pFNLTP8). We observed similar transformation efficiencies for E. coli pyrF287 with pFNLTP8 and pF8pyrFfull2, as evidenced by comparable counts of colonies on LB agar plates supplemented with Ap and Km (Fig. 3). However, only the E. coli pyrF287/pF8pyrFfull2 strain formed colonies on CDM agar, indicating that the F. tularensis pyrF strain complemented this strain's uracil auxotrophy (Fig. 3). This heterologous complementation verifies that the F. tularensis PyrF protein functions as an orotidine-5′-phosphate decarboxylase.
FIG. 3.
Heterologous expression of F. tularensis pyrF rescues the uracil auxotrophy of E. coli SKP10. E. coli SKP10 (pyrF287) was transformed with pF8pyrFfull2 (carrying pyrFLVS) or pFNLTP8 (empty vector) and was plated on LB supplemented with ampicillin (Ap) and kanamycin (Km) or on CDM. This experiment was performed on two separate occasions, with similar results.
F. tularensis pyrF is required for intramacrophage replication.
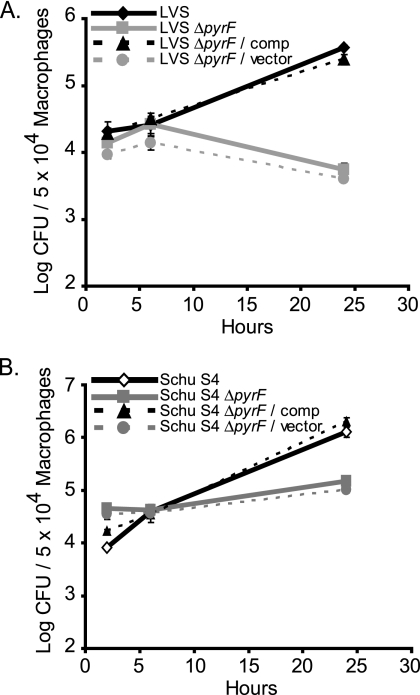
Pyrimidine anabolism is a central metabolic pathway. We hypothesized that the LVS and Schu S4 ΔpyrF strains would therefore be attenuated for pathogenesis. To test this, primary human monocyte-derived macrophages were infected with F. tularensis LVS and LVS ΔpyrF in vitro because intramacrophage growth is traditionally associated with F. tularensis virulence. At various time points, the macrophages were lysed, and the lysates were diluted and plated for enumeration of viable CFU. We observed a reduction in intracellular LVS ΔpyrF bacteria in macrophages at 24 h postinfection relative to the levels observed at earlier time points (Fig. 4A). Upon complementation of LVS ΔpyrF in trans, the wild-type level of growth was restored (Fig. 4A). In addition, the LVS ΔpyrF strain containing the empty vector showed a level of attenuation for growth similar to that observed for the LVS ΔpyrF strain (Fig. 4A). Expression of the vector containing the truncated pyrF promoter (pF8pyrFpart) in LVS ΔpyrF resulted in an incomplete complementation for replication in macrophages (Fig. 2C), a result consistent with the partial rescuing of the uracil auxotrophy (Fig. 2B). These results confirmed that the reduced intracellular fitness of LVS ΔpyrF was due specifically to the absence of pyrF and not attributable to polar effects or unknown mutations.
FIG. 4.
F. tularensis ΔpyrF mutants do not replicate in primary human macrophages. Macrophages were infected with the designated LVS (A) or Schu S4 (B) strains (MOI, 500) using a gentamicin protection assay. Macrophages were lysed at the indicated time points, and lysates were diluted and plated to enumerate intracellular CFU. Data shown are means ± SEM of results from triplicate wells within one experiment and are representative of three or four experiments performed using cells from separate donors. The number of viable Schu S4 ΔpyrF CFU seen after 24 h in this experiment was the most among the experiments conducted; other experiments showed a decline in Schu S4 ΔpyrF numbers similar to that observed for LVS ΔpyrF (data not shown). The abbreviation “comp” refers to the complementing construct, pF8pyrFfull2, and “vector” designates the empty shuttle plasmid, pFNLTP8. For growth in macrophages at 24 h, P was <0.001 for LVS versus LVS ΔpyrF, and P was <0.001 for Schu S4 versus Schu S4 ΔpyrF.
We conducted a similar experiment with the virulent F. tularensis Schu S4 strain (Fig. 4B). Here, primary human macrophages were infected with F. tularensis Schu S4, Schu S4 ΔpyrF, the trans-complemented Schu S4 ΔpyrF strain, or Schu S4 ΔpyrF containing the empty vector. Both wild-type Schu S4 and the trans-complemented Schu S4 ΔpyrF strain showed exponential intramacrophage growth, whereas Schu S4 ΔpyrF and Schu S4 ΔpyrF containing the empty vector exhibited no substantial growth (Fig. 4B). In additional experiments using human monocyte-derived macrophages from different donors, the numbers of viable Schu S4 ΔpyrF bacteria declined similarly to those of LVS ΔpyrF bacteria (data not shown). These data show that pyrF is required for intramacrophage replication in model strains of F. tularensis.
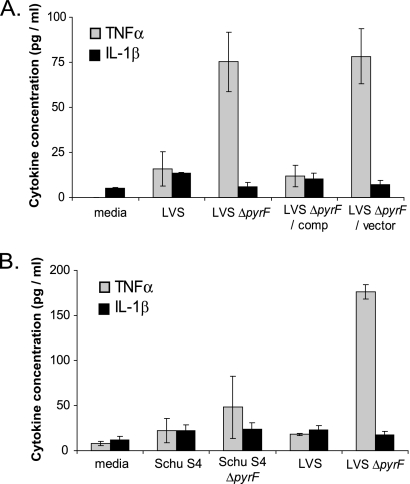
Both F. tularensis LVS and Schu S4 have been shown to suppress the production of proinflammatory cytokines by macrophages and dendritic cells (7, 9, 12, 60, 61). Because of the intramacrophage growth defect, we hypothesized that the ΔpyrF mutants would enhance cytokine production from infected macrophages in comparison to the level for the wild type. Macrophages infected with F. tularensis LVS ΔpyrF secreted significantly higher levels of tumor necrosis factor alpha (TNF-α) than those infected with wild-type LVS (Fig. 5A). Expression of the complementing plasmid restored wild-type levels of TNF-α induction to the LVS ΔpyrF strain, whereas expression of the empty vector alone resulted in maintenance of high levels of cytokine production from host cells (Fig. 5A). The reduction in viable LVS ΔpyrF bacteria observed in Fig. 4A was therefore associated with heightened macrophage response, suggesting that this strain also lost its ability to silence macrophage activation (7, 9, 12, 60, 61). Although we observed an increase in the production of TNF-α from macrophages infected with LVS ΔpyrF, the levels of another proinflammatory cytokine, interleukin-1β (IL-1β), were similar across all groups (Fig. 5A).
FIG. 5.
F. tularensis LVS ΔpyrF, but not Schu S4 ΔpyrF, stimulates primary macrophages to produce the proinflammatory cytokine TNF-α. Data are depicted as mean ± SEM levels of TNF-α and IL-1β secretion by primary human macrophages following a 24-h culture with the indicated strains (MOI, 10). Each panel represents a combination of three individual experiments using cells from separate blood donors. For panel B, LVS and LVS ΔpyrF were included in a single experiment for comparison. Uninfected control wells contained macrophages with no bacteria added (media). For TNF-α in panel A, P was <0.05 for LVS versus LVS ΔpyrF; for TNF-α in panel B, P was >0.05 for Schu S4 versus Schu S4 ΔpyrF.
We also assessed cytokine production by human macrophages infected with the wild type and with Schu S4 ΔpyrF (Fig. 5B). In these experiments, we included LVS and LVS ΔpyrF as positive and negative controls for TNF-α secretion (Fig. 5B). In contrast to LVS ΔpyrF, the Schu S4 ΔpyrF strain did not induce significantly higher levels of TNF-α production from human macrophages (Fig. 5B). Similarly to LVS, there was no difference in the IL-1β responses to these Schu S4 strains. The contrasting patterns of TNF-α release suggest that F. tularensis Schu S4 has additional mechanisms for silencing macrophages in comparison to LVS.
F. tularensis ΔpyrF strains retain in vivo virulence.
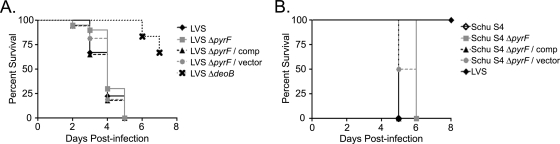
The ability of F. tularensis to replicate within a macrophage is closely associated with this organism's capability to cause disease in an animal (4). Therefore, we expected that the ΔpyrF strains of both LVS and Schu S4 would be sharply attenuated for virulence during animal infection. To test this with LVS, we employed the chicken embryo infection model (15, 27, 42, 62). Here, each chicken embryo was infected with ∼103, ∼105, or ∼107 bacteria (Fig. 6A). Surprisingly, the LVS ΔpyrF mutant was virulent and resulted in the death of the chicken embryo, similar to what was found for the wild type, in all three experiments (Fig. 6A). Also, the chicken embryos infected with LVS ΔpyrF harboring either the complementing plasmid or the empty shuttle vector did not show a substantial difference in survival rate compared to the level for the wild type (Fig. 6A). As controls, chicken embryos were treated with PBS or LVS ΔdeoB, since a functional deoB gene is required for F. tularensis pathogenesis in this model (27). All of the chicken embryos treated with PBS survived the duration of the experiment (data not shown). Furthermore, chicken embryos infected with LVS ΔdeoB exhibited significant survival compared to those infected with LVS or LVS ΔpyrF (Fig. 5A). This indicates that the mortality of the chicken embryos infected with LVS and LVS ΔpyrF was directly attributable to the virulence of these strains and not to nonspecific inflammation or procedural trauma.
FIG. 6.
F. tularensis ΔpyrF mutants retain virulence in animal models of infection. Chicken embryos (A) or mice (B) were infected with the indicated strains. Data represent a combination of 3 (A) or 2 (B) experiments and are shown as Kaplan-Meier survival curves depicting percent survival over time. (A) Chicken embryos were infected with ∼103, ∼105, or ∼107 CFU. All bacterial strains were used to infect chicken embryos in three experiments except LVS ΔdeoB, which was used in only one trial. Twenty embryos were used for LVS ΔpyrF, 16 for LVS ΔpyrF/pF8pyrFfull2 (comp), 16 for LVS ΔpyrF/pFNLTP8 (vector), and 6 for LVS ΔdeoB. For each experiment, the actual numbers of CFU administered to the chicken embryos were as follows: for LVS, 8.0 × 102, 2.8 × 105, and 5.0 × 107; for LVS ΔpyrF, 1.6 × 103, 9.0 × 104, and 1.2 × 107; for LVS ΔpyrF/comp, 1.1 × 103, 1.8 × 105, and 4.6 × 107; for ΔpyrF/vector, 6.2 × 102, 2.6 × 105, and 1.7 × 107; and for LVS ΔdeoB, 2.5 × 102. P was <0.0001 for LVS versus LVS ΔdeoB. (B) Mice were infected (i.t.) with ∼101 or ∼103 CFU of each strain. Ten mice (two experiments) were used for each infecting strain except LVS, for which five mice (included in only one experiment) were used. For each experiment, the actual numbers of CFU administered to mice were as follows: for Schu S4, 37 and 350; for Schu S4 ΔpyrF, 14 and 500; for Schu S4 ΔpyrF/comp, 19 and 250; for Schu S4 ΔpyrF/vector, 49 and 850; and for LVS, 850. A subset of mice was sacrificed at 2 h postinfection, and their lungs were homogenized and plated to confirm the efficacy of bacterial delivery to pulmonary tissue, which indicated comparable rates of delivery for all strains (not shown). P was 0.0002 for LVS versus Schu S4 ΔpyrF; P was <0.0001 for Schu S4 versus Schu S4 ΔpyrF.
To test the virulence of the F. tularensis Schu S4 ΔpyrF strain, we conducted two experiments where mice were infected i.t. with ∼101 or ∼103 bacteria (Fig. 6B). Here, LVS was used as a control, as it is not lethal to mice in the dose and time frame tested (Fig. 6B). In each experiment, infection with Schu S4, Schu S4 ΔpyrF, Schu S4 ΔpyrF/pF8pyrFfull2, and Schu S4 ΔpyrF/pFNLTP8 all resulted in 100% mortality by day 6, whereas the control mice (LVS-infected) survived (Fig. 6B). To ensure that Schu S4 ΔpyrF did not repair its pyrimidine biosynthesis machinery during infection, bacteria were recovered from tissues of mice infected with this strain after euthanasia. These bacteria were patched onto CDM with or without uracil and CHAB with or without FOA. All bacteria tested were uracil auxotrophs and resistant to FOA, indicating that the deletion of pyrF and the associated phenotypes were maintained during infection. The F. tularensis ΔpyrF strains characterized here are the first examples of mutants of this organism that cannot replicate in macrophages in vitro but are still virulent in vivo. This may suggest that a significant portion of the pathogenesis of F. tularensis is independent of replication within macrophages.
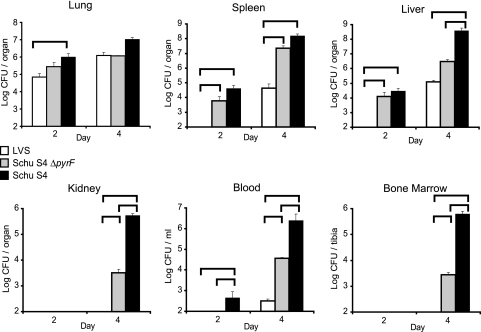
To examine further the in vivo pathogenesis of F. tularensis Schu S4 ΔpyrF, we measured the bacterial burden from organs and tissues of mice sacrificed at days 2 and 4 postinfection in a respiratory tularemia model (Fig. 7). Mice were infected i.t. with ∼102 CFU of F. tularensis Schu S4, Schu S4 ΔpyrF, or LVS, and organs were harvested for CFU at the indicated time points (Fig. 7). As expected, CFU data suggest that wild-type Schu S4 grew and disseminated more rapidly than LVS (Fig. 7). In addition, the bacterial burden associated with Schu S4 ΔpyrF in the extrapulmonary tissues was substantially higher, in general, than that of LVS (Fig. 7). High bacterial burdens of the Schu S4 and Schu S4 ΔpyrF strains were also found in the spleens and the livers at 2 days postinfection (Fig. 7). Similarly, the Schu S4 strains were readily detected in the kidneys, blood, and bone marrow at 4 days postinfection (Fig. 7).
FIG. 7.
F. tularensis Schu S4 ΔpyrF exhibits dissemination to peripheral organs in a murine respiratory tularemia model. Mice were infected (i.t.) with ∼102 CFU of F. tularensis Schu S4, Schu S4 ΔpyrF, or LVS. The average numbers of CFU administered to mice over both experiments were as follows: for Schu S4, 200; for Schu S4 ΔpyrF, 190; and for LVS, 140. A subset of mice was sacrificed at 2 h postinfection, and their lungs were homogenized and plated to confirm the efficacy of bacterial delivery to pulmonary tissue, which indicated comparable rates of delivery for all strains (not shown). At day 2 or 4 postinfection, mice were sacrificed and the designated organs and tissues were harvested, homogenized, diluted, and plated for CFU enumeration. The limit of detection was 100 CFU per organ (or per ml blood), except the liver, which was 200 CFU. Data, displayed as mean numbers of CFU ± SEM, represent a combination of two independent experiments, each having three mice per bacterial strain per time point. The comparisons in which P was <0.05 are designated by brackets.
The spatial distribution of Schu S4 ΔpyrF CFU also differed from that of wild-type CFU in some instances (Fig. 7). This may suggest an impaired fitness in particular cell types, such as macrophages, that occupy these tissues. Although the total numbers of Schu S4 ΔpyrF bacteria were less than the numbers of wild-type bacteria in some tissues (Fig. 7), the numbers of mutant bacteria appear sufficient for these bacteria to be pathogenic (Fig. 6B).
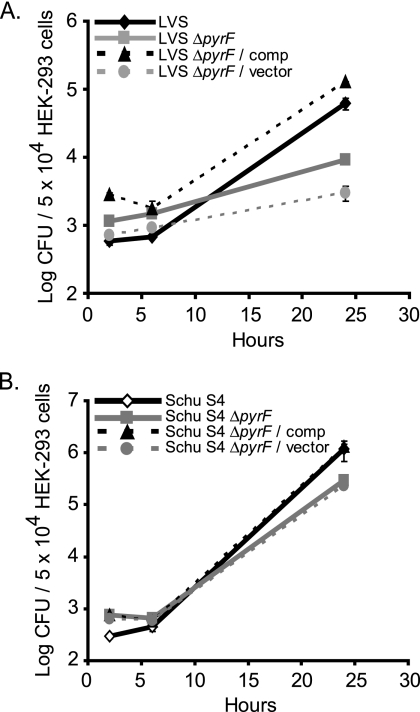
F. tularensis ΔpyrF strains replicate in nonmacrophage host cells.
Although the F. tularensis ΔpyrF strains were unable to replicate in macrophages in vitro, we hypothesized that these cells may still be able to grow in nonmacrophages because of the high CFU burdens observed in vivo. If this hypothesis was true, then growth in nonmacrophage host cells could explain a mechanism by which these pyrF mutants remained virulent and invaded peripheral organs. Because the Schu S4 ΔpyrF strain was able to invade the kidney (Fig. 7), we used a human kidney epithelial cell line (HEK-293) to test our hypothesis. Moreover, F. tularensis is often isolated or identified in kidney tissues during natural animal infection (1, 35). In contrast to the results obtained with macrophages (Fig. 4), the ΔpyrF mutants of LVS and Schu S4 retained the ability to replicate in HEK-293 cells, albeit at a slightly lower rate than the wild type (Fig. 8A and B).
FIG. 8.
F. tularensis ΔpyrF mutants retain the ability to replicate in nonmacrophages. HEK-293 cells were infected with the designated LVS (A) or Schu S4 (B) strains (MOI, 500) using a gentamicin protection assay. HEK-293 cells were lysed at the indicated time points, and the lysates were diluted and plated to enumerate intracellular CFU. Data shown are means ± SEM of results from triplicate wells within one experiment and are representative of at least three independent experiments. The abbreviations are the same as those in Fig. 4. For growth in HEK-293 cells at 24 h, P was 0.0083 for LVS versus LVS ΔpyrF, and P was 0.076 for Schu S4 versus Schu S4 ΔpyrF.
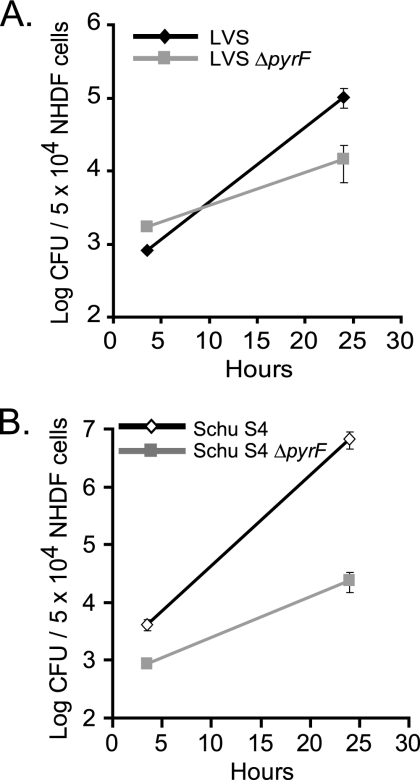
As an alternative to HEK-293 cells, we conducted an intracellular growth assay using normal human dermal fibroblasts (NHDF). Similarly to the HEK-293 cells, the ΔpyrF mutants of LVS (Fig. 9A) and Schu S4 (Fig. 9B) grew in NHDF cells at a slightly lower rate than the cognate wild-type strains.
FIG. 9.
F. tularensis ΔpyrF mutants retain the ability to replicate in normal fibroblasts. NHDF cells were infected with the designated LVS (A) or Schu S4 (B) strains (MOI, 500) using a gentamicin protection assay. NHDF cells were lysed at the indicated times, and the lysates were diluted and plated to enumerate CFU. Data shown are means ± SEM of results from triplicate wells within one experiment and are representative of at least three independent experiments. The abbreviations are the same as those in Fig. 4.
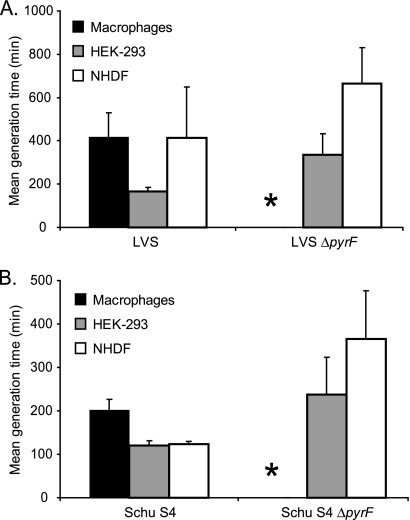
These results are more clearly illustrated by examining the mean generation times of these F. tularensis strains in macrophages, HEK-293 cells, and NHDF cells (Fig. 10A and B). For wild-type LVS and Schu S4, the growth rates in the nonmacrophage cells (HEK-293 and NHDF) were at least as high, and generally higher, than those in macrophages. The numbers of ΔpyrF bacteria do not increase in macrophages, and therefore, the generation time is not measurable (asterisk in Fig. 10A). However, both ΔpyrF mutants can replicate in the nonmacrophage cells (Fig. 10A). This suggests that the F. tularensis ΔpyrF mutants retained virulence due to their ability to replicate in nonmacrophage cells of the host. Therefore, intramacrophage growth may be expendable for virulence, provided that F. tularensis can still replicate in other cells.
FIG. 10.
Intracellular growth rate of wild-type F. tularensis and ΔpyrF mutants. Mean generation time (± SEM) was calculated for bacterial replication in primary human macrophages, HEK-293 cells, or NHDF cells from at least three combined independent experiments. Panel A shows the mean generation time comparison of LVS and LVS ΔpyrF, and panel B depicts the Schu S4 and Schu S4 ΔpyrF data. For both panels, the generation time of the ΔpyrF strains in macrophages could not be calculated, because the mean numbers of viable CFU across experiments were lower at 24 h than at 2 h postinfection (asterisk).
More F. tularensis Schu S4 ΔpyrF bacteria are associated with nonmacrophages than macrophages in infected lungs.
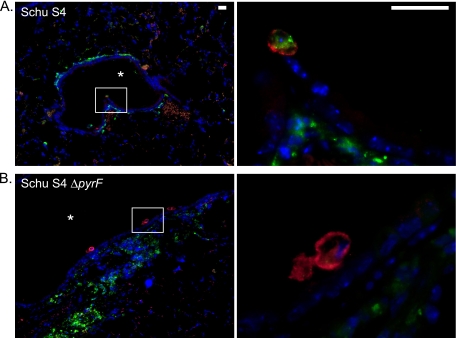
The in vitro data presented above (Fig. 4B, 8B, and 10B) suggest that F. tularensis Schu S4 ΔpyrF cannot replicate in macrophages but is capable of multiplying in nonmacrophages. We hypothesized that abundant bacteria, both wild-type and ΔpyrF mutant Schu S4, would be found in nonmacrophages in vivo. Therefore, we localized bacteria using immunofluorescence microscopy on lung sections from infected mice. Tissue sections were probed with antibodies specific for F. tularensis and F4/80, a macrophage lineage marker. Fluorescent secondary antibodies were used to visualize macrophages (F4/80+) in red and F. tularensis in green. Nuclei were stained blue with DAPI (Fig. 11). In regions of the lung that had been colonized by bacteria, we observed abundant staining for wild-type Schu S4 in both F4/80+ and F4/80− cells on both day 2 (data not shown) and day 4 (Fig. 11A) postinfection. In contrast, we consistently observed much less bacterial staining within F4/80+ cells in lungs of mice infected with F. tularensis Schu S4 ΔpyrF (Fig. 11B). Intense bacterial staining was still observed, however, in F4/80− cells in lungs from mice that had been infected with the mutant strain (Fig. 11B). These data are consistent with the hypothesis that although F. tularensis Schu S4 ΔpyrF has reduced fitness within host macrophages, it remains virulent by replicating in nonmacrophages.
FIG. 11.
Immunofluorescence microscopy of lung sections from mice infected with F. tularensis Schu S4 or Schu S4 ΔpyrF. Mice were infected i.t. as described in the legend to Fig. 7. On day 4 postinfection, lungs were harvested from mice infected with Schu S4 (A) or Schu S4 ΔpyrF (B), were fixed in formalin, and were subsequently embedded in paraffin. Deparaffinized lung sections were probed with rat anti-mouse F4/80 to detect macrophages and with rabbit anti-F. tularensis. The secondary antibodies used were Alexa Fluor 555 goat anti-rat immunoglobulin and Alexa Fluor 488 donkey anti-rabbit immunoglobulin. DNA was stained with DAPI. For both panels, the color images represent a three-color merge (red, F4/80; green, F. tularensis; and blue, DAPI). The first color image represents low-power magnification, and the second image is a high-power magnification of the boxed section. In the low-power images, the asterisk designates a major airway. The scale bars in the upper right hand corners of the images in panel A represent a length of 20 μm.
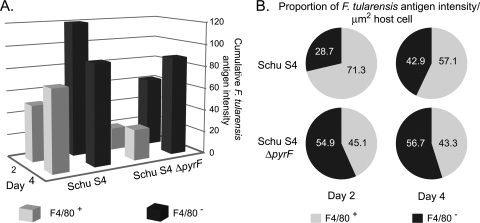
Quantification of bacteria associated with either F4/80+ or F4/80− cells supported the observation depicted in Fig. 11. There was significantly more bacterial antigen present in F4/80+ cells in lungs of mice infected with F. tularensis Schu S4 than in those in lungs of mice infected with the ΔpyrF strain (Fig. 12A). In addition, the level of change of staining in F4/80+ cells over the measured interval was 3-fold higher for the wild type than for the ΔpyrF mutant (Fig. 12A), consistent with greater wild-type proliferation in the F4/80+ cells. However, bacterial antigen intensities were comparable in F4/80− cells between Schu S4 and Schu S4 ΔpyrF, especially on day 4 postinfection (Fig. 12A). The change of Schu S4 ΔpyrF staining in F4/80− cells was 3.5-fold greater than that in the F4/80+ cells over the time interval, further indicating that this mutant proliferates better in nonmacrophages than in macrophages. Similar findings were obtained by measuring the mean bacterial fluorescence intensity per unit area of the host cell (Fig. 12B). This analysis normalized the fluorescence intensity to the area of the infected host cells to minimize any overrepresentation of bacteria by disparities in the infected cell size or host cell number in a given field. Using this analysis, we found a greater proportion of Schu S4 ΔpyrF bacteria localized to the F4/80− population at both 2 and 4 days after infection (Fig. 12B). In contrast, the antigen intensity of wild-type Schu S4 was significantly more abundant in F4/80+ cells both 2 and 4 days after infection (Fig. 12B). These results corroborate the in vitro data and are consistent with the hypothesis that the Schu S4 ΔpyrF strain replicates in nonmacrophages in vivo, although it is attenuated in macrophages. Collectively, the data indicate that replication in nonmacrophages is sufficient for in vivo pathogenesis of F. tularensis.
FIG. 12.
Quantification of Schu S4 and ΔpyrF mutant staining during pulmonary infection. Lung sections from mice infected with Schu S4 and Schu S4 ΔpyrF were harvested at day 2 or 4 postinfection. F. tularensis fluorescence (green) was quantified from infected F4/80+ and F4/80− cells using MicroSuite Basic Edition software. Data shown are from two independent infections and comprise at least three mice per time point. Fluorescence intensity was measured from regions exhibiting F. tularensis colonization in which three separate fields per section were quantified from each tissue section. (A) Cumulative green fluorescence intensity in F4/80+ and F4/80− cells. The average cumulative green fluorescence intensities ± standard errors (SE) were as follows: for Schu S4 F4/80+, 50.1 ± 16.0 (day 2) and 72.0 ± 12.0 (day 4); for Schu S4 F4/80−, 120.0 ± 48.0 (day 2) and 89.6 ± 42.3 (day 4); for Schu S4 ΔpyrF F4/80+, 20.0 ± 8.8 (day 2) and 27.4 ± 6.7 (day 4); and for Schu S4 ΔpyrF F4/80−, 62.0 ± 23.3 (day 2) and 88.3 ± 12.6 (day 4). The ratio of F. tularensis fluorescence in F4/80+ cells to the total (F4/80+ plus F4/80−) was significantly greater in wild-type Schu S4 than in the ΔpyrF mutant (χ2 = 4.637; P < 0.05). (B) Average green fluorescence per μm2 host cell. The percentage of green fluorescence intensity per μm2 within F4/80+ host cells was significantly greater for Schu S4 (expected) than for Schu S4 ΔpyrF (observed) (χ2 = 12.96; P < 0.001).
DISCUSSION
The ability of many pathogens, including F. tularensis, to cause disease often depends on their ability to invade and replicate in the infected host. In this report, we have investigated bacterial phenotypes after deleting the pyrF gene and have characterized an unanticipated role for bacterial proliferation in cells other than macrophages. Proliferation in nonmacrophage cell types appears sufficient to sustain F. tularensis pathogenesis.
F. tularensis ΔpyrF mutants could not replicate in primary human macrophages (Fig. 4A and B); however, these strains retained virulence in animal models of infection (Fig. 6). It is possible that there was a modest defect in the pathogenesis of the Schu S4 ΔpyrF strain that could be attributable to the lack of intramacrophage replication since some differences in survival were statistically significant (Fig. 6B). However, mice were infected with as few as 14 CFU of Schu S4 ΔpyrF, and mice from all experimental conditions were moribund within 24 h of one another, indicating that any virulence defect of Schu S4 ΔpyrF had a limited biological impact. The retention of virulence correlated with the ability to replicate in nonmacrophage cells (Fig. 8A and B and 10A and B). In addition, there were substantially fewer F. tularensis Schu S4 ΔpyrF bacteria than wild-type bacteria associated with lung macrophages in vivo (Fig. 11 and 12). These results indicate that growth in macrophages is expendable provided that the infecting F. tularensis strain can sustain itself in nonmacrophage host cells. This interpretation is consistent with data presented by Bosio and Dow in which mice were treated with clodronate to deplete pulmonary macrophages and dendritic cells (7). Although depletion of macrophages and dendritic cells delayed the time to death following a pulmonary F. tularensis infection, all animals in this experiment died by 8 days postinfection (7). Thus, elimination of macrophages still resulted in the death of the animals, further indicating that F. tularensis replication in nonmacrophages is adequate to cause morbidity and mortality.
Upon entering macrophages by phagocytosis, F. tularensis is able to alter normal bactericidal responses, escape the phagosome, and replicate within the cytosol (44). Mutation of F. tularensis genes encoding proteins responsible for escape of the phagosome is essential for replication in macrophages and virulence in animal models, associating intramacrophage replication with in vivo pathogenesis (3, 8, 23, 52). Recent data suggest that the activity of a secretion system encoded by the Francisella pathogenicity island is essential for this phagosomal escape (3). However, mutation of genes encoding proteins that mediate resistance to macrophage killing mechanisms may also have pleiotropic effects, complicating an interpretation of data that links in vitro phenomena directly with in vivo phenotypes. Some genes that are required for replication in macrophages are also required for intracellular growth in other host cell types (Table 2). We have hypothesized that because the efficiencies of bactericidal activity differ among host cell types, some F. tularensis genes that are essential for bacterial replication in highly bactericidal host cells, such as macrophages, may not be necessary in more-vulnerable cells. The F. tularensis ΔpyrF data presented in this study support this hypothesis (Fig. 4 and 6 to 12). In future studies, these strains may be used to better understand Francisella mechanisms for replication in nonmacrophage host cells.
TABLE 2.
Pathogenesis phenotypes of F. tularensis mutant strainsa
| Locus | Strain | Growth in nonmacrophage cells | Animal virulence | Source or reference |
|---|---|---|---|---|
| pyrF | LVS | +b | +c | This study |
| Schu S4 | +b | +d | This study | |
| FTT_1103 | Schu S4 | −e | −d | 48 |
| purMCD | Schu S4 | −f | −d | 43 |
| dsbB | Schu S4 | −e | −d | 49 |
| ripA | LVS | −g | −d | 22 |
A comprehensive list is shown for F. tularensis mutants deficient for intramacrophage replication that have also been tested for growth in nonphagocytic cells and virulence in an animal. Growth in macrophages was not detected for any of the loci tested.
HEK-293 epithelial cells.
Chicken embryo.
Mouse.
HepG2 hepatoma cells.
A549 epithelial cells.
TC-1 epithelial cells.
Our investigations have shown that Francisella has the capacity to thrive in alternative, nonmacrophage cells of the host. This capability may be particularly important when the macrophage environment is excessively hostile, providing a possible explanation of other observations in the literature. Prestimulation of mice with a nontypeable Haemophilus influenzae lysate increased the time to median death and reduced the lung bacterial burden following intranasal delivery of F. tularensis Schu S4 (19). Compared to the other pathogens tested, however, this treatment did not affect the cumulative mortality induced by F. tularensis (19). Growth in nonmacrophage cells may account for F. tularensis's virulence despite broad stimulation of innate immune cells. Similarly, stimulation of macrophages by proinflammatory cytokines can reduce F. tularensis proliferation in vivo (17). However, this approach was ineffective during infection with a virulent type A strain (39), which may reflect this strain's ability to replicate in nonmacrophage cells of the host (Fig. 10). Together with our results obtained using F. tularensis Schu S4 ΔpyrF, replicating in cells other than macrophages appears to contribute to the pathogenesis of tularemia.
F. tularensis has a significant extracellular phase in blood during infection of the animal host (20), raising the possibility that replication outside host cells may be important for sustenance of in vivo pathogenesis. However, growth of F. tularensis outside host cells has never been demonstrated during in vivo infection. In addition, we did not observe substantial growth of F. tularensis (wild type or ΔpyrF) in 10% serum (DMEM, HEPES, and GlutaMAX base tissue culture medium) (data not shown), making extracellular growth an unlikely explanation for the generation times measured in the in vitro intracellular replication assays.
We searched the literature to identify F. tularensis strains that have a defect for intramacrophage replication that have also been tested for growth in phagocytic cells and virulence in an animal (Table 2). In support of our interpretation, all of the F. tularensis mutants showing severe attenuation in vivo also have a defect for growth in both macrophages and nonmacrophage cells (Table 2). Mutants of another gene encoding an enzyme of de novo pyrimidine biosynthesis, pyrB, have been generated by different laboratories in both F. tularensis LVS and Schu S4 (32, 47, 56). Although the F. tularensis Schu S4 pyrB strains were not tested for replication in primary macrophages, the LVS pyrB mutant showed severe attenuation in these cells (56). Both the LVS and the Schu S4 pyrB mutants showed some replication in HepG2 hepatocytes, suggesting by our explanation that these strains may still be virulent in vivo (47, 56). Both the Schu S4 pyrB transposon mutant (47) and a Schu S4 pyrB deletion mutant (32) were used in murine infection models. While the Schu S4 pyrB transposon mutant resulted in a slight delay in time to mouse death, the Schu S4 pyrB deletion mutant showed no in vivo virulence attenuation (32, 47), suggesting that both of these mutants were pathogenic. Our results, along with the historical data presented in Table 2, reinforce the hypothesis that replication in nonmacrophages is also important for in vivo virulence of F. tularensis. This highlights the value of studying Francisella interactions with nonmacrophage host cells (22, 43, 48, 49).
By showing that the ΔpyrF mutants of F. tularensis LVS and Schu S4 were deficient in de novo pyrimidine biosynthesis and resistant to FOA and that expression of pyrFLVS rescued the uracil auxotrophy of E. coli pyrF287, we confirmed that this gene encodes an authentic orotidine-5′-phosphate decarboxylase. F. tularensis pyrF may be used as a selectable and counterselectable marker using both uracil auxotrophy and FOA resistance. Similar systems have been exploited in numerous organisms, including Saccharomyces cerevisiae, archaea, pseudomonads, and mycobacteria (5, 30, 54, 55). Importantly, use of antibiotic selection markers is restricted in F. tularensis because this approach raises concerns over the unlikely escape of resistant organisms from the research setting. In addition, antibiotic-resistant F. tularensis strains would have limited clinical utility as a live attenuated vaccine. These concerns are true for all biodefense and nonbiodefense agents, highlighting the need for innovative strategies, such as the use of nonantibiotic selectable markers, like the pyrF system, to perform genetic manipulations of pathogens without resorting to antibiotic resistance.
Acknowledgments
We thank Daniel F. Voytas for E. coli SKP10 pyrF287. We are grateful to Dana Previte for assistance with processing of the organs for histology, Deanna Schmitt for assistance with mouse infections, and Joshua Mattila and Joanne Flynn for technical assistance with processing of the tissue sections for immunofluorescence microscopy. We are thankful to Cory Robinson for providing materials and for insightful discussion.
This work was funded by National Institutes of Health grants AI074402 and AI050018. J.H. is a recipient of T32 AI060525, “Immunology of Infectious Disease.”
Editor: S. R. Blanke
Footnotes
Published ahead of print on 12 April 2010.
REFERENCES
- 1.Abril, C., H. Nimmervoll, P. Pilo, I. Brodard, B. Korczak, S. Markus, R. Miserez, and J. Frey. 2008. Rapid diagnosis and quantification of Francisella tularensis in organs of naturally infected common squirrel monkeys (Saimiri sciureus). Vet. Microbiol. 127:203-208. [DOI] [PubMed] [Google Scholar]
- 2.Bach, M. L., F. Lacroute, and D. Botstein. 1979. Evidence for transcriptional regulation of orotidine-5′-phosphate decarboxylase in yeast by hybridization of mRNA to the yeast structural gene cloned in Escherichia coli. Proc. Natl. Acad. Sci. U. S. A. 76:386-390. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Barker, J. R., A. Chong, T. D. Wehrly, J. J. Yu, S. A. Rodriguez, J. Liu, J. Celli, B. P. Arulanandam, and K. E. Klose. 2009. The Francisella tularensis pathogenicity island encodes a secretion system that is required for phagosome escape and virulence. Mol. Microbiol. 74:1459-1470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Barker, J. R., and K. E. Klose. 2007. Molecular and genetic basis of pathogenesis in Francisella tularensis. Ann. N. Y. Acad. Sci. 1105:138-159. [DOI] [PubMed] [Google Scholar]
- 5.Boeke, J. D., F. LaCroute, and G. R. Fink. 1984. A positive selection for mutants lacking orotidine-5′-phosphate decarboxylase activity in yeast: 5-fluoro-orotic acid resistance. Mol. Gen. Genet. 197:345-346. [DOI] [PubMed] [Google Scholar]
- 6.Bokhari, S. M., K. J. Kim, D. M. Pinson, J. Slusser, H. W. Yeh, and M. J. Parmely. 2008. NK cells and gamma interferon coordinate the formation and function of hepatic granulomas in mice infected with the Francisella tularensis live vaccine strain. Infect. Immun. 76:1379-1389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bosio, C. M., and S. W. Dow. 2005. Francisella tularensis induces aberrant activation of pulmonary dendritic cells. J. Immunol. 175:6792-6801. [DOI] [PubMed] [Google Scholar]
- 8.Brotcke, A., D. S. Weiss, C. C. Kim, P. Chain, S. Malfatti, E. Garcia, and D. M. Monack. 2006. Identification of MglA-regulated genes reveals novel virulence factors in Francisella tularensis. Infect. Immun. 74:6642-6655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carlson, P. E., Jr., J. A. Carroll, D. M. O'Dee, and G. J. Nau. 2007. Modulation of virulence factors in Francisella tularensis determines human macrophage responses. Microb. Pathog. 42:204-214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Carlson, P. E., Jr., J. Horzempa, D. M. O'Dee, C. M. Robinson, P. Neophytou, A. Labrinidis, and G. J. Nau. 2009. Global transcriptional response to spermine, a component of the intramacrophage environment, reveals regulation of Francisella gene expression through insertion sequence elements. J. Bacteriol. 191:6855-6864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Chamberlain, R. E. 1965. Evaluation of live tularemia vaccine prepared in a chemically defined medium. Appl. Microbiol. 13:232-235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Chase, J. C., J. Celli, and C. M. Bosio. 2009. Direct and indirect impairment of human dendritic cell function by virulent Francisella tularensis Schu S4. Infect. Immun. 77:180-195. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Choulika, A., A. Perrin, B. Dujon, and J. F. Nicolas. 1995. Induction of homologous recombination in mammalian chromosomes by using the I-SceI system of Saccharomyces cerevisiae. Mol. Cell Biol. 15:1968-1973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Craven, R. R., J. D. Hall, J. R. Fuller, S. Taft-Benz, and T. H. Kawula. 2008. Francisella tularensis invasion of lung epithelial cells. Infect. Immun. 76:2833-2842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.de Bruin, O. M., J. S. Ludu, and F. E. Nano. 2007. The Francisella pathogenicity island protein IglA localizes to the bacterial cytoplasm and is needed for intracellular growth. BMC Microbiol. 7:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Dennis, D. T., T. V. Inglesby, D. A. Henderson, J. G. Bartlett, M. S. Ascher, E. Eitzen, A. D. Fine, A. M. Friedlander, J. Hauer, M. Layton, S. R. Lillibridge, J. E. McDade, M. T. Osterholm, T. O'Toole, G. Parker, T. M. Perl, P. K. Russell, and K. Tonat. 2001. Tularemia as a biological weapon: medical and public health management. JAMA 285:2763-2773. [DOI] [PubMed] [Google Scholar]
- 17.Duckett, N. S., S. Olmos, D. M. Durrant, and D. W. Metzger. 2005. Intranasal interleukin-12 treatment for protection against respiratory infection with the Francisella tularensis live vaccine strain. Infect. Immun. 73:2306-2311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Evans, D. R., and H. I. Guy. 2004. Mammalian pyrimidine biosynthesis: fresh insights into an ancient pathway. J. Biol. Chem. 279:33035-33038. [DOI] [PubMed] [Google Scholar]
- 19.Evans, S. E., B. L. Scott, C. G. Clement, D. T. Larson, D. Kontoyiannis, R. E. Lewis, P. R. Lasala, J. Pawlik, J. W. Peterson, A. K. Chopra, G. Klimpel, G. Bowden, M. Hook, Y. Xu, M. J. Tuvim, and B. F. Dickey. 2010. Stimulated innate resistance of lung epithelium protects mice broadly against bacteria and fungi. Am. J. Respir. Cell Mol. Biol. 42:40-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Forestal, C. A., M. Malik, S. V. Catlett, A. G. Savitt, J. L. Benach, T. J. Sellati, and M. B. Furie. 2007. Francisella tularensis has a significant extracellular phase in infected mice. J. Infect. Dis. 196:134-137. [DOI] [PubMed] [Google Scholar]
- 21.Fujita, H., Y. Watanabe, T. Sato, Y. Ohara, and M. Homma. 1993. The entry and intracellular multiplication of Francisella tularensis in cultured cells: its correlation with virulence in experimental mice. Microbiol. Immunol. 37:837-842. [DOI] [PubMed] [Google Scholar]
- 22.Fuller, J. R., R. R. Craven, J. D. Hall, T. M. Kijek, S. Taft-Benz, and T. H. Kawula. 2008. RipA, a cytoplasmic membrane protein conserved among Francisella species, is required for intracellular survival. Infect. Immun. 76:4934-4943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Golovliov, I., A. Sjostedt, A. Mokrievich, and V. Pavlov. 2003. A method for allelic replacement in Francisella tularensis. FEMS Microbiol. Lett. 222:273-280. [DOI] [PubMed] [Google Scholar]
- 24.Haidl, I. D., and W. A. Jefferies. 1996. The macrophage cell surface glycoprotein F4/80 is a highly glycosylated proteoglycan. Eur. J. Immunol. 26:1139-1146. [DOI] [PubMed] [Google Scholar]
- 25.Hall, J. D., R. R. Craven, J. R. Fuller, R. J. Pickles, and T. H. Kawula. 2007. Francisella tularensis replicates within alveolar type II epithelial cells in vitro and in vivo following inhalation. Infect. Immun. 75:1034-1039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hall, J. D., M. D. Woolard, B. M. Gunn, R. R. Craven, S. Taft-Benz, J. A. Frelinger, and T. H. Kawula. 2008. Infected-host-cell repertoire and cellular response in the lung following inhalation of Francisella tularensis Schu S4, LVS, or U112. Infect. Immun. 76:5843-5852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Horzempa, J., P. E. Carlson, Jr., D. M. O'Dee, R. M. Shanks, and G. J. Nau. 2008. Global transcriptional response to mammalian temperature provides new insight into Francisella tularensis pathogenesis. BMC Microbiol. 8:172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Horzempa, J., R. M. Q. Shanks, M. J. Brown, B. C. Russo, D. M. O'Dee, and G. J. Nau. 2010. Utilization of an unstable plasmid and the I-SceI endonuclease to generate routine markerless deletion mutants in Francisella tularensis. J. Microbiol. Methods 80:106-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Horzempa, J., D. M. Tarwacki, P. E. Carlson, Jr., C. M. Robinson, and G. J. Nau. 2008. Characterization and application of a glucose-repressible promoter in Francisella tularensis. Appl. Environ. Microbiol. 74:2161-2170. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Husson, R. N., B. E. James, and R. A. Young. 1990. Gene replacement and expression of foreign DNA in mycobacteria. J. Bacteriol. 172:519-524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Janes, B. K., and S. Stibitz. 2006. Routine markerless gene replacement in Bacillus anthracis. Infect. Immun. 74:1949-1953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kadzhaev, K., C. Zingmark, I. Golovliov, M. Bolanowski, H. Shen, W. Conlan, and A. Sjostedt. 2009. Identification of genes contributing to the virulence of Francisella tularensis SCHU S4 in a mouse intradermal infection model. PLoS One 4:e5463. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Lai, L., N. Alaverdi, L. Maltais, and H. C. Morse III. 1998. Mouse cell surface antigens: nomenclature and immunophenotyping. J. Immunol. 160:3861-3868. [PubMed] [Google Scholar]
- 34.Lai, X. H., I. Golovliov, and A. Sjostedt. 2004. Expression of IglC is necessary for intracellular growth and induction of apoptosis in murine macrophages by Francisella tularensis. Microb. Pathog. 37:225-230. [DOI] [PubMed] [Google Scholar]
- 35.Lamps, L. W., J. M. Havens, A. Sjostedt, D. L. Page, and M. A. Scott. 2004. Histologic and molecular diagnosis of tularemia: a potential bioterrorism agent endemic to North America. Mod. Pathol. 17:489-495. [DOI] [PubMed] [Google Scholar]
- 36.Maier, T. M., A. Havig, M. Casey, F. E. Nano, D. W. Frank, and T. C. Zahrt. 2004. Construction and characterization of a highly efficient Francisella shuttle plasmid. Appl. Environ. Microbiol. 70:7511-7519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.McGarry, M. P., and C. C. Stewart. 1991. Murine eosinophil granulocytes bind the murine macrophage-monocyte specific monoclonal antibody F4/80. J. Leukoc. Biol. 50:471-478. [DOI] [PubMed] [Google Scholar]
- 38.McKnight, A. J., A. J. Macfarlane, P. Dri, L. Turley, A. C. Willis, and S. Gordon. 1996. Molecular cloning of F4/80, a murine macrophage-restricted cell surface glycoprotein with homology to the G-protein-linked transmembrane 7 hormone receptor family. J. Biol. Chem. 271:486-489. [DOI] [PubMed] [Google Scholar]
- 39.Metzger, D. W., C. S. Bakshi, and G. Kirimanjeswara. 2007. Mucosal immunopathogenesis of Francisella tularensis. Ann. N. Y. Acad. Sci. 1105:266-283. [DOI] [PubMed] [Google Scholar]
- 40.Monteilhet, C., A. Perrin, A. Thierry, L. Colleaux, and B. Dujon. 1990. Purification and characterization of the in vitro activity of I-Sce I, a novel and highly specific endonuclease encoded by a group I intron. Nucleic Acids Res. 18:1407-1413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nemzek, J. A., S. J. Ebong, J. Kim, G. L. Bolgos, and D. G. Remick. 2002. Keratinocyte growth factor pretreatment is associated with decreased macrophage inflammatory protein-2alpha concentrations and reduced neutrophil recruitment in acid aspiration lung injury. Shock 18:501-506. [DOI] [PubMed] [Google Scholar]
- 42.Nix, E. B., K. K. Cheung, D. Wang, N. Zhang, R. D. Burke, and F. E. Nano. 2006. Virulence of Francisella spp. in chicken embryos. Infect. Immun. 74:4809-4816. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Pechous, R. D., T. R. McCarthy, N. P. Mohapatra, S. Soni, R. M. Penoske, N. H. Salzman, D. W. Frank, J. S. Gunn, and T. C. Zahrt. 2008. A Francisella tularensis Schu S4 purine auxotroph is highly attenuated in mice but offers limited protection against homologous intranasal challenge. PLoS One 3:e2487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Pechous, R. D., T. R. McCarthy, and T. C. Zahrt. 2009. Working toward the future: insights into Francisella tularensis pathogenesis and vaccine development. Microbiol. Mol. Biol. Rev. 73:684-711. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Peck, R. F., S. DasSarma, and M. P. Krebs. 2000. Homologous gene knockout in the archaeon Halobacterium salinarum with ura3 as a counterselectable marker. Mol. Microbiol. 35:667-676. [DOI] [PubMed] [Google Scholar]
- 46.Posfai, G., V. Kolisnychenko, Z. Bereczki, and F. R. Blattner. 1999. Markerless gene replacement in Escherichia coli stimulated by a double-strand break in the chromosome. Nucleic Acids Res. 27:4409-4415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Qin, A., and B. J. Mann. 2006. Identification of transposon insertion mutants of Francisella tularensis tularensis strain Schu S4 deficient in intracellular replication in the hepatic cell line HepG2. BMC Microbiol. 6:69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Qin, A., D. W. Scott, and B. J. Mann. 2008. Francisella tularensis subsp. tularensis Schu S4 disulfide bond formation protein B, but not an RND-type efflux pump, is required for virulence. Infect. Immun. 76:3086-3092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Qin, A., D. W. Scott, J. A. Thompson, and B. J. Mann. 2009. Identification of an essential Francisella tularensis subsp. tularensis virulence factor. Infect. Immun. 77:152-161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Robinson, C. M., and G. J. Nau. 2008. Interleukin-12 and interleukin-27 regulate macrophage control of Mycobacterium tuberculosis. J. Infect. Dis. 198:359-366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Rong, Y. S., S. W. Titen, H. B. Xie, M. M. Golic, M. Bastiani, P. Bandyopadhyay, B. M. Olivera, M. Brodsky, G. M. Rubin, and K. G. Golic. 2002. Targeted mutagenesis by homologous recombination in D. melanogaster. Genes Dev. 16:1568-1581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Santic, M., M. Molmeret, K. E. Klose, S. Jones, and Y. A. Kwaik. 2005. The Francisella tularensis pathogenicity island protein IglC and its regulator MglA are essential for modulating phagosome biogenesis and subsequent bacterial escape into the cytoplasm. Cell. Microbiol. 7:969-979. [DOI] [PubMed] [Google Scholar]
- 53.Saslaw, S., H. T. Eigelsbach, J. A. Prior, H. E. Wilson, and S. Carhart. 1961. Tularemia vaccine study. II. Respiratory challenge. Arch. Intern. Med. 107:702-714. [DOI] [PubMed] [Google Scholar]
- 54.Sato, T., T. Fukui, H. Atomi, and T. Imanaka. 2003. Targeted gene disruption by homologous recombination in the hyperthermophilic archaeon Thermococcus kodakaraensis KOD1. J. Bacteriol. 185:210-220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Schneider, J. C., A. F. Jenings, D. M. Mun, P. M. McGovern, and L. C. Chew. 2005. Auxotrophic markers pyrF and proC can replace antibiotic markers on protein production plasmids in high-cell-density Pseudomonas fluorescens fermentation. Biotechnol. Prog. 21:343-348. [DOI] [PubMed] [Google Scholar]
- 56.Schulert, G. S., R. L. McCaffrey, B. W. Buchan, S. R. Lindemann, C. Hollenback, B. D. Jones, and L. A. Allen. 2009. Francisella tularensis genes required for inhibition of the neutrophil respiratory burst and intramacrophage growth identified by random transposon mutagenesis of strain LVS. Infect. Immun. 77:1324-1336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Shambaugh, G. E., III. 1979. Pyrimidine biosynthesis. Am. J. Clin. Nutr. 32:1290-1297. [DOI] [PubMed] [Google Scholar]
- 58.Small, P. L., R. R. Isberg, and S. Falkow. 1987. Comparison of the ability of enteroinvasive Escherichia coli, Salmonella typhimurium, Yersinia pseudotuberculosis, and Yersinia enterocolitica to enter and replicate within HEp-2 cells. Infect. Immun. 55:1674-1679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Tachado, S. D., J. Zhang, J. Zhu, N. Patel, M. Cushion, and H. Koziel. 2007. Pneumocystis-mediated IL-8 release by macrophages requires coexpression of mannose receptors and TLR2. J. Leukoc. Biol. 81:205-211. [DOI] [PubMed] [Google Scholar]
- 60.Telepnev, M., I. Golovliov, T. Grundstrom, A. Tarnvik, and A. Sjostedt. 2003. Francisella tularensis inhibits Toll-like receptor-mediated activation of intracellular signalling and secretion of TNF-alpha and IL-1 from murine macrophages. Cell. Microbiol. 5:41-51. [DOI] [PubMed] [Google Scholar]
- 61.Telepnev, M., I. Golovliov, and A. Sjostedt. 2005. Francisella tularensis LVS initially activates but subsequently down-regulates intracellular signaling and cytokine secretion in mouse monocytic and human peripheral blood mononuclear cells. Microb. Pathog. 38:239-247. [DOI] [PubMed] [Google Scholar]
- 62.Townsend, M. K., N. J. Carr, J. G. Iyer, S. M. Horne, P. S. Gibbs, and B. M. Pruss. 2008. Pleiotropic phenotypes of a Yersinia enterocolitica flhD mutant include reduced lethality in a chicken embryo model. BMC Microbiol. 8:12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Wickstrum, J. R., S. M. Bokhari, J. L. Fischer, D. M. Pinson, H. W. Yeh, R. T. Horvat, and M. J. Parmely. 2009. Francisella tularensis induces extensive caspase-3 activation and apoptotic cell death in the tissues of infected mice. Infect. Immun. 77:4827-4836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Wright, D. A., S. K. Park, D. Wu, G. J. Phillips, S. R. Rodermel, and D. F. Voytas. 1997. Recovery of YAC-end sequences through complementation of an Escherichia coli pyrF mutation. Nucleic Acids Res. 25:2679-2680. [DOI] [PMC free article] [PubMed] [Google Scholar]