Abstract
Although mucosal CD8+ T-cell responses are important in combating mucosal infections, the generation of such immune responses by vaccination remains problematic. In the present study, we evaluated the ability of plasmid DNA to induce local and systemic antigen-specific CD8+ T-cell responses after pulmonary administration. We show that the pulmonary delivery of plasmid DNA formulated with polyethyleneimine (PEI-DNA) induced robust systemic CD8+ T-cell responses that were comparable in magnitude to those generated by intramuscular (i.m.) immunization. Most importantly, we observed that the pulmonary delivery of PEI-DNA elicited a 10-fold-greater antigen-specific CD8+ T-cell response in lungs and draining lymph nodes of mice than that of i.m. immunization. The functional evaluation of these pulmonary CD8+ T cells revealed that they produced type I cytokines, and pulmonary immunization with PEI-DNA induced lung-associated antigen-specific CD4+ T cells that produced higher levels of interleukin-2 than those induced by i.m. immunization. Pulmonary PEI-DNA immunization also induced CD8+ T-cell responses in the gut and vaginal mucosa. Finally, pulmonary, but not i.m., plasmid DNA vaccination protected mice from a lethal recombinant vaccinia virus challenge. These findings suggest that pulmonary PEI-DNA immunization might be a useful approach for immunizing against pulmonary pathogens and might also protect against infections initiated at other mucosal sites.
Since establishing that antigen-specific CD8+ T-cell populations in mucosal sites may confer protection against intracellular pathogens that initiate infections at mucosal surfaces, vaccine strategies have been explored for eliciting cellular immune responses in mucosal tissues (40). Studies have been done to evaluate the immunogenicity of vaccines delivered to a variety of mucosal surfaces, including those of the nose, intestine, rectum, and vagina. These studies have shown that immunization at mucosal sites can induce larger numbers of antigen-specific CD8+ T cells in mucosal tissues than parenteral immunization (3).
Particular attention has focused on the lungs as a target for mucosal immunization. The lungs are an important mucosal portal of entry for pathogens. They are also a readily accessed mucosal site for the delivery of immunogens that might induce diverse mucosal immune responses. Pulmonary immunization strategies have been shown to generate potent Th1 responses and protective immunity against respiratory challenge with pathogens in several animal models (4, 29, 32, 37, 38).
Because of the ease of generating vaccine constructs and the ability to administer repeated inoculations of the same vector, DNA immunization remains a promising vaccination strategy for eliciting cellular immune responses. Only a limited number of studies have been done to evaluate the immunogenicity of DNA vaccines following pulmonary delivery (4, 32). Although the importance of CD8+ T lymphocytes in eradicating mucosal infections has been well established, it has not been determined whether pulmonary DNA immunization can induce robust functional CD8+ T-cell responses.
In the present study, we characterized antigen-specific CD8+ T lymphocytes in mice induced by the noninvasive pulmonary administration of plasmid DNA complexed to the cationic polymer polyethyleneimine (PEI). We demonstrate that the delivery of a DNA vaccine to the airways can induce a high frequency of functional antigen-specific CD8+ T cells in both systemic and mucosal sites.
MATERIALS AND METHODS
DNA vectors.
The codon-optimized HIV-1 HXB2 env and the firefly-luciferase genes were cloned separately into the VRC vector (DNA-gp120 and DNA-luc, respectively). The empty VRC vector was provided by G. Nabel (Vaccine Research Center, National Institute of Allergy and Infectious Diseases, National Institute of Health). Plasmids were prepared using the Endo-free plasmid Giga kit (Qiagen) and had endotoxin levels lower than 0.1 EU/μg DNA.
Preparation of PEI-DNA complexes.
Plasmid DNA was complexed with in vivo jetPEI (Polyplus transfection) according to the manufacturer's guidelines. In brief, 0.7 mg/ml plasmid DNA solution in 5% glucose was mixed with jetPEI solution to achieve a final DNA concentration of 0.4 mg/ml and a nitrogen-to-phosphate ratio (N/P) of 7.5. The mixture was incubated for at least 30 min at room temperature for the complexes to form before being injected to the mice.
Mice and immunizations.
BALB/c female mice, 8 to 12 weeks old, were purchased from Charles River Laboratories (Wilmington, MA) and maintained under specific-pathogen-free (SPF) conditions. Research on mice was approved by the Beth Israel Deaconess Institutional Animal Care and Use Committee. Mice were immunized intramuscularly (i.m.) with 20 μg of DNA in solution or complexed to jetPEI in a 100-μl total injection volume (50 μl delivered into each quadricep muscle). Noninvasive aerosol application was performed using the technique described by Bivas-Benita et al. (5): mice were endotracheally intubated with the Penn-Century Microsprayer (Penn-Century Inc.), and a 50-μl formulation consisting of 20 μg DNA in solution or complexed to jetPEI was sprayed directly in the airways. Identical procedures were used for the gp120 and luciferase expression vectors. Mice immunized with the gp120 plasmid were boosted 6 weeks after being primed with a homologous immunization dose.
In vivo bioluminescence analysis.
The bioimaging of luciferase protein expression was performed using the In Vivo Imaging System 110 (IVIS-110; Xenogen, Alameda, CA). Mice were anesthetized with a 50-mg/ml ketamine and 5-mg/ml xylazine mixture (Sigma-Aldrich) and injected intraperitoneally with 100 μl of an isotonic salt solution containing 30 mg/ml d-luciferin (Xenogen). Fifteen minutes after luciferin injection, photonic emissions were measured with an integration time of 1 min. Luminescence measurements were performed using Living Image software (Xenogen).
Phenotypic T-lymphocyte analyses.
H-2Dd tetramer complexes folded with the gp120 p18 epitope peptide (RGPGRAFVTI) (36) were prepared as previously described (35). Blood samples from individual mice were collected in RPMI 1640 supplemented with 40 U/ml heparin, and blood mononuclear cells were isolated by density separation using Lympholyte-M (Cedarlane). Cells collected from the gradient interface were washed with phosphate-buffered saline (PBS) containing 2% fetal bovine serum (FBS) and stained for 20 min with phycoerythrin (PE)-conjugated H-2Dd/p18 tetramer at room temperature. Cells then were stained for an additional 15 min at room temperature with the following monoclonal antibodies (MAbs): anti-CD8a-peridinin chlorophyll protein (PerCP)-Cy5.5 (53-6.7; BD Biosciences), anti-CD62L-fluorescein isothiocyanate (FITC) (MEL-14; eBioscience), anti-CD127-PE-Cy7 (A7R34; eBioscience), and anti-CD27-allophycocyanin (APC) (LG.7F9; eBioscience). Following staining, cells were washed once and fixed with PBS containing 2% paraformaldehyde. Samples were analyzed using an LSR II flow cytometer (BD Biosciences) and FlowJo software (Tree Star). Tetramer-binding CD8+ T cells were expressed as a percentage of the total CD8+ T-cell population. For the phenotypic analysis of memory T-cell subsets, a gating strategy using fluorescence-minus-one (FMO) controls was used as previously described (23).
Lymphocyte isolation from mucosal tissues.
Murine respiratory tract, vaginal tract, and small bowel were removed aseptically and cut into small pieces using straight scissors. Bowel specimens were processed as previously described (26). Respiratory and reproductive tract tissues were incubated with 1.33 mg/ml collagenase D and 0.2 mg/ml DNase (Roche) in Hanks balanced salt solution (HBSS) for 1 h at 37°C under vigorous shaking. Tissue fragments then were crushed through a 70-μm-pore-size filter, and cells were washed once. Cells were resuspended in 40% Percoll (Sigma-aldrich), layered over 67% Percoll, and centrifuged at 1,900 rpm for 25 min. The lymphocytes were present in the interface between the two Percoll layers. For tissue tetramer staining, lymphocytes were collected from the gradient interface, washed, and stained as described above for blood samples.
ICS assay.
For intracellular cytokine staining (ICS), lymphocytes isolated from the lung preparations were washed with PBS-2% FBS, counted, and stained with the PE-conjugated H-2Dd/p18 tetramer. The cells then were resuspended in RPMI 1640 supplemented with 10% FBS, 20 U/ml penicillin, 20 μg/ml streptomycin, 25 mM HEPES, 2 mM l-glutamine, 1 mM sodium pyruvate, and 0.1 mM nonessential amino acids (0.5 × 106 cells per tube). T-cell stimulation medium included Golgi Stop (2 μl/ml; BD Biosciences), anti-CD28 (2 μg/ml; BD Biosciences), and anti-CD49d (2 μg/ml; BD Biosciences). p18 peptide (2 μg/ml) was used for CD8+ stimulation, and for CD4+ T-cell stimulation cells were incubated with an Env peptide pool (2 μg/ml from each peptide) consisting of 47 overlapping 15-mer peptides spanning the HIV-1 IIIB gp120 protein (Centralized Facility for AIDS Reagents, Potters Bar, United Kingdom). Unstimulated cells were incubated with all of the reagents but not with the peptides. Positive control stimulation was performed using phorbol myristate acetate (PMA; 2 μg/ml) and ionomycin (10 μg/ml). The cells were incubated for 6 h at 37°C, washed with PBS-2% FBS, and stained with Live/Dead fixable dead cell stain (Invitrogen). After being washed, cells were stained with PE-conjugated H-2Dd/p18 tetramer for 20 min, followed by cell surface molecule staining with anti-CD3-APC Cy7 (145-2C11; BD Biosciences), anti-CD8a-PerCP-Cy5.5 (53-6.7; BD Biosciences), and anti-CD4-Pacific Blue (RM4-5; BD Biosciences) for an additional 15 min. Cells were fixed and permeabilized overnight at 4°C with Cytofix/Cytoperm solution (BD Biosciences). Permeabilized cells were washed with Perm/Wash buffer (BD Biosciences) and stained with the cytokine-specific Abs anti-tumor necrosis factor alpha (TNF-α)-Alexa Fluor 700 (MP6-XT22; BD Biosciences), anti-gamma interferon (IFN-γ)-PE-Cy7 (XMG1.2; BD Biosciences), and anti-IL-2-APC (JES6-5H4; BD Biosciences). After an additional wash with Perm/Wash buffer, cells were fixed in 2% formaldehyde-PBS solution. Samples were analyzed using an LSR II flow cytometer and FlowJo software.
Recombinant vaccinia virus challenge.
Groups of mice were challenged 12 weeks after homologous boost with replication-competent NYCBH strain vaccinia virus expressing HIV-1 B10 (rVac-gp160) (provided by D. Panicali, Therion Biologics Corporation). Mice were anesthetized by intraperitoneal injection with a ketamine (100 mg/kg of body weight)-xylazine (10 mg/kg) mixture, and 2 × 106 PFU rVac-gp160 (10 times the 50% lethal dose [LD50] of intranasally applied rVac-gp160) was instilled intranasally. Infected mice were monitored for clinical condition and body weight, and mice with weight loss of >20% were euthanized as required by our institutional guidelines. To evaluate vaccinia virus titers, mice were immunized and challenged as described above. Five days later, mice were sacrificed and both lungs and ovaries were removed, homogenized, sonicated, and freeze-thawed twice. Vaccinia virus titers were determined by plating 10-fold serial dilutions of the homogenized ovaries and lungs on a 6-well plate of confluent CV-1 cells. Following a 48-h incubation, cells were stained with crystal violet and plaques were counted. Titers were calculated as PFU/total tissue.
Statistical analysis.
Immune response data are presented as means with standard errors (SE) for each experimental group. Data statistical analyses were performed using the two-sided Student's t test or one-way analysis of variance (ANOVA) test, and P < 0.05 was considered significant.
RESULTS
Formulation of plasmid DNA with PEI improves transgene expression and CD8+ T-cell responses following pulmonary but not intramuscular immunization.
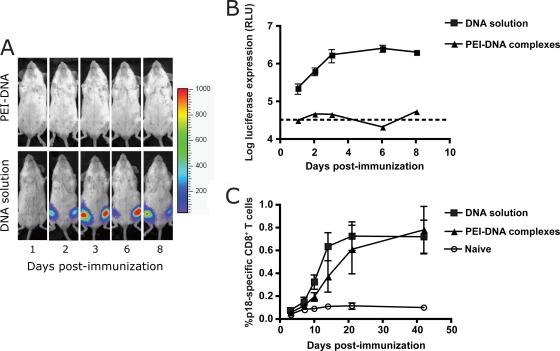
With a goal of improving its immunogenicity, we have been exploring various formulations and routes of delivery of plasmid DNA. We evaluated PEI as a vaccine carrier because of its ability to deliver DNA across cell membranes and enhance protein expression by releasing the DNA from the endosomal compartment and transferring it across the nuclear membrane. The effect of formulating plasmid DNA with PEI was evaluated first for i.m. immunization by monitoring the magnitude and kinetics of transgene expression. Mice were immunized i.m. with 20 μg of DNA-luc with or without PEI, and luciferase protein expression was monitored in vivo using the IVIS-110. Following the i.m. administration of DNA-luc solution, protein expression was localized in the muscle and peaked 6 days after injection, while no protein expression was detected following PEI-DNA-luc administration (Fig. 1A and B).
FIG. 1.
Kinetics of in vivo gene expression following intramuscular (i.m.) DNA immunization. Mice were immunized with 20 μg of luciferase DNA or plasmid DNA expressing the HIV-1 HXB2 gp120 protein either in solution or complexed to PEI. (A) Representative IVIS images of luciferase expression in a mouse immunized with luciferase DNA. (B) Log relative light units (RLU) expressed by groups of six to eight mice ± SE. (C) Kinetics of p18-specific CD8+ T-cell response in the peripheral blood of HIV-1 HXB2 gp120-immunized mice. Data represent means from five mice ± SE.
Since Takahashi et al. previously demonstrated that the entire CD8+ T-cell response of H2-Dd mice to HXBc2 gp120 is focused on a 10-amino-acid dominant epitope (p18), we vaccinated mice with HXBc2 gp120 DNA and monitored the elicited CD8+ T-cell responses using a p18/H-2Dd tetramer (36). Interestingly, no significant differences in peak peripheral blood mononuclear cell (PBMC) p18-specific CD8+ T-cell responses were observed in mice immunized with DNA-gp120 and mice immunized with PEI-DNA-gp120 complexes (Fig. 1C).
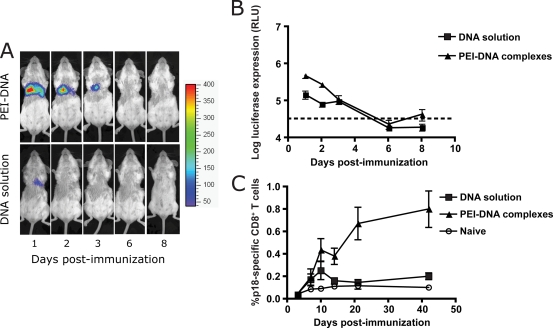
We then evaluated transgene expression and systemic antigen-specific CD8+ T-cell responses after pulmonary immunization. To ensure the reliable and reproducible pulmonary delivery of the DNA immunogen, we used a noninvasive endotracheal aerosolization technique that ensures the full instillation of the vaccine dose in the mouse airways. In contrast to what was observed for i.m. injections, the pulmonary administration of PEI-DNA-luc complexes resulted in higher luciferase expression than the administration of DNA-luc without adjuvant for 3 days following immunization (Fig. 2A and B). The p18-specific CD8+ T-cell response in PBMCs of mice immunized by the pulmonary route with PEI-DNA-gp120 was greater than that of mice receiving unadjuvanted DNA-gp120 (Fig. 2C). Following pulmonary immunization with PEI-DNA-gp120 complexes, peripheral blood p18-specific T-cell responses slowly increased for 42 days, while after pulmonary immunization with unadjuvanted DNA-gp120, a low-frequency peak p18-specific response was observed at day 10, followed by a decrease to baseline levels by day 21. The peak level of tetramer-binding CD8+ T cells in PBMCs of mice immunized by the pulmonary administration of PEI-DNA-gp120 complexes was comparable to that observed in mice immunized with this plasmid DNA construct intramuscularly (Fig. 1C). The peak peripheral blood p18-specific T-cell response following pulmonary PEI-DNA-gp120 administration was reached on day 42, while the peak response following i.m. immunization with DNA-gp120 was observed on day 21 (Fig. 1C and 2C).
FIG. 2.
Kinetics of in vivo gene expression following pulmonary DNA immunization. Mice were immunized with 20 μg of luciferase DNA or plasmid DNA expressing the HIV-1 HXB2 gp120 protein either in solution or complexed to PEI. (A) Representative IVIS images of luciferase expression in a mouse immunized with luciferase DNA. (B) Log relative light units (RLU) expressed by groups of six to eight mice ± SE. (C) Kinetics of p18-specific CD8+ T-cell responses in the peripheral blood of HIV-1 HXB2 gp120 immunized mice. Data represent means from six to eight mice ± SE.
These data indicate that i.m.- and pulmonary-administered plasmid DNA have distinct in vivo gene expression kinetics. Nevertheless, these different routes of DNA vaccine delivery can elicit comparable systemic antigen-specific CD8+ T-cell responses. The present findings also suggest that formulating plasmid DNA with PEI is important for enhancing both gene expression and antigen-specific CD8+ T-cell responses following pulmonary delivery. Based on these data, we used unadjuvanted plasmid DNA-gp120 for i.m. delivery and PEI-DNA-gp120 complexes for pulmonary delivery to further characterize the immune responses generated by these two routes of administration.
Pulmonary and intramuscular DNA immunization induce memory CD8+ T-cell populations with distinct expansion kinetics and CD27 expression.
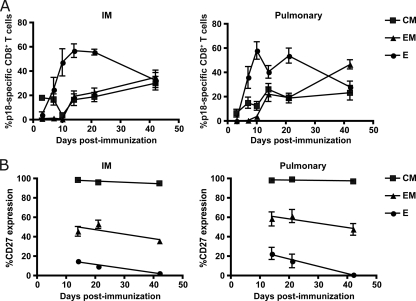
To characterize the differentiation of antigen-specific CD8+ T cells induced by pulmonary and intramuscular immunization, we evaluated the vaccination-induced memory CD8+ T-cell subpopulations using cell surface staining and multiparameter flow-cytometric analysis. Three functionally distinct memory subpopulations were defined according to their surface expression of cell surface molecules: effector (CD62Llo CD127lo), effector memory (CD62Llo CD127hi), and central memory (CD62Lhi CD127hi). Mice immunized with DNA-gp120 i.m. showed a significant rise in effector p18-specific CD8+ T cells at the time of the peak immune response (Fig. 3A). However, in mice immunized by the pulmonary route with PEI-DNA-gp120 complexes, the increase of effector cells occurred with more rapid kinetics than those after i.m. immunization. A larger fraction of p18-specific CD8+ T cells differentiated into effector memory cells by day 42 in mice immunized by the pulmonary route than in mice immunized by the i.m. route. However, the magnitude of this difference did not reach statistical significance.
FIG. 3.
Kinetics of responding memory subpopulations of p18-specific CD8+ T cells and the surface expression of CD27 on these lymphocyte subpopulations. Mice were primed by i.m. inoculation with 20 μg DNA expressing HIV-1 HXB2 gp120 protein or the pulmonary inoculation of this DNA formulated with PEI. (A) p18-specific CD8+ T cells were divided into effector (CD62Llo CD127lo) (E), effector memory (CD62Llo CD127hi) (EM), and central memory (CD62Lhi CD127hi) (CM) subpopulations. (B) Expression of CD27 on effector, effector memory, and central memory p18-specific CD8+ T cells. Data represent means from five to seven mice per group ± SE.
The expression of CD27 has been shown to be important in stimulating the survival of activated CD8+ T cells and maintaining the CD8+ T-cell pool at the priming site and its draining lymph nodes (LN) (17, 18). To further characterize the immunization-induced memory CD8+ T-cell responses, we evaluated the surface expression of CD27 on the different T-cell subpopulations as a marker for the long-term survival of antigen-specific CD8+ T cells. Following the pulmonary and i.m. administration of DNA-gp120, almost all central memory p18-specific CD8+ T cells maintained the expression of CD27 during the 42 days of the study, while CD27 expression on effector and effector memory p18-specific CD8+ T cells decreased over time (Fig. 3B). Although the levels of CD27 expression by these cell subpopulations differed in the two groups of mice, the differences in these expression levels between tetramer-binding CD8+ T cells in mice immunized by different routes of administration did not achieve statistical significance.
Pulmonary plasmid DNA immunization induces higher- frequency pulmonary cellular immune responses than i.m. immunization.
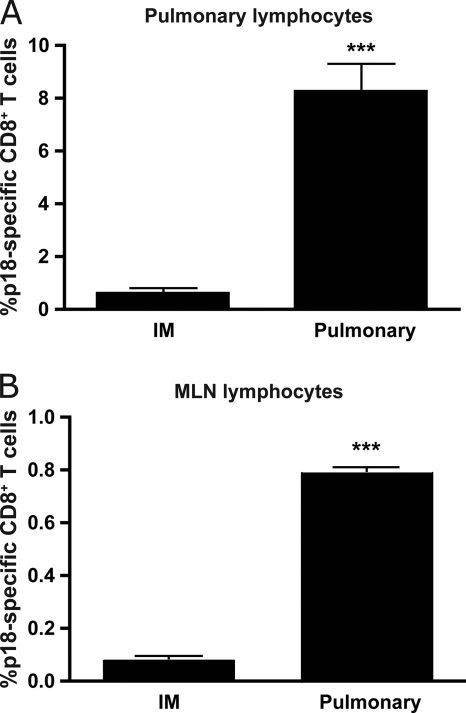
The mucosal administration of some vaccine vectors has been shown to induce mucosal immunity and protection against mucosally acquired pathogens or against pathogens that preferentially proliferate in mucosal tissues. To determine whether this is true for plasmid DNA immunization, antigen-specific cellular immune responses were monitored in the lungs of pulmonary PEI-DNA-gp120-immunized and i.m. DNA-gp120-immunized mice. We harvested the lungs 3 weeks after vaccine administration and evaluated p18-specific CD8+ T-cell responses in the pulmonary compartment. The p18-specific CD8+ T-cell responses elicited in the lungs of the pulmonary-immunized mice were 10-fold higher than those in the lungs of i.m.-immunized mice (Fig. 4A). Furthermore, the magnitude of the p18-specific CD8+ T-cell responses of the pulmonary-immunized mice was higher in the lungs than in blood. These findings indicate that pulmonary DNA immunization induces systemic immunogenicity that is comparable to that induced by i.m. administration and a more robust pulmonary mucosal immune response.
FIG. 4.
Effect of the route of immunization on pulmonary p18-specific CD8+ T-cell responses. Pulmonary (A) and mediastinal lymph node (MLN) (B) p18-specific CD8+ T-cell responses of mice immunized with DNA-gp120 by the i.m. route or DNA-gp120-PEI by the pulmonary route. Pulmonary data were generated from nine mice, and data are represented as the percent tetramer-binding CD8+ T cells ± SE. MLN data were generated from three independent pools of three mice. Statistically significant differences between groups were analyzed with Student's t test (***, P < 0.001).
We next assessed whether pulmonary PEI-DNA-gp120 immunization induced antigen-specific CD8+ T cells in the draining lymph nodes of the lungs. Three weeks after immunization, mediastinal lymph node (MLN) were harvested, and the presence of antigen-specific CD8+ T cells in this compartment was evaluated. Similarly to the results seen for the lung tissue, the magnitude of p18-specific CD8+ T-cell responses in the MLN of pulmonary-immunized mice was 10-fold higher than the response in MLN of i.m.-immunized mice (Fig. 4B). These findings show that local pulmonary DNA administration has a significant advantage over i.m. DNA immunization in initiating antigen-specific CD8+ T-cell responses in the lung and its draining lymph node.
Functional CD8+ and CD4+ T cells are generated following pulmonary plasmid DNA immunization.
To characterize the functionality of vaccine-elicited T cells in the lungs, we performed ICS to evaluate IFN-γ, IL-2, and TNF-α production by antigen-specific T cells. Lungs were harvested 3 weeks after pulmonary immunization with plasmid DNA-gp120-PEI or i.m. immunization with plasmid DNA-gp120, and the lung-associated lymphocytes were exposed to the p18 epitope peptide of gp120 and then assessed by MAb staining and multiparameter flow-cytometric analysis. Lung-associated p18-specific CD8+ T cells from pulmonary-immunized mice produced significantly higher IFN-γ and TNF-α levels but not IL-2 levels following p18 stimulation than did cells incubated with medium (Fig. 5A). We were unable to analyze cytokine production by pulmonary p18-specific CD8+ T cells from i.m.-immunized mice because of the low frequency of these cells.
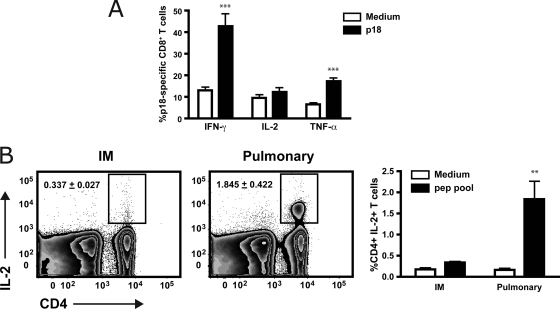
FIG. 5.
Influence of the route of immunization on the function of pulmonary CD8+ and CD4+ T cells in immunized mice. Mice were immunized with DNA-gp120 by the i.m. route or DNA-gp120-PEI by the pulmonary route, and 3 weeks later pulmonary lymphocytes were harvested. (A) Pulmonary lymphocytes were exposed to medium alone (Med) or p18 peptide (p18) for 6 h. Data are presented as percentages of CD3+ CD8+ p18 tetramer+ cells staining positive for IFN-γ, IL-2, or TNF-α from pulmonary immunized mice (six mice per group ± SE). (B) Pulmonary lymphocytes were exposed to medium alone or a pool of 47 overlapping peptides spanning the HIV-1 HXB2 gp120 protein (pep pool). Data are presented as percentages of CD3+ CD4+ cells staining positive for IL-2 (six mice per group ± SE). Statistically significant differences between groups were analyzed with Student's t test (**, P < 0.01; ***, P < 0.001).
We also assessed the cytokine production by gp120-specific CD4+ T cells from the lungs of i.m.- and pulmonary-immunized mice. In this ICS assay, a pool of peptides spanning the HIV-1 gp120 protein was used for the in vitro stimulation of CD4+ T cells. A significantly larger percentage of gp120-specific CD4+ T cells from pulmonary-immunized mice than from i.m. DNA-gp120-immunized mice secreted IL-2 (Fig. 5B). These data suggest that pulmonary immunization with PEI-DNA-gp120 generates a high-frequency, functional CD8+ T-cell response in the lung mucosa. Furthermore, this immunization route induces a higher-frequency functional CD4+ T-cell response in the lung than does i.m. immunization.
Pulmonary PEI-DNA immunization generates antigen-specific CD8+ T cells in distant mucosal inductive sites.
The most potent cellular immune response induced by mucosal immunization should be detected at the site of vaccine administration. However, T-cell responses in other mucosal tissues also may be generated using this vaccination strategy. We therefore evaluated the p18-specific CD8+ T-cell responses in the vaginal and intestinal mucosa following pulmonary immunization. Mucosal tissues were harvested 3 weeks after immunization, and p18-specific CD8+ T cells were evaluated using the p18 tetramer. We observed a trend toward higher p18-specific CD8+ T-cell responses in the vaginal mucosa (Fig. 6A) and the intestinal mucosa (Fig. 6B) following pulmonary PEI-DNA-gp120 immunization than those after i.m. DNA-gp120 immunization. However, these differences did not achieve statistical significance. The particularly high frequency of p18-specific CD8+ T cells in the vaginal mucosa following the i.m. and pulmonary administration of the immunogen was consistent with results of previous studies using other vaccine modalities, such as recombinant adenovirus (26). These data demonstrate that pulmonary and i.m. DNA immunization can induce antigen-specific T-cell responses not only at the immunization site but also at distal mucosal sites.
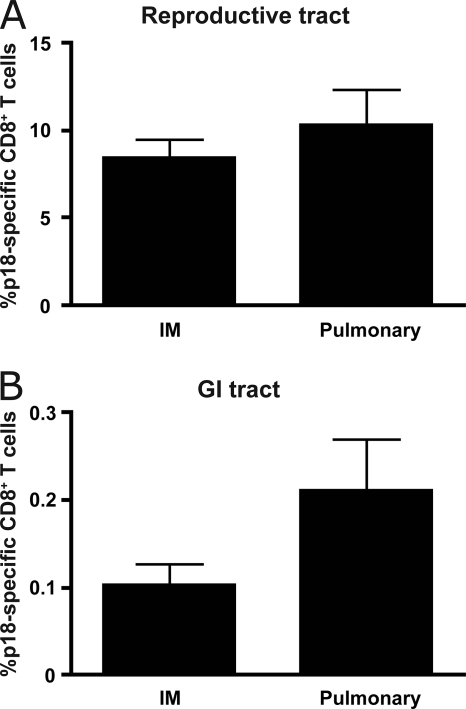
FIG. 6.
p18-specific CD8+ T-cell responses in mucosal sites following i.m. and pulmonary DNA-gp120 immunization. Reproductive (A) and gastrointestinal (GI) (B) tract p18-specific CD8+ T-cell responses of mice immunized with DNA-gp120 by the i.m. route or DNA-gp120-PEI by the pulmonary route. Reproductive tract data were generated from three independent pools of three to five mice. GI tract data represent eight mice per group. Data are represented as means ± SE.
Systemic primary T-cell responses induced by pulmonary immunization can be efficiently boosted.
To explore further the potential utility of pulmonary PEI-DNA immunization, we assessed the functionality of the vaccine-induced primary CD8+ T cells and their ability to expand following a boost immunization. Mice were boosted 6 weeks after priming with various combinations of i.m. and pulmonary immunizations, and peripheral blood gp120-specific CD8+ T-cell responses were monitored for 42 days. The site of the boosting immunization determined the kinetics of the secondary CD8+ T-cell responses. i.m. boosting resulted in a robust secondary CD8+ T-cell expansion, both in pulmonary- and i.m.-primed mice (Fig. 7B), and the differences in the magnitudes of the p18-specific CD8+ T-cell responses between the groups were statistically significant 7 days following the boost (P < 0.01). The assessment of memory subpopulations following boosting was performed by dividing the antigen-specific CD8+ T cells into effector, effector memory, and central memory populations. In contrast to what was observed following the priming immunization, the secondary p18-specific CD8+ T cells differentiated predominantly to effector and effector memory populations following the boosting immunization (Fig. 8B). The kinetics of this differentiation was not significantly affected by the site of boosting. However, statistically significant differences were observed in the effector CD8+ T-cell populations on day 42 following boost (P < 0.01) in these groups of mice, and higher effector responses were observed following a heterologous boost. These findings demonstrate that pulmonary immunization can prime functional systemic antigen-specific CD8+ T cells, and these responses can be boosted efficiently.
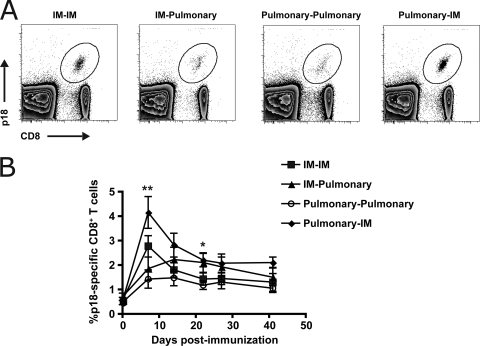
FIG. 7.
Kinetics of secondary CD8+ T-cell responses following i.m. and pulmonary DNA-gp120 immunization. Mice primed by the i.m. inoculation of DNA-gp120 or pulmonary inoculation of DNA-gp120-PEI were boosted by the i.m. or pulmonary delivery of the same immunogens. (A) Representative flow plots display the frequency of p18-specific CD8+ T cells in PBMCs of the immunized mice on day 7. (B) Kinetics of p18-specific CD8+ T-cell responses in the peripheral blood of mice following the boost immunization. Differences between groups were analyzed with a one-way ANOVA test (*, P < 0.05; **, P < 0.01).
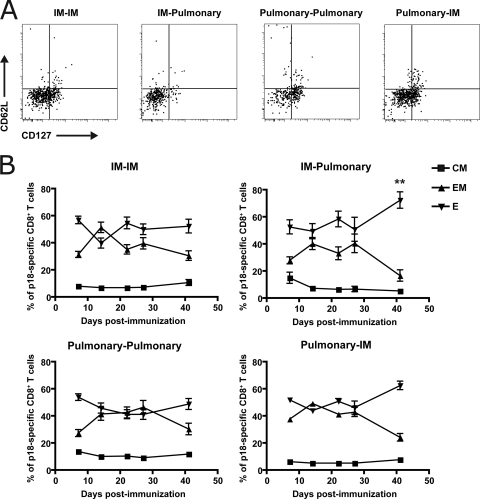
FIG. 8.
Kinetics of secondary memory subpopulations of p18-specific CD8+ T cells. Mice primed by the i.m. inoculation of DNA-gp120 or pulmonary inoculation of DNA-gp120-PEI were boosted by the i.m. or pulmonary delivery of the same immunogens. p18-specific CD8+ T cells were divided into effector (CD62Llo CD127lo), effector memory (CD62Llo CD127hi), and central memory (CD62Lhi CD127hi) subpopulations. (A) Representative flow plots display the different p18-specific CD8+ T-cell memory subpopulations in the peripheral blood of mice following the boost immunization. (B) Kinetics of the p18-specific CD8+ T-cell memory subpopulations in the peripheral blood of immunized mice. Data represent means from five to eight mice per group ± SE. Differences between groups were analyzed with a one-way ANOVA test (*, P < 0.05; **, P < 0.01).
Pulmonary plasmid DNA immunization protects mice from a lethal rVac-gp160 challenge.
We then assessed whether the mucosal immune responses generated following pulmonary DNA immunization could protect mice against an intranasal viral infection. We first harvested the lungs and MLN 12 weeks after boost immunization in i.m.- and pulmonary-immunized mice to determine the levels of p18-specific CD8+ T cells in these compartments during the memory phase of the immune response, after the levels of p18-specific CD8+ T cells in the blood had reached plateau. The p18-specific CD8+ T-cell responses in the lungs and the MLN of pulmonary-immunized mice were significantly higher than those in the lungs and MLN of i.m.-immunized mice (Fig. 9A). Furthermore, the magnitude of the p18-specific CD8+ T-cell responses 12 weeks following pulmonary and i.m. boost immunization was 3- to 5-fold higher in the lungs and 2- to 3-fold higher in the MLN than the magnitude of the response measured following the priming immunization (Fig. 4). These findings indicate that pulmonary DNA immunization induces robust mucosal antigen-specific CD8+ T-cell responses in the lungs and its draining lymph nodes, and their high frequency is maintained for long periods of time.
FIG. 9.
Effect of the route of immunization on pulmonary CD8+ T-cell responses and protection against intranasal vaccinia virus challenge. Mice primed by the i.m. inoculation of DNA-gp120 or pulmonary inoculation of PEI-DNA-gp120 received homologous boosting immunizations with the same immunogen using the same route of administration. Twelve weeks following the boost immunization, mice were challenged by the intranasal instillation of a lethal dose (2 × 106 PFU) of vaccinia virus. (A) p18-specific CD8+ T cells in the lungs and MLN of immunized mice 12 weeks following the boost immunization. Pulmonary immunity data were generated from five to six mice/group, and data are represented as percentages of tetramer-binding CD8+ T cells ± SE. MLN data were generated from three independent pools of three mice. Statistically significant differences between groups were analyzed using Student's t test (***, P < 0.001). (B) Weight loss following intranasal vaccinia virus challenge (five to eight mice per group); cross symbols indicate mortality. (C) Vaccinia virus titers in the lungs and ovaries of immunized mice were determined 5 days following challenge (five to nine mice per group). Differences between groups were analyzed with a one-way ANOVA test (***, P < 0.001).
We next evaluated whether the immune responses generated following pulmonary immunization were protective against an intranasal viral challenge. Naïve and i.m.- and pulmonary-immunized mice were challenged by the intranasal route 12 weeks after boost immunization with 2 × 106 PFU rVac-gp160, corresponding to a dose of 10 times the LD50. This challenge was 100% lethal in the unvaccinated mice (Fig. 9B). Pulmonary-immunized mice were protected against intranasal vaccinia virus challenge, losing 15% of their body weight by day 4 but then regaining almost all of their lost weight by day 11. However, the i.m.-immunized mice lost 25% of their body weight by day 6 and had to be euthanized.
To determine whether the weight loss correlated with the in vivo viral load, we evaluated viral titers in lungs and ovaries of immunized mice 5 days following intranasal vaccinia virus challenge. Viral loads in lungs and ovaries of pulmonary-immunized mice were approximately 3 logs lower than those of i.m.-immunized animals (Fig. 9C). The differences in viral titers between the groups were statistically significant in both tissues (P < 0.001). These data suggest that pulmonary PEI-DNA-gp120 immunization generated protective immune responses against intranasal vaccinia virus challenge, while i.m. DNA-gp120-immunized mice were not protected against this viral challenge.
DISCUSSION
The goal of immunization against mucosal pathogens is to induce potent, long-lasting mucosal immunity that protects against infection initiated by the mucosal route. Although i.m. immunization with plasmid DNA has been shown to induce potent systemic T-cell responses, it has not generated effective mucosal immunity (13, 25, 40). In the present study, we assessed the pulmonary administration of plasmid DNA as a strategy for eliciting mucosal T-cell immunity. Since plasmid DNA has been shown to be a poor immunogen for eliciting antibody responses, we have not pursued experiments in the present study to evaluate IgA antibody induction. We found that pulmonary delivery of plasmid DNA formulated with PEI generated robust systemic CD8+ T-cell responses that were comparable in both magnitude and kinetics to CD8+ T-cell responses generated by i.m. administration of DNA. We also observed responses that were comparable in magnitude in the gut and vaginal mucosa after i.m. and mucosal application of plasmid PEI-DNA. Importantly, we observed a dramatic expansion of antigen-specific CD8+ T cells in the lung tissue and its draining LNs following pulmonary PEI-DNA delivery. Furthermore, these notable pulmonary CD8+ T-cell immune responses were correlated with better protection against intranasal vaccinia virus challenge.
The formulation of plasmid DNA vaccines can have a major impact on the immune responses that they induce. In the present study, we have used the cationic polymer PEI to increase DNA transfection efficiency and, as a consequence, the immunogenicity of DNA. PEI has been shown to be safe for local and systemic administration without inducing tissue pathology or the secretion of proinflammatory cytokines (6, 15). The enhanced transfection efficiency of DNA when formulated with PEI has been attributed to the polymer's ability to protect DNA from degradation (12), facilitate its survival in the endosomal compartment after cellular uptake (27, 34), and deliver it into the cell nucleus (8, 31). Interestingly, PEI diminished the transfection efficiency of DNA in muscle. However, despite the low expression level of PEI-DNA in muscle, the systemic CD8+ T-cell responses measured after PEI-DNA-gp120 i.m. administration was comparable to that of DNA alone delivered i.m. by day 42. This suggests that although the low-level transfection of the PEI-DNA was detected in muscle by IVIS, protein expression was sufficient to stimulate antigen-specific T-cell responses.
Pulmonary immunization with DNA-gp120 without PEI resulted in low-level protein expression and modest systemic antigen-specific CD8+ T-cell responses. Formulating the DNA with PEI enhanced protein expression and significantly increased systemic antigen-specific CD8+ T-cell responses after pulmonary administration. Studies have shown that PEI efficiently transfects epithelial cells of the conducting airways. This activity could increase the level of DNA expression in the lung and result in enhanced antigen presentation and immunogenicity (14). The enhanced CD8+ T-cell responses following the pulmonary delivery of PEI-DNA could be a consequence of increased DNA uptake by pulmonary dendritic cells (DCs) with the subsequent priming of CD8+ T-cell responses by cross-presentation. This possible mechanism was supported by the recent observation that pulmonary CD103+ DCs preferentially take up antigen-conjugated particles and induce the expansion of antigen-specific CD8+ T cells (24). The delayed kinetics of antigen-specific CD8+ T cells observed following pulmonary immunization with PEI-DNA could be a result of the prolonged residence time of the PEI-DNA complexes in the cell nucleus (7, 9). Furthermore, prolonged antigen presentation by DCs in the draining lymph nodes of the airways could shape the kinetics of both systemic and locally activated T cells (41).
The kinetics of antigen-specific CD8+ T-cell differentiation were different following immunization by the i.m. and pulmonary administration of DNA. Pulmonary PEI-DNA-gp120 immunization generated systemic antigen-specific effector cells with more rapid kinetics than i.m. immunization. Furthermore, a larger proportion of p18-specific CD8+ T cells differentiated into effector memory cells following pulmonary PEI-DNA delivery than after i.m. administration of plasmid DNA. The differentiation of primary CD8+ T cells was found to be dependent on the duration of exposure to the antigen. Therefore, this observation could be explained partly by the kinetics of transgene expression in the immunized mice (1). In accordance with this model, pulmonary PEI-DNA administration resulted in transient transgene expression, which would prevent CD127 downregulation, maintain a large effector memory T-cell population, and support the differentiation of these cells to a central memory phenotype.
Since CD27 plays a critical role in promoting the survival of activated T cells and generating T-cell memory (16, 17), its expression on T-cell subsets following DNA immunization likely indicates whether a signal for T-cell survival and maturation was triggered. The high expression of CD27 on effector and, especially, effector memory p18-specific CD8+ T cells following pulmonary PEI-DNA-gp120 immunization could be the consequence of persistent antigen presentation in the draining pulmonary LNs (39). Although central memory T cells maintained high steady-state CD27 expression, this expression on effector and effector memory T cells decreased over time. The declining CD27 expression on effector and effector memory T cells could be a consequence of the maturation of these lymphocyte subsets and an increase in the central memory T-cell pool (20, 23). These findings suggest that pulmonary PEI-DNA immunization generates systemic antigen-specific memory T cells, and the distinctive features of these memory T cells are determined by the site of antigen encounter.
The generation of mucosal immune responses through vaccination should contribute to the control of mucosally acquired pathogens (19). We generated p18-specific CD8+ T-cell responses in the lung following the pulmonary administration of PEI-DNA-gp120 that were 10-fold greater than the responses in the lung after i.m. DNA-gp120 immunization. A comparable fold increase in p18-specific CD8+ T cells was observed in the draining lymph nodes of the lungs after the pulmonary administration of this immunogen. The p18-specific CD8+ T cells that were generated following pulmonary immunization were type I in nature and produced IFN-γ and TNF-α. Furthermore, we demonstrated that pulmonary-associated gp120-specific CD4+ T cells secreted higher levels of IL-2 following pulmonary immunization than following i.m. immunization. The generation of functional CD4+ T cells in the lungs is important for providing help for CD8+ T cells and for the generation of CD4+ memory cells that reside in the lung and mediate protective cellular responses (10, 21). The robust pulmonary cellular immune responses induced in the present study indicate that significant local antigen stimulation after pulmonary immunization generates T cells that persist to form a pulmonary memory T-cell population. Despite the well-documented ability of effector memory CD8+ T cells to migrate to nonlymphoid organs from the site at which they were initially activated (30), studies have shown that long-lived memory CD8+ T cells can persist in the mucosal sites where they first encountered antigen (13). Therefore, the present findings suggest that pulmonary immunization generates effective immunity against respiratory pathogens.
The present study indicates that immunization via the pulmonary route with plasmid DNA adjuvanted with PEI induces systemic T-cell responses and T-cell responses in diverse mucosal sites. We observed efficient priming of systemic antigen-specific CD8+ T cells following pulmonary immunization, and those responses could be boosted. Furthermore, pulmonary immunization generated modestly higher responses of p18-specific CD8+ T cells in the vaginal and the gut mucosa than those by i.m. immunization. The vaginal mucosa had particularly high frequencies of antigen-specific CD8+ T cells following vaccine administration by both routes, possibly as a result of lymphocyte migration. This phenomenon previously has been shown using a variety of vaccine modalities and administration routes (2, 26). The induction of cellular responses in the vaginal mucosa is consistent with the mucosal compartmentalization model that links immune induction in the respiratory and vaginal mucosa (22, 28). More p18-specific CD8+ T lymphocytes were present in the gut mucosa after pulmonary immunization than after i.m. immunization, indicating that pulmonary priming can induce lymphocyte trafficking. These observations show that T-cell dissemination to peripheral tissues following DNA immunization is influenced by the site of priming.
Perhaps the most striking finding in the current study is the protection against viral challenge conferred by pulmonary DNA immunization. We observed long-lived CD8+ T cells in the lungs and MLN of mice immunized by the pulmonary route 12 weeks following homologous boost, and these mice were protected against a lethal intranasal vaccinia virus challenge. These results suggest that the high levels of pulmonary antigen-specific CD8+ T cells confer protection against intranasal vaccinia virus challenge, which is in accord with previously published work (11, 33). An association between the vaccine-elicited CD8+ T-cell response and this protection could be formally confirmed only with in vivo CD8+ T-cell depletion studies or experiments using β2 microglobulin knockout mice.
These data demonstrate that pulmonary DNA immunization is an effective strategy to generate protective immunity against respiratory pathogens. However, the immune responses detected in the systemic and distant mucosal compartments suggest it also might protect against infections that are initiated at other mucosal sites. This method of vaccine delivery could be applied to humans using dry-powder inhalers or aerosol devices. This would enable efficient immunization while avoiding the use of needles.
Acknowledgments
We are grateful to Michelle Lifton, Kathryn Furr, Evita Grant, Shana Shields, and Ralf Geiben-Lynn for their scientific input to these studies. The HIV-1 HXB2 gp120 overlapping peptides were provided by the EU program EVA/MRC Centralized Facility for AIDS Reagents, National Institute for Biological Standards and Control, United Kingdom.
This work was supported by the NIAID Center for HIV/AIDS Vaccine Immunology grant AI-067854.
Footnotes
Published ahead of print on 24 March 2010.
REFERENCES
- 1.Bachmann, M. F., P. Wolint, K. Schwarz, P. Jager, and A. Oxenius. 2005. Functional properties and lineage relationship of CD8+ T-cell subsets identified by expression of IL-7 receptor alpha and CD62L. J. Immunol. 175:4686-4696. [DOI] [PubMed] [Google Scholar]
- 2.Barnett, S. W., I. K. Srivastava, E. Kan, F. Zhou, A. Goodsell, A. D. Cristillo, M. G. Ferrai, D. E. Weiss, N. L. Letvin, D. Montefiori, R. Pal, and M. Vajdy. 2008. Protection of macaques against vaginal SHIV challenge by systemic or mucosal and systemic vaccinations with HIV-envelope. AIDS 22:339-348. [DOI] [PubMed] [Google Scholar]
- 3.Belyakov, I. M., D. Isakov, Q. Zhu, A. Dzutsev, and J. A. Berzofsky. 2007. A novel functional CTL avidity/activity compartmentalization to the site of mucosal immunization contributes to protection of macaques against simian/human immunodeficiency viral depletion of mucosal CD4+ T cells. J. Immunol. 178:7211-7221. [DOI] [PubMed] [Google Scholar]
- 4.Bivas-Benita, M., M. Y. Lin, S. M. Bal, K. E. van Meijgaarden, K. L. Franken, A. H. Friggen, H. E. Junginger, G. Borchard, M. R. Klein, and T. H. Ottenhoff. 2009. Pulmonary delivery of DNA encoding Mycobacterium tuberculosis latency antigen Rv1733c associated to PLGA-PEI nanoparticles enhances T-cell responses in a DNA prime/protein boost vaccination regimen in mice. Vaccine 27:4010-4017. [DOI] [PubMed] [Google Scholar]
- 5.Bivas-Benita, M., R. Zwier, H. E. Junginger, and G. Borchard. 2005. Non-invasive pulmonary aerosol delivery in mice by the endotracheal route. Eur. J. Pharm. Biopharm. 61:214-218. [DOI] [PubMed] [Google Scholar]
- 6.Bonnet, M. E., P. Erbacher, and A. L. Bolcato-Bellemin. 2008. Systemic delivery of DNA or siRNA mediated by linear polyethylenimine (L-PEI) does not induce an inflammatory response. Pharm. Res. 25:2972-2982. [DOI] [PubMed] [Google Scholar]
- 7.Breuzard, G., M. Tertil, C. Goncalves, H. Cheradame, P. Geguan, C. Pichon, and P. Midoux. 2008. Nuclear delivery of NFkappaB-assisted DNA/polymer complexes: plasmid DNA quantitation by confocal laser scanning microscopy and evidence of nuclear polyplexes by FRET imaging. Nucleic Acids Res. 36:e71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Brunner, S., E. Furtbauer, T. Sauer, M. Kursa, and E. Wagner. 2002. Overcoming the nuclear barrier: cell cycle independent nonviral gene transfer with linear polyethylenimine or electroporation. Mol. Ther. 5:80-86. [DOI] [PubMed] [Google Scholar]
- 9.Chen, H. H., Y. P. Ho, X. Jiang, H. Q. Mao, T. H. Wang, and K. W. Leong. 2008. Quantitative comparison of intracellular unpacking kinetics of polyplexes by a model constructed from quantum dot-FRET. Mol. Ther. 16:324-332. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.de Bree, G. J., H. Daniels, M. Schilfgaarde, H. M. Jansen, T. A. Out, R. A. van Lier, and R. E. Jonkers. 2007. Characterization of CD4+ memory T-cell responses directed against common respiratory pathogens in peripheral blood and lung. J. Infect. Dis. 195:1718-1725. [DOI] [PubMed] [Google Scholar]
- 11.Deliyannis, G., K. Kedzierska, Y. F. Lau, W. Zeng, S. J. Turner, D. C. Jackson, and L. E. Brown. 2006. Intranasal lipopeptide primes lung-resident memory CD8+ T cells for long-term pulmonary protection against influenza. Eur. J. Immunol. 36:770-778. [DOI] [PubMed] [Google Scholar]
- 12.Demeneix, B., and J. P. Behr. 2005. Polyethylenimine (PEI). Adv. Genet. 53:217-230. [PubMed] [Google Scholar]
- 13.Gallichan, W. S., and K. L. Rosenthal. 1996. Long-lived cytotoxic T lymphocyte memory in mucosal tissues after mucosal but not systemic immunization. J. Exp. Med. 184:1879-1890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Gautam, A., C. L. Densmore, E. Golunski, B. Xu, and J. C. Waldrep. 2001. Transgene expression in mouse airway epithelium by aerosol gene therapy with PEI-DNA complexes. Mol. Ther. 3:551-556. [DOI] [PubMed] [Google Scholar]
- 15.Gautam, A., C. L. Densmore, B. Xu, and J. C. Waldrep. 2000. Enhanced gene expression in mouse lung after PEI-DNA aerosol delivery. Mol. Ther. 2:63-70. [DOI] [PubMed] [Google Scholar]
- 16.Hamann, D., P. A. Baars, M. H. Rep, B. Hooibrink, S. R. Kerkhof-Garde, M. R. Klein, and R. A. van Lier. 1997. Phenotypic and functional separation of memory and effector human CD8+ T cells. J. Exp. Med. 186:1407-1418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hendriks, J., L. A. Gravestein, K. Tesselaar, R. A. van Lier, T. N. Schumacher, and J. Borst. 2000. CD27 is required for generation and long-term maintenance of T-cell immunity. Nat. Immunol. 1:433-440. [DOI] [PubMed] [Google Scholar]
- 18.Hendriks, J., Y. Xiao, and J. Borst. 2003. CD27 promotes survival of activated T cells and complements CD28 in generation and establishment of the effector T-cell pool. J. Exp. Med. 198:1369-1380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hikono, H., J. E. Kohlmeier, K. H. Ely, I. Scott, A. D. Roberts, M. A. Blackman, and D. L. Woodland. 2006. T-cell memory and recall responses to respiratory virus infections. Immunol. Rev. 211:119-132. [DOI] [PubMed] [Google Scholar]
- 20.Hintzen, R. Q., R. de Jong, S. M. Lens, and R. A. van Lier. 1994. CD27: marker and mediator of T-cell activation? Immunol. Today 15:307-311. [DOI] [PubMed] [Google Scholar]
- 21.Hogan, R. J., W. Zhong, E. J. Usherwood, T. Cookenham, A. D. Roberts, and D. L. Woodland. 2001. Protection from respiratory virus infections can be mediated by antigen-specific CD4(+) T cells that persist in the lungs. J. Exp. Med. 193:981-986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Holmgren, J., and C. Czerkinsky. 2005. Mucosal immunity and vaccines. Nat. Med. 11:S45-53. [DOI] [PubMed] [Google Scholar]
- 23.Hovav, A. H., M. W. Panas, C. E. Osuna, M. J. Cayabyab, P. Autissier, and N. L. Letvin. 2007. The impact of a boosting immunogen on the differentiation of secondary memory CD8+ T cells. J. Virol. 81:12793-12802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jakubzick, C., J. Helft, T. J. Kaplan, and G. J. Randolph. 2008. Optimization of methods to study pulmonary dendritic cell migration reveals distinct capacities of DC subsets to acquire soluble versus particulate antigen. J. Immunol. Methods 337:121-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Jeyanathan, M., J. Mu, K. Kugathasan, X. Zhang, D. Damjanovic, C. Small, M. Divangahi, B. J. Petrof, C. M. Hogaboam, and Z. Xing. 2008. Airway delivery of soluble mycobacterial antigens restores protective mucosal immunity by single intramuscular plasmid DNA tuberculosis vaccination: role of proinflammatory signals in the lung. J. Immunol. 181:5618-5626. [DOI] [PubMed] [Google Scholar]
- 26.Kaufman, D. R., J. Liu, A. Carville, K. G. Mansfield, M. J. Havenga, J. Goudsmit, and D. H. Barouch. 2008. Trafficking of antigen-specific CD8+ T lymphocytes to mucosal surfaces following intramuscular vaccination. J. Immunol. 181:4188-4198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kichler, A., C. Leborgne, E. Coeytaux, and O. Danos. 2001. Polyethylenimine-mediated gene delivery: a mechanistic study. J. Gene Med. 3:135-144. [DOI] [PubMed] [Google Scholar]
- 28.Klavinskis, L. S., C. Barnfield, L. Gao, and S. Parker. 1999. Intranasal immunization with plasmid DNA-lipid complexes elicits mucosal immunity in the female genital and rectal tracts. J. Immunol. 162:254-262. [PubMed] [Google Scholar]
- 29.Lagranderie, M., P. Ravisse, G. Marchal, M. Gheorghiu, V. Balasubramanian, E. H. Weigeshaus, and D. W. Smith. 1993. BCG-induced protection in guinea pigs vaccinated and challenged via the respiratory route. Tuberc. Lung Dis. 74:38-46. [DOI] [PubMed] [Google Scholar]
- 30.Masopust, D., V. Vezys, E. J. Usherwood, L. S. Cauley, S. Olson, A. L. Marzo, R. L. Ward, D. L. Woodland, and L. Lefrancois. 2004. Activated primary and memory CD8 T cells migrate to nonlymphoid tissues regardless of site of activation or tissue of origin. J. Immunol. 172:4875-4882. [DOI] [PubMed] [Google Scholar]
- 31.Pollard, H., J. S. Remy, G. Loussouarn, S. Demolombe, J. P. Behr, and D. Escande. 1998. Polyethylenimine but not cationic lipids promotes transgene delivery to the nucleus in mammalian cells. J. Biol. Chem. 273:7507-7511. [DOI] [PubMed] [Google Scholar]
- 32.Reina, R., C. Barbezange, H. Niesalla, X. de Andres, H. Arnarson, E. Biescas, M. Mazzei, C. Fraisier, T. N. McNeilly, C. Liu, M. Perez, M. L. Carrozza, P. Bandecchi, C. Solano, H. Crespo, I. Glaria, C. Huard, D. J. Shaw, I. de Blas, D. de Andres, F. Tolari, S. Rosati, M. Suzan-Monti, V. Andresdottir, S. Torsteinsdottir, G. Petursson, L. Lujan, M. Pepin, B. Amorena, B. Blacklaws, and G. D. Harkiss. 2008. Mucosal immunization against ovine lentivirus using PEI-DNA complexes and modified vaccinia Ankara encoding the gag and/or env genes. Vaccine 26:4494-4505. [DOI] [PubMed] [Google Scholar]
- 33.Santosuosso, M., S. McCormick, X. Zhang, A. Zganiacz, and Z. Xing. 2006. Intranasal boosting with an adenovirus-vectored vaccine markedly enhances protection by parenteral Mycobacterium bovis BCG immunization against pulmonary tuberculosis. Infect. Immun. 74:4634-4643. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Sonawane, N. D., F. C. Szoka, Jr., and A. S. Verkman. 2003. Chloride accumulation and swelling in endosomes enhances DNA transfer by polyamine-DNA polyplexes. J. Biol. Chem. 278:44826-44831. [DOI] [PubMed] [Google Scholar]
- 35.Staats, H. F., C. P. Bradney, W. M. Gwinn, S. S. Jackson, G. D. Sempowski, H. X. Liao, N. L. Letvin, and B. F. Haynes. 2001. Cytokine requirements for induction of systemic and mucosal CTL after nasal immunization. J. Immunol. 167:5386-5394. [DOI] [PubMed] [Google Scholar]
- 36.Takahashi, H., Y. Nakagawa, C. D. Pendleton, R. A. Houghten, K. Yokomuro, R. N. Germain, and J. A. Berzofsky. 1992. Induction of broadly cross-reactive cytotoxic T cells recognizing an HIV-1 envelope determinant. Science 255:333-336. [DOI] [PubMed] [Google Scholar]
- 37.Wayne Conlan, J., H. Shen, R. Kuolee, X. Zhao, and W. Chen. 2005. Aerosol-, but not intradermal-immunization with the live vaccine strain of Francisella tularensis protects mice against subsequent aerosol challenge with a highly virulent type A strain of the pathogen by an alphabeta T cell- and interferon gamma-dependent mechanism. Vaccine 23:2477-2485. [DOI] [PubMed] [Google Scholar]
- 38.Wee, J. L., J. P. Scheerlinck, K. J. Snibson, S. Edwards, M. Pearse, C. Quinn, and P. Sutton. 2008. Pulmonary delivery of ISCOMATRIX influenza vaccine induces both systemic and mucosal immunity with antigen dose sparing. Mucosal Immunol. 1:489-496. [DOI] [PubMed] [Google Scholar]
- 39.Wikstrom, M. E., and P. A. Stumbles. 2007. Mouse respiratory tract dendritic cell subsets and the immunological fate of inhaled antigens. Immunol. Cell Biol. 85:182-188. [DOI] [PubMed] [Google Scholar]
- 40.Woodland, D. L., and J. E. Kohlmeier. 2009. Migration, maintenance and recall of memory T cells in peripheral tissues. Nat. Rev. Immunol. 9:153-161. [DOI] [PubMed] [Google Scholar]
- 41.Zammit, D. J., D. L. Turner, K. D. Klonowski, L. Lefrancois, and L. S. Cauley. 2006. Residual antigen presentation after influenza virus infection affects CD8 T-cell activation and migration. Immunity 24:439-449. [DOI] [PMC free article] [PubMed] [Google Scholar]