Abstract
Cell culture-adaptive mutations within the hepatitis C virus (HCV) E2 glycoprotein have been widely reported. We identify here a single mutation (N415D) in E2 that arose during long-term passaging of HCV strain JFH1-infected cells. This mutation was located within E2 residues 412 to 423, a highly conserved region that is recognized by several broadly neutralizing antibodies, including the mouse monoclonal antibody (MAb) AP33. Introduction of N415D into the wild-type (WT) JFH1 genome increased the affinity of E2 to the CD81 receptor and made the virus less sensitive to neutralization by an antiserum to another essential entry factor, SR-BI. Unlike JFH1WT, the JFH1N415D was not neutralized by AP33. In contrast, it was highly sensitive to neutralization by patient-derived antibodies, suggesting an increased availability of other neutralizing epitopes on the virus particle. We included in this analysis viruses carrying four other single mutations located within this conserved E2 region: T416A, N417S, and I422L were cell culture-adaptive mutations reported previously, while G418D was generated here by growing JFH1WT under MAb AP33 selective pressure. MAb AP33 neutralized JFH1T416A and JFH1I422L more efficiently than the WT virus, while neutralization of JFH1N417S and JFH1G418D was abrogated. The properties of all of these viruses in terms of receptor reactivity and neutralization by human antibodies were similar to JFH1N415D, highlighting the importance of the E2 412-423 region in virus entry.
Hepatitis C virus (HCV), which belongs to the Flaviviridae family, has a positive-sense single-stranded RNA genome encoding a polyprotein that is cleaved by cellular and viral proteases to yield mature structural and nonstructural proteins. The structural proteins consist of core, E1 and E2, while the nonstructural proteins are p7, NS2, NS3, NS4A, NS4B, NS5A, and NS5B (42). The hepatitis C virion comprises the RNA genome surrounded by the structural proteins core (nucleocapsid) and E1 and E2 (envelope glycoproteins). The HCV glycoproteins lie within a lipid envelope surrounding the nucleocapsid and play a major role in HCV entry into host cells (21). The development of retrovirus-based HCV pseudoparticles (HCVpp) (3) and the cell culture infectious clone JFH1 (HCVcc) (61) has provided powerful tools to study HCV entry.
HCV entry is initiated by the binding of virus particles to attachment factors which are believed to be glycosaminoglycans (2), low-density lipoprotein receptor (41), and C-type lectins such as DC-SIGN and L-SIGN (12, 37, 38). Upon attachment at least four entry factors are important for particle internalization. These include CD81 (50), SR-BI (53) and the tight junction proteins claudin-1 (15) and occludin (6, 36, 51).
CD81, a member of the tetraspanin family, is a cell surface protein with various functions including tissue differentiation, cell-cell adhesion and immune cell maturation (34). It consists of a small and a large extracellular loop (LEL) with four transmembrane domains. Viral entry is dependent on HCV E2 binding to the LEL of CD81 (3, 50). The importance of HCV glycoprotein interaction with CD81 is underlined by the fact that many neutralizing antibodies compete with CD81 and act in a CD81-blocking manner (1, 5, 20, 45).
SR-BI is a multiligand receptor expressed on liver cells and on steroidogenic tissue. It binds to high-density lipoproteins (HDL), low-density lipoproteins (LDL), and very low-density lipoproteins (VLDL) (31). The SR-BI binding site is mapped to the hypervariable region 1 (HVR-1) of HCV E2 (53). SR-BI ligands, such as HDL and oxidized LDL have been found to affect HCV infectivity (4, 14, 58-60). Indeed, HDL has been shown to enhance HCV infection in an SR-BI-dependent manner (4, 14, 58, 59). Antibodies against SR-BI and knockdown of SR-BI in cells result in a significant inhibition of viral infection in both the HCVpp and the HCVcc systems (5, 25, 32).
Although clearly involved in entry and immune recognition, the more downstream function(s) of HCV glycoproteins are poorly understood, as their structure has not yet been solved. Nonetheless, mutational analysis and mapping of neutralizing antibody epitopes have delineated several discontinuous regions of E2 that are essential for HCV particle binding and entry (24, 33, 45, 47). One of these is a highly conserved sequence spanning E2 residues 412 to 423 (QLINTNGSWHIN). Several broadly neutralizing monoclonal antibodies (MAbs) bind to this epitope. These include mouse monoclonal antibody (MAb) AP33, rat MAb 3/11, and the human MAbs e137, HCV1, and 95-2 (8, 16, 44, 45, 49). Of these, MAbs AP33, 3/11, and e137 are known to block the binding of E2 to CD81.
Cell culture-adaptive mutations within the HCV glycoproteins are valuable for investigating the virus interaction(s) with cellular receptors (18). In the present study, we characterize an asparagine-to-aspartic acid mutation at residue 415 (N415D) in HCV strain JFH1 E2 that arose during the long-term passaging of infected human hepatoma Huh-7 cells. Alongside N415D, we also characterize three adjacent cell culture adaptive mutations reported previously and a novel substitution generated in the present study by propagating virus under MAb AP33 selective pressure to gain further insight into the function of this region of E2 in viral infection.
MATERIALS AND METHODS
Cell culture and antibodies.
Human embryo kidney (HEK)-293T cells (ATCC CRL-1573) and the human hepatoma Huh-7 cells (43) were grown in Dulbecco modified Eagle medium (Invitrogen, United Kingdom) supplemented with 10% fetal calf serum, 100 U of penicillin/ml, 100 μg of streptomycin/ml, 10 mM HEPES, 0.1 mM nonessential amino acids, and 2 mM glutamine. The secreted alkaline phosphatase (SEAP) reporter cell line Huh7J-20 was described previously (23).
The anti-E2 MAbs AP33, CBH-4B, CBH-5, and HC-11 and the purified polyclonal immunoglobulins (IgGs) from an uninfected individual (IgG20) and HCV-infected patients (IgG2, IgG4, IgG17, and IgG19) have been described previously (11, 19, 20, 45). The anti-E2 MAb 3/11 (16), the anti-NS5A MAb 9E10 (35), and the sheep anti-NS5A antiserum (39) were kindly provided by J. McKeating, C. M. Rice, and M. Harris, respectively. The anti-CD81 MAb (clone JS-81) and the anti-SR-BI MAb CLA-1 were purchased from BD Biosciences. The anti-SR-BI rat serum was generated as described previously (63). The murine leukemia virus (MLV) gag-specific MAb was obtained from rat hybridoma cells (CRL-1912; American Type Culture Collection).
Plasmid constructs and mutagenesis.
The plasmid pUC-JFH1 carries the full-length cDNA of HCV genotype 2a strain JFH1. The plasmid pUC-GND JFH1 is identical except for the GND mutation in the NS5B-encoding sequence (61). The plasmids used to generate HCV pseudoparticles (HCVpp) containing the strain JFH1 envelope glycoproteins have been described previously (62). Site-directed mutagenesis was carried out by using a QuikChange-II kit (Stratagene) according to the manufacturer's instructions to introduce amino acid substitutions at the target sites in E2. Briefly, the amino acid substitutions N415D, T416A, N417S, G418D, and I422L in the E2-coding region were individually introduced into the plasmid pUC-JFH1 using appropriate primers (the sequences of which are available upon request). The presence of the desired mutation in the resulting clones was confirmed by nucleotide sequencing the DNA fragment between the BsiWI restriction site (nucleotides 1380 to 1386) and the BsaBI restriction site (nucleotides 2597 to 2606). Sequences carrying the appropriate mutation were subcloned back into pUC-JFH1 and the HCVpp E1E2 expression vector using the restriction enzymes described above.
Generation of HCVcc virus.
The JFH1 HCVcc was generated essentially as described previously (61). Briefly, linearized plasmids carrying HCVcc genomic cDNA were used as a template to generate viral genomic RNA by in vitro transcription. Approximately 4 × 106 Huh-7 cells were added to a 0.4-cm Gene Pulser cuvette (VWR) suspended in 400 μl of phosphate-buffered saline (PBS). Ten μg of in vitro-synthesized RNA was then added and pulsed once at 960 μF and 270 V by using a GenePulser Xcell (Bio-Rad) electroporator. The transfected cells were allowed to rest for 10 min before mixing them with fresh medium and seeding them into tissue culture dishes. After incubation at 37°C for the indicated time period, the medium containing the infectious virus progeny was filtered through a 0.45-μm-pore-size membrane before the infectivity was determined as described below.
Determination of virus infectivity and RNA replication.
To monitor wild-type (WT) JFH1 replication during serial passaging, 5 × 106 naive Huh-7 cells were infected in a T80 flask at a multiplicity of infection (MOI) of 0.005 in a total volume of 10 ml. Subconfluent cells were split 1:10 into a new flask containing 24 ml of fresh medium. At each passage the cell culture supernatants were harvested, and their tissue culture 50% infective dose(s) (TCID50) were determined by infection of naive cells, followed by immunostaining for NS5A as described previously (35). To measure virus replication after electroporation, the cells were transfected with viral transcript and seeded into 10-cm culture dishes. Fours hours later, cells were treated with trypsin and split 1:3 into T25 flasks. After incubation at 37°C for 72 h, culture supernatants were harvested, and the virus titers were determined as described above. Total RNA was prepared from cells by using an RNeasy kit (Qiagen), and the HCV RNA content was measured by quantitative reverse transcription real-time PCR (qRT-PCR) as described previously (62). To measure virus replication postinfection, cells in six-well culture dishes were infected at the indicated MOIs. After incubation at 37°C for 24, 48, and 72 h, infectious virus yields in the medium and the intracellular viral RNA levels were determined as described above.
Virus infectivity and replication were determined by using the focus-forming assay (64) or the recently described reporter cell line, Huh7-J20 (23). For the focus-forming assay, Huh-7 cells were fixed in methanol at 2 days postinfection and immunostained for NS5A using MAb 9E10, and the HCV-positive foci were counted by fluorescence microscopy to calculate focus-forming units (FFU) as described previously (64). The Huh7-J20 cell line is engineered to release SEAP reporter into the medium following HCV infection, thus enabling a rapid and sensitive quantification of virus infectivity and replication (23). The SEAP activity in the medium was measured 72 h postinfection as described previously (23).
The effect of HDL on HCVcc infectivity was tested essentially as described previously (59). Briefly, Huh7-J20 cells were preincubated for 2 h at 37°C in medium supplemented with 3% lipoprotein-deficient fetal calf serum (LPDS). The cells were then infected with WT or mutant HCVcc (generated in medium containing 3% LPDS) in the presence or absence of 20 μg of human HDL (Athens Research Technology)/ml for 3 h at 37°C. Three hours later, the inoculum was replaced with normal medium, and the SEAP activity in the medium was measured at 72 h postinfection.
Identification of cell culture adaptive mutations.
Total RNA was prepared from cells infected with virus collected from passage 9 cells (see Results) as described above. RNA was converted to first-strand DNA by using a Superscript III first-strand synthesis kit (Invitrogen) with the primer 5′-TTGCGAGTGCCCCGGGA-3′. After digestion with 1 U of RNase H (Invitrogen) for 20 min at 37°C, one-quarter of the RT reaction was amplified with appropriate primers that are available on request. The PCR products were gel purified by gel extraction (Qiagen) and used directly for sequencing.
HCVcc neutralization assays.
Antibody inhibition assays were performed using either Huh-7 or Huh7-J20 cells, and virus infectivity levels were determined by FFU or SEAP reporter assay, respectively, as described previously (23, 57). Briefly, Huh-7 cells were plated out at a density of 3 × 103 per well in a 96-well plate. For anti-E2 antibody neutralization assays, ∼50 FFU of virus was preincubated at 37°C for 1 h with the appropriate inhibitory or control antibody prior to infecting cells. To test neutralization by anti-receptor antibodies, cells were preincubated with appropriate antibodies for 1 h at 37°C prior to infection with 50 FFU of the virus. At 3 h postinfection, the inoculum was replaced with fresh medium and incubated for 48 h. The infectivity was determined as FFU following immunostaining of the cells for NS5A as described above. The Huh7-J20 reporter cells were infected in the presence or absence of appropriate antibody essentially as described above, and the virus infectivity levels were determined by measurement of the SEAP activity released into the medium.
RNA interference.
Two prevalidated small interfering RNA (siRNA) duplexes (Applied Biosystems) targeting different regions of human CD81 (14501 and 146379) and SR-BI (s2650 and s2649) were used. The negative control siRNA was composed of a scrambled sequence. Naive Huh-7 cells were transfected with Lipofectamine RNAiMax (Invitrogen) and 50 nM siRNAs according to the manufacturer's protocol and incubated for 2 days prior to virus infection. The efficiency of each gene knockdown at the time of infection was determined by measuring the mRNA transcripts by qRT-PCR using TaqMan probes (ABI) specific for SR-BI (Hs00969819) and CD81 (Hs00174717). In parallel, the cell surface expression of each receptor was measured by incubating cells with the anti-CD81 MAb (JS-81) or the anti-SR-BI MAb CLA-1, followed by an anti-mouse IgG-fluorescein isothiocyanate (FITC) conjugated secondary antibody. A subtype IgG1 was used as control. The cells were then analyzed by flow cytometry in a FACSCalibur using CellQuest software (BD Bisociences). The cell viability of siRNA-treated cells was measured by using the colorimetric WST-1 assay (Roche), according to the manufacturer's instructions.
HCVpp genesis, infection, and neutralization assays.
HCVpp were generated in HEK-293T cells, following cotransfection with plasmids expressing the MLV Gag-Pol and the MLV transfer vector carrying the firefly luciferase reporter (kindly provided by F.-L. Cosset and J. Dubuisson, respectively), and HCV E1 and E2 as described previously (3, 57, 62). The medium containing HCVpp was collected, clarified, filtered through a 0.45-μm-pore-size membrane, and used to infect the Huh-7 target cells. At 3 days postinfection, the luciferase activity in the cell lysates was measured by using a Bright-Glo luciferase assay system (Promega). The levels of particle secretion were tested by immunoblotting for MLV gag protein and E2 in the cell supernatants. For this, 10 ml of medium was pelleted through a 20% sucrose cushion (wt/vol) in PBS at 116,000 × g for 4 h. Virus pellets were analyzed for HCV E2 and MLV gag by Western immunoblotting. For neutralization assays, HCVpp preparations were mixed with appropriate amounts of inhibitory or control antibody and incubated for 1 h at 37°C prior to infection. To control the particle to antibody ratio, each pseudoparticle inoculum was adjusted to the same level of infectivity. The percentage neutralization was expressed relative to infection in the absence of antibody.
For immunoprecipitation of E1 and E2 glycoproteins, HEK-293T cells transfected with the HCV glycoprotein-expressing plasmids were radiolabeled with [35S]methionine and cysteine as described previously (47), and the labeled proteins were immunoprecipitated using the anti-E2 human MAb CBH-5. The immune complexes were subjected to SDS-PAGE, and the proteins were visualized with a Bio-Rad Personal FX phosphorimager.
GNA and CD81 capture assay for E2 analysis.
Galanthus nivalis agglutinin (GNA)-capture enzyme-linked immunosorbent assays (ELISAs) to detect MAb binding to E2 glycoprotein in lysates from electroporated Huh-7 cells were performed essentially as described previously (48). Bound glycoproteins were detected using the anti-E2 MAbs AP33, CBH-4B, and 3/11, followed by an anti-species IgG-horseradish peroxidase-conjugated antibody and 3,3′5,5′-tetramethylbenzidine (TMB) substrate. Absorbance values were determined at 450 nm after stopping the reaction with 0.5 M sulfuric acid. To assay E2-CD81 binding, E2 from cell lysates was captured onto an ELISA plate coated with human CD81-LEL fused to glutathione S-transferase (hCD81-LEL), and the bound E2 was detected using the anti-E2 human MAb CBH-4B as described previously (11).
Isolation of MAb AP33 escape mutants.
To isolate MAb AP33 neutralization escape mutants, a selection protocol using a two-chamber cell culture system was developed. JFH1WT RNA-electroporated Huh-7 cells were seeded into 1-μm-pore-size membrane of Thincert tissue culture inserts (Greiner), while naive Huh-7 cells were grown into the lower compartment underside of the membrane. To select for antibody neutralization escape mutants, MAb AP33 was added to the medium at 100% neutralizing concentration. This system ensures that the naive recipient cells are only infected via cell-free HCVcc that has escaped the neutralizing concentration of AP33 and avoids infection with JFH1WT, thus allowing rapid enrichment and propagation of antibody escape mutants. After approximately 3 days, the infected recipient cells were treated with trypsin and seeded in a fresh insert and placed in a well seeded with naive Huh-7 cells in the medium containing the same neutralizing concentration of MAb AP33. This process was repeated eight times. At each passage, the cells were collected for analysis by immunofluorescence using MAb AP33 and the anti-NS5A antiserum and to prepare total RNA from which the viral RNA was reverse transcribed, and the resulting cDNA was PCR amplified and sequenced as described above.
Amino acid sequence analysis.
A total of 1,311 full-length E2 protein sequences were downloaded from the HCV Sequence Database at Los Alamos National Laboratory (http://hcv.lanl.gov). Sequences annotated as “bad” and sequences containing obvious long frameshifts were excluded. Alignments were performed by using MAFFT (26) and analyzed in MEGA (54).
RESULTS
Identification of a cell culture-adaptive mutation in E2.
Naive Huh-7 cells were infected at a low MOI with the HCV JFH1WT virus generated from cells electroporated with viral RNA and serially passaged over a period of 6 weeks (nine passages). As shown in Fig. 1A, the infectious virus yields in the culture supernatants increased up to cell passage 6 (cp6), at which time the titers peaked at 105. Interestingly, ∼100-fold-higher virus yields were obtained after infection of naive Huh-7 cells with the virus collected from cp9 (sp1). Sequence analysis of the structural genes of the JFH1sp1 virus revealed a single mutation in E2 (N415D) located within the highly conserved region that represents an epitope for the broadly neutralizing antibodies, MAb AP33, 3/11, e137, HCV1, and 95-2 (8, 45, 49, 56). Three recent studies have also reported adaptive E2 mutations within this epitope, at positions T416 (10), N417 (52), and I422 (27) (Fig. 1B). These were generated in Huh-7.5 cells using the chimeric J6/JFH1 (T416A) or the WT JFH1 (N417S and I422L) HCVcc. We examined the effect of these four closely positioned mutations on JFH1 infectivity and antibody-mediated neutralization.
FIG. 1.
Determination of infectious virus yield during serial passage of infected cells. (A) Huh-7 cells were infected with the JFH1WT at an MOI of 0.005 and serially passaged (cp) nine times. At each passage, virus released into the medium was titrated by TCID50 assay. Similarly, virus generated at passage 9 (sp1) was used to infect naive Huh-7 cells, and the resultant infectious yield in the medium was measured as described above. (B) The location of adaptive mutations within the E2 residues 412 to 423 characterized in the present study. The arrows denote amino acid substitution.
Effects of E2 mutations on virus infection.
The four E2 mutations were introduced individually into the JFH1 genome by site-directed mutagenesis, and their effect on RNA replication and virus release after transfection in Huh-7 cells was determined. In contrast to JFH1GND (which served as a negative control), both the WT and all E2 mutant virus RNAs were replication competent (Fig. 2A). The released infectious virus yield and intracellular RNA levels of all four mutants were only slightly higher than WT, showing no significant difference at 72 h posttransfection.
FIG. 2.
Determination of infectious virus yield and replication. (A) Huh-7 cells were electroporated with in vitro-transcribed viral RNA. At 72 h posttransfection, virus released in the medium was titrated by TCID50 (light gray bar) and intracellular RNA (black bar) was quantified by qRT-PCR. Means and error ranges from duplicate assays are shown. (B and C) Naive Huh-7 cells were infected at an MOI of 0.1 with virus collected from the electroporated cells above. At 24 h (black bars), 48 h (light gray bars), and 72 h (dark gray bars) postinfection, (B) the virus yield in the culture medium of infected cells and (C) the intracellular viral RNA levels were determined by TCID50 and qRT-PCR, respectively. Means and error ranges from triplicate assays are shown.
We next determined the ability of mutant viruses to expand in naive cells following infection. Extracellular virus collected at 72 h posttransfection was used to inoculate naive Huh-7 cells at an MOI of 0.1. At 24, 48, and 72 h postinfection, the infectious virus released into the medium and the intracellular viral RNA levels were determined. The infectious yield of each mutant was found to be increased compared to the WT (Fig. 2B). Although the average values of each mutant were higher than WT at 48 and 72 h, our statistical analysis found this not to be significant (n = 3; P = <0.054, <0.171, <0.063, and <0.139, respectively, for mutants N415D, T416A, N417S, and I422L; unpaired Student t test). The intracellular HCV RNA levels in cells infected with the E2 mutants were unaltered compared to the WT virus (Fig. 2C). Interestingly, the JFH1sp1 virus, which was included for comparison, produced infectious titers 100-fold greater than WT at 72 h postinfection (data not shown), indicating that this virus is better adapted likely due to the presence of additional mutation(s) in the nonstructural regions of the genome.
E2 mutations alter virus-receptor interactions.
To establish whether the mutations have altered the affinity of E2 for the virus receptor CD81, a competition assay using the soluble form of CD81 (hCD81-LEL) was performed. This protein has been shown to interact with the E2 glycoprotein and inhibit HCV infection (5). All four mutant viruses showed increased sensitivity to neutralization by hCD81-LEL (Fig. 3A). To investigate whether this was due to a change in their affinity to CD81, we tested the reactivity of the intracellular viral glycoproteins to hCD81-LEL. The levels of WT or mutant E2 in Huh-7 cells transfected with appropriate viral RNAs was first normalized by measuring their binding to the conformation-sensitive anti-E2 human MAb CBH-4B (see Fig. S1a in the supplemental material). Notably, the various E2s also bound an anti-E2 MAb that recognizes a linear epitope with comparable efficiency (see Fig. S1b in the supplemental material). Consistent with the increased sensitivity of the viruses to hCD81-LEL neutralization, the affinity of E2 mutants N415D, T416A, and N417S to hCD81-LEL was enhanced in a dose-dependent fashion (see Fig. S1c and S1d in the supplemental material), by up to 38, 106, and 64%, respectively (Fig. 3b), indicating an increased exposure of CD81 binding residues on these mutant glycoproteins. However, for reasons that are unclear, the property of the E2 I422L mutant is at odds with this hypothesis as it bound hCD81-LEL with comparable affinity to WT E2 (Fig. 3B and see Fig. S1c and S1d in the supplemental material). A potential explanation for the phenotype of E2 I422L is that some local change may occur during the virion assembly process leading to a better exposure of the CD81-binding region and therefore enhanced neutralization. Incubation of naive cells with anti-CD81 MAb prior to infection showed no difference in inhibition of WT and mutant viruses (Fig. 3C). This may be explained by the higher affinity of the MAb outcompeting the binding of both WT and mutant virus glycoproteins to cellular CD81.
FIG. 3.
E2 mutants have altered affinity for CD81 and SR-BI. (A) JFH1WT (•), JFH1N415D (○), JFH1T416A (▾), JFH1N417S (▵), or JFH1I422L (▪) HCVcc was incubated with different concentrations of hCD81-LEL for 1 h prior to infecting target cells. At 2 days postinfection, virus infectivity was determined by FFU assay. Percent neutralization was calculated by quantifying viral infectivity in the presence of hCD81-LEL relative to standard infection. (B) The levels of WT or mutant E2 in Huh-7 cells transfected with appropriate viral RNAs was first normalized by measuring their binding to the conformation-sensitive anti-E2 human MAb CBH-4B (see Fig. S1 in the supplemental material). Lysates containing equivalent E2 were assessed for binding to hCD81-LEL by ELISA, and the data are presented as the averages of two independent experiments, each performed in triplicate. (C and D) Naive Huh-7 cells were preincubated for 1 h with different amounts of antibodies against (C) CD81 or (D) SR-BI before infection. Cells were then infected with 50 FFU of WT or mutant viruses (key to symbols as in panel A above) for 2 days, and the infectivity levels were determined by FFU assay. The percent neutralization was calculated by quantifying viral infectivity in the presence of inhibitory antibodies relative to a standard “no antibody” infection. (E) Huh7-J20 cells were infected with WT or mutant viruses in the presence or absence of HDL and virus infectivity determined by SEAP assay as described in Materials and Methods. Error bars indicate standard deviation from the mean (n = 3; P = <0.05, unpaired Student t test).
Having established that these mutations influence the HCV-CD81 interaction, we next investigated their effects on SR-BI-dependent entry. Naive cells were preincubated with different concentrations of a neutralizing anti-SRBI rat serum (63) prior to infection with each virus. Interestingly, all mutants were less sensitive than WT to neutralization by this antiserum (Fig. 3D and Table 1). As expected, a control serum had no effect on virus infectivity (data not shown). We next tested the effect of HDL, an SR-BI ligand known to enhance HCV entry through a process that requires the lipid transfer function of SR-BI (see the introduction), on mutant virus infection. As shown in Fig. 3E, while the infectivity of WT was significantly enhanced, the E2 mutants appeared insensitive to HDL treatment. Together, these data suggest that each adaptive mutation alters HDL/SR-BI-mediated uptake of the virus during entry.
TABLE 1.
IC50s of CD81-LEL and inhibitory antibodies for each virus
| Inhibitor | IC50 (μg/ml)a |
|||||
|---|---|---|---|---|---|---|
| WT | N415D | T416A | N417S | G418D | I422L | |
| hCD81-LEL | >50 | 4.4 | 3.4 | 3.7 | 2.0 | 3 |
| Anti-CD81 | 0.12 | 0.1 | 0.13 | 0.07 | 0.12 | 0.13 |
| Anti-SR-BI | 1:560 | 1:40 | 1:25 | <1:20 | 1:170 | 1:100 |
| IgG17 | 12.11 | 0.2 | 0.3 | 0.66 | ND | 0.3 |
| IgG19 | 22 | 1.1 | 1.3 | 1.4 | ND | 2.5 |
| IgG2 | >50 | ND | ND | ND | 1.2 | ND |
| IgG4 | >50 | ND | ND | ND | 1.8 | ND |
| CBH-5 | 0.6 | 0.02 | 0.02 | 0.05 | 0.12 | 0.035 |
| AP33 | 1.5 | NN | 0.06 | NN | NN | 0.12 |
| HC11 | 7.0 | 0.001 | 0.0003 | 0.004 | ND | 0.002 |
| 3/11 | 44.9 | NN | 4.1 | NN | NN | 7.12 |
| AP33 (HCVpp) | 1.0 | NN | 0.01 | NN | ND | 0.02 |
| CBH-5 (HCVpp) | 2.3 | 0.01 | 0.016 | 0.03 | ND | 0.036 |
NN, non-neutralizable; ND, not done. The anti-SR-BI IC50s are represented as serum dilutions.
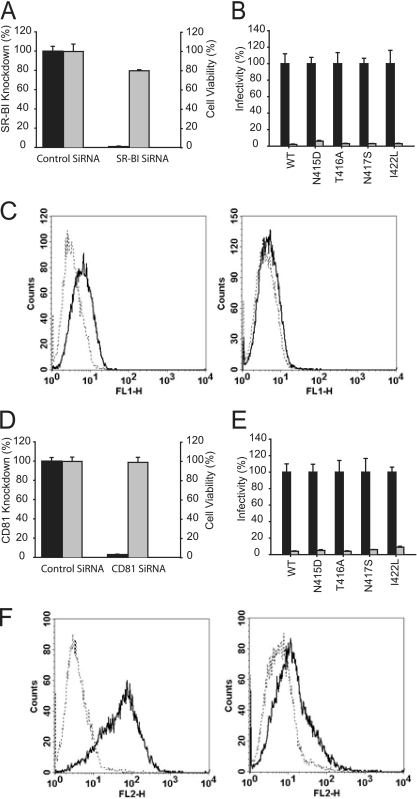
To investigate the possibility of these mutants having reduced SR-BI dependency, two siRNAs targeting different regions of SR-BI mRNA were transfected into Huh-7 cells to silence its expression. At the time of infection, these cells expressed 99% less SR-BI mRNA while maintaining 80% of the control cell viability (Fig. 4A). The knockdown of cell surface-expressed SR-BI was also confirmed by FACS analysis (Fig. 4C). Under these conditions, the infectivity of all viruses was inhibited by 94 to 98%, showing the E2 mutant viruses still require sufficient expression of SR-BI for infection (Fig. 4B). Similarly, efficient knockdown of CD81 reduced the infectivity of all viruses (Fig. 4D to F).
FIG. 4.
Silencing CD81 and SR-BI gene expression inhibits E2 mutant virus infection. Huh-7 cells were transfected with control siRNAs or siRNAs targeting SR-BI (A to C) or CD81 (D to F). At 2 days posttransfection, the cell viability (gray bar) and mRNA expression levels (black bar) of SR-BI (A) and CD81 (D) were measured by ELISA and qRT-PCR, respectively. The expression of SR-BI (C) and CD81 (F) on the surface of Huh-7 cells transfected with control siRNAs (left panel) or receptor-specific siRNAs (right panel) was determined by FACS analysis as described in Materials and Methods. Solid and broken lines represent cells stained with an anti-CD81 or anti-SR-BI antibody and IgG subtype control, respectively. In parallel, the control siRNA-transfected Huh-7 cells (black bars) or the SR-BI (B) or CD81 (E) knockout cells (gray bars) were infected with WT or mutant viruses and the intracellular HCV RNA levels measured by qRT-PCR to quantitate infectivity.
E2 mutations alter sensitivity to neutralizing antibodies.
Previously, we reported a range of polyclonal anti-HCV IgGs purified from HCV-infected patients that inhibited infection after virus attachment to the cell (19). Here, the sensitivity of the WT and the E2 mutant viruses to neutralization by two of these IgG preparations (IgG17 and IgG19) was tested. The degree of inhibition of the WT virus afforded by both of these IgGs was in accordance with our previous findings (19). However, the mutant viruses were more sensitive to neutralization, with IC50s 18- to 60-fold lower for IgG17 and 9- to 20-fold lower for IgG19 (Fig. 5A and B; Table 1). It is noteworthy that these IgGs did not block E2-CD81 interaction (data not shown). As expected, antibodies purified from an uninfected individual (IgG20) had no effect on virus infectivity (data not shown). We next tested the efficiency of neutralization of all viruses by the conformation-sensitive anti-E2 human MAbs (HMAbs), CBH-5 and HC-11. Both of these HMAbs recognize discontinuous overlapping epitopes within the domain B of E2 and inhibit viral entry into cells by blocking the E2-CD81 interaction (28-30, 46). We found that each mutant virus was more sensitive to neutralization by these HMAbs compared to JFH1WT, with the IC50s reducing by 12- to 30-fold for CBH-5 and strikingly, by 3 to 4 log for HC-11 (Fig. 5C and D and Table 1). Together, these results suggest that all four mutations enhance the exposure of antibody neutralizing epitopes on the virus particle.
FIG. 5.
E2 mutant viruses have increased sensitivity to neutralization by human anti-envelope antibodies. JFH1WT (•), JFH1N415D (○), JFH1T416A (▾), JFH1N417S (▵), or JFH1I422L (▪) HCVcc was incubated for 1 h with different amounts of HCV-infected patient IgGs IgG17 (A) or IgG19 (B), or the human MAbs CBH-5 (C) and HC-11 (D) prior to infection of target cells. The level of virus inhibition was assayed as described in Materials and Methods. The percent neutralization was calculated by quantifying viral infectivity in the presence of anti-HCV glycoprotein specific antibodies relative to infection in the absence of antibodies.
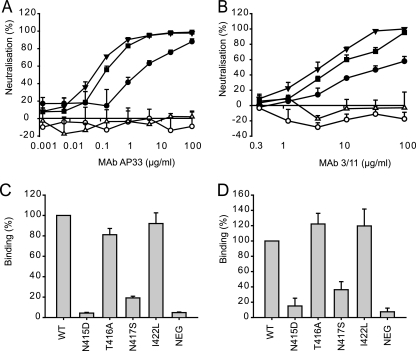
We next measured the neutralization of these viruses using the broadly neutralizing MAbs AP33 and 3/11, which recognize distinct but overlapping epitopes within the highly conserved region of E2 spanning residues 412 to 423 (QLINTNGSWHIN) (56), where our four mutations are located. We found that JFH1T416A and JFH1I422L were highly sensitive to neutralization by both AP33 and 3/11, whereas JFH1N415D and JFH1N417S were completely resistant (Fig. 6A and B, respectively; Table 1). We next tested the reactivity of MAbs AP33 and 3/11 to each mutant E2 by ELISA. Normalized E2 from transfected cell lysates was captured onto GNA coated plates and probed with either AP33 or 3/11. Consistent with the neutralization data, both AP33 and 3/11 showed very weak binding to the E2 from JFH1N415D and JFH1N417S (Fig. 6C and D). Together, the neutralization and ELISA data show that the N415D and N417S mutations disrupt the binding of MAbs AP33 and 3/11 to E2. However, while the reactivity of mutants T416A and I422L to both MAbs was unaltered, they were more sensitive to neutralization by these antibodies. The latter phenotype is similar to what we observed in the hCD81-LEL inhibition and binding assays (Fig. 3A and B), again supporting the notion that local changes may occur to E2 during virion assembly affecting neutralization. The increased sensitivity to neutralization by the rodent MAbs (i.e., where the antibody reactivity is not compromised) together with the heightened inhibition of the mutant viruses to human antibodies described above (Fig. 5) indicates that the mutations may induce global conformational alterations in virion E2 allowing enhanced epitope exposure.
FIG. 6.
E2 mutations alter virus neutralization by MAbs AP33 and 3/11. JFH1WT (•), JFH1N415D (○), JFH1T416A (▾), JFH1N417S (▵), or JFH1I422L (▪) HCVcc was preincubated for 1 h with different concentrations of MAb AP33 (A) and 3/11 (B) before infecting target cells. The level of virus inhibition was assayed as described in Materials and Methods. The percent neutralization was calculated by quantifying viral infectivity in the presence of anti-E2 specific MAbs relative to infection in the absence of antibodies. (C and D) Reactivity of MAb AP33 or 3/11 to HCV E2. WT or mutant E2 from electroporated Huh-7 cells was normalized as described in the legend to Fig. 3 and tested for reactivity to MAb (C) AP33 or (D) 3/11 by GNA-capture ELISA, and the data are presented as the averages of two independent experiments, each performed in triplicate. Reactivity is expressed as the percentage of binding relative to the WT E2.
Infectivity and neutralization profiling in HCVpp system.
We previously showed that T416A mutation in the HCV genotype 1a strain H77 E2 abolished HCVpp infection (47). However, the results presented here show that the same mutation in the strain JFH1 HCVcc system does not affect infectivity. To resolve this discrepancy, we assessed the infectivity of the JFH1 E2 mutants in the HCVpp system. Although no differences in infectivity was observed for WT and T416A in HCVcc, we found a notable reduction in the infectivity of HCVpp carrying the same mutations (Fig. 7A). Nevertheless, neutralization assays using MAbs AP33 (Fig. 7C) and CBH-5 (Fig. 7D) showed that the effects of the mutations on antibody reactivity were very similar in HCVcc and HCVpp (Table 1). These data further support our notion that the mutations within the amino acids 412 to 423 alter the conformation of E2 on the virus particle.
FIG. 7.
E2 mutations affect the infectivity conferred by E1E2 in the HCVpp assay. (A) HCVpp bearing WT JFH1 E2 or mutant JFH1 E2 were generated in HEK-293T cells cotransfected with appropriate constructs as described in Materials and Methods. Naive Huh-7 cells were infected with HCVpp and infectivity was determined by measuring luciferase levels (top panel). Sucrose cushion enriched HCVpp preparations were Western blotted to detect virion incorporation of E2 using an anti-E2 MAb (middle panel) and MLV gag proteins using a gag-specific MAb (bottom panel). (B) Immunoprecipitation of radiolabeled E1 and E2 proteins expressed in HEK-293T cells was performed using the anti-E2 HMAb CBH-5 as described in Materials and Methods. (C and D) HCVpp bearing WT JFH1 E2 (•), JFH1 E2 carrying N415D (○), T416A (▾), N417S (▵), or I422L (▪) mutation were first normalized with respect to their infectivity (luciferase) values and then mixed with MAbs AP33 (B) or CBH-5 (C) 1 h prior to infecting Huh-7 cells. Virus infectivity was measured 3 days postinfection by quantifying luciferase activity. The percent neutralization was calculated by quantifying viral infectivity in the presence of anti-E2 specific MAbs relative to infection in the absence of MAbs.
Using E2 GNA-capture ELISA, we confirmed that the WT and the mutant E2 were expressed in comparable quantities (not shown), and that the mutations affected neither the E2 incorporation into HCVpps nor the E1E2 heterodimer formation (Fig. 7A and B). Thus, the reasons for the lower infectivity of mutant HCVpps are not clear. Several studies have demonstrated functional differences between HCVpp and HCVcc. It is conceivable that the former being a surrogate system may not always mimic the authentic virus in terms of glycoprotein presentation and function. Furthermore, HCVpp purely measure virus entry, excluding complications such as virus spread and RNA replication that exist within the HCVcc system when measuring virus infectivity. Therefore, direct comparisons in infectivity between these two systems are not always appropriate. This point is further strengthened by the observation that the G451R adaptive mutation, which enhances HCVcc infection, renders HCVpps noninfectious (18).
Induced selection of a MAb AP33 escape mutant virus.
The cell culture adaptive E2 mutations characterized above occurred in viral variants that emerged after prolonged passaging of infected cells under standard tissue culture conditions. It is intriguing that they each carry an amino acid substitution within a highly conserved E2 region conferring significant phenotypic changes in relation to antibody neutralization and virus entry. We sought to determine whether neutralization escape mutants within the MAb AP33 epitope could be generated under constant antibody selective pressure, and if so, whether such mutants would be phenotypically similar to those arising by spontaneous selection. JFH1WT virus was subjected to several rounds of growth in the continuous presence of a neutralizing concentration of AP33 in the two-chamber Thincert tissue culture system as described in Materials and Methods. The antibody was excluded in a parallel control experiment. The emergence of AP33 escape mutants was examined by dual immunostaining, using MAb AP33 and the sheep anti-NS5A antiserum, of naive cells infected with virus collected at each round of selection. The infectious virus yield arising from cells under antibody selective pressure was considerably lower during the early passages compared to the control cultures. A majority (>90%) of the virus in these early round preparations produced infectious foci in naive cells that were MAb AP33-negative but anti-NS5A-positive in immunofluorescence assay (data not shown). The proportion of the variant virus relative to the WT virus increased at each round of selection, and reached 100% by the eighth passage. Nucleotide sequence analysis of the E1 and E2 coding region of the RT-PCR product of early passage infected cell RNA revealed a single mutation (G to D) in E2 at residue 418 (G418D), which remained fixed throughout the passaging period. In contrast, no mutations were found in the E1 and E2 coding regions of virus passaged in parallel in the absence of MAb AP33.
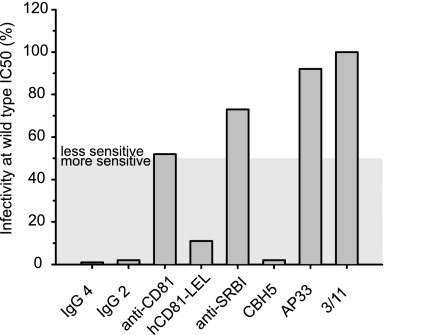
The glycine at position 418 is one of the residues critical for AP33 recognition (56). To verify that the G418D substitution was responsible for the escape of AP33 neutralization, it was introduced into the JFH-1WT genome. We then characterized the phenotype of the JFH1G418D virus in terms of virus infectivity, receptor affinity, and antibody neutralization. Similar to all of the adaptive mutants described above, the JFH1G418D virus was more sensitive to neutralization by the patient IgGs, the human anti-E2 MAb CBH-5 and soluble hCD81-LEL, and less sensitive to inhibition by the anti-SR-BI antiserum (Fig. 8A and Table 1). Furthermore, like JFH1N415D and JFH1N417S, this mutant was resistant to neutralization by both MAbs AP33 and 3/11. As with the adaptive mutants, the infectivity of JFH1G418D was not drastically altered (data not shown).
FIG. 8.
Characterization of JFH1G418D virus. Huh7-J20 cells were infected with the JFH1WT or JFH1G418D virus that had been preincubated with different concentrations of IgG2 or IgG4, hCD81-LEL, or the anti-E2 MAbs AP33, 3/11, or CBH-5. Alternatively, Huh7-J20 cells preincubated with different concentrations of the anti-CD81 MAb or an anti-SR-BI antiserum were infected with JFH1WT or JFH1G418D virus. At 3 days postinfection the virus infectivity levels were determined by measuring SEAP activity in the culture medium. The results are presented as the percent inhibition of JFH1G418D infection by the indicated molecules at 50% inhibitory (IC50) concentrations for the WT virus.
Amino acid sequence analysis.
We next investigated the frequency of changes, if any, of the relevant E2 residues in naturally occurring HCV isolates by sequence alignment. This analysis showed that substitution from N to D at position 415 was very rare in naturally occurring sequences, being found in only a single sequence among a sample of 1,311 full-length E2 protein sequences (Table 2). The substitutions from T to A at position 416 and from N to S at position 417 were more common, being found 13 and 17 times, respectively, within the same sample. Position 416 was more generally variable, with 182 of the 1,311 sequences differing from this residue in the JFH1 sequence. Position 418, in contrast, was extremely conserved. Only 2 of 1,311 sequences varied from the G found in JFH1, and neither of these has the G-to-D substitution produced here. The substitution from I to L at position 422 was also rare, being found only five times.
TABLE 2.
Naturally occurring substitutions in 1311 HCV E2 protein sequences
| Position | JFH1 residue | Varianta | No.b | Totalc | Prop.d | Accession no. (genotype)e |
|---|---|---|---|---|---|---|
| 415 | N | D | 1 | 37 | 0.03 | EU482838 (1a) |
| 416 | T | A | 13 | 182 | 0.07 | AY956468 (1a), AY958005 (3a), EU155215 (1a), EU155249 (1a), EU155282 (1a), EU155285 (1a), EU155288 (1a), EU155379 (1a), EU255930 (1a), EU255980 (1a), EU482845 (1a), EU482836 (1a), EU643835 (6) |
| 417 | N | S | 17 | 27 | 0.63 | EU256046 (1a), EU256031 (1a), EU255964 (1a), EU255952 (1a), EU255943 (1a), EU155354 (1a), EU155347 (1a), EU155297 (1a), EU155274 (1a), EU155215 (1a), EF407468 (1b), EF407466 (1a), EF407477 (1a), EU407415 (1a), EF026073 (2/5 natural recombinant), AY957988 (3a), AM408911 (2/5) |
| 418 | G | D | 0 | 2 | 0.00 | |
| 422 | I | L | 5 | 38 | 0.13 | AB047643 (2a), AF271632 (1a), FJ828970 (1a), FJ828971 (1a), M62321 (1a) |
That is, substitutions as described in the text.
That is, the total number of sequences in a sample of 1,311 HCV E2 proteins with the same substitution.
That is, the total number of substituted residues in the sample of 1,311 (see Table 3).
Prop., the proportion of naturally occurring substitutions that are identical to the substitutions produced in the present study.
The accession number(s) of HCV sequences (genotypes are shown in parentheses) carrying the relevant variant is listed.
Analysis of the total number of naturally occurring substitutions at the relevant E2 positions identified the residue at position 415 as the most variable in terms of number of residues used (eight in total), contrasting with the use of only G and very rarely S at position 418 (Table 3). Although position 416 was the most likely to be substituted in naturally occurring sequences with 182 substitutions found, it used fewer residues than position 415. Position 422 had almost the same overall number of substituted sequences as position 415 (38 versus 37) but used a far lower number of residues (4 compared to 8).
TABLE 3.
Total number of naturally occurring substitutions in 1,311 HCV E2 protein sequences
| Protein sequence | Residue at position: |
||||
|---|---|---|---|---|---|
| 415 | 416 | 417 | 418 | 422 | |
| JFH1 | N | T | N | G | I |
| Variantsa | K | N | S | S | L |
| 1 | Y | S | D | V | |
| 2 | H | A | H | T | |
| 3 | S | I | G | ||
| 4 | T | K | T | ||
| 5 | R | R | |||
| 6 | D | ||||
| Total no.b | 37 | 182 | 27 | 2 | 38 |
Substitutions occurring in the sample of 1,311 E2 protein sequences.
Total number of sequences with a substitution. Position 416 is the most polymorphic in terms of total number of substitutions at 14% (182 in 1,311 sequences). However, position 415 has a greater diversity of variants (8 amino acids used at least once, despite only 37 substitutions).
DISCUSSION
In this study, we demonstrate that several mutations located within a conserved E2 region encompassing residues 412 to 423 influence the viral glycoprotein interaction(s) with cell receptors and neutralizing antibodies. This region carries residues that are critical for recognition of two broadly neutralizing antibodies used here, MAbs AP33 and 3/11 (45, 56). These residues—L413, N415, G418, and W420 (AP33) and N415, W420, and H421 (3/11)—are well conserved, which is relevant for future vaccine design. However, this requires a better understanding of the epitope-antibody interaction at the structural level. In this respect, studies of viral variants that escape antibody-mediated neutralization should provide useful information and help identify the role of other residues in antigen-antibody interaction.
Three of the five HCV JFH1 E2 mutations (N415D, N417S, and G418D) described in the present study abrogated E2 reactivity to, and virus neutralization by, MAbs AP33 and 3/11. The N415D and N417S mutations arose spontaneously during cell passaging, while the G418D was generated under AP33 selective pressure. Our amino acid sequence alignment shows that N415D and G418D are extremely rare (1 and 0 occurrences, respectively, out of a sample of 1,311 sequences) in natural sequences, whereas N417S, although by no means common, is the major naturally occurring variant (17 occurrences of 27) (Table 2). Recently, we described a MAb AP33 neutralization escape variant of a genotype 1a/2a chimeric HCVcc following repetitive rounds of antibody neutralization and amplification in cell culture (17). This virus contained N415Y and E655G mutations in the E2 glycoprotein. The N415Y mutation alone severely attenuated MAb AP33 (and 3/11) recognition and neutralization, but it did not enhance sensitivity to neutralization by other human anti-E2 MAbs and, interestingly, it substantially reduced viral fitness. Y at position 415 occurs 9 times in natural HCV sequences. Of the 37 variant residues at this position (Table 3) it is the third most common, found in genotypes 1a, 1b, 4b, and 6. In contrast, the N415D mutation, although found much rarely in patient isolates, maintained HCVcc fitness, as was the case for the other E2 cell culture-adaptive mutations characterized in the present study. This is likely due to the nature of the substituted amino acid and/or genotypic differences in the E2 glycoprotein. The difference in the E2 sequence could also account for the fact that the repetitive passaging of the genotype 2a JFH1 HCVcc in the presence of a neutralizing concentration of MAb AP33 allowed selection of a virus carrying the E2 G418D substitution. However, the different selection protocols used between the previous (17) and the present study may, at least in part, be responsible.
We previously showed that alanine replacement of the residue N417 in the HCV genotype 1a H77 E2 moderately reduced MAb AP33 and 3/11 binding (56). In the present study, a change to serine at this position in the genotype 2a JFH1 strain drastically reduced AP33 and 3/11 binding, rendering JFH1N417S HCVcc resistant to neutralization by either antibody and highlighting the contribution of N417 to their binding sites on E2. Furthermore, the residue N417 is part of an N-linked glycosylation site (22, 47), the removal of which from genotype 1a E2 (N417Q) has been shown to increase the sensitivity of HCVpp to antibody neutralization and to increase CD81 binding (22). The latter observations are also in keeping with our findings. Our data show that the molecular weight of the genotype 2a E2 N417S mutant is identical to the WT glycoprotein (Fig. 7b); however, it would be inappropriate to conclude on this basis that this site is not used for glycosylation. This is because the N417S change potentially creates a new N glycosylation site over positions 415 to 417 (i.e., a change from NTN to NTS, see Fig. 1b), which, if utilized, will not alter the migration of the mutant E2 in SDS-PAGE. Clearly, further studies are required to clarify this issue. The N417S change occurs in 17 of the 27 variants at this position (Table 2), suggesting that it may be naturally selected.
Bungyoku et al. (10) previously showed that the E2 T416A mutation in a chimeric J6/JFH1 HCVcc background does not alter virus infectivity in the Huh-7-derived sub line Huh7.5 (7). In accordance with these data, we find here that the same mutation has no significant affect on HCVcc spread in Huh-7 cells. Furthermore, we previously showed that the T416A mutation in the genotype 1a HCVpp system moderately reduced MAb AP33 and 3/11 recognition (56), enhanced CD81 binding, and abrogated pseudoparticle infectivity (47). In contrast, we show here that this mutation in the genotype 2a JFH1 HCVcc enhances E2 reactivity to MAbs AP33 and 3/11 and maintains WT virus infectivity. Together, the different infection systems, viral isolates and/or cell lines used in each study likely account for these inconsistencies. T416A is one of seven variants at a locus subject to positive selection (9), and although occurring 13 times in our sample, is only a minor component (7% of substitutions) of the extensive variability in this position.
The I422L mutation was first isolated alongside other structural and nonstructural mutations after several rounds of JFH1 HCVcc passaging in Huh-7.5 cells and was shown not to alter virus infectivity, which is in agreement with our findings in Huh-7 cells (27). Consistent with our previous findings for I422A (56), the I422L mutation did not affect E2 recognition by MAbs AP33 and 3/11, confirming that this residue is not critical for E2 recognition by either MAb. I422L occurs five times in our sample of 1311 E2 sequences, constituting 13% of the substitutions at this position (Table 2).
The reduced sensitivity of these mutants to inhibition by the anti-SR-BI antibody was an unexpected result. In keeping with these observations, we found that all of the mutants studied here were insensitive to HDL-mediated enhancement of virus infection. The exact mechanism by which the HDL-SR-BI association facilitates HCV entry is currently unknown. Although no interaction between HDL and HCVpp particles has been demonstrated in culture medium, the possibility of an association occurring at a postbinding stage cannot be discounted (58). More importantly, the binding of HDL to HCVcc virions has yet to be investigated. Also, it has been postulated that the lipid transfer events resulting from HDL-SR-BI binding, known to be essential for regulating the properties of cells membranes, may affect the fusion efficiency of the HCV envelope with cell membranes (58). SR-BI was first identified as a putative HCV receptor based on its ability to bind soluble, truncated E2 (sE2) via HVR1 (53). However, sE2 may not fully mimic E2 structures on the HCV virion (11, 28) and an interaction between SR-BI and the E1E2 heterodimers has yet to be confirmed. In addition, the initial binding of serum HCV to SR-BI was found not to be mediated by HVR-1 or indeed other regions of the E2 glycoprotein. Instead, the association of VLDL with virus particles appeared to play a critical role in the primary interaction with SR-BI (40). Thus, there is much uncertainty as to how HCV utilizes this receptor during virus entry. In the absence of definitive assays that can measure an interaction between SR-BI with full-length E1E2 or indeed HCVcc virions, it is difficult to decipher the effects caused by our E2 mutations to the entry process via this receptor. However, the siRNA knockdown experiment shows that SR-BI is not dispensable for the mutant virus entry.
Substitution of N415, T416, and N417 resulted in increased E2-CD81 binding, whereas the binding of E2 I422L mutant to CD81 was unaltered. Moreover, each mutant virus, including JFH1G418D, exhibited a significantly greater sensitivity to neutralization by hCD81-LEL, suggesting an increased affinity of the mutated glycoproteins for CD81. This suggests that the adaptive mutations improve the accessibility of CD81 binding residues of the E2 present on mature virions. The heightened inhibition of these mutants by a range of human anti-HCV glycoprotein antibodies (and by the anti-E2 rodent MAbs AP33 and 3/11 in the case of mutants T416A and I422L) supports this theory.
Other studies have identified cell culture-adaptive mutations within the E2 glycoprotein (13, 18, 65). In particular, the mutation G451R has been extensively characterized (18, 65). This single mutation increases the buoyant density of the virus, as well as its ability to bind CD81. G451R also reduces SR-BI dependency and increases virus sensitivity to neutralization by E2 specific antibodies, indicating the greater availability of epitopes on the mutant particle. The mutations characterized in the present study have very similar phenotypes to G451R, suggesting that the E2 mutations selected in HCVcc may have arisen in response to similar selective pressures. For example, to persist during long-term culture subtle alterations to E2 conformation may enhance virus-receptor interactions and maintain spread. In line with this, it has been shown that during persistent infection of JFH1 in cell culture certain cell populations emerge that are less permissive to HCV infection due to a decrease in the cell surface expression of CD81 (65). Although this possibility was not investigated in our study or the others (10, 27, 52), the increased affinity of each mutant to CD81 (Fig. 3) may assist viral spread in cells presenting less CD81.
The E2 region studied here lies immediately C-terminal to the HVR-1, in which positive selection is active. In contrast, the region of interest has only a single site detected as positively selected—that at position 416 (9). Consistent with this, the survey of 1311 E2 sequences reported here shows that 182 of them are variants (ca. 14%) at position 416. At the remaining sites of interest, substitution is much rarer, never higher than 4% of the total sample (Table 3). In addition, the specific mutations described here occur relatively rarely in natural HCV sequences (Table 2). For instance, the G-to-D change at position 418 is not found at all in our sample of 1,311 sequences. Indeed, this position is extremely conserved, with only two substitutions found in the full-length E2 sequences sampled (Tables 2 and 3). Both of those substitutions are G to S and occur in closely related sequences (not shown). The N415D change is similarly very rare in our sample, occurring only once.
The I-to-L substitution at position 422 is also rare (Table 2). Where substitution does occur naturally at position 422, it is confined to relatively hydrophobic residues (Table 3), suggesting that a selective constraint for hydrophobicity applies at this position. In contrast, the N417S change constitutes 63% of all variants found at that position, occurring 17 times (Table 2). The T416A change is intermediate in frequency, constituting 7% of all naturally occurring substitutions at that position. The naturally occurring variants at all positions are found in a wide range of genotypes (Table 2). For instance, position 416 has T to A substitution in genotypes 1a, 3a, and 6 and position 417 has N-to-S substitutions in 1a, 1b, 3a, and 2/5 recombinants. The substitutions produced in the present study at positions 415 to 417 and 422 are spontaneous occurrences in long-term cell passage, where selective conditions may be very different to those found in the natural host. This is a plausible explanation for the relative rarity of these substitutions in naturally occurring sequences.
Broadly neutralizing MAbs to this conserved region hold great promise as therapeutics. Moreover, the epitope recognized by these MAbs can be considered a valid lead for future vaccine design. However, an in-depth understanding of how the neutralizing antibodies interact with E2 is necessary, for both effective vaccine design and understanding the role of the epitope in receptor interaction and virus entry. An additional challenge for vaccine design is the emergence of viral variants during the course of infection that escape antibody neutralization. In vivo, the prevalence of antibodies reactive to the E2 region 412-423 (QLINTNGSWHIN) is <2.5% (55). Therefore, there is no great selective pressure acting on this region driving the emergence of neutralization escape mutations. If such mutants do arise spontaneously, they are likely to confer either reduced virus fitness (17) or an increased vulnerability to neutralization by circulating antibodies targeting various glycoprotein regions, thereby eliminating these variants from the virus pool. In summary, our data contribute to further defining the role of key residues within the HCV E2 412-423 region that influence virus-receptor interactions and antibody-mediated neutralization.
Supplementary Material
Acknowledgments
We are grateful to F.-L. Cosset, J. Dubuisson, M. Harris, J. A. McKeating, C. M. Rice, and T. Wakita for provision of reagents. We thank Gabrielle Vieyres for expert technical assistance.
This study was funded by the Medical Research Council, United Kingdom, and European Union FP6 contract MRTN-CT-2006-035599 and supported in part by PHS grants HL079381 and AI081903 to S.K.H.F.
Footnotes
Published ahead of print on 17 March 2010.
Supplemental material for this article may be found at http://jvi.asm.org/.
REFERENCES
- 1.Allander, T., K. Drakenberg, A. Beyene, D. Rosa, S. Abrignani, M. Houghton, A. Widell, L. Grillner, and M. A. Persson. 2000. Recombinant human monoclonal antibodies against different conformational epitopes of the E2 envelope glycoprotein of hepatitis C virus that inhibit its interaction with CD81. J. Gen. Virol. 81:2451-2459. [DOI] [PubMed] [Google Scholar]
- 2.Barth, H., C. Schafer, M. I. Adah, F. Zhang, R. J. Linhardt, H. Toyoda, A. Kinoshita-Toyoda, T. Toida, T. H. Van Kuppevelt, E. Depla, F. Von Weizsacker, H. E. Blum, and T. F. Baumert. 2003. Cellular binding of hepatitis C virus envelope glycoprotein E2 requires cell surface heparan sulfate. J. Biol. Chem. 278:41003-41012. [DOI] [PubMed] [Google Scholar]
- 3.Bartosch, B., J. Dubuisson, and F. L. Cosset. 2003. Infectious hepatitis C virus pseudo-particles containing functional E1-E2 envelope protein complexes. J. Exp. Med. 197:633-642. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Bartosch, B., G. Verney, M. Dreux, P. Donot, Y. Morice, F. Penin, J. M. Pawlotsky, D. Lavillette, and F. L. Cosset. 2005. An interplay between hypervariable region 1 of the hepatitis C virus E2 glycoprotein, the scavenger receptor BI, and high-density lipoprotein promotes both enhancement of infection and protection against neutralizing antibodies. J. Virol. 79:8217-8229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bartosch, B., A. Vitelli, C. Granier, C. Goujon, J. Dubuisson, S. Pascale, E. Scarselli, R. Cortese, A. Nicosia, and F. L. Cosset. 2003. Cell entry of hepatitis C virus requires a set of coreceptors that include the CD81 tetraspanin and the SR-BI scavenger receptor. J. Biol. Chem. 278:41624-41630. [DOI] [PubMed] [Google Scholar]
- 6.Benedicto, I., F. Molina-Jimenez, B. Bartosch, F. L. Cosset, D. Lavillette, J. Prieto, R. Moreno-Otero, A. Valenzuela-Fernandez, R. Aldabe, M. Lopez-Cabrera, and P. L. Majano. 2009. The tight junction-associated protein occludin is required for a postbinding step in hepatitis C virus entry and infection. J. Virol. 83:8012-8020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Blight, K. J., J. A. McKeating, and C. M. Rice. 2002. Highly permissive cell lines for subgenomic and genomic hepatitis C virus RNA replication. J. Virol. 76:13001-13014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Broering, T. J., K. A. Garrity, N. K. Boatright, S. E. Sloan, F. Sandor, W. D. Thomas, Jr., G. Szabo, R. W. Finberg, D. M. Ambrosino, and G. J. Babcock. 16 September 2009, posting date. Identification and characterization of broadly neutralizing human monoclonal antibodies directed against the E2 envelope glycoprotein of hepatitis C virus. J. Virol. doi: 10.1128/JVI.01138-09. [DOI] [PMC free article] [PubMed]
- 9.Brown, R. J., V. S. Juttla, A. W. Tarr, R. Finnis, W. L. Irving, S. Hemsley, D. R. Flower, P. Borrow, and J. K. Ball. 2005. Evolutionary dynamics of hepatitis C virus envelope genes during chronic infection. J. Gen. Virol. 86:1931-1942. [DOI] [PubMed] [Google Scholar]
- 10.Bungyoku, Y., I. Shoji, T. Makine, T. Adachi, K. Hayashida, M. Nagano-Fujii, Y. H. Ide, L. Deng, and H. Hotta. 2009. Efficient production of infectious hepatitis C virus with adaptive mutations in cultured hepatoma cells. J. Gen. Virol. 90:1681-1691. [DOI] [PubMed] [Google Scholar]
- 11.Clayton, R. F., A. Owsianka, J. Aitken, S. Graham, D. Bhella, and A. H. Patel. 2002. Analysis of antigenicity and topology of E2 glycoprotein present on recombinant hepatitis C virus-like particles. J. Virol. 76:7672-7682. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cormier, E. G., R. J. Durso, F. Tsamis, L. Boussemart, C. Manix, W. C. Olson, J. P. Gardner, and T. Dragic. 2004. L-SIGN (CD209L) and DC-SIGN (CD209) mediate transinfection of liver cells by hepatitis C virus. Proc. Natl. Acad. Sci. U. S. A. 101:14067-14072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Delgrange, D., A. Pillez, S. Castelain, L. Cocquerel, Y. Rouille, J. Dubuisson, T. Wakita, G. Duverlie, and C. Wychowski. 2007. Robust production of infectious viral particles in Huh-7 cells by introducing mutations in hepatitis C virus structural proteins. J. Gen. Virol. 88:2495-2503. [DOI] [PubMed] [Google Scholar]
- 14.Dreux, M., T. Pietschmann, C. Granier, C. Voisset, S. Ricard-Blum, P. E. Mangeot, Z. Keck, S. Foung, N. Vu-Dac, J. Dubuisson, R. Bartenschlager, D. Lavillette, and F. L. Cosset. 2006. High-density lipoprotein inhibits hepatitis C virus-neutralizing antibodies by stimulating cell entry via activation of the scavenger receptor BI. J. Biol. Chem. 281:18285-18295. [DOI] [PubMed] [Google Scholar]
- 15.Evans, M. J., T. von Hahn, D. M. Tscherne, A. J. Syder, M. Panis, B. Wolk, T. Hatziioannou, J. A. McKeating, P. D. Bieniasz, and C. M. Rice. 2007. Claudin-1 is a hepatitis C virus coreceptor required for a late step in entry. Nature 446:801-805. [DOI] [PubMed] [Google Scholar]
- 16.Flint, M., C. Maidens, L. D. Loomis-Price, C. Shotton, J. Dubuisson, P. Monk, A. Higginbottom, S. Levy, and J. A. McKeating. 1999. Characterization of hepatitis C virus E2 glycoprotein interaction with a putative cellular receptor, CD81. J. Virol. 73:6235-6244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gal-Tanamy, M., Z. Y. Keck, M. Yi, J. A. McKeating, A. H. Patel, S. K. Foung, and S. M. Lemon. 2008. In vitro selection of a neutralization-resistant hepatitis C virus escape mutant. Proc. Natl. Acad. Sci. U. S. A. 105:19450-19455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Grove, J., S. Nielsen, J. Zhong, M. F. Bassendine, H. E. Drummer, P. Balfe, and J. A. McKeating. 2008. Identification of a residue in hepatitis C virus E2 glycoprotein that determines scavenger receptor BI and CD81 receptor dependency and sensitivity to neutralizing antibodies. J. Virol. 82:12020-12029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Haberstroh, A., E. K. Schnober, M. B. Zeisel, P. Carolla, H. Barth, H. E. Blum, F.-L. Cosset, G. Koutsoudakis, R. Bartenschlager, A. Union, E. Depla, A. Owsianka, A. H. Patel, C. Schuster, F. Stoll-Keller, M. Doffoël, M. Dreux, and T. F. Baumert. 2008. Neutralizing host responses in hepatitis C virus infection target viral entry at post-binding steps and membrane fusion. Gastroenterology 135:1719-1728. [DOI] [PubMed] [Google Scholar]
- 20.Hadlock, K. G., R. E. Lanford, S. Perkins, J. Rowe, Q. Yang, S. Levy, P. Pileri, S. Abrignani, and S. K. Foung. 2000. Human monoclonal antibodies that inhibit binding of hepatitis C virus E2 protein to CD81 and recognize conserved conformational epitopes. J. Virol. 74:10407-10416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Helle, F., and J. Dubuisson. 2008. Hepatitis C virus entry into host cells. Cell Mol. Life Sci. 65:100-112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Helle, F., A. Goffard, V. Morel, G. Duverlie, J. McKeating, Z. Y. Keck, S. Foung, F. Penin, J. Dubuisson, and C. Voisset. 2007. The neutralizing activity of anti-HCV antibodies is modulated by specific glycans on the E2 envelope protein. J. Virol. 81:8101-8111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Iro, M., J. Witteveldt, A. G. Angus, I. Woerz, A. Kaul, R. Bartenschlager, and A. H. Patel. 2009. A reporter cell line for rapid and sensitive evaluation of hepatitis C virus infectivity and replication. Antivir. Res. 83:148-155. [DOI] [PubMed] [Google Scholar]
- 24.Johansson, D. X., C. Voisset, A. W. Tarr, M. Aung, J. K. Ball, J. Dubuisson, and M. A. Persson. 2007. Human combinatorial libraries yield rare antibodies that broadly neutralize hepatitis C virus. Proc. Natl. Acad. Sci. U. S. A. 104:16269-16274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kapadia, S. B., H. Barth, T. Baumert, J. A. McKeating, and F. V. Chisari. 2007. Initiation of hepatitis C virus infection is dependent on cholesterol and cooperativity between CD81 and scavenger receptor B type I. J. Virol. 81:374-383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Katoh, K., K. Kuma, H. Toh, and T. Miyata. 2005. MAFFT version 5: improvement in accuracy of multiple sequence alignment. Nucleic Acids Res. 33:511-518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kaul, A., I. Woerz, P. Meuleman, G. Leroux-Roels, and R. Bartenschlager. 2007. Cell culture adaptation of hepatitis C virus and in vivo viability of an adapted variant. J. Virol. 81:13168-131679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Keck, Z. Y., T. K. Li, J. Xia, B. Bartosch, F. L. Cosset, J. Dubuisson, and S. K. Foung. 2005. Analysis of a highly flexible conformational immunogenic domain a in hepatitis C virus E2. J. Virol. 79:13199-13208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Keck, Z. Y., T. K. Li, J. Xia, M. Gal-Tanamy, O. Olson, S. H. Li, A. H. Patel, J. K. Ball, S. M. Lemon, and S. K. Foung. 2008. Definition of a conserved immunodominant domain on hepatitis C virus E2 glycoprotein by neutralizing human monoclonal antibodies. J. Virol. 82:6061-6066. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Keck, Z. Y., A. Op De Beeck, K. G. Hadlock, J. Xia, T. K. Li, J. Dubuisson, and S. K. Foung. 2004. Hepatitis C virus E2 has three immunogenic domains containing conformational epitopes with distinct properties and biological functions. J. Virol. 78:9224-9232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Krieger, M. 2001. Scavenger receptor class B type I is a multiligand HDL receptor that influences diverse physiologic systems. J. Clin. Invest. 108:793-797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Lavillette, D., A. W. Tarr, C. Voisset, P. Donot, B. Bartosch, C. Bain, A. H. Patel, J. Dubuisson, J. K. Ball, and F. L. Cosset. 2005. Characterization of host-range and cell entry properties of the major genotypes and subtypes of hepatitis C virus. Hepatology 41:265-274. [DOI] [PubMed] [Google Scholar]
- 33.Law, M., T. Maruyama, J. Lewis, E. Giang, A. W. Tarr, Z. Stamataki, P. Gastaminza, F. V. Chisari, I. M. Jones, R. I. Fox, J. K. Ball, J. A. McKeating, N. M. Kneteman, and D. R. Burton. 2008. Broadly neutralizing antibodies protect against hepatitis C virus quasispecies challenge. Nat. Med. 14:25-27. [DOI] [PubMed] [Google Scholar]
- 34.Levy, S., S. C. Todd, and H. T. Maecker. 1998. CD81 (TAPA-1): a molecule involved in signal transduction and cell adhesion in the immune system. Annu. Rev. Immunol. 16:89-109. [DOI] [PubMed] [Google Scholar]
- 35.Lindenbach, B. D., M. J. Evans, A. J. Syder, B. Wolk, T. L. Tellinghuisen, C. C. Liu, T. Maruyama, R. O. Hynes, D. R. Burton, J. A. McKeating, and C. M. Rice. 2005. Complete replication of hepatitis C virus in cell culture. Science 309:623-626. [DOI] [PubMed] [Google Scholar]
- 36.Liu, S., W. Yang, L. Shen, J. R. Turner, C. B. Coyne, and T. Wang. 2009. Tight junction proteins claudin-1 and occludin control hepatitis C virus entry and are downregulated during infection to prevent superinfection. J. Virol. 83:2011-2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Lozach, P. Y., A. Amara, B. Bartosch, J. L. Virelizier, F. Arenzana-Seisdedos, F. L. Cosset, and R. Altmeyer. 2004. C-type lectins L-SIGN and DC-SIGN capture and transmit infectious hepatitis C virus pseudotype particles. J. Biol. Chem. 279:32035-32045. [DOI] [PubMed] [Google Scholar]
- 38.Lozach, P. Y., H. Lortat-Jacob, A. de Lacroix de Lavalette, I. Staropoli, S. Foung, A. Amara, C. Houles, F. Fieschi, O. Schwartz, J. L. Virelizier, F. Arenzana-Seisdedos, and R. Altmeyer. 2003. DC-SIGN and L-SIGN are high-affinity binding receptors for hepatitis C virus glycoprotein E2. J. Biol. Chem. 278:20358-20366. [DOI] [PubMed] [Google Scholar]
- 39.Macdonald, A., K. Crowder, A. Street, C. McCormick, K. Saksela, and M. Harris. 2003. The hepatitis C virus nonstructural NS5A protein inhibits activating protein-1 function by perturbing ras-ERK pathway signaling. J. Biol. Chem. 278:17775-17784. [DOI] [PubMed] [Google Scholar]
- 40.Maillard, P., T. Huby, U. Andreo, M. Moreau, J. Chapman, and A. Budkowska. 2006. The interaction of natural hepatitis C virus with human scavenger receptor SR-BI/ClaI is mediated by ApoB-containing lipoproteins. FASEB J. 20:735-737. [DOI] [PubMed] [Google Scholar]
- 41.Molina, S., V. Castet, C. Fournier-Wirth, L. Pichard-Garcia, R. Avner, D. Harats, J. Roitelman, R. Barbaras, P. Graber, P. Ghersa, M. Smolarsky, A. Funaro, F. Malavasi, D. Larrey, J. Coste, J. M. Fabre, A. Sa-Cunha, and P. Maurel. 2007. The low-density lipoprotein receptor plays a role in the infection of primary human hepatocytes by hepatitis C virus. J. Hepatol. 46:411-419. [DOI] [PubMed] [Google Scholar]
- 42.Moradpour, D., F. Penin, and C. M. Rice. 2007. Replication of hepatitis C virus. Nat. Rev. Microbiol. 5:453-463. [DOI] [PubMed] [Google Scholar]
- 43.Nakabayashi, H., K. Taketa, K. Miyano, T. Yamane, and J. Sato. 1982. Growth of human hepatoma cells lines with differentiated functions in chemically defined medium. Cancer Res. 42:3858-3863. [PubMed] [Google Scholar]
- 44.Owsianka, A., R. F. Clayton, L. D. Loomis-Price, J. A. McKeating, and A. H. Patel. 2001. Functional analysis of hepatitis C virus E2 glycoproteins and virus-like particles reveals structural dissimilarities between different forms of E2. J. Gen. Virol. 82:1877-1883. [DOI] [PubMed] [Google Scholar]
- 45.Owsianka, A., A. W. Tarr, V. S. Juttla, D. Lavillette, B. Bartosch, F. L. Cosset, J. K. Ball, and A. H. Patel. 2005. Monoclonal antibody AP33 defines a broadly neutralizing epitope on the hepatitis C virus E2 envelope glycoprotein. J. Virol. 79:11095-11104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Owsianka, A. M., A. W. Tarr, Z. Y. Keck, T. K. Li, J. Witteveldt, R. Adair, S. K. Foung, J. K. Ball, and A. H. Patel. 2008. Broadly neutralizing human monoclonal antibodies to the hepatitis C virus E2 glycoprotein. J. Gen. Virol. 89:653-659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Owsianka, A. M., J. M. Timms, A. W. Tarr, R. J. Brown, T. P. Hickling, A. Szwejk, K. Bienkowska-Szewczyk, B. J. Thomson, A. H. Patel, and J. K. Ball. 2006. Identification of conserved residues in the E2 envelope glycoprotein of the hepatitis C virus that are critical for CD81 binding. J. Virol. 80:8695-8704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Patel, A. H., J. Wood, F. Penin, J. Dubuisson, and J. A. McKeating. 2000. Construction and characterization of chimeric hepatitis C virus E2 glycoproteins: analysis of regions critical for glycoprotein aggregation and CD81 binding. J. Gen. Virol. 81:2873-2883. [DOI] [PubMed] [Google Scholar]
- 49.Perotti, M., N. Mancini, R. A. Diotti, A. W. Tarr, J. K. Ball, A. Owsianka, R. Adair, A. H. Patel, M. Clementi, and R. Burioni. 2008. Identification of a broadly cross-reacting and neutralizing human monoclonal antibody directed against the hepatitis C virus E2 protein. J. Virol. 82:1047-1052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pileri, P., Y. Uematsu, S. Campagnoli, G. Galli, F. Falugi, R. Petracca, A. J. Weiner, M. Houghton, D. Rosa, G. Grandi, and S. Abrignani. 1998. Binding of hepatitis C virus to CD81. Science 282:938-941. [DOI] [PubMed] [Google Scholar]
- 51.Ploss, A., M. J. Evans, V. A. Gaysinskaya, M. Panis, H. You, Y. P. de Jong, and C. M. Rice. 2009. Human occludin is a hepatitis C virus entry factor required for infection of mouse cells. Nature 457:882-886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Russell, R. S., J. C. Meunier, S. Takikawa, K. Faulk, R. E. Engle, J. Bukh, R. H. Purcell, and S. U. Emerson. 2008. Advantages of a single-cycle production assay to study cell culture-adaptive mutations of hepatitis C virus. Proc. Natl. Acad. Sci. U. S. A. 105:4370-4375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Scarselli, E., H. Ansuini, R. Cerino, R. M. Roccasecca, S. Acali, G. Filocamo, C. Traboni, A. Nicosia, R. Cortese, and A. Vitelli. 2002. The human scavenger receptor class B type I is a novel candidate receptor for the hepatitis C virus. EMBO J. 21:5017-5025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Tamura, K., J. Dudley, M. Nei, and S. Kumar. 2007. MEGA4: Molecular Evolutionary Genetics Analysis (MEGA) software version 4.0. Mol. Biol. Evol. 24:1596-1599. [DOI] [PubMed] [Google Scholar]
- 55.Tarr, A. W., A. M. Owsianka, D. Jayaraj, R. J. Brown, T. P. Hickling, W. L. Irving, A. H. Patel, and J. K. Ball. 2007. Determination of the human antibody response to the epitope defined by the hepatitis C virus-neutralizing monoclonal antibody AP33. J. Gen. Virol. 88:2991-3001. [DOI] [PubMed] [Google Scholar]
- 56.Tarr, A. W., A. M. Owsianka, J. M. Timms, C. P. McClure, R. J. Brown, T. P. Hickling, T. Pietschmann, R. Bartenschlager, A. H. Patel, and J. K. Ball. 2006. Characterization of the hepatitis C virus E2 epitope defined by the broadly neutralizing monoclonal antibody AP33. Hepatology 43:592-601. [DOI] [PubMed] [Google Scholar]
- 57.Vieyres, G., A. G. Angus, A. Haberstroh, T. F. Baumert, J. Dubuisson, and A. H. Patel. 2009. Rapid synchronization of hepatitis C virus infection by magnetic adsorption. J. Virol. Methods 157:69-79. [DOI] [PubMed] [Google Scholar]
- 58.Voisset, C., N. Callens, E. Blanchard, A. Op De Beeck, J. Dubuisson, and N. Vu-Dac. 2005. High density lipoproteins facilitate hepatitis C virus entry through the scavenger receptor class B type I. J. Biol. Chem. 280:7793-7799. [DOI] [PubMed] [Google Scholar]
- 59.Voisset, C., A. Op de Beeck, P. Horellou, M. Dreux, T. Gustot, G. Duverlie, F. L. Cosset, N. Vu-Dac, and J. Dubuisson. 2006. High-density lipoproteins reduce the neutralizing effect of hepatitis C virus (HCV)-infected patient antibodies by promoting HCV entry. J. Gen. Virol. 87:2577-2581. [DOI] [PubMed] [Google Scholar]
- 60.von Hahn, T., B. D. Lindenbach, A. Boullier, O. Quehenberger, M. Paulson, C. M. Rice, and J. A. McKeating. 2006. Oxidized low-density lipoprotein inhibits hepatitis C virus cell entry in human hepatoma cells. Hepatology 43:932-942. [DOI] [PubMed] [Google Scholar]
- 61.Wakita, T., T. Pietschmann, T. Kato, T. Date, M. Miyamoto, Z. Zhao, K. Murthy, A. Habermann, H. G. Krausslich, M. Mizokami, R. Bartenschlager, and T. J. Liang. 2005. Production of infectious hepatitis C virus in tissue culture from a cloned viral genome. Nat. Med. 11:791-796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Witteveldt, J., M. J. Evans, J. Bitzegeio, G. Koutsoudakis, A. M. Owsianka, A. G. Angus, Z. Y. Keck, S. K. Foung, T. Pietschmann, C. M. Rice, and A. H. Patel. 2009. CD81 is dispensable for hepatitis C virus cell-to-cell transmission in hepatoma cells. J. Gen. Virol. 90:48-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Zeisel, M. B., G. Koutsoudakis, E. K. Schnober, A. Haberstroh, H. E. Blum, F. L. Cosset, T. Wakita, D. Jaeck, M. Doffoel, C. Royer, E. Soulier, E. Schvoerer, C. Schuster, F. Stoll-Keller, R. Bartenschlager, T. Pietschmann, H. Barth, and T. F. Baumert. 2007. Scavenger receptor class B type I is a key host factor for hepatitis C virus infection required for an entry step closely linked to CD81. Hepatology 46:1722-1731. [DOI] [PubMed] [Google Scholar]
- 64.Zhong, J., P. Gastaminza, G. Cheng, S. Kapadia, T. Kato, D. R. Burton, S. F. Wieland, S. L. Uprichard, T. Wakita, and F. V. Chisari. 2005. Robust hepatitis C virus infection in vitro. Proc. Natl. Acad. Sci. U. S. A. 102:9294-9299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Zhong, J., P. Gastaminza, J. Chung, Z. Stamataki, M. Isogawa, G. Cheng, J. A. McKeating, and F. V. Chisari. 2006. Persistent hepatitis C virus infection in vitro: coevolution of virus and host. J. Virol. 80:11082-11093. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.