Abstract
Purpose:
This study was performed to explore the cost-effectiveness of total hip replacement compared with hemiarthroplasty in the treatment of displaced femoral neck fractures in active otherwise healthy older patients in whom the optimum treatment is believed to be an arthroplasty procedure.
Methods:
A Markov decision model was used to determine whether total hip arthroplasty or hemiarthroplasty was most cost-effective for the management of a displaced femoral neck fracture in this patient population.
Results:
Total hip arthroplasty was associated with an average cost $3,000 more than hemiarthroplasty, and the average quality-adjusted life year gain was 1.53. The incremental cost-effectiveness ratio associated with the total hip replacement treatment strategy is $1960 per quality-adjusted life-year.
Conclusion:
Currently available data support the use of total hip arthroplasty as the more cost-effective treatment strategy in this specific population. The increased upfront cost appears to be offset by the improved functional results when compared with hemiarthroplasty in this select patient group.
Introduction
Treatment choice for displaced femoral neck fractures continues to be a challenge to the orthopaedic surgeon. 1 Surgeons and patients make treatment decisions based upon the individual patient's functional ability, risks and preferences. Treatment options are all associated with a unique set of potential benefits and risks. Arthroplasty procedures are most commonly selected in patients age 65 to 75, in an attempt to achieve more consistent results than are possible with internal fixation due to lower revision rates. 1 4 5 However, once the decision to perform an arthroplasty procedure is made, the most appropriate choice of implant, a hemiarthroplasty or total hip arthroplasty, remains unclear. Many patients in this age group remain active. The trade-offs behind this decision are that the added morbidity of total hip arthroplasty, including potential increased operative time, blood loss, infection rates, and peri-operative mortality, and the increased possibility of post-operative dislocation, may be compensated by increased functional results and long-term implant survival compared with hemiarthroplasty, which has demonstrated deterioration of function over time and acetabular erosion, which correlates with physical activity, for this subset of active patients. 4,6-10 11 12 13 Recent studies, have demonstrated a substantial number of surgeons using both total hip arthroplasty and hemiarthroplasty for patients with femoral neck fractures, highlighting the decisional conflict. 1 Studies of hospital resource consumption in the treatment of femoral neck fractures have shown that the primary operative technique is one of the most important factors in determining the total cost of treating these fractures. 14 A recent review of the Cochrane database reported there is insufficient evidence to determine whether hemiarthroplasty or total hip replacement is the preferred arthroplasty for the treatment of displaced femoral neck fractures. 15 This study was performed to explore the cost-effectiveness on the population level of total hip replacement compared with hemiarthroplasty for the treatment of displaced femoral neck fractures in a distinct subset of the hip fracture population, active, healthy, elderly patients.
Methods
Patient Population
To model the healthy, active, elderly patient population, we evaluated a theoretical cohort of patients aged 70 years old, who sustained a displaced femoral neck fracture. This age was chosen to represent a typical age for patients where both a hemiarthroplasty and a total hip replacement may be indicated. All patients were assumed to have fractures that would be ideally treated with an arthroplasty procedure, although in practice, the clinical criteria for this lies with individual surgeons and remains to be clearly defined.
Model Design
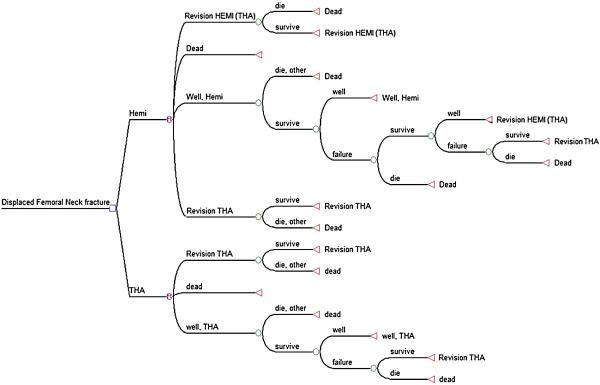
A Markov decision model16 was used to determine whether total hip arthroplasty (THA) or hemiarthroplasty (HEMI) was most cost-effective for the management of the population of patients with a displaced femoral neck fracture. The Markov model depicting the risks faced annually by patients undergoing either procedure is shown in figure 1. The health states in the model were: “well (post-procedure, THA or HEMI)”, “revision of HEMI to THA”, “revision THA,” and “death.” Each health state was assigned both a cost and a health utility, defined as the numeric representation of the value patients assign a particular health state. Utilities represent how health states are valued, not the specific characteristics of that health state. Utilities are measured between the extremes of perfect health, which is assigned a value of 1, and death, which is assigned a value of 0.17 Utilities are used to estimate quality-adjusted life years (QALYs), which measure effectiveness. In addition, a cost was assigned to every primary and revision procedure within the model. Patients transition between health states at an age-dependent frequency determined by specific transition probabilities. The methods used to obtain the transition probabilities associated with changing health states, including the probability of revision and the probability of death, are detailed below. As the theoretical patient cohort transitions between health states, he/she accumulates costs and utilities, which are used to estimate cost and effectiveness of each treatment over time. All costs and utilities incurred after time zero were discounted at a rate of 3% per year to be consistent with current practices of cost-effectiveness analysis in medicine.17 After completion of the model, the total tabulated costs and QALYs were used to evaluate the overall cost-effectiveness of the THA and HEMI strategies. The model was constructed using decision analysis software (TreeAge Pro 2007, Williamstown, MA).
Figure 1.
The figure represents the Markov model used to model patients with a displaced fracture of the femoral neck. Each patient receives a hemiarthroplasty (HEMI) or a total hip arthroplasty (THA) procedure. They stay well until they die from other causes or need a revision. If a patient has a revision and survives, they are assumed stay well with that revision until they die from other causes. The model continues until all patients reach the death health state.
Model Parameters
The following general assumptions were made in constructing the model: 1) the patient population was defined as individuals 70 years old, who have sustained a displaced femoral neck fracture; 2) all fractures were treated with an arthroplasty procedure, either a THA or a HEMI; 3) all revision surgery involved revision to a total hip construct; 4) patient mortality rates after they have recovered from their arthroplasty operation were not different than the age-adjusted mortality rate of a patient who has not had an arthroplasty procedure. The parameter values used in the decision model are shown in Table 1, and are individually described in further detail below.
TABLE 1.
Model parameters used for base case.
| Variable | Baseline Value |
|---|---|
| Utility | |
| Total Hip Arthroplasty | 0.69 |
| Hemiarthroplasty | 0.53 |
| Revision | 0.5 |
|
| |
| Disutility | |
| Total Hip Arthroplasty | −0.15 |
|
| |
| Hemiarthroplasty | −0.1 |
|
| |
| Revision | −0.2 |
|
| |
| Cost | |
| Total Hip Arthroplasty | $38,758 |
| Hemiarthroplasty | $34,249 |
| Revision | $51,000 |
Implant Survival Rates
Long-term data regarding the survivorship of hemiarthroplasty and total hip replacement for the treatment of displaced femoral neck fractures in the United States is lacking. Therefore, data from the Swedish Arthroplasty Register were used to estimate the probability of revision of a THA. 18These data were used to set the annual probability of revision of a total hip replacement for patients in the model equal to the annual probability of revision of a total hip replacements for any reason in the Swedish Arthroplasty Register for years 1 through 20. The revision rate for hemiarthroplasty was expressed relative to the revision rate of total hip arthroplasty, and was assumed to be equal for the base case. A variety of differing revision rates have been reported for the treatment of displaced femoral neck fractures with hemiarthroplasty or total hip arthroplasty from case series and trials in the literature; 10 9 7,19 Therefore, for the base case the revision rate was assumed to be equal for femoral neck fractures treated with hemiarthroplasty or total hip arthroplasty.
Mortality Rates
Numerous studies have demonstrated an increased short-term mortality rate for patients with hip factures. 9,20 21 Studies have also shown similar mortality rates for hemiarthroplasty and total hip replacement in this population, 10 9 7 22 4 whereas other authors have suggested the increased magnitude of surgery due to the need to resurfacing of both the femoral head and acetabulum leads to increased blood loss with total hip replacement, which could impact mortality. 2 For the base case, we set mortality during the first for hemiarthroplasty and total hip replacement equal to each other. A recent analysis of mortality after hip fracture in over 25,000 Medicare beneficiaries, adjusted for age, sex, race, pre-fracture functional status, functional impairments and comorbid conditions, found the mortality to be 6.3 times greater during the first six months, with no increase at further follow-up. 23 A study of 836 fractures found that the increased mortality may persist for at least two years. The 2-year mortality in a recent randomized trial was 15 to 16% for patients treated with an arthroplasty procedure. 9 Therefore, we set the mortality rate during the first two years in the model equal to 6.3 times the age-specific rate of death for the patient's age according to the 2001 U.S. Life Tables. 24 The probability of peri-operative death of revision total hip was estimated from a Medicare study of 61,568 primary THAs and 13,483 revision THAs, which found 90-day mortality rates of 2.6% respectively. 25 This assumes that the majority of revisions will take place more than 2 years after the index procedure and that patients have returned to their normal mortality risk level for surgery. Studies have shown that once recovery from thes einjuries has occurred, healthy patients sustaining femoral neck fractures, classified as American Society of Anesthesiolgists classification group I or II, have minimal increased mortality risk. 21 Therefore, the age-specific probability of death from causes unrelated to arthroplasty after the initial two year period where mortality rates may be much higher was made equal to the probability of death at each specific age, and was taken from the 2001 US Life Tables. 24
Costs
Cost data were obtained from the 2003 National Inpatient Survey and were estimated from the average charges for treating femoral neck fractures with total hip replacement or hemiarthroplasty. The database contained information on 1575 patients with femoral neck fractures treated with total hip replacement and 18,233 patients with femoral neck fractures treated with hemiarthroplasty and found the average hospital charges were $38,758 and $34, 249, respectively. The cost of a revision was estimated from the average hospital charges for 8,153 patients having a partial hip revision at $51,000.
Utility Values
As noted earlier (REF MODELING SECTION HERE), QALYs were used to measure treatment effectiveness based on health utlities values assigned to model health states and disutility values assigned to treatment procedures. Utilities used in the model were set equal to the utility scores for patients receiving hemiarthroplasty and total hip arthroplasty in a recently published randomized controlled trial of the treatment of femoral neck fractures, and are meant to represent the average utility achieved by a population of patients having femoral neck fractures treated with either total hip replacement or hemiarthroplasty. 9 The utility value after total hip arthroplasty was set at 0.69, which is the average utility value of patients with femoral neck fractures treated with this arthroplasty one year after their operation. The utility value after hemiarthroplasty was set at 75% of this value for the base analysis, giving a base case value of 0.53, which is equivalent to the average utility value of patients with femoral neck fractures treated with this arthroplasty one year after their operation in Keating's randomized trial. 9 Studies have shown that the results of revision arthroplasty, including hip revision, are poorer than after a primary procedure. Therefore, the utility value after a revision was assigned an initial value of 0.5.
Disutilities represent the negative preference patients have for a particular health state or outcome, such as an arthroplasty procedure. 16 These negative utility values, or disutilities, account for the decreased mobility, increased pain, and potential complications, which are incurred during the recovery period after surgery. The disutility of having a THA, HEMI, and a revision arthroplasty were included in the model as a decrement in QALYs assigned to patient's total QALY count, at the time a patient undergoes any procedure within the model, as a one time acute procedure toll to account for the morbidity of these procedures. The disutility of having a THA, HEMI and revision were set at −0.15, −0.1 and −0.2 respectively.
Analysis
Cost effectiveness is typically expressed as the incremental cost-effectiveness ratio (ICER), which is the ratio of the difference in cost divided by the difference in effectiveness, in this model expressed in QALYs, between two different treatment strategies when they are ranked in order of increasing cost.17 The ICER reflects the cost of purchasing each additional QALY when selecting one treatment strategy over the other. The difference of the total accumulated costs of the THA and HEMI strategies, including the cost of future revision procedures, was divided by the difference in the total accumulated QALYs obtained in each arm by patients over a twenty year period, to determine the ICER.16
ICER = (Total CostTHA strategy − Total CostHEMI strategy) / (Total QALYsTHA strategy − Total QALYsHEMI strategy).
We considered cost profiles with ICERs of less than $50,000 per QALY to be reasonably cost-effective.17 Both future costs and future utilities, or QALYs, were discounted at 3% to be consistent with current practices in cost-effectiveness analysis. 17
Sensitivity analysis is a test of the stability of conclusions conducted by varying a variable, or variables, over a stated range and evaluating the effect of this variation on the outcome, in this study the ICER, of the model. 16 Two-way sensitivity analysis was used to examine the effect of varying two parameters on the cost-effectiveness of the treatment of femoral neck fractures.
Results
The results for the base case are shown in Table 2. Using the parameters discussed in the methods section and shown in Table 2, total hip arthroplasty (THA) was associated with an average cost $3,000 higher than hemiarthroplasty (HEMI), and the average utility gain was 1.53 quality-adjusted life-years over the 20 year period of the Markov model. This resulted in an incremental cost-effectiveness ratio of $1,960 for the THA treatment strategy, which is well below the $50,000 threshold used for determining the cost-effectiveness of treatment interventions.
Table 2.
The results of the analysis for the base case are shown below. Results are the average lifetime cost and quality-adjusted life-years gained per patient.
| Strategy | Average Cost |
Average QALYs# |
Average ΔCost |
Average ΔQALY |
ICER+ |
|---|---|---|---|---|---|
| HEMI* | $38,100 | 4.44 | - | - | - |
| THA** | $41,100 | 5.97 | −$3,000 | 1.53 | $1,960 |
HEMI(Hemiarthroplasty);
THA (total hip arthroplasty) ;
QALY (quality-adjusted life-year);
ICER (Incremental Cost-effectiveness Ratio)
The results of sensitivity analyses are shown in Figures 2 through 5. Figure 2 illustrates the effect of varying the utility value of THA and HEMI. Each procedure was more likely to be favored as the utility value associated with the procedure increases. However, at higher utility values, if the utility of these two procedures were equal, THA was more cost-effective. For example, if both procedures were associated with a utility value of 0.5, THA would be more cost-effective. The utility value of HEMI must be greater than THA in order for HEMI to be the more cost-effective procedure.
Figure 2.
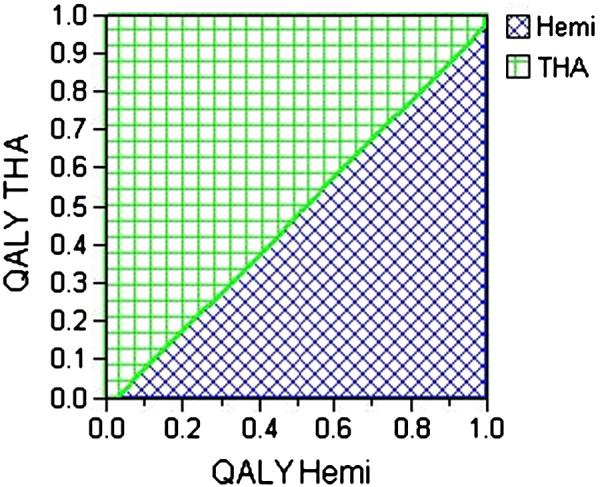
The figure demonstrates the results of sensitivity analysis comparing the effect varying the utility values, expressed in quality-adjusted life-years (QALYs), of total hip arthroplasty (THA) and hemiarthroplasty (HEMI). Areas indicated in green demonstrate the profiles where THA is cost-effective. For example, if the utility of HEMI is 0.5, THA will be cost-effective if the utility is greater than 0.45.
Figure 5.
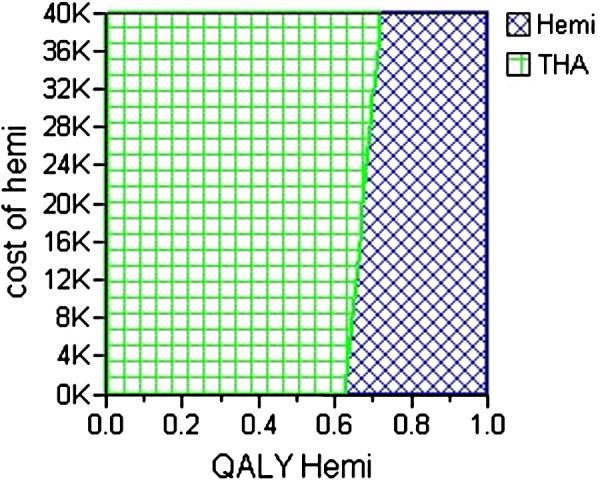
The figure demonstrates the results of sensitivity analysis comparing the effect varying the cost of hemiarthroplasty (HEMI) and the utility value of HEMI, measured in quality-adjusted life-years (QALYs) compared with total hip arthroplasty (THA). Areas indicated in green demonstrate the profiles where THA is cost-effective. For example, if the utility of HEMI is 0.7, THA will be cost-effective if the cost of HEMI is less than $18,000.
Figure 3 illustrates the effect of varying the cost of THA and HEMI. It demonstrates that the lifetime cost associated with treating a patient with THA must be greater than $78,000, while the lifetime cost associated with using a hemiarthroplasty must be less than $22,000 for HEMI to be the more cost-effective treatment option.
Figure 3.
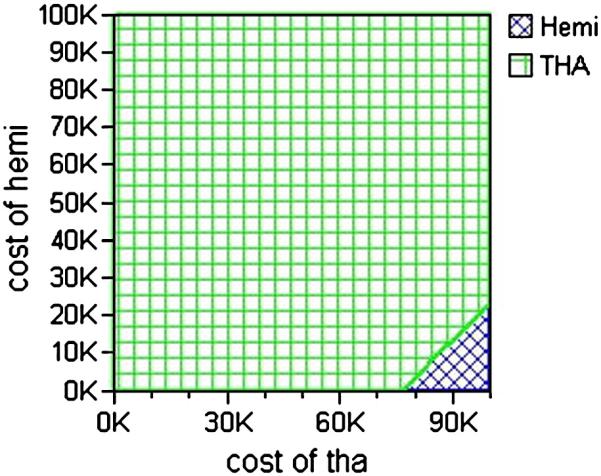
The figure demonstrates the results of sensitivity analysis comparing the effect varying the cost of total hip arthroplasty (THA) and hemiarthroplasty (HEMI). Areas indicated in green demonstrate the profiles where THA is cost-effective. For example, if the cost of THA is $80,000, THA will be cost-effective unless the cost of HEMI is less than $12,000.
Figure 4 illustrates the effect of varying the utility value of HEMI along with the relative revision rate of HEMI compared with THA. It demonstrates that the utility value of HEMI must be 0.68, even if there are no revisions of hemiarthroplasties, for HEMI to be the more cost-effective strategy. If utility value associated with hemiarthroplasty was less than 0.68, THA would be more cost-effective in all instances. If the utility value of HEMI reaches 1.0, reflecting perfect health, the revision rate must be seven times the rate of THA, before THA would be more cost-effective.
Figure 4.
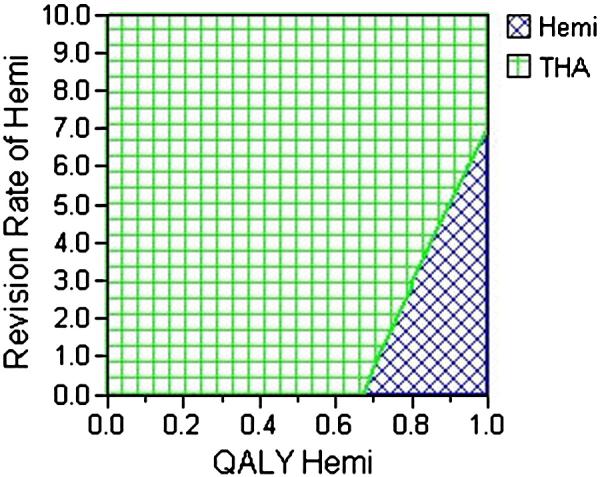
The figure demonstrates the results of sensitivity analysis comparing the effect varying the utility values, expressed in quality-adjusted life-years (QALYs), of hemiarthroplasty (HEMI) and the relative revision rate of HEMI compared with total hip arthroplasty (THA). Areas indicated in green demonstrate the profiles where THA is cost-effective. THA is the more cost-effective option, unless the utility of HEMI is at least 0.7 and the revision rate is between 0 and 7 times the revision rate of THA.
Figure 5 illustrates the effect of varying the cost of hemiarthroplasty and the average utility value of hemiarthroplasty. It demonstrates that at current cost estimates for hemiarthroplasty the utility value associated with that procedure must be greater than 0.7 before hemiarthroplasty becomes the more cost-effective treatment option. It also illustrates that as the cost increases, the utility value required to make hemiarthroplasty the more cost-effective treatment also increases.
Discussion
This study focuses on a narrow subset of patients who have sustained a displaced femoral neck fracture, the active, healthy elderly patient. The results of this analysis demonstrate several important points. First, it appears that total hip replacement is the more cost-effective arthroplasty option for displaced femoral neck fractures in the active, healthy, elderly patient population, despite the potential for increased morbidity compared with hemiarthroplasty. The incremental cost-effectiveness ratio is $1,960 per QALY, which is well below the $50,000 per QALY threshold needed to make an intervention cost-effective. 17 The cost-effectiveness of total hip replacement in this patient population is due to the increased quality of life for patients with well-functioning total hip replacements compared with hemiarthroplasty patients, reflected in the higher average utility values achieved with this procedure. 9
Second, the procedure which generates the highest average utility for patients is likely to be the most cost-effective option, and this utility value is the most important parameter in determining cost-effectiveness. This is demonstrated in several ways. For example, if the revision rate of hemiarthroplasty is greater than the rate for total hip replacement, then the average utility value associated with hemiarthroplasty must be greater than the average value achieved with THA for it to be the more cost-effective strategy (Figure 2). However, this is not consistent with the utility values achieved with hemiarthroplasty in recent studies. 9 In addition, Figure 3 demonstrates that cost does not appear to be as important as the average utility value achieved with each procedure, as the cost differences between the two procedures must reach unlikely extremes before hemiarthroplasty becomes the more cost-effective option when using the average utility values currently reported in the literature for these two procedures in this patient population. Furthermore, many patients will not undergo a revision during their remaining lifetime, which makes the average utility value achieved with the index arthroplasty procedure, a more important variable then the revision rate. This is illustrated in Figure 4, which shows the revision rate of hemiarthroplasty must increase to seven times the rate for total hip replacement before total hip becomes the more cost-effective treatment if the utility value of HEMI increases from 0.68 to 1.0. The importance of the utility value of the index procedure is also demonstrated by the fact that even if the revision rate of hemiarthroplasty is 0%, it still is only the more cost-effective option if the average utility value associated with it is 0.68 or greater, which is greater than the average value achieved in patients with displaced femoral neck fractures treated with total hip replacement in recent trials (Figure 4). 9 Therefore, if total hip replacement results in a higher average utility value than hemiarthroplasty in the treatment of displaced femoral neck fractures, as recent studies have found 9, it very likely will be the more cost-effective treatment option for this injury. This is important for future investigators to understand and highlights the need for studies precisely evaluating the utility value of these arthroplasty procedures for large numbers of patients with femoral neck fractures over time.
This analysis examined the patient population of active, healthy, elderly patients with displaced femoral neck fracture thought to be best treated with an arthroplasty procedure. The patient population that fits this description remains to be clearly defined.1 It should be noted that this is a population based analysis and not an analysis of individual patient preferences or characteristics. Therefore, surgeons will need to continue to practice the art of medicine, weighing each individual patient's medical and social situation, personal risk preferences, as well as their own surgical resources and capabilities, in deciding the best treatment option for elderly patients who sustain a displaced femoral neck fracture. The factors involved in the long-term outcome of femoral neck fractures treated with an arthroplasty procedure are difficult to weigh against each other. A limitation of the model used in this study is the estimation of the transition probabilities, such as the rate of revision surgery or peri-operative mortality, as well as the utilities and disutilities used within the model. The only definitive way to truly determine the cost-effectiveness of the two treatment strategies would be to prospectively measure the health utility and costs associated with each treatment and all its sequelae for a large patient population over an extended period of time.
Currently available data support the use of total hip arthroplasty as the more cost-effective treatment strategy in active, healthy, elderly patients with displaced femoral neck fractures. The increased upfront cost appears to be offset by the improved functional results measured by higher average post-operative utility values, when compared with hemiarthroplasty in this select patient group, resulting in an incremental cost-effectiveness ratio well below accepted thresholds for determining cost-effective treatment strategies.
Acknowledgments
This research was supported in part with funding from the National Institute of Arthritis and Musculoskeletal and Skin Diseases (P60 AR48094).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Bhandari M, et al. Operative management of displaced femoral neck fractures in elderly patients. An international survey. J Bone Joint Surg Am. 2005;87(9):2122–30. doi: 10.2106/JBJS.E.00535. [DOI] [PubMed] [Google Scholar]
- 2.Bucholz R, Heckman J, Court-Brown C. Rockwood and Green's: Fractures in Adults. 2006:1753–91. [Google Scholar]
- 3.Callaghan J, Rosenberg A, Rubash H. Hip Fractures Treated by Arhtroplasty. The Adult Hip. 2007:1187–1210. [Google Scholar]
- 4.Bhandari M, et al. Internal fixation compared with arthroplasty for displaced fractures of the femoral neck. A meta-analysis. J Bone Joint Surg Am. 2003;85-A(9):1673–81. doi: 10.2106/00004623-200309000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Hudson JI, Kenzora JE, Hebel JR, Gardner JF, Scherlis L, Epstein RS, Magaziner JS. Eight-year outcome associated with clinical options in the management of femoral neck fractures. Clin Orthop Relat Res. 1998;(348):59–66. [PubMed] [Google Scholar]
- 6.Ravikumar KJ, Marsh G. Internal fixation versus hemiarthroplasty versus total hip arthroplasty for displaced subcapital fractures of femur--13 year results of a prospective randomised study. Injury. 2000;31(10):793–7. doi: 10.1016/s0020-1383(00)00125-x. [DOI] [PubMed] [Google Scholar]
- 7.Baker RP, Squires B, Gargan MF, Bannister GC. Total hip arthroplasty and hemiarthroplasty in mobile, independent patients with a displaced intracapsular fracture of the femoral neck. A randomized, controlled trial. J Bone Joint Surg Am. 2006;88(12):2583–9. doi: 10.2106/JBJS.E.01373. [DOI] [PubMed] [Google Scholar]
- 8.Dorr LD, Glousman R, Hoy AL, Vanis R, Chandler R. Treatment of femoral neck fractures with total hip replacement versus cemented and noncemented hemiarthroplasty. J Arthroplasty. 1986;1(1):21–8. doi: 10.1016/s0883-5403(86)80006-7. [DOI] [PubMed] [Google Scholar]
- 9.Keating JF, Grant A, Masson M, Scott NW, Forbes JF. Randomized comparison of reduction and fixation, bipolar hemiarthroplasty, and total hip arthroplasty. Treatment of displaced intracapsular hip fractures in healthy older patients. J Bone Joint Surg Am. 2006;88(2):249–60. doi: 10.2106/JBJS.E.00215. [DOI] [PubMed] [Google Scholar]
- 10.Iorio R, Healy WL, Lemos DW, Appleby D, Lucchesi CA, Saleh KJ. Displaced femoral neck fractures in the elderly: outcomes and cost effectiveness. Clin Orthop Relat Res. 2001;(383):229–42. doi: 10.1097/00003086-200102000-00027. [DOI] [PubMed] [Google Scholar]
- 11.Kofoed H, Kofod J. Moore prosthesis in the treatment of fresh femoral neck fractures. A critical review with special attention to secondary acetabular degeneration. Injury. 1983;14(6):531–40. doi: 10.1016/0020-1383(83)90057-8. [DOI] [PubMed] [Google Scholar]
- 12.Phillips TW. The Bateman bipolar femoral head replacement. A fluoroscopic study of movement over a four-year period. J Bone Joint Surg Br. 1987;69(5):761–4. doi: 10.1302/0301-620X.69B5.3680337. [DOI] [PubMed] [Google Scholar]
- 13.Clayer M, Bruckner J. The outcome of Austin-Moore hemiarthroplasty for fracture of the femoral neck. Am J Orthop. 1997;26(10):681–4. [PubMed] [Google Scholar]
- 14.Holmberg S, Thorngren KG. Consumption of hospital resources for femoral neck fracture. Acta Orthop Scand. 1988;59(4):377–81. doi: 10.3109/17453678809149385. [DOI] [PubMed] [Google Scholar]
- 15.Parker MJ, Gurusamy K. Arthroplasties (with and without bone cement) for proximal femoral fractures in adults. Cochrane Database Syst Rev. 2004;(2):CD001706. doi: 10.1002/14651858.CD001706.pub2. [DOI] [PubMed] [Google Scholar]
- 16.Hunink M. Decision Making in Health and Medicine. Cambridge University Press; 2003. e. a. [Google Scholar]
- 17.Gold M. Cost-Effectiveness in Health and Medicine. Oxford University Press; 1998. e. a. [Google Scholar]
- 18.The Swedish Hip Arthroplasty Register Annual Report. 2006 www.jru.orthop.gu.se.
- 19.Gebhard JS, Amstutz HC, Zinar DM, Dorey FJ. A comparison of total hip arthroplasty and hemiarthroplasty for treatment of acute fracture of the femoral neck. Clin Orthop Relat Res. 1992;(282):123–31. [PubMed] [Google Scholar]
- 20.Magaziner J, Simonsick EM, Kashner TM, Hebel JR, Kenzora JE. Survival experience of aged hip fracture patients. Am J Public Health. 1989;79(3):274–8. doi: 10.2105/ajph.79.3.274. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Richmond J, Aharonoff GB, Zuckerman JD, Koval KJ. Mortality risk after hip fracture. J Orthop Trauma. 2003;17(8 Suppl):S2–5. doi: 10.1097/00005131-200309001-00002. 2003. [DOI] [PubMed] [Google Scholar]
- 22.Parker MJ, Khan RJ, Crawford J, Pryor GA. Hemiarthroplasty versus internal fixation for displaced intracapsular hip fractures in the elderly. A randomised trial of 455 patients. J Bone Joint Surg Br. 2002;84(8):1150–5. doi: 10.1302/0301-620x.84b8.13522. [DOI] [PubMed] [Google Scholar]
- 23.Tosteson A, Gottlieb D, Radley D, Fisher E, Melton L. Excess Mortality Following Hip fracture: Role of Underlying Health Status. Osteoporosis International. 2007;18(11):1463–72. doi: 10.1007/s00198-007-0429-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Arias E. National Vital Statistics Reports, Vol. 52, No 14. U.S. Department of Health and Human Services; Center for Disease Control and Prevention; 2004. United States Life Tables, 2001. [PubMed] [Google Scholar]
- 25.Mahomed NN, et al. Rates and outcomes of primary and revision total hip replacement in the United States medicare population. J Bone Joint Surg Am. 2003;85-A(1):27–32. doi: 10.2106/00004623-200301000-00005. [DOI] [PubMed] [Google Scholar]
- 26.Robinson CM, Saran D, Annan IH. Intracapsular hip fractures. Results of management adopting a treatment protocol. Clin Orthop Relat Res. 1994;(302):83–91. [PubMed] [Google Scholar]