Abstract
Background and purpose
Reversed shoulder arthroplasty may be used for severe arthropathy where conventional prostheses cannot restore the function sufficiently. We analyzed the medium–term results and potential complications of the reversed prostheses, and also the influence of etiology on the result.
Methods
52 women and 7 men, average age 70 (60–82) years, were followed for mean 4 (2–7) years. The indications were cuff tear arthropathy (CTA) (23), fracture sequelae (20), and revision of a failed conventional arthroplasty (16).
Results
The average Constant score improved from 18 (2–55) points to 59 (17–96) points. It rose from 26 to 74 points in patients with CTA, from 12 to 48 in those with fracture sequelae, and from 10 to 54 points in revision arthroplasty. We also found an overall improvement in active forward flexion from 47° to 105°, and in active abduction from 46° to 93°. Scapular notching was seen in 51 shoulders. Radiolucent lines below the base–plate were present in 2 cases. There were no instances of loosening. Revisions were necessary in 15 patients: 5 with infections (all had had prior surgery), 5 with hematoma, 3 with dislocations, and 2 with disconnections of the shaft components.
Interpretation
Reversed prosthetic replacement is a suitable method for restoring function and attaining pain relief in severe arthropathies. The results in revision arthroplasty are less predictable, with complications and revision rates higher than those in CTA patients. The reversed prosthesis should therefore only be used when conventional methods have failed.
Introduction
A painful malfunctioning shoulder due to joint incongruence in combination with a loss of the centering action of the rotator muscles may be caused by severe rotator cuff arthritis, malunited/pseudarthrotic fractures, or loss of the tubercles in prosthesis revision. Contraction of the deltoid muscle when raising the arm induces a cranial migration of the head. An anatomically unconstrained prosthesis does not restore a stable center of rotation and is likely to fail (Nwakama et al. 2000, Edwards et al. 2002).
A reversed prosthesis is a way out of this dilemma, since it allows reconstruction of a stable center of rotation besides replacement of the articular surfaces (Grammont and Baulot 1993, Boileau et al. 2001, Sirveaux et al. 2004, Jouve et al. 2006, Molé et al. 2006, Wall et al. 2006, Bufquin et al. 2007, Irlenbusch et al. 2008c). Despite severe damage and loss of balance in the rotator cuff, free elevation can be attained through the sole action of the external shoulder muscles.
We compared the results and the complication rates after implantation of a reversed prosthesis in the 3 diagnosis groups. Preoperatively, the groups showed substantial differences in terms of loss of function and degree of destruction.
Patients and methods
We treated 68 consecutive shoulders with a reversed Delta III prosthesis (DePuy) during the period 2002 – 2007. 59 patients (52 women) with an average age of 70 (60–82) years participated in this study and they were followed prospectively for mean 4 (2–7) years. The indications were cuff tear arthropathy (CTA) in 23 patients, fracture sequelae in 20 patients, and revision of a conventional prosthesis in 16 patients.
9 patients did not show up for follow–up because of living too far away (3) or because they were satisfied with the result and did not see any reason for a repeat examination (2). 1 patient was dissatisfied and had undergone further surgery, and 3 could not be reached.
Clinical criteria
The clinical outcome was evaluated using the Constant score, by investigators not involved in the surgery. Strength was measured with a tensiometer at the wrist joint in maximal abduction in the scapular plane. Preoperative and postoperative mobility and pain relief were registered.
Radiographic criteria
CTA was classified according to Hamada et al. (1990). None of the 23 patients in the CTA group were assigned to group I, 2 patients were in group II, (incipient decentering, acromiohumeral distance/AHD ≤ 5 mm), 6 patients were in group III (decrease of the AHD and acetabularization), 11 patients were in group IV (additional narrowing of the articular space/osteoarthritis), and 4 patients were in group V (manifest cuff tear arthropathy with collapse of the head of the humerus) (Figure 1).
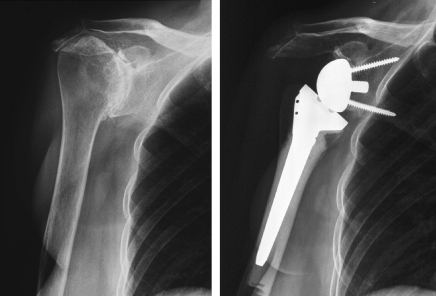
Figure 1.
Delta III prosthesis in CTA type V according to Hamada.
20 patients had fracture sequelae (Figure 2), which were classified in 4 types according to Boileau and Walch (Boileau et al. 2006). 2 patients were type I, 2 type II, 3 type III, and 13 patients were type IV.
Figure 2.
Delta III prosthesis in fracture sequelae type IV according to Boileau and Walch, with persistent dislocation and healing of the fragments with massive deformation.
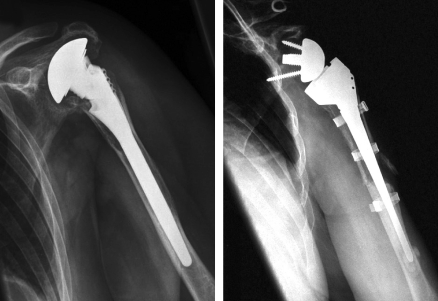
Prosthesis revision was done in 16 patients (Figure 3). This was due to migration of the prosthesis due to necrosis of the tubercles in 9 cases, and secondary rotator cuff rupture in 1 case. A 2–stage prosthesis revision was necessary in 6 patients because of septic loosening. No aseptic shaft loosening, glenoid loosening, or glenoid erosions occurred in this group.
Figure 3.
Delta III prostheses after failed fracture of prosthesis due to necrosis of the tubercles, and resulting anterior–superior migration.
The extent of scapular notching was classified according to Sirveaux et al. (2004) using exact orthograde scans. In addition, the radiolucent lines on the glenoid were recorded according to Gonzales et al. (2006).
Rotator cuff condition and rupture size were recorded during surgery (Bateman 1963, Patte 1990).
Statistics
Constant score values are given as mean and median values, as well as 25% and 75% percentiles.
Abduction, flexion, and strength parameters were tested non–parametrically with regard to the diagnoses using the Wilcoxon test. The p–values of each comparison were adjusted using the Bonferroni method.
Multiple regression models were calculated to compare the diagnostic significance of the Constant score with respect to diagnosis (analysis of variance with consideration of age and gender). Separate models for the follow–up examinations (pooled for months 3–36 and more) were estimated. The pooled models also included the months as covariant. The distribution of the residues was checked for normal distribution using Q–Q plots or scatter plots.
Results
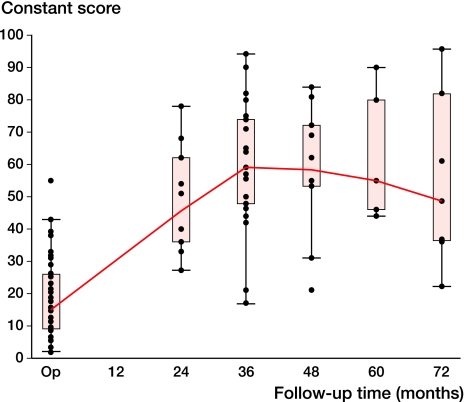
The average Constant score improved from 18 to 59 points in the overall patient population after 36 months (Figure 4), but dropped to 55 after more than 72 months.
Figure 4.
Development of the Constant score adjusted for age and gender over the period of investigation (median values, interquartile range 25% and 75%, min., max., l = outlier that lie between 1.5 and 3 times the interquartile range).
At average follow–up, the Constant score rose from 15 (2–55) to 55 (17–96) in the overall patient population (a difference of 40), from 26 (2–55) to 74 (44–96) in CTA (a difference of 48), from 12 (2–38) to 48 (17–90) in fracture sequelae (a difference of 36), and from 10 (2–26) to 54 (21–75) points in the revision operations (a difference of 44). The global postoperative gain and the gain per diagnosis group were statistically significant (p < 0.001).
The improvement comprised all components of the Constant score, but in particular pain relief and improvement in strength (Table 1). The most pronounced relief of pain and improvement in strength were attained in the CTA group. Force could not be measured in the fracture sequelae group and the revision group preoperatively because of low abduction angles.
Table 1.
Relief of pain and improvement in strength depending on the underlying diagnosis (mean values)
| Strength | Pain | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| max. 25 points | max. 15 points | |||||||||
| Preop. | SD | Postop. | SD | p–value | Preop. | SD | Postop. | SD | p–value | |
| Cuff tear arthropathy (n = 23) | 2 | 4 | 12 | 6.9 | < 0.001 | 3 | 4 | 14 | 2 | < 0.001 |
| Fracture sequelae (n = 20) | 1 | 1 | 7 | 5.7 | < 0.001 | 3 | 5 | 12 | 3 | < 0.001 |
| Revision arthroplasty (n = 16) | 1 | 1 | 8 | 5.1 | < 0.001 | 1 | 2 | 12 | 4 | < 0.001 |
| Total (n = 59) | 1 | 3 | 9 | 5.9 | < 0.001 | 2 | 4 | 13 | 3 | < 0.001 |
Preop.: at baseline; Postop.: at last follow–up; CTA: cuff tear arthropathy.
These results are also reflected in the improvement in active forward flexion in the overall patient population from 47° (0–100) to 105° (30–180) (Table 2) and in active abduction from 46° (10–90) to 93° (45–180). On the other hand, external rotation with the upper arm held close to the body only increased from 9° (minus 20–5) to 19° (minus 20–80). External rotation with the arm abducted increased from –3° (–20 to 20) to 35° (0–90). It is especially striking that the improvement in external rotation in the CTA group was markedly higher (with a difference of 61) than in the fracture sequelae group (with a difference of 23) and the revision group (with a difference of 23). Preoperative and postoperative changes were statistically significant in all groups whereas differences between the groups were not (p = 0.4).
Table 2.
Improvement in active range of motion (ROM) depending on the diagnosis. Values are mean degrees
| Total | Cuff tear arthropathy | Fracture sequelae | Revision arthroplasty | |
|---|---|---|---|---|
| (n = 59) | (n = 23) | (n = 20) | (n = 16) | |
| Abduction | ||||
| Preop. | 46 | 53 | 30 | 43 |
| Postop. | 93 | 115 | 79 | 78 |
| p–value | < 0.001 | 0.002 | < 0.001 | 0.006 |
| Forward flexion | ||||
| Preop. | 47 | 52 | 17 | 53 |
| Postop. | 105 | 134 | 89 | 84 |
| p–value | < 0.001 | < 0.001 | < 0.001 | 0.007 |
| External rotation in 0° abduction | ||||
| Preop. | –9 | 5 | –5 | 0 |
| Postop. | 19 | 28 | 11 | 12 |
| p–value | < 0.001 | < 0.001 | 0.01 | 0.02 |
| External rotation in 90° abduction | ||||
| Preop. | –3 | 2 | –4 | –9 |
| Postop. | 35 | 63 | 19 | 1 |
| p–value | < 0.001 | < 0.001 | 0.02 | 0.003 |
Preop: at baseline; Postop: at last FU.
We observed scapular notching in 51 of 59 shoulders: Sirveaux grade 0 in 8 cases, grade 1 in 27 cases, grade 2 in 21 cases, grade 3 in 2 cases, and grade 4 in 1 case. There were no statistically significant differences between the groups. No effect on the Constant score could be seen.
Radiographically detectable limited lysis was observed once in zone 1 (upper base–plate of the glenoid component) and once in zone 2 (lower base–plate). Manifest loosening was not observed. No resorption zones were detected around the peg and the screws in the glenoid and in the humerus shaft. Heterotopic ossifications occurred in the region of the lower joint capsule in 14 cases. However, a bony spur was present on the medial margin of the scapular notch in 38 patients (≤ 2 mm in 17, ≤ 4 mm in 11, ≤ 6 mm in 5, and ≥ 6 mm in 5). Consequently, the notching appeared deeper than it actually was.
We noted 3 cases of dislocation (in 1 instance because of trauma/fall), 1 case of acromion fracture, 1 case of fracture of the coracoid process, and 2 disconnections of the shaft components associated with massive scapular notching. Hematomas led to revisions in 5 cases. Infections were observed in 5 joints. All infections occurred after prior surgery, i.e. 3 after osteosynthesis and 2 after prosthesis revision because of deep infection. This means that 2 of the 6 patients who were admitted to the hospital with a pre–existing prosthesis infection had a reinfection. Overall revisions were necessary in 15 patients. Transient neurological deficits were observed in 2 patients.
Discussion
Implantation of a reversed prosthesis restores a stable center of rotation and thus provides the prerequisites for restoration of function. Considering the often catastrophic initial situation, the outcome was surprisingly good. It is not so much the plain postoperative functional score that is important but rather the gain in function, as a measure for comparison of the preoperative and postoperative state (the “Delta constant”). In the individual patient, a low postoperative value in absolute terms may nevertheless signify a major improvement compared to the preoperative situation.
The Constant score obtained in our study was lower than or similar to that in the literature (Table 3). However, the initial preoperative values were also lower in all 3 groups. In view of the low initial values, it is on a level similar to that for data reported in the literature. The greatest improvement in Constant score was achieved in CTA group, followed by revision arthroplasty and fracture sequelae. This is to some extent contrary to the results published in the literature. In most papers, the fracture sequelae attained a higher level than revisions (Boileau et al. 2006a, Jouve et al. 2006, Wall et al. 2007). We attribute the somewhat smaller functional gain in the CTA group in our study to the strict selection criteria used, i.e. the fact that we only included patients with advanced CTA. By contrast, in the literature reversed prostheses are also recommended for complete rotator cuff ruptures in the absence of obvious degenerative joint lesions (Gonzales et al. 2006, Molé et al. 2006). We prefer to perform a muscle transfer operation (latissimus dorsi or pectoralis major) in cases of irreparable rotator cuff defect without joint deterioration—even in the case of a failed cuff repair—as opposed to a reversed prosthesis (Irlenbusch et al. 2003, 2008a, b, Gerber et al. 2006). For this reason, our CTA group comprised exclusively patients with advanced cuff tear arthritis, especially of Hamada grade 4 and 5 (Hamada et al. 1990).
Table 3.
Published results on reversed shoulder replacement
| A | B | C | D | E | F | G | H | I | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Sirveaux 2004 | CTA | 80 | 44 | 73 | 138 | 4 c | 11 c | 23 P | 66 P | – | – | 2.7 b | 13.4 b |
| 17 d | 40 d | ||||||||||||
| Frankle 2005 | CTA | 60 | 36 | 55 | 105 | 12 | 41 | – | – | 34 | 68 | 6.3 a | 2.2 a |
| Seebauer 2005 | CTA | 57 | 18 | – | – | – | – | 26–43% | 85–97% | – | – | – | 12.8 b |
| Boileau 2006 | Diff. | 45 | 40 | 55 | 121 | 7 | 11 | 17 P | 58 P | – | – | – | 3.2 a |
| Favard 2006 | CTA | 127 | 49 | 70 | 135 | 8 c | 23 P | 65 P | – | – | 3 b | 13 b | 46 d |
| Gohlke 2006 | Revision fracture prostheses | 20 | 18 | – | – | – | – | 18% | 63% | – | – | 88% | good or excellent |
| Gonzales 2006 | CTA, revision | 42 | 50 | 82 | 123 | 5 | 7 | 25 P | 56 P | – | – | 3.3 b | 11.1 b |
| Jouve 2006 | Diff. | 65 | 46 | 49 | 116 | 2 c | 2.5 c | 17 P | 49 P | – | – | 3.2 b | 10.5 b |
| 12 d | 27 d | ||||||||||||
| Klein 2006 | Diff. | 46 | 13 | – | – | – | – | – | 86% | – | – | – | – |
| Molé 2006 | RC rupture | 47 | 30 | 80 | 133 | 10 | 13 | 40% | 90% | – | – | 4 b | 12.7 b |
| Paladini 2005 | Revision head prostheses | 7 | 36 | – | – | – | – | 23 P | 49 P | – | – | – | – |
| Wall 2006 | Revision total arthroplasty | 24 | 38 | 61 | 114 | 18 c | 11 c | ||||||
| 51 d | 46 d | 33% | 71% | – | – | 5.3 b | 11.1 b | ||||||
| Werner/Gerber 2006 | CTA | 58 | 38 | 42 | 100 | 17 c | 12 c | 29% | 64% | – | – | 5.2 b | 10.5 b |
| Irlenbusch 2009 | Diff. | 59 | 46 | 47 | 105 | –3 d | 35 d | 15 P | 55 P | – | – | 2.6 b | 12.9 b |
a max. 10 points/VAS.
b max. 15 points.
c 0° abduction.
d 90° abduction.
A Authors
B Diagnosis
CTA: cuff tear arthropathy;
RC rupture: rotator cuff rupture;
Diff.: different diagnosis groups;
C n
D Follow–up (months)
E Forward flexion (°), pre/post
F External rotation (°), pre/post
G Constant score, pre/post
P: points in Constant score;
%: corrected Constant score.
H ASES, pre/post
I Pain, pre/post
Functional improvement is particularly attributable to the increase in flexion and abduction, but not to external rotation, which did not usually improve—or not significantly. Thus, various authors now evaluate the degree of active external rotation (specifically of the teres minor muscle) preoperatively using MRI and, if appropriate, carry out a latissimus dorsi transfer in the same session (Gerber et al. 2007, Boileau et al. 2008). Restoration of useful external rotation is possible in some patients, even without any muscle transfer operation. This depends in particular on the presence of a functional infraspinatus and teres minor (Simovitch et al. 2007a). In our patients, it was striking that the external rotation results achieved in the CTA group were markedly better than those in the fracture sequelae group and in the prosthesis revision group (Table 2). This indicates that care should be taken, if anatomically possible, to ensure meticulous reconstruction of the rotator cuff, even in reversed prosthesis implantation. It was not possible to appraise the significance of the condition of the teres minor muscle in our study since MRI films were not available in all patients preoperatively.
Looking at the individual components of the Constant score, pain relief and increase in strength appear to be the most important parameters affecting the general improvement of function (Table 1). This is, of course, mainly due to the number of points attributed to them in the Constant evaluation system (15 and 25 points, respectively) as compared to a maximum of 10 points for the other parameters. It is noteworthy that once again our best results were attained in the CTA group, whereas the fracture sequelae group and the prosthesis revision group showed a lower increase in strength and a lower degree of pain relief. This is consistent with the data published by Wall et al. (2007).
In our opinion, the most interesting result of our investigation was the continuous fall in score values starting after 3 years postoperatively (Figure 4). Several factors would probably explain this decline. Less intensive physiotherapy may play a major role, and patients adapt to an increasing loss of function.
Several factors contributed to the low dislocation rate (3/59) in our series compared to up to 25% in the literature. Important factors are meticulous positioning of the implant components, pre–tensioning of the deltoid and coracobrachial muscles, extensive mobilization, and resection of scarred and contracted parts of the capsule and bone fragments, as well as the best possible reconstruction of the external and internal rotators of the rotator cuff (Boileau et al. 2006a, b, Favard et al. 2006, Wall et al. 2006).
In a survey of the literature, we found relatively high levels of scapular notching (Sirveaux et al. 2004, Werner et al. 2005, Simovitch et al. 2007b). The low rate of dislocation and revision indicates that mistakes in the surgical technique cannot account for the high incidence of scapular notching. Even mild degrees of osteolysis (Sirveaux I and II) are detected using a meticulous radiographic technique. It must be borne in mind that the confirmation of a notching of grade 1 or 2 according to Sirveaux requires an exactly orthograde scan. Otherwise, an incorrectly low notching rate is registered (Sirveaux et al. 2004). It must also be considered that it was not common practice to implant the metal back (metaglene) in a caudal position, consequently at the time of implantation, as recommended today (Nyffeler et al. 2005).
The revision rate (15/59) is similar to that reported in the literature (17–50%) (Werner et al. 2005, Frankle et al. 2006, Molé et al. 2006, Wall et al. 2006, Levy et al. 2007). All revisions were performed in patients with fracture sequelae or prosthesis revision. Similarly, a lower rate of reoperations has been reported in the literature for CTA patients than for those with fracture sequelae or prosthesis revision (Boileau et al. 2006b, Wall et al. 2007). Also, all cases requiring revision due to infection involved patients with preoperative fracture sequelae or revision of a prosthesis.
We found a complication rate of one–third when scapular notching was not taken into account. This is similar to that reported by Levy et al. (2007) for prosthesis revision. Counting all complications (including minor ones), Wall et al. (2006) and Werner et al. (2005) found a complication rate as high as 50%.
In agreement with numerous reports in the literature, our findings indicate that the reversed shoulder prosthesis must be regarded as a salvage procedure despite the astonishingly good results. The gain of function is impressive and depends strongly on etiology, but there are high rates of complications and revisions.
Acknowledgments
No competing interests declared.
All authors contributed equally to the manuscript.
References
- Bateman JE. The diagnosis and treatment of ruptures of the rotator cuff. Surg Clin North Am. 1963;43:1523–30. doi: 10.1016/s0039-6109(16)37139-0. [DOI] [PubMed] [Google Scholar]
- Boileau P, Watkinson DJ, Hatzidakis AM, Balg F. Grammont reverse prosthesis: design, rationale and biomechanics. J Shoulder Elbow Surg (Suppl 1) 2001;14:S147–S61. doi: 10.1016/j.jse.2004.10.006. [DOI] [PubMed] [Google Scholar]
- Boileau P, Chuinard C, Le Huec JC, Walch G, Trojani C. Proximale humerus fracture sequelae: impact of a new radiographic classification on arthroplasty. Clin Orthop. 2006a;((442)):121–30. doi: 10.1097/01.blo.0000195679.87258.6e. [DOI] [PubMed] [Google Scholar]
- Boileau P, Watkinson D, Hatzidakis AM, Hovorka I. The Grammont reverse shoulder prosthesis: Results in cuff tear arthritis, fracture sequelae and revision arthroplasty. J Shoulder Elbow Surg. 2006;15:527–40. doi: 10.1016/j.jse.2006.01.003. [DOI] [PubMed] [Google Scholar]
- Boileau P, Chuinard C, Rousanne Y, Bicknell RT, Rochet N, Trojani C. Reverse shoulder arthroplasty combined with a modified latissimus dorsi and teres major tendon transfer for shoulder paralysis associated with dropping arm . Clin Orthop. 2008;((466)):584–93. doi: 10.1007/s11999-008-0114-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bufquin T, Hersan A, Hubert L, Massin P. Reverse shoulder arthroplasty for the treatment of three– and four–part fractures of the proximal humerus in the elderly. J Bone Joint Surg (Br) 2007;89:516–20. doi: 10.1302/0301-620X.89B4.18435. [DOI] [PubMed] [Google Scholar]
- Edwards TB, Boulahia A, Kempf JF, Boileau P, Nemoz C, Walch G. The influence of rotator cuff disease on the results of shoulder arthroplasty for primary osteoarthritis: results of a multicenter study. J Bone Joint Surg (Am) 2002;84:2240–8. doi: 10.2106/00004623-200212000-00018. [DOI] [PubMed] [Google Scholar]
- Favard L, Le Du C, Bicknell R, Sirveaux F, Levigne C, Boileau P, Molé D, Walch G. Sauramps medical; Montpellier: 2006. Nice shoulder course: Reverse shoulder arthroplasty; pp. 113–23. [Google Scholar]
- Frankle M, Levy JC, Pupello D, Siegal S, Saleem A, Mighell M, Vasey M. The reverse shoulder prosthesis for glenohumeral arthritis associated with severe rotator cuff defiency. A minimum two–year follow–up study of sixty patients. Surgical technique. J Bone Joint Surg (Am) 2006;88:178–90. doi: 10.2106/JBJS.F.00123. [DOI] [PubMed] [Google Scholar]
- Gerber C, Maquieira G, Espinosa N. Latissimus dorsi transfer for the treatment of irreparable rotator cuff tears. J Bone Joint Surg (Am) 2006;88:113–20. doi: 10.2106/JBJS.E.00282. [DOI] [PubMed] [Google Scholar]
- Gerber C, Pennington SD, Lingenfelter EJ, Sukthankar A. Reverse Delta–III total shoulder replacement combined with latissimus dorsi transfer. A preliminary report. J Bone Joint Surg (Am) 2007;89:940–7. doi: 10.2106/JBJS.F.00955. [DOI] [PubMed] [Google Scholar]
- Gonzales JF, Chuinard CH, Boileau P. Sauramps medical; Montpellier: 2006. Reverse total shoulder arthroplasty after failed rotator cuff surgery. Nice shoulder course: Reverse shoulder arthroplasty. pp. 133–47. [DOI] [PubMed] [Google Scholar]
- Grammont PM, Baulot E. Delta shoulder prosthesis for rotator cuff rupture. Orthopedics. 1993;16:65–8. doi: 10.3928/0147-7447-19930101-11. [DOI] [PubMed] [Google Scholar]
- Hamada K, Fukuda H, Mikasa M, Kobayashi Y. Clin Orthop. (254) 1990. Roentgenographic findings in massive rotator cuff tears. A long term observation; pp. 92–6. [PubMed] [Google Scholar]
- Irlenbusch U, Bernsdorf M, Gansen HK, Lorenz U. Latissimus dorsi transfer in case of irreparable rotator cuff tear – a comparative analysis of primary and failed rotator cuff surgery, in dependence on deficiency grade and additional lesions. Z Orthop. 2003;141:650–6. doi: 10.1055/s-2003-812410. [DOI] [PubMed] [Google Scholar]
- Irlenbusch U, Bernsdorf M, Born S, Gansen HK, Lorenz U. Muscular function analysis by electromyography after the latissimus dorsi tendon transfer. J Shoulder Elbow Surg. 2008;17:492–9. doi: 10.1016/j.jse.2007.11.012. [DOI] [PubMed] [Google Scholar]
- Irlenbusch U, Bernsdorf M, Bracht M, Gansen HK, Lorenz U, Thiel J. Latissimus dorsi transfer in case of an irreparable rotator cuff tear – a longitudinal study of 52 patients over 50 months. J Shoulder Elbow Surg. 2008;17:527–34. doi: 10.1016/j.jse.2007.11.022. [DOI] [PubMed] [Google Scholar]
- Irlenbusch U, Fuhrmann U, Rott O. Differential indication of anatomic and reversed shoulder prostheses in fracture sequelae. Z Orthop Unfall. 2008;146:478–85. doi: 10.1055/s-2008-1038814. [DOI] [PubMed] [Google Scholar]
- Jouve F, Wall B, Walch G. Sauramps medical; Montpellier: 2006. Revision of shoulder hemiarthroplasty with reverse prosthesis. Nice shoulder course: Reverse shoulder arthroplasty; pp. 217–28. [Google Scholar]
- Levy J, Frankle M, Mighell M, Pupello D. The use of reversed shoulder prosthesis for the treatment of failed hemiarthroplasty for proximal humerus fracture. J Bone Joint Surg (Am) 2007;89:292–300. doi: 10.2106/JBJS.E.01310. [DOI] [PubMed] [Google Scholar]
- Molé D, Navez G, Turell P, Roche O, Sirveaux F. Sauramps medical; Montpellier: 2006. Reversed prostheses for massive cuff tear without gleno–humeral osteoarthritis. Nice shoulder course: Reverse shoulder arthroplasty; pp. 125–32. [Google Scholar]
- Nwakama AC, Cofield RH, Kavanagh BF, Loehr JF. Semiconstrained total shoulder arthroplasty for glenohumeral arthritis and massive rotator cuff tearing. J Shoulder Elbow Surg. 2000;9:302–7. doi: 10.1067/mse.2000.106467. [DOI] [PubMed] [Google Scholar]
- Nyffeler RW, Werner CM, Simmen BR, Gerber C. Biomechanical relevance of glenoid component positioning in the reverse Delta III total shoulder prosthesis. J Shoulder Elbow Surg. 2005;14:524–8. doi: 10.1016/j.jse.2004.09.010. [DOI] [PubMed] [Google Scholar]
- Patte D. Clin Orthop. (254) 1990. Classification of rotator cuff lesions; pp. 81–6. [PubMed] [Google Scholar]
- Simovitch RW, Naeder H, Zumstein MA, Gerber C. Impact of fatty infiltration if the teres minor muscle on the outcome of reverse total shoulder arthroplasty. J Bone Joint Surg (Am) 2007;89:934–9. doi: 10.2106/JBJS.F.01075. [DOI] [PubMed] [Google Scholar]
- Simovitch RW, Zumstein MA, Lohri E, Helmy N, Gerber C. Predictors of scapular notching in patients managed with the Delta III reverse total shoulder replacement. J Bone Joint Surg (Am) 2007;89:588–600. doi: 10.2106/JBJS.F.00226. [DOI] [PubMed] [Google Scholar]
- Sirveaux F, Favard L, Oudet D, Huquet D, Walch G, Mole D. Grammont inverted total shoulder arthroplasty in the treatment of glenohumeral osteoarthritis with massive rupture of the cuff. Results of a multicentre study of 80 shoulders. J Bone Joint Surg (Br) 2004;86:388–95. doi: 10.1302/0301-620x.86b3.14024. [DOI] [PubMed] [Google Scholar]
- Wall B, Walch G, Jouve F, Mottier F. Sauramps medical; Montpellier: 2006. The reverse shoulder prosthesis for revision of failed total shoulder arthroplasty. Nice shoulder course: Reverse shoulder arthroplasty; pp. 231–42. [Google Scholar]
- Wall B, Nové–Josserand L, O Conner DP, Edwards B, Walch G. Reverse total shoulder arthroplasty: a review of results according to etiology. J Bone Joint Surg (Am) 2007;89:1476–85. doi: 10.2106/JBJS.F.00666. [DOI] [PubMed] [Google Scholar]
- Werner CM, Steinmann PA, Gilbart M, Gerber C. Treatment of painful pseudoparesis due to irreparable rotator cuff dysfunction with the Delta III reverse–ball–and–socket total shoulder prosthesis. J Bone Joint Surg (Am) 2005;87:1476–86. doi: 10.2106/JBJS.D.02342. [DOI] [PubMed] [Google Scholar]