Abstract
Migraine patients who do not respond to conventional therapy, develop unacceptable side-effects, or are reluctant to take medicines resort to complementary and alternative medicines (CAM). Globally, patients have been seeking various non-conventional modes of therapy for the management of their headaches. An Ayurvedic Treatment Protocol (AyTP) comprising five Ayurvedic medicines, namely Narikel Lavan, Sootshekhar Rasa, Sitopaladi Churna, Rason Vati and Godanti Mishran along with regulated diet and lifestyle modifications such as minimum 8 h sleep, 30-60 min morning or evening walk and abstention from smoking/drinking, was tried for migraine treatment. The duration of the therapy was 90 days. Out of 406 migraine patients who were offered this AyTP, 204 patients completed 90 days of treatment. Complete disappearance of headache and associated symptoms at completion of AyTP was observed in 72 (35.2%); mild episode of headache without need of any conventional medicines in 72 (35.2%); low intensity of pain along with conventional medicines in 50 (24.5%); no improvement in seven (3.4%) and worst pain was noted in three (1.4%) patients, respectively. In 144 (70.5%) of patients marked reduction of migraine frequency and pain intensity observed may be because of the AyTP. Though the uncontrolled open-label design of this study does not allow us to draw a definite conclusion, from this observational study we can make a preliminary assessment regarding the effectiveness of this ayurvedic treatment protocol.
Keywords: Alternative therapy, Ayurveda, CAM, migraine
INTRODUCTION
Migraine is a widespread, chronic and intermittently disabling disorder characterized by recurrent headaches with or without aura.[1] Recent studies estimate the prevalence of migraine at about 6-8% in men and 12-15% in women. In terms of actual numbers of attacks, combined figures from prevalence and incidence studies suggest 3000 migraine attacks occur every day for each million of the general population.[2] The rate of migraine varies globally, and although there is a lack of epidemiological data available in many countries at present, recent anecdotal evidence suggests higher rates in certain places like India.[3]
Pharmaceutical treatment of migraine is complex, with no agreed upon guidelines. Most individuals often need medication during acute attacks and some prophylactic measure to reduce attacks.[2] Moreover, the uncertainty regarding treatment and the need to perhaps trial patients on a variety of drugs adds to the escalating costs. Some specific drugs such as Triptans and ergotamine tartrate are often expensive and not commonly used in resource-poor countries, resulting in a significant amount of pain and disability.[4] Another problem is the actual overuse of such medications which causes ‘medication overuse headache’ (MOH), further complicating management strategies.[5]
A large percentage of patients do not respond to pharmacological interventions for migraine headache, develop unacceptable side-effects, or are reluctant to take medications[6]. As a result many patients resort to many complementary and alternative therapies like acupuncture,[7] biofeedback therapy,[8] relaxation therapy, herbal remedies and vitamin or mineral supplementation.[6] Recent studies have demonstrated the effectiveness of acupuncture[9] and Yoga[10] in the reduction of migraine headache. The use of complementary and alternative medicine (CAM) in migraine is a growing phenomenon which, though increasingly widespread, is poorly understood.[11] Ayurveda is a traditional medical system used by a majority of India's 1.1 billion population.[12] The principal author in his clinical practice first observed that a judicious combination of five Ayurvedic medicines can markedly reduced the migraine frequency in some migraine patients. Later, an Ayurvedic Treatment Protocol (AyTP) comprising these five ayurvedic medicines along with regulated diet and lifestyle modifications was developed for migraine treatment. This AyTP was tried by over 600 migraine patients.[13] The background work of this AyTP was first carried out in Dhanwamtari Ayurvedic College and Hospital, Chandigarh from June 2002 to December 2004. [13] In this series we report the analysis of the observational prospective clinical study of this AyTP carried on 406 migraine patients in nine major cities of south India.
MATERIALS AND METHODS
Study period
May 2005 to March 2007.
Settings
This study was carried out in the clinics of 17 Vaidyas in nine major cities of South India, the details of which are given in Table 1.
Table 1.
Study carried out in the clinics of 17 Vaidyas in nine major cities of South India
| Place | Name of Vaidya | Patients Enrolled |
|---|---|---|
| Aurangabad | Vd. N Patil | 7 |
| Bengaluru | Vd. SS Hiremath, Vd. S Kulkarni, Vd. VM | 264 |
| (Bangalore) | Bhat Aroor, Vd. Prashanth MV, Vd, R Babu | |
| Bellary | Vd. Shailaja HB, Vd. Hema Desai DN, Vd. Savitha BP | 37 |
| Dharwad | Vd. Sushma RH | 10 |
| Hyderabad | Vd. Sangamesh Benne, Vd. Vijaysimha R | 12 |
| Mysore | Vd. Prasanna Venkatesh TS, Vd. K Suresh Kumar | 31 |
| Shimoga | Vd. Chitralekha V Krishna | 8 |
| Tumkur | Vd. Sunil Kumar K | 31 |
| Warangal | Vd. Mallikarjun K | 6 |
Treatment Protocol
The treatment protocol was derived from the Ayurvedic concept of diagnosis of Amla-Pitta a state of acid-alkali imbalance causing one of the symptoms of Shiro ruja (headache). A uniform AyTP was developed which comprised of a combination of five ayurvedic formulations (Narikel Lavan (NL), Sootshekhar Rasa (SR), Sitopaladi Churna (SC), Rason Vati (RV) and Godanti Mishran (GM)[14,15] along with regulated diet (three meals and three snacks providing adequate calories and meals devoid of nicotine, caffeine, reheated food, aerated drink), and lifestyle modification included minimum 8 h sleep, moderate exercise such as morning or evening walk for 30-60 min and abstention from smoking / drinking.
Composition
Narikela Lavan
Narikel shell - Cocus nucifera
Saindhava lavana - Rock salt
A fully-ripe coconut is taken, the shell is removed and a hole is made at the top of the coconut. Powdered rock salt is put through the hole till the water in the coconut rises to the level of the hole. The coconut is then covered by clay smeared cloth in three consecutive layers and dried. This is put into a puta of 10-15 cowdung cakes/ furnace. When cool, the charred coconut containing salt is powdered in a khalva.
The composition of other medicines is given in Tables 2–5.
Table 2.
Composition of Sootshekhar Rasa
| Traditional name | English / scientific name | Proportion |
|---|---|---|
| Suddha Parada | Processed cinnabar | 1 part |
| Suddha Gandhaka | Processed sulphur | 1 part |
| Dalchini | Cinnamomum zeylanica | 1 part |
| Chhoti Elachi | Elleteria cardamomum | 1 part |
| Tej patta | Cinnamomum tamala | 1 part |
| Nagkesar | Mesua jerrea | 1 part |
| Shankh Bhasma | Turbinella pyrum | 1 part |
| Swarna makshika Bhasma | Chalco pyrite | 1 part |
| Ropya Bhasma | Argentum | 1 part |
| Tamra Bhasma | Cuprum | 1 part |
| Dhatura's seed | Datura metel | 1 part |
| Suhaga | Borax sodium borate | 1 part |
| Saunti | Zingiber officinale | 1 part |
| Kali mircha | Piper nigrum | 1 part |
| Chhoti pippal | Piper longum | 1 part |
| Bhringraj swarasa | Eclipta Alba | Q.S (for mardana) |
Table 5.
Composition of Godanti Mishran
| Traditional name | English / scientific name | Proportion |
|---|---|---|
| Godanti bhasma | Gypsum | 8 parts |
| Jahar mohara pisti | Serpentine | 2 parts |
| Rasadi vati | 2 parts |
Table 3.
Composition of Sitopaladi Churna
| Traditional name | English / scientific name | Proportion |
|---|---|---|
| Mishri | Sugar candy | 16 parts |
| Vanslochan | Bambusa arumdimaceo | 8 parts |
| Chhoti Pippali | Piper longum | 4 parts |
| Chhoti Elachi | Ellettaria cardamomum | 2 parts |
| Dalchini | Cinnamomum zeylanica | 1 part |
Table 4.
Composition of Rason Vati
| Traditional name | English / scientific name | Proportion |
|---|---|---|
| Lasuna | Allium sativum | 1 part |
| Jiraka | Cuminum cyminum | 1 part |
| Saindhava lavana | Rock salt | 1 part |
| Gandhaka-suddha | Processed sulphur | 1 part |
| Sunthi | Zingiber officinale | 1 part |
| Marica | Piper nigrum | 1 part |
| Pippali | Piper longum | 1 part |
| Hingu | Ferula foetida | 1 part |
| Nimbu rasa | Citrus medica juice | QS for bhavana |
Medicine dosage and duration
The daily recommended doses of these combined formulations were 7.3 g per day (NL 2000 mg, SR 375 mg, SC 1425 mg, RV 3000 mg, GM 500 mg). The treatment period was for 90 days. During AyTP the patients were not allowed to take any other alternative medications.
Manufacturing of Medicine
The Ayurvedic medicines were prepared by Bharat Bhaishajaya Shala Private Limited, Dehradun under the manufacturing license issued by the Government of Uttarakhand, India. The medicines are manufactured under the GMP guidelines and following the stringent procedures as mentioned in the classical texts of Ayurveda.
Subjects and Diagnosis
A total of 406 migraine patients (M:133; F:273) were offered this AyTP. All the patients were chronic sufferers and had earlier consulted a neurologist for their migraine.
Eligibility
Criteria for inclusion were: individuals of either gender, age 10 and above, meeting the International Classification of Headache Disorders (ICHD) criteria [16] for migraine without aura [Table 6]. Exclusion criteria included marked depression, anxiety or psychosis; more than two visits/month for mental healthcare; more than one psychiatric medication; major medical illness under treatment; pregnancy.
Table 6.
Eligibility of subjects for observational clinical study on AyTP for migraine
| Inclusion Criteria | Exclusion Criteria |
|---|---|
| Subject > 10 years of age | Marked depression, anxiety or |
| Either gender | psychosis |
| Meet ICHD* criteria for migraine | Major medical illness under |
| Headache history > 2 years | treatment |
| Willing to follow the dietary | Pregnancy |
| restriction | Clotting disorders |
| Willing to complete daily diary | More than 2 visits/month for |
| Willing to take the medication | mental healthcar |
| for 90 days | Use of any other alternative |
| medication during AyTP study | |
| period |
International Classification of Headache Disorders
Screening, consent, and enrollment
Interested migraine patients who contacted Vaidyas in their clinics were first screened for eligibility. The patients then underwent a baseline medical assessment, including a complete medical history and physical examination. The abdomen of all patients was especially examined. Patients having any serious health problem or comorbid illness were not selected for undergoing AyTP. Eligible patients were first explained the treatment procedure in detail. Patients who were willing to follow the set norms of the AyTP were then enrolled for the study after taking a written consent. Clinical details of the patients were entered in a clinical record form (CRF), which was updated after each visit.
Monitoring Progress of Patients
Eligible patients were instructed to maintain a daily headache diary after the start of AyTP. Subjects had the option of completing the diary either on paper / postcard and mailing it to their respective Vaidyas. Alternatively, they could report via telephone. However, all patients were asked to visit the clinics at the start of therapy, then at Day 30, 60 and at stoppage of therapy at Day 90. However, patients were advised to report to the clinic in case of emergency.
Outcome Measures
The primary outcome variables for this study included frequency and intensity of headache and self-perceived benefit of the intervention at Day 30, 60 and 90. Detailed description of these variables follows:
Headache frequency
Determination from the daily headache diary the total number of headache frequency the patient had after the start of therapy. The subjects were also instructed to record the presence and intensity of their headaches on a daily basis. Additionally, the subjects were invited to comment on the nature of their headache, the associated symptoms, and the suspected triggers.
Headache intensity
The visual analogue scale (VAS) and numeric rating scale (NRS) was used to measure the intensity of pain. VAS from no pain (= 0) to worst pain imaginable [=10 (or 100)] and the five- point categorical verbal rating scale (VRS) i.e., score 0 = none; 1-3 = mild; 4-6 = moderate; 7-8 = severe; 9-10 = worst. Guide to grading headache intensity was included with each diary.
Headache-related disability: MIDAS
Disability, defined as the consequences of illness on the ability to work and function, is measured using the Migraine Disability Assessment Score (MIDAS).[17] Derived from the Headache Impact Test, MIDAS is a seven-item questionnaire that assesses the number of days during the previous three months that respondents missed work or school, experienced decreased productivity at work or home, or missed social engagements because of headaches. The definition of various grades is mentioned in Table 7.
Table 7.
The definition of various grades
| Grade | Definition | Score |
|---|---|---|
| I | Minimal or infrequent disability | 0-5 |
| II | Mild or infrequent disability | 6-10 |
| III | Moderate disability | 11-20 |
| IV | Severe disability | 21+ |
Adverse events
Reports of adverse events were obtained from the patients during their visit to the clinic, self-reports in the headache diaries or by direct contact with patients via telephone.
Statistical Analysis
Kruskal Wallis test was used to compare the VAS score on day 30, day 60 and day 90 from the base line. Paired t-test was used to compare the headache days. The level of significance was set at P<0.05. The statistical analysis was performed using the Statistical Package for Social Sciences (SPSS 12.0).
RESULT
The prevalence of migraine was found to be higher in the age group 20-50 years, with the highest ranging between >30-< 40 years [Figure 1]. Around 90% of the patients were non-vegetarian and 155 (38%) patients had family history of headache. Details of the prior treatment of migraine patients indicated that 231 (57%) patients were totally dependent on allopathic medicine; 167 (41%) patients had tried both allopathic and alternative medicine such as Homeopathy, Unani / Siddha, Ayurveda and Naturopathy etc., and eight (2%) patients were totally dependent on alternative medicine. It was found that exertion, lack of sleep and hunger were the three most important factors for aggravating migraine, and details of other factors are given in Figure 2. History of headache of migraine patients ranged from 1 to 60 years [Figure 3]. At the time of enrollment all the patients reported more than five attacks in a year from occasional, daily, alternate day and five to eight days in a month. The maximum patients those who were enrolled had migraine attack once a week. Maximum migraineurs complained of nausea, photo phobia, phono phobia, and vomiting as associated symptoms [Figure 4]. Nearly 50% reported moderate to extreme fatigue besides heartburn, belching, blurred vision, flatus, constipation etc.
Figure 1.
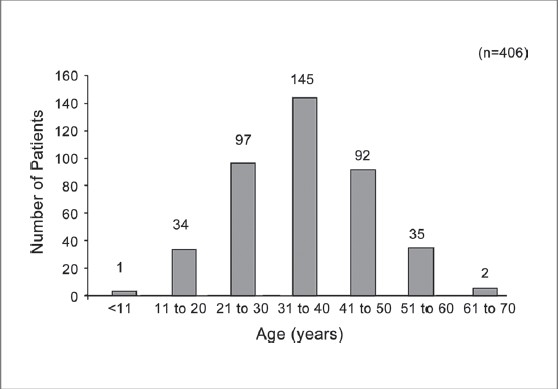
Agewise distribution of migraine patients
Figure 2.
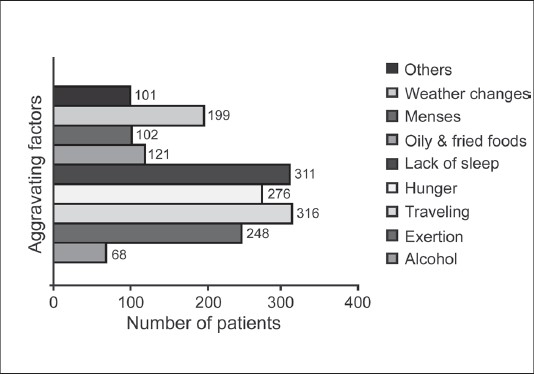
Various aggravating factors reported by migraine patients
Figure 3.
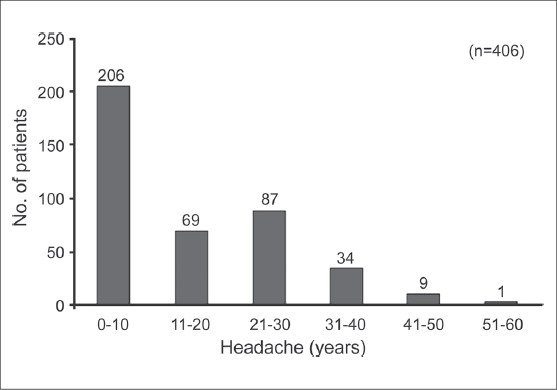
History of headache of migraine patients
Figure 4.
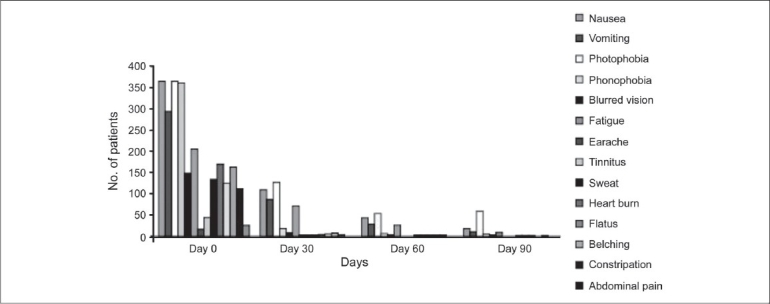
Various associated symptoms with migraine
A total of 406 patients were offered this AyTP, however, after 30 days 129 (31.7%) and after 60 days 41(14.8%) patients dropped out, respectively. A total of 204 (50.2%) patients completed 90 days of therapy. Complete disappearance of headache and associated symptoms at completion of AyTP was observed in 72 (35.2%); mild episode of headache without need of any conventional medicines in 72 (35.2%); low intensity of pain along with conventional medicines in 50 (24.5%); no improvement in seven (3.4%) and worst pain was noted in three (1.4%) patients, respectively [Figure 5]. There was a significant reduction in the VAS score after the start of AyTP [Table 8].
Figure 5.
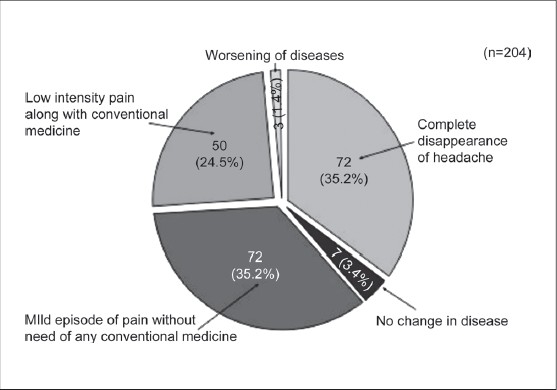
Overall response of Ayurvedic treatment protocol on completion of 90 days of therapy
Table 8.
Effect of AyTP on VAS score of migraine patients
| VAS score | N | Mean | SD | P value |
|---|---|---|---|---|
| Day 0 | 356 | 0.72 | ---- | |
| Day 30 | 204 | 2.15 | 1.11 | <0.001 |
| Day 60 | 1.40 | 1.08 | <0.001 | |
| Day 90 | 1.0 | 0.93 | <0.001 |
To study the impact of the AyTP on headache days 166 patients were randomly interviewed at the time of enrollment and after completing 90 days of treatment. It was observed that there was a highly significant reduction in headache days among the treated migraineurs [Figure 6]. Decrease in MIDAS score was observed after 90 days of therapy. At the start of therapy the number of patients assigned various grades of MIDAS were as follows: Grade I -110 (27.0%); Grade II - 70 (17.2%); Grade III-100 (24.6%); Grade IV-126 (31.0%), which changed after the completion of therapy viz. Grade I-171 (83.8%); Grade II -18 (8.8%); Grade III-nine (4.4%), and Grade IV-four (1.9%), respectively.
Figure 6.
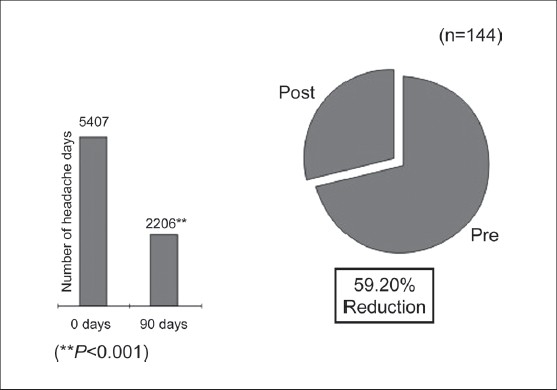
Impact of AyTP on days of occurrence of headache
In 45 (11.0%) patients it was observed that the clinical condition deteriorated after the start of AyTP, hence, the therapy was stopped immediately. However, patients who responded to this therapy and completed 90 days of treatment did not show any noticeable side-effects.
DISCUSSION
Though Ayurvedic therapy is popular among migraine sufferers, there are very few reports available on the efficacy and toxicity of these therapies. Moreover, classical Vaidyas treat patients on the basis of presenting symptoms and hence, there is quite a variation in the selection of Ayurvedic medicines by different Vaidyas. However, for the present study a uniform treatment protocol (AyTP) was first designed and the same was offered to all migraine patients. Generally, the patients who visited the clinics for AyTP were not satisfied with conventional therapy. Many wanted to try the AyTP on an experimental basis. The first author in his clinical practice observed that the combination of five Ayurvedic therapy can reduce the migraine frequency and intensity of pain in some patients and hence further collected sufficient evidence to start a clinical trial on 131 migraine patients in the Dhanwamtari Ayurvedic College and Hospital, Chandigarh in 2002.[15] The results of the trial encouraged us to take up the present investigation in a planned manner. This AyTP is now being used by various Vaidyas in various places of India, especially in the southern parts.
Migraine was distinguished from common headache by Tissot in 1783 for the first time who ascribed it to a supra-orbital neuralgia provoked by reflexes from the stomach, gall bladder or uterus. Later, migraine was classified as a neurological disorder. Our hypothesis is quite similar to Tissot's idea on the pathogenesis of migraine, viz. that it usually arose from stomach disturbance.[18] Incidentally, there is a close correlation between the symptoms of migraine with those of Amla-pitta (state of acid-alkali imbalance in the body) causing symptoms such as: brahma (confusion), moorcha (fainting), aruchi (anorexia), aalasya (fatigue), chardi (vomiting), prasek (nausea), mukhmadhurya (sweetness in the mouth) and shiroruja (headache). The correlation between the cause and symptoms of Amla-pitta match the current diagnosis criteria of migraine. It may be possible that the combination of Narikel Lavan, Sootashekhara Rasa, Sitopaladi Churna, Rason Vati and Godanti Mishran in conjunction with regulated lifestyle and diet may have restored the acid-alkali balance, and restored / strengthened the functioning of the gastrointestinal system. A better acid-alkali balance in the body may have been responsible for reducing the frequency of migraine.
The herbo-mineral Ayurvedic medicines used for the migraine treatment contained Bhasma[19] of silver, copper and mercury and many immunomodulatory medicinal herbs, namely Alium sativum, Eclipta alba, Cinnmomum zeylanica, Zingiber officinalis, Piper longum, Piper nigrum, Bambusa arumdinaceae, Ellettaria cardamomum and Cinnamomum cassia, Ferula northrax, Citrus acida etc. Some ingredients used for medicine preparations are moderate to severely toxic in the raw form (ashodhit). However, intrigue processing (shodhan) converts these toxic materials to complex mineral forms which are nontoxic. However, improper processing/ manufacturing of Ayurvedic medicines may result in severe toxicity.[20] Hence, the safety profile of the combined formulations was first established in animal models. It was observed that mice feed four times and rats 10 times more the daily equivalent human dose did not produce any toxicity.[21] In this present study it was observed that in 11% of patients the clinical conditions deteriorated after the start of the AyTP. We are at this moment unable to explain what was the exact cause for this; however, the Ayurvedic medicine was well tolerated by other patients.
During the last few decades, plants have been increasingly employed as a herbal remedy for migraine treatment and prophylaxis,[22] examples include Feverfew (Tanacetum parthenium),[23] Butterbur (Petasites hybridus),[24], etc. Most surveys agree that herbal remedies are amongst the most prevalent therapies and that headache/migraine is one of the most frequent reasons for trying plant-derived medications.[25] Complimentary and Alternative Medicine (CAM) is often perceived by the public to be more helpful than conventional care for the treatment of headache.[26] Recent studies have indicated that Ayurvedic medicines can be effective in treatment of tension-type headache.[27]
From this observational study we can make a preliminary assessment regarding the effectiveness of this Ayurvedic treatment protocol in migraine treatment. Baring a few, the Ayurvedic medications were well tolerated by patients. Marked reduction of migraine frequency and pain intensity observed in patients with AyTP needs attention. However, to ascertain the real effectiveness of this AyTP a properly controlled clinical trial with a larger patient population is required.
Acknowledgments
The authors like to thank Dr. Sanjoy Kumar Pal, Sr. Scientific Manager, Ipca Traditional Remedies Pvt. Ltd. for drafting this manuscript. Mr. Nitin Chandurkar and Mitesh Sharma from Ipca Laboratories limited for data management and statistical analysis.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Lantéri-Minet M. The role of general practitioner in migraine management. Cephalalgia. 2008;28:1–8. doi: 10.1111/j.1468-2982.2008.01684.x. [DOI] [PubMed] [Google Scholar]
- 2.Vijayan S. Migraine: An expensive headache to the world. Available from http://thelancetstudent.com/2008/03/16/ migraine-an-expensive-headache-to-the-globe/. [last assessed on 2010 Feb 10]
- 3.Ravishankar K. Barriers to headache care in India and effort to improve the situation. Lancet Neurol. 2004;3:564–7. doi: 10.1016/S1474-4422(04)00855-5. [DOI] [PubMed] [Google Scholar]
- 4.Neurological Disorders: Public health challenges. World Health Organization. 2006.
- 5.Limmroth V, Kazarawa Z, Fritsche G, Diener HC. Headache after frequent use of serotonin agonists zolmitriptan and naratriptan. Lancet. 1999;353:78. doi: 10.1016/S0140-6736(05)74950-3. [DOI] [PubMed] [Google Scholar]
- 6.Mauskop A. Complementary and alternative treatments for migraine. Drug Dev Res. 2008;68:424–7. [Google Scholar]
- 7.Witt CM, Reinhold T, Jena S, Brinkhaus B, Willich SN. Cephalalgia. 2008;28:334–45. doi: 10.1111/j.1468-2982.2007.01504.x. [DOI] [PubMed] [Google Scholar]
- 8.Nestoriuc Y, Martin A, Rief W, Andrasik F. Biofeedback treatment for headache disorders: A comprehensive efficacy review. Appl Psychophysiol Biofeedback. 2008;33:125–40. doi: 10.1007/s10484-008-9060-3. [DOI] [PubMed] [Google Scholar]
- 9.Facco E, Liguori A, Petti F, Zanette G, Coluzzi F, De Nardin M, et al. Traditional acupuncture in migraine: A controlled, randomized study. Headache. 2008;48:398–407. doi: 10.1111/j.1526-4610.2007.00916.x. [DOI] [PubMed] [Google Scholar]
- 10.John PJ, Sharma N, Sharma CM, Kankane A. Effectiveness of yoga therapy in the treatment of migraine without aura: A randomized controlled trial. Headache. 2007;47:654–61. doi: 10.1111/j.1526-4610.2007.00789.x. [DOI] [PubMed] [Google Scholar]
- 11.Rossi P, Di Lorenzo G, Malpezzi MG, Faroni J, Cesarino F, Di Lorenzo C, et al. Prevalence, pattern and predictors of use of complementary and alternative medicine (CAM) in migraine patients attending a headache clinic in Italy. Cephalalgia. 2005;25:493–506. doi: 10.1111/j.1468-2982.2005.00898.x. [DOI] [PubMed] [Google Scholar]
- 12.Gogtay NJ, Bhatt HA, Dalvi SS, Kshirsagar NA. The use and safety of non-allopathic Indian medicines. Drug Saf. 2002;25:1005–19. doi: 10.2165/00002018-200225140-00003. [DOI] [PubMed] [Google Scholar]
- 13.Prakash VB, Pareek A, Bhat V, Chandrukar N, Babu R. Response to ayurvedic treatment in prevention of migraine: An update of multicentric observational clinical study. Cephalalgia. 2007;27:745. [Google Scholar]
- 14.Acharya Jadavji Trikramji. Siddha Yogya Sangrah [Hindi] 13th ed. Jhansi, India: Baidyanath Bhawan; 1935. [Google Scholar]
- 15.Prakash VB, Pareek A, Narayan JP. Observational study of ayurvedic treatment on migraine without aura. Int J Head. 2006;26:1317. [Google Scholar]
- 16.ICHD-2. The International classification of Headache Disorder. 2nd ed. Cephalalgia: 2004. pp. 1– 160. [Google Scholar]
- 17.Stewart WF, Lipton RB, Dowson AJ, Sawyer J, Lee C, Liberman JN. Development and testing of the Migraine Disability Assessment (MIDAS) Questionnaire to assess headache-related disability. Neurology. 2001;56:SS20–228. doi: 10.1212/wnl.56.suppl_1.s20. [DOI] [PubMed] [Google Scholar]
- 18.Eadie MJ. An 18th century understanding of migraine - Samuel Tissot (1728-1797) J Clin Neurosci. 2003;10:414–9. doi: 10.1016/s0967-5868(03)00067-5. [DOI] [PubMed] [Google Scholar]
- 19.Bhasma, Wikipedia Available from: http://en.wikipedia.org/wiki/Bhasma.[last assessed on 2010 Feb 10]
- 20.Karri SK, Saper RB, Kales SN. Lead encephalopathy due to traditional medicines. Curr Drug Saf. 2008;3:54–9. doi: 10.2174/157488608783333907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Pal SK, Prakash VB, Chandurkar N, Saraf MN. Safety studies on combination of four Rasa-aushadies in rodents using OECD parameters. In program and abstract book of Symposium on Safety Profile of Rasaushadhies. 2009 Held at Banaras Hindu University, Varanasi on February 06-07. [Google Scholar]
- 22.Vogler BK, Pittler MH, Ernst E. Feverfew as a preventive treatment for migraine: A systematic review. Cephalalgia. 1998;18:704–8. doi: 10.1046/j.1468-2982.1998.1810704.x. [DOI] [PubMed] [Google Scholar]
- 23.Evans RW, Taylor FR. “Natural” or alternative medication for migraine prevention. Headache. 2006;46:1012–8. doi: 10.1111/j.1526-4610.2006.00473.x. [DOI] [PubMed] [Google Scholar]
- 24.Grossmann W, Schmidramsl H. An extract of Petasites hybridus is effective in the prophylaxis of migraine. Altern Med Rev. 2001;6:303–10. [PubMed] [Google Scholar]
- 25.Astin JA. Why patients use alternative medicine: Results of a national study. J Am Med Assoc. 1998;279:1548–53. doi: 10.1001/jama.279.19.1548. [DOI] [PubMed] [Google Scholar]
- 26.MacLennan AH, Wii DH, Taylor AW. Prevalence and cost of alternative medicine in Australia. Lancet. 1996:347569–73. doi: 10.1016/s0140-6736(96)91271-4. [DOI] [PubMed] [Google Scholar]
- 27.Rastogi S. Management of tension-type headache with ayurveda. Alter Compl Ther. 2009;15:113–8. [Google Scholar]


