Abstract
This article describes the development and validation of an instrument to assess cognitively mediated functional abilities in older adults, Everyday Cognition (ECog). The ECog is an informant-rated questionnaire comprised of multiple subscales. Confirmatory factor analysis (CFA) was used to examine its factor structure. Convergent validity was evaluated by comparing it to established measures of everyday function. External validity was evaluated by comparing ECog results across different clinical groups [cognitively normal, mild cognitive impairment (MCI), dementia]. CFA supported a seven-factor model including one global factor and six domain-specific factors (Everyday Memory, Language, Visuospatial Abilities, Planning, Organization, and Divided attention). The ECog correlated with established measures of functional status and global cognition, but only weakly with age and education. The clinical groups performed differently in each domain. In addition to the global factor, the Everyday Memory factor independently differentiated MCI from Normal, while the Everyday Language domain differentiated Dementia from MCI. Different subtypes of MCI also showed different patterns. Results suggest the ECog shows promise as a useful tool for the measurement of general and domain-specific everyday functions in the elderly.
Keywords: functional impairment, everyday function, aging, instrument validation, factor analysis
The impact of cognitive loss on everyday function is a major issue for elderly persons and those who care for them. Impairments in real-world functioning are associated with reduced quality of life for patients and their caregivers, increased economic burden, and can ultimately result in the loss of the ability to live independently (Ernst, 1997; Hope, Keene, Gedling, Fairburn, & Jacob, 1998; Jorm, 1994; Wolinsky & Johnson, 1991). The early detection and systematic characterization of functional impairment has important clinical and research applications. From a diagnostic perspective, dementia is a syndrome defined by both cognitive and functional impairments. Systematic assessment of daily function also offers the potential for improving our understanding of the determinants of functional impairment—specific cognitive deficits, for example—and may guide the development of new interventions aimed at prolonging independent function in the elderly. Thus, estimating an individual's ability to function in daily life is frequently an important aspect of neuropsychological evaluation. Despite its importance, deficiencies in methods of assessing everyday function currently limit scientific progress on this topic.
There are three general approaches to measuring everyday function: self-report, informant-report, and performance-based measures. Self-report has been shown to be problematic in individuals with cognitive impairment as evidenced by poor self and informant agreement, a gap that widens with dementia severity (DeBettignies, Mahurin, & Pirozzolo, 1990; Seltzer, Vasterling, Mathias, & Brennan, 2001). Alternatively, several performance-based measures of everyday functioning have been developed in which patients carry out specific, well-defined functional tasks under the direct observation of a trained rater. Some investigators have argued that this is the most valid and reliable method of assessing functional abilities (Giovannetti, Schmidt, Gallo, Sestito, & Libon, 2006). However, performance-based measures are most often administered under artificial conditions in which the individual is prompted to engage in a task and provided with all of the materials they need. Observed behavior under such contrived situations may differ greatly from what the individual does spontaneously in their real and familiar environment. Additionally, most performance-based scales are time consuming and require extensive equipment, rendering them impractical for routine use. More practical in many situations is obtaining ratings by someone who knows the patient well. Use of an informant or proxy to rate an individual's everyday functioning has been shown to be useful in differentiating individuals with dementia from healthy elders (DeBettignies et al., 1990; Isella et al., 2006; Jorm & Jacomb, 1989; Jorm & Korten, 1988; Kemp, Brodaty, Pond, & Luscombe, 2002; Seltzer et al., 2001) and in predicting who will go on to show further decline (Jorm, Christensen, Jacomb, Korten, & Mackinnon, 2001) or develop a dementia (Daly et al., 2000b; Harwood, Hope, & Jacoby, 1997). This method of functional assessment has the advantage of utilizing raters who are familiar with the individual's performance in real-world environments. Although an informant is not available for everyone, the approach is, in most situations, highly cost-effective and time efficient and easily implemented in both clinical settings and large-scale research studies.
A number of informant-based measures of everyday function currently exist. However, all suffer from a number of limitations, one of which has been an overreliance on global indices of functional status that lump potentially disparate functional abilities together. The proposition that there are distinguishable domains of cognitive function and that these can be measured relatively specifically by targeted neuropsychological tests is not controversial. That is, despite ongoing controversies regarding theoretical conceptualization of precise cognitive functions and how they are represented in the brain, it is clear that tests of episodic memory, for example, measure memory function, which is distinguishable from a set of expressive language functions that can also be measured by appropriate tests. However, very few instruments have been developed to specifically measure the everyday correlates of different neuropsychological domains. Those instruments that do exist focus on only one or a limited number of domains (Grace, Stout, & Malloy, 1999; Jorm & Korten, 1988; Williams, 1987).
The predominant model of everyday function in older adults has remained essentially unchanged for the last four decades. It broadly divides activities of daily living (ADLs) into low-level basic self-care behaviors and higher-level “instrumental” ADLs (IADL). Research has generally supported this hierarchical arrangement of functional skills by demonstrating that instrumental ADLs are affected earlier in the course of dementia (Kemp et al., 2002; Richardson, Nadler, & Malloy, 1995; Tomaszewski Farias, Mungas, & Jagust, 2005), whereas basic ADLs are preserved until relatively late in the course (Sclan & Reisber, 1992; Suurmeijer et al., 1994). Studies have also shown that instrumental ADLs with a strong cognitive component can reliably be distinguished from more basic ADLs (Fitzgerald, Smith, Martin, Freedman, & Wolinsky, 1993; Wolinsky & Johnson, 1991). Although the dominant model had divided ADLs into basic and instrumental ADLs, the critical underlying constructs may not reflect the distinction between whether an activity is “basic” or “instrumental” but rather may be based on the relevant abilities that support performance of the activities. It is likely that activities that would broadly be construed as instrumental or higher level functional activities could be further subdivided to reflect relevant underlying cognitive abilities. Thus, an alternative approach hypothesizes that different daily tasks vary in the degree to which they require specific cognitive abilities and that it will be useful to categorize functional tasks according to the underlying cognitive abilities that they require. Some tasks may require mostly episodic memory, for instance recalling items to be purchased at the store, whereas others may require mainly spatial abilities, for example, navigating the route to the store. If everyday function could be fractionated in this way, it would permit rationally based investigations of the relationships between specific types of neuropsychological deficit and specific types of functional impairments. The ability to link domains of daily function to particular domains of cognitive function could lead to a greatly improved understanding of daily function. For example, this might improve our ability to make meaningful predictions about which specific functional declines might result from specific cognitive impairments or about how the nature of functional change may vary across different clinical disorders that have different cognitive/neuropsychological profiles.
Two additional limitations of previously developed measures of everyday function include poor sensitivity to mild functional impairment and to change over time. Most previous functional instruments were developed to assess functional impairments that occur in the midst of a frank dementia, with the focus often being on functional impairments that occur within the moderate and severe stages of disease. With the emerging emphasis on identifying the prodromal stages of dementia [e.g., a state often referred to as Mild Cognitive Impairment (MCI)] in anticipation of disease altering treatments, it is important to be able to detect the very mild functional changes that occur before a dementia can be diagnosed. Finally, increased sensitivity to subtle differences in function will likely result in a more accurate assessment of change over time. This will have the benefit of improving our ability to characterize the patterns of change in function over time and to monitor change in response to treatment.
To address the limitations of existing functional instruments, we have developed a new functional instrument called Everyday Cognition (ECog). The goal was to create a psychometrically rigorous instrument to assess the functional abilities of older adults across a wide range of ability, spanning normal aging through mild to moderate dementia. Particular emphasis was placed on assessing those functional changes that may occur very early in the course of an incipient degenerative disease, for example during the syndrome of MCI. Development of the ECog was guided by an underlying conceptual model that suggests (1) everyday functioning is a multidimensional rather than a uni-dimensional construct and, (2) different domains of everyday function can be measured by identifying functional tasks that rely, to large extent, on particular cognitive abilities. Thus, an a priori goal was to develop a multidimensional instrument capable of measuring impairment and change in domains of everyday/real-world functioning relevant to specific neuropsychological domains: Everyday Memory, Everyday Language, Everyday Semantic Knowledge, Everyday Visuospatial abilities, and three everyday executive domains including Everyday Planning, Everyday Organization, and Everyday Divided Attention. These functional domains were identified because they correspond to well-accepted domains of cognitive functioning and are important in the evaluation of different types of dementia in older adults.
In this paper we describe the development and initial validation of the ECog. Confirmatory factor analysis (CFA) was used to evaluate the construct validity of the ECog, and to determine whether the factor structure of the instrument supports the proposed individual subscales or domains. We expected that items would be highly intercorrelated but that within-domain correlations would be stronger than cross-domain correlations. Thus, individual items would be influenced by a nonspecific factor representing overall level of functional impairment and by an independent domain-specific factor corresponding to the functional domains measured by the ECog. Next, associations between the ECog and established measures of everyday function and disease/cognitive impairment severity were evaluated (convergent validity). Finally, we examined how different clinical groups (healthy older adults, older adults with MCI, and those with dementia) performed on each of the scales of the ECog (external validity). The incremental validity of the domain specific ECog factors in discriminating the clinical groups was also examined.
Method
Instrument Development
Initial item development
An initial pool of possible items was developed first by surveying existing measures and reviewing the literature to identify functional activities important in the assessment of older adults. We then identified eight experts of various disciplines (e.g., neuropsychologists, neurologists, nurses) who all had clinical and research expertise in aging and dementia. These experts were asked to generate items of everyday functioning within each of the seven a priori domains (Everyday Memory, Everyday Language, Everyday Semantic Knowledge, Everyday Visuospatial abilities, Everyday Planning, Everyday Organization, and Everyday Divided Attention). These two methods resulted in a total of 138 potential items.
The next step was to identify a subset of the items that experts viewed as particularly important and also best corresponded to the domains in which they were included (content validity). To identify this subset of items, the experts rated the 138 items along a variety of dimensions. First, each item was rated as to what stage of dementia the ability would most typically be affected. These ratings were based on a 5-point scale: 1 = occurs in very early/preclinical stage of dementia and possibly with normal aging, 2 = occurs in patients with mild cognitive impairment not meeting criteria for dementia (MCI), 3 = occurs with mild dementia, 4 = occurs with moderate dementia, 5 = occurs with severe dementia. With these ratings we identified and retained items at each ability level. Because of the emphasis on functional change associated with early stages of disease, more items representing the earliest stages were retained, as compared to items reflecting later-stage disease impairments. Next, each item was given an overall priority rating according to how clinically relevant and important the item was to the cognitive and functional assessment of older adults. These ratings were also made on a five-point scale ranging from: 5 = very important item to 1 = very poor item/do not recommend retention of item. Only items that received a high priority score were retained (generally scores of ≥3). Finally, all of items were shuffled into a random order and five of the experts were asked to identify which domain they believed each item fell into (Everyday Memory, Everyday Language, etc.). Based on these ratings, an item was dropped if less than four of the five raters agreed on the domain in which it fell. The above process resulted in 74 items being retained for pilot testing, these included 15 items related to Everyday Memory, 10 items related to Everyday Language, 4 items related to Everyday Semantic Knowledge, 14 items related to Everyday Visuoperceptual skills, 13 items related to Everyday Planning, 9 items related to Everyday Organization, and 9 items related to Everyday Divided attention.
Item response options
A four-point response option was chosen to maximize the degree to which variability in impairment could be captured. We also wanted to minimize the influence of participant demographic variables, such as education, on test results. Therefore, informants completing the instrument were asked to compare a participant's current level of everyday functioning with how he or she functioned 10 years earlier. In this way, individuals serve as their own control, or reference point. Using this approach, someone who, for example, was always poor at following a map but has not experienced a change in this ability would be rated as showing no change. Response options included: 1 = better or no change compared to 10 years earlier, 2 = questionable/occasionally worse, 3 = consistently a little worse, 4 = consistently much worse. An “I don't know” response option is also included. This response format has been used with other instruments (i.e., Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE), (Jorm & Jacomb, 1989; Jorm & Korten, 1988; Jorm, Scott, Cullen, & Mackinnon, 1991) and has proven useful across different ethnic groups and minimizes effects of patient education on ratings (Del-Ser, Morales, Barguero, Canton, & Bermejo, 1997; S. T. Farias, Mungas, Reed, Haan, & Jagust, 2004; Morales, Bermejo, Romero, & Del-Ser, 1997).
Pilot testing and further item refinement
After the initial development phase the 74-item version of the ECog was administered to the informants/caregivers of 194 older adults consecutively seen at a University based Alzheimer's disease Research Center (ADRC). All participants had undergone a complete diagnostic dementia work-up through the ADRC. A total of 29 participants were cognitively normal, 53 had a diagnosis of MCI, and 112 were diagnosed with a dementia. The mean age of the sample was 76.5 (8.4) and the mean number of years of education was 14.0 (3.6), ranging from 2 to 22 years of formal education. Fifty-four percent of the sample was female. The majority of the participants were White (79%), 8% were Hispanic, 7% were African American, 2% were Asian, and 4% were of another racial group. With regard to demographic information of the informants who rated the participants' level of everyday functioning, 56% were spouses of the participant, 35% were their adult children, 5% were other family members, and 4% had other types of relationships to the participant. On average, informants spent 88.5 hours a week with the participants. The goal of this phase of development was to identify and discard items with obviously poor psychometric properties. Based on this pilot study, items were deleted if a high percentage of informants indicated that they could not adequately rate the item (as indicated by a high frequency of “I don”t know responses'). Generally, items for which 20% to 30% or more of the pilot sample responded in this way were deleted, as they were unlikely to be tasks commonly engaged in by older adults. Based on the initial pilot study, 39 of the original 74 items were retained. This 39-item version of the ECog was used in the current validation study.
Participants
Data for the main study was collected from 576 individuals who were evaluated at the ADRC. Participants are recruited to the ADRC through two routes: (1) clinic referrals and (2) community outreach. Clinic referral sources include community agencies and health care systems. Community recruitment supplements clinical recruitment to maximize demographic and cognitive diversity to better represent the demographic characteristics and range of cognitive function. The ECog was collected on essentially all individuals consecutively seen in the ADRC with the exception of those who did not have an informant (in most cases these were cognitively normal volunteers). The mean age of the entire sample was 76.7 (8.0) and the mean number of years of education was 13.8 (3.7), ranging from 0 to 22 years of formal education. Fifty-nine percent of the sample was female. The majority of the participants were White (60%), 12% were Hispanic, 14% were African American, 3% were Asian, and 11% were of another racial group or the information was not available. An individual familiar with the identified participant served as the informant and completed the ECog: 48% were spouses of the participant, 41% were their adult children (or spouses of their adult children), 5% were other family members, 5% were friends of the participant, and 1% had some other relationship. The average age of the informant was 61.8 (23.9); informants had a mean of 15.1 (4.0) years of education and 73% of them were female. On average, informants had known participants for 44.8 years and spent an average 75.2 hours a week with them.
All participants, regardless of recruitment source, had undergone a complete clinical diagnostic dementia work-up, which included a neurological evaluation, clinical neuropsychological testing, brain imaging, and appropriate lab work. Diagnostic decisions were made without knowledge of the results of the ECog. Participants received a clinical diagnosis of either normal cognition, MCI, or dementia based on an ADRC consensus diagnostic conference. Diagnoses were assigned based on the judgment of a neurologist (C.D.) and at least two neuropsychologists (S.T.F, D.M., B.R.), all of whom have expertise in the diagnosis of dementia and MCI. A diagnosis of dementia was based on DSM-IV criteria, which requires neuropsychological impairments in multiple cognitive domains in addition to significant functional disability in basic or instrumental activities of daily living. Although no strict psychometric cut-off scores were used to define cognitive impairment, cognitive impairment is clinically identified by ADC neuropsychologists when a participant's performance falls approximately 1.5 standard deviations below age-matched norms and in reference to their educational and socioeconomic background. Individuals with less severe cognitive changes not meeting the DMS-IV criteria for a dementia were diagnosed with MCI. Individuals with MCI could either have (1) a single memory impairment (amnestic MCI), (2) an impairment in one nonmemory domain (single non-memory MCI), or (3) subtle changes in multiple cognitive domains (multiple domain MCI). Persons with multiple neuropsychological impairments were diagnosed with MCI if reliable informants indicated that there was no significant functional impairment. Individuals with MCI could not have impairments in basic ADLs or be dependent on others in any instrumental ADLs. A diagnosis of MCI did not require subjective memory complaints. For the purposes of the clinical diagnosis, functional change was assessed using a variety of standardized instruments (e.g., Clinical Dementia Rating Scale) but was also based on clinical interviews with the patient and an informant, all of which were collected separately from, and without knowledge of the result of the ECog. ECog scores were not available to the clinicians.
A total of 174 participants were cognitively normal, 126 individuals had a diagnosis of MCI, and 276 were diagnosed with dementia. Table 1 presents demographic and cognitive information broken down by diagnostic group. Of those participants diagnosed with dementia, 208 (75%) had possible or probable Alzheimer's disease (AD), 20 (7%) had a mixed AD/vascular dementia, 13 (5%) had vascular dementia, 13 (5%) had possible or probable Dementia with Lewy Bodies, 9 (3%) had frontotemporal dementia, and the remaining 5% had other less common dementias. Of those individuals with a diagnosis of MCI, 58 (46%) individuals had amnestic MCI, 22 (18%) had a single nonmemory impairment, and 46 (37%) individuals had multiple domain MCI.
Table 1.
Participant Characteristics
| Normal | MCI | Dementia | |
|---|---|---|---|
| MMSE | 28.3 (1.8) | 25.9 (3.4) | 18.3 (6.7) |
| Age | 75.1 (7.3) | 77.1 (7.3) | 78.3 (8.1) |
| Gender (% female) | 64% | 49% | 60% |
| Education | 14.4 (3.2) | 14.2 (4.2) | 13.3 (3.8) |
| Ethnicity (% White) | 48% | 62% | 68% |
Instruments
Previously established measures of functional status
The Blessed Dementia Rating Scale (BDRS) (Blessed, Tomlinson, & Roth, 1988, 1968). The BDRS is a widely used instrument to measure functional activities. It consists of 22 items assessing functional activities including basic ADLs (e.g., eating, dressing, and toileting) and instrumental ADLs (e.g., housekeeping and money management). It also includes items assessing various behavioral problems. Patients are rated on each item based on an interview with an informant. Ratings range from 0 = normal, .5 = has some trouble, and 1 = unable to complete. The BDRS has been shown to correlate with postmortem biochemical and neuro-pathologic changes. It has also been shown to be sensitive to loss in function over time in individuals diagnosed with a dementia (Stern, Hesdorffer, Sano, & Mayeuz, 1990; Stern, Mayeuz, & Sano, 1987).
The Clinical Dementia Rating Scale (CDR) (Morris, 1993). The CDR is based on a structured caregiver interview. Scores are obtained in six different functional domains (memory, orientation, judgment and problem solving, community affairs, home and hobbies, and personal care). A variety of scores can be calculated but for the purposes of this study we used the “sum of boxes” score that is the arithmetic sum of the six subscores (Daly et al., 2000a). Neither instrument was used in any algorithmic way to determine clinical diagnosis and instrument scores could diverge from clinical diagnosis (e.g., patients with a CDR of 0.5 were not necessarily diagnosed as MCI.)
Measure of global cognitive function
Mini-Mental State Exam (MMSE) (Folstein, Folstein, & McHugh, 1975). This is a widely used instrument used to obtain an estimate of global cognitive function and screen for dementia. It consists of 30 items assessing orientation, attention/working memory, memory, language, and visuospatial skills. It has been shown to effectively discriminate old adults with dementia from those without dementia (Filley et al., 1989) and is sensitive to progressive deterioration in dementing patients (Morris et al., 1989; Teng, Chui, Schneider, & Metzger, 1987).
Procedure
The ECog was completed by an informant who accompanied the patient to a clinical appointment. At the end of the questionnaire informants answered several demographic questions about themselves (e.g., their age, education level, etc.). Instruments used to establish the validity of the ECog are routinely administered as part of the patient's clinical evaluation and were collected as part of the same clinical visit. They represent the standard instruments of everyday function that are currently available.
Data Analysis
Confirmatory factor analysis (CFA) was used to test whether the correlational structure of the ECog was consistent with our proposed multidimensional model. It was expected that items would be strongly intercorrelated such that a general, nonspecific dimension of everyday function would account for substantial variance in all items. However, it was also expected that domain-specific dimensions corresponding to the multidimensional conceptual model that were independent of the general everyday function dimension would be identified. A bifactor factor model (McDonald, 1999) was used to test the fit of the conceptual model underlying the development of the ECog to the observed correlation structure. This approach first used a single, primary general factor to account for intercorrelations among all items. It then added domain-specific factors to account for residual intercorrelation not explained by the general factor. Thus, the nonspecific and domain-specific factors were completely uncorrelated; the domain-specific factors accounted for unique variance not explained by the general nonspecific factor. The domain-specific factors were defined to evaluate different competing models for explaining the residual intercorrelation.
The Mplus application (Muthen & Muthen, 2004b) was used and ECog items were modeled as categorical indicators of the latent factors. This approach assumes that there is a latent continuous variable underlying each categorical variable, with the categories defined by threshold or cut-off values related to the underlying continuous variable. Latent continuous variables are assumed to have a multivariate normal distribution. Thresholds are estimated along with factor loadings, which like traditional loadings for continuous variables, relate the continuous variable underlying the categorical variables to latent factors. There is no single accepted criterion index to judge model fit so we report several goodness-of-fit indices identified by Hu and Bentler (Hu & Bentler, 1998) as recommended fit indices for continuous indicators and by Yu and colleagues (Yu, 2002) for categorical indicators. These indices included the comparative fit index (CFI) (Bentler, 1989, 1990), the root mean square error of approximation (RMSEA) (Cudek & Browne, 1983), and the Tucker-Lewis index (TLI) (Tucker & Lewis, 1973). The CFI and the TLI measure the fit of the model relative to the null model. The CFI incorporates a correction for model complexity, and the TLI takes degrees of freedom into account. The RMSEA takes model parsimony into account, which is important because goodness-of-fit values can sometimes be artificially inflated as the number of parameters in the model is increased. Guidelines for interpretation of these indices are similar for analyses involving continuous and categorical indicators. The TLI and CFI range from 0 (poor fit) to 1 (perfect fit); values of .95 or higher are indicative of a good model fit. RMSEA values lower than .08 are considered to reflect adequate fit, values less than .05 to .06 indicate good fit. Model fit was also evaluated by examining residual intercorrelations among items. As a general rule residual intercorrelations less than .10 are considered to indicate good fit (McDonald, 1999). A mean and variance adjusted weighted least squares estimator (WLSMV; Muthen & Muthen, 2004a, 2006) was used for all analyses.
Model estimation proceeded as follows. Thresholds were freely estimated in all models. First, a one-dimensional model was evaluated. Loadings of all items on a single, common, primary dimension were freely estimated with the variance of the latent dimension constrained to unity. Then, a series of models tested relative ability of different secondary factor structures to account for residual intercorrelation of items. For each model, secondary factors were constrained to be uncorrelated with the primary general factor and to have variances of 1.0, but intercorrelations of secondary, domain-specific factors were freely estimated. Competing models were as follows: (1) two dimensions corresponding to memory and nonmemory items; (2) four dimensions with Everyday Memory, Language/Semantic Knowledge, Visual spatial abilities, and Executive Functions (Planning, Organization, Divided Attention); (3) five dimensions with Everyday Memory, Language, Semantic Knowledge, Visual Spatial Functions, and Executive Functions; (4) six dimensions with Memory, Language/Semantic Knowledge, Visual Spatial, Planning, Organization, and Divided Attention; and (5) seven dimensions with Memory, Language, Semantic Knowledge, Visual Spatial, Planning, Organization, Divided Attention. The initial single dimension model was nested within each of the subsequent models since it essentially constrains domain-specific factor loading to zero. Improvement of model fit associated with freely estimating domain-specific factors was evaluated with a modification of the chi-square difference test appropriate for the WLSMV estimator used in these analyses (Muthen & Muthen, 2004a, 2006). Competing secondary factor models were not nested, but relative fit was evaluated using fit indices and residual correlations.
Factor scores were generated from the model that was chosen as providing the best fit, and these factor scores were then used as variables in subsequent analyses to evaluate the relationship of the ECog dimensions with external variables including: (1) demographic variables, (2) clinical validation measures of global cognition and existing measures of independent function, (3) clinical syndrome diagnosis, and (4) MCI subtype.
Simple bivariate correlation coefficients were used to characterize the strength of association of ECog factors with demographic variables and clinical validation measures and to assess short-term test–retest reliability. A multivariate analysis of variance (MANOVA) was used to evaluate the relationship of clinical syndrome diagnosis with ECog factors, and MCI subtype with ECog factors. These analyses included the ECog factor scores as multiple dependent variables and the diagnosis groups as independent variables. Age and education were included as covariates. The diagnosis by ECog factors interaction was of primary interest. A significant multivariate test for this effect indicated that diagnosis effects differed across ECog factors, and was followed by univariate analyses of variance to clarify the pattern of significant results across factors. Bonferroni correction using a p value of .007 (.05/7) was used to adjust for the multiple analyses. Significant effects in the univariate analyses involving diagnosis were further evaluated using pairwise comparisons of Normal with MCI and MCI with Demented. A Bonferroni corrected p value of .0035 (.05/7/2) was used for these comparisons. Finally, diagnosis effect size estimates were derived from the univariate analyses; the R2 value for a model that included only age and education was subtracted from the R2 value from a model with age, education, and diagnosis. In addition, effect sizes for pairwise comparisons were calculated by subtracting one mean from the other and dividing by the pooled standard deviation for all diagnostic groups involved in the analysis of variance (d = M1 − M2/SDpooled).
An additional group of analyses examined the ability of ECog factors to discriminate clinical syndrome diagnoses. Multinomial logistic regression was used in which diagnosis was the dependent variable and ECog factors were independent variables. MCI was coded as the reference group, so these analyses examined the ability to discriminate Normal from MCI and MCI from Demented. Age and education were included as covariates in these analyses. Separate analyses were first performed adding each ECog factor to age and education as independent variables. A final model entered ECog factors jointly. In addition, based on this analysis we calculated sensitivity and specificity estimates for discriminating groups using the ECog total score.
Results
Factor Structure
Table 2 presents the fit indices for the various models that were evaluated. The one-factor model yielded a significant chi-square statistic, as did all of the subsequently tested models, indicating a less than perfect fit. However, the chi-square statistic is highly sensitive to sample size and may overstate the lack of fit of a model (Bollen, 1989), and for this reason, the model fit was primarily evaluated using fit indices and residual correlations. For the one-factor model, TLI indicated good fit but CFI and RMSEA indicated poor fit. Approximately 14% of the residual interitem correlations exceeded a value of 0.10. We next examined various models that included a general, nonspecific factor and domain-specific factors that were uncorrelated with the general factor. All of these models provided a significantly better fit than the one factor model, as determined by the modified chi-square difference test (ps < .0001). The best fit was obtained with the model that included a primary global factor and seven domain-specific factors (8-Factor model), but the fit for the model with six domain-specific factors was about the same (7-Factor model). All fit indices for these two models showed adequate to good fit, and for both models, there were no residual correlations that exceeded .10 and only 3% of residual correlations exceeded .05. In the 8-Factor model the correlation between the Language and Semantic Knowledge factors was 0.89 suggesting that in fact these two factors were not very distinct from one another. This high interfactor correlation was in contrast to the rather modest correlations between the other factors (see Table 3). Consequently, the seven factor solution (one global factor, six domain-specific factors) was selected as the best fitting model for subsequent analyses. Figure 1 presents a diagrammatic representation of the final model.
Table 2.
Relative Fit Indices for Each of the Models Tested
| Model | χ2 (DF) | CFI (>.95) | TLI (>.95) | RMSEA (<.O8) |
|---|---|---|---|---|
| 1 Factor Model (glob) | 1273.1 ( 69) | .931 | .989 | .172 |
| 3 Factor Model (glob, mem, nonmem) | 891.5 (105) | .955 | .995 | .113 |
| 5 Factor Model (glob, mem, lang/sem, vsp, exec) | 606.5 (133) | .973 | .998 | .078 |
| 6 Factor Model (glob, mem, lang, sem, vsp, exec) | 596.7 (133) | .973 | .998 | .077 |
| 7 Factor Model (glob, mem, lang/sem, vsp, plan, org, div att) | 460.2 (139) | .982 | .999 | .063 |
| 8 Factor Model (glob, mem, lang, sem, vsp, plan, org, div att) | 452.1 (139) | .982 | .999 | .062 |
Notes. glob = global; mem = memory; nonmem = non-memory; lang = language; sem = semantic knowledge; vsp = visual spatial; exec = executive; plan = planning; org = organization; div att = divided attention; CFI = comparative fit index; RMSEA = root mean square error of approximation; TLI = Tucker-Lewis Index. The TLI and CFI range from 0 (poor fit) to 1 (perfect fit); values of .95 or higher are indicative of a good model fit. RMSEA values lower than .08 are considered to reflect adequate fit, values less than .05 to .06 indicate good fit.
Table 3.
Factor Loadings for 7-Factor Model
| Factor |
|||||||
|---|---|---|---|---|---|---|---|
| Glob | Mem | Lang | VSp | Plan | Org | Div Att | |
| Remembering a few shopping items without a list. | 0.89 | 0.26 | |||||
| Remembering things that happened recently (such as recent outings, events in the news). | 0.83 | 0.45 | |||||
| Recalling conversations a few days later. | 0.83 | 0.47 | |||||
| Remembering where she/he has placed objects. | 0.87 | 0.21 | |||||
| Repeating stories and/or questions. | 0.82 | 0.47 | |||||
| Remembering the current date or day of the week. | 0.90 | 0.23 | |||||
| Remembering he/she has already told someone something. | 0.83 | 0.41 | |||||
| Remembering appointments, meetings, or engagements. | 0.90 | 0.17 | |||||
| Verbally giving instructions to others. | 0.73 | 0.55 | |||||
| Following a story in a book. | 0.78 | 0.45 | |||||
| Understanding the point of what other people are trying to say. | 0.72 | 0.55 | |||||
| Describing a program he/she has watched on TV. | 0.81 | 0.45 | |||||
| Understanding spoken directions or instructions. | 0.75 | 0.44 | |||||
| Forgetting the names of objects | 0.63 | 0.63 | |||||
| Finding the right words to use in a conversation. | 0.55 | 0.71 | |||||
| Remembering the meaning of common words. | 0.68 | 0.62 | |||||
| Communicating thoughts in a conversation. | 0.65 | 0.67 | |||||
| Following a map to find a new location. | 0.82 | 0.56 | |||||
| Reading a map and helping with directions when someone else is driving. | 0.84 | 0.51 | |||||
| Finding his/her car in a parking lot. | 0.91 | 0.25 | |||||
| Finding the way back to a meeting spot in the shopping mall or other location. | 0.94 | 0.23 | |||||
| Finding his/her way around a familiar neighborhood. | .89 | 0.35 | |||||
| Finding his/her way around a familiar store. | .90 | 0.37 | |||||
| Finding his/her way around a house visited many times. | .89 | 0.33 | |||||
| Planning the sequence of stops on a shopping trip. | .95 | 0.20 | |||||
| The ability to anticipate weather changes and plan accordingly. | .86 | 0.27 | |||||
| Developing a schedule in advance of anticipated events. | .91 | 0.29 | |||||
| Thinking ahead. | .80 | 0.58 | |||||
| Thinking things through before acting. | .87 | 0.42 | |||||
| Keeping living and work space organized. | .74 | 0.46 | |||||
| Balancing the checkbook without error. | .91 | 0.35 | |||||
| Keeping financial records organized. | .91 | 0.38 | |||||
| Prioritizing tasks by importance. | .90 | 0.36 | |||||
| Using an organized strategy to manage a medication schedule. | .91 | 0.23 | |||||
| Keeping mail and papers organized. | .85 | 0.38 | |||||
| The ability to do two things at once. | .85 | 0.42 | |||||
| Returning to a task after being interrupted. | .88 | 0.37 | |||||
| The ability to concentrate on a task without being distracted by external things in the environment. | .84 | 0.42 | |||||
| Cooking or working and talking at the same time. | .85 | 0.44 | |||||
Note. All factor loadings are statistically significant (p < .05). Glob = global; Mem = memory; Lang = language; VSp = visual spatial; Plan = planning; Org = organization; Div Att = divided attention.
Figure 1.
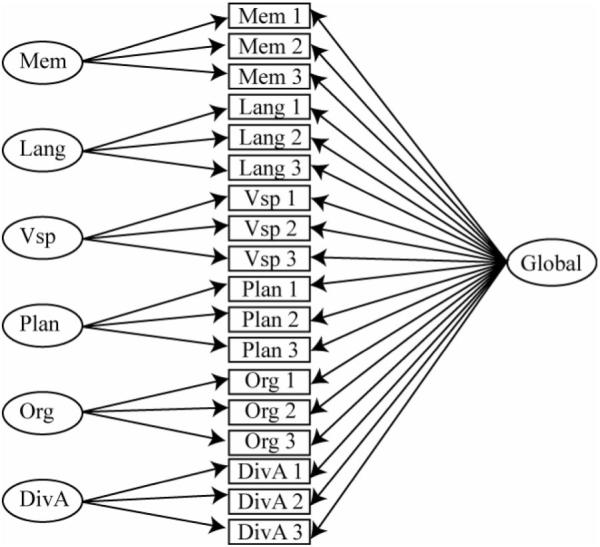
Seven Factor Model containing one global factor and six domain-specific factors.
Table 3 shows standardized factor loadings for the model that included the general factor plus the six domain-specific factors (7-factor model). Standardized loadings of individual items on the general, nonspecific factor ranged from 0.55 to 0.95 (average = 0.83), and therefore accounted for substantial variance in all items (30–90%). The Everyday Memory factor had four items (out of eight) with standardized loadings that exceeded .30, a generally accepted threshold for a salient loading (McDonald, 1999). All nine Everyday Language/Semantic Knowledge items had loadings that exceeded .30 (average = .57), and in general, the nonspecific factor explained the least variance in these items. Five of six Everyday Visual Spatial items had loadings >.30, as did two of five Planning items, five of six Organization items, and all four Divided Attention items. Table 4 shows intercorrelations of the six domain-specific factors. After accounting for the general, nonspecific factor at the individual item level, there was only modest intercorrelation of domain-specific factors. As would be expected, the three everyday executive subdomains (Planning, Organization, Divided Attention) had relatively strong intercorrelations. The Everyday Memory factor had relatively weak correlations with the nonmemory factors.
Table 4.
Correlations Among the Six Domain-Specific Factors
| Mem | Lang | VSp | Plan | Org | |
|---|---|---|---|---|---|
| Everyday Memory | — | ||||
| Everyday Language | 0.34 | — | |||
| Everyday Visuospatial | 0.22 | 0.49 | — | ||
| Everyday Planning | 0.35 | 0.60 | 0.42 | — | |
| Everyday Organization | 0.21 | 0.43 | 0.27 | 0.66 | — |
| Everyday Divided Attention | 0.38 | 0.55 | 0.35 | 0.64 | 0.58 |
Note. All correlations are statistically significant (p < .05). Mem = memory; Lang = language; VSp = visual spatial; Plan = planning; Org = organization.
Relationship to Demographic Variables and Test–Retest Reliability
Table 5 presents the correlations between the ECog scales and participants' age and years of education. Age and education had weak relationships with the ECog nonspecific factor, each accounting for less than 4% of the variance. Age and education had negligible associations with the domain-specific ECog factors, indicating that these demographic variables do not differentially influence more specific domains of everyday function.
Table 5.
Correlations Between the ECog Scales, Demographic Variables, Global Cognitive Function, Established Measures of Everyday Function, and Clinical Diagnosis. Higher ECog Score Indicates Worse Daily Function
| Age | Education | MMSE | CDR | BDRS | Clinical diagnosis* | |
|---|---|---|---|---|---|---|
| Everyday Global Function | .19 | −.16 | −.67 | .74 | .74 | .72 |
| Everyday Memory | −.06NS | .04NS | −.14 | .22 | .15 | .23 |
| Everyday Language/Semantic | −.06NS | −.08 | −.23 | .18 | .23 | .16 |
| Everyday Visuospatial | −.01NS | −.12 | −.08 | .01NS | .14 | .07NS |
| Everyday Planning | −.01NS | −.05NS | −.18 | .15 | .20 | .11 |
| Everyday Organization | −.02NS | −.01NS | −.12 | .14 | .18 | .09NS |
| Everyday Divided Attention | −.02NS | −.01NS | −.17 | .19 | .25 | .12 |
Notes.
Multiple correlation coefficient from regression of ECog factor on clinical syndrome diagnosis.
NS = Not statistically significant.
A subsample of 27 informants completed two separate ECogs on research participants within a maximum of a 4 month time window to assess test–retest reliability (average time between assessments = 29 days, range = 2 to 113 days). The correlation between the first and second ECog indicated good reliability (r = .82, p < .0001).
Relationship to Other Measures of Everyday Function and Global Cognition (Convergent Validity)
Convergent validity of the ECog was assessed by comparing it to the results of other previously validated global measures of everyday function (BDRS and CDR) and cognition variables. Table 5 presents the correlations between the ECog and existing measures of daily function. These measures were strongly correlated the ECog general factor and were weakly correlated (with one exception) with domain-specific factors.
As also shown in Table 5, the MMSE was moderate to strongly correlated with the ECog global factor, and more weakly correlated with the other domain specific factors. Using an ECog total raw score, the shared variance between the ECog and the MMSE was 53% (p < .0001). Such findings suggest that the ECog correlates with actual impairment as measured by cognitive testing.
Relationship to Clinical Diagnosis (External Validity)
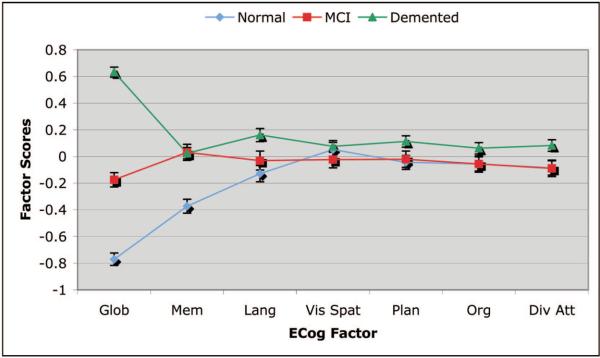
Next, to assess external validity we examined the relationship of the three diagnostic groups (Normal, MCI, Demented) with all seven ECog factors. Figure 2 presents box plots of each ECog domain, showing the median score, and upper and lower quartiles for each clinical group. Across all of the ECog domains and the total score, a consistent stepwise pattern is observed where the normals show the least problems in everyday function, the MCI group is intermediate, and the demented group shows the highest level of impairment. The figure also demonstrates that each ECog domain and the total score show considerable variability within both the demented and MCI groups suggesting that the instrument is sensitive to interindividual differences within these groups. Everyday Memory as well as Everyday Divided Attention, in particular, also shows considerable variability within the cognitively normal group, suggesting that these domains are also sensitive to the effects of normal aging. Figure 3 presents the mean factor scores (error bars represent the standard error of the mean) for each diagnostic group across the ECog factors (higher factor scores are associated with a greater degree of impairment). The diagnosis main effect was significant, F(2, 562) = 35.0, p < .0001 as was the diagnosis by factor interaction (approximate F(12, 1118) = 24.1, p < .0001). In univariate analyses, the diagnosis effect was significant for the general, nonspecific factor (diagnosis accounted for 47.3% of the variance independent of age and education). The diagnosis effect was also significant for the Everyday Memory (6.5%) and Everyday Language (2.4%) factors. Post hoc pairwise comparisons of Normal with MCI, MCI with Demented, and Demented with Normal were highly significant for the general factor (ps < .0001, d = −0.98, −1.32, and −2.30, respectively). The Normal versus MCI comparison was also significant for the Everyday Memory factor (p < .0001, d = −0.58). The MCI with Demented comparison for the Everyday Language factor approached significance (p = .03, d = −0.24), but was not significant after Bonferroni correction.
Figure 2.
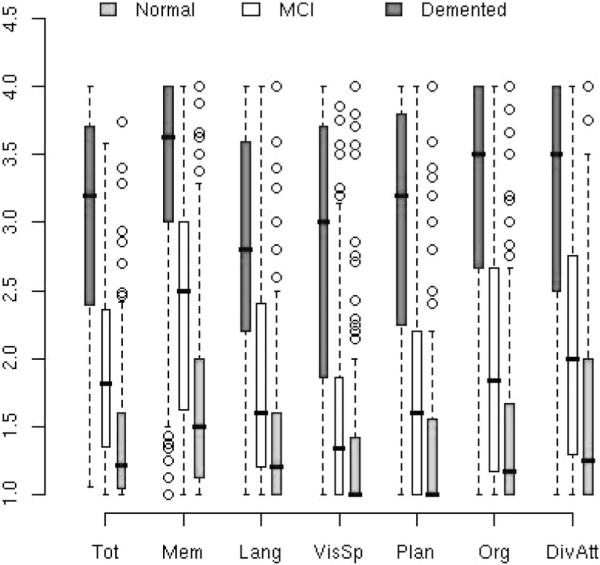
Box and Whisker plots of ECog total and subscale median scores across diagnostic groups.
Figure 3.
ECog factors scores for each of the three diagnostic groups (Normal, MCI and Demented).
Next we sought to more directly test whether the ECog factors could accurately discriminate between clinical groups. The general, nonspecific factor significantly discriminated Normal from MCI (χ2[1] = 52.9, p < .0001) and MCI from Demented (χ2[1] = 80.1, p < .0001), independent of effects of age and education. Everyday Memory discriminated Normal from MCI (χ2[1] = 23.6, p < .0001), Everyday Language discriminated MCI from Demented (χ2[1] = 4.8, p < .03), and Everyday Divided attention discriminated MCI from Demented (χ2[1] = 5.0, p < .03). When these four variables were entered jointly as independent variables along with age and education, the general, nonspecific factor independently discriminated Normal from MCI (χ2[1] = 48.8, p < .0001) and MCI from Demented (χ2[1] = 80.7, p < .0001), Everyday Memory independently discriminated Normal from MCI (χ2[1] = 16.0, p < .0001), and Everyday Language discriminated MCI from Demented (χ2[1] = 6.0, p < .01). These results show that the general factor strongly discriminates diagnostic groups, and the Everyday Memory subscale adds incremental discrimination of Normal from MCI, and the Everyday Language subscale adds to discrimination of MCI and Demented. We also calculated estimates of sensitivity and specificity in association with the ability of the ECog total score to discriminate clinical groups. At a specificity value of .80, the ECog total was associated with a sensitivity of .93 in discriminating dementia from normal, a sensitivity of .75 in discriminating MCI from dementia, and a sensitivity of .67 in discriminating MCI from Normals.
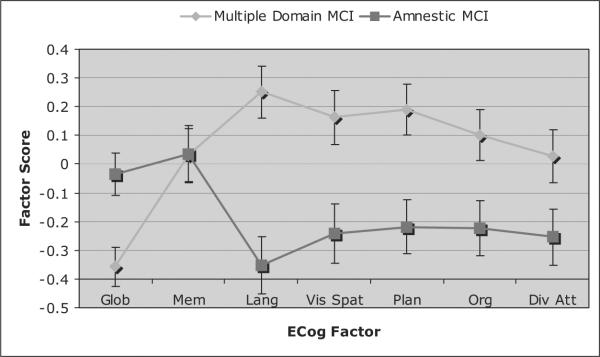
Relationship to MCI Subtype (External Validity)
We examined the relationship of the seven ECog factors with MCI subtype (Amnestic MCI vs. Multiple Domain MCI). Results are show in Figure 4 (again, higher factor scores are associated with a greater degree of impairment). The diagnosis main effect was significant, F(1, 121) = 10.1, p < .002 as was the diagnosis by factor interaction (approximate F(6, 116) = 4.8, p < .0003). In univariate analyses, the diagnosis effect was significant for all variables except for Everyday Memory (p > .47), although the Divided Attention (p < .054) and Organization factors (p = .027) did not reach statistical significance after a Bonferroni correction (effect sizes for the significant comparisons ranged from d = 0.52 to 0.79). That is, the two MCI groups had distinguishable profiles across the ECog scales. The multiple domain MCI group showed greater impairment on most of the domain-specific factors other than Everyday Memory. Conversely, the amnestic MCI group showed a higher degree of impairment on the global, nonspecific factor, but showed lower degrees of impairment on the non-memory domain-specific factors (that are independent of the general factor). This indicates that the amnestic MCI group was more impaired overall, but after controlling for overall impairment, was less impaired in nonmemory domains. Incremental variance explained by diagnosis after accounting for age and education was: Language − 12.7%, Visual Spatial − 6.1%, Planning − 6.3%, Organization − 7.3%, Global − 6.1%.
Figure 4.
ECog factors scores in Amnestic MCI versus Multiple Domain MCI.
Discussion
The ECog was designed to be a multidimensional, psychometrically sound measure of everyday function in older adults. The guiding hypothesis was that daily tasks vary in the degree to which they require specific cognitive abilities. Accordingly, the ECog was designed to measure everyday function in multiple domains, each domain defined by the underlying cognitive abilities thought to be most critical to that group of daily activities. The instrument is intended to have both research and clinical utility. From a research perspective, an instrument with good psychometric properties has obvious advantages for detecting between both group differences as well as longitudinal change, and its multidimensional structure permits a more detailed investigation of the determinants and course of functional impairment. Measuring multiple domains of everyday function has potential for helping in diagnostic differentiation and for improved understanding of the limits, care needs, and interventions appropriate to individuals.
Although we hypothesized that everyday function is a multidimensional construct, it was also anticipated that the different functional domains would be inherently intercorrelated so that all domains would be influenced by, or represented in, a nonspecific factor. It has been a long held belief that intellectual or cognitive abilities can be represented, in part, by a general, nonspecific factor (the `g' factor), but that there is also remaining variance that can be parceled into more specific domains. Traditional approaches to neuropsychological assessment have generally used measures that include both nonspecific and domain-specific components of variation. While acknowledging the intercorrelations between these domains, this approach generally does not explicitly utilize models to separate specific and nonspecific contributions to the test scores. We used an alternate strategy in this study (bifactor model), that is, we explicitly and independently modeled domain specific and nonspecific contributions to everyday function. This approach is particularly relevant to examining the utility of forming subscales (Reise, Morizot, & Hays, 2007) and has been used to investigate the psychometric properties of other instruments (Chen, West, & Sousa, 2006; Patrick, Hicks, Nichol, & Krueger, 2007; Reise et al., 2007; Stockdale, Gridley, Ware Balogh, & Holtgraves, 2002).
Thus, confirmatory factor analysis, using a bifactor approach was used to examine the latent factor structure of the ECog to determine if there was support for our hypothesized multifactorial model. We first examined the fit of a simple one-factor model, which represented everyday function as a unitary construct, and this model did not adequately fit the data. As such, we then evaluated a variety of different multidimensional models. Subsequent models included a general, nonspecific factor, along with various domain-specific factors that were uncorrelated with the general factor. In this way, the domain-specific factors account for unique variance not explained by the general factor.
All of the multifactorial models fit the data better than the one-factor model, supporting the notion that everyday function should be thought of as a multidimensional construct. In the simplest multifactorial model, which included an everyday memory and a nonmemory factor (in addition to the global factor), one of the fit indices (RMSEA) still suggested an inadequate fit. Expanding the model to include domain-specific factors associated with Everyday Memory, Language, Visuospatial, and Executive function improved the fit indices such that they were all within acceptable ranges. Further dividing the Everyday Executive factor into Planning, Organization and Divided Attention further improved model fit. However, we did not see a similar pattern of improved fit when separating Everyday Language and Everyday Semantic Knowledge into separate factors (the fit of the seven and eight factor models was almost identical). In addition, these two factors, unlike the others were highly correlated. Based on these results we chose to retain the model represented by one general factor and six domain-specific factors (Everyday Memory, Everyday Language, Everyday Visuospatial Function, Everyday Planning, Everyday Organization, and Everyday Divided attention). Thus, the final model we used was a modified version of our a priori model in that we collapsed the Language and Semantic Knowledge factors.
To provide support of convergent validity the relationships between the ECog and traditional measures of everyday function were evaluated. As expected, there was a strong relationship between the ECog general factor and the two established measures of global functional status (the CDR and BRDS). However, the domain-specific factors of the ECog were correlated much more modestly with these existing instruments. Thus, as expected, nonspecific functional impairment accounts for most of the correlation with these global measures; the domain specific ECog components are not strongly correlated with the external measures independent of the nonspecific ECog component. Such findings suggest that the domain-specific factors are measuring something not captured by these traditional instruments.
Next, we examined whether there were clinical group differences on each of the ECog factors. We focused on three groups of older adults: those who are cognitively normal, those with MCI, and individuals with a clinical diagnosis of dementia. Results showed large group differences on the general factor of the ECog. This indicates that there are significant differences in the overall levels of everyday function across these clinical groups, with the normal person showing the least degree of change relative to their baseline, the MCI group showing an intermediate level of functional impairment, and the demented group showing the greatest degree of functional impairment. This was so even though MCI had been diagnosed using standard criteria that excluded cases with clinically significant functional impairment. Thus, this is an important finding in that there are few existing instruments to assess everyday function that are sensitive to the relatively subtle changes that occur in the transition from normal function to MCI and dementia.
When all of the factor scores were entered together into a discriminant function analysis, again the general factor discriminated all three of the groups; however, other specific domains added incremental discriminative power. Specifically, Everyday Memory added to the discrimination of Normal from MCI, whereas Everyday Language helped discriminate dementia from MCI. Such findings provide evidence of incremental validity of both Everyday Memory and Everyday Language. These findings are conceptually consistent with the progression of pathology and neuropsychological impairment that occurs with Alzheimer's disease. That is, the syndrome of MCI in our sample (and in the literature) is most often associated with memory impairment, which is in keeping with the notion that early memory decline is a harbinger of AD secondary to the early involvement of the medial temporal lobe structures. As the disease progresses to include greater cortical involvement, other neuropsychological domains become involved. For example, it is well known that AD pathology typically progresses from the hippocampus to involve temporal lobe cortical regions quite early in the course of the disease (Braak & Braak, 1991), resulting in early language changes. Thus, the fact that functional changes associated with memory discriminate MCI from normal older adults, and language-related functional changes discriminate dementia from MCI is consistent with the pathological and neuropsychological progression of early AD. The fact that other domain-specific factors did not add discriminative power may reflect the fact that our dementia group was rather mildly impaired.
The syndrome of MCI is known to be heterogeneous; therefore, we further examined whether different subtypes of MCI showed different ECog factor profiles. For these analyses, because of the sample sizes, we examined the difference between two groups, amnestic MCI and multiple domain MCI. The amnestic MCI group had predominant memory impairment, whereas the multiple domain MCI group was comprised of individuals who typically had mild neuropsychological impairments on measures of memory and at least one other neuropsychological domain. We found that while the amnestic MCI and the multiple domain MCI groups did not differ in terms of Everyday Memory, the multiple domain MCI group showed greater functional impairment in most of the non-memory functional domains including Everyday Language, Everyday Visuoperception, and Everyday Planning (with statistical trends indicating more impairment in Everyday Organization and Divided Attention). Such findings support the association between impairment in neuropsychological domains and impairment in domain-specific functional domains. Interestingly, the amnestic MCI group showed more impairment on the general, nonspecific factor of the ECog than the multiple domain MCI group. This may seem counterintuitive, but it is important to remember that the domain-specific ECog factors are independent of the general factor. It suggests that the multidomain cases had milder, but more diffuse impairment.
Further evidence of the domain-specificity of these scales might also be obtained by comparing the ECog profiles of various diagnostic groups known to have different cognitive profiles. For example, we hypothesize that although the general, nonspecific functional factor may show similar degrees of impairment across different dementia types who are at similar disease stages, there will be domain-specific differences such that AD is associated with prominent Everyday Memory impairments, frontotemporal dementia is associated with prominent impairments in everyday executive domains such as Everyday Planning, and syndromes such as Primary Progressive Aphasia or Semantic Dementia will be associated with a prominent Everyday Language impairment. Thus, it is possible that the pattern of functional impairment, like the pattern of neuropsychological impairment, will aid in differential diagnosis of these disorders. Our current sample included only small numbers of non-AD dementia types and therefore precluded this type of analysis but this is an area of ongoing investigation at our Center.
Although we hypothesize that to at least some extent the specific everyday cognitive domains will relate to their neuropsychological counterparts, this remains an important empirical question that we are also pursuing. It is likely that there will be complex relationships between neuropsychological functions and everyday cognition. For example, we suspect that there are a variety of different scenarios in which different neuropsychological impairment(s) could lead to similar functional deficits. For example, it may be that neuropsychological deficits in memory lead to problems in Everyday Memory but that deficits in executive functions can also lead to similar changes in Everyday Memory (although in the later case functional changes may also occur across a wider range of functional domains). Importantly this instrument will serve as a tool to systematically collect information on how a person is functioning in different cognitive domains of everyday function, and to test theoretically driven hypotheses about how specific neuropsychological impairments affect specific areas of everyday function.
All of the ECog scales had very low correlations with participants' level of education. This is in contrast to the typically strong association between neuropsychological test scores and education, suggesting that particularly for individuals with very low or very high levels of education, assessment of everyday function using the ECog may represent an indicator of an incipient dementia that is less confounded than cognitive testing by education and related demographic characteristics. In designing the response options for the questionnaire items, we specifically chose to obtain ratings of a person's current level of functioning compared to their own baseline because we wanted to measure new or acquired functional changes, rather than preexisting or lifelong difficulties. This type of response option has been used successfully with other informant-based measures of cognitive and functional change (i.e., IQCODE) and has shown similar low relationships with demographic variables (Del-Ser et al., 1997; Farias et al., 2004; Morales et al., 1997).
We explicitly modeled nonspecific and domain-specific dimensions of independent function in this study. This has conceptual and methodological advantages in that it separates these sources of variation, but has a relative practical disadvantage in terms of the complexity of calculating factor scores. This is because item loadings are weighted so that the general factor is uncorrelated with specific factors, and as a result, computer scoring is required for practical applications. A different approach would use correlated factors defined by the items contributing to the domain-specific factors in this study. This approach would not include a general factor, and nonspecific variance would be included in the factor scores for the specific domains. This second approach is more commonly used in neuropsychology, where scores from different domains are known to be correlated, and domain-specific effects are inferred from relative peaks and valleys across profiles. An advantage of the second approach is that use of a simple summary score for each ECog domain (by summing items and dividing by the number of items completed) would yield domain scores that would closely approximate scores from a confirmatory factor analysis, and thus this approach can be implemented in applied settings without computer scoring. These two approaches are closely related conceptually; factors in the second approach essentially correspond to each domain-specific factor from the first approach being added to the general factor. We have used the second approach in a previous publication (Farias et al., 2006). Ultimately, either approach could be used depending on the specific needs and resources.
There are likely other important dimensions of everyday function, not included in the ECog. To this end, the ECog is not exhaustive in terms of its assessment of all possible important domains. For example, social judgment and self regulation behaviors are not explicitly measured. However, there are a number of other informant-based ratings scales that assess these frontally mediated behavioral syndromes (i.e., FrSBe; Grace et al., 1999).
There are limitations to relying on the reports of informants because they can be subject to the effects of systematic bias. For example, informant characteristics such as mood or degree of caregiver burden (Jorm et al., 1994; Teri, 1997) can affect ratings. Informant report has, however, been shown to reliably differentiate demented from nondemented individuals and such information can be useful in predicting who will go on to develop further changes (Daly et al., 2000b; Monnot, Brosey, & Ross, 2005). These previous findings, along with some of the results in this paper, provide evidence that informants can reliably judge the functional and cognitive abilities of patients. Informants may not be as accurate in rating the everyday cognitive abilities of individuals with only mild changes, and thus there may be a threshold level of functional change that informants can accurately observed. However, the present study demonstrates that informant ratings of individuals with only mild cognitive impairment but not demented, differ both from the informant ratings of cognitively normal elders and those with dementia.
In summary, the present data indicate that the ECog is a promising instrument for the measurement of daily function in older adults. One of the major advantages of the ECog is that it was derived from an explicit rational model. The factor analytic work reported here lends strong support to the idea that it measures both a general, nonspecific factor underlying everyday function, as well as six domain-specific factors, an important advantage over other instrument. It is sensitive to differences in levels of functional impairment across clinical groups and is also able to capture domain-specific differences in patterns of functional impairment in different clinical groups (e.g., amnestic vs. multiple domain MCI). The assessment of everyday function is an important part of clinical neuropsychological evaluations, and a critical outcome in a wide variety of neurological insults. Although there are a plethora of neuropsychological instruments to test a wide range of cognitive functions, there are a limited number of instruments available to systematically assess everyday functions. The ECog will provide a means of studying the determinants and course of change in more specific domains of daily function than has been previously possible. By measuring everyday function in more meaningful ways, neuropsychologists can make important contributions to understanding and predicting daily function and so improve patient care.
Acknowledgments
This work was supported by Grants AG021511 from the National Institute on Aging, Bethesda, MD and the California Department of Health Services.
References
- Bentler PM. Eqs Structural Equations program manual. BMDP Statistical Software; Los Angeles: 1989. [Google Scholar]
- Bentler PM. Comparative fit indices in structural models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Blessed GT, Tomlinson BE, Roth BE. Blessed-Roth Dementia Scale. Psychopharmacology Bulletin. 1988;24:705–708. [PubMed] [Google Scholar]
- Blessed GT, Tomlinson BE, Roth M. The association between quantitative measures of dementia and of senile change in the cerebral grey matter of elderly subjects. British Journal of Psychiatry. 1968;114:797–811. doi: 10.1192/bjp.114.512.797. [DOI] [PubMed] [Google Scholar]
- Bollen KA. Structural equations with latent variables. Wiley; New York: 1989. [Google Scholar]
- Braak H, Braak E. Neuropathological staging of Alzheimer-related changes. Acta Neuropathologica. 1991;82:239–259. doi: 10.1007/BF00308809. [DOI] [PubMed] [Google Scholar]
- Chen FF, West SG, Sousa KH. A comparison of bifactor and second-order models of quality of life. Multivariate Behavioral Research. 2006;41:189–225. doi: 10.1207/s15327906mbr4102_5. [DOI] [PubMed] [Google Scholar]
- Cudek R, Browne MW. Cross-validation of covariance structures. Multivariate Behavioral Research. 1983;18:147–167. doi: 10.1207/s15327906mbr1802_2. [DOI] [PubMed] [Google Scholar]
- Daly E, Zaitchik D, Copeland M, Schmahmann J, Gunther J, Albert M. Predicting conversion to Alzheimer disease using standardized clinical information. Archives of Neurology. 2000a;57:675–680. doi: 10.1001/archneur.57.5.675. [DOI] [PubMed] [Google Scholar]
- Daly E, Zaitchik D, Copeland M, Schmahmann J, Gunther J, Albert M. Predicting conversion to Alzheimer's disease using standardized clinical information. Archives of Neurology. 2000b;57:675–680. doi: 10.1001/archneur.57.5.675. [DOI] [PubMed] [Google Scholar]
- DeBettignies BH, Mahurin RK, Pirozzolo FJ. Insight for impairment in independent living skills in Alzheimer's disease and multi-infarct dementia. Journal of Clinical and Experimental Neuropsychology. 1990;12:355–363. doi: 10.1080/01688639008400980. [DOI] [PubMed] [Google Scholar]
- Del-Ser T, Morales JM, Barguero MS, Canton R, Bermejo F. Application of the Spanish version of the “Informant Questionnaire on Cognitive Decline in the Elderly” in the clinical assessment of dementia. Alzheimer Disease and Associated Disorders. 1997;11:3–8. doi: 10.1097/00002093-199703000-00002. [DOI] [PubMed] [Google Scholar]
- Ernst RL, Hay JW. Economic research on Alzheimer's Disease: A review of the literature. Alzheimer's Disease and Associated Disorders. 1997;11:135–145. [PubMed] [Google Scholar]
- Farias ST, Mungas D, Reed BR, Haan MN, Jagust WJ. Everyday functioning in relation to cognitive functioning and neuroimaging in community-dwelling Hispanic and non-Hispanic older adults. Journal of the International Neuropsychological Society. 2004;10:342–354. doi: 10.1017/S1355617704103020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Farias ST, Mungas D, Reed BR, Harvey D, Cahn-Weiner D, DeCarli C. MCI is associated with deficits in everyday functioning. Alzheimer Disease and Associated Disorders. 2006;20:217–223. doi: 10.1097/01.wad.0000213849.51495.d9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Filley CM, Davis KA, Schmitz SP, Stears JC, Heaton RK, Kelly J, et al. Neuropsychological performance and magnetic resonance imaging in Alzheimer's disease and normal aging. Neuropsychiatry, Neuropsychology, and Behavioral Neurology. 1989;2:81–91. [Google Scholar]
- Fitzgerald JF, Smith DM, Martin DK, Freedman JA, Wolinsky FD. Replication of the multidimensionality of activities of daily living. Journal of Gerontology Series B: Psychological Sciences and Social Sciences. 1993;48:S28–S31. doi: 10.1093/geronj/48.1.s28. [DOI] [PubMed] [Google Scholar]
- Folstein M, Folstein S, McHugh PR. Mini-mental state: A practical method for grading the cognitive state of patients for the clinician. Journal of Psychiatric Research. 1975;12:189–198. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- Giovannetti T, Schmidt KS, Gallo JL, Sestito N, Libon DJ. Everyday action in dementia: Evidence for differential deficits in Alzheimer's disease versus subcortical vascular dementia. Journal International Neuropsychological Society. 2006;12:45–53. doi: 10.1017/S1355617706060012. [DOI] [PubMed] [Google Scholar]
- Grace J, Stout J, Malloy P. Assessing frontal behavior syndromes with the Frontal Lobe Personality Scale. Assessment. 1999;6:269–284. doi: 10.1177/107319119900600307. [DOI] [PubMed] [Google Scholar]
- Harwood DM, Hope T, Jacoby R. Cognitive impairment in medical patients. I: Screening for dementia - is history better than mental state? Age and Ageing. 1997;26:31–35. doi: 10.1093/ageing/26.1.31. [DOI] [PubMed] [Google Scholar]
- Hope T, Keene J, Gedling K, Fairburn CG, Jacob R. Predictors of institutionalization for people with dementia living at home with a carer. International Journal of Geriatric Psychiatry. 1998;13:682–690. doi: 10.1002/(sici)1099-1166(1998100)13:10<682::aid-gps847>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Fit indices in covariance structure modeling: Sensitivity to underparameterized model misspecification. Psychological Methods. 1998;3:424–453. [Google Scholar]
- Isella V, Villa L, Russo A, Regazzoni R, Ferrarese C, Appollonio IM. Discriminative and predictive power of an informant report in mild cognitive impairment. Journal of Neurology, Neurosurgery, and Psychiatry. 2006;77:166–171. doi: 10.1136/jnnp.2005.069765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jorm AF. Disability in dementia: Assessment, prevention and rehabilitation. Disability Rehabilitation. 1994;16:98–108. doi: 10.3109/09638289409166286. [DOI] [PubMed] [Google Scholar]
- Jorm AF, Christensen H, Henderson AS, Korten AE, Mackinnon AJ, Scott R. Complaints of cognitive decline in the elderly: A comparison of reports by subjects and informants in a community survey. Psychological Medicine. 1994;24:365–374. doi: 10.1017/s0033291700027343. [DOI] [PubMed] [Google Scholar]
- Jorm AF, Christensen H, Jacomb PA, Korten AE, Mackinnon AJ. The Cognitive Decline Scale of the Psychogeriatric Assessment Scales (PAS): longitudinal data on its validity. International Journal of Geriatric Psychiatry. 2001;16:261–265. doi: 10.1002/gps.326. [DOI] [PubMed] [Google Scholar]
- Jorm AF, Jacomb PA. The informant questionnaire on cognitive decline in the elderly (IQCODE): socio-demographic correlates, reliability, validity and some norms. Psychological Medicine. 1989;19:1015–1022. doi: 10.1017/s0033291700005742. [DOI] [PubMed] [Google Scholar]
- Jorm AF, Korten E. Assessment of cognitive decline in the elderly by informant interview. British Journal of Psychiatry. 1988;152:209–213. doi: 10.1192/bjp.152.2.209. [DOI] [PubMed] [Google Scholar]
- Jorm AF, Scott R, Cullen JS, Mackinnon AJ. Performance of the informant questionnaire on cognitive decline in the elderly (IQCODE) as a screening test for dementia. Psychological Medicine. 1991;21:785–790. doi: 10.1017/s0033291700022418. [DOI] [PubMed] [Google Scholar]
- Kemp NM, Brodaty H, Pond D, Luscombe G. Diagnosing dementia in primary care: The accuracy of informant reports. Alzheimer Disease and Associated Disorders. 2002;16:171–176. doi: 10.1097/00002093-200207000-00007. [DOI] [PubMed] [Google Scholar]
- McDonald RP. Test theory: A unified treatment. Erlbaum; Mahwah, NJ: 1999. [Google Scholar]
- Monnot M, Brosey M, Ross E. Screening for Dementia: Family caregiver questionnaires reliably predict dementia. Journal of American Board of Family Practice. 2005;18:240–256. doi: 10.3122/jabfm.18.4.240. [DOI] [PubMed] [Google Scholar]
- Morales J, Bermejo F, Romero M, Del-Ser T. Screening of dementia in community-dwelling elderly through informant report. Journal of Geriatric Psychiatry. 1997;12:808–816. [PubMed] [Google Scholar]
- Morris JC. The Clinical Dementia Rating (CDR): Current version and scoring rules. Neurology. 1993;43:2412–2414. doi: 10.1212/wnl.43.11.2412-a. [DOI] [PubMed] [Google Scholar]
- Morris JC, Heyman A, Mohs RC, Hughes JP, van Belle G, Fillenbaum G, et al. The Consortium to Establish a Registry for Alzheimer's Disease (CERAD). Part i. Clinical and neuropsychological assessment of Alzheimer's disease. Neurology. 1989;39:1159–1165. doi: 10.1212/wnl.39.9.1159. [DOI] [PubMed] [Google Scholar]
- Muthen LK, Muthen BO. Mplus user's guide. Muthen & Muthen; Los Angeles: 2004a. [Google Scholar]
- Muthen LK, Muthen BO. MPlus user's guide. 2nd ed. Muthen & Muthen; Los Angeles: 2004b. [Google Scholar]
- Muthen LK, Muthen BO. Mplus: Statistical analysis with latent variables. Muthen & Muthen; Los Angeles: 2006. [Google Scholar]
- Patrick CJ, Hicks BM, Nichol PE, Krueger RF. A bifactor approach to modeling the structure of the Psychopathy Checklist-Revised. Journal of Personality Disorders. 2007;21:118–141. doi: 10.1521/pedi.2007.21.2.118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reise SP, Morizot J, Hays RD. The role of bifactor model in resolving dimensionality issues in health outcome measures. Quality of Life Research. 2007;16:19–31. doi: 10.1007/s11136-007-9183-7. [DOI] [PubMed] [Google Scholar]
- Richardson ED, Nadler JD, Malloy PF. Neuropsychological predictions of performance measures of daily living skills in geriatric patients. Neuropsychology. 1995;9:565–572. [Google Scholar]
- Sclan SG, Reisber B. Functional Assessment (FAST) in Alzheimer's disease; Reliability, validity, and ordinality. International Psychogeriatrics. 1992;4:55–69. doi: 10.1017/s1041610292001157. [DOI] [PubMed] [Google Scholar]
- Seltzer B, Vasterling JJ, Mathias CW, Brennan A. Clinical and neuropsychological correlates of impaired awareness of deficits in Alzheimer disease and Parkinson disease: A comparative study. Neuropsychiatry, Neuropsychology, and Behavioral Neurology. 2001;14:122–129. [PubMed] [Google Scholar]
- Stern Y, Hesdorffer D, Sano M, Mayeuz R. Measurement and prediction of functional capacity in Alzheimer's disease. Neurology. 1990;40:8–14. doi: 10.1212/wnl.40.1.8. [DOI] [PubMed] [Google Scholar]
- Stern Y, Mayeuz R, Sano M. Predictors of disease course in patients with probable Alzheimer's disease. Neurology. 1987;37:1649–1653. doi: 10.1212/wnl.37.10.1649. [DOI] [PubMed] [Google Scholar]
- Stockdale GD, Gridley BE, Ware Balogh D, Holtgraves T. Confirmatory factor analysis of single- and multiple-factor competing models of the Dissociative Experiences Scale in a nonclinical sample. Assessment. 2002;9:94–106. doi: 10.1177/1073191102009001011. [DOI] [PubMed] [Google Scholar]
- Suurmeijer T, Doeglas DM, Mourm T, Briancon S, Krol B, Sanderman R, et al. The Groningen Activity Restriction Scale for measuring disability: Its utility in international comparison. American Journal of Public Health. 1994;84:1270–1273. doi: 10.2105/ajph.84.8.1270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teng EI, Chui HC, Schneider LS, Metzger LE. Alzheimer's dementia: Performance on the Mini-Mental State Examination. Journal of Consulting and Clinical Psychology. 1987;55:96–100. doi: 10.1037//0022-006x.55.1.96. [DOI] [PubMed] [Google Scholar]
- Teri L. Behavior and caregiver burden: Behavioral problems in patients with Alzheimer disease and its association with caregiver distress. Alzheimer's Disease and Associated Disorders. 1997;11:S35–S38. [PubMed] [Google Scholar]
- Tomaszewski Farias S, Mungas D, Jagust W. Degree of discrepancy between self and other-reported everyday functioning by cognitive status: Dementia, mild cognitive impairment, and healthy elders. International Journal of Geriatric Psychiatry. 2005;20:1–8. doi: 10.1002/gps.1367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tucker LR, Lewis C. A reliability coefficient for maximum likelihood factor analysis. Psychometrika. 1973;38:1–10. [Google Scholar]
- Williams JM. Cognitive Behavior Rating Scale. Psychological Assessment Resources; Odessa, FL: 1987. [Google Scholar]
- Wolinsky FD, Johnson RJ. The use of health services by older adults. Journal of Gerontology series B: Psychological Sciences and Social Sciences. 1991;46:S345–357. doi: 10.1093/geronj/46.6.s345. [DOI] [PubMed] [Google Scholar]
- Yu CY. Evaluation cutoff criteria of model fit indices for latent variable models with categorical and continuous outcomes. University of California; Los Angeles: 2002. Unpublished manuscript. [Google Scholar]