Abstract
Purpose
This study aims to develop a theoretical framework of the relationship among religiosity, spirituality, and depression, potentially explaining the often mixed and inconsistent associations between religiosity and depression.
Methods
In this cross-sectional study, 367 men (average age of 66 ± 9 years) with prostate cancer completed measures of religiosity (extrinsic/intrinsic), spirituality (FACIT Spiritual Well-Being Scale), quality of life (FACT-G) and depression (Hospital Anxiety and Depression Scale).
Results
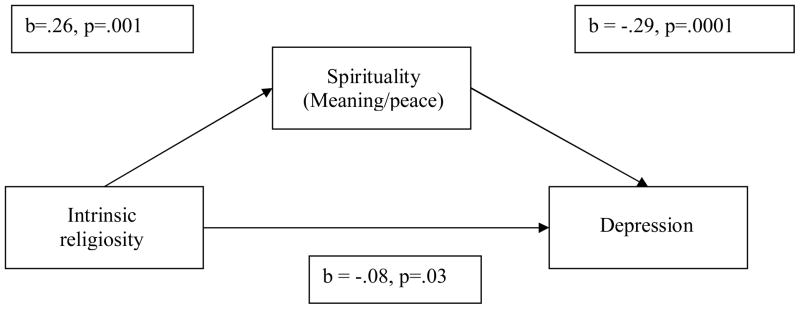
There was a small relationship between intrinsic religiosity and depression (r = −0.23, p<0.05) but a strong association between spirituality and depression (r = −0.58, p<0.01). Using a mediation model, the meaning/peace subscale of the spirituality measure mediated the relationship between intrinsic religiosity and depression. This model controlled for age, marital status, stage of disease, time since diagnosis, hormone therapy, quality of life, and anxiety.
Conclusions
When examining religiosity and spirituality, the main component that may help reduce depression is a sense of meaning and peace. These results highlight the potential importance of developing a patient’s sense of meaning through activities/interventions (not exclusive to religious involvement) to achieve this goal.
Introduction
Depression is considered one of the most common psychiatric disorders in the world affecting over 300 million people (1) . In general, the rate of depression for women ranges from 5% to 12% and the rate for men ranges from 2% to 3% (2) in community samples in the United States. One out of five Americans will develop depression in their lifetime, and approximately 6% of the US population will experience a depressive episode that will last 6 months (3). A diagnosis of depression increases both psychological suffering and mortality rates (3, 4).
The risk for developing a depressive disorder or experiencing distressing symptoms of depression for people with cancer is even greater than for the general public (5). Reported prevalence rates of depression among cancer patients have been estimated as high as 38% for major depression and 58% for depression spectrum syndromes (3). Prostate cancer is the most common site of cancer in men in the US impacting more than 230,000 men a year (6). Roth and colleagues (1998) reported that over 30% of men with prostate cancer had levels of distress high enough to warrant a referral for evaluation (7). The current study aims to clarify the relationships among spirituality, religiosity and depression in this high-risk sample.
Distinction between Religiosity and Spirituality
When discussing spirituality, it is important to make a distinction between religiosity and spirituality. Although for many years researchers have conceptualized religiosity and spirituality as synonymous, the social science literature has recently begun to disentangle these two constructs. Spirituality is defined as helping one understand and find purpose and meaning in life (8). Spirituality can be described as a broader and more universal construct than religiosity, framing spirituality as a subjective experience that can exist both inside and outside a religious framework (9). Hence, spirituality can exist in people who consider themselves very religious, slightly religious, or not at all religious (10). Religiosity is a related, but distinct construct that refers to organized behaviors intended to put spirituality into practice (11, 12). Thus, religion refers to an organized system of beliefs, practices, and ways of worship (13) that can serve as a way to channel or direct the expression of spirituality (14). Although religion provides a structured set of practices to help people become spiritual, religious affiliation does not guarantee spirituality and many individuals actively participate in religious rituals and practices without seeking or finding the deeper meaning that is a part of all organized religions (15).
Given the prevalence and debilitating impact of depression among both the healthy and the medically ill, the importance of identifying factors that may help attenuate depression is quite clear. Spirituality and religiosity may be two specific resources that are associated with lower rates of depression, and may help men with prostate cancer more effectively manage their distress. Spirituality may be a useful coping mechanism as men with prostate cancer deal with the existential issues that accompany this disease. In fact, spirituality has been identified as a potential mediator of psychological distress among patients with advanced cancer and AIDS (16, 17). Since older men tend to underutilize mental health services, spirituality may further serve as a means of informal support for them (18).
Since social scientists have only recently separated these two constructs, a vast majority of research studying religiosity and depression has viewed spirituality and religiosity as synonymous, and has generally operationalized these constructs as religious involvement or conviction. The literature examining this relationship has found a weak and at times inconsistent association between religion and depression. In a meta-analysis including 147 studies (N = 98, 975), Smith, McCullough, and Poll (2003) found a small significant correlation (r = −.096) between religiosity and depression (19). A common explanation for these weak and inconsistent findings is that the measurement of religion in most of the studies was inadequate (17, 20). A majority of these studies have measured religiosity simplistically, often times using one or two items such as the frequency of religious involvement or “belief” in religious faith (20–22).
Studies that have used multi-question measures of religiosity have found stronger relationships in univariate analyses (23, 24). In a review of the literature, McCullough and Larson (1999) estimated a small overall association between religiosity and depression (r = −.20) in univariate analyses when researchers used multiple question measures of religiosity (20). However, this relationship was substantially lower among the studies that conducted multivariate analyses (20), and in some occasions these effects drop to non-significance (25–28). In studies published since the above meta-analysis and review, there continue to be contradictory results examining the relationship between religiosity and depression (29–33). Additionally, the authors of these studies point out the need for more studies investigating mediating factors between these variables, and a better application to clinical practice. The current study aims to address both of these issues raised in the review.
Religiosity as a Multidimensional Construct
An important addition to this literature has been the conceptualization of religiosity as a multi-faceted construct (e.g. (34–36). Several studies have utilized Allport’s original conceptualization of intrinsic and extrinsic religiosity (34). According to Allport’s construct, intrinsically religious individuals “live” their religion and use it to develop a meaning-endowed framework to help understand life. In contrast, extrinsically religious individuals “use” religion as a means of comfort and social convention in a self-serving way (15). In general, these studies found a negative correlation between intrinsic religiosity and depression, with a corresponding inconclusive or positive relationship between extrinsic religiosity and depression (37–40). McCullough and Larson (1999) estimated the overall univariate relationship between intrinsic religiosity and depression to be r = −0.20, the same value reported using multi-question measures of religiosity and depression (20). However, few of these studies have used multivariate analysis to control for relevant demographic and psychosocial variables that may influence the relationship between intrinsic religiosity and depression.
Relationship between Spirituality and Depression
Recently, some authors have explored the association between spirituality (as a distinct construct from religiosity) and depression (16, 17, 41, 42). The initial results of these studies are promising, indicating that higher levels of spirituality are correlated with lower levels of depression. For example, in a sample of 162 terminally ill cancer and AIDS patients, Nelson et al. (2002) found a negative relationship (r = −0.40) between FACIT spiritual well-being scores (11) and scores on the Hamilton Depression Rating Scale (HDRS; (43) (17). This relationship remained significant (beta = −0.30) in a multivariate model after controlling for religiosity, number of physical symptoms, social support, and physical functioning. In a subsequent analysis, after replacing total FACIT scores with the two subscales of the FACIT (i.e., meaning/peace and faith) in the multivariate model, it was apparent that the meaning/peace subscale (beta = −0.34), as opposed to the faith subscale (non-significant), accounted for the association between spirituality and depression. In a sample of terminally ill cancer patients, McClain, Rosenfeld, and Breitbart (2003) also found a relationship between FACIT scores and scores on the HDRS (r = −0.51) (16). In this study, both the meaning/peace subscale (r = −0.52) and the faith subscale (r = −0.39) produced a negative correlation with depression. However, these relationships were not tested in a multivariate model as in the current study.
Spirituality as a Potential Mediator between Religiosity and Depression
The concept of spirituality may provide an important link when attempting to explain the inconsistent findings between religion and depression. Although the relationship between religiosity and depression has been extensively researched, the mechanisms through which these two constructs are related still require further exploration. As stated above, religion refers to an organized system of beliefs and ways of worship (13) that can serve as a method to channel or direct the expression of spirituality (14), however, religious activities do not ensure spirituality, as many individuals participate without seeking or finding the deeper spiritual meaning (15). A crucial factor in determining the emotional outcome of stressful life events is how individuals interpret those events (44). The power of spirituality is that it can provide a framework through which someone may interpret events to help gain an understanding of him or herself and cope with unpleasant or unavoidable circumstances without becoming depressed (45, 46).
Spirituality may be of particular importance for those diagnosed with cancer, as this diagnosis often forces patients to think about their mortality, while the unpredictable nature of the disease may limit the usefulness of previously used coping strategies (47). One novel hypothesis, supported by the research on spirituality cited above, is that spirituality may be the important link between religiosity and depression, and may mediate this relationship. If this is the case, the relationship between religiosity and depression will depend on how effective religiosity is at promoting the specific aspects of spirituality that are most strongly related to depression. This mediation model may account for the weak and inconsistent associations between religiosity and depression. Despite this possible explanation, few studies have examined the pathways among religiosity, spirituality, and depression.
Current Study and Hypotheses
The current study makes a distinction between religiosity and spirituality. Religiosity is defined with Allport’s concepts of intrinsic and extrinsic religiosity while spirituality is conceptualized to have two main aspects: meaning/peace and faith. Our hypotheses are: 1) intrinsic religiosity will have a significant positive association with spirituality, 2) both intrinsic religiosity and spirituality (specifically meaning/peace) will have a significant inverse relationship with depression, and 3) meaning/peace will mediate the relationship between religiosity and depression.
Method
Participants
The current cross-sectional study was part of a larger investigation examining anxiety in men with prostate cancer. Participants were recruited from the Urologic and Genito-Urologic Medical Oncology clinics at Memorial Sloan-Kettering Cancer Center in New York City during routine oncology appointments. To be eligible, participants were required to speak English, be at least 18 years old, and have a diagnosis of prostate cancer. Men who met these requirements were informed of the risks and benefits of study participation, and provided written informed consent if eligible and willing to participate. The Institutional Review Board (IRB) of Memorial Sloan-Kettering Cancer Center approved this study.
Procedure
Patients who provided informed consent were administered a series of self-report questionnaires while waiting for their appointment. General sociodemographic information (e.g., age, marital status, and ethnicity) and disease specific information (e.g., type of treatment, time since diagnosis) were collected.
Religiosity and Spirituality Measures
Religiosity was measured with the Age Universal I-E Scale–12 (I-E; (48), a 12-item self-report religious orientation scale which distinguishes between intrinsic and extrinsic religiosity The scale uses age universal language and a three-point scale (yes, not certain, and no). The intrinsic scale contains 6 items. Examples include, “I enjoy reading about my religion” and “My whole approach to life is based on my religion.” The extrinsic scale also contains 6 items. Examples include, “What religion offers me most is comfort in times of trouble and sorrow” and “I go to church because it helps me make friends.” Both the intrinsic and extrinsic religiosity scales have shown good internal consistency in previous research with Cronbach alpha coefficients ranging from .66 to .82 (49). In this sample, the Cronbach alpha coefficient for the intrinsic religiosity scale was .86 and for the extrinsic religiosity scale it was .73.
Spirituality was assessed with the Functional Assessment of Chronic Illness Therapy (FACIT)-Spiritual Well-Being Scale (SWB); (11), which includes two subscales: meaning/peace and faith. This scale was developed with the input of cancer patients, psychotherapists, and religious/spiritual advisors and designed to measure aspects of spirituality such as a sense of meaning in one’s life, harmony, peacefulness, and a sense of strength of one’s faith (11). The FACIT is a 12-item self-report scale that uses a five-point Likert response format (0–4). This scale has strong internal consistency, with a Cronbach alpha of .87 (11). The first factor is “meaning/peace” which corresponds to a sense of meaning, peace, and purpose in life. This factor contains eight questions. Examples include “My life has been productive” and “My life lacks meaning and purpose.” The internal consistency (Cronbach alpha) of this subscale was .84 in initial validation research (11). In the current study, the Cronbach alpha coefficient was .84. The second factor termed “faith” measures the comfort or strength derived from one’s faith. This factor contains four questions. Examples include “I find comfort in my faith or spiritual beliefs” and “My illness has strengthened my faith or spiritual beliefs.” The internal consistency of this subscale was .88 (11). In the current study, the Cronbach alpha coefficient was .87.
Psychosocial Measures
Depression and anxiety were measured by the Hospital Anxiety and Depression Scale (HADS) (50). This is a 14-item self-report questionnaire, which has been well tested in cancer populations. Responses are scored on a 4-point scale, and it is considered particularly useful for patients with chronic diseases because of the absence of somatic items that often confound the determination of psychiatric problems among the medically ill. As its name implies, the HADS has a depression and anxiety subscale, each consisting of 7-items. The HADS has demonstrated strong test-retest reliability in both elderly patients and patients with AIDS (51, 52).
Quality-of-life, which was used as a covariate in this study, was measured with the Functional Assessment of Cancer Therapy (FACT-G) (53, 54). The FACT-G is a quality of life questionnaire which includes a 27-item ‘core’ quality of life measure grouped into four subscales: physical well-being, social/family well-being, emotional well-being, and functional well-being. The FACT-G items are rated on a 5-item Likert scale, from 0, ‘not at all’ to 4, ‘very much’. The patients also completed the prostate specific subscale of the FACT, the FACT-P, which contains 12 questions rated on the same 5 point Likert scale, which address specific prostate cancer symptoms and side effects of treatment. The internal consistency of the subscales of the FACT-G ranges from acceptable to excellent, from .65–.82. The total FACT-G demonstrates excellent internal consistency with an alpha coefficient of .89. The test-retest reliability of the FACT-G is also excellent within a 7 day period, with correlations ranging from .82–.92 (53). The internal consistency of the FACT-P subscale is adequate, with a alpha coefficient of .69 (54).
Results
Participant Characteristics
Three hundred and sixty seven patients were recruited into the study. Of this total, 164 (45%) had early stage disease while 203 (55%) were classified with advanced disease. The average age of the sample was 66 years old (S.D.= 9.25; range, 41–91). A vast majority of the sample was Caucasian (n=326; 89%), whereas 24 (6%) were African-American and 17 (5%) were listed as “other.” Three hundred and five (84%) of the men were married and 270 (74%) had earned a college or advanced degree. Additional sociodemographic and medical characteristics for this sample are presented in Table 1.
Table 1.
Demographic Variables
| Demographics Variables: | N | % |
|---|---|---|
| Age | ||
| 40–55 | 45 | 12.3 |
| 56–65 | 129 | 35.1 |
| 66–75 | 141 | 38.4 |
| 76 and over | 52 | 14.2 |
| Ethnicity | ||
| White, non-Hispanic | 326 | 88.8 |
| African-American | 24 | 6.0 |
| Other | 17 | 5.2 |
| Marital Status | ||
| Married | 305 | 83.8 |
| Other | 60 | 16.2 |
| Disease Stage | ||
| Early (Local) | 164 | 44.8 |
| Adv. (Metastatic) | 203 | 55.2 |
| Baseline PSA | ||
| Under .05 | 114 | 33.4 |
| .05–5.00 | 103 | 30.0 |
| 5.01–10.00 | 25 | 7.2 |
| Over 10.00 | 101 | 29.4 |
| Treatment History | ||
| Prostatectomy | 196 | 53.4 |
| Radiation Therapy | 137 | 37.3 |
| Seed Implants | 22 | 6.0 |
| Orchiectomy | 7 | 1.9 |
| Hormone Therapy | 174 | 47.4 |
| Chemotherapy | 67 | 18.3 |
| Observation Only | 37 | 10.1 |
| Other Treatment | 30 | 8.2 |
Depression
The mean of the HADS depression subscale was 3.15 with a standard deviation of 3.00 and a range of 17. Using a cut-off of 7 or greater to indicate clinically meaningful depressive symptoms, 51 subjects (14%) scored above this cut-off score. Cutoff scores of both 7 and 8 have been reported in the literature. We selected 7 as a cutoff score for the HADS depression scale because lower cutoff scores for the HADS subscale have been reported to have greater sensitivity and specificity in prostate and breast cancer patients (55).
Religiosity and Spirituality
Table 2 lists the Pearson product-moment correlation coefficients between the intrinsic and extrinsic religiosity scores and the meaning/peace and faith subscales of the FACIT. There was a small (using guidelines as proposed by Cohen, 1988) (56) positive correlation between intrinsic religiosity and the meaning/peace subscale (r = 0.26, p < .01), and there was a large positive correlation between intrinsic religiosity and the faith subscale (r = 0.72, p < .01). When examining extrinsic religiosity, there was no significant correlation between extrinsic religiosity and the meaning/peace subscale. There was a large positive correlation between extrinsic religiosity and the faith subscale (r = 0.51, p < .01).
Table 2.
Correlations among religiosity, depression and spiritual well-being Scale
| Total Religiosity | Intrinsic | Extrinsic | Total SWB | Meaning/Peace | Faith | |
|---|---|---|---|---|---|---|
| Total Religiosity | 1.00 | |||||
| -Intrinsic | .94** | |||||
| -Extrinsic | 86** | .63** | ||||
| Total SWB | .50** | .54** | .32** | |||
| -Meaning/Peace | .21** | .26** | .10 | .88** | ||
| -Faith | .70** | .72** | .51** | .83** | .47** | 1.00 |
| HADS Dep. | −.18** | −.23** | −.07 | −.58** | −.64** | −.35** |
Note:
p < .01
Religiosity, Spirituality, and Depression
Table 2 also displays the Pearson product moment correlations among the intrinsic and extrinsic religiosity scales, the meaning/peace and faith subscales of the FACIT, and the depression subscale of the HADS. When examining religiosity, there was a small association between intrinsic religiosity and depression scores (r = −0.23 p < .01), while there was no association between extrinsic religiosity and depression scores. Of the subscales of the spiritual well-being scale, the meaning/peace subscale produced a large association with depression scores (r = −0.64 p < .01); the faith subscale demonstrated a medium correlation with depression (r = −0.35 p < .01).
Multi-variate analyses assessing the independent relationship among spirituality, intrinsic religiosity and depression
Multiple regression analysis was used to determine if the relationships among intrinsic religiosity, spiritual well-being (meaning/peace and faith), and depression remained after controlling for potential confounding variables that have demonstrated an association with depression. These confounding variables were selected through a review of the literature on depression in cancer patients and where possible, specifically in prostate cancer patients. Those variables identified in the literature to have a possible association with depression were selected to enter into the multiple regression equation (3, 5, 7, 57–61). The demographic variables selected were age and marital status (married/partnered vs. no partner); the disease specific variables were disease stage (early vs. late), time since diagnosis, and hormone therapy (hormones vs. no hormone); and the psychosocial variables were quality of life (FACT-G and FACT-P scores) and anxiety (HADS Anxiety scores).
For the religiosity analysis, the intrinsic religiosity subscale was used because previous literature has shown consistent relationships between intrinsic religiosity and depression, and those results were confirmed in the above analysis. We excluded extrinsic religiosity from this analysis, as previous research as shown primarily a non-significant association between extrinsic religiosity and depression, and this was also confirmed by the above results. Intrinsic religiosity was entered into the model with the co-variates (listed above), and produced a significant model (F=50.31, p<.01), which explained 60% of the variance in depression scores. Intrinsic religiosity was a significant predictor in the model (beta = −.08, p = .03, see Table 3).
Table 3.
Multiple regression models predicting HADS depression scores including intrinsic religiosity, total SWB scores and subscale scores, and the final mediational model.
| Source | Beta | t | p |
|---|---|---|---|
| Model 1- Intrinsic religiosity | |||
| Age | .10 | 2.36 | .02 |
| Marital Status | .01 | .16 | .87 |
| Stage of Disease | .00 | −.01 | .99 |
| Time since dx | .10 | 2.23 | .03 |
| Hormone Therapy | −.09 | −.1.98 | .05 |
| FACT-G | −.60 | −11.40 | .0001 |
| FACT-Prostate | −.06 | −1.30 | .19 |
| HADS Anxiety | .22 | 5.20 | .0001 |
| Intrinsic religiosity | −.08 | −2.18 | .03 |
| Model 2- SWB subscales | |||
| Age | .10 | 2.50 | .01 |
| Marital Status | .00 | −.07 | .94 |
| Stage of Disease | .00 | .03 | .98 |
| Time since dx | .09 | 2.18 | .03 |
| Hormone Therapy | −.05 | −1.25 | .21 |
| FACT-G | −.46 | −8.29 | .0001 |
| FACT-P | −.06 | −1.47 | .14 |
| HADS Anxiety | .13 | 3.18 | .01 |
| SWB: Meaning/peace | −.29 | −5.80 | .0001 |
| SWB: Faith | .00 | .04 | .97 |
| Model 3- Mediational Model | |||
| Age | .10 | 2.47 | .01 |
| Marital Status | .0 | −.12 | .91 |
| Stage of Disease | −.01 | −.18 | .86 |
| Time since dx | .09 | 2.23 | .03 |
| Hormone Therapy | −.05 | −1.16 | .25 |
| FACT-G | −.46 | −8.25 | .0001 |
| FACT-P | −.07 | −1.52 | .13 |
| HADS Anxiety | .14 | 3.39 | .002 |
| SWB: Meaning/peace | −.30 | −5.90 | .0001 |
| SWB: Faith | .07 | 1.13 | .26 |
| Intrinsic religiosity | −.08 | −1.48 | .14 |
Note:
M1 R2=.60, F (9, 305) = 50.31, p = .0001
M2 R2=.64, F (10, 309) = 54.06, p = .0001
M3 R2=.64, F (11, 303) = 48.84, p = .0001
This analysis was repeated with the Meaning/peace and faith subscales of the FACIT replacing intrinsic religiosity in the model. We chose to include both of these subscales as both have significantly associated with depression scores in the literature and in the results above. This model also was significant (F= 54.06, p<.01) and explained 64% of the variance in depression scores. Interestingly, the meaning/peace subscale was a significant predictor (beta = −0.29, p =.0001) whereas the faith subscale was not significant (see Table 3).
The Mediating Effect of Meaning/peace
Lastly, we included intrinsic religiosity with the two FACIT subscales (meaning/peace and faith), and the co-variates together in an analysis predicting HADS depression scores. Since any type of statistical method used to reduce the number variables in a regression equation (e.g., univariate prescreening, stepwise regression procedures) leads to model overfitting (62), those variables selected to be used in the previous models will be retained regardless of significance in those models. This model was significant, F (11, 303) = 48.84, p = .0001, and explained 64% of the variance in HADS depression scores (see Table 3). While the meaning/peace subscale was a significant predictor (beta = −0.29, p = .0001), the intrinsic religiosity subscale and the faith subscale were not significant in this model. In these analyses, the meaning/peace subscale satisfies the criteria of a mediating variable outlined by Baron and Kenny (1986) (63). Specifically, intrinsic religiosity was associated with depression scores, meaning/peace was associated with depression scores, and intrinsic religiosity was associated with meaning/peace. When meaning/peace was entered into the equation with intrinsic religiosity predicting depression scores, meaning/peace was a significant variable in the equation while intrinsic religiosity was not significant (See Figure 1). In addition, we tested the significance of the mediating model with the Sobel test, which indicated that the meaning/peace subscale was a significant mediating variable (Sobel test = 3.73, p = .0002).
Figure 1.
Diagram of the Mediation Model
Discussion
The current study further clarifies the relationship between religiosity and spirituality, demonstrating the similarities and differences between the underlying components of these constructs. As expected, the results demonstrated strong associations between religiosity and spirituality among our sample of men with prostate cancer. When analyzing the components of these measures, religiosity demonstrated a stronger association with the faith aspect of spirituality as compared to the meaning and peace component. In addition, the study explored the relative importance of each construct in predicting depression in this population.
Our results supported past research suggesting that religiosity and spirituality are negatively related to depression. However, in both univariate and multivariate analyses, spirituality emerged as the construct that was most strongly negatively associated with depression. More specifically, it appears that meaning/peace mediates the relationship between religion and depression. It is important to note that this is cross-sectional research, and we are proposing one explanation for these findings. However, it is also possible that the “arrows go the other way” and that those who are less depressed have a better capacity to establish meaning and peace in their lives. Future longitudinal data should address this question.
With this caveat, the possible explanation that meaning/peace may mediate the relationship between intrinsic religiosity and depression is intriguing. There is a consistent body of literature supporting the relationship between intrinsic religiosity and depression; however few studies have used a multivariate analysis to estimate the impact of other psychosocial variables (20). We found that the meaning/peace subscale mediates this relationship between intrinsic religiosity and depression. This is not necessarily surprising given previous studies that have shown that it is the meaning/peace component of spirituality, as compared to a measure of religiosity or the faith component of spirituality, which has the strongest buffering effects against depression and psychological distress (16, 17). This finding supports a theoretical model that suggests that meaning, whether achieved through a religious framework or other means, is most helpful when coping with depression.
The findings of this study may shed light on the relative inconsistent findings in the rather large body of literature regarding the relationship between religion and depression. It may be only for those who find meaning from their religious beliefs and activities that religiosity buffers depression. Although our research did not directly test the notion of positive vs. negative religious coping (64), it is possible that those who find meaning in their religion are those individuals who use religion as a positive coping resource. If this is true, these findings support the work of Pargament and others who have studied different aspect of religious coping. Inconsistencies in the religion and depression literature also exist due to the poor measurement of religion and spirituality. The fact that the components of religiosity and spirituality were differentially correlated with one another and with depression levels stresses the importance of conceptualizing religiosity and spirituality as unique, separate constructs in research and clinical applications.
These findings have important implications for clinicians who work with medically ill patients. It appears that helping patients establish meaning/peace in their lives may be a beneficial component in treating depression. The results of this study indicate that meaning may mediate the positive effects that religion may play in combating depression, and that those who are religious or non-religious may benefit from establishing meaning in their lives. Those patients open to religious interventions may benefit from referral to an appropriate religious support. However, those patients who do not identify with religious perspectives can also benefit from an intervention designed to bolster or support meaning in their lives. In contrast to a religious referral, helping patients explore the meaning in their lives can fall under the purview of psychosocial care workers. Some authors have suggested the potential of “benefit finding” as a way to help patients find some positive aspects or potential purpose in their diagnosis of cancer. There has been an increase in the recent literature on “benefit finding,” at times combined with cognitive behavioral stress management interventions, in several different medical populations including breast and prostate cancer and in multiple sclerosis. Although the results appear to be mixed (e.g. (65–68), these studies may provide further evidence for the findings of the current study postulating how meaning/purpose can serve as a protective mechanism.
The finding that meaning is beneficial to mental health raises a number of important questions regarding the sources of meaning in people’s lives. This study did not investigate how or from where these individual developed this meaning; this topic is an important area for future research. In addition to “benefit finding” discussed above, several research groups are currently examining exciting interventions designed to directly help individuals bolster the meaning in their lives (69, 70). For example, Breitbart and colleagues (71) are currently conducting feasibility and efficacy research on an intervention, based on Victor Frankl’s logotherapy, designed to assist patients in continuing to find meaning in their lives in the face of cancer. Chochinov and colleagues developed dignity therapy, which was designed to assist terminally ill patients proceed through the dying process with a continued sense of dignity through specifically addressing their existential concerns and bolstering a sense of purpose (72). Initial outcome data on the effectiveness of dignity therapy showed a decrease in depression scores and an increased will to live among those who received the treatment (72). Finally, Kissane and colleagues are currently developing an intervention designed to treat “demoralization syndrome” among cancer patients (73).
This study is not without limitations. First, the demographic characteristics of the study sample must be taken into account before the results can be generalized. The sample consisted of all men, between the ages of 45 and 95, most of whom were Caucasian and well-educated. Past research shows that minority populations tend to report higher levels of spirituality and religiosity than Caucasians (74). Additionally, findings should be interpreted with caution because this sample was made up entirely of prostate cancer patients. In other samples, findings may differ as women respond differently and samples free of disease many also produce varied results. Furthermore, the men in this sample reported overall high levels of meaning and peace. It is possible that different samples may have more evenly distributed levels of meaning/peace, which may affect the relationships among religiosity, meaning, and depression. It is important to address the limitations of our sample by conducting similar research studies with more diverse populations. As stated above, another limitation of this study is that it was a cross-sectional design. Therefore, causal relationships among spirituality, religiosity, and depression cannot be considered, and thus there may be additional predictor or mediating variables that have yet to be identified. Finally, the argument has been raised that spiritual well-being may simply be the opposite of depression. However, past research indicates that the Interclass Correlation Coefficient (ICC) between measures of depression with depression, and spirituality with spirituality are higher than the ICC between spirituality and depression (17). In another related research study (16), spirituality and depression each contributed unique variance toward a third variable, indicating that the two are separate, orthogonal constructs.
In conclusion, this study found that among men with prostate cancer, spirituality, specifically meaning/peace, was the salient variable that accounts for the relationship between religiosity and depression. These results highlight the complex relationship between religiosity and depression which when empirically tested often produces weak or inconsistent results. Furthermore, the study demonstrated that meaning/peace need not be associated with religiosity to be predictive of depression. Therefore, interventions designed to bolster meaning/peace in patients lives may be developed and delivered by not only pastoral care workers, but also psychosocial professionals.
References
- 1.National Mental Health Strategy (Australia), Australia. Dept. of Health and Aged Care. National action plan for depression : under the National Mental Health Plan: 1998–2003. Canberra: Mental Health and Special Programs Branch, Commonwealth Dept. of Health and Aged Care; 2001. Mental Health and Special Programs Branch. [Google Scholar]
- 2.American Psychiatric Association., American Psychiatric Association. Diagnostic and statistical manual of mental disorders : DSM-IV. 4. Washington, DC: American Psychiatric Association; 1994. Task Force on DSM-IV. [Google Scholar]
- 3.Massie MJ. Prevalence of depression in patients with cancer. J Natl Cancer Inst Monogr. 2004:57–71. doi: 10.1093/jncimonographs/lgh014. [DOI] [PubMed] [Google Scholar]
- 4.Wulsin LR, Vaillant GE, Wells VE. A systematic review of the mortality of depression. Psychosom Med. 1999;61:6–17. doi: 10.1097/00006842-199901000-00003. [DOI] [PubMed] [Google Scholar]
- 5.van’t Spijker A, Trijsburg RW, Duivenvoorden HJ. Psychological sequelae of cancer diagnosis: a meta-analytical review of 58 studies after 1980. Psychosom Med. 1997;59:280–293. doi: 10.1097/00006842-199705000-00011. [DOI] [PubMed] [Google Scholar]
- 6.American Cancer Society. from www.cancer.org.
- 7.Roth AJ, Kornblith AB, Batel-Copel L, et al. Rapid screening for psychologic distress in men with prostate carcinoma: a pilot study. Cancer. 1998;82:1904–1908. doi: 10.1002/(sici)1097-0142(19980515)82:10<1904::aid-cncr13>3.0.co;2-x. [DOI] [PubMed] [Google Scholar]
- 8.Muldoon M, King N. Spirituality, health care, and bioethics. J Relig Health. 1995;34:329–349. doi: 10.1007/BF02248742. [DOI] [PubMed] [Google Scholar]
- 9.Vaughan R, Wittine B, Walsh R. Transpersonal Psychology and the Religious Person. In: Shafranske EP, editor. Religion and the Clinical Practice of Psychology. Washington D.C.: American Psychological Association; 1988. pp. 483–509. [Google Scholar]
- 10.Ellerhorst-Ryan JM. Measuring Aspects of Spirituality. In: Frank-Stromborg M, editor. Instruments for Clinical Nursing Research. Norwalk, CT: Appleton and Lange; 1988. pp. 141–149. [Google Scholar]
- 11.Brady MJ, Peterman AH, Fitchett G, Mo M, Cella D. A case for including spirituality in quality of life measurement in oncology. Psychooncology. 1999;8:417–428. doi: 10.1002/(sici)1099-1611(199909/10)8:5<417::aid-pon398>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 12.Miller WR, Thoresen CE. Spirituality, religion, and health. An emerging research field. Am Psychol. 2003;58:24–35. doi: 10.1037/0003-066x.58.1.24. [DOI] [PubMed] [Google Scholar]
- 13.Emblen JD. Religion and spirituality defined according to current use in nursing literature. J Prof Nurs. 1992;8:41–47. doi: 10.1016/8755-7223(92)90116-g. [DOI] [PubMed] [Google Scholar]
- 14.Elkins DN, Hedstrom LJ, Hughes LL, Leaf JA, et al. Toward a humanistic-phenomenological spirituality: Definition, description, and measurement. Journal of Humanistic Psychology. 1988;28:5–18. [Google Scholar]
- 15.Donahue MJ. Intrinsic and extrinsic religiousness: Review and meta-analysis. Journal of Personality and Social Psychology. 1985;48:400–419. [Google Scholar]
- 16.McClain CS, Rosenfeld B, Breitbart W. Effect of spiritual well-being on end-of-life despair in terminally-ill cancer patients. Lancet. 2003;361:1603–1607. doi: 10.1016/S0140-6736(03)13310-7. [DOI] [PubMed] [Google Scholar]
- 17.Nelson CJ, Rosenfeld B, Breitbart W, Galietta M. Spirituality, religion, and depression in the terminally ill. Psychosomatics. 2002;43:213–220. doi: 10.1176/appi.psy.43.3.213. [DOI] [PubMed] [Google Scholar]
- 18.Klap R, Unroe KT, Unutzer J. Caring for mental illness in the United States: a focus on older adults. Am J Geriatr Psychiatry. 2003;11:517–524. [PubMed] [Google Scholar]
- 19.Smith TB, McCullough ME, Poll J. Religiousness and depression: evidence for a main effect and the moderating influence of stressful life events. Psychol Bull. 2003;129:614–636. doi: 10.1037/0033-2909.129.4.614. [DOI] [PubMed] [Google Scholar]
- 20.McCullough ME, Larson DB. Religion and depression: a review of the literature. Twin Res. 1999;2:126–136. doi: 10.1375/136905299320565997. [DOI] [PubMed] [Google Scholar]
- 21.Koenig HG, Hays JC, George LK, et al. Modeling the cross-sectional relationships between religion, physical health, social support, and depressive symptoms. Am J Geriatr Psychiatry. 1997;5:131–144. [PubMed] [Google Scholar]
- 22.Levin JS, Markides KS, Ray LA. Religious attendance and psychological well-being in Mexican Americans: a panel analysis of three-generations data. Gerontologist. 1996;36:454–463. doi: 10.1093/geront/36.4.454. [DOI] [PubMed] [Google Scholar]
- 23.Bienenfeld D, Koenig HG, Larson DB, Sherrill KA. Psychosocial predictors of mental health in a population of elderly women. Test of an explanatory model. Am J Geriatr Psychiatry. 1997;5:43–53. [PubMed] [Google Scholar]
- 24.Pressman P, Lyons JS, Larson DB, Strain JJ. Religious belief, depression, and ambulation status in elderly women with broken hips. Am J Psychiatry. 1990;147:758–760. doi: 10.1176/ajp.147.6.758. [DOI] [PubMed] [Google Scholar]
- 25.Brown DR, Gary LE. Religious involvement and health status among African-American males. J Natl Med Assoc. 1994;86:825–831. [PMC free article] [PubMed] [Google Scholar]
- 26.Ferraro K. Firm Believers? Religion, Body Weight, and Well-being. Rev Religion Res. 1998:39. [Google Scholar]
- 27.Musick MA, Koenig HG, Hays JC, Cohen HJ. Religious activity and depression among community-dwelling elderly persons with cancer: the moderating effect of race. J Gerontol B Psychol Sci Soc Sci. 1998;53:S218–227. doi: 10.1093/geronb/53b.4.s218. [DOI] [PubMed] [Google Scholar]
- 28.Strawbridge WJ, Shema SJ, Cohen RD, Roberts RE, Kaplan GA. Religiosity buffers effects of some stressors on depression but exacerbates others. J Gerontol B Psychol Sci Soc Sci. 1998;53:S118–126. doi: 10.1093/geronb/53b.3.s118. [DOI] [PubMed] [Google Scholar]
- 29.Koenig HG. Religion and depression in older medical inpatients. Am J Geriatr Psychiatry. 2007;15:282–291. doi: 10.1097/01.JGP.0000246875.93674.0c. [DOI] [PubMed] [Google Scholar]
- 30.Koenig HG, George LK, Titus P. Religion, spirituality, and health in medically ill hospitalized older patients. J Am Geriatr Soc. 2004;52:554–562. doi: 10.1111/j.1532-5415.2004.52161.x. [DOI] [PubMed] [Google Scholar]
- 31.Koenig HG, George LK, Titus P, Meador KG. Religion, spirituality, and acute care hospitalization and long-term care use by older patients. Arch Intern Med. 2004;164:1579–1585. doi: 10.1001/archinte.164.14.1579. [DOI] [PubMed] [Google Scholar]
- 32.King DA, Lyness JM, Duberstein PR, et al. Religious involvement and depressive symptoms in primary care elders. Psychol Med. 2007:1–9. doi: 10.1017/S0033291707000591. [DOI] [PubMed] [Google Scholar]
- 33.Moreira-Almeida A, Neto FL, Koenig HG. Religiousness and Mental Health: A Review. Revista Brasileira de Psiquiatria. 2006;28:242–250. doi: 10.1590/s1516-44462006000300018. [DOI] [PubMed] [Google Scholar]
- 34.Allport GW, Ross JM. Personal religious orientation and prejudice. J Pers Soc Psychol. 1967;5:432–443. doi: 10.1037/0022-3514.5.4.432. [DOI] [PubMed] [Google Scholar]
- 35.Kendler KS, Liu XQ, Gardner CO, et al. Dimensions of religiosity and their relationship to lifetime psychiatric and substance use disorders. Am J Psychiatry. 2003;160:496–503. doi: 10.1176/appi.ajp.160.3.496. [DOI] [PubMed] [Google Scholar]
- 36.Krause N. Measuring religiosity in later life. Research on Aging. 1993;15:170–197. [Google Scholar]
- 37.Fehring RJ, Miller JF, Shaw C. Spiritual well-being, religiosity, hope, depression, and other mood states in elderly people coping with cancer. Oncol Nurs Forum. 1997;24:663–671. [PubMed] [Google Scholar]
- 38.Ginia V, Shaw DG. Religion, Intrinsic-Extrinsic Orientation, and Depression. Review of Religious Research. 1991;32:276–283. [Google Scholar]
- 39.Nelson PB. Ethnic differences in intrinsic/extrinsic religious orientation and depression in the elderly. Arch Psychiatr Nurs. 1989;3:199–204. [PubMed] [Google Scholar]
- 40.Watson PJ, Hood RW, Foster SG, et al. Sin, Depression, and Narcissism. Review of Religious Research. 1988;29:295–305. [Google Scholar]
- 41.Yi MS, Mrus JM, Wade TJ, et al. Religion, spirituality, and depressive symptoms in patients with HIV/AIDS. J Gen Intern Med. 2006;21(Suppl 5):S21–27. doi: 10.1111/j.1525-1497.2006.00643.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.McCoubrie RC, Davies AN. Is there a correlation between spirituality and anxiety and depression in patients with advanced cancer? Support Care Cancer. 2006;14:379–385. doi: 10.1007/s00520-005-0892-6. [DOI] [PubMed] [Google Scholar]
- 43.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lazarus RS, Folkman S. Stress, appraisal, and coping. New York: Springer Pub. Co; 1984. [Google Scholar]
- 45.Brewer EDC. Life stages and spiritual well-being. In: Moberg DO, editor. Spiritual Well-Being, Sociological Perspectives. Washington, D.C.: University Press; 1979. pp. 99–111. [Google Scholar]
- 46.Fife BL. The conceptualization of meaning in illness. Soc Sci Med. 1994;38:309–316. doi: 10.1016/0277-9536(94)90400-6. [DOI] [PubMed] [Google Scholar]
- 47.Hilton BA. The relationship of uncertainty, control, commitment, and threat of recurrence to coping strategies used by women diagnosed with breast cancer. J Behav Med. 1989;12:39–54. doi: 10.1007/BF00844748. [DOI] [PubMed] [Google Scholar]
- 48.Maltby J. The internal structure of a derived, revised, and amended measure of the Religious Orientation Scale: The ‘Age-Universal’ I-E Scale-12. Social Behavior and Personality. 1999;27:407–412. [Google Scholar]
- 49.Trimble DR. The religious orientation scale: Review and meta-analysis of social desirablity effects. Educational and Psychological Measurement. 1997;57:970–986. [Google Scholar]
- 50.Zigmond AS, Snaith RP. The hospital anxiety and depression scale. Acta Psychiatr Scand. 1983;67:361–370. doi: 10.1111/j.1600-0447.1983.tb09716.x. [DOI] [PubMed] [Google Scholar]
- 51.Spinhoven P, Ormel J, Sloekers PP, et al. A validation study of the Hospital Anxiety and Depression Scale (HADS) in different groups of Dutch subjects. Psychol Med. 1997;27:363–370. doi: 10.1017/s0033291796004382. [DOI] [PubMed] [Google Scholar]
- 52.Savard J, Laberge B, Gauthier JG, Ivers H, Bergeron MG. Evaluating anxiety and depression in HIV-infected patients. J Pers Assess. 1998;71:349–367. doi: 10.1207/s15327752jpa7103_5. [DOI] [PubMed] [Google Scholar]
- 53.Cella DDF, Tulsky DDS, Gray GG, et al. The Functional Assessment of Cancer Therapy scale: development and validation of the general measure. Journal of Clinical Oncology. 1993;11:570. doi: 10.1200/JCO.1993.11.3.570. [DOI] [PubMed] [Google Scholar]
- 54.Esper PP, Mo FF, Chodak GG, et al. Measuring quality of life in men with prostate cancer using the functional assessment of cancer therapy-prostate instrument. Urology. 1997;50:920. doi: 10.1016/S0090-4295(97)00459-7. [DOI] [PubMed] [Google Scholar]
- 55.Nelson CJ, Holland J, Roth AJ. Assessing depression in geriatric cancer patients: Do we have appropriate measures?. Abstract to be Presented at the Annual Conference of the American Psych-Oncology Society; Irvine, CA. 2008. [Google Scholar]
- 56.Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, N.J.: L. Erlbaum Associates; 1988. [Google Scholar]
- 57.Roth A, Nelson CJ, Rosenfeld B, et al. Assessing anxiety in men with prostate cancer: further data on the reliability and validity of the Memorial Anxiety Scale for Prostate Cancer (MAX-PC) Psychosomatics. 2006;47:340–347. doi: 10.1176/appi.psy.47.4.340. [DOI] [PubMed] [Google Scholar]
- 58.Nelson CJ, Holland J, Roth AJ. Does growing older help cancer patients cope? Understanding how age impacts distress, anxiety, and depression in prostate cancer patients. Paper will be presented at the Annual Meeting of the American Psycho-Oncology Society; Irvine, CA. 2008. [Google Scholar]
- 59.Nelson CJ, Bhaskaran V, Breitbart W, BR, AR Distress in African-American men with prostate cancer. [Abstract] Annual Meeting of the Society of Behavioral Medicine; 2007. [Google Scholar]
- 60.Pirl WF, Mello J. Psychological complications of prostate cancer. Oncology (Williston Park) 2002;16:1448–1453. discussion 1453–1444, 1457–1448, 1467. [PubMed] [Google Scholar]
- 61.Pirl WF, Siegel GI, Goode MJ, Smith MR. Depression in men receiving androgen deprivation therapy for prostate cancer: a pilot study. Psychooncology. 2002;11:518–523. doi: 10.1002/pon.592. [DOI] [PubMed] [Google Scholar]
- 62.Babyak MA. What you see may not be what you get: a brief, nontechnical introduction to overfitting in regression-type models. Psychosom Med. 2004;66:411–421. doi: 10.1097/01.psy.0000127692.23278.a9. [DOI] [PubMed] [Google Scholar]
- 63.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 64.Bjorck JP, Thurman JW. Negative Life Events, Patterns of Positive and Negative Religious Coping, and Psychological Functioning. Journal for the Scientific Study of Religion. 2007;46:159–167. [Google Scholar]
- 65.Hart SL, Vella L, Mohr DC. Relationships among depressive symptoms, benefit-finding, optimism, and positive affect in multiple sclerosis patients after psychotherapy for depression. Health Psychol. 2008;27:230–238. doi: 10.1037/0278-6133.27.2.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.McGregor BA, Antoni MH, Boyers A, et al. Cognitive-behavioral stress management increases benefit finding and immune function among women with early-stage breast cancer. J Psychosom Res. 2004;56:1–8. doi: 10.1016/S0022-3999(03)00036-9. [DOI] [PubMed] [Google Scholar]
- 67.Carver CS, Antoni MH. Finding benefit in breast cancer during the year after diagnosis predicts better adjustment 5 to 8 years after diagnosis. Health Psychol. 2004;23:595–598. doi: 10.1037/0278-6133.23.6.595. [DOI] [PubMed] [Google Scholar]
- 68.Penedo FJ, Antoni MH, Schneiderman N. Cognitive-behavioral stress management for prostate cancer recovery : facilitator guide. Oxford ; New York: Oxford University Press; 2008. [Google Scholar]
- 69.Kinney CK, Rodgers DM, Nash KA, Bray CO. Holistic healing for women with breast cancer through a mind, body, and spirit self-empowerment program. J Holist Nurs. 2003;21:260–279. doi: 10.1177/0898010103254919. [DOI] [PubMed] [Google Scholar]
- 70.Freeman L, Cohen L, Stewart M, et al. Imagery intervention for recovering breast cancer patients: clinical trial of safety and efficacy. J Soc Integr Oncol. 2008;6:67–75. [PubMed] [Google Scholar]
- 71.Breitbart W, Gibson C, Poppito SR, Berg A. Psychotherapeutic interventions at the end of life: a focus on meaning and spirituality. Can J Psychiatry. 2004;49:366–372. doi: 10.1177/070674370404900605. [DOI] [PubMed] [Google Scholar]
- 72.Chochinov HM, Hack T, Hassard T, et al. Dignity therapy: a novel psychotherapeutic intervention for patients near the end of life. J Clin Oncol. 2005;23:5520–5525. doi: 10.1200/JCO.2005.08.391. [DOI] [PubMed] [Google Scholar]
- 73.Kissane DW, Clarke DM, Street AF. Demoralization syndrome--a relevant psychiatric diagnosis for palliative care. J Palliat Care. 2001;17:12–21. [PubMed] [Google Scholar]
- 74.Taylor RJ, Chatters LM, Jackson JS. Religious and spiritual involvement among older african americans, Caribbean blacks, and non-Hispanic whites: findings from the national survey of american life. J Gerontol B Psychol Sci Soc Sci. 2007;62:S238–250. doi: 10.1093/geronb/62.4.s238. [DOI] [PubMed] [Google Scholar]