Abstract
Introduction
Financial access to promotive, preventive, curative and rehabilitative healthcare by every one remains a challenge globally. The requirement to make direct payments at the time of consuming health services is one of the reasons why it persists. In this paper, we present findings on the financial risks households bear as a result of healthcare consumption in one district in Uganda.
Methodology
Using simple random sampling, we selected 384 household heads in 3 health sub districts. A structured questionnaire was to conduct the survey. Focus group discussions and Key Informant interviews were also conducted.
Results
Up to 77% (297/384) of households reported making direct payments for healthcare when a household member fell ill, 45% (174/384) did so each time a household member fell ill. Payment for healthcare was associated with employment of the household head in the informal sector (OR 1.6, 95% 1.2–2.1), presence of children OR 1.5, 95% 1.3–1.9 or someone with chronic illness OR 3, 95% 1.5–6 respectively and history of hospitalization (OR 3, 95% 1.7–6.5).
Conclusion
A high burden of healthcare needs, disproportionately affect children and women among households in Jinja. Direct payments for healthcare still occur in spite of the abolishment of user fees at public health facilities and tax based financing of health services in Uganda.
Introduction
Financial access to promotive, preventive, curative and rehabilitative healthcare by every one when they need it still poses a challenge globally. The requirement by households and individuals to make directs payments for healthcare presents one of the most common reasons why this challenge persists. WHO estimates that 100 million people are pushed into poverty every year as a result of direct (out-of-pocket payments) for healthcare. In addition, the poor are reluctant to seek healthcare as a result of the unpredictability of the cost1. Governments as stewards of their countries' health systems are called upon to ensure equitable access to health services by all citizens irrespective of economic circumstance2.
Although the Uganda government abolished the payment of user fees at public health facilities in 2001 financial access to healthcare has remained a challenge among households3,4. The total health expenditure of US$18 per capita is less than half of US$40 recommended by the WHO to finance a basic package of health services5,6,7. Moreover, about half of the total health expenditure occurs at household level as out of pocket payments and the health sector budget has remained below the 15% Abuja target8,9. More efforts are required to alleviate the financial burden of healthcare costs as well as the economic consequences of healthcare consumption among households. In this paper, we present the financial risks households bear as a result of healthcare consumption in one district in Uganda.
Methods
We conducted a cross-sectional survey from January to February 2006 in three of five health sub-districts in Jinja district, south eastern Uganda. Using simple random sampling, we selected 384 households in the three health sub districts based on the formula by Kish10 for survey sampling in prevalence studies when the outcome of interest is categorical. The number of households visited in each health subdistrict was proportional to the population of the health sub-district in relation to the total population of the three health sub districts selected.
A structured questionnaire was developed to conduct the field survey, covering: 1) household characteristics including size, gender of head, sources of income; 2) presence or absence of a household member with, chronic illness, history of delivery and or hospitalization in the past one year, and or recent illness in the three months preceding the survey; 3) whether the household sought healthcare when any one fell ill or gave birth and if so where and why; 4) who took the decision to seek healthcare; 5) whether the household made any payments for healthcare whenever any household member fell sick and how this was done. The data were collected by trained health workers who also participated in pre-testing of the data collection tools.
Data collectors went from house to house and surveyed those households in which the household head was present and voluntarily willing to participate at the time of the survey. All the people interviewed participated voluntarily and were requested to answer the questions freely. Medical/ prescription forms were used to verify the medical conditions reported in the survey, where this was not possible the conditions were verified on the basis of the description of symptoms and signs given by the household head.
Qualitative data collection methods such as Focus group discussions and Key Informant interviews were also employed to triangulate the data to overcome potential bias, and lead to greater validity and reliability.
Approval was obtained from Makerere University Higher Degrees Ethical Committee before commencement of the study.
Results
The mean household size was five people; 81% (310/384) of the households had children and 64% (246/384) of the heads were employed in the informal sector.
Payments for healthcare among households
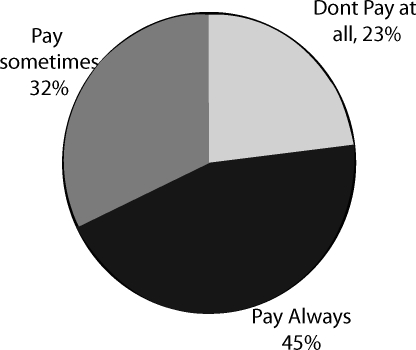
Up to 77% (297/384) of the households reported making healthcare payments at one time or another when a household member fell ill. Forty five percent (174/384) did so every time a household member fell ill. This was consistent with the findings from focus group discussions: For example during a FGD a woman said,
Healthcare is expensive for us; there is practically nothing for free even in public health facilities.
The payments made were sometimes unofficial and made to individuals not the health facility, as seen from some of the comments during FGD by one man;
If you come for an operation to remove your abscess and a health worker says there are no gloves in the clinic, you then have to pay and she brings the gloves.
Payment for healthcare was associated with employment of the household head in the informal sector (OR 1.6, 95% 1.2–2.1), presence of children or someone with chronic illness (OR 1.5, 95% 1.3–1.9 and OR 3, 95% 1.5–6 respectively) and history of admission (OR 3, 95% 1.7–6.5). There was no relationship between payment for healthcare and urban or rural location of households or the sex of the household head.
Seventy seven percent (172/224) of households reported paying between Ush1,000 (0.56 USD) and 10,000 (5.6 USD) per illness episode treated on outpatient basis. About two thirds (96/145) of households reported paying over Ush.10,000 per episode treated on inpatient basis. Most of the reported healthcare payments had been made at public health facilities (51%), followed by private-for-profit health facilities (47%). Table 1 gives a summary of the average amount of money paid on outpatient as well as inpatient basis by households per illness episode treated.
Table 1.
Amount of money paid per episode of illness treated
| Amount of money |
Out patient treatment (n=224) |
Inpatient treatment (n=145) |
||
| Uganda Shillings | Frequency | % | Frequency | % |
| 1,000 – 10,000 | 172 | 76.7 | 49 | 33.8 |
| 11,000 – 20,000 | 27 | 12.1 | 35 | 24.1 |
| 21,000 – 30,000 | 5 | 2.2 | 27 | 18.6 |
| 31,000 – 40,000 | 5 | 2.2 | 6 | 4.1 |
| 41,000 – 50,000 | 8 | 3.6 | 13 | 9 |
| Above 50,000 | 7 | 3.1 | 15 | 0.3 |
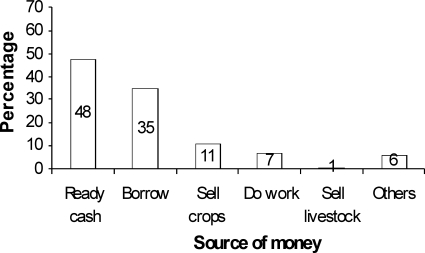
Only 47.9% (184/384) of households reported having disposable income that could be spent on healthcare. About thirty five percent (133/384) said they borrowed from someone in order to pay for healthcare. Figure 2 gives a summary of sources of money used to pay for healthcare by households.
Figure 2.
Sources of money used to pay for healthcare by households (n=384)
Healthcare needs among households
In 26% (99/384) of the households someone had been to hospital in the year preceding the study; 24% (93/384) had someone with a chronic health condition. In 21% (79/384) of households, someone had fallen sick three months prior to the survey and in 10% (38/384) of households someone had given birth in the year that had preceded the study. Of those that were reportedly admitted, 71% had been female and 29% less than five years old. Households with children (OR 2.3, 95% 1.14 – 4.5) were more likely to have had someone that had been admitted. There was no relationship between sex, occupation of the household head or location of household and occurrence of admission. Seventy one percent of those reported to have been admitted in the previous year were female while 26% of them were children under five years of age.
Households in rural areas (OR 1.5, 95% 1.16–1.97) or with children (OR 4.3, 95% 1.49 – 8.56) were more likely to have someone that had suffered a recent illness. There was no relationship between sex or occupation of the household head and a history of recent illness. Peptic Ulcer Disease (PUD) was the commonest chronic health condition, reported by 45% (42/93) of households who reported chronic health conditions in the household, and followed by HIV 19% (18/93), Chest diseases 18% (17/93) hypertension 11% (10/93).
Discussion
Healthcare needs among the households included in this study were high as evidenced by high levels of admission, recent illness, chronic health problems and delivery. There is an associated high household expenditure on healthcare, yet household incomes are low. This places households in difficulty if they are to pay for healthcare at the time of consuming health services as ready cash is not readily available as shown in Figure 2 where 52% of the population had no ready cash earmarked for healthcare consumption. Households are thus prone to catastrophic expenditure on healthcare which impoverishes them further.
Women and children were disproportionately suffering from illness that required admission suggesting that to improve women's as well as child health it is necessary to include improving financial access of households to health services.
Payment for healthcare at household level
A significant number of households continue to make out-of-pocket payments for healthcare at public health facilities in spite of the abolition of user fees. The abolition of user fees at lower level public health facilities did not translate into elimination of the requirement by households to pay for healthcare.
Indeed Xu et al4 have also shown that abolition of user fees in Uganda did not achieve reduction in catastrophic spending. Their explanation was that individuals were forced to seek better health services at private-for-profit and private-not-for-profit health facilities where they had to pay to receive services. But in this study, we found a significant number of households still pay at public health facilities.
Similar findings were also reported in the Uganda Participatory Poverty Assessment Process (UPPAP)11 in Jinja, which reported that patients were often told that there were no drugs at a health facility, but on making a payment drugs, suddenly became available. This highlights the need for additional efforts to protect households from the ill effects of out-of-pocket payments for healthcare, beyond the mere abolishment of user fees at public health facilities.
Most households engaging in payment for healthcare are already vulnerable because they have someone with a chronic illness; or the head does not a have stable income; or have children. This underscores the importance of and urgency needed in dealing with the problem of direct payments health services among households, especially because of the magnitude of healthcare needs among households shown in this study.
About a third of the households borrow money from a friend or money lender in order to pay for healthcare. This is not surprising, since payment for healthcare is associated with employment of the household head in the informal sector. In the absence of a readily available source from which to borrow money they are likely to resort to the sale of family assets in order to pay for healthcare. Many households are thus exposed to the risk of impoverishment due to having to pay for healthcare. This undermines the efforts of the Poverty Eradication Action Plan12, a government planning framework aimed at reducing mass poverty.
Conclusion
In this study we have found that households in Jinja district still face a high burden of healthcare needs that disproportionately affect children and women. In addition direct payment for healthcare still goes on for a significant number of households at the time of consuming health services. Most of the households make these payments at public facilities in spite of the abolishment of user fees at these facilities and the employment of the tax based financing of health services in Uganda.
We recommend that government, communities and households work towards establishment of alternative health financing mechanisms such as community health insurance. This will improve predictability of healthcare costs for households and dissociate the time of payment from the time of consuming health services13. Rural households, women and children need to be prioritized in view of disproportionately higher healthcare needs and unstable income. In addition government should work towards increasing the health sector budget to meet and even exceed the 15% commitment made in the Abuja declaration.
Figure 1.
Frequency of payments for health services among households (n=384)
Acknowledgement
The authors acknowledge EQUINET, the Uganda Health equity network and Makerere University School of Public Health for capacity support towards the publication of this paper.
References
- 1.WHO, author. The World Health Report 2000. Geneva: WHO; 2000. Health Systems: Improving performance. [Google Scholar]
- 2.WHO, author. Technical Briefs for Policy-Makers 2. Geneva: WHO; 2005. Designing Health Financing Systems to Reduce Catastrophic Health Expenditure. [Google Scholar]
- 3.MOH, author. 2003: Health sector strategic plan 2000/01 – 2004/5 Mid Term Review report. Uganda: Ministry of Health; 2003. Apr, [Google Scholar]
- 4.Xe Xu, David BE, Kadama P, Nabyonga J, Ogwang OP, Ana MA. Understanding the impact of eliminating user fees: Utilization and catastrophic health expenditures in Uganda. Social Science & Medicine. 2006;62(2):866–876. doi: 10.1016/j.socscimed.2005.07.004. [DOI] [PubMed] [Google Scholar]
- 5.MOH, author. 2005: Annual Health sector Performance report for Financial Year 2004/2005. Uganda: Ministry of Health; 2005. Oct, [Google Scholar]
- 6.World Health Organisation (WHO), author Report of the Commission on Macroeconomics and Health. Geneva: WHO; 2001. Macroeconomics and Health: Investing in Health for Economic Development. [Google Scholar]
- 7.WHO, author. Technical Briefs for Policy-Makers 2. Geneva: WHO; 2005. Designing Health Financing Systems to Reduce Catastrophic Health Expenditure. [Google Scholar]
- 8.African Union, author. The Abuja Declaration and Framework for Action for the fight against HIV/AIDS, tuberculosis and other related infectious diseases in Africa, 27th April 2001. Abuja: African Union; 2001. [Google Scholar]
- 9.Basaza R, Criel B, Van der Stuyf P. Low enrolment in Uganda Community Health Insurance Schemes: Underlying causes and policy implications. BMC Health Services Research. 2007;7:105. doi: 10.1186/1472-6963-7-105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kish L. Sampling organizations and groups of unequal sizes. American Sociological Review. 1965;30:564–572. [PubMed] [Google Scholar]
- 11.Ministry of Finance Planning and Economic Development, author. Uganda Participatory Poverty Assessment Process: Jinja District Report. Kampala: Government of Uganda; 2003. [Google Scholar]
- 12.Ministry of Finance Planning and Economic Development, author. The Poverty Eradication Action Plan (PEAP): Vol.1-Strategic Policy Framework. ( www.finance.go.ug)
- 13.Dong H, Kouyate B, Cairns J, Saueborn R. Differential willingness of household heads to pay community-based health insurance premia for themselves and other household members. Health Policy and Planning. 2004;19(2):120–126. doi: 10.1093/heapol/czh014. [DOI] [PubMed] [Google Scholar]