Abstract
Background
Despite the importance of functional status to older persons and their families, little is known about the course of disability at the end of life.
Methods
We evaluated data on 383 decedents from a longitudinal study involving 754 community-dwelling older persons. None of the subjects had disability in essential activities of daily living at the beginning of the study, and the level of disability was ascertained during monthly interviews for more than 10 years. Information on the conditions leading to death was obtained from death certificates and comprehensive assessments that were completed at 18-month intervals after the baseline assessment.
Results
In the last year of life, five distinct trajectories were identified, from no disability to the most severe disability: 65 subjects had no disability (17.0%), 76 had catastrophic disability (19.8%), 67 had accelerated disability (17.5%), 91 had progressive disability (23.8%), and 84 had persistently severe disability (21.9%). The most common condition leading to death was frailty (in 107 subjects [27.9%]), followed by organ failure (in 82 subjects [21.4%]), cancer (in 74 subjects [19.3%]), other causes (in 57 subjects [14.9%]), advanced dementia (in 53 subjects [13.8%]), and sudden death (in 10 subjects [2.6%]). When the distribution of the disability trajectories was evaluated according to the conditions leading to death, a predominant trajectory was observed only for subjects who died from advanced dementia (67.9% of these subjects had a trajectory of persistently severe disability) and sudden death (50.0% of these subjects had no disability). For the four other conditions leading to death, no more than 34% of the subjects had any of the disability trajectories. The distribution of disability trajectories was particularly heterogeneous among the subjects with organ failure (from 12.2 to 32.9% of the subjects followed a specific trajectory) and frailty (from 14.0 to 27.1% of the subjects followed a specific trajectory).
Conclusions
In most of the decedents, the course of disability in the last year of life did not follow a predictable pattern based on the condition leading to death.
According to the hypothesis of a compression of morbidity, if the onset of disability could be postponed, then life-time disability could be compressed into a shorter average period before death.1 Supporting this hypothesis, data from several large national surveys have shown a decline in disability rates that exceeds the observed decline in mortality.2,3 Although informative at the population level, these results may not be directly relevant to individual patients, their families, or their physicians, who may be more interested in knowing the likelihood and course of disability at the end of life. Previous research has shown that the majority of older persons are disabled in the last year of life.4,5 Much less is known, however, about the trajectories of disability at the end of life.
We conducted a study to identify clinically distinct trajectories of disability in the last year of life and to determine whether and how the distribution of these trajectories differs according to the condition leading to death. We postulated that for each condition there would be considerable heterogeneity in the disability trajectories at the end of life. To accomplish our objectives, we used data from a longitudinal study that included monthly assessments of disability for more than 10 years in a large cohort of older persons.
Methods
Study Population
Participants were drawn from an ongoing longitudinal study, described in detail elsewhere,6,7 involving 754 community-dwelling persons who were members of a large health plan. Eligible participants were 70 years of age or older and initially had no disability in the performance of four essential activities of daily living: bathing, dressing, walking, and transferring from a chair to a standing position. Subjects were excluded from enrollment in the study if they had clinically significant cognitive impairment with no available proxy,8 a life expectancy of less than 12 months, plans to move out of the area, or an inability to speak English. Persons with slow gait speed (i.e., those who required >10 seconds to walk along a 10-ft [3.0-m] course and back as quickly as possible) were oversampled. Only 4.6% of the persons contacted declined to undergo screening; 75.2% of those who were eligible for the study agreed to participate and were enrolled between March 1998 and October 1999.
Of the 405 participants who had died by December 31, 2008, a total of 17 had dropped out of the study after a median follow-up of 24 months (4.2%) and information on the condition leading to death was not available for 5 (1.2%), leaving 383 decedents in the analytic sample.
Data Collection
Comprehensive home-based assessments were completed at baseline and subsequently at 18-month intervals for 108 months, and telephone interviews were completed monthly through December 2008. Deaths were ascertained by review of the local obituaries, from the next of kin or another knowledgeable person during a subsequent telephone interview, or by both methods. The cause of death was coded, with the use of information from the death certificate, by a nosologist who had no access to other data on the participants. During the comprehensive assessments, data were collected on demographic characteristics, presence or absence of nine self-reported chronic conditions diagnosed by a physician, cognitive status,9 and status with respect to frailty.10
Assessment of Disability
Complete details regarding the assessment of disability, including the use of proxy respondents and formal tests of reliability and accuracy, are provided elsewhere.7,8 During the monthly interviews, for each of the four essential activities of daily living, we asked participants, “At the present time, do you need help from another person to (complete the task)?” Disability was defined as the need for personal assistance, and the severity of disability was indicated by the number of activities of daily living that the person was unable to carry out independently (from none to four) in a specific month. Disability in one or two activities of daily living was considered mild, and disability in three or four activities of daily living was considered severe.7,11
The completion rate for the monthly interviews was greater than 99%, with little difference between the subjects who had died and subjects who had not died. To account for the small amount of missing data on disability, we used a multiple-imputation technique with 100 random draws per missing observation.12
Classification of Conditions Leading to Death
To classify the conditions leading to death, we used a modified version of the protocol developed by Lunney and colleagues,13 with two major differences (Table 1). First, we added advanced dementia as a condition leading to death. Second, rather than defining frailty on the basis of any nursing home admission during the follow-up period, we used data from the comprehensive assessments to define the frailty phenotype according to the description by Fried et al.10,14 In addition, we made two modifications to the protocol developed by Lunney et al. in the category of organ failure. First, we included chronic kidney disease or cirrhosis, in addition to congestive heart failure and chronic lung disease. Second, to enhance specificity, we required that these diagnoses appear as the immediate or underlying cause of death, rather than in any diagnosis field, on the death certificate.
Table 1. Protocol for Classifying the Condition Leading to Death.
| Conditions Leading to Death | Source of Data | Criteria* |
|---|---|---|
| Cancer | Death certificate | ICD-10 codes C00.0–C97, D37.0-D37.9, and D44.0–D48.7 |
| Advanced dementia | Death certificate, comprehensive assessment | ICD-10 codes F01.0–F01.9, F03, G30.0–G30.9, R54, and A81.0; score of ≤10 on Mini–Mental State Examination9 |
| Organ failure | Death certificate | Congestive heart failure (ICD-10 codes I25.5, I42.0–142.9, and I50.0–I51.9), chronic lung disease (ICD-10 codes J43.0–J44.9, J47, J61, and J84.0–J84.9), chronic kidney disease (ICD-10 codes N18.0–N18.9), or cirrhosis (ICD-10 codes K74.0–74.6) |
| Frailty | Comprehensive assessment | Three or more of the following features: weight loss, exhaustion, low physical activity, muscle weakness, and slow gait speed14 |
| Sudden death | Death certificate, comprehensive assessment, monthly interview | Did not meet criteria for cancer, advanced dementia, organ failure, or frailty; reported no history of cancer, heart disease, chronic lung disease, diabetes, hip fracture, or stroke at any point during study; and was not living in a nursing home at time of death |
| Other conditions | Death certificate, comprehensive assessment, monthly interview | Did not meet criteria for cancer, advanced dementia, organ failure, frailty, or sudden death |
The death-certificate criteria were based on the immediate or underlying cause of death. In addition, data were obtained from the comprehensive assessment that was contemporaneous with or immediately preceded the beginning of the disability trajectory. ICD-10 denotes International Classification of Diseases, 10th Revision.
Because the conditions leading to death are not all mutually exclusive, we initially forced assignment of the decedents to unique groups by sequentially identifying each group and removing those decedents from the pool before identifying the next group, according to the modified version of the protocol developed by Lunney et al. The hierarchy of conditions leading to death (i.e., from cancer to advanced dementia to organ failure to frailty)13 was based on the premise that cancer is the predominant illness when it is listed as the immediate or underlying cause of death.
Statistical Analysis
To identify clinically distinct trajectories of disability, we used trajectory modeling15 This method allowed us to simultaneously estimate probabilities for multiple trajectories rather than a single mean for the population, as is the case for traditional regression or growth-curve models. We used the SAS procedure Proc Traj,15,16 which fits a semiparametric (discrete) mixture model to longitudinal data with the use of the maximum-likelihood method. The number of activities of daily living that the person was unable to carry out independently per month in the last year of life was modeled as a zero-inflated Poisson distribution. Participants who died during the first year of follow-up were retained in the primary analysis but were later excluded from a secondary analysis.
We used the Bayesian information criterion (BIC) to test from two to six trajectories and to determine whether each trajectory was best fit by intercept only (i.e., constant) or by linear, quadratic, or cubic terms.15,16 For each number of trajectories, the order of the equations was varied until a best-fitting model was derived with the use of the following formula: 2(ΔBIC) >2.15 Decedents were classified according to a specific trajectory on the basis of the maximum estimated probability of assignment. A probability of 0.9 or higher was considered an excellent fit, whereas a value of less than 0.7 was considered a poor fit.17 These analyses were repeated after adjustment for age, sex, race or ethnic group, years of education, and number of chronic conditions and, subsequently, after exclusion of the participants who died during the first year of follow-up. The proportions of decedents classified according to each trajectory, the mean probability of assignment, and the proportions with poor fit were based on the original data, and 95% confidence intervals were estimated with the use of 1000 bootstrap samples.18
We assessed relevant characteristics of the decedents according to the disability trajectories and conditions leading to death. Age was determined at the start of the disability trajectory, whereas the number of chronic conditions was determined during the comprehensive assessment, which was completed at or immediately before the start of the disability trajectory. In a final set of analyses, we determined the distribution of the disability trajectories for each of the conditions leading to death and subsequently evaluated the effect of overlap among conditions leading to death.
All analyses were performed with the use of SAS software (version 9.2). A two-sided P value of less than 0.05 was considered to indicate statistical significance.
Results
Disability Trajectories
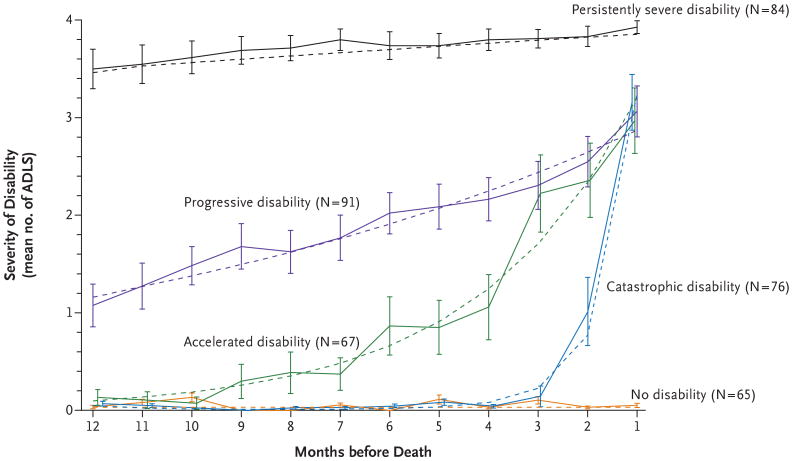
Five distinct trajectories in the last year of life were identified: no disability, catastrophic disability, accelerated disability, progressive disability, and persistently severe disability (Fig. 1). On average, 1 year before death, three of the groups of subjects — those with no disability, those with catastrophic disability, and those with accelerated disability (which combined accounted for more than half of all decedents) — were largely free of disability, whereas subjects in the progressive-disability group had mild disability and subjects in the remaining group had severe disability. The trajectories of the group with accelerated disability and the group with catastrophic disability diverged at about 10 and 3 months before death, respectively, from the trajectory of the group with no disability. The severity of disability in the progressive-disability group increased gradually over the course of the year. Despite these differences in trajectories, in the month before death, the mean (±SD) severity of disability (measured according to the number of activities of daily living that were affected, from zero to four) was similar in the progressive-disability group (3.07±1.27), accelerated-disability group (2.97±1.40), and catastrophic-disability group (3.16±1.27) and was significantly lower in these three groups than in the group with persistently severe disability (3.93±0.30, P<0.001 for each comparison), whose members remained severely disabled throughout the last year of life. For each trajectory, the predicted values for the severity of disability did not differ from the observed values, with only one exception (month 3 in the accelerated-disability group), and the mean probability of assignment to the trajectory was 0.9 or higher. The results shown in Figure 1 did not change appreciably after adjustment for age, sex, race or ethnic group, years of education, and number of chronic conditions or after the 25 participants who died during the first year of follow-up were excluded.
Figure 1. Trajectories of Disability in the Last Year of Life among 383 Decedents.
The severity of disability is indicated by the mean number of activities of daily living (ADLs) in which the subjects had disability. The solid lines indicate the observed trajectories, and the dashed lines indicate the predicted trajectories. The I bars indicate 95% confidence intervals for the observed severity of disability. The probability that the assigned and observed trajectories would be the same was less than 0.70 (range, 0.51 to 0.69) for only 37 of the decedents (9.7%). For all 37 of these decedents, an adjacent trajectory was associated with the next highest probability of assignment (range, 0.21 to 0.49). Nearly two thirds (23) of these 37 decedents had episodes of recovery from a more severe form of disability, whereas approximately 20% (7) had disability in a single activity in the month before death, without any preceding disability.
Characteristics of the Subjects
The characteristics of the decedents according to the trajectory of disability in the last year of life are shown in Table 2. The mean age ranged from 82.1 years in the catastrophic-disability group to 86.8 years in the group with persistently severe disability. Women were overrepresented in the progressive-disability group and the group with persistently severe disability. There were only modest differences in race or ethnic group across the five groups. The educational level was highest in the no-disability and catastrophic-disability groups, with values above the overall mean. The mean number of chronic conditions was similar among all the groups except for the no-disability group.
Table 2. Characteristics of the Decedents in the Last Year of Life, According to Disability Trajectory and Condition Leading to Death*.
| Variable | Subjects | Age | Female Sex | Non-Hispanic White Race or Ethnic Group† | Education | Chronic Conditions‡ |
|---|---|---|---|---|---|---|
| no. (%) | yr | no. (%) | no. (%) | yr | no. | |
| Overall | 383 (100) | 84.4±5.8 | 229 (59.8) | 351 (91.6) | 11.9±2.9 | 2.4+1.3 |
| Disability trajectory§ | ||||||
| No disability | 65 (17.0) | 82.8±5.9 | 37 (56.9) | 61 (93.9) | 12.4±3.0 | 2.0±1.1 |
| Catastrophic disability | 76 (19.8) | 82.1±5.7 | 37 (48.7) | 69 (90.8) | 12.4±2.7 | 2.4±1.3 |
| Accelerated disability | 67 (17.5) | 83.6±5.2 | 30 (44.8) | 60 (89.6) | 11.6±2.9 | 2.6±1.2 |
| Progressive disability | 91 (23.8) | 85.7±5.7 | 62 (68.1) | 86 (94.5) | 11.5±3.1 | 2.5±1.4 |
| Persistently severe disability | 84 (21.9) | 86.8±5.4 | 63 (75.0) | 75 (89.3) | 11.8±2.8 | 2.5±1.5 |
| Condition leading to death | ||||||
| Cancer | 74 (19.3) | 81.9±4.8 | 45 (60.8) | 67 (90.5) | 11.9±2.8 | 2.5±1.1 |
| Advanced dementia | 53 (13.8) | 87.3±5.9 | 36 (67.9) | 49 (92.5) | 11.8±2.9 | 2.0±1.3 |
| Organ failure | 82 (21.4) | 84.2±5.5 | 48 (58.5) | 77 (93.9) | 12.0±3.0 | 2.8±1.3 |
| Frailty | 107 (27.9) | 85.7±6.0 | 63 (58.9) | 98 (91.6) | 11.5±2.9 | 2.5±1.4 |
| Sudden death | 10 (2.6) | 82.5±6.0 | 5 (50.0) | 10 (100.0) | 13.3±3.5 | 1.3±0.7 |
| Other condition | 57 (14.9) | 82.9±5.3 | 32 (56.1) | 50 (87.7) | 12.5±0.9 | 2.2±1.2 |
Plus–minus values are means ±SD. Age was determined at the beginning of the disability trajectory, and the number of chronic conditions was determined during the comprehensive assessment at or immediately before the beginning of the disability trajectory.
Race or ethnic group was self-reported.
Chronic conditions included hypertension, myocardial infarction, congestive heart failure, stroke, diabetes mellitus, arthritis, hip fracture, chronic lung disease, and cancer.
The 95% confidence intervals for the frequency distribution, based on 1000 bootstrap samples, were 12.8 to 22.7 for the no-disability group, 11.5 to 24.7 for the catastrophic-disability group, 12.8 to 23.2 for the accelerated-disability group, 17.5 to 29.0 for the progressive-disability group, and 17.2 to 29.5 for the persistently-severe-disability group.
Disability Trajectories According to Condition Leading to Death
As shown in Table 2, the most common condition leading to death was frailty, followed by organ failure, cancer, another condition, advanced dementia, and sudden death. Overlapping conditions occurred primarily between the subjects with frailty and the subjects with cancer (in 33 of 383 decedents [8.6%]), advanced dementia (in 42 decedents [11.0%]), and organ failure (in 58 decedents [15.1%]). In addition, 5 of 383 decedents (1.3%) met the criteria for frailty, advanced dementia, and organ failure. Of the 57 decedents classified as having another condition, the underlying cause of death was ischemic heart disease in 36.8%, infection in 19.3%, and stroke in 14.4%.
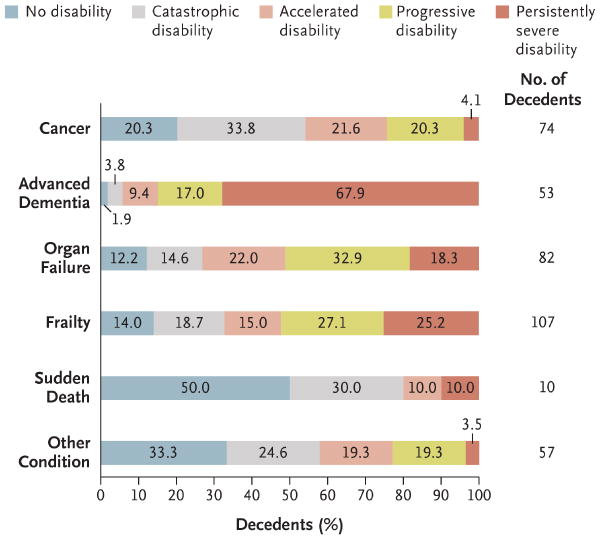
The distribution of the disability trajectories according to the condition leading to death is shown in Figure 2. A predominant trajectory was observed only for advanced dementia (i.e., persistently severe disability) and sudden death (i.e., no disability). For the other four conditions, no more than 34% of the subjects followed any of the disability trajectories. The distribution of the disability trajectories was particularly heterogeneous among the subjects with organ failure (from 12.2 to 32.9% followed a specific trajectory) and frailty (from 14.0 to 27.1% followed a specific trajectory). Considerable heterogeneity was also observed for cancer and the “other condition” category, although persistently severe disability was an uncommon disability trajectory for each. With the exception of advanced dementia, at least one quarter of the decedents with the five other conditions leading to death were not disabled or had very low levels of disability until only a few months before death. The relative distribution of the disability trajectories did not change appreciably when overlap was allowed among the conditions leading to death and when the conditions were sequentially defined, regardless of which order was used to define and remove the groups of subjects.
Figure 2. Distribution of Disability Trajectories in the Last Year of Life, According to Condition Leading to Death among the 383 Decedents.
The values within the bars are the percentages of decedents with the disability trajectories.
Discussion
In this prospective cohort study of community-dwelling older persons, we identified five clinically distinct trajectories of disability in the last year of life, and we found that the distribution of these trajectories was quite varied for several different conditions leading to death. The condition with the least variation was advanced dementia, which was characterized by high levels of disability throughout the last year of life. In contrast, for the five other conditions, from 26.8 to 80.0% of subjects were not disabled or had very low levels of disability until only a few months before death (i.e., they had catastrophic disability). These results indicate that for most decedents the course of disability at the end of life does not follow a predictable pattern based on the condition leading to death.
Despite the importance of functional independence to older persons and their families, little is known about the course of disability at the end of life. We found that most decedents had high levels of disability in the last month of life, yet more than half were not disabled 12 months before death. Among the decedents who were not disabled at the beginning of the study, the subsequent course of disability differed considerably, with about one third remaining free of disability, another third having an accelerated course of disability starting about 10 months before death, and the remainder having a rather abrupt development of disability in the last few months of life. The reasons underlying these different disability trajectories, which were observed commonly for each condition leading to death other than advanced dementia, are uncertain. The relative distribution of the trajectories was not sensitive to changes in the hierarchical order of the conditions leading to death.
The course of disability also differed considerably between the two groups of subjects with disability throughout the last year of life. Specifically, the disability was initially mild in the progressive-disability group and worsened gradually over the course of the year, but it was severe during the entire year in the group with persistently severe disability. Although the characteristics of these two groups differed only modestly, the group with persistently severe disability included a large proportion of subjects with advanced dementia. These results are consistent with those of previous studies, which have shown a high burden of disability at the end of life among older persons with advanced dementia.19
In contrast to decedents with advanced dementia, a sizable minority of participants who died from cancer were not disabled during the last year of life. These results belie the notion that cancer at the end of life invariably leads to disability and functional decline.13,20 We also found that the preceding course of disability varied considerably among the subjects with cancer who were disabled at the time of death; only about 40% of these subjects had a classic terminal phase characterized by an abrupt onset of disability in the last few months of life (i.e., catastrophic disability). This heterogeneity in disability trajectories, which was also observed for the two largest groups of subjects — those with organ failure and those who were frail — suggests that personal care needs at the end of life cannot be easily predicted for most older persons and raises concerns about policies that establish benefits for end-of-life care primarily on the basis of disease-specific criteria.21
Other investigators have postulated and provided supporting evidence that disability at the end of life follows distinct but predictable trajectories for cancer, organ failure, and frailty.13 These findings were based on data collected at annual intervals, and disability scores were averaged across all decedents with a specific condition leading to death. In contrast, we first identified clinically distinct trajectories of disability using data that were collected at monthly intervals, and we subsequently evaluated the distribution of these trajectories according to the condition leading to death. Each of the disability trajectories had considerable face validity, and the predicted values for the severity of disability did not differ from the observed values. In contrast to the approach used in a previous study,13 advanced dementia was evaluated as a distinct condition leading to death, and a widely accepted and validated phenotypic definition of frailty was used.14,22 These enhancements probably explain the smaller proportion of unclassified decedents in the current study than the previous study13 (14.9% vs. 23.6%) and, when coupled with the older average age of subjects and the requirement that decedents also have no reported history of chronic lung disease, they probably account for the relatively small number of sudden deaths in the current study.
Our study has several limitations. First, about one third of the decedents met criteria for more than one condition leading to death. Because older persons often have multiple coexisting conditions,23 the identification of a single condition leading to death may not always be feasible. When overlap was allowed among these conditions, the relative distribution of the disability trajectories did not change appreciably. Second, the use of information from death certificates is an imperfect strategy for classifying conditions leading to death. Previous research has shown that the concordance between coding of death certificates by a nosologist and an adjudicated cause of death is high for cancer and moderate for congestive heart failure and chronic lung disease but only fair for dementia,24 largely because of the underreporting of dementia on death certificates. We used data from cognitive testing in addition to coding by a nosologist to classify advanced dementia as a condition leading to death. Finally, because our study participants were members of a single health plan in a small urban area and were oversampled for slow gait speed, our results may not be generalizable to older persons in other settings. However, the demographic characteristics of our cohort did reflect those of older persons in New Haven County, Connecticut, which are similar to the characteristics of the U.S. population as a whole, with the exception of race or ethnic group.7
Our results suggest that the need for services at the end of life to assist with essential activities of daily living is at least as great for older persons dying from organ failure and frailty as for those dying from a more traditional terminal condition such as cancer, and that the need is much greater for older persons dying from advanced dementia. Nonetheless, the absence of a predictable disability trajectory based on the condition leading to death for most decedents poses challenges for the proper allocation of resources to care for older persons at the end of life.
Acknowledgments
Supported by grants from the National Institute on Aging (R37AG17560 and R01AG022993) and the Yale Claude D. Pepper Older Americans Independence Center (P30AG21342) and by a Midcareer Investigator Award in Patient-Oriented Research from the National Institute on Aging (K24AG021507, to Dr. Gill).
We thank Denise Shepard, B.S.N., M.B.A., Andrea Benjamin, B.S.N., Paula Clark, R.N., Martha Oravetz, R.N., Shirley Hannan, R.N., Barbara Foster, Alice Van Wie, B.S.W., Patricia Fugal, B.S., Amy Shelton, M.P.H., and Alice Kossack for assistance with data collection; Wanda Carr and Geraldine Hawthorne, B.S., for assistance with data entry and management; Peter Charpentier, M.P.H., for development of the participant tracking system; Linda Leo-Summers, M.P.H., for assistance with earlier drafts of the figures; Joanne McGloin, M.Div., M.B.A., for leadership and advice as the project director; and Nathalie de Rekeneire, M.D., for reviewing an earlier draft of the manuscript.
Footnotes
Disclosures provided by the authors are available with the full text of this article at NEJM.org.
References
- 1.Fries JF. Aging, natural death, and the compression of morbidity. N Engl J Med. 1980;303:130–5. doi: 10.1056/NEJM198007173030304. [DOI] [PubMed] [Google Scholar]
- 2.Manton KG, Gu X, Lamb VL. Change in chronic disability from 1982 to 2004/2005 as measured by long-term changes in function and health in the U.S. elderly population. Proc Natl Acad Sci U S A. 2006;103:18374–9. doi: 10.1073/pnas.0608483103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Freedman VA, Martin LG, Schoeni RF. Recent trends in disability and functioning among older adults in the United States: a systematic review. JAMA. 2002;288:3137–46. doi: 10.1001/jama.288.24.3137. [DOI] [PubMed] [Google Scholar]
- 4.Guralnik JM, LaCroix AZ, Branch LG, Kasl SV, Wallace RB. Morbidity and disability in older persons in the years prior to death. Am J Public Health. 1991;81:443–7. doi: 10.2105/ajph.81.4.443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Liao Y, McGee DL, Cao G, Cooper RS. Black-white differences in disability and morbidity in the last years of life. Am J Epidemiol. 1999;149:1097–103. doi: 10.1093/oxfordjournals.aje.a009763. [DOI] [PubMed] [Google Scholar]
- 6.Gill TM, Desai MM, Gahbauer EA, Holford TR, Williams CS. Restricted activity among community-living older persons: incidence, precipitants, and health care utilization. Ann Intern Med. 2001;135:313–21. doi: 10.7326/0003-4819-135-5-200109040-00007. [DOI] [PubMed] [Google Scholar]
- 7.Hardy SE, Gill TM. Recovery from disability among community-dwelling older persons. JAMA. 2004;291:1596–602. doi: 10.1001/jama.291.13.1596. [DOI] [PubMed] [Google Scholar]
- 8.Gill TM, Hardy SE, Williams CS. Underestimation of disability among community-living older persons. J Am Geriatr Soc. 2002;50:1492–7. doi: 10.1046/j.1532-5415.2002.50403.x. [DOI] [PubMed] [Google Scholar]
- 9.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12:189–98. doi: 10.1016/0022-3956(75)90026-6. [DOI] [PubMed] [Google Scholar]
- 10.Gill TM, Gahbauer EA, Allore HG, Han L. Transitions between frailty states among community-living older persons. Arch Intern Med. 2006;166:418–23. doi: 10.1001/archinte.166.4.418. [DOI] [PubMed] [Google Scholar]
- 11.Hardy SE, Dubin JA, Holford TR, Gill TM. Transitions between states of disability and independence among older persons. Am J Epidemiol. 2005;161:575–84. doi: 10.1093/aje/kwi083. [DOI] [PubMed] [Google Scholar]
- 12.Gill TM, Guo Z, Allore HG. Subtypes of disability in older persons over the course of nearly 8 years. J Am Geriatr Soc. 2008;56:436–43. doi: 10.1111/j.1532-5415.2007.01603.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lunney JR, Lynn J, Foley DJ, Lipson S, Guralnik JM. Patterns of functional decline at the end of life. JAMA. 2003;289:2387–92. doi: 10.1001/jama.289.18.2387. [DOI] [PubMed] [Google Scholar]
- 14.Fried LP, Tangen CM, Walston J, et al. Frailty in older adults: evidence for a phenotype. J Gerontol A Biol Sci Med Sci. 2001;56:M146–M156. doi: 10.1093/gerona/56.3.m146. [DOI] [PubMed] [Google Scholar]
- 15.Jones BL, Nagin DS, Roeder K. A SAS procedure based on mixture models for estimating developmental trajectories. Sociol Methods Res. 2001;29:374–93. [Google Scholar]
- 16.Jones BL, Nagin DS. Advances in group-based trajectory modeling and an SAS procedure for estimating them. Sociol Methods Res. 2007;35:542–71. [Google Scholar]
- 17.Nagin DS. Group-based modeling of development. Cambridge, MA: Harvard University Press; 2005. [Google Scholar]
- 18.Efron B, Tibshirani RJ. An introduction to the bootstrap. London: Chapman & Hall/CRC; 1993. [Google Scholar]
- 19.Chen JH, Chan DC, Kiely DK, Morris JN, Mitchell SL. Terminal trajectories of functional decline in the long-term care setting. J Gerontol A Biol Sci Med Sci. 2007;62:531–6. doi: 10.1093/gerona/62.5.531. [DOI] [PubMed] [Google Scholar]
- 20.Lunney JR, Lynn J, Hogan C. Profiles of older Medicare decedents. J Am Geriatr Soc. 2002;50:1108–12. doi: 10.1046/j.1532-5415.2002.50268.x. [DOI] [PubMed] [Google Scholar]
- 21.Gazelle G. Understanding hospice — an underutilized option for life's final chapter. N Engl J Med. 2007;357:321–4. doi: 10.1056/NEJMp078067. [DOI] [PubMed] [Google Scholar]
- 22.Bandeen-Roche K, Xue QL, Ferrucci L, et al. Phenotype of frailty: characterization in the Women's Health and Aging Studies. J Gerontol A Biol Sci Med Sci. 2006;61:262–6. doi: 10.1093/gerona/61.3.262. [DOI] [PubMed] [Google Scholar]
- 23.Weiss CO, Boyd CM, Yu Q, Wolff JL, Leff B. Patterns of prevalent major chronic disease among older adults in the United States. JAMA. 2007;298:1160–2. doi: 10.1001/jama.298.10.1160-b. [DOI] [PubMed] [Google Scholar]
- 24.Ives DG, Samuel P, Psaty BM, Kuller LH. Agreement between nosologist and cardiovascular health study review of deaths: implications of coding differences. J Am Geriatr Soc. 2009;57:133–9. doi: 10.1111/j.1532-5415.2008.02056.x. [DOI] [PMC free article] [PubMed] [Google Scholar]