Abstract
Contagious bovine pleuropneumonia (CBPP) is the most serious cattle disease in Africa, caused by Mycoplasma mycoides subsp. mycoides small-colony type (SC). CBPP control strategies currently rely on vaccination with a vaccine based on live attenuated strains of the organism. Recently, an lppQ− mutant of the existing vaccine strain T1/44 has been developed (Janis et al., 2008). This T1lppQ− mutant strain is devoid of lipoprotein LppQ, a potential virulence attribute of M. mycoides subsp. mycoides SC. It is designated as a potential live DIVA (Differentiating Infected from Vaccinated Animals) vaccine strain allowing both serological and etiological differentiation. The present paper reports on the validation of a control strategy for CBPP in cattle, whereby a TaqMan real-time PCR based on the lppQ gene has been developed for the direct detection of M. mycoides subsp. mycoides SC in ex vivo bronchoalveolar lavage fluids of cows and for the discrimination of wild type strains from the lppQ− mutant vaccine strain.
Keywords: Mycoplasma mycoides subsp. mycoides SC, TaqMan real-time PCR, Bronchoalveolar lavage fluids, lppQ− mutant vaccine strain, DIVA
1. Introduction
Contagious bovine pleuropneumonia (CBPP) caused by Mycoplasma mycoides subsp. mycoides small-colony type (SC), a bacterium belonging to the class Mollicutes, is a major constraint to cattle production in areas of eastern, central and western Africa, either as an endemic or re-emerging disease or in epidemic form (Windsor, 2000; Miltiadou et al., 2009). CBPP is currently considered one of the main stumbling blocks to the growth of the livestock industry on the African continent. Yearly losses directly or indirectly due to CBPP in Africa are estimated to be around 2 billion US dollars (Food and Agriculture Organization of the United Nations, 2004). Control of CBPP is therefore important as a way to salvage the losses and to ensure cattle owners of an income (Tambi et al., 2006). Current strategies to control CBPP rely on local quarantine of affected herds, antibiotic treatment of clinically diseased animals, or vaccination with a vaccine based on live attenuated strains.
Efficient control of CBPP not only requires more efficient vaccine strains (Thiaucourt et al., 2000, 2003; Thiaucourt, 2002; Wesonga et al., 2003; Mbulu et al., 2004; Pilo et al., 2007; Bischof et al., 2009), but also reliable diagnostic strategies that allow differentiating infected from vaccinated animals (DIVA). Lipoprotein LppQ is a particular membrane located protein of M. mycoides subsp. mycoides SC as it is serologically specific to this organism. It has a particularly strong antigenic N-terminal part that is located on the outer surface of the membrane (Bonvin-Klotz et al., 2008) and that elicits a specific and early immune response in naturally and experimentally infected animals (Bruderer et al., 2002). The C-terminal part of LppQ possesses an integral membrane structure built up of repeated units that are suspected to be involved in membrane anchoring (Abdo et al., 2000; Bonvin-Klotz et al., 2008). A recent study has shown that cattle immunized with the recombinant peptide comprising the extracellular N-terminal part of LppQ, using different adjuvant methods, were significantly more susceptible to infection with a virulent M. mycoides subsp. mycoides SC strain than cattle that were not vaccinated with LppQ (Nicholas et al., 2004). Hence, LppQ — which is devoid of protective T-cell epitopes (Dedieu et al., 2009) — appeared to exacerbate the effects of CBPP. Thus, an attenuated mutant lacking lppQ is likely to be a valuable second-generation vaccine and is expected to give lower side effects.
In the view to develop new efficacious and safe vaccine strains, the gene lppQ was inactivated by genetic engineering in the currently used live vaccine strain T1/44 using a transposon-based approach (Janis et al., 2008). In the present work, we aimed to develop a diagnostic tool for detection of M. mycoides subsp. mycoides SC in the lungs of CBPP-affected cattle and which allows discrimination of wild type strains from the recombinant DIVA T1lppQ− mutant vaccine strain.
2. Materials and methods
2.1. Mycoplasma strains, growth conditions and DNA extraction
Strains of mycoplasmas (n = 86) used in this study are listed in Table 1. Cells were grown in a standard mycoplasma medium (Axcell Biotechnologies, St. Genis l'Argentière, France) at 37 °C to a density of 108–109 cells/ml or on solid mycoplasma agar medium (Axcell Biotechnologies). Growth and handling of live M. mycoides subsp. mycoides SC were performed in a biological safety laboratory fulfilling the BL3 containment safety standards. Lysis of mycoplasmas with GES buffer (5 M guanidium thiocyanate, 100 mM EDTA, 0.5% N-lauroylsarcosine) and extraction of genomic DNA were performed as previously described (Vilei and Frey, 2001; Pilo et al., 2005; Bischof et al., 2008).
Table 1.
TaqMan results for the 86 strains of mycoplasmas tested in this study.
| Species | Straina | Origin | Isolated | Host | TaqMan |
|
|---|---|---|---|---|---|---|
| FTb | MGBb | |||||
| M. mycoides subsp. mycoides SC | PG1 | 1931 | Cattle/type strain | + | + | |
| 2059 | Spain | 1984 | Cattle/lung | + | + | |
| B773/125 | Portugal | 1991 | Cattle/semen | + | + | |
| C305 | Portugal | 1993 | Goat/lung | + | + | |
| O326 | Portugal | 1993 | Sheep/milk | + | + | |
| PO 1967 | France | 1967 | Cattle/lung | + | + | |
| PO 2 | France | 1980 | Cattle/lung | + | + | |
| 2022 | France | 1984 | Cattle/lung | + | + | |
| L2 | Italy | 1993 | Cattle/lung | + | + | |
| 402 | Italy | 1990 | Cattle/lung | + | + | |
| 6479 | Italy | 1992 | Cattle/lung | + | + | |
| Afadé | Cameroon | 1968 | Cattle/lung | + | + | |
| 87137-9 | Burkina Faso | 1987 | Cattle | + | + | |
| Filfili | Senegal | Pre-1988 | Cattle | + | + | |
| Fatick | Senegal | 1968 | Cattle | + | + | |
| B17 | Chad | 1967 | Zebu | + | + | |
| 9050-529/1 | Ivory Coast | 1990 | Cattle | + | + | |
| 91130 | Central African Republic | 1991 | Cattle | + | + | |
| 94111 | Rwanda | 1994 | Cattle | + | + | |
| 95014 | Tanzania | 1995 | Cattle | + | + | |
| T1/44 | Tanzania | 1952 | Cattle/vaccine strain | + | + | |
| T1lppQ−MT1 | DIVA mutant | 2008 | Transposon-based random mutagenesis | − | + | |
| T1lppQ−RSP1 | Recombinant mutant | 2008 | Transposon-based random mutagenesis | + | + | |
| T1/Sr50 | Tanzania | 1952 | Cattle/vaccine strain | + | + | |
| KH3J | Sudan | 1940 | Cattle/vaccine strain | + | + | |
| Gladysdale | Australia | Pre-1964 | Cattle | + | + | |
| DVZ | Australia | 1965 | Cattle | + | + | |
| R575 | Australia | 1965–1968 | Cattle | + | + | |
| V5 | Australia | 1936 | Cattle/vaccine strain | + | + | |
| Mycoplasma leachii | PG50 | Australia | 1963 | Cattle/joint/reference strain | + | − |
| B5415 | Portugal | Cattle | + | − | ||
| CP291 | Portugal | Goat/lung | + | − | ||
| PAD3186 | India | 1993 | Goat/milk | + | − | |
| FRD424 | India | 1993 | Goat/milk | + | − | |
| Calf 1 | Nigeria | Cattle/blood | + | − | ||
| D318b | Germany | Cattle/semen | + | − | ||
| C2306 | Portugal | Cattle | + | − | ||
| D424 | Germany | Cattle/preputium | + | − | ||
| QR1/92 | Australia | + | − | |||
| 4055 | France | Cattle/lung | + | − | ||
| B144P | USA | 1956 | Cattle/joint | + | − | |
| M. mycoides subsp. capri | PG3 | Turkey | 1950 | Goat/type strain | − | − |
| N108 | Nigeria | 1977 | Goat | − | − | |
| Capri L | France | 1975 | Goat | − | − | |
| 9139/11-91 | Turkey | 1991 | − | − | ||
| WK354/80 | Switzerland | 1980 | Goat | − | − | |
| 213 | India | 1984 | Goat | − | − | |
| Y-goat | Australia | 1956 | Goat/type strain (serovar MmmLC) | − | − | |
| 152/93 | Grand Canary | 1993 | Goat | − | − | |
| LC8065 | France | Goat | − | − | ||
| D2482/91 | Switzerland | 1991 | Goat | − | − | |
| 950010 | France | 1995 | Goat | − | − | |
| D2083/91 | Switzerland | 1991 | Goat | − | − | |
| CP271 | Portugal | 1991 | Goat | − | − | |
| D2503 | Switzerland | Goat | − | − | ||
| M. capricolum subsp. capricolum | California kid | USA | 1955 | Goat/type strain | − | − |
| 173/87 | Greece | 1987 | Sheep | − | − | |
| 6443.90 | France | 1990 | Goat | − | − | |
| M. capricolum subsp. capripneumoniae | F38 | Kenya | 1976 | Goat/type strain | − | − |
| 9081-487p | Oman | 1990 | Goat | − | − | |
| Gabès | Tunisia | 1981 | Goat | − | − | |
| M. bovis | PG45 | USA | 1962 | Cattle/milk/type strain | − | − |
| ML1 | France | Pre-1999 | Rabbit/lung | − | − | |
| 120/81 | Germany | 1980–1990 | Cattle/milk | − | − | |
| 221/89 | Germany | 1980–1990 | Cattle/milk | − | − | |
| 86p | Belgium | 1990–2000 | Cattle/milk | − | − | |
| 39G | Belgium | 1990–2000 | Cattle/bronchoalveolar lavage fluid | − | − | |
| 0435 | Belgium | 1990–2000 | Cattle/bronchoalveolar lavage fluid | − | − | |
| 9585 | Belgium | 1990–2000 | Cattle/bronchoalveolar lavage fluid | − | − | |
| 2610 | UK | 1990–2000 | Cattle/joint fluid | − | − | |
| 2138 | UK | 1990–2000 | Cattle/milk | − | − | |
| 2960 | UK | 1990–2000 | Cattle/lung | − | − | |
| M. bovirhinis | PG43 | 1967 | Cattle/respiratory tract/type strain | − | − | |
| O/D1467 | Switzerland | 2007 | Cattle/bronchus | − | − | |
| IMD1656 | Switzerland | 2008 | Cattle/bronchus | − | − | |
| M. bovigenitalium | PG11 | United Kingdom | Cattle/type strain | − | − | |
| 2D | Australia | 1974 | Sheep (former serogroup 11 strain) | − | − | |
| M. bovoculi | RF20391 | Cattle | − | − | ||
| M. agalactiae | PG2 | Spain | 1973 | Goat/type strain | − | − |
| 3990 | France | − | − | |||
| 5725 | France | 1990 | Sheep | − | − | |
| M. putrefaciens | KS1 | USA | Goat/type strain | − | − | |
| M. ovipneumoniae | Y98 | Sheep/respiratory tract/type strain | − | − | ||
| M. conjunctivae | HRC/581 | USA | 1972 | Sheep/type strain | − | − |
| M. hyopneumoniae | J | 1965 | Swine/type strain | − | − | |
| M. arginini | G230 | Mouse/brain/type strain | − | − | ||
Collections: the strains were obtained from the Australian Animal Health Laboratory (AAHL), Geelong, Victoria, Australia; Agence Française de Sécurité Sanitaire des Aliments (AFSSA), Lyon, France; BGVV, Jena, Germany; CIRAD-EMVT, Montpellier, France; Faculdad de Veterinaria, Universidad de Las Palmas, Spain; INRA, Villenave d'Ornon, France; Institute of Veterinary Bacteriology, University of Bern, Switzerland; Laboratório Nacional de Investigação Veterinária, Lisboa, Portugal; Laboratoire de Pathologie Bovine, Lyon, France; National Collection of Type Cultures (NCTC), PHLS, London, UK; National Veterinary Institute, Uppsala, Sweden; and Faculty of Veterinary Medicine, University of Liège, Belgium.
As determined in this study by real-time PCR of approximately 10 ng of genomic DNA. FT, TaqMan assay with the lppQ-based FAM probe (Bischof et al., 2006); MGB, TaqMan assay with the lppQ-based minor groove binding probe (Vilei et al., 2007).
Disruption of lppQ in the vaccine T1/44 was achieved by transposon-based genetic engineering to obtain the mutants T1lppQ−MT1 and T1lppQ−RSP1 (Janis et al., 2008) (Table 1).
2.2. PCR and sequencing strategies
Polymerase chain reaction (PCR) was performed with a DNA thermal cycler Gene Amp PCR System 9600 (Applied Biosystems, Foster City, CA, USA) in a 30-μl reaction mixture [1× reaction buffer B (supplied with FIREPol® DNA polymerase), 2.5 mM MgCl2, 250 μM of each dNTP] that contained approximately 50 ng of genomic template DNA, 2.5 U of FIREPol® DNA polymerase (Solis BioDyne, Tartu, Estonia), and 400 nM of oligonucleotide primers MMMLP481 and MMMLP484 (Abdo et al., 2000) for lppQ amplification. The mixtures were subjected to 3-min denaturation at 94 °C followed by 35 cycles of amplification with the parameters: 30 s at 94 °C, 30 s at 48 °C and 3 min extension at 72 °C, and a final extension step at 72 °C for 7 min. Amplicons were purified with the High pure PCR product purification kit (Roche Diagnostics, Rotkreuz, Switzerland).
DNA sequence analysis of the purified amplicons was performed with a DNA Sequenator AB 3100 genetic analyzer and the Taq dye deoxy terminator cycle sequencing kit (Applied Biosystems) using primers MMMLP481 and MMMLP484 for lppQ (Table 2). The assembly of DNA sequences and alignments of sequenced segments were done using the program Sequencher 4.6 (GeneCodes, Ann Arbor, MI, USA). Comparisons of DNA sequences and their deduced amino acid sequences with the EMBL/GenBank database were performed using the BLAST programs blastn, blastx and blastp (Altschul et al., 1990).
Table 2.
Primers and probes used for TaqMan PCR assays deduced from the lppQ gene sequence of M. mycoides subsp. mycoides SC type strain PG1.
| Primer | Sequence (5′–3′) | Positiona |
|---|---|---|
| lppQ-based TaqMan FT PCR (Bischof et al., 2006) | ||
| lppQTM-L | AATAATCAACAAAAAAAAGAGCAAGTAAGTAA | 1166019–1166050; 1189776–1189807 |
| lppQTM-R | TAGCCCTTTTATTTTTAGTAATGCTTGTAA | 1166144–1166115; 1189901–1189872 |
| lppQTM_FT | ACATCTTGTTTTTGTCACTCATTTTTTGGTTCAATTTT | 1166113–1166076; 1189870–1189833 |
| lppQ-based TaqMan MGB PCR (Vilei et al., 2007) | ||
| lppQTM2-L | CTAGAACTGAGGTTTTAGTAATTGGTTATGA | 1166317–1166347; 1190074–1190104 |
| lppQTM2-R | CACGCTCTAGACTAATAATTTCTTCTGGTA | 1166433–1166404; 1190190–1190161 |
| lppQTM2-MGB | AAAAATTTCTGGGTTTGCTCAA | 1166357–1166378; 1190114–1190135 |
Based on nucleotide sequence NC_005364, the complete genome of M. mycoides subsp. mycoides SC type strain PG1 (Westberg et al., 2004). The two copies of lppQ in PG1 span nt 1165902–1167239 and nt 1189659–1190996. Note that lppQ occurs only in one copy in all other M. mycoides subsp. mycoides SC strains (Bischof et al., 2006).
2.3. Selection of primers and TaqMan probes
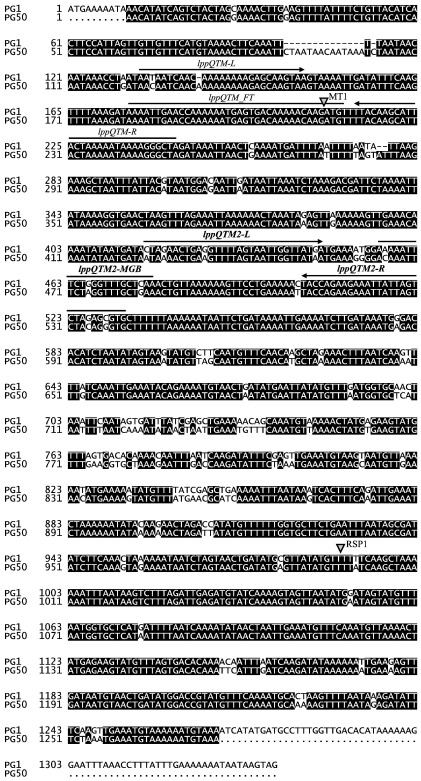
Primer Express 2.0 software (Applied Biosystems) was used to design oligonucleotide primers and fluorogenic probe, to be used in a TaqMan platform, specific to the locus of the gene lppQ of wild type strains of M. mycoides subsp. mycoides SC. The software displayed the two primers lppQTM-L and lppQTM-R, and the probe lppQTM_FT with FAM reporter dye and TAMRA quencher affixed on the 5′ and 3′ ends, respectively (Table 2) (Bischof et al., 2006). This TaqMan FT assay can discriminate wild type strains of M. mycoides subsp. mycoides SC from the recombinant strain T1lppQ−MT1, as the FT probe is concerned by the integration of the transposon after nucleotide position 208 of the lppQ gene (Fig. 1). As strains of Mycoplasma leachii — formerly known as Mycoplasma sp. bovine group 7 (Manso-Silván et al., 2009) — harbour a DNA fragment that is similar to lppQ (Fig. 1), real-time PCR using these oligonucleotides also detected strains of M. leachii. Thus, in the optic to select lppQ-specific TaqMan primers and probe that can discriminate M. mycoides subsp. mycoides SC from M. leachii (as well as from all other mycoplasmas), a new search was performed by using the TaqMan MGB (minor groove binder) primer and probe design option of Primer Express 2.0. MGB is a non-fluorescent quencher and substitutes TAMRA at the 3′ end of the probe. The sequence of the employed 22-nt probe lppQTM2-MGB is indicated in Table 2. As already reported (Vilei et al., 2007), primers lppQTM2-L and lppQTM2-R (Table 2) specifically amplify a 117-bp fragment from the locus of the gene lppQ of M. mycoides subsp. mycoides SC. All three oligonucleotides of the TaqMan MGB assay, however, match with the disrupted lppQ of the DIVA recombinant strain T1lppQ−MT1 (Fig. 1) and hence cannot discriminate the latter.
Fig. 1.
Location of the TaqMan primers and probes within the lppQ gene. The sequence of the lppQ gene from type strain PG1 (where it is present in two copies) of M. mycoides subsp. mycoides SC was aligned with the lppQ pseudogene sequence from the reference strain PG50 of M. leachii using the program DIALIGN 2.2.1 (http://bibiserv.techfak.uni-bielefeld.de/dialign/submission.html), and the alignment was finally elaborated with Boxshade 3.21 (http://www.ch.embnet.org/software/BOX_form.html). Identical nucleotides are shown on black background. The grey arrowheads indicate the site of disruption of lppQ in the mutants T1lppQ−MT1, which produces only 69 N-terminal amino acids of LppQ, and T1lppQ−RSP1, which still produces about 3/4 of the LppQ polypeptide. The mutant strains were achieved by genetic engineering using a transposon-based approach for the random mutagenesis of vaccine strain T1/44 (Janis et al., 2008). TaqMan primers are indicated by arrows, probes by lines.
2.4. Real-time PCR assays
Reactions were performed by using 2.5 µl of samples from each strain or 2.5 µl of 10 min-boiled bronchoalveolar lavage fluids, a 900 nM concentration of each TaqMan primer (Table 2) and 300 nM TaqMan probe (Table 2), and TaqMan Universal PCR Master Mix No AmpErase UNG (Applied Biosystems) in a 25-μl volume. An exogenous Internal Positive Control (IPC) reagent, consisting of 0.5× TaqMan IPC DNA, and 0.5× TaqMan IPC primers and probe (with VIC reporter and TAMRA quencher) (Applied Biosystems), was spiked into each reaction well of the TaqMan MGB assay in order to distinguish true target negatives from PCR inhibition. The concentration of the IPC primers in the PCR reaction was set reasonably lower than that of target primers, so that the amplification efficiency of the target reaction was not compromised. Real-time PCR reactions were run on an ABI 7500 instrument (Applied Biosystems) using the following cycling parameters: after one step at 50 °C for 2 min and at 95 °C for 10 min, 40 cycles of denaturation at 95 °C for 15 s and extension at 60 °C for 1 min were performed. Real-time fluorescence measurements were taken for each sample by using the Sequence Detector software 1.3.1 (Applied Biosystems) and the PCR cycle number at which the fluorescent lppQ-signal crossed the cycle threshold limit for each sample (2.5 µl) was recorded as Ct value. The threshold, i.e., the detected limit where the first PCR cycle has a significant increase in fluorescence signal, was adjusted at 0.1 for the TaqMan FT assay and at 0.2 for the TaqMan MGB assay. In both cases, thresholds were moved higher in the exponential phase of amplification than the default threshold values to avoid background noise. The fluorescence emission baseline was calculated from the first 3 to 15 cycles. Each sample was assayed in duplicate (unless otherwise stated), and the assay was repeated if the standard deviation (SD) between the two replicates was greater than 1 Ct.
2.5. Standard curves and specificity of the TaqMan assays
Three-day cultures (108–109 cells/ml, see above) of M. mycoides subsp. mycoides SC strains C305 and 2022 (Table 1) were centrifuged at 36,000 × g for 30 min. The pellets were washed once and then resuspended at a density of approximately 5 × 1010 cells/ml with the aid of a 27-gauge needle in sterile 0.85% sodium chloride solution. Small aliquots of these mycoplasma suspensions were used to count the number of colony forming units CFU obtained from 10-fold serial dilutions on solid mycoplasma medium (Axcell Biotechnologies). TaqMan standard curves were produced by analyzing serial dilutions of the two strains in lysis buffer (100 mM Tris–HCl, pH 8.5, 0.05% Tween 20, 0.24 mg/ml proteinase K), which contained 1.5 to 1.5 × 107 CFU per reaction (i.e., 600 to 6 × 109 CFU/ml). Samples were mixed for 1 min and incubated for 60 min at 60 °C followed by incubation for 15 min at 95 °C to obtain the lysates as template for PCR reactions in triplicates. The efficiency of the two described TaqMan reactions was calculated considering the slope of their standard curves and using the formula (10− 1/slope).
The specificity of the TaqMan assays was evaluated by testing approximately 10 ng of genomic DNA of each mycoplasma (n = 86) listed in Table 1, which covered the five members of the mycoides cluster that contains M. mycoides subsp. mycoides SC, M. leachii, M. mycoides subsp. capri — that now groups also strains of the serovar M. mycoides subsp. mycoides large-colony type (LC) (Manso-Silván et al., 2009) — Mycoplasma capricolum subsp. capricolum, and M. capricolum subsp. capripneumoniae, as well as a range of other species covering phylogenetically related species and representatives of other animal species. DNA was quantified spectrophotometrically and by visual comparison after gel electrophoresis and ethidium bromide staining.
2.6. Artificial contamination of bronchoalveolar lavage fluid with mycoplasmal preparations
Samples of bronchoalveolar lavages (Baselski and Wunderink, 1994; Miserez et al., 1997) from cattle were contaminated artificially with four consecutively 10-fold diluted suspensions of M. mycoides subsp. mycoides SC strains C305, O326 and 2022 (Table 1) to reach 2.8 × 106 to 2.8 × 109 CFU/ml. Quantification using the M. mycoides subsp. mycoides SC-specific TaqMan MGB assay was performed to confirm these CFU values and to assess the diagnostic efficacy of the lipoprotein gene lppQ-based real-time PCR for detection of M. mycoides subsp. mycoides SC in bronchoalveolar lavage fluids of cows.
2.7. Nucleotide sequence accession numbers
The nucleotide sequence of the lppQ pseudogene from the reference strain PG50 of M. leachii has been deposited under the EMBL/GenBank accession number AM158959 (1276 nucleotides in length).
3. Results
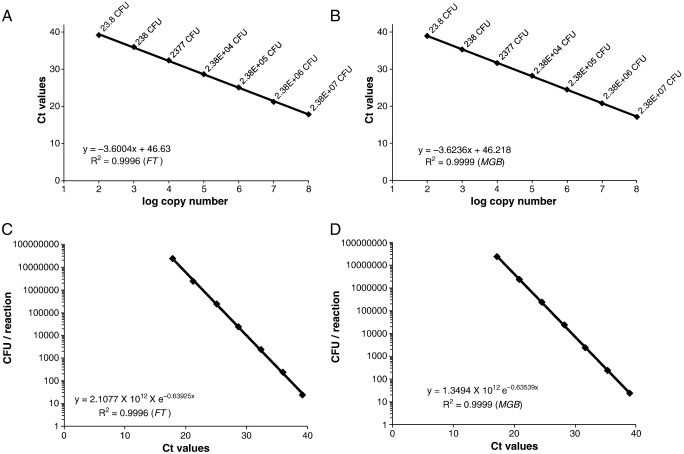
3.1. Standard curve and detection limit of the TaqMan assays
The standard curves for lppQ amplification (Ct values vs. log10(CFU)) generated by 10-fold serial dilutions of the two M. mycoides subsp. mycoides SC strains C305 and 2022 in lysis buffer were linear over a range of 7 log units, as illustrated by R2 values of 0.9996 (FT assay) and 0.9999 (MGB assay). The slopes were − 3.6004 (FT assay; Fig. 2A) and − 3.6236 (MGB assay; Fig. 2B), and the efficiencies (10− 1/slope) of the TaqMan assays were therefore 1.8956 (FT assay) and 1.8879 (MGB assay), both close to 2 (perfect PCR amplification). The detection limit of both TaqMan assays was at ∼ 15 CFU per reaction, corresponding to ∼ 6000 CFU/ml. The estimated quantities of mycoplasmal cells in clinical samples (see below) were determined using the formulas CFUreaction = 2.1077 × 1012 × e− 0.63925 × Ct (FT assay; Fig 2C) and CFUreaction = 1.3494 × 1012 × e− 0.63539 × Ct (MGB assay; Fig 2D), generated by linear regressions of the standard curves.
Fig. 2.
TaqMan PCR amplification of serial 10-fold dilutions of M. mycoides subsp. mycoides SC in lysis buffer. TaqMan FT (panel A) and MGB (panel B) standard curves generated by the analysis of known amounts of cells (CFU) of strains C305 and 2022. Three data sets for each strain and each dilution were used to generate a common standard curve. The mean Ct values are plotted against the log copy numbers of the standard dilutions. The linear regressions and the coefficients of correlation R2 were calculated. TaqMan FT (panel C) and MGB (panel D) standard curves for calculation of the amount of M. mycoides subsp. mycoides SC cells per reaction. The CFU in the reaction tube is plotted against the Ct values obtained with the serial 10-fold dilutions of M. mycoides subsp. mycoides SC. The obtained equation CFUreaction = 1.3494 × 1012 × e− 0.63539 × Ct of the TaqMan MGB assay was used to calculate the load of mycoplasmas in artificially contaminated bronchoalveolar lavage fluids.
3.2. The lppQ pseudogene in M. leachii
M. leachii revealed a pseudogene of lppQ (AM158959) with stop codons in all three forward frames, ruling out the possibility of having any lipoprotein production. It has a nucleotide similarity of 84% to the lppQ gene of M. mycoides subsp. mycoides SC, showing totally 18 gaps (Fig. 1). The TaqMan MGB primers and probe (Table 2) were selected from the available lppQ sequences from strains of M. mycoides subsp. mycoides SC so that they do not anneal to lppQ of M. leachii.
3.3. TaqMan specificities
The wild type strains of M. mycoides subsp. mycoides SC analyzed (n = 27) and the mutant vaccine T1lppQ−RSP1 gave positive signals when 10 ng of genomic DNA were tested in the TaqMan FT assay, yielding a mean Ct value of 19.51 (SD, 0.28). DNA of the mutant vaccine T1lppQ−MT1 remained negative in this TaqMan FT assay. However, strains of M. leachii (n = 12) all gave positive signals (Table 1).
In order to differentiate these latter from M. mycoides subsp. mycoides SC, the TaqMan MGB assay was used. All M. mycoides subsp. mycoides SC strains analyzed (n = 29), including both mutants T1lppQ−MT1 and T1lppQ−RSP1 carrying disrupted lppQ genes, gave specific signals when 10 ng of genomic DNA were tested in this TaqMan MGB assay, yielding a mean Ct value of 18.92 (SD, 0.22). The wide range of other Mycoplasma species (n = 57) gave negative reactions by the TaqMan MGB assay (Table 1).
3.4. Reproducibility of TaqMan MGB quantification with regard to the CFU counts
Linear curves obtained from the lppQ-based TaqMan MGB real-time PCR of bronchoalveolar lavage fluids contaminated artificially with four 10-fold dilutions of M. mycoides subsp. mycoides SC cultures from strains C305, O326 and 2022 had R2 values of > 0.999 (not shown). The estimated quantities of mycoplasmal cells in the suspensions were derived from the linear regression of the standard curve of the M. mycoides subsp. mycoides SC-specific TaqMan MGB assay (see above) and were found to be comparable to the known amount of inoculated cells (CFU), with a maximal divergence of approximately 30% only (Table 3). Using higher concentrations (≥ 2.8 × 108 CFU/ml), the calculated mycoplasmal loads in the suspensions were found to be moderately lower (− 15% to − 30%) compared to the inoculated CFU counts, whereas they were only slightly lower (0% to − 15%) at mycoplasmal concentrations ≤ 2.8 × 107 CFU/ml.
Table 3.
Comparison between TaqMan MGB assay-calculated mycoplasmal loads in artificially contaminated bronchoalveolar lavage fluids and inoculated CFU counts.
| Inoculateda (CFUreaction) | C305 |
O326 |
2022 |
|||
|---|---|---|---|---|---|---|
| Loadreactionb | Δ(%)c | Loadreactionb | Δ(%)c | Loadreactionb | Δ(%)c | |
| 7 × 106 | 5.52 × 106 (± 3.72 × 105) | − 21.08 | 4.93 × 106 (± 3.76 × 105) | − 29.61 | 5.23 × 106 (± 8.94 × 105) | − 25.23 |
| 7 × 105 | 5.94 × 105 (± 3.47 × 104) | − 15.16 | 5.74 × 105 (± 2.58 × 104) | − 18.07 | 5.57 × 105 (± 1.03 × 105) | − 20.38 |
| 7 × 104 | 6.19 × 104 (± 5280) | − 11.64 | 6.41 × 104 (± 5180) | − 8.50 | 6.51 × 104 (± 3801) | − 7.03 |
| 7 × 103 | 6524 (± 1260) | − 6.80 | 6974 (± 250.7) | − 0.37 | 6864 (± 339.2) | − 1.94 |
CFU counts present in 2.5 μl of bronchoalveolar lavage fluids contaminated artificially with 10-fold diluted suspensions of the three strains C305, O326 and 2022.
Mycoplasmal loads obtained by applying the formula loadreaction = 1.3494 × 1012 × e− 0.63539 × Ct generated by the linear regression of the standard curve from the M. mycoides subsp. mycoides SC-specific TaqMan MGB assay. Four data sets for each strain and each dilution were used.
Percent difference between calculated mycoplasma loads and inoculated CFU counts.
4. Discussion
The high specificity and strong antigenicity of LppQ have been already exploited for the development of a robust indirect ELISA test for serological diagnosis and for epidemiological investigations of CBPP (Bruderer et al., 2002). This ELISA test is able to differentiate infected cattle from cattle immunized with the M. mycoides subsp. mycoides SC DIVA strain T1lppQ−MT1, as the latter produces no LppQ (Janis et al., 2008). Also several DNA-based assays, which are less burdensome than diagnostic methods based on immunological tests, have already been developed for the efficient detection of M. mycoides subsp. mycoides SC: these include Southern blotting (Frey et al., 1995; Vilei et al., 1999; Pilo et al., 2003), conventional PCR tests (Bashiruddin et al., 1994; Dedieu et al., 1994; Miserez et al., 1997; Bashiruddin et al., 1999; Persson et al., 1999; Vilei et al., 2000; Vilei and Frey, 2004; Miles et al., 2006) and real-time PCR assays (Gorton et al., 2005; Bischof et al., 2006, 2008; Vilei et al., 2007; Fitzmaurice et al., 2008; Lorenzon et al., 2008).
The current study has evidenced that the real-time PCR assay using primers lppQTM-L and lppQTM-R, and the probe lppQTM_FT (Table 2) in the lppQ-based TaqMan FT assay (Bischof et al., 2006) works in such a discriminatory way that the disrupted lppQ gene in the LppQ− mutant vaccine T1lppQ−MT1 is not detected. However, this TaqMan FT assay also recognizes strains of M. leachii because the latter harbour an lppQ pseudogene that is not expressed due to stop codons in all three forward frames. On the other hand, the second lppQ-based real-time PCR assay employed in this study, which uses primers lppQTM2-L and lppQTM2-R, and the probe lppQTM2-MGB (Table 2) in the TaqMan MGB assay (Vilei et al., 2007) may be applied to specifically monitor M. mycoides subsp. mycoides SC in the lungs of cattle presenting CBPP symptoms. In fact, this TaqMan MGB assay was able to detect all DNAs extracted from M. mycoides subsp. mycoides SC strains while the wide range of related Mycoplasma species, including M. leachii, gave no reactions. Another important feature is the sensitivity of both lppQ-based TaqMan assays, whereby as less as 6000 mycoplasmal cells/ml can be detected efficiently. While validating the reproducibility of the M. mycoides subsp. mycoides SC-specific TaqMan MGB assay, the estimated quantities of mycoplasmal cells in the artificially contaminated clinical samples were comparable to the inoculated CFU counts, showing divergences lower than 30%. Sensitivity and specificity of the test under field conditions (living animals) remain to be explored.
In conclusion, the two lipoprotein gene lppQ-based TaqMan real-time PCR assays described in this paper constitute a rapid, specific and sensitive test for the detection of M. mycoides subsp. mycoides SC. The MGB assay is specifically designed to monitor efficiently the mycoplasma in the bronchoalveolar lavage fluids of cattle presenting CBPP symptoms, while the FT assay will be applicable for future differentiation of cattle infected with wild type strains of M. mycoides subsp. mycoides SC from those immunized with the DIVA vaccine, i.e., the T1lppQ−MT1 derivative of the classical T1/44 vaccine strain.
Acknowledgements
We are grateful to C. Janis, A. Blanchard and P. Sirand-Pugnet (INRA, Université Victor Segalen Bordeaux 2, Villenave d'Ornon, France) for providing us with the two T1lppQ− mutant vaccine strains. This study was supported by grant no. 075804 “A genomics approach to understanding the immunopathology of contagious bovine pleuropneumonia (CBPP): improvement of current live vaccines and the development of next generation vaccines” of the Wellcome Trust (London, UK) and research contract no. 13813 “Control of CBPP” of the IAEA CRP D32024.
References
- Abdo E.-M., Nicolet J., Frey J. Antigenic and genetic characterization of lipoprotein LppQ from Mycoplasma mycoides subsp. mycoides SC. Clin. Diagn. Lab. Immunol. 2000;7:588–595. doi: 10.1128/cdli.7.4.588-595.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Altschul S.F., Gish W., Miller W., Myers E.W., Lipman D.J. Basic local alignment search tool. J. Mol. Biol. 1990;215:403–410. doi: 10.1016/S0022-2836(05)80360-2. [DOI] [PubMed] [Google Scholar]
- Baselski V.S., Wunderink R.G. Bronchoscopic diagnosis of pneumonia. Clin. Microbiol. Rev. 1994;7:533–558. doi: 10.1128/cmr.7.4.533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bashiruddin J.B., Taylor T.K., Gould A.R. A PCR-based test for the specific identification of Mycoplasma mycoides subspecies mycoides SC. J. Vet. Diagn. Invest. 1994;6:428–434. doi: 10.1177/104063879400600405. [DOI] [PubMed] [Google Scholar]
- Bashiruddin J.B., DeSantis P., Vacciana A., Santini F.G. Detection of Mycoplasma mycoides subspecies mycoides SC in clinical material by a rapid colorimetric PCR. Mol. Cell. Probes. 1999;13:23–28. doi: 10.1006/mcpr.1998.0206. [DOI] [PubMed] [Google Scholar]
- Bischof D.F., Vilei E.M., Frey J. Genomic differences between type strain PG1 and field strains of Mycoplasma mycoides subsp. mycoides small-colony type. Genomics. 2006;88:633–641. doi: 10.1016/j.ygeno.2006.06.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bischof D.F., Janis C., Vilei E.M., Bertoni G., Frey J. Cytotoxicity of Mycoplasma mycoides subsp. mycoides Small Colony type to bovine epithelial cells. Infect. Immun. 2008;76:263–269. doi: 10.1128/IAI.00938-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bischof D.F., Vilei E.M., Frey J. Functional and antigenic properties of GlpO from Mycoplasma mycoides subsp. mycoides SC: characterization of a flavin adenine dinucleotide-binding site deletion mutant. Vet. Res. 2009;40:35. doi: 10.1051/vetres/2009018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bonvin-Klotz L., Vilei E.M., Kühni-Boghenbor K., Kapp N., Frey J., Stoffel M.H. Domain analysis of lipoprotein LppQ in Mycoplasma mycoides subsp. mycoides SC. Antonie Van Leeuwenhoek. 2008;93:175–183. doi: 10.1007/s10482-007-9191-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruderer U., Regalla J., Abdo E.-M., Huebschle O.J.B., Frey J. Serodiagnosis and monitoring of contagious bovine pleuropneumonia (CBPP) with an indirect ELISA based on the specific lipoprotein LppQ of Mycoplasma mycoides subsp. mycoides SC. Vet. Microbiol. 2002;84:195–205. doi: 10.1016/s0378-1135(01)00466-7. [DOI] [PubMed] [Google Scholar]
- Dedieu L., Mady V., Lefevre P.C. Development of a selective polymerase chain reaction assay for the detection of Mycoplasma mycoides subsp. mycoides SC (contagious bovine pleuropneumonia agent) Vet. Microbiol. 1994;42:327–339. doi: 10.1016/0378-1135(94)90064-7. [DOI] [PubMed] [Google Scholar]
- Dedieu L., Totte P., Rodrigues V., Vilei E.M., Frey J. Comparative analysis of four lipoproteins from Mycoplasma mycoides subsp. mycoides Small Colony identifies LppA as a major T-cell antigen. Comp. Immunol. Microbiol. Infect. Dis. 2009 doi: 10.1016/j.cimid.2008.08.011. [DOI] [PubMed] [Google Scholar]
- Fitzmaurice J., Sewell M., Manso-Silván L., Thiaucourt F., McDonald W.L., O'Keefe J.S. Real-time polymerase chain reaction assays for the detection of members of the Mycoplasma mycoides cluster. N. Z. Vet. J. 2008;56:40–47. doi: 10.1080/00480169.2008.36803. [DOI] [PubMed] [Google Scholar]
- Food and Agriculture Organization of the United Nations . Proceedings of the 3rd Meeting of the FAO-OIE-OAU/IBAR-IAEA Consultative Group on CBPP (Rome, 12–14 November 2003). Rome, Italy. 2004. Towards sustainable CBPP control programmes for Africa. [Google Scholar]
- Frey J., Cheng X., Kuhnert P., Nicolet J. Identification and characterization of IS1296 in Mycoplasma mycoides subsp. mycoides SC and presence in related mycoplasmas. Gene. 1995;160:95–100. doi: 10.1016/0378-1119(95)00195-c. [DOI] [PubMed] [Google Scholar]
- Gorton T.S., Barnett M.M., Gull T., French R.A., Lu Z., Kutish G.F., Adams L.G., Geary S.J. Development of real-time diagnostic assays specific for Mycoplasma mycoides subspecies mycoides Small Colony. Vet. Microbiol. 2005;111:51–58. doi: 10.1016/j.vetmic.2005.09.013. [DOI] [PubMed] [Google Scholar]
- Janis C., Bischof D., Gourgues G., Frey J., Blanchard A., Sirand-Pugnet P. Unmarked insertional mutagenesis in the bovine pathogen Mycoplasma mycoides subsp. mycoides SC: characterization of a lppQ mutant. Microbiology. 2008;154:2427–2436. doi: 10.1099/mic.0.2008/017640-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lorenzon S., Manso-Silván L., Thiaucourt F. Specific real-time PCR assays for the detection and quantification of Mycoplasma mycoides subsp. mycoides SC and Mycoplasma capricolum subsp. capripneumoniae. Mol. Cell Probes. 2008;22:324–328. doi: 10.1016/j.mcp.2008.07.003. [DOI] [PubMed] [Google Scholar]
- Manso-Silván L., Vilei E.M., Sachse K., Djordjevic S.P., Thiaucourt F., Frey J. Proposal to assign Mycoplasma leachii sp. nov. as a new species designation for Mycoplasma sp. bovine group 7 of Leach, and to reclassify Mycoplasma mycoides subsp. mycoides LC as a serovar of Mycoplasma mycoides subsp. capri. Int. J. Syst. Evol. Microbiol. 2009;59:1353–1358. doi: 10.1099/ijs.0.005546-0. [DOI] [PubMed] [Google Scholar]
- Mbulu R.S., Tjipura-Zaire G., Lelli R., Frey J., Pilo P., Vilei E.M., Mettler F., Nicholas R.A., Huebschle O.J. Contagious bovine pleuropneumonia (CBPP) caused by vaccine strain T1/44 of Mycoplasma mycoides subsp. mycoides SC. Vet. Microbiol. 2004;98:229–234. doi: 10.1016/j.vetmic.2003.11.007. [DOI] [PubMed] [Google Scholar]
- Miles K., Churchward C.P., McAuliffe L., Ayling R.D., Nicholas R.A. Identification and differentiation of European and African/Australian strains of Mycoplasma mycoides subspecies mycoides small-colony type using polymerase chain reaction analysis. J. Vet. Diagn. Invest. 2006;18:168–171. doi: 10.1177/104063870601800205. [DOI] [PubMed] [Google Scholar]
- Miltiadou D.R., Mather A., Vilei E.M., du Plessis D.H. Identification of genes coding for B cell antigens of Mycoplasma mycoides subsp. mycoides Small Colony (MmmSC) by using phage display. BMC Microbiol. 2009;9:215. doi: 10.1186/1471-2180-9-215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miserez R., Pilloud T., Cheng X., Nicolet J., Griot C., Frey J. Development of a sensitive nested PCR method for the specific detection of Mycoplasma mycoides subsp. mycoides SC. Mol. Cell Probes. 1997;11:103–111. doi: 10.1006/mcpr.1996.0088. [DOI] [PubMed] [Google Scholar]
- Nicholas R.A.J., Tjipura-Zaire G., Mbulu R.S., Scacchia M., Mettler F., Frey J., Abusugra I., Huebschle O.J.B. Proceedings of the 3rd Meeting of the FAO-OIE-OAU/IBAR-IAEA Consultative Group on CBPP. Towards Sustainable CBPP Control Programmes for Africa (Rome, 12–14 November 2003) FAO; Rome, Italy: 2004. An inactivated whole cell vaccine and LppQ subunit vaccine appear to exacerbate the effects of CBPP in adult cattle; pp. 91–97. [Google Scholar]
- Persson A., Pettersson B., Bolske G., Johansson K.E. Diagnosis of contagious bovine pleuropneumonia by PCR-laser-induced fluorescence and PCR-restriction endonuclease analysis based on the 16S rRNA genes of Mycoplasma mycoides subsp. mycoides SC. J. Clin. Microbiol. 1999;37:3815–3821. doi: 10.1128/jcm.37.12.3815-3821.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilo P., Martig S., Frey J., Vilei E.M. Antigenic and genetic characterisation of lipoprotein LppC from Mycoplasma mycoides subsp. mycoides SC. Vet. Res. 2003;34:761–775. doi: 10.1051/vetres:2003035. [DOI] [PubMed] [Google Scholar]
- Pilo P., Vilei E.M., Peterhans E., Bonvin-Klotz L., Stoffel M.H., Dobbelaere D., Frey J. A metabolic enzyme as a primary virulence factor of Mycoplasma mycoides subsp. mycoides Small Colony. J. Bacteriol. 2005;187:6824–6831. doi: 10.1128/JB.187.19.6824-6831.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilo P., Frey J., Vilei E.M. Molecular mechanisms of pathogenicity of Mycoplasma mycoides subsp. mycoides SC. Vet. J. 2007;174:513–521. doi: 10.1016/j.tvjl.2006.10.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tambi N.E., Maina W.O., Ndi C. An estimation of the economic impact of contagious bovine pleuropneumonia in Africa. Rev. Sci. Tech. 2006;25:999–1011. [PubMed] [Google Scholar]
- Thiaucourt F. Contagious bovine pleuropneumonia and vaccine strain T1/44. Vet. Rec. 2002;151:156. [PubMed] [Google Scholar]
- Thiaucourt F., Yaya A., Wesonga H., Huebschle O.J.B., Tulasne J.J., Provost A. Contagious bovine pleuropneumonia: a reassessment of the efficacy of vaccines used in Africa. Ann. N. Y. Acad. Sci. 2000;916:71–80. doi: 10.1111/j.1749-6632.2000.tb05276.x. [DOI] [PubMed] [Google Scholar]
- Thiaucourt F., Dedieu L., Maillard J.C., Bonnet P., Lesnoff M., Laval G., Provost A. Contagious bovine pleuropneumonia vaccines, historic highlights, present situation and hopes. Dev. Biol. (Basel) 2003;114:147–160. [PubMed] [Google Scholar]
- Vilei E.M., Frey J. Genetic and biochemical characterization of glycerol uptake in Mycoplasma mycoides subsp. mycoides SC: its impact on H2O2 production and virulence. Clin. Diagn. Lab. Immunol. 2001;8:85–92. doi: 10.1128/CDLI.8.1.85-92.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vilei E.M., Frey J. Differential clustering of Mycoplasma mycoides subsp. mycoides SC strains by PCR-REA of the bgl locus. Vet. Microbiol. 2004;100:283–288. doi: 10.1016/j.vetmic.2004.02.005. [DOI] [PubMed] [Google Scholar]
- Vilei E.M., Nicolet J., Frey J. IS1634, a novel insertion element creating long, variable-length direct repeats which is specific for Mycoplasma mycoides subsp. mycoides small-colony type. J. Bacteriol. 1999;181:1319–1323. doi: 10.1128/jb.181.4.1319-1323.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vilei E.M., Abdo E.-M., Nicolet J., Botelho A., Gonçalves R., Frey J. Genomic and antigenic differences between the European and African/Australian clusters of Mycoplasma mycoides subsp. mycoides SC. Microbiology. 2000;146:477–486. doi: 10.1099/00221287-146-2-477. [DOI] [PubMed] [Google Scholar]
- Vilei E.M., Correia I., Ferronha M.H., Bischof D.F., Frey J. β-D-Glucoside utilization by Mycoplasma mycoides subsp. mycoides SC: possible involvement in the control of cytotoxicity towards bovine lung cells. BMC Microbiol. 2007;7:31. doi: 10.1186/1471-2180-7-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wesonga H., Manso-Silván L., Thiaucourt F. Proceedings of the 3rd Meeting of the FAO/OIE/OAU-IBAR/IAEA Consultative Group in CBPP in Africa. Rome, November 12–14, 2003. FAO Publications Rome; Rome: 2003. CBPP vaccine strain T1/44: possible reversion to virulence. [Google Scholar]
- Westberg J., Persson A., Holmberg A., Goesmann A., Lundeberg J., Johansson K.E., Pettersson B., Uhlen M. The genome sequence of Mycoplasma mycoides subsp. mycoides SC type strain PG1T, the causative agent of contagious bovine pleuropneumonia (CBPP) Genome Res. 2004;14:221–227. doi: 10.1101/gr.1673304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Windsor R.S. The eradication of contagious bovine pleuropneumonia from south western Africa. A plan for action. Ann. N. Y. Acad. Sci. 2000;916:326–332. doi: 10.1111/j.1749-6632.2000.tb05309.x. [DOI] [PubMed] [Google Scholar]