Abstract
Objective
To assess equity in health outcomes and interventions for maternal and child health (MCH) services in Thailand.
Methods
Women of reproductive age in 40 000 nationally representative households responded to the Multiple Indicator Cluster Survey in 2005–2006. We used a concentration index (CI) to assess distribution of nine MCH indicator groups across the household wealth index. For each indicator we also compared the richest and poorest quintiles or deciles, urban and rural domiciles, and mothers or caregivers with or without secondary school education.
Findings
Child underweight (CI: −0.2192; P < 0.01) and stunting (CI: −0.1767; P < 0.01) were least equitably distributed, being disproportionately concentrated among the poor; these were followed by teenage pregnancy (CI: −0.1073; P < 0.01), and child pneumonia (CI: −0.0896; P < 0.05) and diarrhoea (CI: −0.0531; P < 0.1). Distribution of the MCH interventions was fairly equitable, but richer women were more likely to receive prenatal care and delivery by a skilled health worker or in a health facility. The most equitably distributed interventions were child immunization and family planning. All undesirable health outcomes were more prevalent among rural residents, although the urban–rural gap in MCH services was small. Where mothers or caregivers had no formal education, all outcome indicators were worse than in the group with the highest level of education.
Conclusion
Equity of coverage in key MCH services is high throughout Thailand. Inequitable health outcomes are largely due to socioeconomic factors, especially differences in the educational level of mothers or caregivers.
ملخص
الغرض
تقدير مدى العدالة في النتائج الصحية ومداخلات الخدمات الصحية للأم والطفل في تايلاند.
الطريقة
ما بين العامين 2005 و2006 استجابت النساء في سن الإنجاب ضمن 40000 عائلة ممثلة على الصعيد الوطني للمسح العنقودي المتعدد المؤشرات. وقد استخدم الباحثون منسب التركيز لقياس توزيع تسع مجموعات من مؤشرات صحة الأم والطفل مقارنة بمنسب الثروة العائلية. وقارن الباحثون أيضا لكل مؤشر بين أغنى وأفقر شريحتين خمسيتين وعُشريتين، وبين المنازل الحضرية والريفية، وبين الأمهات أو مقدمات الرعاية سواء من حصلن منهن على التعليم الثانوي أو عدمه.
الموجودات
كان الوزن المنخفض للطفل (منسب التركيز: −0.2192؛ وقوة الاحتمال P أقل من 0.01) والتقزم (منسب التركيز: −0.1767؛ وقوة الاحتمال P أقل من 0.01) هما الأقل عدالة في التوزع، حيث تركزا بصورة غير متكافئة بين الفقراء، وتلاهما الحمل في سن المراهقة (منسب التركيز: −0.1073؛ وقوة الاحتمال P أقل من 0.01)، والالتهاب الرئوي في الأطفال (منسب التركيز: −0.0896؛ وقوة الاحتمال P أقل من 0.05)، والإسهال (منسب التركيز: −0.0531؛ وقوة الاحتمال P أقل من 0.01). أما توزع مداخلات صحة الأم والطفل فكانت متساوية تقريباً، غير أن النساء الثريات كن أكثر تمتعاً بإمكانية الحصول على الرعاية السابقة للولادة والولادة تحت إشراف عامل صحي متمرس أو الولادة في أحد المرافق الصحية. أما أكثر المداخلات عدلاً في التوزع فتمثلت في تمنيع الأطفال وتنظيم الأسرة. وكانت جميع النتائج الصحية غير المرغوبة أكثر انتشاراً بين قاطني المناطق الريفية على الرغم من ضآلة الفجوة بين المناطق الحضرية والمناطق الريفية في ما يتعلق بخدمات رعاية صحة الأم والطفل. وكانت مؤشرات النتائج أسوأ مع عدم حصول الأمهات أو مقدمات الرعاية على أية تعليم رسمي مقارنة بمن حصلن على أعلى مستويات التعليم.
الاستنتاج
عدالة التغطية بخدمات رعاية صحة الأم والطفل الرئيسية على مستوى عال في تايلاند. وتعزى النتائج الصحية غير العادلة، بدرجة كبيرة، إلى عوامل اجتماعية واقتصادية، ولاسيما الاختلافات في مستوى تعليم الأمهات ومقدمات الرعاية.
Résumé
Objectif
Évaluer l'équité en termes d'évènements et d'interventions sanitaires faisant intervenir les services de santé maternelle et de l'enfant (MCH) en Thaïlande.
Méthodes
Des femmes en âge de procréer appartenant à 40 000 ménages représentatifs au plan national ont répondu à une enquête en grappes à indicateurs multiples sur la période 2005–2006. Nous avons utilisé l'indice de concentration (IC) pour évaluer la distribution de neuf groupes d'indicateurs concernant les services MCH en fonction de l'indice de richesse des ménages. Pour chaque indicateur, nous avons aussi effectué des comparaisons entre le quintile ou le décile le plus riche et le plus pauvre, entre origine urbaine et rurale et entre mères ou personnes s'occupant des enfants ayant reçu ou n'ayant pas reçu une éducation secondaire.
Résultats
C'étaient le déficit pondéral (IC: −0,2192 ; p < 0,01) et le retard de croissance (IC: −0,1767 ; p < 0,01) qui présentaient la distribution la moins équitable, avec une concentration disproportionnée chez les plus démunis ; venaient ensuite les grossesses à l'adolescence (IC: −0,1073 ; p < 0,01), la pneumonie infanto-juvénile (IC: −0,0896 ; p < 0,05) et la diarrhée (IC: −0,0531 ; p < 0,1). La distribution des interventions des MCH était plutôt équitable, mais les femmes riches avaient une plus grande probabilité de bénéficier de soins prénatals et d'un accouchement assisté par du personnel médical qualifié ou dans un établissement de soins. Les interventions les plus équitablement distribuées étaient la vaccination infantile et la planification familiale. Dans leur ensemble, les événements sanitaires indésirables présentaient une plus forte prévalence chez les ruraux, même si l'écart rural-urbain était faible dans le cas des services MCH. Lorsque la mère ou la personne s'occupant de l'enfant n'avait reçu aucune éducation formelle, tous les indicateurs d'événements étaient moins bons que dans le groupe disposant d'un plus haut niveau d'éducation.
Conclusion
En matière de couverture par les services MCH essentiels, un haut niveau d'équité est atteint dans l'ensemble de la Thaïlande. Les événements sanitaires indésirables sont largement dus à des facteurs socioéconomiques et notamment aux différences dans le niveau d'éducation des mères ou des personnes s'occupant des enfants.
Resumen
Objetivo
Evaluar la equidad en materia de resultados e intervenciones sanitarias de salud maternoinfantil (SMI) en Tailandia.
Métodos
Mujeres en edad fecunda de 40 000 hogares representativos a nivel nacional respondieron a la Encuesta de Indicadores Múltiples por Conglomerados de 2005-2006. Usamos un índice de concentración (IC) para evaluar la distribución de nueve grupos de indicadores de la salud maternoinfantil en un gradiente del índice de riqueza de los hogares. Para cada indicador comparamos también los quintiles o deciles más rico y más pobre, los hogares urbanos y rurales, y las madres o cuidadores con o sin educación secundaria.
Resultados
La insuficiencia ponderal (IC: 0,2192; P < 0,01) y el retraso del crecimiento (IC: 0,1767; P < 0,01) infantiles fueron los problemas distribuidos menos equitativamente, pues se concentraban de manera desproporcionada entre los pobres; les siguieron el embarazo en la adolescencia (IC: 0,1073, P < 0,01), y la neumonía (IC: 0,0896, P < 0,05) y la diarrea (IC: 0,0531, P < 0,1) infantiles. La distribución de las intervenciones de salud maternoinfantil fue bastante equitativa, pero las mujeres más ricas tenían más probabilidades de recibir atención prenatal y, en el momento del parto, atención especializada o en un centro de salud. Las intervenciones distribuidas de forma más equitativa fueron la inmunización infantil y la planificación familiar. Todos los resultados sanitarios desfavorables fueron más frecuentes en las zonas rurales, si bien la brecha urbano-rural en los servicios de salud maternoinfantil era pequeña. Entre las madres y los cuidadores sin estudios, todos los indicadores de resultados fueron peores que en el grupo con mayor nivel de educación.
Conclusión
Se observa en toda Tailandia una alta equidad en materia de cobertura de los principales servicios de salud maternoinfantil. Los resultados sanitarios no equitativos se deben en gran medida a factores socioeconómicos, en particular al diferente nivel educativo de las madres y los cuidadores.
Introduction
Globally, half a million women die each year during pregnancy and delivery, and 10 million children aged under five years die, mainly due to limited access to basic but effective health interventions.1 Achieving the United Nations Millennium Development Goal for maternal and child health (MCH) requires strong health systems.2 The strength of a country’s health system is reflected in the distribution of health outcomes.3
Universal social protection and equity from birth are part of a new agenda for global health equity.4 Ensuring that key health interventions are widely and equitably available is critical for improved child survival.5 For example, many studies have found that women who are better off economically have greater access to a skilled birth attendant.6,7 In Thailand, universal health coverage was achieved in 2002, and the health system is seen as equitable.8 The scheme is financed through taxation in such a way that those on higher incomes pay more than those on lower incomes.9 Ambulatory and hospital care are available to the poor through a geographically widespread network of district-level government health facilities.10 Few households become impoverished through health care costs because the health service is comprehensive and free of charge at the point of service.11 This progressive financing model, in addition to the equitable use of health services and public spending on health, have made Thailand one of the best performers in the Asia–Pacific region.12–15 Equity in the Thai health systems has been attributed to the extension of health facilities and human resources over the past three decades16 and to the policy transition from “piecemeal targeting” to an approach that focuses on universality.17
Among 30 low- and middle-income countries, Thailand has been one of the most effective countries in reducing mortality in children under five.18 For example, the mortality rate fell from 58 per 1000 live births in 1980 to 30 in 1990 and to 23 in 2000.19 The improvement in child survival has been accompanied by a remarkably small disparity between rich and poor.20
This study of MCH equity in Thailand is the first to make use of a nationally representative household survey. The study assesses equity in health service use and for all key MCH outcomes. For example, it includes child malnourishment because it is an underlying cause of death associated with infectious diseases, and diarrhoea and pneumonia because they are the diseases most often associated with child deaths.21
Methods
Data sources
Data were obtained from the Multiple Indicator Cluster Survey, which was conducted by the National Statistical Office of Thailand from December 2005 to February 2006. The survey used structured, face-to-face interviews with women of reproductive age (15–49 years) in all provinces, and anthropometric measurement of children less than 5 years of age. An original sample of 43 440 nationally representative households was selected using a two-stage, stratified sampling technique. In this sample, 40 511 (or 93.3%) responded to the survey.
Indicators
Nine groups of MCH indicators were used as measures of health outcomes and coverage of health care interventions. The maternal health indicator was teenage pregnancy; this was applied to the 12 million women in Thailand aged 15–49 years who had given birth before the survey started. The coverage of maternal health indicators were family planning, prenatal care and delivery by a skilled health worker, and delivery in a health facility. The family planning indicator targeted the approximately 13 million women married to or living with their male partners and not pregnant; and the prenatal and delivery indicators targeted the 2 million mothers who had given birth during the previous two years.
Child health indicators were low birth weight, moderate-to-severe child malnourishment and childhood illnesses. Low birth weight, defined as a weight of < 2.5 kg at birth, was assessed for the children of mothers who had given birth in the previous two years (i.e. 2 million mothers). Malnourishment in children was indicated by underweight, stunting (chronic malnutrition) and wasting (acute malnutrition), based on United States National Center for Health Statistics and World Health Organization standards. Child illnesses were diarrhoea and suspected pneumonia, both very common. Child malnourishment and illnesses were counted directly for those less than 5 years of age (estimated at 5 million).
Coverage of child health indicators were treatment for child illness (diarrhoea and suspected pneumonia) and child immunization. For the latter, the target population was children aged 12–23 months (estimated at 1 million) who had received the following before they reached the age of 1 year: one dose of bacille Calmette–Guérin (BCG) vaccine and of vaccine against measles, mumps and rubella (MMR); three doses of oral polio vaccine (OPV) and of vaccine against diphtheria, pertussis (whooping cough) and tetanus (DPT); and one dose of hepatitis B vaccine.
Equity stratifiers and measures
To assess wealth, we used the presence (or absence) of selected assets and durables in a sample household, because asset ownership tends to fluctuate less than individual income or expenditure. The assets we considered in houses were permanent floors, roofs or walls; flush or pour-flush toilets; transportation, including bicycles, motorcycles, cars or trucks; and electrical equipment, including radios, televisions, line or mobile telephones, refrigerators and computers. Households with these assets were considered richer than those without. We used principal component analysis of all household samples to generate a wealth index for each household, and we used this as an equity stratifier.
Using a standard method, we summarized the distribution of each MCH indicator over a gradient of the wealth index by a concentration index (CI) and a concentration curve (CC).22 The CI, which ranges from −1.0 to +1.0, captures the extent to which health outcomes and service use are concentrated among different population groups (in this case, the richest and the poorest). A CI of zero means an equal distribution of a particular indicator throughout the economic gradients. A negative CI indicates a concentration among those who are poorer (i.e. the CC lies above the equality line of 45 degrees), and a positive CI reflects a concentration among those who are richer (i.e. the CC lies below the equality line).
We compared the prevalence of health outcomes and the coverage of the MCH interventions between the richest and the poorest subgroups using a risk ratio (RR). All households were ranked according to their wealth indices, which were divided equally into quintile (5) and decile (10) subgroups. Only the top (richest) and bottom (poorest) quintiles and deciles were selected for the RR calculation, to demonstrate any disparity between rich and poor. We also used ratio analysis to compare urban with rural domiciles, and mothers or caregivers educated beyond secondary school level with those lacking formal education.
Based on the results of the analyses, we estimated figures for the population of Thailand using the individual household members’ sampling weights provided by the National Statistical Office.
Results
Table 1 summarizes the definition and number of the samples surveyed for each indicator, and the eligible estimated population in each case. Table 2 summarizes equity measures for all MCH indicators in terms of CI and RR between the richest and poorest quintiles and deciles.
Table 1. Definition and number of surveyed samples and estimated population for each indicator of maternal and child health, Thailand, 2005–2006.
| MCH indicator | Definitiona | Eligible populationb | No. of samples (no. of estimated populationc) |
|---|---|---|---|
| I. Maternal health | |||
| Outcome indicator | |||
| 1. Teenage pregnancy | First pregnancy at age under 20 years | Women aged 15–49 years, having given birth | 24 018 (11 950 095) |
| Coverage indicator | |||
| 2. Family planning | Use of modern contraceptive methods including sterilization, pill, injection, implantation, IUD and condom | Women 15–49 years, married to or living with male partner and not known to be pregnant | 26 119 (13 079 990) |
| 3. Prenatal care | Pregnancy cared for by physicians, nurses, midwives or auxiliary midwives | Women 15–49 years, giving birth during the previous 2 years |
3 365 (1 848 734) |
| 4. Delivery care |
4.1 Delivery by physicians, nurses, midwives or auxiliary midwives | ||
| 4.2 Delivery in subdistrict health centres; district, provincial and teaching hospitals; and private health facilities | |||
| II. Child health | |||
| Outcome indicator | |||
| 5. Low birth weight | Babies born with weight below 2.5 kg | Women 15–49 years, giving birth during the previous 2 years | 3 365 (1 848 734) |
| 6. Child moderate-to-severe malnourishment | 6.1 Weight below 2 SD of the mean for the same age (underweight) 6.2 Height below 2 SD of the mean for the same age (stunting) 6.3 Weight below 2 SD of the mean for the same height (wasting) |
Children 0–59 months successfully measured for weight and height | 8 993 (4 632 238) |
| 7. Child illness | 7.1 Mothers or caregivers reporting diarrhoea in the last 2 weeks 7.2 Mothers or caregivers reporting cough with difficulty in breathing and tightness in the chest (suspected pneumonia) in the last 2 weeks |
Children 0–59 months | 9 409 (4 837 701) |
| Coverage indicator | |||
| 8. Treatment for child illness | 8.1 Receiving ORS/ORT | 8.1 Children 0–59 months with diarrhoea | 767 (419 756) |
| 8.2 Receiving advice/treatment from public and private health providers | 8.2 Children 0–59 months with suspected pneumonia | 379 (219 ) | |
| 9. Child immunization | Receiving one dose of BCG vaccine and MMR vaccine, and three doses of OPV, DPT vaccine and HBV vaccine in their first year of life | Children 12–23 months | 1 932 (974 880) |
BCG, bacille Calmette–Guérin; DPT, diphtheria, pertussis (whooping cough) and tetanus; HBV, hepatitis B virus; IUD, intrauterine device; MCH, maternal and child health; MMR, measles, mumps and rubella; OPV, oral polio vaccine; ORS/ORT, oral rehydration salts/oral rehydration therapy; SD, standard deviation.
a The numerator for calculating the prevalence or coverage for MCH indicator.
b The denominator for calculating the prevalence or coverage for MCH indicator.
c For the whole country, based on individual household members’ weights of the surveyed samples.
Table 2. Concentration index and ratio of richest to poorest quintile or decile for each indicator of maternal and child health, Thailand, 2005–2006.
| MCH indicator | CI | RR(quintile 5: quintile 1)a | RR(decile 10: decile 1)b |
|---|---|---|---|
| I. Maternal health | |||
| Outcome indicator | |||
| 1. Teenage pregnancy | −0.1073*** | 0.51*** | 0.42*** |
| Coverage indicator | |||
| 2. Family planning | −0.0005 | 0.99*** | 1.07*** |
| 3. Prenatal care by skilled health worker | 0.0078*** | 1.05*** | 1.08*** |
| 4. Delivery care | |||
| By skilled health worker | 0.0172*** | 1.10*** | 1.16*** |
| In health facility |
0.0173*** |
1.10*** |
1.15*** |
| II. Child health | |||
| Outcome indicator | |||
| 5. Low birth weight | 0.0367 | 0.92*** | 0.91*** |
| 6. Child malnourishment | |||
| Underweight | −0.2192*** | 0.24*** | 0.28*** |
| Stunting | −0.1767*** | 0.34*** | 0.21*** |
| Wasting | −0.0655 | 0.79*** | 0.88*** |
| 7. Child illness | |||
| Diarrhoea | −0.0531* | 0.65*** | 0.53*** |
| Suspected pneumonia | −0.0896** | 0.60*** | 0.60*** |
| Coverage indicator | |||
| 8. Child illness treatment | |||
| ORS/ORT for diarrhoea | 0.0220 | 1.22*** | 1.30*** |
| Appropriate provider for pneumonia | −0.0164 | 0.92*** | 0.72*** |
| 9. Child immunization | |||
| BCG | −0.0104 | 0.94*** | 0.93*** |
| MMR | −0.0041 | 0.91*** | 0.89*** |
| OPV | 0.0002 | 0.99*** | 1.02*** |
| DPT | 0.0002 | 0.99*** | 1.02*** |
| HBV | −0.0052 | 0.97*** | 1.03*** |
* P < 0.1; ** P < 0.05; *** P < 0.01.
BCG, bacille Calmette–Guérin; CI, concentration index; DPT, diphtheria, pertussis (whooping cough) and tetanus; HBV, hepatitis B virus; MCH, maternal and child health; MMR, measles, mumps and rubella; OPV, oral polio vaccine; ORS/ORT, oral rehydration salts/oral rehydration therapy; RR, risk ratio.
a Quintile 5 is the richest; quintile 1 is the poorest.
b Decile 10 is the richest; decile 1 is the poorest.
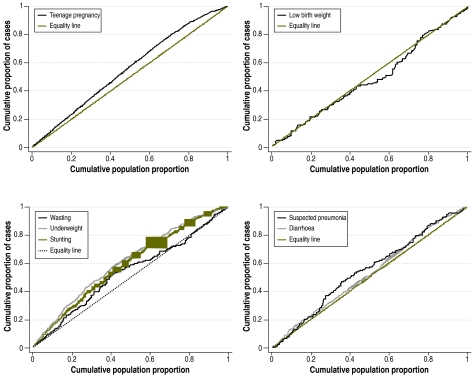
Economic inequity in health outcomes
Economic inequity in MCH was apparent in teenage pregnancy, low birth weight, child malnourishment and child illness (Fig. 1). These undesirable health outcomes were concentrated in the poorer subgroups (as shown by the negative CIs in Table 2). Concentration among the poor was greatest and was statistical significant for child underweight and stunting. The CI of child wasting was negative, but this had no statistical significance. Teenage pregnancy ranked third in magnitude of concentration among the poor. Suspected pneumonia and diarrhoea in children less than 5 years of age were also more concentrated among the poor (Table 2).
Fig. 1.
Concentration curves for teenage pregnancy, low birth weight, child malnourishment and child illness, Thailand, 2005–2006
In comparing MCH outcomes between the top and bottom wealth quintiles, RRs were consistent with the computed CI. Teenage pregnancy, child underweight, and reported diarrhoea and suspected pneumonia were more concentrated in the poorer than in the richer households. The RR between the top and bottom quintiles ranged from 0.24 for child underweight to 0.79 for child wasting (Table 2).
Economic disparity in low birth weight was less clear. The positive CI reflected its concentration among relatively rich households, but without statistical significance. Also, the corresponding CC in Fig. 1 shows that the concentration occurred mainly in the third and fourth wealthiest quintiles, which were not particularly rich in absolute terms.
Economic inequity in service coverage
The key interventions for MCH were more uniformly distributed across economic strata than were the health outcomes (Table 2).
For the maternal care interventions, prenatal and delivery care either by a skilled health worker or in a health facility showed a statistically significant concentration among the rich. However, the magnitude of the CI was modest and the RR between the richest and the poorest groups was close to one, indicating a negligible gap between rich and poor.
Coverage with oral rehydration salts/oral rehydration therapy for diarrhoea was greatest in the richest quintile and decile. In contrast, coverage with appropriate health-care providers for suspected pneumonia was greatest in the poorest quintile and decile.
Table 2 shows that, for childhood immunization coverage, the CI of the five vaccine types ranged from −0.0104 to 0.0002, and that the CI for family planning (at −0.0005) was not statistically different from zero. Thus, there was almost equitable service coverage for these indicators. Results on RR for these indicators were mixed (Table 2); all were less than one for comparison between the first and fifth quintiles, and two of the six were less than one between the first and fifth deciles, with the remaining four slightly positive.
Geographic disparity of MCH
Health outcome prevalences were as follows: teenage pregnancy among all mothers, 37.3%; low birth weight, 8.3%; and child stunting, 11.9% (Table 3). Service coverage was more equitable; for example, on average, more than 97% of respondents had prenatal care delivered either by skilled health workers or in health facilities, and more than 90% of children had received all vaccinations except the one against hepatitis B virus.
Table 3. Prevalence, service coverage and risk ratio with respect to urban–rural areas and educational attainment, Thailand, 2005–2006.
| MCH indicator | Average prevalence or coverage(%) | RR between urban and rural areas | RR between higher and no formal education a |
|---|---|---|---|
| I. Maternal health | |||
| Outcome indicator | |||
| 1. Teenage pregnancy | 37.3 | 0.76*** | 0.10*** |
| Coverage indicator | |||
| 2. Family planning | 72.6 | 0.92*** | 1.10*** |
| 3. Prenatal care by skilled health worker | 97.8 | 1.0006** | 1.10*** |
| 4. Delivery care | |||
| By skilled health worker | 97.3 | 1.03*** | 1.23*** |
| In health facility |
96.8 |
1.04*** |
1.28*** |
| II. Child health | |||
| Outcome indicator | |||
| 5. Low birth weight | 8.3 | 1.15*** | 0.91*** |
| 6. Child malnourishment | |||
| Underweight | 9.3 | 0.52*** | 0.29*** |
| Stunting | 11.9 | 0.66*** | 0.39*** |
| Wasting | 4.1 | 0.92*** | 0.52*** |
| 7. Child illness | |||
| Diarrhoea | 8.7 | 0.90*** | 0.62*** |
| Suspected pneumonia | 4.6 | 0.62*** | 0.93*** |
| Coverage indicator | |||
| 8. Child illness treatment | |||
| ORS/ORT for diarrhoea | 68.3 | 0.91*** | 1.05*** |
| Appropriate provider for pneumonia | 84.7 | 0.93*** | 0.91*** |
| 9. Child immunization | |||
| BCG | 98.0 | 0.94*** | 0.92*** |
| MMR | 91.4 | 0.90*** | 1.00 |
| OPV | 91.5 | 0.94*** | 0.95*** |
| DPT | 91.4 | 0.94*** | 0.95*** |
| HBV | 85.7 | 0.97*** | 0.91*** |
** P < 0.05; *** P < 0.01.
BCG, bacille Calmette–Guérin; DPT, diptheria, pertussis (whooping cough) and tetanus; HBV, hepatitis B virus; MMR, measles, mumps and rubella; OPV, oral polio vaccine; ORS/ORT, oral rehydration salts/oral rehydration therapy; RR, risk ratio.
a Higher education refers to schooling beyond the secondary level.
Table 3 also summarizes the urban–rural and educational disparity in MCH, as reflected by the RR. Except for low birth weight, all undesirable MCH indicators were more concentrated in rural than in urban areas. The most profound health gap was child underweight, which was 48% more prevalent in rural than in urban areas. Child wasting and reported diarrhoea had the narrowest urban–rural disparity. In contrast, low birth weight was more prevalent in urban than in rural areas by 15%.
The urban–rural gap for MCH service coverage was small. Women living in urban areas were up to 4% more likely than those in rural areas to receive prenatal and delivery care from a skilled health worker, and delivery in a health facility. Although overall coverage at the national level of these recommended maternal care indicators was high (> 95%), the lowest coverage was in the southern region of Thailand, especially in the three southernmost provinces, where the population is mainly Muslim (data not shown). Coverage of family planning by modern methods in the southern region was only 60%, lower than the national average of 73%. In contrast, coverage of family planning and all types of child immunization was greater in rural areas (Table 3). Notably, immunization coverage in Bangkok was lower than in all other regions (data not shown).
Educational disparity and MCH inequity
Formal education of the mother or caregiver of children is a major determinant of MCH inequity; those who were more educated fared better on all outcome indicators. The difference was most striking for teenage pregnancy. Uneducated women (3% of the 12 million mothers) were 90% more likely than those educated beyond secondary school (10% of the 12 million mothers) to have their first pregnancy before the age of 20 years.
Children who were underweight, stunted or wasted were more likely (71%, 61% and 48%, respectively) to have mothers or caregivers with no formal education (4% of 5 million children) than with education beyond secondary school (12% of 5 million children). Educational inequity among mothers of children who were ill or had low birth weight was small, but these indicators were still more prevalent in the subgroup with mothers or caregivers lacking education (Table 3).
Women who were educated beyond secondary school were 10–28% more likely than those without any formal education to receive family planning, prenatal care and delivery by a skilled health worker or in a health facility. There was also a consistent increase in maternal care coverage with higher educational attainment, with a significantly sharp difference (RR: 1.1–1.28; P < 0.01) noted between the uneducated and those who had completed primary school (data not shown). Surprisingly, children born to mothers or cared for by someone who had been educated beyond the secondary level were 5–9% less likely than those not in this subgroup to receive all types of vaccination (except MMR vaccine) before the first year of age. The coverage for all five vaccines in the subgroup educated beyond the secondary level was also lower than in two other subgroups: those educated to the primary and secondary levels (data not shown).
Discussion
A clear policy message emerges from this study – universal access to health care is fundamental to achieving the goal of health equity. In Thailand, child immunization was distributed uniformly over the economic gradient of mothers or caregivers. Surprisingly, immunization coverage in rural areas and in the children whose mothers or caregivers had no formal education was slightly higher than in urban areas and in those educated beyond secondary school. These findings suggest that better service coverage is provided in rural areas (mainly by district health systems) than in urban areas. In spite of a positive CI, coverage of maternal care by skilled health workers in Thailand is not as concentrated among the rich as it is in other developing countries under the Demographic and Health Survey (DHS) programme (for prenatal care, Thailand has a CI of 0.0078, compared to 0.1095 for DHS; for delivery, Thailand has a CI of 0.0172, compared to 0.2747 for DHS).23
The relatively equitable distribution of MCH service coverage in Thailand – between rich and poor, urban and rural – can be explained by government commitment to investment in health infrastructure and expansion of health insurance coverage over the past three decades.24 The country’s well functioning primary health-care service is facilitated by the government’s pro-rural policy of mandatory public service by all medical, pharmacist, dentist and nurse graduates at the district level, as well as by other paramedics at subdistrict levels.17 The geographic coverage of district hospitals and subdistrict health centres has continued to expand over the past three decades. District health systems, including hospitals and health centres, are at the forefront in providing a comprehensive range of curative, preventative and health-promotion services, including MCH.16.This in-country study supports findings from cross-country analyses that have found a negative correlation between the overall level of MCH interventions and the rich–poor gap in such coverage,7 and a strong positive association between health-worker density and child immunization coverage.25
However, some disparity in child health outcomes is still noticeable between rich and poor, and between urban and rural areas in Thailand. For example, the country’s CIs for diarrhoea, malnourishment, underweight and stunting are comparable to those of the DHS for developing countries.23
Education is one of the most important social determinants of health inequity. This study found that education gaps for the indicators of teenage pregnancy and child malnourishment were much larger than those for the urban–rural differential. Prevalence of teenage pregnancy and child malnourishment decreased as the formal education level of the mother or caregiver increased (data not shown). In particular, the prevalence of teenage pregnancy dropped sharply among those educated beyond the secondary level. It is clear from this and other studies that maternal education is a vital part of policies to improve MCH.
In the context of universal health coverage, access to MCH services is fairly equitable in Thailand. The remaining challenge is inequity in health outcomes, for which social determinants (e.g. poverty, maternal education and other structural social inequities) are important, although they are often outside the mandate of the health sector. The overall prevalence of child underweight, stunting and wasting in this study was 9%, 12% and 4%, respectively. Wasting in children indicates acute malnutrition and stunting indicates chronic malnutrition, which is generally a result of chronic household poverty. Policies should address inequity from birth; they should, for example, tackle issues such as low birth weight, teenage pregnancy and child malnutrition, for which the Commission on Social Determinants of Health recommends multisectoral actions.4 Inequity at birth has long-term negative implications; undernutrition, for instance, is associated with a decrease in human capital (i.e. the skills and knowledge that enable people to work and thus produce economic value).26
A limitation of this study is its cross-sectional nature. Time trend information could not be extracted from the data because the Multiple Indicator Cluster Survey 2006 was the first survey wave in Thailand. A sample size of over 40 000 representative households is adequate when compared to numbers used in typical surveys conducted in Thailand by the National Statistical Office. A strength of this study is the application of a wealth index, which better reflects a household’s economic status than personal income and is easier and quicker to assess.
Conclusion
Universal health coverage in Thailand has resulted in a fairly equitable distribution of MCH services. Major challenges remain in connection with inequity in health outcomes, particularly in the areas of teenage pregnancy and child malnourishment. The gaps between rich and poor and between urban and rural areas reveal a similar pattern. Maternal education is the main determinant of health inequity. Key policy leverage and multisectoral actions will be required to close the gap.4
Acknowledgements
We acknowledge a genuine partnership between Thailand’s National Statistical Office and Ministry of Public Health in past decades. A constructive engagement between the two constituencies has produced a strong foundation for evidence-based policy decisions. This study was made possible by permission from the National Statistical Office to use the 2006 Multiple Indicator Cluster Survey data set.
Funding:
The United Nations Children’s Fund (UNICEF) provides technical and financial support to the National Statistical Office for the Multiple Indicator Cluster Survey. No funding support was received for this study.
Competing interests:
None declared.
References
- 1.The world health report 2005: make every mother and child count Geneva: World Health Organization; 2005. [DOI] [PubMed] [Google Scholar]
- 2.Wagstaff A, Claeson M. The Millennium Development Goals for health: rising to the challenges Washington, DC: The World Bank; 2004. [Google Scholar]
- 3.The world health report 2000: health systems: improving performance Geneva: World Health Organization; 2000. [Google Scholar]
- 4.Closing the gap in a generation: health equity through action on the social determinants of health. Final report of the Commission on Social Determinants of Health Geneva: World Health Organization; 2008. [DOI] [PubMed] [Google Scholar]
- 5.Bryce J, Arifeen S, Pariyo G, Lanata CF, Gwatkin D, Habicht JP, The Multi-country Evaluation of IMCI Study Group Reducing child mortality: can public health deliver? Lancet. 2003;362:159–64. doi: 10.1016/S0140-6736(03)13870-6. [DOI] [PubMed] [Google Scholar]
- 6.Say L, Raine R. A systematic review of inequalities in the use of maternal health care in developing countries: examining the scale of the problem and the importance of context. Bull World Health Organ. 2007;85:812–9. doi: 10.2471/BLT.06.035659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Houweling TAJ, Ronsmans C, Campbell OMR, Kunst AE. Huge poor-rich inequalities in maternity care: an international comparative study of maternity and child care in developing countries. Bull World Health Organ. 2007;85:745–54. doi: 10.2471/BLT.06.038588. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Limwattananon S, Tangcharoensathien V, Prakongsai P. Equity in financing healthcare: impact of universal access to healthcare in Thailand May 2005. (EQUITAP project working paper 16). Available from: http://www.equitap.org [accessed 19 April 2009].
- 9.Prakongsai P, Tangcharoensathien V, Limwattananon S. Equity in health care finance and financial risk protection prior to and after universal coverage in Thailand. Presented at the: International Society for Pharmacoeconomics and Outcomes Research Thailand Annual Conference, Bangkok, Thailand, 2008 [Google Scholar]
- 10.Prakongsai P, Limwattananon S, Tangcharoensathien V. Integrating financing schemes to achieve universal coverage in Thailand: analysis of the equity achievements. Presented at the: 7th World Congress of Health Economics, Beijing, China, 2009 [Google Scholar]
- 11.Limwattananon S, Tangcharoensathien V, Prakongsai P. Catastrophic and poverty impacts of health payments: Results from national household surveys in Thailand. Bull World Health Organ. 2007;85:600–6. doi: 10.2471/BLT.06.033720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.O’Donnell O, van Doorslaer E, Rannan-Eliya RP, Somanathan A, Adhikari SR, Harbianto D, et al. The incidence of public spending on healthcare: Comparative evidence from Asia. World Bank Econ Rev. 2007;21:93–123. doi: 10.1093/wber/lhl009. [DOI] [Google Scholar]
- 13.O’Donnell O, van Doorslaer E, Rannan-Eliya RP, Somanathan A, Adhikari SR, Akkazieva B, et al. Who pays for health care in Asia? J Health Econ. 2008;27:460–75. doi: 10.1016/j.jhealeco.2007.08.005. [DOI] [PubMed] [Google Scholar]
- 14.van Doorslaer E, O’Donnell O, Rannan-Eliya RP, Somanathan A, Adhikari SR, Garg CC, et al. Effect of payments for health care on poverty estimates in 11 countries in Asia: an analysis of household survey data. Lancet. 2006;368:1357–64. doi: 10.1016/S0140-6736(06)69560-3. [DOI] [PubMed] [Google Scholar]
- 15.van Doorslaer E, O’Donnell O, Rannan-Eliya RP, Somanathan A, Adhikari SR, Garg CC, et al. Catastrophic payments for health care in Asia. Health Econ. 2007;16:1159–84. doi: 10.1002/hec.1209. [DOI] [PubMed] [Google Scholar]
- 16.Prakongsai P, Limwattananon S, Tangcharoensathien V. The equity impact of the universal coverage policy: lessons from Thailand. In Chernichovsky D, Hanson K, eds. Innovations in health system finance in developing and transitional economies Bingley: Emerald; 2009. [PubMed] [Google Scholar]
- 17.Tangcharoensathien V, Prakongsai P, Limwattananon S, Patcharanarumol W, Jongudomsuk P. From targeting to universality: lessons from the health system in Thailand. In: Townsend P, ed. Building decent societies: rethinking the role of social security in development Basingstoke: Macmillan; 2009. [Google Scholar]
- 18.Rohde J, Cousens S, Chopra M, Tangcharoensathien V, Black R, Bhutta Z, et al. Alma-Ata: rebirth and revision 4, 30 years after Alma-Ata: has primary health care worked in countries? Lancet. 2008;372:950–61. doi: 10.1016/S0140-6736(08)61405-1. [DOI] [PubMed] [Google Scholar]
- 19.Hill K, Vapattanawong P, Prasartkul P, Porapakkham Y, Lim SS, Lopez AD. Epidemiologic transition interrupted: a reassessment of mortality trends in Thailand, 1980-2000. Int J Epidemiol. 2007;36:374–84. doi: 10.1093/ije/dyl257. [DOI] [PubMed] [Google Scholar]
- 20.Vapattanawong P, Hogan MC, Hanvoravongchai P, Gakidou E, Vos T, Lopez AD, et al. Reductions in child mortality levels and inequalities in Thailand: analysis of two censuses. Lancet. 2007;369:850–5. doi: 10.1016/S0140-6736(07)60413-9. [DOI] [PubMed] [Google Scholar]
- 21.Black RE, Morris SS, Bryce J. Where and why are 10 million children dying every year? Lancet. 2003;361:2226–34. doi: 10.1016/S0140-6736(03)13779-8. [DOI] [PubMed] [Google Scholar]
- 22.O’Donnell O, van Doorslaer E, Wagstaff A. Analyzing health equity using household survey data: a guide to techniques and their implementation Washington, DC: The World Bank Institute; 2008. [Google Scholar]
- 23.Gwatkin DR, Rutstein S, Johnson K, Suliman E, Wagstaff A, Amouzou A. Socio-economic differences in health, nutrition, and population within developing countries: an overview Washington, DC: The World Bank; 2007. [PubMed] [Google Scholar]
- 24.Wibulpolprasert S, Thaiprayoon S. Thailand: Good practice in expanding health coverage – lessons from the Thai health care reforms. In: Gottret P, Schieber GJ, Waters HR, eds. Good practices in health financing: lessons from reforms in low- and middle-income countries Washington, DC: The World Bank; 2008. [Google Scholar]
- 25.Anand S, Bamighausen T. Health workers and vaccination coverage in developing countries: an econometric analysis. Lancet. 2007;369:1277–85. doi: 10.1016/S0140-6736(07)60599-6. [DOI] [PubMed] [Google Scholar]
- 26.Victora CG, Adair L, Fall C, Hallal PC, Martorell R, Richter L, et al. Maternal and child under-nutrition: consequences for adult health and human capital. Lancet. 2008;371:340–57. doi: 10.1016/S0140-6736(07)61692-4. [DOI] [PMC free article] [PubMed] [Google Scholar]