Abstract
Objectives
To characterize the beliefs and opinions of nursing home (NH) and emergency medicine providers about communication between NH and emergency departments (ED) during transitions of care of NH residents.
Design
A cross-sectional study using a mailed and internet survey.
Participants and Setting
Physicians, nurse practitioners, physician’s assistants and nurses who practice in ED settings and NH settings, affiliated with hospitals of an academic medical center in Rochester, New York.
Measurements
Opinions on communication; beliefs about frequency of information transmission; opinions on how often verbal communication should occur.
Results
A total of 155 nurses and medical providers participated in the survey for a response rate of 32.2% (155/481). Of the survey participants, 63.0% and 56.8% had been more than 5 years in their position and facility, respectively. The majority of respondents felt that important information was lost during patient transfers between NH and ED settings. Providers from ED and NH settings had different opinions on the likelihood that key information would be readily identifiable at patient transfer and that care would include requested tests and follow-up. Providers from both sites of care supported verbal communication at their position when NH residents are transferred to the other setting.
Conclusion
Nurses and medical providers from both emergency and NH settings agree that transitional communication is poor between NHs and EDs and support a role for verbal communication during the ED transitions of care of NH residents.
Keywords: transitions of care, nursing homes, emergency medicine
Introduction
Approximately 1.5 million adults currently reside in nursing homes (NHs) (1). These individuals frequently use emergency department (ED) services, with more than 25% of NH residents receiving ED care annually (1–3). These transitions of care between NHs and acute care settings are vulnerable periods for older adults. Poor transitions may result in medication errors, adverse drug events, a lack of appropriate follow-up care, and otherwise avoidable re-hospitalization (4–6).
Poor communication has been cited as the main cause of poor transitions between NH and EDs (7). Significant variability in the quality and volume of care information provided with transitioning NH residents has been noted. Ten percent of NH residents arrive in the ED without any documentation and the remaining 90% of NH-to-ED transfers are often missing the patient information necessary to render safe, efficient care, such as reason for transfer to the ED, usual mental status, and medication lists (8–12). Poor quality communication with ED providers upon the return of patients to NHs has also been noted, including lack of communication about ED diagnosis, tests and treatments provided in the ED, and treatment recommendations (7, 13).
Quality indicators for transitional care between NHs and EDs were recently developed by the Geriatric Task Force of the Society for Academic Emergency Medicine (14). These quality indicators identify processes which are essential for effective transitional care for NH residents. To our knowledge, only observational reports and focus groups have been used to describe provider’s perceptions about transitions between NH and ED settings (7, 9) No quantitative surveys of provider opinions on transitional care communication between NHs and EDs have been reported, nor has the feasibility of capturing these quality indicators in existing medical records been reported. This study uses the Geriatric Task Force of the Society for Academic Emergency Medicine’s quality indicators for transitional care as a framework to measure and compare the opinions of NH and ED providers on the current quality of NH-ED transitions.
Methods
In September 2008, a total of 481 full- and part-time adult nurses and medical providers who work in either NH or ED settings were invited to participate in a voluntary survey about patient transitions between the NH and ED settings. Medical providers included physicians, nurse practitioners and physician’s assistants. From the ED care setting, physicians (n=38), nurse practitioners and physician’s assistants (n=61) and registered and licensed practical nurses (n=170) from two University of Rochester Medical Center EDs (Strong Memorial Hospital or Highland Hospital) were invited by e-mail to participate by in an internet-based survey. University of Rochester Medical Centers EDs were selected because of their role as key referral hospitals for NHs patients in the greater Rochester region. Strong Memorial Hospital is a tertiary care academic medical center that serves as the largest referral hospital for the greater Rochester region. The Strong Memorial Hospital ED cares for almost 100,000 patients annually. Highland Hospital is a community teaching hospital with expert focus in geriatric care. The ED at Highland Hospital cares for approximately 30,000 patients annually.
From the NH setting, University of Rochester Division of Geriatrics/Aging faculty physicians (n=22), nurse practitioners and physician’s assistants (n= 24) who serve as the primary care providers for residents of 17 skilled nursing facilities were invited by e-mail to participate in the same internet-based survey. Licensed practical and registered nurses employed at Monroe Community Hospital, a 566-bed county-owned NH, were also invited to participate in this study (n=166). Monroe Community Hospital was selected because it is one of the county’s largest NHs and its residents are frequently transferred to the EDs of the University of Rochester Medical Center for evaluation and care. Because of available resources within the NH, these nurses were invited by written letter and given the opportunity to complete a written questionnaire rather than an internet based survey. NH and ED nurses and medical providers answered identical survey questions. In appreciation of their time for completing the survey, participants were invited to partake in a raffle for one of ten twenty-five dollar gift-cards to a local grocery store. The raffle participation was separate from the survey. This study was reviewed by the Research Subjects Review Board of the University of Rochester and met exempt criteria.
Survey Design
The survey was developed by an emergency medicine physician (MNS) and a geriatric medicine physician (SMG) with a focus in nursing home care (Appendix A). The main themes of the survey were influenced by quality indicators for transitional care between NHs and EDs developed by the Geriatric Task Force of the Society for Academic Emergency Medicine (14). The survey was reviewed and revised by an emergency medicine physician, 2 geriatric medicine physicians, 3 nurses, and a psychologist with an expertise in survey methodology.
The survey had three main themes. The first theme focused on perception of how often key clinical information is readily identifiable when NH residents are transferred to the ED. Respondents were asked how often they believed each of the following pieces of key clinical information would be easily identifiable when NH residents are transferred to the ED for care: reason for transfer, code status, usual mental status, allergies, medical problem list, current medication list, and contact information for the NH staff. Participants were asked how often they believed that transfer information would be easy to read and how often they believed the transfer information needed to care for the NH resident would be identifiable in less than 2 minutes. Respondents also rated their confidence that ED providers’ evaluations of NH residents in the ED would include specific tests requested by NH providers.
The second theme targeted perceptions of communication when NH residents are released from the ED back to the NH. Respondents were asked how often they believed each of the following pieces of key clinical information would be easily identifiable in the transfer paperwork when a NH resident is released from the ED back to the NH for care: ED diagnosis; the results of tests performed; a list of tests with results pending; and recommendations for treatment after once back in the NH. They were also asked how often they believed that the information provided by the ED to the NH would be easy to read and to rate their confidence that the patient’s treatment plan will be carried out according to ED recommendations.
The third theme targeted providers’ opinions about the role of verbal communication in transitional care between NH and EDs. Participants were asked if they believed the quality of communication between NHs and EDs was good and whether they believed important information was lost during those transitions. Participants were also asked how often they believed verbal communication should occur at their position for NH to ED and ED to NH transitions.
Statistical Analysis
Because both groups were asked the same questions, analysis was performed to describe the beliefs of the groups and compare the mean opinions of ED providers and NH providers. Survey responses were analyzed using SPSS (version 17.0). Comparison between ED providers and NH providers were made using independent t-tests. A p value <0.05 was considered statistically significant.
Results
Of the 481 nurses and medical providers invited, a total of 155 participated in the survey for an overall response rate of 32.2%. Response rates were highest for physicians, with 23/38 (60.5%) of emergency medicine and 13/22 (59.1%) of geriatric medicine physicians responding. Response rates for emergency medicine and NH nurses were 44/170 (25.9%) and 54/166 (32.5%), respectively. Respondents’ demographics are presented in Table 1. As seen in Table 1, they were predominantly female and had been employed in their professional position and facility for more than 5 years (table 1).
Table 1.
Demographics of survey respondents (n=155).
| Total N=155 |
Emergency Medicine N=76 |
Nursing Home N=79 |
|
|---|---|---|---|
| HealthCare Providers N (%): | |||
| Physicians | 36 (23.2) | 23 (30.3) | 13 (16.5) |
| Nurse Practitioner | 15 (9.7) | 5 (6.6) | 10 (12.6) |
| Physician’s Assistant | 6 (3.9) | 4 (5.3) | 2 (2.5) |
| Nurses: | |||
| RN | 56 (36.1) | 35 (46.0) | 21 (26.6) |
| LPN | 42 (27.1) | 9 (11.8) | 33 (41.8) |
| Gender* N (%): | |||
| Male | 29 (18.7) | 17 (22.4) | 12 (15.2) |
| Female | 123 (79.3) | 56 (73.7) | 67 (84.8) |
| Years in Position** N (%): | |||
| Less than 1 year | 10 (6.5) | 6 (8.0) | 4 (5.1) |
| 1 to 5 years | 47 (30.3) | 24 (32.0) | 23 (29.1) |
| 6 to 10 years | 34 (21.9) | 17 (22.7) | 17 (21.5) |
| 11 years or more | 63 (40.6) | 28 (37.3) | 35 (44.3) |
| Years in Facility N (%): | |||
| Less than 1 year | 19 (12.3) | 10 (13.2) | 9 (11.4) |
| 1 to 5 years | 48 (31.0) | 29 (38.2) | 19 (24.0) |
| 6 to 10 years | 39 (25.1) | 15 (19.7) | 24 (30.4) |
| 11 years or more | 49 (31.6) | 22 (28.9) | 27 (34.2) |
3 subjects did not report their gender (all ED subjects).
1 ED subject did not respond
Beliefs Regarding Nursing Home to Emergency Department Transitions
The nursing and medical providers’ beliefs about transitional care communication for nursing home (NH) to emergency department (ED) transitions are presented in Table 2. As can be seen in Table 2, the nursing home staff’s perceptions about the adequacy of their information provided in NH to ED transfers was significantly more positive than the perceptions of the ED staff. Of particular concern were the nurses and medical providers’ beliefs that important patient care information would not always be easy to read or identifiable in less than 2 minutes. Both NH and ED providers lacked confidence that ED evaluations would include tests specifically requested by NH providers.
Table 2.
Nursing and medical providers’ beliefs about transitional care communication for nursing home (NH) to emergency department (ED) transitions, all respondents (n=155)*.
| Please indicate how often you believe the following occurs when a NH resident is transferred to the ED for care (scale 1=never, 7=always): |
All mean±SE |
Emergency Medicine mean±SE |
Nursing Home mean±SE |
Statistical Significance |
|---|---|---|---|---|
| The reason for transfer is easily identifiable. |
4.92±0.128 N=148 |
4.18±0.18 N=76 |
5.69±0.13 N=72 |
<.01 |
| The NH resident’s code status is easily identifiable. |
4.85±0.139 N=148 |
3.92±0.185 N=76 |
5.83±0.13 N=72 |
<.01 |
| A NH resident’s usual mental status is easily identifiable. |
3.71±0.128 N=147 |
3.12±0.163 N=76 |
4.35±0.169 N=71 |
<.01 |
| The NH resident’s allergies are easily identifiable. |
5.26±0.131 N=146 |
4.54±0.193 N=74 |
6.00±0.130 N=72 |
<.01 |
| The NH resident’s medical problem list is easily identifiable. |
5.18±0.137 N=148 |
4.42±0.195 N=76 |
5.99±0.142 N=72 |
<.01 |
| The NH resident’s current medication list is easily identifiable. |
5.32±0.134 N=147 |
4.65±0.198 N=75 |
6.01±0.141 N=72 |
<.01 |
| Contact information for NH staff is easily identifiable. |
4.20±0.162 N=145 |
3.27±0.207 N=75 |
5.20±0.193 N=70 |
<.001 |
| The transfer information is easy to read. |
4.48±0.131 N=144 |
3.89±0.177 N=76 |
5.13±0.161 N=68 |
<0.01 |
| I can find the transfer information I need to care for the NH resident in less than 2 minutes. |
3.65±0.159 N=129 |
3.03±0.210 N=71 |
4.41±0.204 N=58 |
<0.01 |
| ED evaluation will include specific tests requested by NH providers. |
3.75±0.143 N=134 |
3.54±0.195 N=74 |
4.00±0.209 N=60 |
.11 |
Some subjects did not respond to all questions.
Beliefs Regarding Emergency Department to Nursing Home Transitions
The nursing and medical providers’ beliefs about transitional care communication for emergency department (ED) to nursing home (NH) transitions are presented in Table 3. As can be seen in Table 3, there was congruence in the perceptions of ED and NH staff in the adequacy of test results and treatment recommendations. But, ED staff significantly believed that the ED documentation was easier to read and diagnostic information was more easily identifiable compared to the NH staff. ED staff also was significantly less confident that the treatment plan will be carried out according to ED recommendations compared to NH staff.
Table 3.
Nursing and medical care providers’ beliefs about transitional care communication for ED to NH transitions, all respondents (n=155)*.
| Please indicate how often you believe the following occur when a NH resident is released from the emergency department back to the NH for care (scale 1=never, 7=always): |
All mean±SE |
Emergency Medicine mean±SE |
Nursing Home mean±SE |
Statistical Significance |
|---|---|---|---|---|
| Diagnosis made by the ED care team is easily identifiable in the transfer paperwork. |
4.79±0.132 N=148 |
5.18±0.189 N=71 |
4.43±0.176 N=77 |
<.05 |
| The results of tests performed in the ED are easily identifiable in the transfer paperwork. |
4.01±0.130 N=147 |
4.06±0.198 N=71 |
3.97±0.172 N=76 |
.75 |
| A list of tests with results pending at the time of patient release is easily identifiable in the transfer paperwork. |
3.57±0.127 N=143 |
3.53±0.199 N=68 |
3.61±0.161 N=75 |
.74 |
| Recommendations for treatment in the next 24 hours are easily identifiable in the transfer paperwork. |
4.68±0.126 N=148 |
4.70±0.191 N=72 |
4.66±0.169 N=77 |
.87 |
| When a NH resident is released from the ED back to the NH, I am confident that the treatment plan will be carried out according to ED recommendations. |
4.18±0.141 N=147 |
3.69±0.205 N=72 |
4.64±0.181 N=75 |
<.01 |
| The information provided by the ED is easy to read. |
4.43±0.138 N=145 |
4.84±0.217 N=69 |
4.05±0.165 N=76 |
<.05 |
Some subjects did not respond to all questions.
Role of Verbal Communication in Transitional Care between Nursing Homes and Emergency Departments
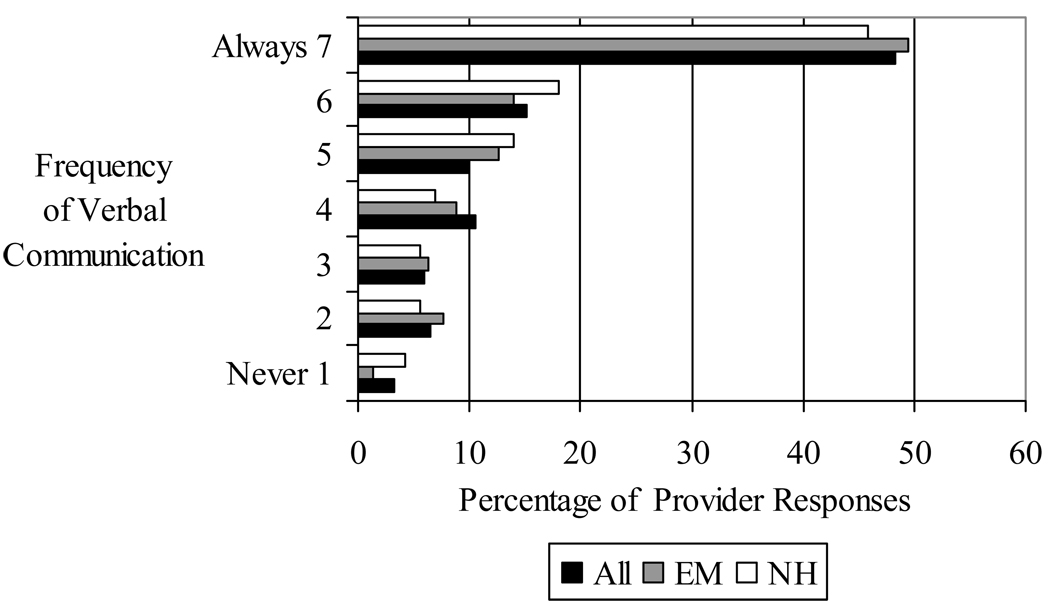
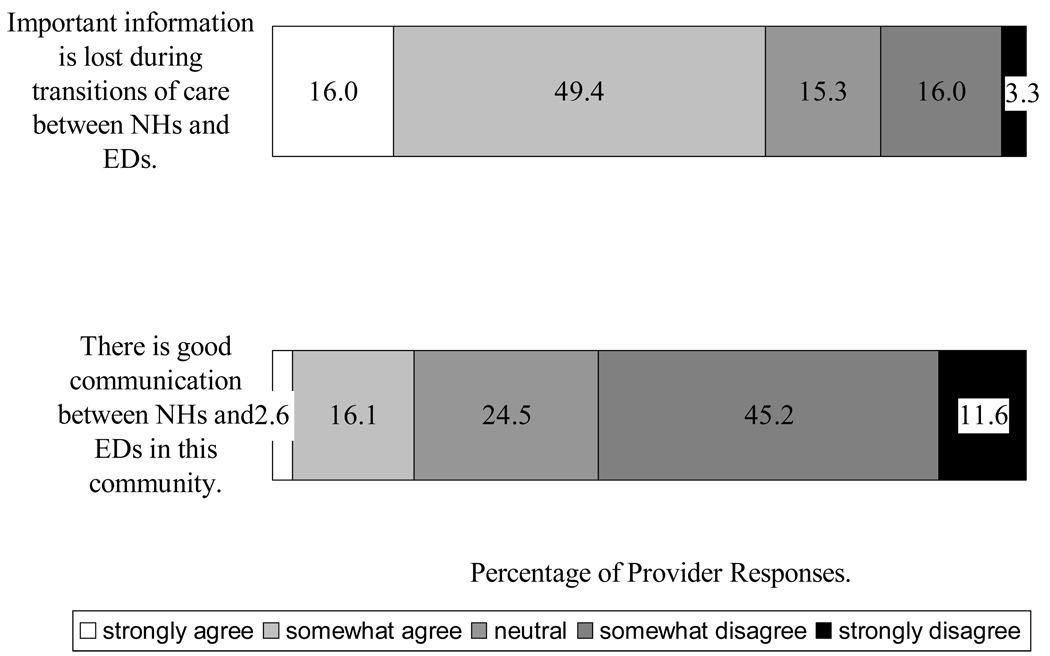
Verbal communication was strongly supported by both ED and NH groups, as seen in Figure 1. Support of verbal communication was noted for nursing and medical providers at both NH-to-ED transitions and ED-to-NH transitions. As can be seen in Figure 2, nurses and medical providers from both ED settings and NH settings believed that important information was lost during care transitions between the two sites. Both groups disagreed with the statement “there is good communication between EDs and NHs in this community” (mean 3.24 SE 0.120). However, nurses and medical providers from NH settings had higher mean ratings than those from ED sites of care (mean 3.51 SE 0.179 vs. mean 2.96 SE 0.154, p<0.05).
Figure 1.
Opinion of nursing and medical providers on how often verbal communciation between NH and ED care providers at their position/level should occur when NH residents are transferred to the ED (N=151).
Figure 2.
Opinions of nursing and medical providers of communication between nursing homes and emergency rooms.
Discussion
With our aging population, transitions of care between NHs and ED settings will continue to be common. This study provides an important description of the lack of confidence that NH and ED providers hold about the communication between them during NH residents’ transitions of care. Only 19% of survey respondents felt that there was good communication between these sites of care and 65% felt that important information was lost during care transitions. Concerns about communication at handoffs and transitions are not unique to ED and NH transitions. A database of hospital employees surveyed about patient safety reported that only 42% of acute hospital employees disagreed or strongly disagreed with the statement “problems often occur in the exchange of information across hospital units.” (15). Improving the effectiveness of communication among caregivers, including “hand-off” or transitional communication is a 2009 National Patient Safety Goal established by the Joint Commission. Surveys of Patient Safety Culture have been developed for acute hospitals, ambulatory outpatient medical office and NH settings by the Agency for Healthcare Research and Quality. These surveys are used to assess the patient safety culture of a healthcare facility, to track changes in patient safety over time and are powerful benchmarking tools for quality improvement initiatives targeting communication in health care facilities (16). Each of these surveys contains its own items to address relevant handoff communication. Similar tools may improve communication between acute and long-term healthcare facilities. A tool, designed for use by ED and NH caregivers, that specifically targets the culture and safety of transitions of care between health care facilities, would offer valuable information for groups working together to improving the quality and safety of care transitions in their community. This study lays groundwork for development of this type of survey tool.
In this study, we found that providers from our EDs and NHs have some different perceptions about the communication processes between NH to ED settings. For NH-to-ED transitions, NH nurses and medical providers had significantly greater confidence than ED nurses and medical providers that elements of patient information would be present and readily identifiable. Similarly, ED and NH providers expressed different perceptions with regards to the communication of ED diagnosis and their confidence that treatment plans will be carried out according to ED recommendations. Joint initiatives between long-term care and emergency providers to develop standardized transitional care communication tools that are concise, readily identifiable and in a format that targets the learning style and care needs of receiving care providers are needed.
Direct verbal communication between providers was identified by the Geriatric Task Force of the Society for Academic Emergency Medicine as an essential element of ensuring high-quality transitions of care between NHs and EDs(15). To our knowledge, opinions about the role of verbal communication between ED and NH nurses and medical providers have not been previously reported. In our study, the majority of nurses and medical providers also felt that verbal communication should occur for most, if not all, patient transitions between NH and EDs. It remains unclear, however, whether this opinion is influenced by a lack of provider confidence in current communication processes, which variably include verbal communication between care givers, or if verbal communication offers additional essential benefits. Additional research is necessary to define the role of verbal communication during transitions of care between NHs and EDs.
This study is limited by its inclusion of only one university health system and a low response rate among nurses. Larger studies of provider opinions of the quality and safety of transitions between NHs and EDs, undertaken in a variety of communities will improve understanding of transitional communication. A second limitation of this study is that it reports opinions and perceptions without corresponding measured rates of transferred information. The perceptions of the nursing and medical providers may not equal reality. For example, providers may feel that the reason for transfer isn't communicated very often, when it may, in fact, be present 90% of the time. Research to determine the actual frequencies of data transfer, in comparison to staff perceptions of data availability is needed. Another limitation of this study is that reasons for staff beliefs were not evaluated. For instance, the reason why ED providers feel that NH requested test will not be done may differ from the reason why NH providers feel the same way. However, we feel that this study is an important step in designing and tracking the impact of initiatives focused on improving the transitional care of NH residents. For transitional care to improve, healthcare communities will need to join forces and work together towards shared goals. Alignment of incentives across sites of care will likely be an important factor in motivating these efforts.
Conclusion
Providers from both ED and NH settings agree that transitional communication is poor between NHs and EDs. Additional research is needed to determine the actual frequencies of data transfer, to establish the reliability of nursing and medical provider perceptions about transitional communication and to discover ways to improve communication. Both groups of providers feel that verbal communication is important during care transitions between these sites of care, but the exact role is unclear.
Acknowledgments
This study was supported by an American Medical Director’s Association Foundation/Pfizer Quality Improvement Award.
Dr. Gillespie is a recipient of a Geriatric Academic Career Award administered by the Bureau of Health Professions, Health Resources and Services Administration, U.S. Department of Health and Human Services. Dr. Gillespie gratefully acknowledges the support of the American Medical Directors Association (AMDA) Foundation for award of an AMDA Foundation Pfizer Quality Improvement Award which supported this study.
Dr. Shah is supported by the Paul B. Beeson Career Development Award (NIA 1K23AG028942).
References
- 1.Centers for Disease Control and Prevention/National Center for Health Statistics. [Accessed July 23, 2009];The National Nursing Home Survey. 2004 Available at http://www.cdc.gov/nchs/nnhs.htm.
- 2.Bergman H, Clarfield AM. Appropriateness of patient transfer from a nursing home to an acute-care hospital: a study of emergency room visits and hospital admissions. J Am Geriatr Soc. 1991;39:1164–1168. doi: 10.1111/j.1532-5415.1991.tb03568.x. [DOI] [PubMed] [Google Scholar]
- 3.Nawar EW, Niska RW, Xu J. National Hospital Ambulatory Medical Care Survey: 2005 Emergency Department Summary. Adv Data. 2007:1–32. [PubMed] [Google Scholar]
- 4.Coleman EA, Parry C, Chalmers S, Min SJ. The Care Transitions Intervention: Results of a Randomized Controlled Trial. Arch Intern Med. 2006;166:1822–1828. doi: 10.1001/archinte.166.17.1822. [DOI] [PubMed] [Google Scholar]
- 5.Boockvar K, Fishman E, Kyriacou CK, et al. Adverse events due to discontinuations in drug use and dose changes in patients transferred between acute and long-term care facilities. Arch Intern Med. 2004;164:545–550. doi: 10.1001/archinte.164.5.545. [DOI] [PubMed] [Google Scholar]
- 6.American Medical Director’s Association. [Accessed on April 22, 2009];Improving care transitions from the nursing facility to a community based setting. Available at www.amda.com/governance/whitepapers/transitions_of_care.cfm.
- 7.Terrell KM, Miller DK. Challenges in transitional care between nursing homes and emergency departments. J Am Med Dir Assoc. 2006;7:499–505. doi: 10.1016/j.jamda.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 8.Davis MN, Brumfield VC, Smith ST, et al. A one-page nursing home to Emergency room transfer form: what a difference it can make in an emergency! Ann of Long-Term Care. 2005;13(11):34–38. [Google Scholar]
- 9.Jones JS, Dwyer PR, White LJ, Firman R. Patient transfer from nursing home to emergency department: outcomes and policy implications. Acad Emerg Med. 1997;4:908–915. doi: 10.1111/j.1553-2712.1997.tb03818.x. [DOI] [PubMed] [Google Scholar]
- 10.Terrell KM, Brizendine EJ, Bean WF, Giles BK, et al. An extended care facility to emergency department transfer form improves communication. Acad Emerg Med. 2005;12(2):114–118. doi: 10.1197/j.aem.2004.10.013. [DOI] [PubMed] [Google Scholar]
- 11.Boockvar KS, Fridman B, Marturano C. Ineffective communication of mental status information during care transfer of older adults. J Gen Intern Med. 2005;20:1146–1150. doi: 10.1111/j.1525-1497.2005.00262.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Stier PA, Biles BK, Olinger Ml, Brizendine EJ, Cordell WH. Do transfer records for extended care facility patients sent to the emergency department contain essential information? Ann Emerg Med. 2001;38:S102. [Google Scholar]
- 13.Davis MN, Smith ST, Tyler A. Improving transition and communication between acute care and long-term care: a system for better continuity of care. Ann of Long-Term Care. 2005;13(5):25–32. [Google Scholar]
- 14.Terrell KM, Hustey FM, Hwang U, et al. Quality indicators for geriatric emergency care. Acad Emerg Med. 2009;16:441–449. doi: 10.1111/j.1553-2712.2009.00382.x. [DOI] [PubMed] [Google Scholar]
- 15.Hospital Survey on Patient Safety Culture. [Accessed July 22, 2009];Rockville, MD: Agency for Healthcare Research and Quality. 2009 March; Available at http://www.ahrq.gov/qual/patientsafetyculture/hospsurvindex.html.
- 16.Patient Safety Culture Surveys. [Accessed July 22, 2009];Rockville, MD: Agency for Healthcare Research and Quality. Available at http://www.ahrq.gov/qual/patientsafetyculture.