Abstract
Objective:
The objective of the study was to assess whether a targeted intervention improved the satisfaction of neonatal parents with primary medical provider communication.
Study Design:
The study design was a survey assessment of parents in a neonatal intensive care unit regarding their satisfaction with physician and nurse practitioner communication. Serial cohorts were surveyed before and after an intervention, including educating providers about family communication, distributing contact cards to families and showing a poster of providers in the unit.
Result:
More subjects in the post-intervention cohort (n=33) were satisfied (95%) with provider communication than in the pre-intervention cohort (n=50, 74% P<0.01). Parents who reported talking with a provider in the previous 7 days were more satisfied than parents who did not (P<0.001). After the intervention, fewer families (36 versus 65%) reported a desire for more frequent provider contact (P<0.01).
Conclusion:
A targeted intervention improved parent satisfaction with provider communication. Improving the quality and quantity of parent–provider communication increased parent satisfaction with communication with their baby's medical providers.
Keywords: family-centered care, physician communication, physician–patient/parent communication, quality improvement, survey
Introduction
Communication between parents and their baby's principal medical care providers is important in the neonatal intensive care unit (NICU) setting.1, 2 It is important for parents to feel that they can communicate with the doctors and neonatal nurse practitioners (NNPs) in the NICU,3 so that they can understand their baby's condition, participate in medical decision making and care for their baby appropriately. The stress, technology and dynamic intensity of the NICU environment can be barriers to communication between parents and medical providers.4, 5, 6 Additional barriers at some institutions include complex physician rotation schedules and language differences.7
Taking a family-centered approach to parent–provider communication may improve parent satisfaction.1, 8, 9 Potentially better practices for improving parent–provider communication have been developed, based on institutional self-analysis, literature review, benchmarking site visits, expert consultation and multidisciplinary discussions.10, 11, 12, 13 Several tools have been created to measure parent satisfaction with communication in the NICU14, 15, 16 and other pediatric settings,17, 18 but a targeted intervention that improves communication between parents and physicians in an academic NICU has not been previously reported.
Pediatric interns, residents, neonatal fellows, attending neonatologists and NNPs are the principal medical providers (PMPs) in the NICU at the University of California, San Diego (UCSD). We hypothesized that an intervention targeted to improve the quality and quantity of communication between parents and PMPs in the UCSD NICU would improve parent satisfaction with PMP communication.
Methods
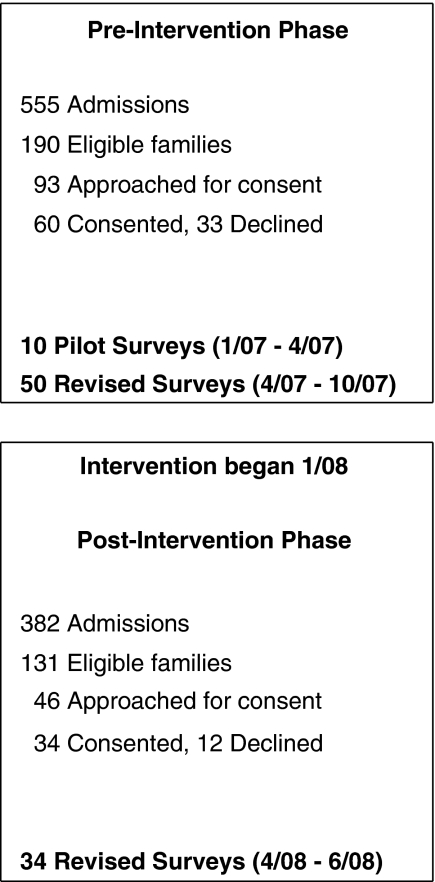
This before-and-after assessment of the effect of a new family–PMP communication intervention was divided into three phases, as illustrated in Figure 1. Birth parents of any baby who had been in the NICU for 7 days or more were eligible for enrollment. Foster parents and surrogates were excluded because they are generally not involved in the care of infants in the NICU at UCSD. The study was approved by the institutional review board of the UCSD. Consent was obtained from the subjects after the nature of the study had been fully explained.
Figure 1.
The study timeline. The study had three phases: pre-intervention cohort phase, intervention phase and post-intervention cohort phase.
During this study, the level III, 40-bed academic NICU at UCSD was staffed by a group of 57 rotating PMPs: 9 attending physicians, 7 NICU fellows, 37 pediatric residents and 4 NNPs. During the daytime, each patient was cared for by a team including one neonatal attending, one neonatal fellow, and one resident, intern or NNP. At night, the covering team consisted of a fellow, a resident and an intern. Attending physicians rotated weekly, fellows rotated every 3 weeks, residents and interns rotated monthly and the NNPs rotated daily.
Pre-intervention
Parents visiting their babies in the NICU were approached for consent by investigators between January and October 2007, as a convenience sample that, in an effort to include all parents, included weekdays, weekends, and evenings. On the seventh day after the baby's admission, an investigator met with consenting parents and read a brief script, explaining that the survey was designed to help NICU doctors improve parent communication. The investigator then read the survey aloud to parents. Parents could choose to complete the survey together with the investigator or complete the survey independently and return it anonymously through drop-box in the NICU or by postage-paid mail. Consents and surveys were available in English and Spanish. Interpreters were used when the investigator did not speak the language of the parents. Demographic and clinical patient data from medical records was recorded on electronic data sheets for each consenting family.
A pilot survey consisting of content-validated Likert scale questions, written by Press Ganey and the Picker Institute, was given to 20 families.18, 19, 20, 21 A total of 10 families (50%) returned the completed pilot surveys. The survey was then revised on the basis of the pilot responses to obtain more quantitative data about the specific constructs of communication: quantity, availability, understanding, reciprocity and empathy.22, 23 The revised survey (see Supplementary Figure S1) included six open-ended questions about quantity of communication and six four-point Likert scale questions addressing availability, understanding, reciprocity and empathy.
Intervention
The intervention, introduced in January 2008, was developed in response to the pre-intervention surveys, which reported very low quantity of PMP–parent communication and low PMP availability. The intervention was designed to increase PMP availability and communication frequency. It consisted of (1) a brief education module for PMPs as summarized in Supplementary Figure S2, (2) a contact card for parents with PMP names, job descriptions and contact information (see Supplementary Figure S3) and (3) a large poster of the faces, names and titles of the PMPs on display at the parent entrance of the NICU.
The education module consisted of a single 30-min moderated slideshow for PMPs that introduced a communication plan, in which PMPs establish a thread of family communication from an infant's admission to discharge. The module recommended that PMPs meet with families on a daily basis initially, and at least weekly once the patients became stable. The module emphasized important principles of communication, including use of interpreters, contact frequency and essential elements of NICU family meetings. All PMPs participated in the module before the end of their first week in the NICU. The contact cards, printed on a 6 × 4 inch green card stock, contained the names of all PMPs, rotation durations and brief job descriptions. Upon NICU admission, a PMP gave each family a contact card and circled the names of the PMPs on duty, explaining the provider rotation system. As new interns and residents rotated into the NICU, they gave parents updated contact cards.
In addition to the PMP education module, nursing leaders and NICU support staff heard a 5-min presentation during a routine meeting. Subsequently, the investigators presented a 20-min overview of the pre-intervention survey results, and the introduction of the PMP education module, contact cards and poster to both the family-centered care nursing group and the entire nursing staff. Total staff education was 5 min for NICU support staff in one single meeting, 20 min for each nurse who attended one of two repeated meetings and 30 min for each PMP who attended one of six repeated meetings.
Post-intervention
Post-intervention cohort enrollment occurred between April and June 2008, starting 2 months after the intervention was introduced. The post-intervention cohort comprised a second, separate cohort of parents. Parents were approached for consent under the same circumstances as the pre-intervention cohort, using the same script to present the survey and the same method of survey administration and collection as described in the pre-intervention section.
Statistical analysis
Interval data that were normally distributed were analyzed by independent t-tests; if the data distribution was found to deviate significantly from the normal distribution, they were instead compared using Mann–Whitney U-tests. Open responses to frequency-related questions were categorized as: more than daily, daily, every other day, every few days, weekly, less than weekly or never, and analyzed as ordinal data. Data from Likert scales were analyzed as ordinal data using Kruskal–Wallace tests. Dichotomized data from these scales, including those from main and subgroup analyses, were analyzed using chi-square test or Fisher's exact test when any group had fewer than five subjects. Dichotomized data were also analyzed by two-sample test of proportions when appropriate. Differences were considered statistically significant at an alpha of 0.05 (P<0.05). Data analysis was carried out with NeoOffice, Houston, TX, USA and SPSS 16.0, Chicago, IL, USA.
Ambiguous pre-intervention survey results, such as a mark between two Likert options and more than one answer for a question, were interpreted as the more satisfied response, and this occurred in two pre-intervention surveys and one post-intervention survey. Unclear responses, such as attempted erasures or unclear handwriting, were treated as missing data and omitted from further analysis.
Results
There were no significant demographic differences between the cohorts, as shown in Table 1. Pre-intervention surveys (n=50) were completed at an average of 30 days of admission. Post-intervention surveys (n=34) were completed at an average of 26 days. In all, 16% (8/50) of pre-intervention and 18% (6/33) of post-intervention families had NNPs as their PMP. The remaining families had interns or residents. All babies were also cared for by neonatal fellows and attending physicians as described above. Care by NNP versus intern or resident was not associated with satisfaction. In the pre-intervention group, 78% (39/50) of the families completed the survey in the presence of the investigator. The remaining 22% completed the survey independently. Similarly, 85% (28/33) of the post-intervention families completed the survey with the investigator present (P=0.44). Investigator presence during the survey did not correlate with satisfaction in either cohort (P=0.50, P=1.00).
Table 1. Demographic data for the two cohorts.
| Pre-intervention cohort | Post-intervention cohort | P-valuea | |
|---|---|---|---|
| n | 50 | 34 | |
| Gestational age (weeks)b | 32±4.4 | 32±9.0 | 0.82 |
| Infant age at survey (days)c | 22 (11–40) | 20 (12–50) | 0.98 |
| Birth weight (g)d | 1803±877 (400–4295) | 1639±1088 (405–5600) | 0.36 |
| Maternal characteristics | |||
| Age (years)b | 30±7.8 | 26±8.3 | 0.97 |
| Primiparity | 56% (28/50) | 41% (13/32) | 0.17 |
| Married | 54% (27/50) | 42% (13/31) | 0.29 |
| Maternal education past high school | 68% (32/47) | 56% (18/32) | 0.28 |
| Mother has private insurance | 52% (26/50) | 34% (11/32) | 0.12 |
| Parent speaks and understands English | 78% (39/50) | 82% (27/33) | 0.67 |
| Ethnicity | |||
| Hispanic | 40% (20/50) | 33% (11/33) | 0.54 |
| Caucasian | 40% (20/50) | 33% (11/33) | 0.54 |
| Asian/Pacific Islander | 8% (4/50) | 6% (2/33) | 0.74 |
| Black | 4% (2/50) | 15% (5/33) | 0.11 |
| Other ethnicity | 8% (4/50) | 9% (4/33) | 0.53 |
| Clinical data | |||
| Pregnancy complications | 66% (33/50) | 56% (18/32) | 0.37 |
| Delivery complications | 18% (9/50) | 25% (8/33) | 0.45 |
| General anesthesia | 4% (2/50) | 6% (2/32) | 0.67 |
| Vaginal deliveries | 36% (18/50) | 50% (16/32) | 0.21 |
χ2-test.
Mean±s.d.
Median (25 to 75 percentile).
Mean±s.d. (range).
Overall satisfaction
Overall satisfaction, based on the ordinal analysis of the five-point Likert scale, was significantly higher after the intervention (P<0.01) as shown in Table 2. Overall satisfaction, dichotomized into a satisfied subgroup (74%, 37/50) and a dissatisfied subgroup for each cohort, was also significantly increased after the intervention (97%, 32/33; P=0.01). The satisfied subgroup was defined as families who marked ‘very satisfied' or ‘somewhat satisfied' for their overall satisfaction with PMP communication. The dissatisfied subgroup was defined as families who marked ‘unsure', ‘somewhat dissatisfied' or ‘very dissatisfied.' Parents who marked ‘unsure' were considered dissatisfied because ‘unsure' is neutral and not an affirmation of satisfaction.
Table 2. Parent satisfaction survey results.
| Pre-intervention cohort | Post-intervention cohort | P-value | |
|---|---|---|---|
| n | 50 | 34 | |
| Overall satisfactiona | <0.01 | ||
| Very satisfiedb | 48% (24/50) | 82% (27/33) | <0.01 |
| Very satisfied or somewhat satisfiedb | 74% (37/50) | 97% (32/33) | 0.01 |
| Quantity | |||
| Talked with PMP before baby was bornc | 76% (38/50) | 97% (32/33) | 0.01 |
| Since NICU admission, did not talk to a PMPb | 17% (8/47) | 0% (0/33) | 0.01 |
| Would like to talk to PMP more oftenc | 65% (31/48) | 36% (12/33) | <0.01 |
| PMPs are available to parentsb | |||
| Always | 22% (9/41) | 60% (18/30) | <0.01 |
| Usually or always | 61% (25/41) | 87% (26/30) | 0.02 |
| Parents understand what PMPs sayb | |||
| Always | 60% (26/43) | 68% (23/34) | 0.52 |
| Usually or always | 79% (34/43) | 88% (30/34) | 0.29 |
| Parents can ask PMP questionsb | |||
| Always | 90% (37/41) | 97% (33/34) | 0.24 |
| Usually or always | 95% (39/41) | 100% (34/34) | 0.19 |
| PMP understands parents' concernsb | |||
| Always | 66% (27/41) | 91% (30/33) | 0.01 |
| Usually or always | 90% (37/41) | 94% (31/33) | 0.56 |
Kruskal–Wallace analysis of ordinal Likert data.
Two-sample test of proportions.
χ2-test.
Subgroup analysis
In the pre-intervention cohort, non-English speakers tended to be less satisfied than English speakers, though this did not reach statistical significance (P=0.06). Although the majority of non-English speaking families were of Hispanic origin, Hispanic families were not less satisfied than the other families (P=0.39). No other maternal factors were associated with satisfaction in the pre-intervention cohort, including insurance status, marital status, parity, mode of delivery or complications of pregnancy or delivery. There were not enough post-intervention dissatisfied families (n=1) to form a significant subgroup for analysis.
Quantity of communication
Post-intervention families reported more communication with PMPs before birth (P=0.01) and during their baby's admission (P=0.01). Pre-intervention families reported that communication with PMPs occurred every other day (median) compared with daily communication in the post-intervention cohort. In the pre-intervention cohort, 66% (31/47) reported speaking with their PMP in the week before the survey compared with 88% (29/33) in the post-intervention cohort. Of the pre-intervention families, 83% (39/47) reported communication with PMPs during hospitalization, whereas all 100% (34/34) of post-intervention families reported some contact, with 88% (29/33) of them reporting PMP contact within the past week (P<0.01). Of pre-intervention families 65% (31/48) indicated a preference for more frequent PMP communication than they reported experiencing, as compared with 36% (12/36) of the post-intervention families (P=0.01).
Comparing the reported frequency of the parents of PMP communication with ‘how often [they] would like to talk with [PMPs]' showed that significantly more families before the intervention 65% (31/48), versus 36% (12/36) after the intervention, preferred more frequent PMP communication than they experienced (P=0.01). The ordinal analysis of the four-point Likert parent responses to whether PMPs talk with them enough also showed a significant improvement after the intervention (P<0.01).
Quality of communication
Compared to the pre-intervention cohort, significantly more parents after the intervention reported PMPs were always available when parents wanted to talk with them (P<0.01). Families from both cohorts were satisfied with PMP understanding, as evidenced by responses to how often they understood what PMPs said. Reciprocity, as indicated by parent responses to whether they could ask PMPs questions, was demonstrated both before and after the intervention. Empathy, as assessed by parents indicating that PMPs always understood their concerns about their baby, was also significantly higher after the intervention (P<0.01).
The comments of the pre-intervention parents suggested that PMPs give more information (15/39 written comments), make more frequent contact with parents (13/39), be more available (24/39) and use interpreter services (6/39). After the intervention, the comments of the parents were generally more positive than before (68%, 19/28 versus 13%, 5/39), as detailed in Supplementary Figure S4. Typical post-intervention comments were statements such as ‘communication is good', affirmations of PMP availability and contact card use, suggestions to increase interpreter involvement and set appointments for PMP communication.
Discussion
An assessment of the constructs of communication—quantity, availability, understanding, reciprocity and empathy22, 23—is a more feasible approach for studying communication than assessing communication in its entirety. The construct-based survey used in this study has improved content and construct validity when compared with the pilot survey questions, validated by Press Ganey and the Picker Institute.18, 19, 20 The intervention was designed to meet the communication needs of the NICU parents, based on the pre-intervention survey responses, in the context of previous studies of parent satisfaction in the NICU, including potentially better NICU practices.11, 14, 16, 23, 24 As assessed by the construct-based survey, parent satisfaction with PMP communication improved after the intervention.
The language difference between families and PMPs was associated with decreased satisfaction with communication before the intervention, whereas maternal ethnicity was not. Satisfaction among non-English-speaking families increased after the intervention, thus highlighting the importance of interpreter services.
Communication styles differ among parents, and the communication needs of the parents change over their time in the NICU.6, 22 Communication needs also change with a baby's acuity of illness.5 This study did not have sufficient sample size to address how acuity, degree of prematurity or parental stress influence changing communication needs, communication patterns or parent satisfaction. The study was also limited by examining a convenience sample; it did not include parents who did not visit the NICU during investigator research hours. Interpreter usage, hospital records of family visits and PMP contact were not included in this study and would be valuable topics for future studies.
Investigator presence during survey responses is potentially a significant source bias. However, the parents who were surveyed with investigators present did not give more positive responses than parents who completed the survey without the investigator. Although surveys were anonymous, identified only by number, several parents waived their anonymity at the time of the survey, asking the investigator to facilitate contact with the PMP. To avoid the bias of demand characteristics, both cohorts were approached in an identical scripted manner.
The NICU staff awareness of this study likely contributed to improved parent–PMP communication and parent satisfaction. Many nurses supported communication efforts by encouraging use of the contact cards and facilitating communication between parents and PMPs. Many parents, both satisfied and unsatisfied, gave suggestions for improvement. It is important to give parents a forum for feedback to target areas for improvement. Including parents and staff in a multidisciplinary approach to improving communication can lead to a significant improvement in parent satisfaction with communication.
Conclusion
Parent satisfaction with PMP communication can be improved by establishing a thread of communication between parents and PMPs, starting with a careful introduction catalyzed by a handheld contact card and maintaining at least weekly contact throughout the NICU experience of the family. Interpreter services are essential for clear communication between parents and providers who do not speak the same language. Further development and validation of assessment tools, such as the survey used in this study, are essential to improve parent satisfaction and quality of care.
Acknowledgments
We thank the Picker Institute and Press Ganey for the use of their survey questions, Dr Atkinson and Dr Ganiats for their help with survey revision, Dr Finer for the paper and methodological review, the Weiss family for their tireless support, the incredible UCSD NICU nurses and staff and our babies and their families. Pilot survey questions were provided by the Picker Institute, Europe, Oxford, UK and Press Ganey Company.
The authors declare no conflict of interest.
Footnotes
Supplementary Information accompanies the paper on the Journal of Perinatology website (http://www.nature.com/jp)
Supplementary Material
References
- Harrison H. The principles for family-centered neonatal care. Pediatrics. 1993;92:643–650. [PubMed] [Google Scholar]
- Urden LD. Patient satisfaction measurement, current issues and implications. Lippincotts Case Manag. 2002;7:194–200. doi: 10.1097/00129234-200209000-00006. [DOI] [PubMed] [Google Scholar]
- Davidson JE, Powers K, Hedayat KM, Tieszen M, Kon AA, Shepard E, et al. Clinical practice guidelines for support of the family in the patient-centered intensive care unit: American College of Critical Care Medicine Task Force 2004 to 2005. Crit Care Med. 2007;35:605–622. doi: 10.1097/01.CCM.0000254067.14607.EB. [DOI] [PubMed] [Google Scholar]
- Shellabarger SG, Thompson TL. The critical times: meeting parental communication needs throughout the NICU experience. Neonatal Netw. 1993;12:39–45. [PubMed] [Google Scholar]
- McCormick MC, Escobar GJ, Zheng Z, Richardson DK. Factors influencing parental satisfaction with neonatal intensive care among the families of moderately premature infants. Pediatrics. 2008;121:1111–1118. doi: 10.1542/peds.2007-1700. [DOI] [PubMed] [Google Scholar]
- Ngui EM, Flores G. Satisfaction with care and ease of using health care services among parents of children with special health care needs: the roles of race/ethnicity, insurance, language, and adequacy of family-centered care. Pediatrics. 2006;117:1184–1196. doi: 10.1542/peds.2005-1088. [DOI] [PubMed] [Google Scholar]
- Vincent JL. Communication in the ICU. Intensive Care Med. 1997;23:1093–1098. doi: 10.1007/s001340050462. [DOI] [PubMed] [Google Scholar]
- Griffin T. Family-centered care in the NICU. J Perinat Neonatal Nurs. 2006;20:98–102. doi: 10.1097/00005237-200601000-00029. [DOI] [PubMed] [Google Scholar]
- Cooper LG, Gooding JS, Gallagher J, Sternesky L, Ledsky R, Berns SD. Impact of a family-centered care initiative on NICU care, staff, and families. J Perinatol. 2007;27:S32–S37. doi: 10.1038/sj.jp.7211840. [DOI] [PubMed] [Google Scholar]
- Dunn MS, Reilly MC, Johnston AM, Hoopes RD, Jr, Abraham MR. Development and dissemination of potentially better practices for the provision of family-centered care in neonatology: the family-centered care map. Pediatrics. 2006;118S2:S95–S107. doi: 10.1542/peds.2006-0913F. [DOI] [PubMed] [Google Scholar]
- Cisneros Moore KA, Coker K, DuBuisson AB, Swett B, Edwards WH. Implementing potentially better practices for improving family-centered care in neonatal intensive care units: successes and challenges. Pediatrics. 2003;111:450–460. [PubMed] [Google Scholar]
- Saunders RP, Abraham MR, Crosby MJ, Thomas K, Edwards WH. Evaluation and development of potentially better practices for improving family-centered care in neonatal intensive care units. Pediatrics. 2003;111:437–449. [PubMed] [Google Scholar]
- Berns SD, Boyle MD, Popper B, Gooding JS. Results of the premature birth national need-gap study. J Perinatol. 2007;27:S38–S44. doi: 10.1038/sj.jp.7211841. [DOI] [PubMed] [Google Scholar]
- Conner J, Nelson EC. Neonatal intensive care: satisfaction measured from a parent's perspective. Pediatrics. 1999;103:336–349. [PubMed] [Google Scholar]
- Mitchell-Dicenso A, Guyatt G, Paes B, Blatz S, Kirpalani H, Fryers M, et al. A new measure of parent satisfaction with medical care provided in the neonatal intensive care unit. J Clin Epidemiol. 1996;49:313–318. doi: 10.1016/0895-4356(95)00531-5. [DOI] [PubMed] [Google Scholar]
- Blackington SM, McLauchlan T. Continuous quality improvement in the neonatal intensive care unit: evaluating parent satisfaction. J Nurs Care Qual. 1995;9:78–85. doi: 10.1097/00001786-199507000-00011. [DOI] [PubMed] [Google Scholar]
- Latour JM, Hazelzet JA, Van der Heijden AJ. Parent satisfaction in pediatric intensive care: a critical appraisal of the literature. Pediatr Crit Care Med. 2005;6:578–584. doi: 10.1097/01.pcc.0000164637.88469.74. [DOI] [PubMed] [Google Scholar]
- McPherson ML, Sachdeva RC, Jefferson LS. Development of a survey to measure parent satisfaction in a pediatric intensive care unit. Crit Care Med. 2000;28:3009–3013. doi: 10.1097/00003246-200008000-00055. [DOI] [PubMed] [Google Scholar]
- Jenkinson C, Coulter A, Bruster S. The Picker Patient Experience Questionnaire: development and validation using data from in-patient surveys in five countries. Int J Qual Health Care. 2002;14:353–358. doi: 10.1093/intqhc/14.5.353. [DOI] [PubMed] [Google Scholar]
- Crofton C, Darby C, Farquhar M, Clancy CM. The CAHPS hospital survey: development, testing, and use. Jt Comm J Qual Patient Saf. 2005;31:655–659. doi: 10.1016/s1553-7250(05)31084-1. [DOI] [PubMed] [Google Scholar]
- Miceli PJ. Validating a patient satisfaction survey translated into Spanish. J Healthc Qual. 2004;26:4–13. doi: 10.1111/j.1945-1474.2004.tb00501.x. [DOI] [PubMed] [Google Scholar]
- Roter DL, Hall JA. Studies of doctor-patient interaction. Annu Rev Public Health. 1989;10:163–180. doi: 10.1146/annurev.pu.10.050189.001115. [DOI] [PubMed] [Google Scholar]
- Makoul G. The interplay between education and research about patient–provider communication. Patient Educ Couns. 2003;50:79–84. doi: 10.1016/s0738-3991(03)00085-5. [DOI] [PubMed] [Google Scholar]
- Desmond J, Copeland LR. Communicating with Today's Patient: Essentials to Save Time, Decrease Risk, and Increase Patient Compliance. Jossey-Bass: New York; 2000. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.