Abstract
Oral manifestations of tuberculosis are quite rare with an incidence rate of 1.4%. The tongue is the most common site of oral tuberculosis having varied presentations. Lingual tuberculosis is a diagnostic dilemma because of its rarity, particularly in immunocompetent patients. We are reporting a rare case of primary tuberculosis of the tongue in a 38 year old male diagnosed on fine needle aspiration cytology.
Keywords: Tuberculosis, Tongue, Cytology
Introduction
Tuberculosis affects about 8 million people worldwide with high incidence in the Indian subcontinent, Southeast Asia and Africa [1].The incidence of tuberculosis in the oral cavity is quite rare. It could be either primary or secondary to pulmonary disease [2]. There are about 1–1.5% cases of pulmonary tuberculosis with associated oral cavity lesions. The oral sites most frequently affected are the tongue, palate, tonsil, pharynx, and buccal mucosa [3]. Morgagni described the first case of lingual tuberculosis in 1761 [4]. The commonest manifestation of primary oral tuberculosis is ulcer formation along the lateral border of tongue which rests against a rough, sharp, broken tooth or at the site with other irritants [5]. Although oral tuberculosis can affect persons of all age groups, middle aged males with a history of smoking are more commonly affected [6]. Patients with oral tubercular lesion often give a history of pre-existing trauma. Any area of chronic irritation or inflammation may favour localization of mycobacterium associated with the disease. Secondary tuberculosis of the oral cavity may arise in a previously sensitised individual and is associated with pulmonary lesions [7].
A Case Report
A 38 year old male presented with a one month history of a painless ulcerated swelling on the right lateral tongue. There was no history of cough, fever, haemoptysis or weight loss. The patient was a farmer from the nearby village. He had a habit of consuming raw milk and also chewed tobacco for 15 years. There was no personal or family history of any chronic illness. On examination the patient was of average built with mild pallor. Examination of the oral cavity revealed a 2.5 × 1.5 cm grey-white ulcerated lesion on the right lateral border of tongue with irregular margins and whitish patch (Fig. 1). Multiple carious teeth were also seen. No lymphadenopathy or organomegaly was found. Systemic examination done by the clinician did not reveal any abnormal findings. A clinical diagnosis of malignancy was suspected. Laboratory investigations revealed haemoglobin-10 gm% with a normocytic normochromic picture; Total Leucocyte Count- 7,000/cmm; Differential Leucocyte Count- Polymorph: 64%, Lymphocyte: 34%, Monocyte: 1%, Eosinophil: 1%; Platelets 2.8 lac/cmm. A fine needle aspiration cytology (FNAC) was performed and revealed numerous epithelioid cell granulomas with few multinucleated giant cells in a background of mixed inflammatory cells and necrosis (Fig. 2). Zeihl Neelsen stain for acid fast bacilli was positive (Fig. 3). A cytological diagnosis of tuberculosis of tongue was made. Subsequent investigations revealed ESR-42 mm at the end of the 1st h, Mantoux test performed with PPD antigen measured 14 mm after 72 h and ELISA test for HIV was nonreactive. Chest X-ray PA view examination was within normal limits. With a final diagnosis of primary lingual tuberculosis, the patient was placed on antitubercular therapy with a four drug regimen for 6 months. The response was dramatic with considerable healing of the ulcer within 1 month of the treatment. The patient is on regular follow-up with no signs of recurrence.
Fig. 1.
Photograph showing ulcer on the lateral margin of tongue
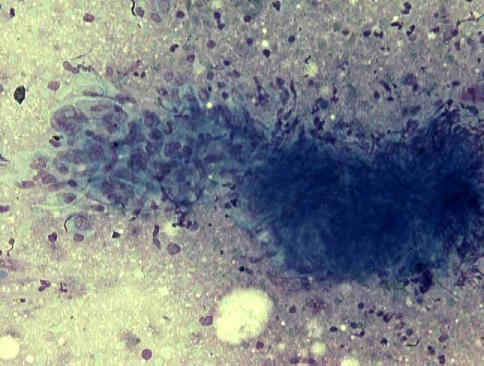
Fig. 2.
Photomicrograph showing epithelioid cell granuloma in a necrotic background. (MGG stain: 40×)
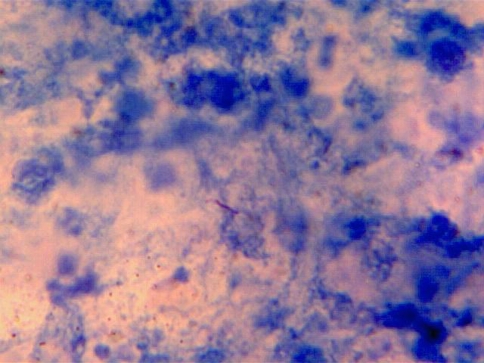
Fig. 3.
Photomicrograph showing acid fast bacilli in cytology smear. (ZN stain: 100×)
Discussion
Primary tuberculosis is rarely found in the oral cavity. However, the tongue is the most common oral site for primary tuberculosis and 93% of oral lesions present as ulcers [5, 8]. A lowered host resistance due to primary or secondary immunosuppression and nutritional deficiencies form the spectrum of systemic predisposing factors in such cases. In cases with primary oral tuberculosis, the organisms are directly transferred from the infected sputum or infected raw cow milk to the oral mucous membranes, open pulp of carious tooth, extraction wound, gingival margin or perforation of erupting tooth. In the oral cavity, soft tissues are more frequently involved compared to the bony structures. A regional extension of the soft tissue lesion may involve the underlying bone. However, involvement of the mandible by tuberculous infection is extremely rare as it contains less cancellous bone [9]. In the secondary type, oral tuberculosis coexists with the pulmonary disorder. Self-inoculation may take place from infected sputum or haematogenous seeding. However, the role of trauma cannot be underestimated, as the stratified squamous epithelium of the oral cavity normally resists direct penetration by the tubercle bacilli [10]. The most vulnerable areas in the oral cavity are gingiva, extraction sockets, buccal folds and tongue. Clinically, tuberculous ulcers can occur on the tip, lateral border, dorsal tongue towards midline, or base of tongue. Lesions are irregular, pale, with undermined margins, granulation tissue and sometimes have a thin slough [11]. Tubercular lesions are usually more irregular than punched out lesions of carcinoma [12].
Aird [13] has described five pathological types of this lesion:
Tubercular ulcers: It is painful and usually develops as a small tubercle which later on softens to form an ulcer on tip of the tongue. Typically they are shallow, often multiple, ovoid and lined with pale granulation tissue.
Tuberculoma: It originates as a lump anywhere in the tongue resembling lingual gumma. The lump in due course of time softens to form an ulcer.
Tuberculous fissure: They usually occur on the side of tongue and their extent can be appreciated only by separating their edges.
Tubercular papilloma: An overgrowth of the margins of tubercular fissures.
Tubercular cold abscess is due to breakdown of a tuberculoma.
The history, clinical examination and the radiographic findings play an important role in the diagnosis of oral tuberculosis. However, a clinical diagnosis of lingual tuberculosis is often not possible and techniques like FNAC can help in the early diagnosis of such lesions. Aspiration cytology is a useful cost effective investigative procedure which can be performed in outpatient clinics. It can provide early and reliable diagnosis in such lesions of tongue.
Clinically, differential diagnoses of oral ulcers include traumatic ulcer, aphthous ulcer, actinomycosis, syphilitic ulcer, Wegener’s granuloma and carcinoma. Diagnosis of lingual tuberculosis can generally be made on aspiration cytology but if required biopsy can also be performed for confirmation. Deeper biopsies are advocated in such cases as superficial biopsies may not be representative [12]. Histopathological evaluation reveals caseating epithelioid cell granulomas with Langhan’s and/or foreign body giant cells. Most often complete remission of the tubercular ulcer of tongue takes place after standard antitubercular treatment using drugs like isoniazid, rifampicin, pyrazinamide, and ethambutol for a period of 6 months [7].
Although rare, an early suspicion and timely intervention can lead to a favourable outcome in such cases, both for the patient and community. Even though primary tuberculosis in the oral cavity is a rare finding in an immunocompetent patient, it must be included in differential diagnosis of the mucosal lesions in the oral cavity. Fine needle aspiration cytology can act as an important diagnostic tool for an early and rapid diagnosis of such lesions.
References
- 1.Yepes JF, Sullivan J, Pinto A. Tuberculosis: medical management update. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2004;98:267–273. doi: 10.1016/j.tripleo.2004.05.012. [DOI] [PubMed] [Google Scholar]
- 2.Rinaggio J. Tuberculosis. Dent Clin North Am. 2003;47:449–465. doi: 10.1016/S0011-8532(03)00015-6. [DOI] [PubMed] [Google Scholar]
- 3.Sharma AB, Laishram DK, Sarma B. Primary tuberculosis of tongue. Ind J Pathol Microbiol. 2008;51:65–66. doi: 10.4103/0377-4929.40402. [DOI] [PubMed] [Google Scholar]
- 4.Vishwakarma SK, Jain S, Gupta M. Primary lingual tuberculosis presenting as a cold abscess tongue: a case report. Indian Journal Otolaryngology and Head and Neck Surgery. 2006;58:87–88. doi: 10.1007/BF02907752. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hashimoto Y, Tanioka H. Primary tuberculosis of the tongue: report of a case. J Oral Maxillofac Surg. 1989;47:744–746. doi: 10.1016/S0278-2391(89)80019-9. [DOI] [PubMed] [Google Scholar]
- 6.Prabhu SR, Sengupta SK. Bacterial infections due to mycobacteria. In: Prabhu SR, Wilson DF, Daftary DK, Johnson NW, editors. Oral diseases in the tropics. Oxford: Oxford University Press; 1993. pp. 195–202. [Google Scholar]
- 7.Garg RK, Singhal P. Primary tuberculosis of the tongue: a case report. J Contemp Dent Pract. 2007;8:74–80. [PubMed] [Google Scholar]
- 8.Bhatt AP, Dholakia HM. Tuberculosis of oral mucosa. J Indian Dent Assoc. 1974;46:161. [Google Scholar]
- 9.Dinkar AD, Prabhudesai B. Primary tuberculous osteomyelitis of the mandible: a case report. Dentomaxillofacial Radiology. 2008;37:415–420. doi: 10.1259/dmfr/73393014. [DOI] [PubMed] [Google Scholar]
- 10.Fujibayashi T, Takahashi Y, Yoneda T, et al. Tuberculosis of the tongue. A case report with immunologic study. Oral Surg Oral Med Oral Pathol. 1979;47:427–435. doi: 10.1016/0030-4220(79)90124-5. [DOI] [PubMed] [Google Scholar]
- 11.Bhat P, Mehndiratta A, D’Costa L, et al. Tuberculosis of tongue: a case report. Indian J Tuberc. 1997;44:31–33. [Google Scholar]
- 12.Das P, Suri V, Arora R, et al. Primary lingual tuberculosis mimicking malignancy: a report of two cases and review of literature. The Internet Journal of Pathology. 2007;6:2. [Google Scholar]
- 13.Khatri BK, Jhalla GS. Tuberculosis of tongue: a case report. Indian J Tuberc. 1971;18:58–59. [Google Scholar]