Abstract
Background
The Internet has become a major component to health care and has important implications for the future of the health care system. One of the most notable aspects of the Web is its ability to provide efficient, interactive, and tailored content to the user. Given the wide reach and extensive capabilities of the Internet, researchers in behavioral medicine have been using it to develop and deliver interactive and comprehensive treatment programs with the ultimate goal of impacting patient behavior and reducing unwanted symptoms. To date, however, many of these interventions have not been grounded in theory or developed from behavior change models, and no overarching model to explain behavior change in Internet interventions has yet been published.
Purpose
The purpose of this article is to propose a model to help guide future Internet intervention development and predict and explain behavior changes and symptom improvement produced by Internet interventions.
Results
The model purports that effective Internet interventions produce (and maintain) behavior change and symptom improvement via nine nonlinear steps: the user, influenced by environmental factors, affects website use and adherence, which is influenced by support and website characteristics. Website use leads to behavior change and symptom improvement through various mechanisms of change. The improvements are sustained via treatment maintenance.
Conclusion
By grounding Internet intervention research within a scientific framework, developers can plan feasible, informed, and testable Internet interventions, and this form of treatment will become more firmly established.
Keywords: Internet interventions, eHealth, Online treatment, Behavior change, Behavior change model, Scientific framework
Introduction
Over the past decade, a substantial effort has been made by researchers across the world to utilize the power of the Internet to create online prevention and treatment programs [1–5]. These Internet interventions are usually behavioral treatments that have been operationalized and transformed for delivery over the Internet. They are typically based on effective and empirically validated face-to-face interventions; personalized and tailored to the user; highly structured; semi-self-guided to fully self-guided; interactive; enhanced by graphics, animations, audio, and video; and often able to provide follow-up and feedback [6, 7]. The advantage of making treatment available to people with Internet access at any time and any location is considerable. Online treatments can reduce traditional face-to-face treatment barriers (i.e., inconvenience of scheduling appointments, missing work/school, traveling to and from a clinician’s office) [6], increase adherence [8], and reduce treatment time and costs [9].
Although there has been a recent proliferation of Internet health interventions [1, 4, 10], there has been no published theoretical model underlying these programs. The field needs a model of Internet interventions to help: (1) describe (and explain) how behaviors change and symptoms improve through use of Internet interventions; (2) guide program development and facilitate testing of the intervention; and (3) firmly establish this method of treatment with a theoretical foundation. To address this void, we have developed a model of behavior change and symptom improvement using Internet interventions.
Although the words are often used interchangeably, the term “model” should be distinguished from “theory.” While theories help explain or predict events by illustrating the relationships among a set of variables, models pull from a number of theories and other models to help explain a particular problem in a specific setting or context [11]. As is often true with models, our model of behavior change through an Internet intervention is informed by multiple theories, as well as empirical findings and clinical experience. No single theory or model fits all cases, and many theories will overlap as they predict the route to symptom improvement [11]. Using models will help us better understand both behavior and symptoms, allowing us to translate our empirical findings into useful strategies for improving health outcomes.
In designing this Internet intervention model, multiple theories from numerous disciplines were integrated to help conceptualize behavior change, measure the change, and identify the factors that might contribute to symptom improvement. Specifically, this model combines information from theories of motivation, other psychological models, social marketing/advertising strategies, Web-based design/development techniques, information architecture and design, models of knowledge transfer and behavior change, and general research and clinical experience [12–18]. Although various books provide recommendations for effective website design [19], we are unaware of literature documenting how technology, specifically the Internet, can be used to promote behavior change and subsequent symptom improvement with an underlying theoretical model. The Internet intervention model facilitates this goal by providing a framework to develop and test Internet interventions designed to promote symptom improvement, helping to conceptualize, identify, and measure factors that may determine behavior change and symptom improvement.
The Internet Intervention Model
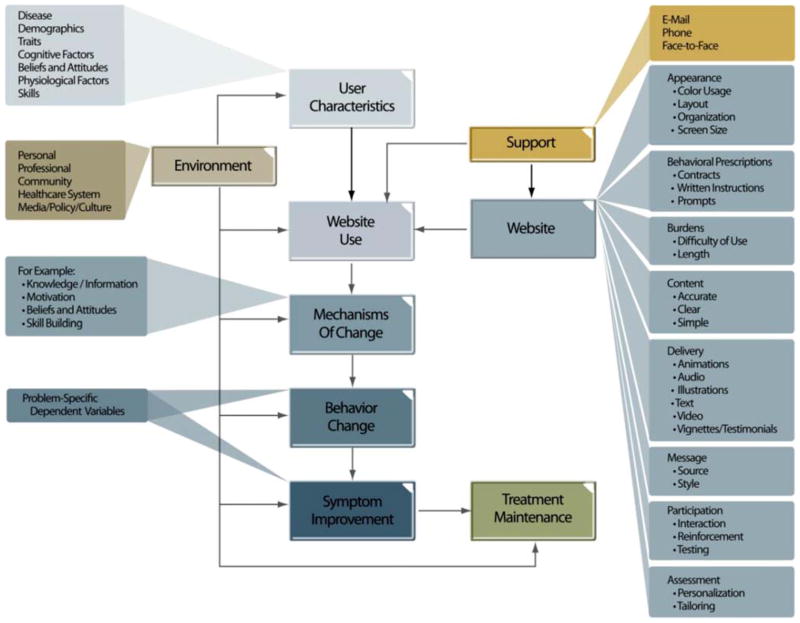
We hypothesize that effective Internet intervention programs will produce change in behaviors and reduce unwanted symptoms (as well as maintain improvement) via the following steps: the user, influenced by environmental factors, affects website use and adherence, which is influenced by support and website characteristics. Website use leads to behavior change via different mechanisms of change (e.g., knowledge and motivation). Behavior change impacts physiology and target behaviors to bring about symptom improvement, and treatment maintenance helps users maintain these gains. See Fig. 1 for a depiction of these steps.
Fig. 1.
Model of Internet interventions
There are nine major components to the Internet Intervention Model (e.g., Website). Each of these model components contain areas that can be observed, evaluated, and in many cases, manipulated (e.g., appearance). The elements are the specific examples in each area (e.g., color usage, layout). Each of the major components will be presented along with the associated areas and elements.
User Characteristics
The user (patient, research participant, consumer) of Internet interventions brings the most complicated and diverse set of variables or characteristics for evaluation. Some of the characteristics are fixed and cannot be manipulated, such as age or gender, but many can be modified (e.g., cognitive factors, beliefs and attitudes, and skills). In fact, these user characteristics may serve as predictor variables [20, 21] or be targeted for change along with the identified problem. In addition, interventions can be tailored based on an individual user’s characteristics. For example, treatment recommendations could be matched to fit a particular user’s stage of readiness to change.
There are seven main areas of user characteristics incorporated into this model. They include disease, including pathology and severity of the disease, and the problem being targeted; demographics, including age, gender, and socioeconomic status (SES); traits, including personality, temperament, and intelligence; cognitive factors, including cognitive style (verbal vs. visual), information processing, developmental stage, goal setting and pursuit, decision making, judgment, self-efficacy, knowledge, and self-regulatory strategies (e.g., planning); beliefs and attitudes, including treatment expectations, intentions, interest, motivation, readiness for change (stage of change), self-efficacy, and perceived benefits and barriers to treatment; physiological factors, including motor functioning; and skills related to both psychological mindedness and computer abilities.
Environment
The environment is composed of multiple influences, including family/significant others/friends, employer/organization/school, the health care system, community, and societal level influences, such as the media, policy and cultural factors. The environment can provide support or serve as a barrier to individuals implementing a self-help treatment program [22]. In the Internet intervention model, environmental factors, similar to Glasgow’s “Pyramid of Influences,” [22] can impact each component of the model in potentially significant ways. Environmental factors can influence user characteristics by shaping a user’s knowledge or motivation to use this treatment approach. Use of the website is partially determined by the support or hindrance of environmental factors such as level of ease accessing the Internet or family members encouraging or discouraging use. Change mechanisms can be influenced by the support of the user’s school; for example, within a weight loss intervention, a school lunch program that makes nutritious lunches available can affect the motivation of obese children. Behavior change is also affected by environmental factors; family and the community can shape behaviors through positive or negative reinforcement. Symptom improvement can be influenced by changes in the user’s surroundings that help to reduce significant symptoms. For example, in insomnia treatment, users are encouraged to examine environmental factors that may contribute to their sleep difficulties, such as noises (e.g., cars honking, loud music from neighbors) or extreme temperatures. Problematic sleep symptoms can be reduced if environmental triggers are identified and corrected. Finally, maintenance of treatment can be influenced by larger societal factors such as public policy. For example, laws restricting smoking can enhance smoking cessation outcomes [23]. Connections between environment and other components of the model can be identified, measured, and evaluated to provide critical information regarding the overall impact of the environment.
Website
The web program, or website, is the application by which the treatment is delivered. The website component is made up of eight main areas, including appearance, behavioral prescriptions, burdens, content, delivery, message, participation, and assessment. Together, these eight areas comprise how the application is developed and functions. Each of these areas contains elements that can be manipulated and modified to provide the most robust treatment. Although preliminary research has demonstrated the importance of some of these elements [24–26], additional work is necessary to determine the best use of each. However, determining an optimal set of elements is complicated by the wide range of intervention types, patient populations, computing systems, and technologies as different elements of varying degrees will likely be necessary depending on the program focus area. These elements dictate the development and use of an Internet intervention.
Appearance is simply the look and feel of the application. Elements include use of color, page/screen layout, organization of content, and screen size. This will, in part, dictate the program’s appeal to the user. Although this issue may seem unimportant, appearance may be critical as it likely encourages initial (and continued) use of the website and may increase overall engagement.
Behavioral prescriptions instruct the user on what to do to address the targeted problem. These prescriptions are part of the treatment and are also designed to increase commitment and boost adherence. Behavioral contracts, concerning what the patient is willing to do (and when), and written instructions are known to enhance behavior change [27]. Additionally, incorporating prompts to engage the user in the prescribed behaviors has also proved beneficial [28]. Examples of such prompts include: automated e-mails sent to all users or users meeting certain conditions (e.g., those who failed to complete an assignment); personalized e-mails sent based on predetermined algorithms or from an individual (e.g., e-mails sent by a clinician when users endorse suicidal ideation); and phone calls triggered by the program or clinician. The use of prompts has significant potential, particularly given the possible integration of mobile phones, PDAs, pagers, and other wireless devices that can all be employed in the deliverance of prompts [29, 30].
Burdens of using the website are different from the barriers to using the program specified in the environment section. Unlike barriers, burdens are specific to the content of the program and not the technological or environmental obstacles to accessing the Internet or to using the program. This includes difficulty of use, covering issues such as poor application navigation and intervention length. At this point, it is not clear how much content is necessary to impact behavior change. It is possible that only core components of a treatment are necessary to reduce symptoms, suggesting that developers and researchers might consider creating “short form” Internet interventions. It is also possible that, if the treatment is too long, users may not be able to persevere, potentially resulting in premature withdrawal and poor outcomes. Although intervention length may vary by the targeted problem, research focused on this area may help establish some general guidelines regarding amount of time individuals are willing to use these applications both on a per sitting, as well as total use, basis.
Dismantling or deconstruction studies, where individual components of an intervention are examined to determine which components are producing the greatest impact, will be an important avenue of research. In fact, Internet interventions lend themselves perfectly to deconstruction studies given that the treatments are standardized and controlled. The ability to precisely provide only certain aspects of a treatment as a way of determining the critical treatment components sets this form of treatment apart from others. Identifying which core components of treatment are necessary for everyone, as well as determining which additional modules are needed by only some users, can help provide treatments that are more efficient, effective, and relevant. Some researchers have already begun conducting these important deconstruction studies with computer and Internet-based programs [31–33], and continued research could help lead to the discovery of findings rarely possible before this mode of delivery.
Content, the actual treatment information, of the website may be the single most important component of the program. Without good content, it is unlikely that behavior would change or symptoms would improve. Given that there is a significant amount of misinformation on the Internet [34], providing accurate, clear, and simple information is critical to creating and delivering efficacious applications that will be well-received.
The delivery area of the website component contains ways in which the content can be delivered. These include using animations, audio (sound that either coincides with the screen text or sound that provides additional content), illustrations/graphics, text, video (recorded content of live or animated information), and vignettes/testimonials/stories. Each of these elements provide a different way of delivering content that may impact use of the system due to the individual’s engagement, usability, and enjoyment of the program, as well as potentially impacting specific mechanisms of change. For example, a particular vignette may resonate with a user and, therefore, have a stronger effect on both this individual’s knowledge (they learn and understand the concept better given the vignette) and motivation (they identify with the story, perhaps helping to normalize his/her situation and increase motivation to continue using the program and improve the condition). These elements have begun to be examined, with an attempt to ascertain which elements are necessary, helpful, preferred, or superfluous. Early findings suggest that users prefer audio, graphics, and interactivity as elements of Internet interventions [24–26].
The message focuses on the source and style of the content, providing important information about who created the content and how that content is presented. These are hypothesized to impact user engagement and other mechanisms of change, including acquisition of knowledge and motivation. The two most important source characteristics are credibility, a combination of trustworthiness and expertise, and likeability, how much users enjoy using the site [35, 36]. There is significant literature outside of Internet treatments demonstrating that the source of a message dictates its “believability” and ability to induce behavior change [35–38]. For example, one might hypothesize that a website will have greater impact if the message source is a major university as opposed to a pharmaceutical or little known industry sponsored site. Users may believe that the content is more credible given an academic source. The style of the application is also important and should match the intended population. For example, a pediatric focused intervention may have greater influence if the style is more child-focused (e.g., use of cartoons) rather than text heavy.
Participation is focused on the program’s ability to engage and involve the user in the treatment. These elements include interaction, reinforcements (rewards), and testing (questions, quizzes). Interaction can be described as elements of an intervention in which the user interfaces with the system producing a cause–effect action. This might be as simple as clicking a button to move to a new screen or a more complex task such as arranging images on a screen as part of a learning task.
Reinforcement is utilized to help motivate the user to learn and progress through the program. For example, a child user can be rewarded for completing a module or unit within a pediatric intervention by making an online game available. Providing feedback can serve as a significant form of reinforcement. Testing also provides a method to teach (or highlight) specific content that can be presented through the use of multiple choice or true/false questions with corrective feedback.
Finally, assessment refers to the system’s ability to measure the needs of the user, personalize the program, and provide tailored content and recommendations. The elements of personalization and tailoring are critical to Internet interventions and could be considered some of the primary elements distinguishing Internet interventions from other self-help programs. Personalization relates to the use of specific program content with which the user may personally identify. For example, there may be gender-specific or ethnic-specific content presented only to those users with particular characteristics. Tailored content is information that specifically meets the needs of the individual user. For example, in an Internet intervention for insomnia, patients are queried about their daily sleep behaviors and symptoms (e.g., number of night-time awakenings), and then, based on the user’s responses to these sleep questions, specific sleep instructions are given (e.g., program restricts time window for sleep) [39]. Tailoring can reduce the overall amount of information provided, as users only receive what they need or want. The ability to personalize or tailor the content to a user’s specific needs or desires has already been shown to have an impact on behavior change and outcome [40, 41]. It likely also further engages the user and may increase the individual’s desire to use the system.
Website Use
Website use is the actual utilization of the intervention. Usage is affected by the user characteristics, environmental factors, the actual website, and support. It can be hypothesized that individuals will use the Web program given specific user characteristics (e.g., users with adequate motivation), environment (e.g., family members encourage use), website elements (e.g., content is simple and clear and the program is engaging), and possible support (e.g., e-mails from clinicians). Determining which characteristics, variables, and elements are necessary or even ideal for the success of different treatment programs is an important endeavor; and one in which the research has only just begun.
In a sense, the website and website use components of this model could be considered a “black box” in that any type of prevention or treatment program could fit here. For example, the intervention could be delivered using mobile phones (or face-to-face for that matter). Regardless of the delivery mechanism, users approach the intervention with a set of user characteristics, and use of that intervention is shaped by various influences including the environment and support. Ultimately, behavior change and symptom improvement occur via various mechanisms of change. Because we are focused on developing and providing Internet interventions, the intervention component of this model focuses on the critical components of the website and its use.
Adherence is a critical area of investigation within the Internet intervention model and a major aspect of website use. As with any health intervention, better understanding adherence can help maximize the impact of treatment, in this case Internet-delivered treatment [42]. In fact, the World Health Report of 2002 declared that adherence was the primary determinant to the effectiveness of treatment [43], with good adherence improving the effectiveness of interventions aimed at promoting healthy lifestyles [44]. Identifying predictors, obstacles, and potential solutions for nonadherence is critical to success, particularly given the fact that participants can both engage and disengage with this type of intervention very easily.
While not using the website as prescribed or dropping out altogether typically reflects a decreased “treatment dose” and implies suboptimal disease management, this should be reconsidered with respect to Internet interventions. People may approach and use Internet interventions differently than any other form of treatment, and it is critical to take into consideration user expectations [45]. Users may expect to complete a limited subset of a program to satisfy their needs, whereas other users may plan and need to complete the full treatment offered. Given these different uses of an Internet intervention, it is much more difficult to make sense of usage data, as someone who appears to be a “dropout” or nonadherent user may actually be someone who obtained “success” with a low treatment dose [45]. Testing this notion through the Internet intervention model will provide valuable information in this important debate.
The Internet intervention model lends itself to testing the impact of adherence on behavior change, as well as testing how other factors influence adherence. More specifically, the model can capture and assess the key factors Eysenbach identified as influencing the shape and steepness of attrition curves [46]: (1) factors related to the intervention itself (e.g., website), (2) participant factors (described in our model as user characteristics), and (3) push factors (e.g., prompts, described as support in our model). Some researchers have been incorporating personalized e-mails and telephone support as methods of increasing adherence [47–49]. By testing this Internet intervention model, the impact of these stepped care approaches on behavior change can be assessed. In a world of limited resources, this information can then help developers of these interventions determine the necessary amount of support, time, and expertise an individual needs.
Support
For purposes of wide-scale dissemination, it may be the ultimate achievement to develop a stand-alone Internet intervention that is able to significantly and independently impact behavior change, eliminate symptoms, and prevent the problems from returning. There is research indicating that external support of the application may improve adherence and outcomes for many disorders [33, 47, 50]; however, this is not always found to be the case [48, 49], and research is needed in order to determine what types of support are effective for which treatments. Within the model, support directly impacts the user’s adherence to using the program (website use). Support also directly impacts the development of the system (website), as this component needs to be implemented into the design of the application.
Support can be delivered in various ways, including personalized e-mails, instant messaging communication, phone sessions, and face-to-face meetings. Costs must also be considered [9] as the incorporation of any support increases the time, effort, and finances to implement an Internet intervention and can significantly reduce the ability to disseminate this type of intervention on any grand scale. As the needs of external support are reduced, the reach of Internet interventions exponentially increases. Without human involvement, Internet interventions can serve as many people as the computer servers are scaled to support.
Mechanisms of Change
Mechanisms of change bring about the desired behavior change and ultimate symptom improvement, functioning as the catalysts for transformation [51]. Examples of mechanisms of change include knowledge/information, motivation, attitude, beliefs, skill building, self-efficacy, cognitive restructuring (self-talk), modeling, self-monitoring, and affect management. It is important to note that many of the user characteristics can be modified through intervention use and serve as mechanisms of change. For example, knowledge, defined as a cognitive factor under user characteristics, can also be a mechanism of change; as the user gains information, she/he may be able to enact the behavior change because of the new knowledge. Testing which mechanisms of change within the model are responsible for bringing about behavior change and ultimate symptom improvement is critical to Internet intervention research as these findings can then be used to refine and improve future Internet interventions.
Behavior Change
While the ultimate measure of success of most Internet interventions is symptom improvement, this is usually dictated by the occurrence of behavior change. Behavior change is typically necessary for the symptoms to improve. The behaviors that are identified for change are dependent variables measured to determine intervention success. The behavior change variables are usually specific to the problem or intervention that is being studied or treated. For example, in insomnia research, sleep-related behaviors such as restriction of time in bed or improved sleep hygiene are targeted for change. However, attempts to change these behaviors would obviously have little value in smoking cessation treatment. It is important that researchers identify and understand which behaviors are critical to change to reduce associated symptoms and achieve a positive outcome.
Symptom Improvement
Symptom improvement (and then maintenance of these gains) is the goal of most Internet interventions. The symptoms measured in symptom improvement will be affected by the modification of behaviors in the behavior change component via the change mechanisms. For example, depressive affect (the symptom) may be reduced by helping the user to incorporate cognitive restructuring techniques (the change mechanism) by monitoring and challenging distorted thoughts in a thought record (the behavior). Similarly, obesity (the symptom) can be, in part, addressed by improving eating habits and incorporating exercise into one’s routine (the change mechanism) by consuming healthier foods and walking each day (the behavior). Obviously, the symptoms are specific to the problem and treatment application.
Researchers and clinicians tend to focus on the physical and psychological changes seen in symptom improvement, but there are two other important areas that should be examined as part of this component of the model: cost (financial) and time (of user and possibly of clinician). Cost-effectiveness analyses consider the monetary and opportunity costs relative to the benefits and are critical to determining whether the application provides sufficient improvements in health outcomes to justify the cost. It is important to consider that an Internet intervention may not have to be as effective as the gold standard (typically face-to-face care) to still be highly cost-effective and a worthy treatment approach. The benefits of such a system, including widespread use and accessibility, may far outweigh reduced effectiveness compared to the gold standard. The application should, however, meet some minimum requirements of effectiveness [9].
Within Internet intervention research, more investigation is needed with respect to time of the clinician and user [52]. While some interventions are purely self-guided applications, other researchers have developed semi-self-guided applications that require clinician assistance. Examining the time savings (and thus cost savings) of the clinicians is key. The goal is to reduce clinician time (and requisite training needs for supportive clinicians) while maintaining significant symptom improvement. The less the clinician needs to be involved, the greater the number of individuals that can be helped. For example, there is a huge need for psychological services for the treatment of insomnia, a significant health problem with one third of the adult population reporting symptoms of insomnia and approximately 10% meeting diagnostic criteria for an insomnia disorder [53–56]. However, most of those who suffer from chronic insomnia do not have access to psychologically based treatment [57]. If, however, a smaller amount (if any) of clinician time is necessary to help bring about symptom relief, then a much larger percentage of this unserved population could receive care. It is possible that Internet interventions designed to treat some disorders (e.g., PTSD) will require more clinician assistance than those treating other disorders (e.g., blood glucose management), and this question should be evaluated empirically within the model.
Treatment Maintenance
Eventually, some form of relapse prevention is typically provided within the Internet intervention to help users maintain treatment gains [58]. Relapse prevention information is incorporated in order to help the user reduce the possibility of problems returning and develop plans to address future problems should they occur. Once symptom improvement is achieved, treatment maintenance can be difficult, depending on the original disorder. However, relapse prevention can be used to avert deterioration and maintain successes and can be used to enhance the maintenance of behavior change and symptom improvements [59].
Summary
The model for Internet interventions proposes that individuals approach an Internet intervention with a set of user characteristics that are influenced by environmental factors. The user characteristics in turn impact their use of the website. Website use is also influenced by website characteristics, adherence to the site, and support offered by the program to assist users in their use of the intervention. The model then predicts that website use leads to behavior change via various mechanisms of change and that the behavior changes result in symptom improvement. Treatment success is maintained through relapse prevention.
Evaluation of the Internet Intervention Model
In order to test the model for Internet interventions, a final component must be superimposed on Fig. 1 called measurement. The usefulness of any model is determined by how well it can be evaluated, and the current model and its components can be operationalized and measured in numerous ways. Measurement indicates that each component, area, and element of the model can be examined and measured. For example, user characteristics may predict use of the website, as well as ultimate symptom improvement, and evaluating these user variables (e.g., disease severity, readiness for change) could help future developers tailor the intervention accordingly. The environment affects all components of the model, and measuring these influences is important to understanding the impact of the environment on the user, usage of the system, change mechanisms, changing of behaviors, symptom improvement, and treatment maintenance.
Measurement of the website and its various parts is a unique aspect of this model. Preliminary research has already been conducted in this area [24–26]; however, much more work is needed to understand how best to develop, operationalize, and deliver Internet interventions. Clearly, some elements will need to be incorporated into all Internet interventions (e.g., understandable content); however, different elements (and varying amounts of these elements) will be necessary for diverse treatments and populations. Although evaluating different aspects of the website (e.g., color, layout, organization) is a time-intensive undertaking, it is essential in helping to predict and explain behavior change via Internet interventions.
Examining website use is another distinctive aspect to the model, potentially providing the most meaningful information to researchers, clinicians, and users. Determining which aspects of a treatment application are utilized may uncover the most helpful aspects of treatment. Dismantling the program and determining which treatment elements help result in positive change should lead to more efficient yet still highly effective programs utilizing only the necessary ingredients. Measuring the associated support component will contribute to a greater understanding of usage and adjunctive assistance. Building in ways of addressing problems with adherence, such as stepped care approaches, and measuring the resulting changes in adherence can provide information and understanding that reaches beyond that of treatment programs delivered via the Internet.
While not unique to Internet interventions, it is critical to also measure the mechanisms of change, behavior change, symptom improvement, and treatment maintenance components to determine the ability of Internet interventions to deliver effective treatments. While feasibility and efficacy data have been established in Internet intervention research, true effectiveness studies are needed. It is this data, based on scientifically grounded Internet interventions, that will fully establish these programs and this form of treatment delivery.
Conclusion
Limitations
Before considering the implications of the model, two important limitations of the model should be noted. First, the model is an oversimplification of how Internet interventions produce behavior change. Although simplification encourages understanding and facilitates use, such brevity fails to capture all aspects of intervention processes. Second, the presentation of the model in Fig. 1 depicts a linear process. Despite this linear depiction, however, the model is not conceptualized as a unidirectional process. Instead, steps can be repeated or even occur out of order. For example, it is possible that environmental influences impact users after they have begun using the system, thus potentially impacting users’ adherence midway through the program. Furthermore, the mechanisms of change, behavior change, and symptom improvement may all have an impact on user characteristics which in turn continue to affect these processes. To clarify, the model depicts a recurrent cyclical process. Users will continue to use the Internet intervention even as they change behaviors and experience symptom improvement, which will cause changes in their user characteristics, which will impact their continued use of the system, and so on.
Implications of the Model
This model extends our knowledge about the development, testing, and usage of Internet interventions and has both important clinical and research implications. This model of Internet interventions helps identify the various components of an Internet intervention and presents the relationships among the various components in an effort to explain and predict behavior change and symptom improvement across interventions. By drawing on multiple disciplines and previously established theories and models, this model enables us to conceptualize, identify, and measure the factors likely to contribute to behavior change (and symptom improvement) in Internet interventions. It is critical for clinicians and researchers to understand how health behavior changes and to transform that knowledge about behavior into useful strategies for health enhancement [11]. The Internet intervention model enables the field to do just that.
Future Directions
This model can be used to help developers plan feasible, informed, and testable Internet interventions. The model can also help researchers identify their assumptions behind interventions and direct them to identify which components, areas, and elements need to be examined and measured. It encourages clinicians and researchers to evaluate the various aspects of their Internet interventions. Finally, as researchers begin testing the model with their interventions and various sample populations, changes to the model can be considered to add explanatory power to the model. That is, data can be gathered across interventions to further support (or not support) the model presented here.
Acknowledgments
This work was supported by the National Institutes of Health National Institute of Mental Health Grant R34MH70805 and the National Institute of Child Health and Development Grant RO1HD028160.
Contributor Information
Lee M. Ritterband, Email: LEER@virginia.edu, Department of Psychiatry and Neurobehavioral Sciences, Behavioral Health and Technology, University of Virginia Health System, P.O. Box 801075, Charlottesville, VA 22908, USA
Frances P. Thorndike, Department of Psychiatry and Neurobehavioral Sciences, Behavioral Health and Technology, University of Virginia Health System, P.O. Box 801075, Charlottesville, VA 22908, USA
Daniel J. Cox, Department of Psychiatry and Neurobehavioral Sciences, Center for Behavioral Medicine Research, University of Virginia Health System, P.O. Box 801075, Charlottesville, VA 22908, USA
Boris P. Kovatchev, Department of Psychiatry and Neurobehavioral Sciences, Diabetes Technology, University of Virginia Health System, P.O. Box 801075, Charlottesville, VA 22908, USA
Linda A. Gonder-Frederick, Department of Psychiatry and Neurobehavioral Sciences, Center for Behavioral Medicine Research, University of Virginia Health System, P.O. Box 801075, Charlottesville, VA 22908, USA
References
- 1.Murray E, Burns J, See TS, Lai R, Nazareth I. Interactive Health Communication Applications for people with chronic disease. Cochrane Database Syst Rev. 2005;(4):CD004274. doi: 10.1002/14651858.CD004274.pub4. [DOI] [PubMed] [Google Scholar]
- 2.Wantland D, Portillo C, Holzemer W, Laughter R, McGhee E. The effectiveness of web-based vs. non-web-based interventions: A meta-analysis of behavioral change outcomes. J Med Internet Res. 2004;6:e40. doi: 10.2196/jmir.6.4.e40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Griffiths KM, Christensen H. Review of randomised controlled trials of Internet interventions for mental health disorders and related conditions. Clin Psychol. 2006;10:16–29. [Google Scholar]
- 4.Marks IM, Cavanagh K, Gega L. Hands-On Help: Computer-Aided Psychotherapy. New York: Psychology; 2007. [Google Scholar]
- 5.Stinson J, Wilson R, Gill N, Yamada J, Holt J. A systematic review of Internet-based self-management interventions for youth with health conditions. J Pediatr Psychol. 2009;34:495–510. doi: 10.1093/jpepsy/jsn115. [DOI] [PubMed] [Google Scholar]
- 6.Ritterband LM, GonderFrederick LA, Cox DJ, Clifton AD, West RW, Borowitz SM. Internet interventions: In review, in use, and into the future. Prof Psychol Res Pract. 2003;34:527–534. [Google Scholar]
- 7.Barak A, Proudfoot JG, Klein B. Defining Internet-supported therapeutic interventions. Ann Behav Med. 2009 doi: 10.1007/s12160-009-9130-7. [DOI] [PubMed] [Google Scholar]
- 8.Celio AA, Winzelberg AJ, Wilfley DE, et al. Reducing risk factors for eating disorders: Comparison of an Internet- and a classroom-delivered psychoeducational program. J Consult Clin Psychol. 2000;68:650–657. [PubMed] [Google Scholar]
- 9.Tate DF, Finkelstein EA, Khavjou O, Gustafson A. Cost effectiveness of Internet interventions: Review and recommendations. Ann Behav Med. 2009 doi: 10.1007/s12160-009-9131-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Barak A, Hen L, Boniel-Nissim M, Shapira N. A comprehensive review and a meta-analysis of the effectiveness of Internet-based psychotherapeutic interventions. J Technol Hum Serv. 2008;26:109–160. [Google Scholar]
- 11.Glanz K, Lewis F, Rimer B. Linking theory, research, and practice. In: Glanz K, Lewis F, Rimer B, editors. Health Behavior and Health Education: Theory, Research, and Practice. 2. San Francisco: Jossey-Bass; 1997. pp. 19–35. [Google Scholar]
- 12.Rosenstock IM. Historical origins of the health belief model. Health Educ Monogr. 1974;2:328–335. [Google Scholar]
- 13.Prochaska JO, DiClemente CC. The transtheoretical approach. In: Norcross JC, Goldfried MR, editors. Handbook of Psychotherapy Integration. New York: Basic Books; 1992. pp. 300–334. [Google Scholar]
- 14.Lefebvre RC, Rochlin L. Social marketing. In: Glanz K, Lewis FM, Rimer B, editors. Health Behavior and Health Education: Theory, Research, and Practice. 2. San Francisco: Jossey-Bass; 1997. pp. 384–402. [Google Scholar]
- 15.Miller NE, Dollard J. Social Learning and Imitation. New Haven: Yale University Press; 1941. [Google Scholar]
- 16.Matarazzo JD, Weiss SM, Herd JA, Miller NE, Weiss SM, editors. Behavioral Health: A Handbook of Health Enhancement and Disease Prevention. New York: Wiley; 1984. [Google Scholar]
- 17.Casmir FL, editor. Building communication theories: A socio/cultural approach. Hillsdale: Erlbaum; 1994. [Google Scholar]
- 18.Fisher JD, Fisher WA. The information-motivation-behavioral skills model. In: DiClemente R, Crosby R, Kegler M, editors. Emerging Theories in Health Promotion Practice and Research. 2. San Francisco: Jossey Bass; 2002. pp. 40–70. [Google Scholar]
- 19.Nielson J. Designing Web Usability. Indianapolis: New Riders; 2000. [Google Scholar]
- 20.Magee JC, Ritterband LM, Thorndike FP, Cox DJ, Borowitz SM. Exploring the relationship between parental worry about their child’s health and usage of an Internet intervention for pediatric encopresis. J Pediatr Psychol. 2009;34:530–538. doi: 10.1093/jpepsy/jsn091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tercyak KP, Abraham AA, Graham AL, Wilson LD, Walker LR. Association of multiple behavioral risk factors with adolescents’ willingness to engage in eHealth promotion. J Pediatr Psychol. 2009;34:457–469. doi: 10.1093/jpepsy/jsn085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Glasgow RE, Eakin EG. Issues in diabetes self-management. In: Shumaker SA, Schron EB, Ockene JK, McBee WL, editors. The Handbook of Health Behavior Change. 2. New York: Springer; 1998. p. 435. [Google Scholar]
- 23.Biener L, Abrams DB, Follick MJ, Dean L. A comparative evaluation of a restrictive smoking policy in a general hospital. Am J Public Health. 1989;79:192–195. doi: 10.2105/ajph.79.2.192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ritterband LM, Cox DJ, Gordon T, et al. The inclusion of audio, graphics, and interactivity in an internet intervention for pediatric encopresis. Child Health Care. 2006;35:47–59. [Google Scholar]
- 25.Danaher BG, Boles SM, Akers L, Gordon JS, Severson HH. Defining participant exposure measures in web-based health behavior change programs. J Med Internet Res. 2006;8:e15. doi: 10.2196/jmir.8.3.e15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hurling R, Fairley BW, Dias MB. Internet-based exercise intervention systems: Are more interactive designs better? Psychol Health. 2006;21:757–772. [Google Scholar]
- 27.Cox DJ, Tisdelle DA, Culbert JP. Increasing adherence to behavioral homework assignments. J Behav Med. 1988;11:519–522. doi: 10.1007/BF00844844. [DOI] [PubMed] [Google Scholar]
- 28.Ritterband LM, Borowitz SM, Cox DJ, et al. Using the Internet to provide information prescriptions. Pediatrics. 2005;116:e643–e647. doi: 10.1542/peds.2005-0404. [DOI] [PubMed] [Google Scholar]
- 29.Hurling R, Catt M, De Boni M, et al. Using Internet and mobile phone technology to deliver an automated physical activity program: Randomized controlled trial. J Med Internet Res. 2007;9:e7. doi: 10.2196/jmir.9.2.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Patrick K, Raab F, Adams MA, et al. A text message-based intervention for weight loss: Randomized controlled trial. J Med Internet Res. 2009;11:e1. doi: 10.2196/jmir.1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Greist JH, Marks IM, Baer L, et al. Behavior therapy for obsessive-compulsive disorder guided by a computer or by a clinician compared with relaxation as a control. J Clin Psychiatry. 2002;63:138–145. doi: 10.4088/jcp.v63n0209. [DOI] [PubMed] [Google Scholar]
- 32.Wright J, Wright A, Albano AM, et al. Computer-assisted cognitive therapy for depression: Maintaining efficacy while reducing therapist time. Am J Psychiatry. 2005;162:1158–1164. doi: 10.1176/appi.ajp.162.6.1158. [DOI] [PubMed] [Google Scholar]
- 33.Tate DF, Jackvony EH, Wing RR. A randomized trial comparing human e-mail counseling, computer-automated tailored counseling, and no counseling in an Internet weight loss program. Arch Intern Med. 2006;166:1620–1625. doi: 10.1001/archinte.166.15.1620. [DOI] [PubMed] [Google Scholar]
- 34.Eysenbach G, Powell J, Kuss O, Sa ER. Empirical studies assessing the quality of health information for consumers on the World Wide Web: A systematic review. JAMA. 2002;287:2691–2700. doi: 10.1001/jama.287.20.2691. [DOI] [PubMed] [Google Scholar]
- 35.Petty RE, Cacioppo JT. Motivational factors in consumer response to advertisements. In: Geen RG, Beatty WW, Arkin RM, editors. Human Motivation. New York: Allyn and Bacon; 1984. pp. 418–454. [Google Scholar]
- 36.Beck RC. Motivation: Theories and Principles. New Jersey: Prentice-Hall; 1990. [Google Scholar]
- 37.US Department of Commerce. A Nation Online: How Americans are Expanding their Use of the Internet. US Department of Commerce. Washington: Government Printing Office; 2002. [Google Scholar]
- 38.Faison EW. Advertising: A Behavioral Approach for Managers. New York: Wiley; 1980. [Google Scholar]
- 39.Ritterband LM, Thorndike FP, Gonder-Frederick L, et al. Efficacy of an Internet-based behavioral intervention for adults with insomnia. Arch Gen Psychiatry. 2009;66:692–698. doi: 10.1001/archgenpsychiatry.2009.66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Brug J, Oenema A, Campbell M. Past, present, and future of computer-tailored nutrition education. Am J Clin Nutr. 2003;77:1028S–1034S. doi: 10.1093/ajcn/77.4.1028S. [DOI] [PubMed] [Google Scholar]
- 41.Oenema A, Tan F, Brug J. Short-term efficacy of a web-based computer-tailored nutrition intervention: Main effects and mediators. Ann Behav Med. 2005;29:54–63. doi: 10.1207/s15324796abm2901_8. [DOI] [PubMed] [Google Scholar]
- 42.Christensen H, Griffiths KM, Farrer L. Adherence in Internet interventions for anxiety and depression. J Med Internet Res. 2009;11:e13. doi: 10.2196/jmir.1194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.World Health Organization. The World Health Report 2002: Reducing Risks, Promoting Healthy Lifestyle. Geneva: WHO; 2002. [Google Scholar]
- 44.Clark DO. Issues of adherence, penetration, and measurement in physical activity effectiveness studies. Med Care. 2001;39:409–412. doi: 10.1097/00005650-200105000-00001. [DOI] [PubMed] [Google Scholar]
- 45.Christensen H, Mackinnon A. The law of attrition revisited. J Med Internet Res. 2006;8:e20. doi: 10.2196/jmir.8.3.e20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Eysenbach G. The law of attrition. J Med Internet Res. 2005;7:e11. doi: 10.2196/jmir.7.1.e11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Spek V, Cuijpers P, Nyklicek I, Riper H, Keyzer J, Pop V. Internet-based cognitive behaviour therapy for symptoms of depression and anxiety: A meta-analysis. Psychol Med. 2007;37:319–328. doi: 10.1017/S0033291706008944. [DOI] [PubMed] [Google Scholar]
- 48.Andersson G, Lundström P, Ström L. Internet-based treatment of headache: Does telephone contact add anything? Headache. 2003;43:353–361. doi: 10.1046/j.1526-4610.2003.03070.x. [DOI] [PubMed] [Google Scholar]
- 49.Klein B, Austin D, Pier C, et al. Internet-based treatment for panic disorder: Does frequency of therapist contact make a difference? Cogn Behav Ther. 2009;38:100–113. doi: 10.1080/16506070802561132. [DOI] [PubMed] [Google Scholar]
- 50.Christensen H, Griffiths KM, Korten AE, Brittliffe K, Groves C. A comparison of changes in anxiety and depression symptoms of spontaneous users and trial participants of a cognitive behavior therapy website. J Med Internet Res. 2004;6:e46. doi: 10.2196/jmir.6.4.e46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kazdin AE. Mediators and mechanisms of change in psychotherapy research. Annu Rev Clin Psychol. 2007;3:1–27. doi: 10.1146/annurev.clinpsy.3.022806.091432. [DOI] [PubMed] [Google Scholar]
- 52.Marks I, Cavanagh K. Computer-aided psychological treatments: Evolving issues. Annu Rev Clin Psychol. 2009;5:121–141. doi: 10.1146/annurev.clinpsy.032408.153538. [DOI] [PubMed] [Google Scholar]
- 53.Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders, an opportunity for prevention? JAMA. 1989;262:1479–1484. doi: 10.1001/jama.262.11.1479. [DOI] [PubMed] [Google Scholar]
- 54.Mellinger GD, Balter MB, Uhlenhuth EH. Insomnia and its treatment. Prevalence and correlates. Arch Gen Psychiatry. 1985;42:225–232. doi: 10.1001/archpsyc.1985.01790260019002. [DOI] [PubMed] [Google Scholar]
- 55.Ohayon MM. Epidemiology of insomnia: What we know and what we still need to learn. Sleep Med Rev. 2002;6:97–111. doi: 10.1053/smrv.2002.0186. [DOI] [PubMed] [Google Scholar]
- 56.Simon GE, VonKorff M. Prevalence, burden, and treatment of insomnia in primary care. Am J Psychiatry. 1997;154:1417–1423. doi: 10.1176/ajp.154.10.1417. [DOI] [PubMed] [Google Scholar]
- 57.Perlis ML, Smith MT, Cacialli DO, Nowakowski S, Orff H. On the comparability of pharmacotherapy and behavior therapy for chronic insomnia. Commentary and implications. J Psychosom Res. 2003;54:51–59. doi: 10.1016/s0022-3999(02)00547-0. [DOI] [PubMed] [Google Scholar]
- 58.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Englewood Cliffs: Prentice-Hall; 1986. [Google Scholar]
- 59.Marlatt GA, George WH. Relapse prevention and the maintenance of optimal health. In: Shumaker SA, Schron EB, Ockene JK, McBee WL, editors. The Handbook of Health Behavior Change. 2. New York: Springer; 2004. pp. 33–58. [Google Scholar]