Abstract
Background
Operating rooms are expensive to run, and hospitals strive to be efficient. The purpose of this study was to evaluate an initiative to improve starting on time in the operating room in an academic pediatric hospital.
Methods
We used an 8-step approach to transforming an organization. A multidisciplinary team defined on-time starts, identified reasons for delays and instituted changes, including improving the same-day admission process, instituting a huddle of operating room staff each morning and providing feedback about on-time starts to staff.
Results
The most common reasons for delay were surgeon and anesthesiologist unavailability and lack of preparedness of patients. The percentage of operations that began on time, defined as the patient being in the room, increased from about 6% to 60% over a 9-month period.
Conclusion
A targeted, multifaceted and multidisciplinary approach can increase the percentage of operations that begin on time in a pediatric hospital.
Abstract
Contexte
Faire fonctionner les blocs opératoires coûte cher et les hôpitaux s’efforcent d’être efficaces. La présente étude avait pour but d’évaluer une initiative visant à améliorer la ponctualité des interventions dans un hôpital universitaire pédiatrique.
Méthodes
Nous avons utilisé une approche en huit étapes appliquée à la transformation organisationnelle. Une équipe multidisciplinaire a établi les critères de ponctualité des interventions, relevé les raisons des retards et instauré les changements voulus, dont l’amélioration de la logistique entourant les admissions d’un jour et la tenue de réunions du personnel du bloc opératoire chaque matin, en plus de mises au point régulières au sujet de la ponctualité à l’intention du personnel.
Résultats
Les raisons les plus souvent invoquées pour expliquer les retards concernaient la disponibilité des chirurgiens et des anesthésistes et la préparation des patients. Le pourcentage des interventions qui ont commencé à l’heure est passé de 6 % à plus de 60 % en l’espace de neuf mois.
Conclusion
Une approche à plusieurs volets, interdisciplinaire et ciblée peut augmenter le pourcentage des interventions qui débutent à l’heure dans un hôpital pédiatrique.
The operating room is one of the most expensive areas in an acute care hospital.1 The intense clinical activity, number of personnel and multiple types of equipment generate high costs. Efficiency is a key issue for profitability in for-profit institutions, and increased efficiency allows more operations to be performed for the same cost in not-for-profit institutions.1 Improving efficiency can focus on reducing costs and/or increasing the amount of work. Costs may be reduced by attention to areas such as salaries, staffing ratios and equipment costs. Improving the amount of work must consider both utilization and productivity.2 Utilization is an evaluation of the clinical activity in a staffed operating room. Productivity is an evaluation of the quality and quantity of work that occurs within a block of surgical time.
A major efficiency effort in most operating rooms is focused on maximizing utilization. Utilization rates are dependant on many factors, including an appropriately booked schedule that starts on time, ends on time, has correct case times and quick turnovers. Despite the intense interest and strong opinions about how to improve the efficiency of operating rooms, most operating rooms resist change or improvement.3 The purpose of this study was to evaluate an initiative to improve the number of on-time starts in an operating room of a pediatric academic health sciences centre.
Methods
The Hospital for Sick Children (SickKids) is the only academic pediatric hospital in metropolitan Toronto, Ontario. SickKids, a level 1 trauma centre with 14 operating rooms that provide surgical care in 10 disciplines, sees about 11 000 surgical procedures per year.
In 2005, the chief of surgery established improving efficiency, safety and quality as objectives for change. These objectives were confirmed during a 1-day staff retreat for the perioperative services including anesthesia, nursing and surgery. Several principles were used to guide the process of change. First, we focused on positive encouragement rather than enforcement and punishment. Second, we used a team approach rather than focusing on a particular discipline; this principle was important in choosing the first efficiency initiative of on-time starts, rather than, for example, turnover times, because starting on time involves all 3 disciplines of surgery, anesthesia and nursing.3 Third, we identified safety and quality as overriding concerns.
We based the process of change on Kotter’s 8 steps to transforming organizations:4 establish a sense of urgency, form a powerful guiding coalition, create a vision, communicate the vision, empower others to act on the vision, plan for and create short-term wins, consolidate improvement and produce more change and institute new approaches.
The first step was to create a sense of urgency and communicate the need for change. Separate formal presentations were made to nurses, anesthetists and surgeons, providing the imperative for change and a forum for feedback. The perioperative services chiefs, who meet biweekly, and the operating room executive committee, who meet monthly, served as guiding coalitions. A general commitment for change came out of a multidisciplinary 1-day retreat for all perioperative care unit (POCU) staff involving surgery, anesthesia and nursing. Although not everyone agreed that efficiency was a concern or that starting on time was a key efficiency target, there was general consensus that efficiency should be addressed and that starting on time was a worthwhile target. A sense of urgency was created by a province-wide surgical efficiency initiative as part of the provincial strategy to address surgical wait times.5 The accountability agreements between the hospitals and the Ministry of Health and Long-Term Care, as part of additional priority wait-time funding, required participating centres to report data on efficiency parameters, including on-time starts. Finally, we communicated the vision for operating room on-time starts through bi-weekly meetings of divisional/departmental chiefs, divisional/departmental meetings, emails and a quarterly POCU newsletter.
Next, we convened a multidisciplinary task force to address starting on time. The task force was co-lead by a surgeon and a nurse to emphasize that multiple disciplines had responsibility for starting on time.3 A task force, rather than a committee, was chosen to indicate that the group had a specific task to accomplish within a projected time frame of 12–18 months. The task force was expected to choose a target and a timeline to achieve the target. Furthermore, the task force was given direct authority to implement change.
The task force defined on-time start, gathered accurate data about on-time starts and determined reasons for delays. The task force met monthly and reported its activities to all POCU staff through minutes distributed by email. Finally, the task force developed and implemented several strategies to improve on-time starts.
Results
The task force leaders recruited volunteers from surgery, anesthesia and nursing. The 7-member team met monthly and assigned tasks to subgroups as tasks arose. Information services supported the group by providing the necessary data.
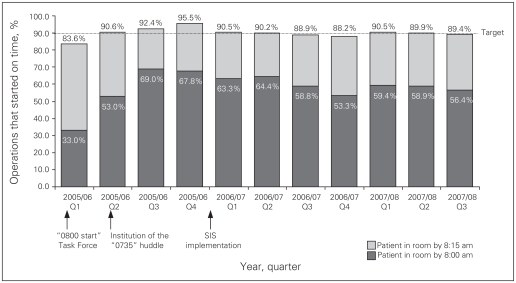
The task force defined starting on time as the patient being in the room by 8:00 am. They also collected data for patients in the room by 8:15 am. The task force used this criteria to determine the frequency of on-time starts and recorded the reasons for delay. Before the beginning of the initiative, the percentage of patients in the room by 8:00 am was about 5%–7% and the percentage in the room by 8:15 am was 70%–75%. Figure 1 shows the efficiency of the operating room by quarter. The reasons for delay were anesthesiologist availability (24%), surgeon availability (21%) and patient readiness owing to missing blood work, investigations or need for preoperative sedation (23%), need for midazolam (13.6%), parent attending induction (11.9%) and consent form not signed (2.5%). Despite the general perception of POCU staff, patient transport was responsible for only 3.7% of delays.
Fig. 1.
Efficiency in the operating room at SickKids from April 2005 to December 2007. The bar graph shows the percentage of operations by quarter that began on time (all services, all patients, excluding patients whose operations were put on hold pending access to a bed in the coronary care unit). SIS = surgical information system.
The task force also examined the barriers to starting on time. Additional staff were assigned to the same day admission unit to ensure that patients were prepared and in the preoperative area by 7:15 am. Electronic patient records were made available to anesthesiologists in each operating room to allow them access to the electronic charts for the patients undergoing surgery the next day. Patients entered the hospital through 5 same day admission units that were geographically and functionally different. These units were consolidated into a single area, which was located in the presurgical anesthesia clinic. However, only 25% of patients are seen in a preanesthetic clinic. This requires anesthesiologists to spend more time addressing parental concerns the morning of surgery. Furthermore, the need to address anxiety with midazolam is often identified in the presurgical holding areas, which can delay the start. Thus, the team considered additional strategies, including increasing the number of patients screened in the preanesthetic clinic and redesigning the preoperative holding area to improve patient flow. During this initiative, a lack of resources precluded addressing these 2 issues.
The task force set a start date of July 1, 2005, and a goal of having 90% of patients in the operating room by 8:00 am. In response to concerns about rushing care, the team agreed that patients would not enter the operating room until it was deemed appropriate by the anesthesiologist.
During the summer of 2005, there was only a modest improvement in the number of on-time starts (Fig. 1). Surgeon and anesthesiologist availability continued to delay the starts. In response to this issue, the “0735” huddle was initiated in September 2005; this huddle involving a meeting at 7:35 am of the staff surgeon, anesthesiologist and nurses to discuss the cases for the day, including any special considerations. The huddle had the dual purpose of enhancing safety through communication and getting everyone to the operating room on time.6 The huddle occurred in the operating room to minimize congestion in the preoperative holding area. As shown in Figure 1, this initiative had the single greatest effect on starting on time.
In November 2005, we began to provide feedback about on-time starts. The percentage of on-time starts for the entire operating room was posted each day on a board across from the main operating room desk. About 1 month later, we began to post the percentage of on-time starts for each service by month in a visible location in the operating room.
Our final strategy was to reward success. The achievement of 3 days in a row of 100% on-time starts was widely publicized, and it was celebrated by a pizza lunch for the entire operating room that was attended by the chief executive officer of the hospital. An additional challenge of achieving a month with at least 90% on-time starts, which was to be rewarded by a POCU staff celebration, was not reached during the study period. The percentage of operations that began on time in 2007 is shown in Table 1.
Table 1.
Percentage of operations that began on time at SickKids in 2007
| Service | Start time, am | Month; % of on-time starts |
12-month average, December 2006–November 2007 |
||||||
|---|---|---|---|---|---|---|---|---|---|
| June | July | Aug. | Sept. | Oct. | Nov. | Rating* | % | ||
| Ophthalmology | 8:00 | 76.9 | 75.0 | 88.2 | 71.4 | 66.7 | 75.0 | Green | 71.7 |
| 8:15 | 92.3 | 93.8 | 100.0 | 100.0 | 76.2 | 95.0 | 94.0 | ||
| Otolaryngology | 8:00 | 70.8 | 62.5 | 67.0 | 54.5 | 67.9 | 74.1 | Yellow | 69.6 |
| 8:15 | 100.0 | 87.5 | 95.7 | 81.8 | 92.9 | 92.6 | 93.0 | ||
| Dentistry | 8:00 | 78.3 | 72.7 | 81.8 | 55.6 | 56.0 | 91.3 | Yellow | 69.0 |
| 8:15 | 87.0 | 86.4 | 100.0 | 83.3 | 88.0 | 100.0 | 92.2 | ||
| Urology | 8:00 | 71.9 | 64.0 | 53.8 | 68.8 | 61.3 | 68.8 | Yellow | 66.1 |
| 8:15 | 100.0 | 100.0 | 92.3 | 84.4 | 93.5 | 96.9 | 94.2 | ||
| Plastic surgery | 8:00 | 41.9 | 56.5 | 47.8 | 53.8 | 43.2 | 65.7 | Red | 53.2 |
| 8:15 | 83.9 | 87.0 | 91.3 | 96.2 | 83.8 | 88.6 | 88.0 | ||
| General surgery | 8:00 | 65.6 | 58.3 | 57.7 | 43.8 | 45.5 | 73.9 | Red | 52.6 |
| 8:15 | 87.5 | 91.7 | 92.3 | 78.1 | 84.8 | 91.3 | 83.5 | ||
| Orthopedic surgery | 8:00 | 67.9 | 37.5 | 58.3 | 64.0 | 60.7 | 57.1 | Red | 50.2 |
| 8:15 | 100.0 | 87.5 | 91.7 | 96.0 | 85.7 | 100.0 | 92.3 | ||
| Neurosurgery | 8:00 | 53.3 | 50.0 | 40.0 | 46.2 | 33.3 | 50.0 | Red | 47.9 |
| 8:15 | 86.7 | 90.0 | 80.0 | 100.0 | 83.3 | 100.0 | 88.6 | ||
| Cardiovascular surgery | 8:00 | 46.7 | 52.6 | 43.8 | 47.4 | 43.5 | 42.9 | Red | 44.9 |
| 8:15 | 93.3 | 78.9 | 87.6 | 81.2 | 91.3 | 86.7 | 86.3 | ||
| All services | 8:00 | 63.9 | 59.0 | 60.9 | 56.9 | 53.6 | 64.5 | Red | 57.9 |
| 8:15 | 91.8 | 89.4 | 92.4 | 88.1 | 86.3 | 93.9 | 89.6 | ||
Green was defined as either > 70% of operations starting at 8 am or > 95% starting at 8:15 am. Yellow was defined as either 60%–70% starting at 8 am or 90%–95% starting at 8:15 am. Red was defined as < 60% starting at 8 am and < 90% starting at 8:15 am. We applied this rating system to the average performance over the previous 12 months. We included all rooms (including image-guided therapy rooms). We excluded patients whose surgeries were on hold pending access to a bed in the cardiac care unit.
Discussion
Starting on time is one of many parameters used to evaluate efficiency of the operating room. Several strategies are available to ensure operations start on time. Other centres have taken a more punitive approach of fining anesthetists and/or withdrawing surgeons’ operating room blocks. Although this strategy would potentially be more effective, it runs the risk of establishing a punitive atmosphere and destroying team functioning.
Our approach was stepwise and collaborative. Although this approach took more time and allowed for some hold-outs to undermine the change initiatives, it was generally perceived as a positive step toward creating a more efficient operating room. The surgeons and anesthesiologists who were persistently late were addressed on an individual level, but no specific punishment was levied. The “0735” huddle was not universally supported by surgeons and anesthesiologists.6 The huddle interfered with morning teaching rounds because staff scheduled to be in the operating room that day were required to leave rounds at 7:30 am. In addition, several physicians resented being told when to arrive in the operating room. However, the huddle had the single largest effect on improving on-time starts. Furthermore, the huddle had a positive effect on nurse’s perceptions of safety in the operating room.6
Although we have yet to achieve our target of 90% of patients in the room by 8 am, starting on time dramatically improved in the SickKids operating rooms, from about 6% to 60%. We are now at the 90% level for on-time starts compared with all other Ontario hospitals that report their on-time starts to the Surgical Efficiency Target Program. This initiative was made possible because of the hard work and collective good will of many individuals. The value of starting on time could be argued against because the extra 15 minutes gained would not allow any additional cases to be performed. However, starting on time means less rush at the beginning and potentially throughout the day; rushing has been identified as one of the factors that leads to an unsafe working environment.7
Our next effort will be to reduce turnover time. If we can reduce turnover by an average of 15 minutes, then we could gain an hour of operating time, resulting in the ability to perform 1 more short surgery each day. Even if an hour of additional operating room time is not gained, ending the day earlier could potentially reduce the amount of overtime paid to staff, which would reduce overall staffing costs for the operating room.
Starting on time is only one aspect of an efficient operating room. We have also been focusing on operating room utilization. We chose to begin with 8:00 am starts because it involves all 3 disciplines. Furthermore, 8:00 am starts provided a single target rather than tackling all aspects of achieving an efficient operating room. For operating rooms that do not start on time, the strategies and process used in this study, based on Kotter’s 8-step approach to changing organizations,4 might be an effective approach. Our next target will involve a new task force to address turnaround time and running beyond the scheduled block of surgical time.
This study has several potential limitations. First, we performed this study in a single hospital. However, we have no reason to believe that a similar strategy would not be effective at other hospitals. Second, the before–after design makes it difficult to determine which aspect of the strategy was effective in improving on-time starts. However, the strong temporal relation between specific strategies, for example the 0735 huddle and on-time starts, suggests a causative relation.
In conclusion, through a staged, multidisciplinary, multifaceted approach, we were able to increase the percentage of operations that began on time from 6% to 60% in the operating room of an academic pediatric hospital.
Footnotes
Competing interests: None declared.
Contributors: All of the authors contributed to the manuscript’s conception and design. Ms. Roche acquired the data, which Dr. Wright analyzed and interpreted. All of the authors were involved in the writing and revision of the manuscript and approved the final version submitted for publication.
References
- 1.Archer T, Macario A. The drive for operating room efficiency will increase quality of patient care. Curr Opin Anaesthesiol. 2006;19:171–6. doi: 10.1097/01.aco.0000192796.02797.82. [DOI] [PubMed] [Google Scholar]
- 2.Hunt PS. Speaking the language of finance. AORN J. 2001;73:774–6. doi: 10.1016/s0001-2092(06)61806-1. [DOI] [PubMed] [Google Scholar]
- 3.Truong A, Tessler MJ, Kleiman SJ, et al. Late operating room starts: experience with an education trial. Can J Anaesth. 1996;43:1233–6. doi: 10.1007/BF03013431. [DOI] [PubMed] [Google Scholar]
- 4.Kotter JP. Leading change: why transformation efforts fail. Harv Bus Rev. 1995;73:59–67. [Google Scholar]
- 5.Ontario Ministry of Health and Long-Term Care. Ontario wait times. Available: www.health.gov.on.ca/transformation/wait_times/wait_mn.html.
- 6.Khoshbin A, Lingard L, Wright JG. Evaluation of preoperative and perioperative briefings at the hospital for Sick Children’s operating rooms. Can J Surg. 2009;52:309–15. [PMC free article] [PubMed] [Google Scholar]
- 7.Greenberg CC, Roth EM, Sheridan TB, et al. Making the operating room of the future safer. Am Surg. 2006;72:1102–8. [PubMed] [Google Scholar]