Summary
With no further intervention, relapse rates in detoxified alcoholics are high and usually exceed 80% of all detoxified patients. It has been suggested that stress and exposure to priming doses of alcohol and to alcohol-associated stimuli (cues) contribute to the relapse risk after detoxification. This article focuses on neuronal correlates of cue responses in detoxified alcoholics. Current brain imaging studies indicate that dysfunction of dopaminergic, glutamatergic, and opioidergic neurotransmission in the brain reward system (ventral striatum including the nucleus accumbens) can be associated with alcohol craving and functional brain activation in neuronal systems that process attentional relevant stimuli, reward expectancy and experience. Increased functional brain activation elicited by such alcohol-associated cues predicted an increased relapse risk, while high brain activity elicited by affectively positive stimuli may represent a protective factor and was correlated with a decreased prospective relapse risk. These findings are discussed with respect to psychotherapeutic and pharmacological treatment options.
Keywords: alcohol craving, functional magnetic resonance imaging, relapse, reward system, dopamine, opioids
Introduction
Without further intervention, detoxification alone does little to prevent subsequent relapse in alcoholics: in the placebo control groups of treatment studies, up to 85% of all patients relapse, even if treated as inpatients until complete remission of physical withdrawal symptoms (Boothby and Doering, 2005). It has been suggested that exposure to stress and to priming doses of alcohol can induce a relapse (Adinoff, 2004; Breese et al., 2005; Cooney, 1997). Another relevant mechanism contributing to the relapse risk is the exposure to stimuli (cues) that have regularly been associated with alcohol intake; such stimuli can become conditioned cues that elicit conditioned responses such as alcohol craving and consumption (Adinoff, 2004; Berridge and Robinson, 1998; Di Chiara and Bassareo, 2007; Everitt and Robbins 2005). Here we review the theoretical background and the results of neuroimaging studies that tried to identify 1) the neuronal networks activated by alcohol-associated versus control cues with functional magnetic resonance imaging, and 2) alterations in relevant neurotransmitter systems that are associated with cue-induced brain activation and craving for alcohol.
A learning theory of alcohol craving
Alcohol dependence and other drug addictions are characterized by criteria such as tolerance development, withdrawal symptoms, drug craving and reduced control of drug intake (American Psychiatric Association, 1994; World Health Organization, 1992). It has been suggested that the development of tolerance, i.e. neuroadaptation of the brain to chronically increased alcohol consumption, results in a new homeostatic balance, which is disturbed when drug or alcohol intake is suddenly interrupted during detoxification and thus results in clinically manifest withdrawal symptoms (Koob, 2003). For example, alcohols sedative effects are mediated by stimulation of GABAergic and inhibition of glutamatergic neurotransmission (Tsai et al., 1995; Krystal et al., 2006). During withdrawal, increased glutamatergic excitation and insufficient GABAergic inhibition may result in epileptic seizures and other withdrawal symptoms (Tsai et al., 1995; Krystal et al., 2006). Patients may relapse because they fear such aversive and dangerous withdrawal symptoms. However, why do patients relapse long after acute withdrawal symptoms have ceased?
One explanation refers to conditioned reactions elicited by conditioned cues, i.e. stimuli that have previously been associated with alcohol intake. In opiate addiction, studies in animals and humans demonstrated that heroin-associated environmental cues triggered conditioned reactions that counteract the expected drug effect (Wikler, 1948; Siegel et al., 1982): rodents, which always received the same dose of opiate in the same cage, displayed a rather high tolerance to this opiate effect. Yet when they received the same dose in a different cage, this conditioned counter-adaptive response did not occur and the animals died because of an overdose. On the other hand, if the animals did not receive the expected opiate dose after being exposed to the contextual cue (cage), they showed symptoms of opiate withdrawal. Therefore it was suggested that the cage served as a conditioned stimulus, which caused a counter-adaptive reaction - opposite to the drug effect – that balances the drug effect or leads to withdrawal symptoms in case the expected drug effect does not arrive (Siegel, 1975). Likewise in alcoholism, contextual cues that characterize situations in which alcohol intake and its associated sedative effects are expected may act as conditioned stimuli that trigger counter-adaptive alterations in neurotransmission such as increased glutamatergic and decreased GABAergic neurotransmission. Again, in the absence of alcohol intake, the resulting hyperexcitation may manifest as withdrawal symptoms and trigger relapse (Verheul et al., 1999). In such situations, patients may experience craving for alcohol motivated by the desire to relieve the unpleasant experience of conditioned withdrawal. Indeed, about one third of all alcoholics in a clinical setting described that their relapse was preceded by a sudden manifestation of withdrawal symptoms, which occurred long after acute detoxification and were often triggered by (previously) “typical” drinking situations (Heinz et al., 2003).
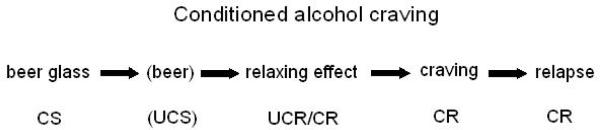
However, craving for alcohol may also be triggered by environmental stimuli that have been associated with the rewarding, subjectively pleasant effects of alcohol intake (Stewart et al., 1984; Verheul et al., 1999; Heinz et al., 2003). According to this theory, originally neutral stimuli can be associated with alcohol's positive effects, so that these stimuli become conditioned stimuli (CS), which are associated with the positive effects of alcohol intake as an unconditioned response (UCR). These conditioned stimuli can elicit craving for the positive effects of alcohol - even without the presence of alcohol – as a conditioned response (CR) (Figure 1). Such formerly neutral stimuli, which are now associated with alcohol's positive effects, can be external cues such as the context, i.e. the environment during former alcohol consumption, or cues associated directly with alcohol intake such as the sight or the smell of the favourite beverage. However, internal stimuli such as feelings of loneliness or memories of conflict situations, which had previously been associated with alcohol intake, can also become conditioned cues that trigger craving for alcohol's positive effects (Drummond, 2000; Heinz et al., 2003; Verheul et al., 1999).
FIGURE 1.
Model of conditioned alcohol craving: a previously neutral stimulus, which has been regularly associated with alcohol consumption (for example the view of a beer glass), can become a conditioned stimulus that is able to elicit alcohol craving.
In the last decade, considerable progress has been made in the attempt to identify the basic neuronal mechanisms that underlie cue-induced alcohol craving. Animal experiments revealed that alcohol and drug associated cues activate dopamine and endorphin release in the medial prefrontal cortex and the ventral striatum including the nucleus accumbens, a core area of the brain reward system (Shalev et al., 2000; Dayas et al., 2007; Di Chiara, 2002). In alcoholism, the sight of the favourite beverage could either elicit conditioned withdrawal symptoms or conditioned craving for alcohol's positive effects and thus facilitate relapse (Heinz et al., 2003). Within the scope of this psychophysiological paradigm, conditioned reactions can be assessed on multiple levels. The levels of reactions differ conceptually and can be influenced by the conditioned cue with different intensity (Carter and Tiffany, 1999). In human studies, a now well-established method to investigate the described theoretical approaches is the combination of a “cue-reactivity” paradigm with functional magnetic resonance imaging (Braus et al., 2001; Drummond, 2000; George et al., 2001; Grüsser et al., 2004).
Empiric relation of craving and relapse
While animal studies strongly support the hypothesis that conditioned drug reactions are involved in the development and maintenance of addictive behaviour and relapse (Robbins and Everitt, 2002; Di Chiara, 2002; Robinson and Berridge, 1993), in alcohol-dependent patients the empiric connection between craving and the following relapse is far less clear. Several studies found no positive correlation between alcohol craving and relapse (Drummond and Glautier, 1994; Grüsser et al., 2004; Junghanns et al., 2005; Kiefer et al., 2005; Litt et al., 2000; Rohsenow et al., 1994), whilst other studies did observe such relationship (Bottlender and Soyka, 2004; Cooney et al., 1997; Heinz et al., 2005c; Ludwig and Wikler, 1974; Monti et al., 1990) (Table 1). In contrast to this, changes in physiological parameters elicited by alcohol-associated cues seem to be more closely connected to relapse (Abrams et al., 1988; Braus et al., 2001; Drummond and Glautier, 1994; Grüsser et al., 2004; Rohsenow et al., 1994).
Table 1.
Correlation between subjective alcohol craving and physiological cue-induced reactions on the one side and relapse on the other side.
| Subjective craving | Physiological reactions |
|---|---|
| Correlation with relapse | |
| Ludwig et al., 1974 | Abrams et al., 1998 |
| Monti et al., 1990 | Rohsenow et al., 1994 |
| Cooney et al., 1997 | Drummond and Glautier, 1994 |
| Bottlender and Soyka, 2004 | Braus et al., 2001 |
| Heinz et al., 2005 | Grüsser et al., 2004 |
| No correlationwith relapse | |
| Drummond and Glautier, 1994 | |
| Rohsenow et al., 1994 | |
| Litt et al., 2000 | |
| Grüsser et al., 2004 | |
| Junghanns et al., 2005 | |
| Kiefer et al.,2005 | |
Within cue-reactivity paradigms, the often low correlation between subjectively reported craving and the actual consumptive behaviour may be explained by divergent reactions to alcohol and alcohol-associated cues, which do not necessarily emerge on all levels (subjective, motor, physiological) at the same time. Tiffany (1990) described a cognitive model in which conscious craving only occurs if the automatic process of drug intake is interrupted, which may be triggered by conditioned stimuli and motivate for drug intake even in the absence of conscious drug urges. Inhomogeneous data concerning the association between craving and relapse could further be explained by the heterogeneous research methods, settings and samples during data collection. For example, it was shown that the psychological level (cue-induced craving) and the physiological level (enhanced drug-like arousal) were dissociated in abstaining alcoholics (Breese et al., 2005). Likewise in a study with cocaine-addicted patients, it was demonstrated that an effective psycho-social treatment with the aim to reduce drug craving helped patients to stay abstinent in spite of the persistence of subjectively high craving (Weiss et al., 2003). It has even been suggested that the conscious sensation of alcohol craving can serve as a warning sign that helps patients to get help and thus maintain abstinence (Drummond and Glautier, 1994; Monti et al., 1990). However, craving seems to lead to relapse if it occurs in stressful situations (Breese et al., 2005; Cooney et al., 1997).
Neurobiological correlates of alcohol craving
In drug and alcohol dependence, different neurotransmitter systems interact with different types of relapse situations (cue-, stress-, or priming-induced) (Shalev et al., 2000; Heinz et al., 2003). Specifically, it was suggested that the rewarding effects of alcohol and all other dugs of abuse are mediated by ethanol-induced dopamine release in the nucleus accumbens (Wise, 1988). In a seminal article, Robinson and Berridge (1993) differed between the subjectively pleasant, hedonic drug effect (“liking”) and the craving for that positive effect (“wanting”) and attributed these effects to different neurotransmitter systems. They suggested that the pleasure (“liking”) during drug intake as well as during consumption of primary reinforcers such as food is caused by opioidergic neurotransmission in the ventral striatum including the nucleus accumbens (Berridge and Robinson, 1998). Berridge and Robinson (1998) also suggested that craving, i.e. the “wanting” or desire for the drug, is not necessarily accompanied by positive feelings. Based e.g. on the work of Schultz and coworkers (1997), they suggested that the neurobiological correlate of “wanting” is (phasic) dopamine release in the ventral striatum.
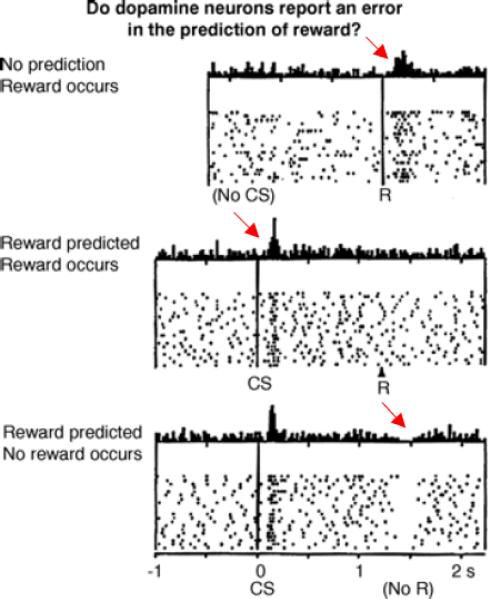
Schultz and others observed that the arrival of unexpected reward elicits a burst of spikes in dopaminergic neurons (Schultz et al., 1997). However, if this incident is predicted by a conditioned cue, the discharge of the dopaminergic neurons occurs directly after the presentation of this conditioned cue and reflects the magnitude of the anticipated reward (Tobler et al., 2005). However, when the reward itself arrives as expected (anticipated), it no longer elicits a dopamine discharge (Schultz et al., 1997) (Figure 2). Robinson and Berridge suggested that phasic dopamine release facilitates the allocation of attention towards salient, reward-indicating stimuli, which can motivate the individual to show a particular behaviour to get the reward.
FIGURE 2.
Reward-associated error signalling by short-term (“phasic”) dopamine release (cf. Schulz et al., 1997). Top: An unexpected reward (banana pallets for rhesus monkeys), which was not predicted by previous stimuli, generates an error in reward prediction (unexpected reward) that is reflected in a short term increase in dopamine firing. Middle: After learning that a previously neutral (now conditioned) stimulus (light) regularly predicts a reward, the surprising appearance of the conditioned stimulus reflects an error in reward prediction and generates a short-term increase in phasic dopamine firing rate. The reward itself is now completely predicted by the conditioned stimulus and does not elicit dopamine firing. Bottom: If a conditioned stimulus is not followed by the expected reward, an error in reward prediction occurs (unexpected lack of reward), which is reflected in a phasic decrease in dopamine firing.
Schultz and coworkers also showed that if the reward does not occur although it was anticipated after the presentation of a reward-indicating, conditioned cue, there is a transient cessation of dopamine neuron firing precisely after the moment when the expected reward does not arrive (Schultz et al., 1997) (Figure 2). Thus the dopaminergic system acts as an error-detection signal, which indicates the unexpected arrival of salient new stimuli and of surprising rewards as well as the non-expected reinforcers. Dopamine release in the nucleus accumbens in response to dopamine neuron firing thus encodes the expected magnitude of a potential reinforcer and therefore contributes to the control of goal directed behaviour. The nucleus accumbens may thus act as a “sensory motor gateway” (Tobler et al., 2005), which controls the effects of salient environmental stimuli on brain areas that regulate motor behaviour.
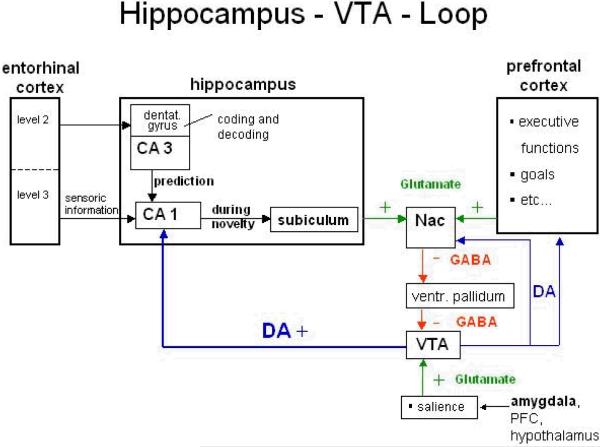
Striatal dopamine release is regulated by the hippocampus, which plays a major role in memory processes (Lisman and Grace, 2005). In rats that had formerly consumed cocaine, the stimulation of glutamatergic neurons in the hippocampus resulted in dopamine release in the ventral striatum and led to renewed drug intake (Vorel et al., 2001). Hippocampal stimulation may reflect real-life situations in which contextual, drug-associated cues activate the hippocampus and thus trigger memories associated with previous drug use (Figure 3). In this situation, hippocampal activation that leads to increases in dopamine neuron activity in the ventral tegmentum can elicit dopamine release in the ventral striatum, which facilitates drug intake (Floresco et al., 2001).
FIGURE 3.
Model of a neuronal network that includes dopamine-related prediction of unexpected or novel reward and reward-associated stimuli: the discrepancy between expected and actual sensory informations is calculated in the hippocampus (CA1) and activates dopaminergic neurons in the brainsteam (VTA) via glutamatergic projections to the nucleus accumbens (ventral striatum). The VTA in turn modulates neuronal transmission in CA1 via an increased dopamine-release in the hippocampus and thus contributes to memory performance. The prefrontal cortex contributes to executive control functions and modulates - just as the limbic system - the firing rate of dopaminergic neurons that project from the brainsteam (VTA) to the nucleus accumbens (modified referring to Lisman and Grace, 2005).
In detoxified alcoholics, brain imaging studies with positron emission tomography (PET) revealed a reduction of availability and sensitivity of central dopamine D2-receptors in alcohol-dependent patients, which may reflect a compensatory down-regulation after chronic alcohol intake and was associated with the subsequent relapse risk (Heinz et al., 1996; Volkow et al., 1996). Further PET studies showed that alcohol craving was specifically correlated with a low dopamine synthesis capacity measured with F-DOPA PET and with reduced dopamine D2 receptor availability in the ventral striatum including the nucleus accumbens (Heinz et al., 2005c; Heinz et al., 2004). During detoxification and early abstinence, dopamine dysfunction may further be augmented by reduced intra-synaptic dopamine release: animal experiments showed that extracellular dopamine concentrations decreased rapidly during detoxification (Rossetti et al., 1992) and a PET study showed that dopamine release following amphetamine administration was significantly reduced in detoxified alcoholics (Martinez et al., 2005). These studies indicate that after detoxification, overall dopaminergic neurotransmission in the ventral striatum of alcohol-dependent patients is reduced. Therefore, it is unlikely that in this situation, the presentation of alcohol-associated cues can cause a significant dopamine release that triggers reward craving or relapse. As a matter of fact, animal studies demonstrated that the presentation of alcohol and drug-associated cues can lead to relapse even if no dopamine is released in the ventral striatum (Shalev et al., 2002). However, as described above, dopamine dysfunction in human studies was correlated with the severity of alcohol craving and also with increased processing of alcohol-associated cues in the anterior cingulate and medial prefrontal cortex (Heinz et al., 2004), brain areas in which an increased processing of alcohol cues has been associated with an increased relapse risk (Grüsser et al., 2004). So how can dopamine dysfunction contribute to alcohol craving and cue reactivity? But before we try to answer this question, we should briefly discuss which other neurotransmitter systems may modulate cue reactivity and craving in alcoholism.
A long-term sensitisation towards the effects of drugs and drug-associated cues can be caused by structural changes in striatal GABAergic neurons, which are innervated by dopaminergic neurons and play a major role in the signal transfer towards the thalamus and the cortex (Robinson and Kolb, 1997). Alcohol stimulates GABA receptors and inhibits the function of glutamatergic NMDA-receptors (Kalivas and Volkow, 2005; Krystal et al., 2006). The alcohol-induced inhibition of the glutamatergic signal transduction results in up-regulation of NMDA receptors (Tsai et al., 1995; Schumann et al., 2005). Loss of alcohol-associated inhibition of NMDA receptor function may result in hyperexcitation and clinically manifest as withdrawal symptoms (Spanagel, 2003). Repeated withdrawals elicit enhanced glutamate release (Kalivas et al., 2005). It has been suggested that glutamatergic neurotransmission in pathways from the prefrontal cortex (PFC), amygdala and hippocampus to the nucleus accumbens and ventral tegmental area (VTA) plays a major role in triggering relapse (Kalivas et al., 2005). Therefore, modulation of NMDA-receptor e.g. by Acamprosate is a promising approach for pharmacological treatment of alcohol craving (Mann et al., 2004; Spanagel, 2003).
Alcohol seems to modulate NMDA receptors via interfering with a glycine binding site on the receptor (Tsai et al., 1995); in that context it is interesting to note that cue-induced relapse was influenced by a glycine binding antagonist but not by competitive nor not-competitive NMDA-receptor antagonists (Bachteler et al., 2005; Backstrom and Hyytia, 2004). Period- (Per-) genes regulate the circadian rhythm and influence glutamatergic neurotransmission. An interesting study found evidence that this gene affects alcohol intake in alcoholics (Spanagel et al., 2005) and in an animal model of excessive alcohol intake: Per2-(Brdm1-) mutant mice revealed an increased glutamate concentration in the suprachiasmatic nucleus and displayed enhanced alcohol intake. Acamprosate normalised glutamate levels and reduced the amount of consumed alcohol (Spanagel et al., 2005). To date, NMDA receptors cannot easily be visualized by PET. However, glutamate concentrations can be measured in vivo with spectroscopy (MRS), and first studies report correlations between glutamate concentrations in the hippocampus and theta oscillations in healthy controls (Gallinat et al., 2006), thus suggesting that MRS may be used to measure glutamate concentrations in association with cue reactivity in alcoholics.
Further neurotransmitter systems which are involved in the development and maintenance of alcohol craving are the cannabinoid and opioidergic system. There is a high concentration of CB1-receptors in the PFC, the amygdala, the VTA, the hippocampus, the nucleus accumbens and the ventral striatum. CB1-receptors modulate the release of DA, GABA and glutamate and elicit long-term changes in synaptic transmission (”long-term potentiation“, LTP and ”long-term depression“, LTD) (De Vries and Schoffelmeer, 2005). The blockade of the CB1-receptors in animal models of excessive nicotine and methamphetamine consumption reduced the drug intake during relapse (De Vries and Schoffelmeer, 2005), and CB1 receptor stimulation in the PFC is required for the behavioural expression of cue-elicited fear conditioning (Laviolette et al., 2005).
Human alcoholics displayed an increase of μ-opiate receptors in the ventral striatum, which was correlated with the severity of alcohol craving (Heinz et al., 2005b). In alcohol-dependent patients, naltrexone blocked alcohol craving and the subjective “high”, i.e. drug “liking”, associated with alcohol intake (O'Brien, 2005). In animal experiments, blockade of μ-opiate receptors with naltrexone reduced dopamine release in the ventral striatum and alcohol intake (Gonzales and Weiss, 1998). In humans, several clinical studies showed that naltrexone treatment can reduce the relapse risk of alcoholics and lower the amount of consumed alcohol (Srisurapanont and Jarusuraisin, 2005; Streeton and Whelan G, 2001, but see Krystal et al., 2001), particularly if applied in patients with a potential high affinity, gain-of-function μ-opiate receptor genotype (Ray and Hutchinson, 2007; Oslin et al., 2003).
Functional imaging studies on cue-induced alcohol craving
Cue-induced functional brain activation can be indirectly assessed by measuring changes in cerebral blood flow with positron emission tomography (PET) or single photon emission computed tomography (SPECT) or by measuring the blood oxygen level dependent (BOLD) response with functional magnetic resonance tomography (fMRI). While these studies revealed considerable inter-individual variance in response to the presentation of alcohol-associated stimuli, there are some core regions which were activated in most studies (de Mendelssohn et al., 2004; Weiss, 2005). These core regions include:
the anterior cingulate (ACC) and the adjacent medial prefrontal cortex, involved in attention-and memory processes, which encode the motivational value of stimuli (Grüsser et al., 2004; Heinz et al., 2004; Myrick et al., 2004; Tapert et al., 2004)
the orbitofrontal cortex (OFC), involved in evaluation of reward of stimuli (Myrick et al., 2004; Wrase et al., 2002)
the basolateral amygdala, which specifies the emotional salience of stimuli and initiates conditioned and unconditioned approach and avoidance behaviour (Schneider et al., 2001)
the ventral striatum (including the nucleus accumbens), which connects motivational aspects of salient stimuli with motor reactions (Wrase et al., 2007; Braus et al., 2001; Wrase et al., 2002)
the dorsal striatum, which consolidates stimulus-reaction-patterns and is involved in habit formation (Grüsser et al., 2004; Modell and Mountz, 1995)
The activation of other brain areas seems to depend upon the sensory quality of presented stimuli (e.g. activation of fusiform gyrus during visual, but not olfactory cues) (Braus et al., 2001) or the state of detoxification and alcohol availability (e.g. activation of the dorsolateral prefrontal cortex, which contributes to executive behaviour control, in acutely drinking patients who were given a priming dose of alcohol, George et al., 2001). However, results concerning the association between cue-induced activity in these brain areas and subjective craving for alcohol are not consistent. One study observed an association between the severity of craving and functional brain activation in the ventral striatum, OFC and ACC (Myrick et al., 2004), another one in the dorsal striatum (Modell and Mountz, 1995), a third in the subcallosal gyrus (Tapert et al., 2004) and some other studies observed no significant correlation between alcohol craving and brain activation (Grüsser et al., 2004; Heinz et al., 2004) (Table 2). A reason for these disparate findings could be the diverse nature of the stimuli used in the different studies: some studies used alcohol related words (Tapert et al., 2004) and others alcohol related pictures, either with (Myrick et al., 2004) or without (Grüsser et al., 2004) a sip of alcohol (“priming dose”). Moreover, in some studies patients were not detoxified and thus able to consume larger amounts of alcohol, at least to a later time point (Myrick et al., 2004), while in other studies the patients were detoxified and participated in an inpatient treatment program, where relapse would cause termination of treatment (Braus et al., 2001; Grüsser et al., 2004; Heinz et al., 2004; Heinz et al., 2007; Wrase et al., 2002; Wrase et al., 2007). The above mentioned difficulties to assess subjective craving may also contribute to these inconsistencies.
Table 2.
Responsive brain activity to alcohol stimuli within adult alcohol-dependent patients vs. healthy controls
| authors | [n] | Activation to alcohol vs. neutral stimuli | regions |
|---|---|---|---|
| Myrick et al., 2004 | 10 patients | pictures | bi insula |
| medial anterior cingulate | |||
| fMRI | 10 controls | bi ventral striatum |
|
| r VTA | |||
|
| |||
| correlation between alcohol pictures and craving | l ventral Striatum |
||
| l orbitofrontal cortex (OFC) | |||
| l anterior cingulate (ACC) | |||
|
| |||
| Tapert et al., 2004 | 8 female patients | words | l subcallosal gyrus |
| l ACC | |||
| fMRI | 9 controls | l DLPFC |
|
| l OFC | |||
| bi insula | |||
| bi uncus | |||
|
| |||
| correlation between alcohol words and craving | l subcallosal gyrus | ||
|
| |||
| Grüsser et al., 2004 | 10 patients | pictures | bi ACC |
| l medial and superior PFC | |||
| FMRI | 10 controls | bi dorsal striatum |
|
| bi secondary visual areas | |||
|
| |||
| correlation between alcohol pictures and craving | no significant activation | ||
|
| |||
| association of alcohol pictures and relapse | medial ACC/medial PFC |
||
| bi dorsal striatum | |||
|
| |||
| Wrase et al., 2002 | 6 patients | pictures | bi ventral striatum |
| bi OFC | |||
| fMRI | bi thalamus |
||
| bi ACC | |||
| bi parietal lobe | |||
| bi DLPFC | |||
| bi fusiform gyrus | |||
| bi occipital lobe | |||
|
| |||
| Braus et al., 2001 | 4 patients | pictures | bi ventral striatum |
| 4 controls | l fusiform gyrus | ||
|
| |||
| after 3 weeks of treatment | l fusiform gyrus | ||
|
| |||
| Schneider et al., 2001 | 10 patients | smell | r amygdala |
| l cerebellum | |||
|
|
|||
| fMRI | 10 controls | after 3 weeks of treatment | r insula |
| r occipital cortex | |||
|
| |||
| George et al., 2001 | 10 patients | pictures | medial thalamus |
| fMRI | 10 controls | l medial frontal gyrus | |
|
| |||
| Modell and Mountz, 1995 | 9 patients | Imagination of pleasant drinking experiences + smell and sip of favourite alcoholic drink | r dorsal striatum |
|
|
|||
| SPECT | no controls | Correlation with craving | r dorsal striatum |
Imaging studies on the prospective relapse risk
While a multitude of studies investigated brain activation during the presentation of alcohol-associated stimuli, only a very few studies assessed to what extent brain activation elicited by alcohol or affective cues predicts an increased relapse risk in the further course of treatment. In a pilot study with alcohol-dependent patients, alcohol cues elicited increased activation of visual association centres and the ventral striatum in detoxified alcoholics compared to control subjects (Braus et al., 2001). Furthermore, patients who suffered from multiple relapses during their previous course of disease and relapsed rather quickly after detoxification showed a stronger cue-induced activation of the ventral striatum than patients who previously managed to abstain from alcohol for longer periods of time and who also managed to abstain during the six-month follow-up period. Grüsser et al. (2004) were able to replicate these findings in another study, again with a rather small sample size: subsequently relapsing patients displayed an increased BOLD response elicited by alcohol-associated stimuli in the anterior cingulate and adjacent medial prefrontal cortex and the central (dorsal) striatum. These observations are in the line with animal experiments in which cue-induced relapse after cocaine consumption was prevented by blockade of dopamine and AMPA glutamate receptors in the dorsal striatum (Vanderschuren et al., 2005). It has been suggested that the dorsal striatum is crucial for habit learning, i.e. for the learning of automated responses, and may thus contribute to the compulsive character of dependent behaviour. On the other hand, in addicted individuals, cue-elicited craving tends to preferentially elicit dopamine release in more dorsal striatal structures, which is thought to reflect a transition from a ventral striatal reward-driven phenomenon to a dorsal striatal stimulus-response habit formation (Berke and Hyman, 2000), in which reward plays a lesser role. Indeed, Robbins and Everitt have proposed that although the initial reinforcing effects of drugs of abuse may activate the ventral striatum, when the drug taking transitions into habitual drug-seeking behaviors, activation of the more dorsal striatal regions predominate (Robbins and Everitt, 2002). Thus, although cue-elicited craving will activate ventral striatal structures in terms of glucose metabolism, in addicted individuals the cues tend to preferentially release dopamine in the dorsal striatum and putamen (Volkow et al., 2006; Wong et al., 2006).
Also, in our clinical experience, many patients describe their relapse in terms of such automated actions and do not remember to have experienced craving before the relapse occurred (Tiffany, 1990). In a recent study, alcohol cues were not presented in a block design for 20 seconds as in the studies of Braus et al. and Grüsser et al. (Braus et al., 2001; Grüsser et al., 2004) but instead were presented only for 750 ms in a single event design (Heinz et al., 2007). The briefly presented alcohol pictures elicited increased brain activation in alcoholics versus controls in the prefrontal and cingulate cortex, however, no significant correlation with the subsequent relapse risk was observed. Sample size limitations or differences in brain activation depending on the duration of stimulus presentation may contribute to these differences. However, increased brain activation elicited by positive versus neutral stimuli in the ventral striatum was correlated with a subsequently reduced relapse risk. If independently replicated, increased responses to affectively pleasant stimuli may represent a protective factor that could potentially be targeted by psychotherapy.
Besides increased responses to alcohol-associated cues in brain areas associated with motivation and affect, dysfunction of brain areas associated with executive behaviour control may also contribute to the relapse risk. Indeed, one study in methamphetamine-dependent patients showed that subsequent relapse was predicted by activation patterns elicited during a two-choice decision-making task in the insula, posterior cingulate and temporal cortex (Paulus et al., 2005). However, so far this hypothesis has not been tested in alcohol-dependent patients.
Neurotransmitter dysfunction and cue reactivity
So far, only a few studies directly examined the correlation between cue-induced brain activation and dopamine dysfunction in alcoholics. To date, no study assessed the correlation between cue-induced brain activation and other neurotransmitter systems such as glutamate or GABA in alcoholics. In recently detoxified alcohol-dependent patients, the prospective risk of relapse was associated with the extent of alcohol craving, which in turn was correlated with both a low dopamine synthesis capacity measured with F-DOPA PET and with a reduced availability of dopamine D2-receptors in the ventral striatum (Heinz et al., 2005c; Heinz et al., 2004). The reduction of dopamine D2-receptors in the ventral striatum was correlated with increased fMRI activation of the anterior cingulate and adjacent medial prefrontal cortex during the presentation of alcohol-associated versus neutral control cues (Heinz et al., 2004). These brain areas have been associated with attribution of attention to salient stimuli (Fuster et al., 1997). But why would alcohol-associated stimuli elicit brain activation in the attention network, if they are presented in a setting that does not offer any chance to obtain alcohol, i.e. in a loud and noisy scanner to patients who are in a detoxification program that excludes any alcohol use?
The work of Schultz et al. (1997) showed that phasic alterations in dopamine release are not only required to learn new stimulus-reward associations but also that they may be necessary to unlearn established associations: a phasic dip of dopamine release occurred whenever a conditioned stimulus is not followed by the anticipated reward (Figure 2). It has been suggested that dopamine dysfunction during early abstinence, i.e. low dopamine synthesis, reduced stimulus-induced dopamine release and D2 receptor availability in the ventral striatum of detoxified alcoholics (Heinz et al., 2005c; Heinz et al., 2004; Martinez et al., 2005) may interfere with this dopamine-dependent signalling of an error in reward expectation (Heinz et al., 2004). Therefore, it may be difficult for alcoholics to divert attention away from conditioned cues, which have well been learned to signal the availability of alcohol (maybe via glutamate-dependent long-term potentiation of the ventral hippocampus-ventral striatal pathway that has been associated with perseverative behaviour; Goto and Grace, 2005), if dopamine dysfunction interferes with the phasic dopamine-dependent error signal indicating that alcohol-associated cues are no longer followed by reward. Indeed, a linear correlation was found between alcohol cue-induced activation of the medial prefrontal cortex and the reduction of dopamine D2 receptor availability in the ventral striatum of detoxified alcoholics, suggesting that the degree of dopamine dysfunction contributes to excessive salience attribution to alcohol-associated cues (Heinz et al., 2004). Maybe that is why in our clinical experience, many detoxified alcohol-dependent patients report difficulty to remaining abstinent when confronted with alcohol advertisements in typical drinking situations (e.g. when sitting alone at home and watching a football game); unfortunately, there are no studies about the impact of alcohol ads on the relapse risk of alcoholics.
If dopamine dysfunction in detoxified alcoholics interferes with phasic changes in dopaminergic neurotransmission, alcohol-dependent patients should also have problems in attributing salience to newly learned conditioned stimuli, which are presented unexpectedly and indicate the availability of reward. Indeed, a reduced functional activation of the ventral striatum was found in alcoholics who were confronted with cues that indicated the availability of reward (Wrase et al., 2007). This reduced activation of the ventral striatum correlated with the severity of alcohol craving and was not explained by differences in performance or mood between alcoholics and control subjects. Reduced brain activation to new reward-indicating stimuli may thus interfere with the patients' motivation to experience new and potentially rewarding situations. Moreover, the same patients displayed an increased activation of the ventral striatum when confronted with alcohol-associated stimuli, which was also correlated with the severity of alcohol craving. This finding is in accordance with the hypothesis that alcohol and other drugs of abuse “hijack” a dysfunctional reward system, which tends to respond too strongly to drug-associated cues while failing to adequately process conventional, primary reinforcers such as food or sex (Volkow et al., 2004). More specifically, within the framework of the studies of Schultz et al. (1997), these findings may help to explain why it can be difficult to motivate detoxified alcoholics to replace alcohol by other reinforcers such as social interactions or new hobbies: their neuronal responses to new reward-indicating stimuli are reduced, while those to alcohol-associated cues are increased, which may make it very difficult to divert attention from alcohol-associated cues signalling the availability of alcohol and its dopamine-stimulating pharmacological effects (Di Chiara, 2002; Di Chiara et al., 2007).
Therapeutical consequences
The presented data suggest different therapeutic consequences. First of all, functional imaging studies can help to identify patients who are particularly at risk to suffer a relapse as a result of increased reactions to alcohol-associated cues. Since imaging techniques such as fMRI are currently too expensive, the employment of less complicated techniques that assess physiological responses to alcohol cues such as the affect-modulated startle response (Heinz et al., 2003) are of particular clinical relevance. Many alcohol-dependent patients deny alcohol craving during the presentation of alcohol-associated pictures, but they show strong appetitive reactions to alcohol cues when assessed with the startle response (Heinz et al., 2003). Secondly, specific psychotherapeutic methods may be developed for alcohol-dependent patients with strong cue reactivity and a high risk for relapse. For example, treatments using cue exposure have repeatedly been investigated in therapeutic studies, however, so far they do not seem to yield significantly better results than standard therapy with cognitive-behavioural and supporting interventions (Kavanagh et al., 2004; Löber et al., 2006). However, this treatment may be specifically successful in patients who show strong cue reactivity. Therefore, identification of patients with strong neuronal responses to alcohol cues may provide an opportunity to successfully treat this subgroup of patients with cue exposure therapy. Thirdly, the results of this review suggest that an effective strategy may involve testing of the effects of additive pharmacotherapy on cue-induced neuronal activation patterns. One pilot study showed that alcohol cue-induced activation of the thalamus is blocked by acute application of amisulpride in detoxified alcoholics (Hermann et al., 2006), however, chronic effects on alcohol intake and the relapse risk remain to be explored.
Summary and outlook
Current research about the different neurobiological mechanisms of relapse raises hope for a therapy of alcohol dependence that is adapted to individual relapse mechanisms and needs. Furthermore, neuroscientific research can contribute to the reduction of the stigmata of addiction. In contrast to common assumptions that prevailed until the second half of the 20th century, relapse in alcohol-dependent patients does not seem to reflect “bad intentions” or “weak willpower”. Rather, in vivo imaging studies point to an increased sensitivity of brain areas to alcohol-associated stimuli, which may be in part genetically influenced (Heinz et al., 2005a). Cue-induced brain activation predicted the relapse risk of alcohol-dependent patients better than conscious craving, which is not surprising given that activation of some brain areas such as the striatum is hardly associated with conscious experiences. Therefore, it seems plausible that patients often relapse “against their own [conscious] will” and they should be treated with the same respect as any other patient in the health care system.
References
- Abrams DB, Monti PM, Carey KB, Pinto RP, Jacobus SI. Reactivity to smoking cues and relapse - two studies of discriminant validity. Behav Res Ther. 1988;26:225–233. doi: 10.1016/0005-7967(88)90003-4. [DOI] [PubMed] [Google Scholar]
- Adinoff B. Neurobiologic processes in drug reward and addiction. Harv Rev Psychiatry. 2004;12:305–320. doi: 10.1080/10673220490910844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- American Psychiatric Association . Diagnostic and Statistical Manual of Mental Disorders. 4th ed. American Psychiatric Press; Washington DC: 1994. [Google Scholar]
- Bachteler D, Economidou D, Danysz W, Ciccocioppo R, Spanagel R. The effects of acamprosate and neramexane on cue-induced reinstatement of ethanol-seeking behaviour in rat. Neuropsychopharmacology. 2005;30:1104–1110. doi: 10.1038/sj.npp.1300657. [DOI] [PubMed] [Google Scholar]
- Backstrom P, Hyytia P. Ionotropic glutamate receptor antagonists modulate cue-induced reinstatement of ethanol-seeking behavior. Alcohol Clin Exp Res. 2004;28:558–565. doi: 10.1097/01.alc.0000122101.13164.21. [DOI] [PubMed] [Google Scholar]
- Berke JD, Hyman SE. Addiction, dopamine, and the molecular mechanisms of memory. Neuron. 2000;25:515–532. doi: 10.1016/s0896-6273(00)81056-9. [DOI] [PubMed] [Google Scholar]
- Berridge KC, Robinson TE. What is the role of dopamine in reward: hedonic impact, reward learning, or incentive salience? Brain Res Brain Res Rev. 1998;28:309–369. doi: 10.1016/s0165-0173(98)00019-8. [DOI] [PubMed] [Google Scholar]
- Boothby LA, Doering PL. A camprosate for the treatment of alcohol dependence. Clin Ther. 2005;27:695–714. doi: 10.1016/j.clinthera.2005.06.015. [DOI] [PubMed] [Google Scholar]
- Bottlender M, Soyka M. Impact of craving on alcohol relapse during, and 12 months following, outpatient treatment. Alcohol Alcohol. 2004;39:357–361. doi: 10.1093/alcalc/agh073. [DOI] [PubMed] [Google Scholar]
- Braus DF, Wrase J, Grüsser S, Hermann D, Ruf M, Flor H, Mann K, Heinz A. Alcohol-associated stimuli activate the ventral striatum in abstinent alcoholics. J Neural Transm. 2001;108:887–894. doi: 10.1007/s007020170038. [DOI] [PubMed] [Google Scholar]
- Breese GR, Chu K, Dayas CV, Funk D, Knapp DJ, Koob GF, Lê DA, O'Dell LE, Overstreet DH, Roberts AJ, Sinha R, Valdez GR, Weiss F. Stress enhancement of craving during sobriety: a risk for relapse. Alcohol Clin Exp Res. 2005;29:185–195. doi: 10.1097/01.alc.0000153544.83656.3c. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter B, Tiffany S. Meta-analysis of cue-reactivity in addiction research. Addiction. 1999;94:327–340. [PubMed] [Google Scholar]
- Cooney NL, Litt MD, Morse PA, Bauer LO, Gaupp L. Alcohol cue reactivity, negative-mood reactivity, and relapse in treated alcoholic men. J Abnorm Psychol. 1997;106:243–250. doi: 10.1037//0021-843x.106.2.243. [DOI] [PubMed] [Google Scholar]
- Dayas CV, Liu X, Simms JA, Weiss F. Distinct patterns of neural activation associated with ethanol seeking: effects of naltrexone. Biol Psychiatry. 2007;61(8):979–989. doi: 10.1016/j.biopsych.2006.07.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Mendelssohn A, Kasper S, Tauscher J. Neuroimaging in substance abuse disorders. Nervenarzt. 2004;75:651–662. doi: 10.1007/s00115-003-1565-7. [DOI] [PubMed] [Google Scholar]
- De Vries TJ, Schoffelmeer ANM. Cannabinoid CB1 receptors control conditioned drug seeking. Trends Pharmacol Sci. 2005;26:420–426. doi: 10.1016/j.tips.2005.06.002. [DOI] [PubMed] [Google Scholar]
- Di Chiara G. Nucleus accumbens shell and core dopamine: differential role in behavior and addiction. Behav Brain Res. 2002;137(1–2):75–114. doi: 10.1016/s0166-4328(02)00286-3. [DOI] [PubMed] [Google Scholar]
- Di Chiara G, Bassareo V. Reward system and addiction: what dopamine does and doesn't do. Curr Opin Pharmacol. 2007;7(1):69–76. doi: 10.1016/j.coph.2006.11.003. [DOI] [PubMed] [Google Scholar]
- Drummond DC. What does cue-reactivity have to offer clinical research? Addiction. 2000;95:S129–S144. doi: 10.1080/09652140050111708. [DOI] [PubMed] [Google Scholar]
- Drummond DC, Glautier S. A controlled trial of cue exposure treatment in alcohol dependence. J Consult Clin Psychol. 1994;62:809–817. doi: 10.1037//0022-006x.62.4.809. [DOI] [PubMed] [Google Scholar]
- Everitt BJ, Robbins TW. Neural systems of reinforcement for drug addiction: from actions to habits to compulsion. Nat Neurosci. 2005;8:1481–1489. doi: 10.1038/nn1579. [DOI] [PubMed] [Google Scholar]
- Floresco SB, Todd CL, Grace AA. Glutamatergic afferents from the hippocampus to the nucleus accumbens regulate activity of ventral tegmental area dopamine neurons. J Neurosci. 2001;21:4915–4922. doi: 10.1523/JNEUROSCI.21-13-04915.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuster JM. The Prefrontal Cortex: Anatomy, Physiology, and Neuropsychology of the Frontal Lobe. Lippincott-Raven; Philadelphia: 1997. [Google Scholar]
- Gallinat J, Kunz D, Senkowski D, Kienast T, Seifert F, Schubert F, Heinz A. Hippocampal glutamate concentration predicts cerebral theta oscillations during cognitive processing. Psychopharmacology. 2006;187(1):103–111. doi: 10.1007/s00213-006-0397-0. [DOI] [PubMed] [Google Scholar]
- George MS, Anton RF, Bloomer C, Teneback C, Drobes DJ, Lorberbaum JP, Nahas Z, Vincent DJ. Activation of prefrontal cortex and anterior thalamus in alcoholic subjects on exposure to alcohol-specific cues. Arch Gen Psychiatry. 2001;58:345–352. doi: 10.1001/archpsyc.58.4.345. [DOI] [PubMed] [Google Scholar]
- Gonzales RA, Weiss F. Suppression of ethanol-reinforced behavior by naltrexone is associated with attenuation of the ethanol-induced increase in dialysate dopamine levels in the nucleus accumbens. J Neurosci. 1998;18:10663–10671. doi: 10.1523/JNEUROSCI.18-24-10663.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goto Y, Grace AA. Dopamine-dependent interactions between limbic and prefrontal cortical synaptic plasticity in the nucleus accumbens: Disruption by cocaine sensitization. Neuron. 2005;47:255–266. doi: 10.1016/j.neuron.2005.06.017. [DOI] [PubMed] [Google Scholar]
- Grüsser SM, Wrase J, Klein S, Hermann D, Smolka MN, Ruf M, Weber-Fahr W, Flor H, Mann K, Braus DF, Heinz A. Cue-induced activation of the striatum and medial prefrontal cortex is associated with subsequent relapse in abstinent alcoholics. Psychopharmacology (Berl) 2004;175:296–302. doi: 10.1007/s00213-004-1828-4. [DOI] [PubMed] [Google Scholar]
- Heinz A, Braus DF, Smolka MN, Wrase J, Puls I, Hermann D, Klein S, Grüsser SM, Flor H, Schumann G, Mann K, Buchel C. Amygdala-prefrontal coupling depends on a genetic variation of the serotonin transporter. Nat Neurosci. 2005a;8:20–21. doi: 10.1038/nn1366. [DOI] [PubMed] [Google Scholar]
- Heinz A, Dufeu P, Kuhn S, Dettling M, Gräf K, Kürten I, Rommelspacher H, Schmidt LG. Psychopathological and behavioral correlates of dopaminergic sensitivity in alcohol dependent patients. Arch Gen Psychiatry. 1996;53:1123–1128. doi: 10.1001/archpsyc.1996.01830120061011. [DOI] [PubMed] [Google Scholar]
- Heinz A, Löber S, Georgi A, Wrase J, Hermann D, Rey ER, Wellek S, Mann K. Reward craving and withdrawal relief craving: assessment of different motivational pathways to alcohol intake. Alcohol Alcohol. 2003;38:35–39. doi: 10.1093/alcalc/agg005. [DOI] [PubMed] [Google Scholar]
- Heinz A, Reimold M, Wrase J, Hermann D, Croissant B, Mundle G, Dohmen BM, Braus DF, Schumann G, Machulla HJ, Bares R, Mann K. Correlation of stable elevations in striatal mu-opioid receptor availability in detoxified alcoholic patients with alcohol craving–A positron emission tomography study using carbon 11-labeled carfentanil. Arch Gen Psychiatry. 2005b;62:57–64. doi: 10.1001/archpsyc.62.1.57. [DOI] [PubMed] [Google Scholar]
- Heinz A, Siessmeier T, Wrase J, Buchholz HG, Gründer G, Kumakura Y, Cumming P, Schreckenberger M, Smolka MN, Rösch F, Mann K, Bartenstein P. Correlation of alcohol craving with striatal dopamine synthesis capacity and D-2/3 receptor availability: a combined [18F]DOPA and [18F]DMFP PET Study in detoxified alcoholic patients. Am J Psychiatry. 2005c;162:1515–1520. doi: 10.1176/appi.ajp.162.8.1515. [DOI] [PubMed] [Google Scholar]
- Heinz A, Siessmeier T, Wrase J, Hermann D, Klein S, Grüsser SM, Flor H, Braus DF, Buchholz HG, Gründer G, Schreckenberger M, Smolka MN, Rösch F, Mann K, Bartenstein P. Correlation between dopamine D-2 receptors in the ventral striatum and central processing of alcohol cues and craving. Am J Psychiatry. 2004;161:1783–1789. doi: 10.1176/appi.ajp.161.10.1783. [DOI] [PubMed] [Google Scholar]
- Heinz A, Wrase J, Kahnt T, Beck A, Bromand Z, Grusser SM, Kienast T, Smolka MN, Flor H, Mann K. Brain activation elicited by affectively positive stimuli is associated with a lower risk of relapse in detoxified alcoholic subjects. Alcohol Clin Exp Res. 2007;31(7):1138–1147. doi: 10.1111/j.1530-0277.2007.00406.x. [DOI] [PubMed] [Google Scholar]
- Hermann D, Smolka MN, Wrase J, Klein S, Nikitopoulos J, Georgi A, Braus DF, Flor H, Mann K, Heinz A. Blockade of cue-induced brain activation of abstinent alcoholics by a single administration of amisulpride as measured with fMRI. Alcohol Clin Exp Res. 2006;30(8):1349–1354. doi: 10.1111/j.1530-0277.2006.00174.x. [DOI] [PubMed] [Google Scholar]
- Junghanns K, Tietz U, Dibbelt L, Kuether M, Jurth R, Ehrenthal D, Blank S, Backhaus J. Attenuated salivary cortisol secretion under cue exposure is associated with early relapse. Alcohol Alcohol. 2005;40:80–85. doi: 10.1093/alcalc/agh107. [DOI] [PubMed] [Google Scholar]
- Kalivas PW, Volkow ND. The neural basis of addiction: a pathology of motivation and choice. Am J Psychiatry. 2005;162:1403–1413. doi: 10.1176/appi.ajp.162.8.1403. [DOI] [PubMed] [Google Scholar]
- Kalivas PW, Volkow N, Seamans J. Unmanageable motivation in addiction: a pathology in prefrontal-accumbens glutamate transmission. Neuron. 2005;45:647–650. doi: 10.1016/j.neuron.2005.02.005. [DOI] [PubMed] [Google Scholar]
- Kavanagh DJ, Andrade J, May J. Beating the urge: implications of research into substance-related desires. Addict Behav. 2004;29:1359–1372. doi: 10.1016/j.addbeh.2004.06.009. [DOI] [PubMed] [Google Scholar]
- Kiefer F, Helwig H, Tarnaske T, Otte C, Jahn H, Wiedemann K. Pharmacological relapse prevention of alcoholism: clinical predictors of outcome. Eur Addict Res. 2005;11:83–91. doi: 10.1159/000083037. [DOI] [PubMed] [Google Scholar]
- Koob GF. Alcoholism: allostasis and beyond. Alcohol Clin Exp Res. 2003;27(2):232–243. doi: 10.1097/01.ALC.0000057122.36127.C2. [DOI] [PubMed] [Google Scholar]
- Krystal JH, Cramer JA, Krol WF, Kirk GF, Rosenheck RA, Veterans Affairs Naltrexone Cooperative Study 425 Group Naltrexone in the treatment of alcohol dependence. N Engl J Med. 2001;345(24):1734–9. doi: 10.1056/NEJMoa011127. [DOI] [PubMed] [Google Scholar]
- Krystal JH, Staley J, Mason G, Petrakis IL, Kaufman J, Harris RA, Gelernter J, Lappalainen J. Gamma-aminobutyric acid type A receptors and alcoholism: intoxication, dependence, vulnerability, and treatment. Arch Gen Psychiatry. 2006;63(9):957–968. doi: 10.1001/archpsyc.63.9.957. [DOI] [PubMed] [Google Scholar]
- Laviolette SR, Lipski WJ, Grace AA. A subpopulation of neurons in the medial prefrontal cortex encode emotional learning with burst and frequency codes through a dopamine D4 receptor-dependent basolateral amygdala input. Journal of Neuroscience. 2005;25:6066–6075. doi: 10.1523/JNEUROSCI.1168-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lisman JE, Grace AA. The hippocampal-VTA loop: controlling the entry of information into long-term memory. Neuron. 2005;46:703–713. doi: 10.1016/j.neuron.2005.05.002. [DOI] [PubMed] [Google Scholar]
- Litt MD, Cooney NL, Morse P. Reactivity to alcohol-related stimuli in the laboratory and in the field: predictors of craving in treated alcoholics. Addiction. 2000;95:889–900. doi: 10.1046/j.1360-0443.2000.9568896.x. [DOI] [PubMed] [Google Scholar]
- Löber S, Croissant B, Heinz A, Mann K, Flor H. Cue exposure in the treatment of alcohol dependence: effects on drinking outcome, craving and self-efficacy. Br J Clin Psychol. 2006;45(Pt 4):515–29. doi: 10.1348/014466505X82586. [DOI] [PubMed] [Google Scholar]
- Ludwig AM, Wikler A. Craving and relapse to drink. Q J Stud Alcohol. 1974;35:108–130. [PubMed] [Google Scholar]
- Mann K, Lehert P, Morgan MY. The efficacy of acamprosate in the maintenance of abstinence in alcohol-dependent individuals: results of a meta-analysis. Alcohol Clin Exp Res. 2004;28:51–63. doi: 10.1097/01.ALC.0000108656.81563.05. [DOI] [PubMed] [Google Scholar]
- Martinez D, Gil R, Slifstein M, Hwang DR, Huang Y, Perez A, Kegeles L, Talbot P, Evans S, Krystal J, Laruelle M, Abi-Dargham A. Alcohol dependence is associated with blunted dopamine transmission in the ventral striatum. Biol Psychiatry. 2005;58:779–786. doi: 10.1016/j.biopsych.2005.04.044. [DOI] [PubMed] [Google Scholar]
- Modell JG, Mountz JM. Focal cerebral blood flow change during craving for alcohol measured by SPECT. J Neuropsychiatry Clin Neurosci. 1995;7:15–22. doi: 10.1176/jnp.7.1.15. [DOI] [PubMed] [Google Scholar]
- Monti PM, Abrams DB, Binkoff JA, Zwick WR, Liepman MR, Nirenberg TD, Rohsenow DJ. Communication skills training, communication skills training with family and cognitive behavioural mood management-training for alcoholics. J Stud Alcohol. 1990;51:263–270. doi: 10.15288/jsa.1990.51.263. [DOI] [PubMed] [Google Scholar]
- Myrick H, Anton RF, Li XB, Henderson S, Drobes D, Voronin K, George MS. Differential brain activity in alcoholics and social drinkers to alcohol cues: relationship to craving. Neuropsychopharmacology. 2004;29:393–402. doi: 10.1038/sj.npp.1300295. [DOI] [PubMed] [Google Scholar]
- O'Brien CP. Anticraving medications for relapse prevention: a possible new class of psychoactive medications. Am J Psychiatry. 2005;162:1423–1431. doi: 10.1176/appi.ajp.162.8.1423. [DOI] [PubMed] [Google Scholar]
- Oslin DW, Berrettini W, Kranzler HR, Pettinati H, Gelernter J, Volpicelli JR, O'Brien CP. A functional polymorphism of the mu-opioid receptor gene is associated with naltrexone response in alcohol-dependent patients. Neuropsychopharmacology. 2003;28(8):1546–52. doi: 10.1038/sj.npp.1300219. [DOI] [PubMed] [Google Scholar]
- Paulus MP, Tapert SF, Schuckit MA. Neural activation patterns of methamphetamine-dependent subjects during decision making predict relapse. Arch Gen Psychiatry. 2005;62(7):761–768. doi: 10.1001/archpsyc.62.7.761. [DOI] [PubMed] [Google Scholar]
- Ray LA, Hutchison KE. Effects of naltrexone on alcohol sensitivity and genetic moderators of medication response: a double-blind placebo-controlled study. Arch Gen Psychiatry. 2007;64(9):1069–77. doi: 10.1001/archpsyc.64.9.1069. [DOI] [PubMed] [Google Scholar]
- Robbins TW, Everitt BJ. Limbic-striatal memory systems and drug addiction. Neurobiol Learn Mem. 2002;78:625–636. doi: 10.1006/nlme.2002.4103. [DOI] [PubMed] [Google Scholar]
- Robinson TE, Berridge KC. The neural basis of drug craving–an incentive-sensitization theory of addiction. Brain Res Brain Res Rev. 1993;18:247–291. doi: 10.1016/0165-0173(93)90013-p. [DOI] [PubMed] [Google Scholar]
- Robinson TE, Kolb B. Persistent structural modifications in nucleus accumbens and prefrontal cortex neurons produced by previous experience with amphetamine. J Neurosci. 1997;17:8491–8497. doi: 10.1523/JNEUROSCI.17-21-08491.1997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rohsenow DJ, Monti PM, Rubonis AV, Sirota AD, Niaura RS, Colby SM, Wunschel SM, Abrams DB. Cue reactivity as a predictor of drinking among male alcoholics. J Consult Clin Psychol. 1994;62:620–626. doi: 10.1037//0022-006x.62.3.620. [DOI] [PubMed] [Google Scholar]
- Rossetti ZL, Melis F, Carboni S, Gessa GL. Dramatic depletion of mesolimbic extracellular dopamine after withdrawal from morphine, alcohol or cocaine–a common neurochemical substrate for drug-dependence. Ann N Y Acad Sci. 1992;654:513–516. doi: 10.1111/j.1749-6632.1992.tb26016.x. [DOI] [PubMed] [Google Scholar]
- Schneider F, Habel U, Wagner M, Franke P, Salloum JB, Shah NJ, Toni I, Sulzbach C, Hönig K, Maier W, Gaebel W, Zilles K. Subcortical correlates of craving in recently abstinent alcoholic patients. Am J Psychiatry. 2001;158:1075–1083. doi: 10.1176/appi.ajp.158.7.1075. [DOI] [PubMed] [Google Scholar]
- Schultz W, Dayan P, Montague PR. A neural substrate of prediction and reward. Science. 1997;275:1593–1599. doi: 10.1126/science.275.5306.1593. [DOI] [PubMed] [Google Scholar]
- Schumann G, Saam C, Heinz A, Mann K, Treutlein J. The NMDA receptor system: genetic risk factor for alcoholism. Nervenarzt. 2005;76:1355–1362. doi: 10.1007/s00115-005-1917-6. [DOI] [PubMed] [Google Scholar]
- Shalev U, Grimm JW, Shaham Y. Neurobiology of relapse to heroin and cocaine seeking: a review. Pharmacol Rev. 2002;54:1–42. doi: 10.1124/pr.54.1.1. [DOI] [PubMed] [Google Scholar]
- Shalev U, Highfield D, Yap J, Shaham Y. Stress and relapse to drug seeking in rats: studies on the generality of the effect. Psychopharmacology (Berl) 2000;150(3):337–46. doi: 10.1007/s002130000441. [DOI] [PubMed] [Google Scholar]
- Siegel S. Evidence from rats that morphinetolerance is a learned response. J Comp Physiol Psychol. 1975;89:498–506. doi: 10.1037/h0077058. [DOI] [PubMed] [Google Scholar]
- Siegel S, Hinson RE, Krank MD, Mccully J. Heroin Overdose Death - Contribution of Drug-Associated Environmental Cues. Science. 1982;216(4544):436–437. doi: 10.1126/science.7200260. [DOI] [PubMed] [Google Scholar]
- Spanagel R. The role of the glutamatergic system in alcohol addiction. Fortschr Neurol Psychiatr. 2003;71:S33–S35. doi: 10.1055/s-2003-40503. [DOI] [PubMed] [Google Scholar]
- Spanagel R, Pendyala G, Abarca C, Zghoul T, Sanchis-Segura C, Magnone MC, Lascorz J, Depner M, Holzberg D, Soyka M, Schreiber S, Matsuda F, Lathrop M, Schumann G, Albrecht U. The clock gene Per2 influences the glutamatergic system and modulates alcohol consumption. Nat Med. 2005;11:35–42. doi: 10.1038/nm1163. [DOI] [PubMed] [Google Scholar]
- Srisurapanont M, Jarusuraisin N. Naltrexone for the treatment of alcoholism: a meta-analysis of randomized controlled trials. Int J Neuropsychopharmacol. 2005;8:267–280. doi: 10.1017/S1461145704004997. [DOI] [PubMed] [Google Scholar]
- Stewart J, Dewit H, Eikelboom R. Role of unconditioned and conditioned drug effects in the self-administration of opiates and stimulants. Psychol Rev. 1984;91:251–268. [PubMed] [Google Scholar]
- Streeton C, Whelan G. Naltrexone, a relapse prevention maintenance treatment of alcohol dependence: a meta-analysis of randomized controlled trials. Alcohol Alcohol. 2001;36:544–552. doi: 10.1093/alcalc/36.6.544. [DOI] [PubMed] [Google Scholar]
- Tapert SF, Brown GG, Baratta MV, Brown SA. FMRI BOLD response to alcohol stimuli in alcohol dependent young women. Addict Behav. 2004;29:33–50. doi: 10.1016/j.addbeh.2003.07.003. [DOI] [PubMed] [Google Scholar]
- Tiffany ST. A cognitive model of drug urges and drug-use behavior–role of automatic and nonautomatic processes. Psychol Rev. 1990;97:147–168. doi: 10.1037/0033-295x.97.2.147. [DOI] [PubMed] [Google Scholar]
- Tobler PN, Fiorillo CD, Schultz W. Adaptive coding of reward value by dopamine neurons. Science. 2005;307:1642–1645. doi: 10.1126/science.1105370. [DOI] [PubMed] [Google Scholar]
- Tsai G, Gastfriend DR, Coyle JT. The glutamatergic basis of human alcoholism. Am J Psychiatry. 1995;152(3):332–40. doi: 10.1176/ajp.152.3.332. [DOI] [PubMed] [Google Scholar]
- Vanderschuren LJ, Di Ciano P, Everitt BJ. Involvement of the dorsal striatum in cue-controlled cocaine seeking. J Neurosci. 2005;25:8665–8670. doi: 10.1523/JNEUROSCI.0925-05.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Verheul R, van den Brink W, Geerlings P. A three-pathway psychobiological model of craving for alcohol. Alcohol Alcohol. 1999;34(2):197–222. doi: 10.1093/alcalc/34.2.197. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Fowler JS, Wang GJ, Swanson JM. Dopamine in drug abuse and addiction: results from imaging studies and treatment implications. Mol Psychiatry. 2004;9(6):557–69. doi: 10.1038/sj.mp.4001507. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Wang GJ, Fowler JS, Logan J, Hitzemann R, Ding YS, Pappas N, Shea C, Piscani K. Decreases in dopamine receptors but not in dopamine transporters in alcoholics. Alcohol Clin Exp Res. 1996;20:1594–1598. doi: 10.1111/j.1530-0277.1996.tb05936.x. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Wang GJ, Telang F, Fowler JS, Logan J, Childress AR, Jayne M, Ma Y, Wong C. Cocaine cues and dopamine in dorsal striatum: mechanism of craving in cocaine addiction. J Neurosci. 2006;26(24):6583–6588. doi: 10.1523/JNEUROSCI.1544-06.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vorel SR, Liu X, Hayes RJ, Spector JA, Gardner EL. Relapse to cocaine-seeking after hippocampal theta burst stimulation. Science. 2001;292:1175–1178. doi: 10.1126/science.1058043. [DOI] [PubMed] [Google Scholar]
- Weiss F. Neurobiology of craving, conditioned reward and relapse. Curr Opin Pharmacol. 2005;5:9–19. doi: 10.1016/j.coph.2004.11.001. [DOI] [PubMed] [Google Scholar]
- Weiss RD, Griffin ML, Mazurick C, Berkman B, Gastfriend DR, Frank A, Barber JP, Blaine J, Salloum I, Moras K. The relationship between cocaine craving, psychosocial treatment, and subsequent cocaine use. Am J Psychiatry. 2003;160:1320–1325. doi: 10.1176/appi.ajp.160.7.1320. [DOI] [PubMed] [Google Scholar]
- Wikler A. Recent Progress in Research on the Neurophysiologic Basis of Morphine Addiction. Am J Psychiatry. 1948;105(5):329–338. doi: 10.1176/ajp.105.5.329. [DOI] [PubMed] [Google Scholar]
- Wise RA. The neurobiology of craving: implications for the understanding and treatment of addiction. J Abnorm Psychol. 1988;97(2):118–32. doi: 10.1037//0021-843x.97.2.118. [DOI] [PubMed] [Google Scholar]
- Wong DF, Kuwabara H, Schretlin D, Bonson K, Zhou Y, Nandi A, Brasic J, Kimes AS, Maris MA, Kumar A, Contoreggi C, Links J, Ernst M, Rousset O, Zukin S, Grace AA, Rohde C, Jasinski DR, Gjedde A, London ED. Increased occupancy of dopamine receptors in human striatum during cue-elicited cocaine craving. Neuropsychopharmacology. 2006;31:2716–2727. doi: 10.1038/sj.npp.1301194. [DOI] [PubMed] [Google Scholar]
- World Health Organization . International Statistical Classification of Diseases and Related Problems. 10th ed. World Health Organization; Geneva: 1992. [Google Scholar]
- Wrase J, Grüsser SM, Klein S, Diener C, Hermann D, Flor H, Mann K, Braus DF, Heinz A. Development of alcohol-associated cues and cue-induced brain activation in alcoholics. Eur Psychiatry. 2002;17:287–291. doi: 10.1016/s0924-9338(02)00676-4. [DOI] [PubMed] [Google Scholar]
- Wrase J, Schlagenhauf F, Kienast T, Wustenberg T, Bermpohl F, Kahnt T, Beck A, Strohle A, Juckel G, Knutson B, Heinz A. Dysfunction of reward processing correlates with alcohol craving in detoxified alcoholics. Neuroimage. 2007;35(2):787–94. doi: 10.1016/j.neuroimage.2006.11.043. [DOI] [PubMed] [Google Scholar]