Abstract
Objectives
To describe and evaluate pharmacy students' knowledge of and comfort in communicating, managing, and preventing medication errors.
Methods
Using a cross-sectional design, a survey instrument was administered to fifth-year pharmacy students. The survey instrument included both open- and close-ended questions to describe and examine factors associated with knowledge and comfort in communication of medication errors.
Results
Survey instruments were completed by 93 students (90% response rate). Nearly 80% reported not having received training in communicating medication errors. The perception of having more adequate training was related to greater knowledge in the communication of medication errors (p ≤ 0.001). Knowledge was also associated with students having greater comfort in communicating medication errors (p ≤ 0.05).
Conclusions
The need and value of additional training for pharmacy students in communicating medication errors was demonstrated. Educational interventions should be developed to provide consistent instruction on these communication issues.
Keywords: medication errors, training, communication
INTRODUCTION
The Accreditation Council for Pharmacy Education and the American Association of Colleges of Pharmacy both recognize the importance of patient safety as a core component of pharmacy education.1,2 The proceedings of a national stakeholder summit listed a recommendation that medication safety should be included in all professional school curriculums.3 The Food and Drug Administration's (FDA) Strategic Plan also supports pharmacists' understanding of the science of safety to ensure their active participation in the development, implementation, and/or evaluation of new initiatives to improve the consumer's safe use of medical products.4
Limited research has been conducted on what pharmacists and pharmacy students have learned about medication safety,5-9 indicating considerable variation on the nature and depth of medication safety topics taught. Pharmacy programs providing medication safety instruction typically offer topics such as the nomenclature, frequency, cost, and morbidity/mortality associated with medication errors. One innovative program augmented the classroom approach by teaching medication safety and error reduction topics through student projects at institutional and community pharmacy sites.9 In this program, student knowledge and motivation to report and prevent errors was improved. It is not clear, however, what schools and colleges of pharmacy teach students about how they should communicate with patients and pharmacy staff members when medication errors occur, and how to prevent and/or intercept errors. Procedural knowledge of actions to take for the management and prevention of errors is vital for pharmacy students to effectively interact with patients and colleagues. During internships, pharmacists and pharmacy students often communicate about issues that arise, such as misunderstanding a prescriber's written or verbal prescription, giving a correctly filled prescription to the wrong patient, and assuming a prescription was checked when it had not been. Depending on the nature of the problem, medication errors often are received by patients as well as pharmacy personnel with considerable worry, fear, and disappointment. Poor communication between providers and patients can contribute to medication errors and other negative outcomes.10-13 Likewise, good provider-patient communication skills facilitate the development of trust between providers and patients, reduce patient anxiety, improve patient satisfaction, and minimize the frequency of lawsuits.14-17
A clinician's lack of comfort with disclosure of medication errors is sometimes a barrier to good communication skills. Clinicians often are reluctant to report and disclose errors. Patients report that they typically are not given a clear explanation on what to do if an unanticipated medication outcome occurs, and they often feel distanced from health care staff members and organizations because they get few answers when a medication error does occur.18 Patients want errors to be disclosed and usually seek information about why the error happened, how the error's consequences are to be mitigated, and how recurrences are to be prevented.19 Harmful and serious medical errors are infrequently disclosed to patients.20 Multiple factors prevent providers from full disclosure of errors including apprehension that informing the patient of the error could lead to a lawsuit, damage to the clinician's reputation, job loss, and awkward clinical interactions.19,20
When medication errors occur, negative outcomes result from poor communication. Pharmacy educators should explore how comfortable students are in communicating with colleagues and patients to manage and prevent medication errors. One study investigated the training of pharmacy students in communicating the management and prevention of medication errors.21 This qualitative study was comprised of 44 in-depth, semi-structured interviews of pharmacy students who were predominantly in their third, fourth, or fifth professional year of a 6-year pharmacy program. Students were interviewed on topics such as communication-related medication errors, and training on how to handle medication errors. Five main themes emerged from the interviews regarding medication errors and communication: (1) pressure to be perfect, (2) feeling comfortable talking about errors, (3) assuming and communicating responsibility for errors, (4) learning how processes can contribute to errors and their prevention, and (5) inadequate and inconsistent training on how to handle medication errors.
Our study aimed to replicate these latter findings using quantitative survey techniques among a more homogenous group of pharmacy students. We further evaluated the factors associated with pharmacy student knowledge and comfort on how to communicate, manage, and prevent medication errors. In addition, we hypothesized that students who perceived they had sufficient training in handling medication errors were more likely to have greater perceived knowledge about the procedures involved in the medication error process (hypothesis 1); and greater comfort in dealing with issues involving medication errors (hypothesis 2). We also expected to find that greater perceived knowledge about the procedures involved in the medication error process is associated with greater comfort in dealing with issues involving medication errors (hypothesis 3).
METHODS
The survey instrument was administered to pharmacy students in year 5 of a 6-year doctor of pharmacy (PharmD) program during a required pharmacotherapy course in the fall of 2006. A day when students were given a planned quiz was chosen to maximize the number of students present and willing to complete the survey instrument. No incentives were provided. The survey instrument was developed based on items used in a prior study.20 The 8-page survey instrument consisted of both close-ended questions with rankings on a 5-point Likert scale ranging from strongly disagree to strongly agree, and open-ended questions. Five sections were included in the survey: background, general communication attitudes, training in communication about medication errors, communication regarding medication errors, and experiences with medication errors. The general communication attitudes section included items related to other research questions beyond the scope of this study. For this reason, we focused on the results related to the other 4 sections of the survey instrument. (The survey instrument is available upon request from the authors.)
The background section asked about the respondent's age, gender, race, educational background, pharmacy practice site experiences, and receipt of prior instruction on communication of medication errors. These items were viewed as potential factors influencing communication about medication errors. Such demographic items were included because students with certain demographic profiles may be more or less likely to feel comfortable with communication in general and regarding medication errors in particular. For example, age and gender influence counseling skills. Younger pharmacists and females are more likely to counsel patients than older pharmacists and males.22-24 We asked about prior pharmacy practice site experiences to test whether students with little or limited practice experience have different attitudes and experiences dealing with medication errors. Students were also asked about prior instruction on communication about medication errors to test whether this is a factor that influenced students' perceived comfort levels.
The second section of the survey instrument included Likert-scale items and several additional questions about the respondent's training experiences. The 3 Likert items involved respondents' attitudes about the sufficiency of training they received on communication issues contributing to medication errors, how to communicate with patients about a medication error, and how to communicate with other pharmacy staff members about a medication error. The Cronbach alpha for these 3 items was 0.76 and deemed to have acceptable reliability. Additional items in this section explored respondents' opinions regarding the training, descriptions of communication strategies they received from the training, personal feedback/advice they were given about handling mistakes when interacting with a patient, and any additional communication strategies learned from others or personally experienced. The frequencies of recurrent themes related to these latter items were identified.
The section about communication involving medication errors asked respondents 6 Likert-scaled items. The first 3 items asked respondents the extent to which they knew what to tell patients when a medication error occurred, their level of knowledge about reporting a medication error, and how to identify the cause of a medication error. These 3 items were summed to form a composite measure of perceived knowledge of communication procedures involving medication errors. The other 3 items asked the extent to which respondents agreed that 1 or more pharmacies they had worked with (1) informed the pharmacy staff when an error occurred, why it happened, and how to avoid if happening again; (2) routinely discussed the occurrence of medication errors; and (3) routinely developed procedures to prevent errors from recurring. These items are described in the Results section but are not used in the bivariate or multivariate analyses as they did not relate specifically to the study hypotheses.
The last section of the survey instrument asked 4 Likert-scaled items about the respondent's comfort in communicating medication errors. Specifically, the items asked respondents the extent to which they would be comfortable reporting an intercepted or actual error that they or someone else made. The Cronbach alpha for these 4 items was 0.84, reflecting good reliability. To conduct the bivariate and logistic regressions, we dichotomized this variable into high or low comfort based on the median score. This section also included several open-ended items asking about the types of errors made, why the respondent felt they were made, how staff members interacted with the patient when the error was made, whether the mistake was documented, what type of communication occurred between the pharmacy staff and the person who made the error, and the respondent's attitudes about whether the pharmacy focused on reducing medication errors. The frequencies of recurrent themes related to these items were identified.
Descriptive statistics (means, standard deviations, modes, frequencies) were performed on all key study variables. Bivariate (Pearson correlations) and multivariate logistic tests were conducted to test the study's 3 hypotheses. Statistical significance was set at a priori 0.05. For the description of themes of key open-ended items, we reported the frequencies and percentage of respondents reporting the theme. We reported only the frequencies of those themes to which at least 10% of respondents provided a response. The study was approved by the university's institutional review board.
RESULTS
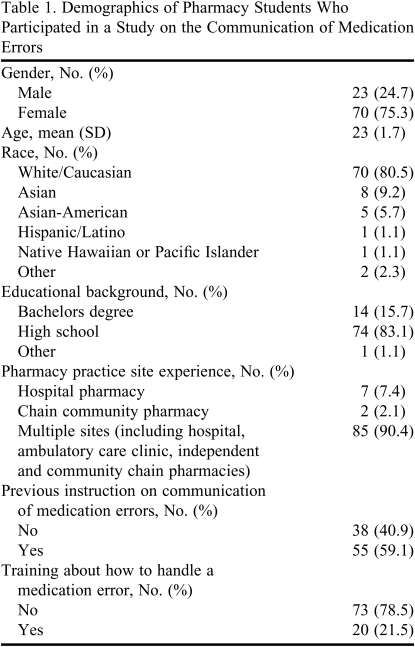
Ninety-three of 103 fifth-year pharmacy students in a required pharmacy course completed the survey instrument, yielding a 90% response rate. The baseline characteristics of respondents are shown in Table 1. Approximately 16% of those sampled had a prior degree, and over 90% had pharmacy experience in multiple pharmacy settings. Almost 60% of the sample reported they received prior instruction in communication of medication errors.
Table 1.
Demographics of Pharmacy Students Who Participated in a Study on the Communication of Medication Errors
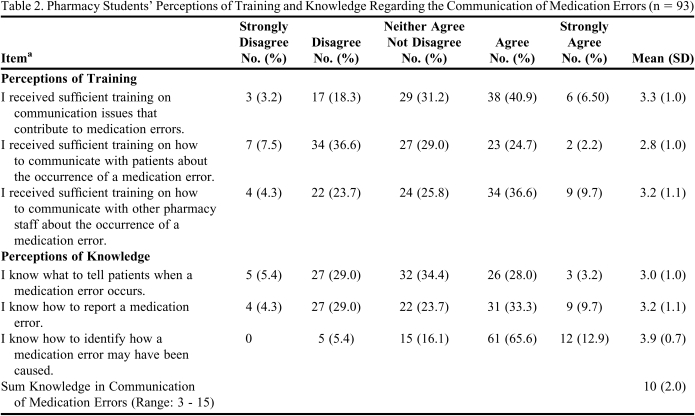
The descriptive results of student perceptions about training and knowledge of communicating medication errors are reported in Table 2. Less than 50% of the sample reported agreement in each of the 3 items regarding the sufficiency of training in the communication of medication errors. Of particular note, only about 25% indicated they agreed they received sufficient training on how to communicate with patients when a medication error occurred. Almost 80% of respondents indicated that they did not receive training on handling an error in a patient's medication order.
Table 2.
Pharmacy Students' Perceptions of Training and Knowledge Regarding the Communication of Medication Errors (n = 93)
a Items rated on a Likert scale on which 1 = strongly disagree; 2 = disagree; 3 = neither disagree nor agree; 4 = agree; 5 = strongly agree
Only a third of the students sampled indicated they knew what to tell patients when a medication error occurs. About 43% indicated they knew how to report a medication error. A larger percentage of students reported they knew how to identify how a medication error may have been caused. When summing the 3 knowledge items, the average total score was 10 ± 2, suggesting a perceived knowledge of 66% for the composite knowledge measure.
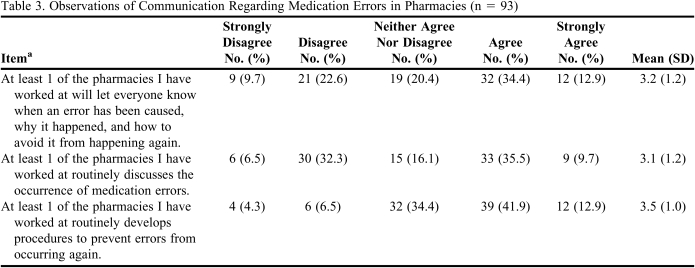
Less than 50% of the respondents agreed that 1 or more of the pharmacies they worked at would alert the pharmacy staff that an error occurred, why it happened, how to avoid it from recurring, and routinely discuss the occurrence of medication errors (Table 3). A little more than 50% reported 1 or more of the pharmacies they worked at routinely developed procedures to prevent errors from recurring.
Table 3.
Observations of Communication Regarding Medication Errors in Pharmacies (n = 93)
a Items rated on a Likert scale on which 1 = strongly disagree; 2 = disagree; 3 = neither disagree nor agree; 4 = agree; 5 = strongly agree
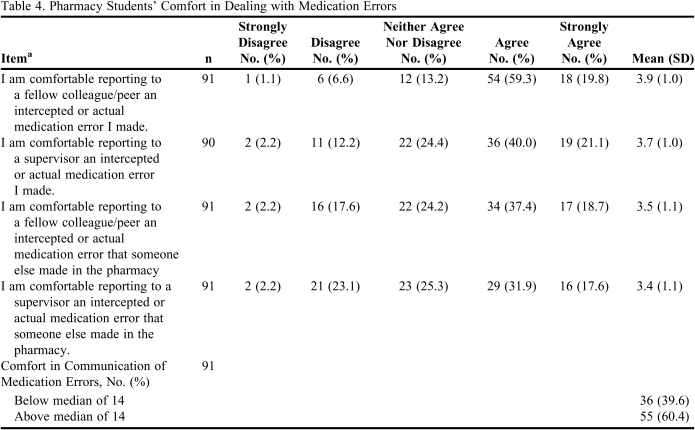
Almost 80% of the respondents indicated they were comfortable in reporting an error they made to a colleague or peer (Table 4). Sixty percent of the respondents reported being comfortable reporting an error they made to a supervisor. Fifty-seven percent indicated comfort reporting an error someone else made to a peer or colleague. Even less (only 48%) said they were comfortable reporting an error someone else made to a supervisor. Using our dichotomous measure for comfort, 60% of the sample was above the median in reporting comfort in communicating a medication error.
Table 4.
Pharmacy Students' Comfort in Dealing with Medication Errors
a Items rated on a Likert scale on which 1 = strongly disagree; 2 = disagree; 3 = neither disagree nor agree; 4 = agree; 5 = strongly agree
Bivariate tests support study hypothesis 1 relating sufficiency of training and knowledge of procedures in medication error process. A significant and positive correlation was found between the perceived sufficiency of training in the communication of medication errors and perceived knowledge of the procedures in the medication error process (r = 0.534, p ≤ 0.001). No significant correlation was found between the perceived sufficiency of training involving the medication error process and greater comfort (dichotomous) in dealing with issues involving medication errors (hypothesis 2). When we did not dichotomize the comfort variable, perceived sufficiency of training was related to greater comfort (p ≤ 0.05). Hypothesis 3 was supported by a significant and positive correlation between greater perceived knowledge of the procedures in the medication error process and greater comfort in dealing with the issues involving medication errors (r = 0.301, p ≤ 0.01).
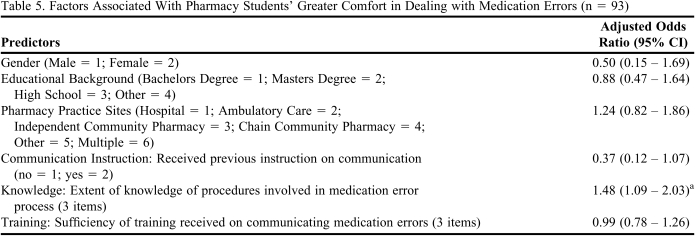
Table 5 provides the results of the multivariate logistic regression predicting degree of comfort in dealing with issues involving medication errors after controlling for gender, educational background, pharmacy practice experiences, and receipt of prior instruction on the communication of medication errors. We found that perceived knowledge of the procedures in the medication error process was the only factor related to greater comfort in dealing with issues involving medication errors (p ≤ 0.05). This finding provides further support for hypothesis 3.
Table 5.
Factors Associated With Pharmacy Students' Greater Comfort in Dealing with Medication Errors (n = 93)
a p ≤ 0.05
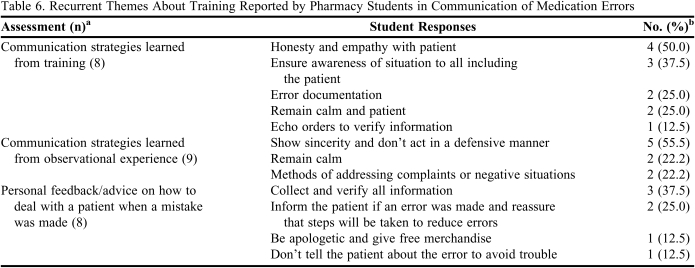
Table 6 indicates key themes about students' perceptions of training they may have had regarding the communication of medication errors. Less than 10% of the survey respondents answered this item. Of those, key communication strategies in dealing with medication errors were to ensure awareness of the situation, to be honest, and to be empathic to involved pharmacy staff members and the patient. Students reported they observed the importance of showing sincerity, not acting defensively, and remaining calm as effective strategies to address complaints or negative situations. Respondents received feedback or advice on the need to collect and verify all information, inform the patient if an error occurred, and to reassure that steps would be taken to reduce errors. Several students stated that they were encouraged to be apologetic and give “free stuff” if an error occurred, and others were instructed not to tell the patient about an error in order to avoid complications.
Table 6.
Recurrent Themes About Training Reported by Pharmacy Students in Communication of Medication Errors
a The n is the total number of respondents who completed this open-ended question
b The number and percent of respondents reporting each theme. There were several cases where the same respondent wrote responses that fit more than one theme
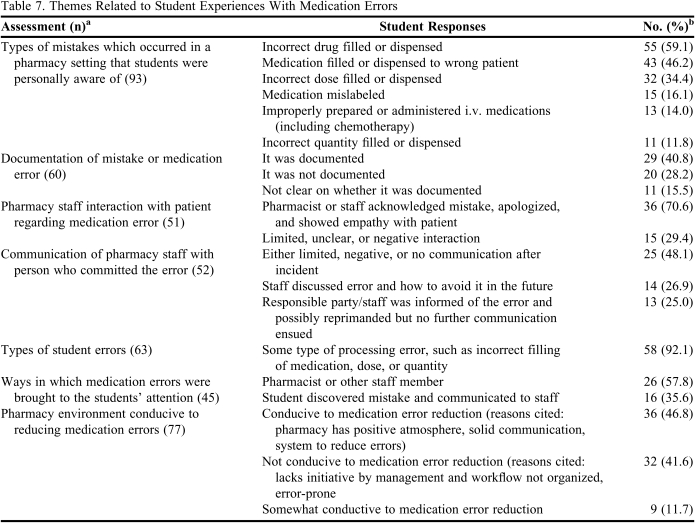
Respondents reported the 3 most common errors in pharmacies were incorrect drug filled or dispensed, medication filled or dispensed to the wrong patient, and incorrect dose filled or dispensed (Table 7). It was nearly an even spilt between those who reported that medication errors were documented and those who reported they were not. Over 70% of the respondents reported they observed the pharmacist or staff acknowledge the error, apologize, and show empathy toward the patient. Almost half of the respondents sampled indicated a negative reaction to the error and/or lack of communication about the medication error after it occurred. About 25% of the respondents indicated the responsible party/staff member was informed of the error but no further communication occurred, and 26.9% indicated the staff member discussed the error and how to avoid it in the future.
Table 7.
Themes Related to Student Experiences With Medication Errors
a The n reported in this column reflects the total number of respondents who completed this open-ended question
b The n reported in this column reflects the number of respondents reporting the theme. There are several cases where the same respondent wrote responses that fit more than 1 theme
Over 90% of the respondents indicated they made a processing error related to the incorrect filling of medication, dose, or quantity. The majority of respondents said they were informed of the errors by pharmacists or other staff members. A few more than a third of the respondents indicated that they discovered the error and mentioned it to a staff member. Slightly more respondents (46.8%) indicated the pharmacy environments they worked at were conducive to reducing medication errors.
DISCUSSION
Five key findings were reported regarding the description of pharmacy student training and its relationship to perceived knowledge and comfort with the communication of medication errors. There was a discrepancy between 60% of the sample indicating they had received prior instruction on the communication of medication errors, and about 80% reporting they had not received any training on how to handle an error made involving a patient. We suspect that students interpreted prior instruction on communication of medication errors as a broader question, capturing numerous aspects of medication errors such as sound-alike and look-alike medications, common transcription errors, and how to report a medication error. To follow up, we consulted a recent curriculum review at the University and found that students in the sample were taught several medication error topics in various courses throughout the curriculum (such as courses on the US health care system, drug information, and pharmacotherapy, respectively). The student responses, however, suggested this prior instruction did not include specific training on handling medication errors involving patients.
These findings support the qualitative results in the only other known study exploring perceptions and experiences of pharmacy students regarding the communication of medication errors.21 Noland and Rickles found a majority of respondents received little or no formal didactic or on-the-job training on how to handle communication of medication errors. Other students reported having learned by observing how others handled medication errors. Those students who reported receiving formal training felt it was insufficient or inadequate. The similarity in findings across both studies provides more confidence in the results because the 2 studies used different methodological approaches.
Study findings identified a clear gap in our curriculum and a possible gap experienced by other schools and colleges of pharmacy. Since this study was completed, specific training has been implemented at our college on how to communicate with patients and others about medication errors in a required pharmacy communication course. Didactic instruction, exposure to a taped counseling scenario involving a standardized patient concerned with the occurrence of a medication error, and class discussions were included. Class discussions have focused on the most effective as well as less ideal strategies in handling different medication error situations.
Few students reported knowing what to say to patients when an error occurs. This result was expected given the high percentage of the sample indicating having received no training on how to communicate with patients about medication errors. A higher percentage of students reported having perceived knowledge about how to identify causes of medication errors and how to report errors. These latter results provided further support that students reporting they had received prior instruction on the communication of medication errors were thinking of the topic broadly relating to the reporting and analyses of errors, and not specifically relating to the interpersonal communication aspects of handling a communication error.
Student comfort levels depended both on who made the error and to whom the error would be reported. Respondents expressed being most comfortable reporting an error to a peer. Respondents indicated moderate comfort when reporting an error made to a supervisor or when reporting an error made by someone else to a peer. Respondents were least comfortable communicating an error that someone else made to a supervisor. Such findings highlighted student discomfort with being the “whistleblower” and how this might affect another person's career. Prior literature also supports clinicians have similar concerns about being a “whistleblower” and the affects of their communicating an error.25
The study confirmed 2 of the 3 study hypotheses. Those students who perceived having sufficient training involving the medication error process had significantly greater perceived knowledge of the procedures in the medication error process. At both the bivariate and multivariate levels, the study also confirmed hypothesis 3, the greater the perceived knowledge of how to communicate medication errors, the more comfortable students were in handling medication errors. The confirmation of these 2 hypotheses is noteworthy because the value of training and how instruction can impact student comfort levels in communicating errors to others is confirmed. While comfort is not necessarily predictive of actual behavior, it is reflective of willingness to communicate errors since it is a reasonable assumption that the more comfortable we are at a task, the more willing we are to perform it.
There was mixed support for the association between sufficiency of training and comfort (hypothesis 2). The association was significant with the continuous but not the dichotomous variable of comfort. The distribution of this sample was not symmetric with a clear peak around a total score of 16. As such, dichotomizing comfort may have further reduced the variability and caused the differences in findings. The lack of clear support may also reflect that the sufficiency of training variable is too relative of a construct to be related to comfort, and that knowledge is a more finite, proximal, and therefore a stronger indicator of comfort. Students indicated they observed pharmacists and other staff members positively interacting with patients when medication errors occurred. However, it was surprising and concerning that there was not ideal communication with staff members regarding responses to or prevention of errors. Less than 50% of the respondents agreed that the pharmacies they worked at had communication systems that would let pharmacy staff know when an error occurred, why it occurred, how to prevent it from happening again, and routinely discuss the occurrence of medication errors. A large number of respondents also indicated there was either limited or no clear documentation of medication errors. These results were also supported by over 40% of respondents indicating that their pharmacies were not conducive environments for medication error reduction. Of concern from an educational perspective is that students learning in practice settings are not receiving effective modeling of best practices, which is crucial to creating a learning culture around the occurrence and prevention of medication errors. If students are not exposed to effective models on how to communicate with others about medication errors, they cannot be expected to perform adequately once they graduate and enter pharmacy practice. Future research should confirm this important finding and explore what organizational factors lead to a greater focus on effective ways to respond to and prevent medication errors.
This study had several limitations. The study evaluated communication of medication errors in 1 school of pharmacy and geographic location. Whether results are generalizable to a larger and more diverse sample is difficult to know. A larger and broader study should be conducted to replicate findings. The study was cross-sectional in nature and representative of one point in time. Third, data were based on student recall and observations which may or may not be accurate estimates of different study variables and outcomes. To this end, it would have been interesting to collect pharmacist data about related perceptions and observations about the communication of medication errors. Fourth, the study involved a number of measures that have not been previously validated and require further psychometric testing. Related to this latter limitation, several items had multiple components (such as the first item in Table 3 and all items in Table 4), that if addressed separately may have yielded different responses. In response to the first item in Table 3, a respondent may have strongly agreed that the pharmacy they worked at would let pharmacy staff know the error occurred, but strongly disagreed that they would discuss how to avoid it from happening again. However, by collapsing these components into 1 item, we would have missed these discrepancies. Additional research should explore if responses are different when components are presented separately. Future research also should explore effective educational interventions to improve student learning of how to communicate medication errors involving patients, physicians, and the entire pharmacy team.
CONCLUSIONS
This study examined how students learn and experience the communication of medication errors. Examining how pharmacy students experience medication errors provided an important opportunity to understand how future pharmacists learn the role that communication plays in the occurrence of, report of, and response to medication errors. Pharmacy students and pharmacists must have formal instruction regarding how communication and poorly designed systems can contribute to medication errors and appropriate responses to medication errors. Students must learn in settings where communication of medication errors effectively occurs among pharmacy staff members, the patient, and other health professionals. The development of appropriate didactic and experiential models for communicating medication errors will lead to better team communication in responding to and preventing medication errors.
ACKNOWLEDGMENTS
The authors would like to thank Jenny Rickles for her assistance in proofreading and for her valuable feedback in the preparation of this manuscript.
REFERENCES
- 1. Accreditation standards and guidelines for the professional program in pharmacy leading to the doctor of pharmacy degree. http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf. Accessed March 30, 2010.
- 2. American Association of Colleges of Pharmacy Center for the Advancement of Pharmaceutical Education (CAPE). Educational Outcomes; 2004. http://www.aacp.org/resources/education/Documents/CAPE2004.pdf. Accessed March 30, 2010.
- 3.Proceedings of a summit on preventing patient harm and death from i.v. medication errors. Am J Health-Syst Pharm. 2008;65(24):2367–2379. [Google Scholar]
- 4. FDA's strategic plan: charting our course for the future. http://www.fda.gov/consumer/updates/strategicplan022908.html. Accessed March 30, 2010.
- 5.Daftary MN, Obisesan OA, Dutta A, Ward YL, Chase VY, Lakew DG. Identifying medication error training in pharmacy. ASHP Midyear Clinical Meeting; Dec. 2001; Vol. 36, pp. P-301E proceedings. [Google Scholar]
- 6.Fuhrman LC, Brady T, Buff W, Sadik F. Development of an all PharmD degree with an emphasis on integrated pharmaceutical care concepts. Am J Pharm Educ. 1997;61(4):107S. [Google Scholar]
- 7.Johnson MS, Latif DA. Medication error instruction in schools of pharmacy curricula: a descriptive study. Am J Pharm Educ. 2002;66(4):364–371. [Google Scholar]
- 8.Sakkara SR, Kasich LD, Tuttle DA, Abu-Baker AM, Howell H. Development and evaluation of a required patient safety course. Am J Pharm Educ. 2008;72(3) doi: 10.5688/aj720365. Article 65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Jackson TL. Application of quality assurance principles: teaching medication error reduction skills in a “real world” environment. Am J Pharm Educ. 2004;68(1) Article 17. [Google Scholar]
- 10.Brown M, Frost R, Ko Y, Woosely R. Diagramming patients' views of root causes of adverse drug events in ambulatory care: an online tool for planning education and research. Patient Educ Couns. 2006;62(3):302–315. doi: 10.1016/j.pec.2006.02.007. [DOI] [PubMed] [Google Scholar]
- 11.Cohen MR. Causes of medication errors. In: Cohen MR, editor. Med Errors. Washington DC: American Pharmacists Association; 2007. pp. 55–66. [Google Scholar]
- 12.Frankel RM, Beckman HB. Conversation and compliance with treatment recommendations: an application of micro-interactional analysis in medicine. In: Grossberg L, O'Keefe BJ, Wartella E, editors. Rethinking Communication: Paradigm Exemplars 2. Newbury Park, CA: Sage; 1989. pp. 60–74. [Google Scholar]
- 13.Gandhi TK, Weingart SN, Borus J, et al. Adverse drug events in ambulatory care. N Engl J Med. 2003;348(16):1556–1564. doi: 10.1056/NEJMsa020703. [DOI] [PubMed] [Google Scholar]
- 14.du Pre A. Communicating About Health: Current Issues and Perspectives. Mountain View, CA: Mayfield; 2000. [Google Scholar]
- 15.Evans BJ, Stanley RO, Burrows GD. Communication skills training and patients' satisfaction. Health Comm. 2000;4(2):155–170. [Google Scholar]
- 16.Noland C, Carl WJ. “It's Not Our Ass”: Medical Resident Sense-Making Regarding Lawsuits. Health Comm. 2006;20(1):81–91. doi: 10.1207/s15327027hc2001_8. [DOI] [PubMed] [Google Scholar]
- 17.Valente CM, Antlitz AM, Boyd MD, Troisi AJ. The importance of physician-patient communication in reducing medical liability. Md Med J. 1988;37(1):75–78. [PubMed] [Google Scholar]
- 18. Aspden P, Wolcott J, Bootman JL, Cronewett LR. Preventing medication errors: quality chasm series. National Academy of Sciences Executive Summary. www.nap.edu. Accessed March 30, 2010.
- 19.Gallagher TH, Waterman AD, Ebers AG, Fraser VJ, Levinson W. Patients' and physicians' attitudes regarding the disclosure of medical errors. JAMA. 2003;289(8):1001–1007. doi: 10.1001/jama.289.8.1001. [DOI] [PubMed] [Google Scholar]
- 20.Levinson W, Gallagher TH. Disclosing medical errors to patients: a status report in 2007. Can Med Assoc J. 2007;177(3):265–267. doi: 10.1503/cmaj.061413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Noland C, Rickles NM. Reflection and analysis of how pharmacy interns learn to communicate about medication errors. Health Comm. 2009;24(4):351–360. doi: 10.1080/10410230902889399. [DOI] [PubMed] [Google Scholar]
- 22.Laurier C, Archambault A, Contrandriopoulos AP. Communication of verbal information by community pharmacists. DICP Ann Pharmacother. 1989;23(11):862–868. doi: 10.1177/106002808902301105. [DOI] [PubMed] [Google Scholar]
- 23.Kirking D. Evaluation of an explanatory model of pharmacists' patient counseling activities. Contemp Pharm Pract. 1982;5(4):230–238. [PubMed] [Google Scholar]
- 24.Laurier C, Poston J. Perceived levels of counseling among Canadian pharmacists. J Soc Admin Pharm. 1992;9(3):104–113. [Google Scholar]
- 25.Thorton BC. Blowing the whistle. In: Thorton BC, Kreps GL, editors. Perspectives on Health Communication. Prospect Heights, IL: Waveland Press; 1993. pp. 181–185. [Google Scholar]