Abstract
Objective
To develop, implement, and evaluate the use of electronic medical records (EMRs) in disease state management activities to teach pharmacy students patient-centered care skills.
Design
Faculty created 12 patient cases and an EMR for each simulated patient. Students used the information in the EMR to confirm the presence of a disease in their patient; to design and monitor an evidence-based patient-centered care plan, and document their assessment, medication, and monitoring recommendations; and to follow up in a SOAP (subjective, objective, assessment, plan) note format within the EMR.
Assessment
A precourse and postcourse survey instrument was administered to assess students' perceived gains in knowledge and attitudes regarding the use of EMRs for learning patient-centered care skills. A grading rubric was used to evaluate each SOAP note.
Conclusion
Implementation of disease state management activities involving EMRs improved pharmacy students' patient care skills.
Keywords: pharmaceutical care, electronic medical record, SOAP, patient-centered care, simulation, patient simulation
INTRODUCTION
The American Association of Colleges of Pharmacy Center for the Advancement of Pharmaceutical Education (CAPE) Advisory Panel on Educational Outcomes has defined criteria for providing pharmaceutical care. The CAPE outcomes state that doctor of pharmacy (PharmD) graduates should be able to provide exemplary patient-centered care including the ability to obtain, interpret, and evaluate patient information; determine the presence of a disease or medical condition; assess the need for treatment and/or referral; and identify patient-specific factors that affect health, pharmacotherapy, and/or disease management. Graduates should also be able to design, implement, monitor, and adjust patient-centered care plans and document care activities to facilitate communication and collaboration among the health care team.1
Standard 11, guideline 11.2, of the Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy outlines the use of innovative instructional technologies, case studies, and simulated electronic patients to foster the development of critical thinking and problem-solving in students.2 Using an EMR to present disease state management cases is a unique learner-centric method of teaching patient-centered care skills to pharmacy students. Active-learning is used within a synchronous environment to guide students in the development of higher-order thinking through the application of didactic coursework topics to disease state management cases.
This article describes how third-year pharmacy students used EMRs to develop skills in patient-centered care.
DESIGN
Pharmaceutical Care Laboratory III is part of a 4-semester laboratory sequence. Eight 2-hour laboratory sections taught by 4 pharmacist faculty members were offered each week, with 12 third-year students enrolled in each section. Laboratory activities focused on nonsterile and sterile compounding, point of care testing, immunizations, and disease state management. Students also practiced basic physical assessment including blood pressure, pulse, and respiration rate. Disease state management activities using the EMR were introduced to provide a platform for students to practice advanced skills in patient-centered care. Activities were designed to correlate with course content taught in a weekly 1-hour pharmaceutical care lecture series and didactic coursework. Previously, disease state management activities had not been emphasized in Pharmaceutical Care Laboratory III.
Disease state management activities were developed in response to the evolving role and responsibilities of pharmacists to provide pharmaceutical care including disease state management and medication therapy management. Faculty members and fourth-year pharmacy students developed and replicated 12 different patient cases for each disease state. Each student within a laboratory section was assigned a unique patient case. Disease state activities were designed to correlate with didactic course content taught throughout the third year. Disease states included tobacco abuse, anticoagulation, hypertension, community acquired pneumonia, and hyperlipidemia. Appendix 1 contains an example of 1 case variation developed for a patient with hypertension. The complexity of each student's patient case increased as additional comorbidities were introduced throughout the semester.
Each student experience was dependent on the assigned case variation. For example, 1 student may have followed a patient who was successful at smoking cessation, had controlled hypertension, uncontrolled hyperlipidemia, contracted community acquired pneumonia, and developed atrial fibrillation over the course of 1 semester. Another student may have followed a patient who refused to consider smoking cessation, had uncontrolled hypertension, uncontrolled hyperlipidemia, required treatment for hospital acquired pneumonia, and developed a deep vein thrombosis.
Students used an EMR to review their patient's active and inactive problems, allergy information, surgical, family and social histories, current medications, nicotine and alcohol use, symptoms, vital signs, and laboratory and radiology reports. Students used evidenced-based patient care guidelines and knowledge gained in didactic courses to confirm the presence of a disease, to design and monitor an evidence-based patient-centered care plan, and to document their assessment, plan, medication and monitoring recommendations, and follow up in a SOAP (subjective, objective, assessment, plan) note within an EMR. Students utilized all levels of Bloom's Taxonomy of the cognitive domain when completing EMR activities.3 For example, when assigned a hypertension case, students were expected to use knowledge and comprehension to recall and explain how risk factors led to the development of hypertension. They used application and analysis to explore the levels of intervention after confirmation of hypertension. Synthesis and evaluation were used as the student defended their recommendation during the composition of their SOAP notes.
The faculty facilitated each EMR activity and provided students with verbal feedback during laboratory and written feedback via a SOAP note grading rubric which evaluated students written patient assessment, goals of therapy, medication and monitoring recommendations, and follow-up. If a student SOAP note was accurate and appropriate, the recommendation was considered to have been accepted by the attending physician and the patient was considered to have been successfully treated. If a student SOAP note was missing information or the information submitted was judged by the instructor to be be harmful to the patient, the student was required to continue to recommend treatment for the previously assigned disease state in addition to any newly introduced disease states.
Prior to attending the laboratory, students were directed to read national treatment guidelines or review articles. This information was used to supplement knowledge gained through didactic coursework and to assist the students in decision making.4 They were also encouraged to use their didactic course notes while in the laboratory. The North Dakota State University Institutional Review Board approved the informed consent documents and survey instruments used to evaluate the disease state management activities.
EVALUATION AND ASSESSMENT
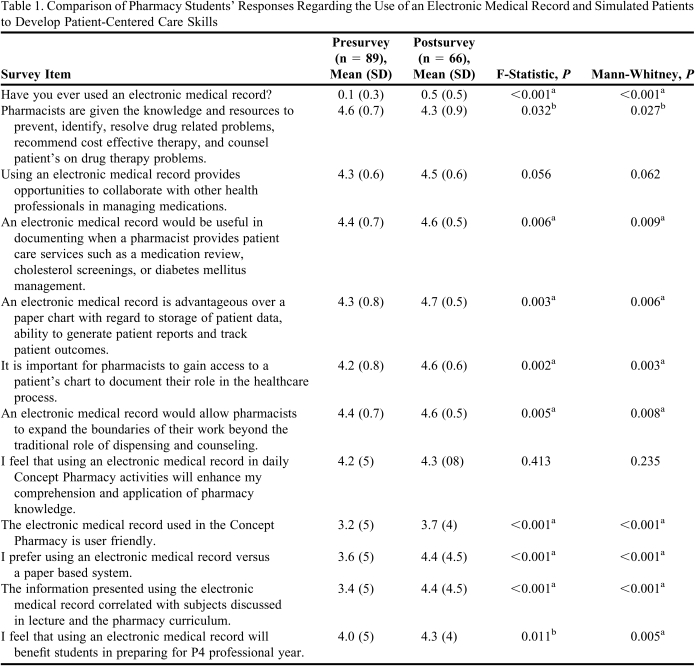
An 18-item precourse and 21-item postcourse survey instrument were administered online to assess students' perceived gains in knowledge secondary to using the EMR. Student participation was voluntary and anonymous. Eighty-nine (95%) students completed the pre-course survey instrument and 66 (70%) students completed the postcourse survey instrument (Table 1). Data were analyzed with ANOVA and Mann-Whitney tests using a 5% significance level. Questions 1 and 2 gathered student demographic information including gender and age. Question 3 asked students whether they had ever used an EMR. Students responded to the remaining questions using a 5-point Likert scale. Questions 4, 6 through 9, and 11 through 14 revealed significant gains in perceived knowledge. By the end of the semester, 88% of students agreed that pharmacists had the knowledge and resources to positively impact patients' drug therapy problems. Ninety-seven percent of students agreed that access to a patient EMR would be useful for documentation of patient care activities. All students thought access to a patient EMR would allow pharmacists to expand their role within the healthcare team.
Table 1.
Comparison of Pharmacy Students' Responses Regarding the Use of an Electronic Medical Record and Simulated Patients to Develop Patient-Centered Care Skills
a Indicates the correlation is significant at the 0.01 level (2-tailed)
b Indicates that the correlation is significant at the 0.05 level (2-tailed)
All students agreed that EMRs provide opportunities to collaborate with other health professionals in managing medications. Students (92%) also agreed that the information presented via the EMR correlated with subjects discussed in didactic course work. Ninety-four percent agreed that disease state management activities were perceived to be beneficial in preparation for advanced pharmacy practice experiences during the fourth year. SOAP notes were graded using a rubric developed by faculty members. The rubric evaluated the student's written patient assessment, goals of therapy, medication and monitoring recommendations, and anticipated follow-up. Each of the focus areas were graded using a 3-point Likert scale on which 1= missing, 3 = incomplete, and 5 = complete. Each activity had a value of 30 points.
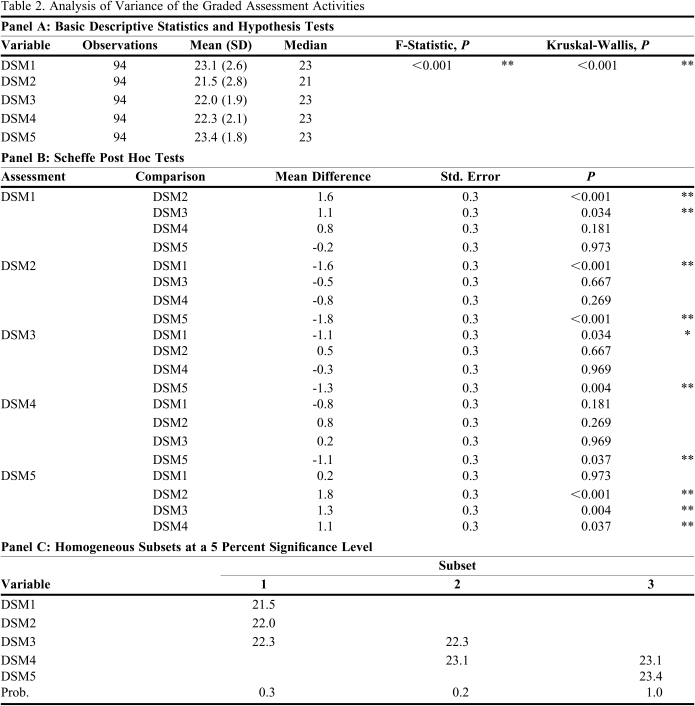
Data were analyzed using F statistics and the Kruskal-Wallis test with a 0.05 significance level. Table 2 illustrates the actual value of the disease management activities by comparing students' perceptions of their overall learning. Students learned the most during activities focused on tobacco abuse and hyperlipidemia. They learned more during activities focused on hypertension and community-acquired pneumonia than anticoagulation. Students may feel that pharmacists have a more pronounced role in the care of patients who wish to stop using tobacco. This may be due to the availability of nonprescription cessation aids and the pharmacist's ability to have an immediate and positive impact on a patient's success by recommending a cessation product and counseling the patient on appropriate use. Increases in SOAP note scores may also indicate that students have a higher interest in tobacco abuse and hyperlipidemia topics.
Table 2.
Analysis of Variance of the Graded Assessment Activities
Abbreviations for EMR Graded Assessment Activities:
DSM1= Assessment of using EMR to provide tobacco abuse disease state management
DSM2 = Assessment of using EMR to provide anticoagulation disease state management
DSM3 = Assessment of using EMR to provide hypertension disease state management
DSM4 = Assessment of using EMR to provide community acquired pneumonia disease state management
DSM5 = Assessment of using EMR to provide hyperlipidemia disease state management
DISCUSSION
With an increasing emphasis on disease state management and medication therapy management, pharmacy students require additional education and training to meet the demands of their evolving roles. Pharmacy students must work to develop skills in patient-centered care.5 We used electronic simulation and instructor feedback to assist students in developing these skills. Simulation enables students to learn through an engaging and interactive training process and to apply their knowledge without risk to a real patient.6 The EMR allowed students access to information which helped them to identify and improve compliance, simplify medication regimens, decrease adverse effects, and effectively control and monitor medication therapy. SOAP note activities have been determined to provide students with realistic simulated patient encounters requiring higher order thinking and improved documentation skills.7
In this course, students longitudinally followed and provided healthcare for 1 patient. Once a large cohort of patients has been established, students could potentially receive more than 1 patient case to follow. An increased case load would further develop the realism of using EMRs. In addition, we will also add diversity to our patient population. Culture and language significantly impact both health care processes and outcomes; therefore, we plan to add diversity to our patient population and promote cultural competency in our students. We will also integrate other pharmaceutical care laboratory activities such as dispensing, consultation, nonsterile and sterile compounding.
Overall, students felt that using EMRs was a constructive experience. Open-ended questions were administered with the postcourse survey to determine what students liked most and least about the EMR activities. They reported feeling as if they were working with a real patient and were excited to be able to apply acquired knowledge to care for the patient. They felt the activities were realistic, practical, and challenged them to think critically. Students were particularly interested in seeing the impact of their recommendations as they progressed through the semester.
The limitations of this study include that self-reported outcome measures and student self-assessments were used. To better control for these variables, a randomized, controlled trial with appropriate outcome measures could provide objective evidence to further the use of EMRs for simulated patients in the pharmacy education curriculum. In addition, certain topics may have correlated better with didactic coursework, so that the information students learned was more recent and accessible leading to higher scores.
SUMMARY
An assignment using EMRs and simulated patients to challenge pharmacy students to develop patient-centered care skills was successfully piloted for third-year students in a pharmaceutical care laboratory course. Students improved their skills in providing patient-centered care during disease state management activities focused on anticoagulation, community-acquired pneumonia, hypertension, hyperlipidemia, and tobacco use.
ACKNOWLEDGEMENTS
The author acknowledges District Five of the National Association of Boards of Pharmacy/American Association of Colleges of Pharmacy for supporting the purchase of SOAPware, version 5 (SOAPWARE Inc., Fayetteville, AR) through an individual study grant. The author thanks Dan Freisner, PhD, from the Department of Pharmacy Practice, for his assistance with data analysis; Collins Mutegi from the Information Technology Services for his assistance in installing and maintaining SOAPware; and Jennifer Bodmer, academic experiential student, for assistance with project launch and maintenance, North Dakota State University, Fargo.
Appendix 1. Patient Case Example
Patient A-female
Hypertension.1
Subjective: “My doctor told me that my blood pressure was high at my last appointment. She suggested I have it checked again in a couple weeks. The pharmacist checked it last week; I think she wrote down the number on a card. Let me see if I can find it.”
Objective: Patient is a 45 yowf who presents to the University Clinic for evaluation. Her pharmacist checked her blood pressure last week and it was 155/98mmHg. Her chart shows a reading of 151/96mmHg at a visit several weeks ago. The patient states she doesn't have time to exercise and doesn't drink alcohol.
REFERENCES
- 1. The AACP Center for the Advancement of Pharmaceutical Education (CAPE) Advisory Panel on Educational Outcomes. 2004 Educational Outcomes. Available at: http://www.aacp.org/resources/education/Documents/CAPE2004.pdf.
- 2. Accreditation Council for Pharmacy Education (ACPE). Accreditation Standards and Guidelines for the Professional Program in Pharmacy Leading to the Doctor of Pharmacy Degree. Chicago, Illinois. 18 May 2009. http://www.acpe-accredit.org/pdf/ACPE_Revised_PharmD_Standards_Adopted_Jan152006.pdf.
- 3.Castle A. Demonstrating critical evaluation skills using Bloom's taxonomy. Int J Ther Rehabil. 2003;10(8):369–373. [Google Scholar]
- 4.Chobanian AV, Bakris GL, Black HR, et al. the National High Blood Pressure Education Program Coordinating Committee. The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The JNC 7 report. JAMA. 2003;289(19):2560–2572. doi: 10.1001/jama.289.19.2560. [DOI] [PubMed] [Google Scholar]
- 5.Weller JM. Simulation in undergraduate medical education: bridging the gap between theory and practice. Med Educ. 2004;38(1):32–38. doi: 10.1111/j.1365-2923.2004.01739.x. [DOI] [PubMed] [Google Scholar]
- 6.Medelez E, Burgun A, Le Duff F, Le Beux P. Integration of electronic resources and communication technologies during clinical reasoning learning sessions. Stud Health Technol Inform. 2002;(90):107–111. [PubMed] [Google Scholar]
- 7.Brown MC, Kotlyar M, Conway J, Seifert R, St. Peter JV. Integration of Internet-based medical chart into a pharmacotherapy lecture series. Am J Pharm Educ. 2007;15;;71(3):53–57. doi: 10.5688/aj710353. [DOI] [PMC free article] [PubMed] [Google Scholar]