Abstract
Pericardial cysts are benign intrathoracic lesions that are considered to be congenital. They are usually found incidentally upon chest radiography and typically cause few symptoms. Their true incidence is unknown.
Herein, we describe the case of a 41-year-old man who, over nearly a decade, had undergone frequent hospital admissions for fever and thoracic pain. Computed tomography had shown no evidence of any intrathoracic mass. He was admitted to the hospital with fever, chest pain, tachycardia, dyspnea, and cough. The symptoms persisted despite medical therapy. Computed tomography revealed a pericardial cyst on the right side of the anterior mediastinum, near the confluence of the brachiocephalic vein and the superior vena cava and very close to the ascending aorta. The mass compressed the right main bronchus. Due to the cyst's unusual location and the ineffectiveness of medical therapy, we excised the tumor via median sternotomy. We found a large (7 × 4-cm), well-circumscribed, unilocular cyst, which unexpectedly involved the outside pericardial surface and the phrenic nerve. Histopathologic examination confirmed that the lesion was a simple mesothelial cyst of the pericardium. After the surgery, the patient's fever and chest pain resolved.
We know of no other report of a pericardial cyst that had gone undetected upon earlier computed tomography. We believe that surgical treatment of pericardial cysts should be reserved for patients who have severe symptoms due to complications, or when diagnosis is uncertain and malignancy is suspected.
Key words: Dyspnea/etiology; mediastinal cyst/complications/diagnosis/pathology/radiography/surgery/ultrasonography; pericardial effusion/etiology; tomography, X-ray computed; treatment outcome
Mesothelial cysts of the pericardium are approximately one third as common as are cardiac myxomas; however, their true incidence is unknown. These cysts typically cause few symptoms and are chiefly found incidentally, on chest radiography.1 Herein, we describe the case of a patient who experienced fever and thoracic pain for nearly a decade, whereupon computed tomography (CT) revealed a previously undetected mesothelial cyst of the pericardium. We are aware of no other report in the medical literature of a newfound pericardial cyst that had gone undetected on previous CT.
Case Report
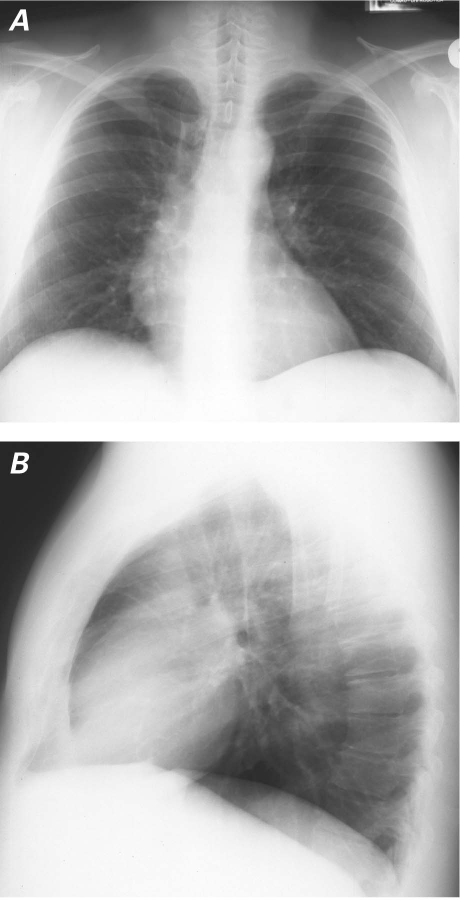
In October 2007, a 41-year-old man was admitted to our hospital with chest pain, fever, tachycardia, dyspnea, and an antibiotic-resistant cough of 10 days' duration. He had hypertension, and he was a smoker. He had a 9-year history of fever and chest pain without signs of myocardial ischemia. Approximately 8 years before the current presentation, CT had shown normal pericardial structure, and chest radiographs 3 and 5 years later had revealed no pericardial mass (Fig. 1).
Fig. 1 In 2002, chest radiographs showed no mass in the A) posteroanterior or B) lateral view.
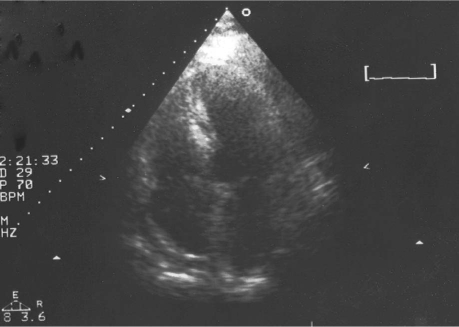
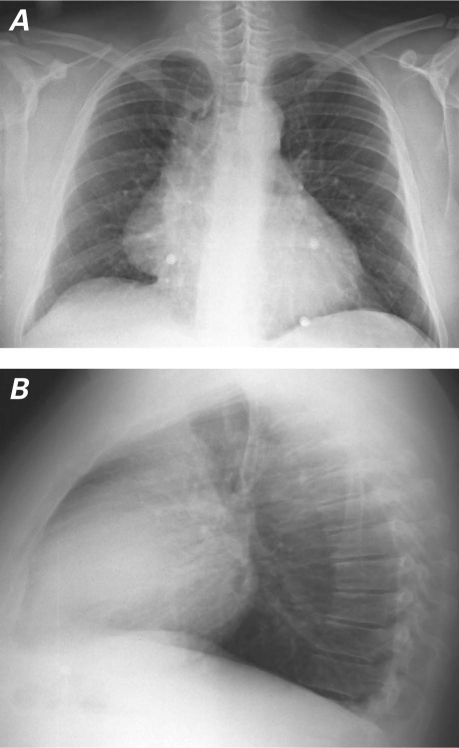
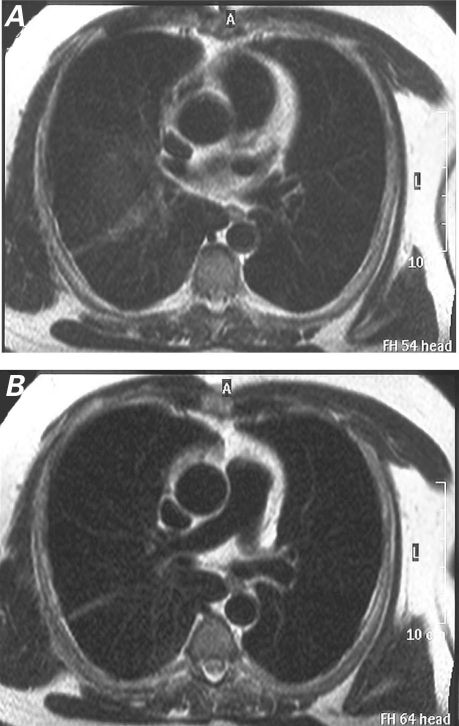
At the current admission, results of an electrocardiogram were normal, and a transthoracic echocardiogram showed mild effusion with a marked increase in pericardial thickness near the right atrium (Fig. 2). The white blood cell count was 12 ×109/L, the C-reactive protein level was 145 mg/L, and the plasma fibrinogen level was approximately 800 mg/dL. All these factors supported the hypothesis of infection. Chest radiography revealed a previously undetected mass on the right profile of the mediastinum (Fig. 3). Computed tomography was performed in order to further characterize the mass and its location. Results showed a large pericardial cyst (diameter, 4 cm) on the right side of the anterior mediastinum near the confluence of the brachiocephalic vein and the superior vena cava, very close to the ascending aorta (Fig. 4). The proximity of the mass to the right main bronchus most likely caused the patient's dyspnea.
Fig. 2 Preoperative transthoracic echocardiogram shows mild effusion with increased pericardial thickness near the right atrium.
Fig. 3 Preoperative chest radiographs in the A) posteroanterior and B) lateral views show a mass on the right profile of the mediastinum.
Fig. 4 Computed tomographic scans in the A) coronal and B) sagittal views show a large pericardial cyst (arrow) on the right side of the anterior mediastinum near the confluence of the brachiocephalic vein and the superior vena cava, close to the ascending aorta.
Because anti-inflammatory medical therapy and intravenous ciprofloxacin and ceftriaxone failed to reduce the patient's fever and dyspnea, the decision was made to resect the mass.
The surgical approach was via median sternotomy. The resection process was difficult because of the cyst's proximity to the superior vena cava and the ascending aorta. Intraoperatively, we observed that the cyst was implanted on the outside pericardial surface, near the phrenic nerve (which we were able to preserve). The well-circumscribed, unilocular cyst was approximately 4 × 7 cm and tan-white in color.
While being weaned from mechanical ventilation, the patient experienced right diaphragmatic paralysis. He underwent respiratory physiotherapy with a continuous positive airway pressure helmet and was discharged from the hospital on the 5th postoperative day. His respiratory function progressively improved. One year later, magnetic resonance imaging showed partial recovery of diaphragmatic function and an absence of residual mass (Fig. 5). After surgery, he experienced no further fever or thoracic pain, which supported the preoperative diagnostic assumption that the pericardial cyst was causing the patient's symptoms. Two years postoperatively, he remained free of symptoms.
Fig. 5 Magnetic resonance images at 1-year follow-up show partial recovery of diaphragmatic function and no residual mass.
Histopathologic Analysis of the Cyst
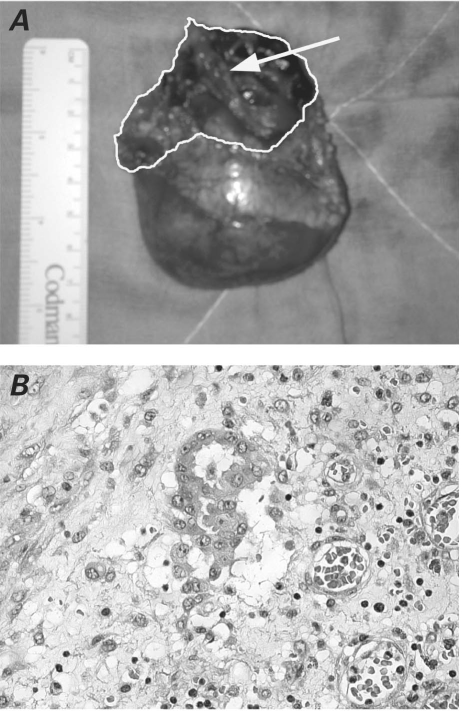
The resected cyst was sent for histopathologic evaluation. The cut surface showed a thickened (2–5 mm), fibrotic, gray-white wall containing hemorrhagic and fibrinous material (Fig. 6A).
Fig. 6 A) Photograph shows the excised pericardial cyst and the area where the cyst was implanted on the outside pericardial surface (arrow). B) Photomicrograph shows that the lesion is characteristic of a simple mesothelial cyst (H & E, orig. ×40).
The tissue was fixed in neutral buffered formalin, embedded in paraffin, and stained with hematoxylin and eosin for conventional histologic analysis. The cyst consisted of a fibrous, ulcerated wall, patchily lined with a single layer of flattened-to-cuboidal mesothelial cells that lacked cytologic atypia. A central area of hemorrhage was observed. Mitotic figures were absent, and nuclear pleomorphism was not seen. Immunohistochemical stain revealed expression of calretinin (a selective mesothelial marker) and positivity for cytokeratin AE1/AE3 antibody in islands of mesothelial cells (Fig. 6B).2,3 The diagnosis of simple mesothelial cyst of the pericardium was made.
Discussion
Pericardial cysts are benign intrathoracic lesions that result from aberrant formation of coelomic cavities. Although these cysts can be found anywhere from the superior mediastinum to the diaphragm, they typically develop in the anterior right cardiophrenic angle. Approximately 40% of mesothelial cysts are in unusual locations, and differentiating them from other mediastinal cysts is difficult.4,5 However, the absence of enhancement after contrast injection is integral to the radiologic diagnosis of a mesothelial cyst.
The natural history of a mesothelial cyst is usually uneventful—in fact, more than 50% of them are asymptomatic and are detected incidentally. Symptoms depend upon the degree of compression of surrounding structures, or on concomitant infection or bleeding. Our patient's fever was related to infection, a conclusion that is supported by the findings of leukocytosis and relevant hematologic signs. The cyst compressed the right main bronchus, causing the dyspnea.
The best treatment of pericardial cysts is not clearly defined and depends on each lesion's characteristics. Many authors agree with surgical excision in cases of complications or uncertain origin. Some suggest endoscopic resection6 or percutaneous aspiration7; unfortunately, adverse events and recurrence have been reported.8 Resection is typically approached via thoracotomy. Due to the location of our patient's cyst and the need to protect the vital structures nearby, we preferred median sternotomy.
The characteristics of our patient's case are unusual. First, the cyst was on the right profile of the mediastinum, far from the right cardiophrenic angle. Next, and in contrast with published data that describe pericardial cysts as congenital, the cyst was not seen upon earlier CT. We have found no previous reports of a similar case. Probably, the CT scan obtained 8 years earlier did not reveal the cyst because the lesion was extremely small and isolated within the pericardial surface. Although we agree that pericardial cysts are congenital lesions, we contend that they may grow as a consequence of chronic stimulation, such as previous pericarditis. In our patient, the pericardium did not show the typical features of chronic inflammation (widespread adhesions, increased thickening, and calcification); however, we cannot exclude the possibility that previous pericarditis (undiagnosed) was the cause of the cyst's development, via the activation of some growth factor or proliferation signal.
In conclusion, considering that the natural history of a pericardial cyst is typically uneventful, we believe that surgical treatment should be reserved for patients who experience severe symptoms due to complications, or when diagnosis is uncertain and malignancy is suspected.
Footnotes
Address for reprints: Fabrizio Sansone, MD, Department of Cardiac Surgery, San Giovanni Battista Hospital, C. so Bramante 88, 10127 Turin, Italy
E-mail: fabrisans@katamail.com
References
- 1.Burke A, Virmani R. Tumors of the heart and great vessels. Fascicle 16, 3rd Series. In: Atlas of tumor pathology. Washington (DC): Armed Forces Institute of Pathology; 1996. p. 99.
- 2.Borges AC, Gellert K, Dietel M, Baumann G, Witt C. Acute right-sided heart failure due to hemorrhage into a pericardial cyst. Ann Thorac Surg 1997;63(3):845–7. [DOI] [PubMed]
- 3.Bandeira FC, de Sa VP, Moriguti JC, Rodrigues AJ, Jurca MC, Almeida-Filho OC, et al. Cardiac tamponade: an unusual complication of pericardial cyst. J Am Soc Echocardiogr 1996;9(1):108–12. [DOI] [PubMed]
- 4.Omeroglu SN, Omeroglu A, Ardal H, Erkilinc A, Bal E, Ipek G, et al. Epicardial mesothelial cyst located over the left anterior descending coronary artery. Tex Heart Inst J 2004;31 (3):313–5. [PMC free article] [PubMed]
- 5.Collison SP, Tomar M, Shrivastava S, Iyer KS. A rare intrapericardial enterogenous cyst presenting in infancy. Ann Thorac Surg 2006;81(4):e11-2. [DOI] [PubMed]
- 6.Mouroux J, Venissac N, Leo F, Guillot F, Padovani B, Hofman P. Usual and unusual locations of intrathoracic mesothelial cysts. Is endoscopic resection always possible? Eur J Cardiothorac Surg 2003;24(5):684–8. [DOI] [PubMed]
- 7.Sharma R, Harden S, Peebles C, Dawkins KD. Percutaneous aspiration of a pericardial cyst: an acceptable treatment for a rare disorder. Heart 2007;93(1):22. [DOI] [PMC free article] [PubMed]
- 8.Westcott JL. Percutaneous needle aspiration of hilar and mediastinal masses. Radiology 1981;141(2):323–9. [DOI] [PubMed]