Abstract
We retrospectively evaluated early clinical results of coronary revascularization using none but arterial grafts in patients aged 65 years and older. The cases of 449 consecutive patients who had undergone isolated myocardial revascularization were divided into 2 groups: the arterial conduit group (n=107) received a left internal mammary artery (LIMA) graft and 1 or both radial arteries (RAs), while the mixed-conduit group (n=342) received a LIMA graft and 1 or more saphenous vein grafts (SVGs), with or without an RA.
There was no significant difference between the groups' rates of mortality. The arterial conduit group had a significantly shorter overall postoperative hospital stay than did the mixed-conduit group (mean, 6.6 ± 0.9 vs 7.2 ± 5 days; P=0.04). Linear regression analysis revealed that the presence of hypertension (β=0.13; 95% confidence interval [CI], 0.054–0.759; P=0.02) and high EuroSCORE (β=0.24; 95% CI, 0.053–0.283; P=0.004) were the major predicting factors for long hospital stay. Graft-harvest-site infection was statistically more frequent in the mixed-conduit group than in the arterial conduit group (6.4% vs 0, respectively; P=0.007). Angiography was performed postoperatively (mean, 24.9 ± 16.3 mo; range, 11–65 mo) in 21 patients. In these patients, all LIMA grafts were patent, as were 86.9% of the SVGs and 90.9% of the RA grafts.
Myocardial revascularization using all arterial grafts (at least 50% RAs) in patients aged 65 years and older is safe and reliable, produces short-term results equal to those of saphenous vein grafting, and can reduce graft-harvest-site infections.
Key words: Aged; coronary artery bypass; coronary disease/surgery; myocardial revascularization; post-operative complications; radial artery/transplantation; retrospective studies; saphenous vein/transplantation; surgical wound infection/prevention & control; tissue and organ harvesting; transplantation, autologous; thoracic arteries/transplantation; treatment outcome
In recent years, more and more elderly patients have been able to undergo coronary artery revascularization because of advancements in surgical techniques.1-3 Although these older individuals are at risk of postoperative sequelae from many concomitant diseases, the operative results associated with revascularization have continued to improve.4,5 Use of the left internal mammary artery (LIMA) as a bypass graft for the left anterior descending coronary artery (LAD) is the main innovation that has improved survival rates and reduced late cardiac events after coronary artery bypass grafting (CABG).6-8 Use of the radial artery (RA) has also yielded favorable angiographic and clinical results, including very good long-term patency, better healing of the forearm than of the leg (as a harvesting site, when use of the RA is compared with use of the saphenous vein), and lower risk of wound infection. Although the RA is now considered a suitable conduit for CABG,9-11 more information is needed on outcomes. We designed this study to evaluate early clinical results of all-arterial revascularization of the coronary arteries using LIMA and RA grafts in patients aged 65 and older.
Patients and Methods
The study sample comprised 449 consecutive patients aged 65 years and older who underwent isolated CABG at Turgut Ozal Medical Center from September 2001 through February 2007. These individuals were divided retrospectively in accordance with the specifics of their operations. One group (the arterial conduit group, n=107) received arterial conduits only: a LIMA graft and 1 or both RAs. The other (the mixed-conduit group, n=342) received a LIMA graft and 1 or more saphenous vein grafts (SVGs), with or without an RA. A computerized clinical database was used to review the details of each case. The exclusion criteria were certain concomitant procedures (left ventricular aneurysmectomy, carotid endarterectomy, and valve or aortic surgery), emergency operation, and reoperation.
Data Collection and Definitions
The variables recorded preoperatively were patient age and sex; body mass index; presence or absence of unstable angina; history of hypertension, diabetes mellitus, smoking, hyperlipidemia, or chronic obstructive pulmonary disease; previous cerebrovascular accident or myocardial infarction (MI); presence or absence of carotid artery disease or renal dysfunction; left ventricular ejection fraction; and presence or absence of left main coronary artery (LMCA) disease. The intraoperative data collected were number of grafts per operation, types of grafts used (for example, LIMA, RA, and venous grafts), cardiopulmonary bypass (CPB) time, and aortic cross-clamp time. The data collected in regard to postoperative outcomes were mechanical ventilation time; need for inotropic or intra-aortic balloon pump support; development of atrial fibrillation, perioperative MI (immediate postoperative period), renal dysfunction, or infective, neurologic or gastrointestinal complications; re-exploration for bleeding or cardiac tamponade; length of stay in the intensive care unit; length of overall hospital stay; and operative death (defined as death in the first 30 days after CABG). In addition, each individual's EuroSCORE was calculated on the basis of his or her demographic and clinical characteristics. Clinical follow-up was done via telephone and routine follow-up appointments. The mean follow-up time was 29.7 ± 11.3 months (range, 3–65 mo). Patients were rechecked at 1 week and 1 month postoperatively, and then every 3 months thereafter.
Surgical Technique
Details of the surgical techniques used for complete revascularization by means of arterial grafts only have been described previously.12 Most of the operations in this study (n=426; 94.9%) were performed using CPB, and the remainder (n=23; 5.1%) were performed off-pump. In each case in which an RA was used, the adequacy of collateral circulation to the hand was evaluated preoperatively with the Allen test, and then again intraoperatively by means of digital plethysmography. Radial-artery harvesting was carried out using our previously documented technique,12 simultaneously with LIMA harvesting. Saphenous veins were harvested using conventional methods. The preoperative exclusion criteria for RA harvesting were a positive Allen test, significant RA stenosis, severe RA plaque or calcification as revealed by Doppler ultrasonography, or a history of vasculitis or Raynaud's disease. The choice of graft material was left to the surgeon, but certain protocols applied. The LIMA was used routinely as a graft for the LAD; RA and SVG conduits were used mainly to bypass vessels other than the LAD; and only RA conduits were used to bypass vessels other than the LAD if those vessels exhibited more than 70% stenosis.
Postoperative Management
Electrocardiographic analyses were performed immediately after each operation; on postoperative days 1, 2, and 4; and just before hospital discharge. Patients received intravenous nitroglycerin for the first 24 hours after surgery, provided that systolic blood pressure was >90 mmHg. A calcium-channel blocker (diltiazem) was administered intravenously during the operation and was continued through day 1. Oral calcium-channel blocker therapy was continued for 1 year after surgery. Patients were also prescribed a regimen of aspirin (300 mg daily), starting immediately after extubation. Cholesterol-lowering agents were prescribed after hospital discharge and, along with aspirin, were continued indefinitely as long-term maintenance therapy.
Statistical Analysis
The data were statistically analyzed using SPSS for Windows, version 10.0 (SPSS Inc.; Chicago, Ill). Data for patient characteristics and outcomes were expressed either as a percentage of total or as mean ± SD. Group categorical data were compared using the χ2 test or Fisher's exact test. Results for continuous variables were compared using an independent t test. A P value of less than 0.05 was considered significant. Linear regression analy-sis and logistic regression analysis, respectively, were performed to identify independent factors associated with hospital stay and harvest-site infections.
Results
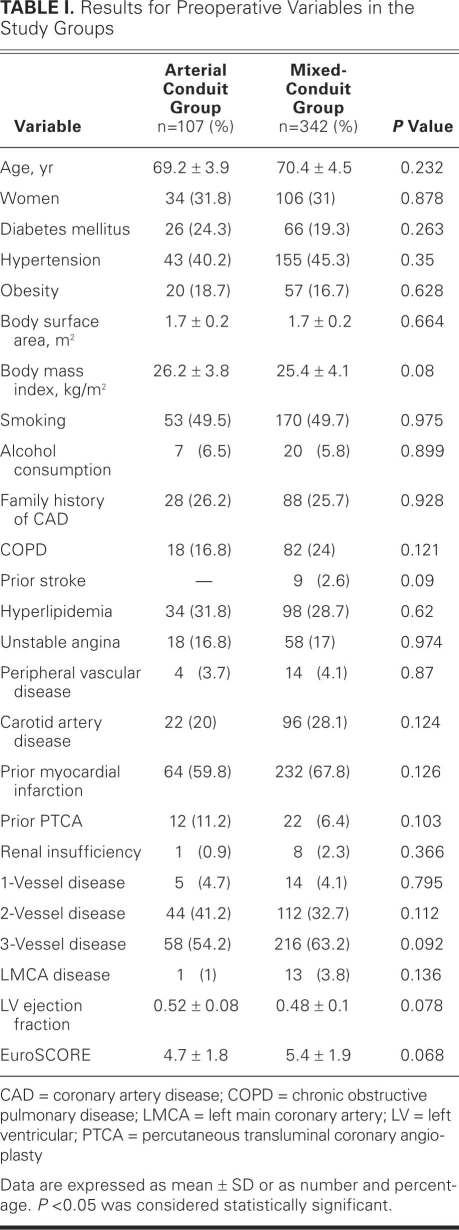
The preoperative demographic characteristics are summarized in Table I. The mean age was 69.2 ± 3.9 years in the arterial conduit group and 70.4 ± 4.5 years in the mixed-conduit group. There were no significant differences between the 2 groups with respect to sex distribution; prevalence of chronic obstructive pulmonary disease; frequency of previous percutaneous transluminal coronary angioplasty; prevalence of hypertension, obesity (body mass index, ≥30 kg/m2), hyperlipidemia, smoking, diabetes mellitus, unstable angina, or LMCA disease; proportions of patients with previous MI or cerebrovascular accident; or proportions of patients with carotid artery disease or renal dysfunction. There were also no statistical differences between the groups with respect to mean number of diseased vessels, mean left ventricular ejection fraction, or EuroSCORE.
TABLE I. Results for Preoperative Variables in the Study Groups
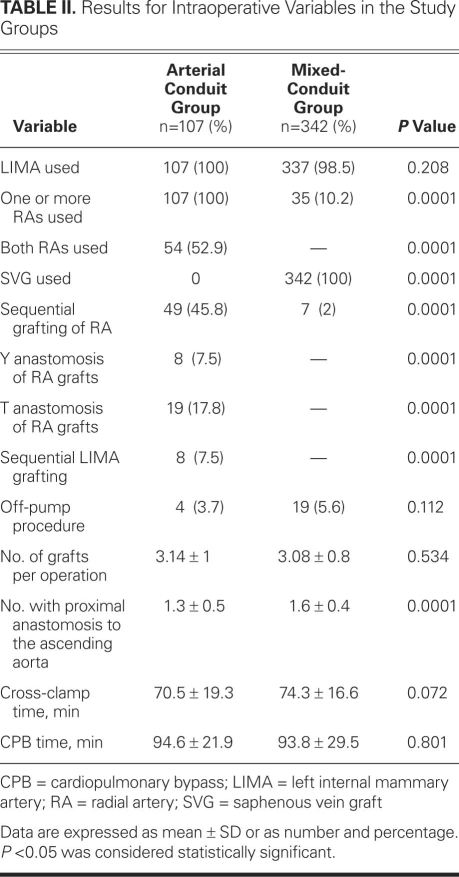
The operative data are presented in Table II. There were no significant differences between the groups' mean cross-clamp times or mean CPB times. The mean numbers of coronary bypass grafts were 3.14 ± 1 in the arterial conduit group and 3.08 ± 0.8 in the mixed-conduit group. The LIMA was used for surgical revascularization of the LAD in all cases in the arterial conduit group (100%), and in 337 (98.5%) of the cases in the mixed-conduit group. The sequential anastomoses in the arterial conduit group were performed using the RA in 49 cases (45.8%) and the LIMA in 8 cases (7.5%). Both RAs were used in 54 (50.5%) of the arterial conduit group. In the mixed-conduit group, SVGs were used for all of the cases. The mean number of patients with proximal anastomosis to the ascending aorta was significantly higher in the mixed-conduit group (1.3 ± 0.5 vs 1.6 ± 0.4; P=0.0001).
TABLE II. Results for Intraoperative Variables in the Study Groups
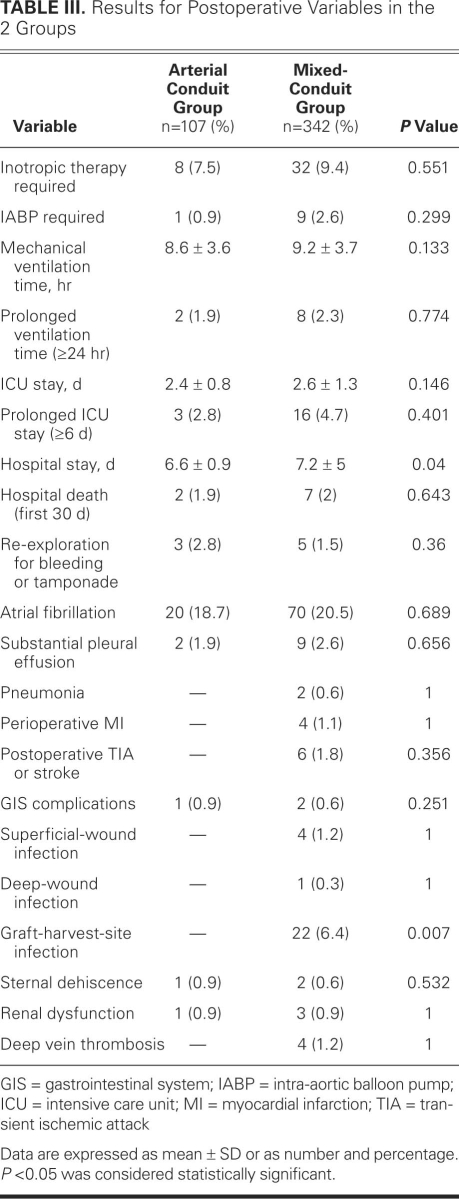
The findings for postoperative outcome are listed in Table III. There was no difference between groups with respect to hospital death (1.9% vs 2%, respectively) or postoperative intensive care unit stay. However, the arterial conduit group had a shorter overall hospital stay than did the mixed-conduit group (6.6 ± 0.9 vs 7.2 ± 5 days; P=0.041). Linear regression analysis to evaluate the factors associated with hospital stay revealed that EuroSCORE (β=0.24; 95% CI, 0.053–0.283; P=0.003) and the presence of hypertension (β=0.13; 95% CI, 0.054–0.759; P=0.03) were factors independently associated with hospital stay. The harvest-site infection rate was significantly higher in alcohol-drinking patients than in nondrinkers (18% vs 5%; P=0.04). However, alcohol was not independently associated with harvest-site infection. There were no significant differences between the groups with respect to the incidence of perioperative low-output syndrome (the requirement for inotropic support or intra-aortic balloon pump support) or mean mechanical ventilation time. There were also no significant differences between the 2 groups' rates of postoperative sequelae, including re-exploration for bleeding or tamponade, atrial fibrillation, perioperative MI, major pleural effusion, pneumonia, gastrointestinal and neurologic events, superficial or deep-wound infection, sternal-wound dehiscence, new-onset renal dysfunction, and deep vein thrombosis (DVT). There were no infections at any of the RA harvesting sites, whereas 22 (6.4%) of the mixed-conduit group developed infection at saphenous-vein harvesting sites (P=0.007). The only complication associated with RA harvesting was transient paresthesia in 15 patients (14%).
TABLE III. Results for Postoperative Variables in the 2 Groups
During follow-up, 21 patients with symptoms of angina (8 in the arterial conduit group and 13 in the mixed-conduit group) underwent angiography at 24.9 ± 16.3 postoperative months (range, 11–65 mo). A total of 66 grafts were examined in these individuals, including 21 LIMAs, 22 RAs, and 23 SVGs. All the LIMAs were patent, as were 90.9% of the RAs and 86.9% of the SVGs.
Discussion
Our findings indicate that, for patients aged 65 years and older, short-term results after revascularization using only arterial conduits (mostly RA grafts) are similar to short-term results observed after conventional coronary surgery using mixed-conduits (including SVG grafts). The only differences we detected between our arterial conduit and mixed-conduit groups were hospital-stay times and harvest-site infection rates, with higher numbers of harvest-site infections and longer hospital stays in the mixed-conduit group.
Although the impact of coronary revascularization with the use of all-arterial grafts has been well documented in the general population, there are few published data on this practice in application to elderly patients. Our study of patients aged 65 years and older suggests that complete arterial revascularization using mostly RAs and conventional CABG using a mixture of arterial grafts and SVGs yield similar early postoperative outcomes. However, we observed higher numbers of graft-harvest-site infections and longer hospital stays among SVG recipients.
The reported incidence rates for leg-wound complications after SVG harvesting in all age groups range from 1% to 24%.13-15 Commonly documented leg-wound complications after SVG harvesting include dermatitis, cellulitis, greater saphenous neuropathy, chronic non-healing wounds, and lymphoceles. These major adverse sequelae result in substantial morbidity and longer hospital stays, higher hospital costs, later mobilization, and additional surgical procedures.16
We used the traditional SVG-harvesting technique in our patients, but there are some effective alternatives. Greenfield and coworkers17 evaluated wound-healing in a group that underwent minimally invasive SVG harvesting by means of the SaphLITE retractor system; and Crouch and coworkers18 evaluated wound complications and vein-graft quality in a group that underwent endoscopic SVG harvesting. Both Greenfield and Crouch reported that their techniques were effective alternatives that led to improved wound-healing and less morbidity, when compared with traditional SVG harvesting. In contrast, arm-wound complications after RA harvesting are rare. Tatoulis and coworkers19 evaluated RA-harvest-site results in 2,417 patients who received one or more RA grafts during CABG and observed a 0.08% incidence of fingertip ischemia. They also reported a 0.4% incidence of forearm hematoma and no major forearm infections. In our study, we observed infection at the harvest site in 22 (6.4%) patients in the mixed-conduit (including SVG) group and no harvest-site infections in the arterial conduit (mostly RA) group. Traditional SVG harvesting often requires a long incision to obtain a suitable length of graft vessel, and this is especially common in elderly patients because of the vein's dilated and ectatic structure in that age group. We observed DVT in 4 patients in our mixed-conduit group (1.2%), and we attribute this to late postoperative mobilization. One of the reasons for early death in this group was acute pulmonary embolism caused by DVT. In contrast, there was no instance of DVT in our arterial conduit group. The hospital stay for this group was significantly shorter than that for the mixed-conduit group in our study, which we attribute to early mobilization—enabled by the absence of a leg incision and the potential sequelae of SVG harvesting. The other major predicting factors for long hospital stay in our study were hypertension and a high EuroSCORE.
Although the difference between our arterial and mixed groups with respect to frequency of cerebrovascular accidents did not reach statistical significance, there was a higher rate of cerebrovascular events among patients who received SVGs. This is noteworthy because the mean number of patients who underwent proximal anastomosis to the ascending aorta was significantly higher in the mixed group. Anastomosis of RA grafts to the LIMA or to other RA grafts in T or Y fashion eliminates the need for proximal anastomosis to the ascending aorta, which is particularly important in elderly patients who have atherosclerosis in this portion of the aorta.
Early RA patency rates for all age groups after CABG (that is, patency in the first 3 months) have been reported to range from 96% to 100%, and the rates at 1 to 2 years range from 84% to 100%.20-22 The patency rates for RA grafts in our elderly patients were similar to those reported in previous studies; however, only a small subset of our patients underwent postoperative angiography.
Other Limitations. Our investigation had several limitations in addition to the general absence of follow-up angiographic results. Our retrospective methodology is among them. Another limitation is that patients were not randomly assigned to receive a single category of graft materials (RA or SVG); rather, decisions about graft types were left mainly to the surgeon, and patients received either a mixture of arterial grafts or a mixture of arterial and saphenous vein grafts.
Conclusion. As we have specified, RA grafts in our study were used only to bypass target vessels that exhibited more than 70% stenosis. We observed that patients 65 years and older who underwent all-arterial revascularization had perioperative morbidity and mortality rates similar to those of patients in the same age cohort who underwent conventional CABG with 1 or more saphenous veins. Further, our data indicate that, for this age group, the use of RAs in CABG may offer the additional benefits of fewer harvest-site infections and, consequently, shorter hospital stays. In alcohol-drinking patients, an RA graft can be chosen to decrease the risk of harvest-site infection. Overall, our findings suggest that all-arterial revascularization using mostly RAs is a reliable, feasible, and safe surgical approach that yields major acute outcomes similar to those of SVG use.
Footnotes
Address for reprints: Nevzat Erdil, MD, Department of Cardiovascular Surgery, Turgut Ozal Medical Center, Inonu University, 44315 Malatya, Turkey
E-mail: nerdil@inonu.edu.tr
References
- 1.Sakamoto S, Matsubara J, Matsubara T, Nagayoshi Y, Nishizawa H, Shouno S, et al. Coronary artery bypass grafting in octogenarians. Cardiovasc Surg 2001;9(5):487–91. [DOI] [PubMed]
- 2.Salomon NW, Page US, Bigelow JC, Krause AH, Okies JE, Metzdorff MT. Coronary artery bypass grafting in elderly patients. Comparative results in a consecutive series of 469 patients older than 75 years. J Thorac Cardiovasc Surg 1991;101 (2):209–18. [PubMed]
- 3.Carey JS, Cukingnan RA, Singer LK. Quality of life after myocardial revascularization. Effect of increasing age. J Thorac Cardiovasc Surg 1992;103(1):108–15. [PubMed]
- 4.Peterson ED, Cowper PA, Jollis JG, Bebchuk JD, DeLong ER, Muhlbaier LH, et al. Outcomes of coronary artery bypass graft surgery in 24,461 patients aged 80 years or older. Circulation 1995;92(9 Suppl):II85-91. [DOI] [PubMed]
- 5.Alexander KP, Anstrom KJ, Muhlbaier LH, Grosswald RD, Smith PK, Jones RH, Peterson ED. Outcomes of cardiac surgery in patients > or = 80 years: results from the National Cardiovascular Network. J Am Coll Cardiol 2000;35(3):731–8. [DOI] [PubMed]
- 6.Naik MJ, Abu-Omar Y, Alvi A, Wright N, Henderson A, Channon K, et al. Total arterial revascularisation as a primary strategy for coronary artery bypass grafting. Postgrad Med J 2003;79(927):43–8. [DOI] [PMC free article] [PubMed]
- 7.Cameron A, Davis KB, Green G, Schaff HV. Coronary bypass surgery with internal-thoracic-artery grafts–effects on survival over a 15-year period. N Engl J Med 1996;334(4):216–9. [DOI] [PubMed]
- 8.Kurlansky PA, Williams DB, Traad EA, Carrillo RG, Schor JS, Zucker M, et al. Arterial grafting results in reduced operative mortality and enhanced long-term quality of life in octogenarians. Ann Thorac Surg 2003;76(2):418–27. [DOI] [PubMed]
- 9.Cohen G, Tamariz MG, Sever JY, Liaghati N, Guru V, Christakis GT, et al. The radial artery versus the saphenous vein graft in contemporary CABG: a case-matched study. Ann Thorac Surg 2001;71(1):180–6. [DOI] [PubMed]
- 10.Acar C, Ramsheyi A, Pagny JY, Jebara V, Barrier P, Fabiani JN, et al. The radial artery for coronary artery bypass grafting: clinical and angiographic results at five years. J Thorac Cardiovasc Surg 1998;116(6):981–9. [DOI] [PubMed]
- 11.Modine T, Al-Ruzzeh S, Mazrani W, Azeem F, Bustami M, Ilsley C, Amrani M. Use of radial artery graft reduces the morbidity of coronary artery bypass graft surgery in patients aged 65 years and older. Ann Thorac Surg 2002;74(4):1144–7. [DOI] [PubMed]
- 12.Nisanoglu V, Battaloglu B, Erdil N, Ozgur B, Aldemir M, Cihan HB. Complete myocardial revascularization using arterial grafts only in patients with unstable angina: impact on early outcome. Thorac Cardiovasc Surg 2007;55(1):7–12. [DOI] [PubMed]
- 13.DeLaria GA, Hunter JA, Goldin MD, Serry C, Javid H, Najafi H. Leg wound complications associated with coronary revascularization. J Thorac Cardiovasc Surg 1981;81(3):403–7. [PubMed]
- 14.Utley JR, Thomason ME, Wallace DJ, Mutch DW, Staton L, Brown V, et al. Preoperative correlates of impaired wound healing after saphenous vein excision. J Thorac Cardiovasc Surg 1989;98(1):147–9. [PubMed]
- 15.Slaughter MS, Olson MM, Lee JT Jr, Ward HB. A fifteen-year wound surveillance study after coronary artery bypass. Ann Thorac Surg 1993;56(5):1063–8. [DOI] [PubMed]
- 16.Paletta CE, Huang DB, Fiore AC, Swartz MT, Rilloraza FL, Gardner JE. Major leg wound complications after saphenous vein harvest for coronary revascularization. Ann Thorac Surg 2000;70(2):492–7. [DOI] [PubMed]
- 17.Greenfield GT, Whitworth WA, Tavares LL, Wittenbraker MT, Wallace DM, Valdivia JA, et al. Minimally invasive vein harvest and wound healing using the SaphLITE Retractor System. Ann Thorac Surg 2001;72(3):S1046-9. [DOI] [PubMed]
- 18.Crouch JD, O'Hair DP, Keuler JP, Barragry TP, Werner PH, Kleinman LH. Open versus endoscopic saphenous vein harvesting: wound complications and vein quality. Ann Thorac Surg 1999;68(4):1513–6. [DOI] [PubMed]
- 19.Tatoulis J, Buxton BF, Fuller JA, Royse AG. Total arterial coronary revascularization: techniques and results in 3,220 patients. Ann Thorac Surg 1999;68(6):2093–9. [DOI] [PubMed]
- 20.Tatoulis J, Buxton BF, Fuller JA. Bilateral radial artery grafts in coronary reconstruction: technique and early results in 261 patients. Ann Thorac Surg 1998;66(3):714–20. [DOI] [PubMed]
- 21.Calafiore AM, Di Giammarco G, Teodori G, D'Annunzio E, Vitolla G, Fino C, Maddestra N. Radial artery and inferior epigastric artery in composite grafts: improved midterm angiographic results. Ann Thorac Surg 1995;60(3):517–24. [DOI] [PubMed]
- 22.Chen AH, Nakao T, Brodman RF, Greenberg M, Charney R, Menegus M, et al. Early postoperative angiographic assessment of radial grafts used for coronary artery bypass grafting. J Thorac Cardiovasc Surg 1996;111(6):1208–12. [DOI] [PubMed]