Abstract
Background
The belief that weight loss improves obstructive sleep apnea (OSA) has limited empirical support. The purpose of this 4-center study was to assess the effects of weight loss on OSA over a 1-year period.
Methods
The study included 264 participants with type 2 diabetes and a mean (SD) age of 61.2 (6.5) years, weight of 102.4 (18.3) kg, body mass index (BMI) (calculated as weight in kilograms divided by height in meters squared) of 36.7 (5.7), and an apnea-hypopnea index (AHI) of 23.2 (16.5) events per hour. The participants were randomly assigned to either a behavioral weight loss program developed specifically for obese patients with type 2 diabetes (intensive lifestyle intervention [ILI]) or 3 group sessions related to effective diabetes management (diabetes support and education [DSE]).
Results
The ILI participants lost more weight at 1 year than did DSE participants (10.8 kg vs 0.6 kg; P < .00l). Relative to the DSE group, the ILI intervention was associated with an adjusted (SE) decrease in AHI of 9.7 (2.0) events per hour (P < .001). At 1 year, more than 3 times as many participants in the ILI group than in the DSE group had total remission of their OSA, and the prevalence of severe OSA among ILI participants was half that of the DSE group. Initial AHI and weight loss were the strongest predictors of changes in AHI at 1 year (P<.01). Participants with a weight loss of 10 kg or more had the greatest reductions in AHI.
Conclusions
Physicians and their patients can expect that weight loss will result in significant and clinically relevant improvements in OSA among obese patients with type 2 diabetes.
Trial Registration
clinicaltrials.gov Identifier: NCT00194259
Weight loss is frequently recommended to improve obstructive sleep apnea (OSA) among obese patients, yet the empirical support for this recommendation is weak. 1,2 Descriptive studies have assessed the apneahypopnea index (AHI) before and after weight loss, although most have examined the effects of surgically induced weight loss.3 The existing studies are limited by small samples (N=8-26 participants), short durations (≤6 months), predominantly male samples (90%), and the lack of comparison groups that do not lose weight.3 One nonrandomized study of 23 participants with a mean (SD) AHI of 55 (8) events per hour and a mean (SD) weight of 112 (7) kg found that the AHI was reduced by 46% in those individuals who had lost 10% of initial weight, while those who were weight stable demonstrated no change in AHI.4 The only randomized study to date was among 72 predominantly male patients with mild apnea (AHI, 5-15) who weighed approximately 97 kg. An 11-kg weight loss reduced the risk of OSA by 76% relative to the control group, which lost 2 kg.5 Epidemiological studies have shown that weight loss reduced the AHI and weight gain increased the AHI, but very few participants in those cohorts had OSA or lost clinically significant amounts of weight.6,7 Therefore, there are few studies indicating whether the amount of weight loss (10%) recommended by expert and government panels is sufficient to improve OSA.8 Such data are necessary to help physicians and their patients understand the expected benefits of weight loss in the management of OSA.
Recently, we documented an extremely high rate (86%) of OSA among obese patients with type 2 diabetes seeking to lose weight.9 The purpose of this study was to assess the effect of weight loss, produced through an intensive lifestyle intervention, on OSA in obese patients with type 2 diabetes. We hypothesized that weight loss would significantly improve OSA. This study addressed the limitations of previous investigations by enrolling a large sample (n=264), with nearly equal numbers of men and women, and by using a randomized controlled trial design over a 1-year period.
METHODS
PARTICIPANTS
Participants for this study were enrolled in the Sleep AHEAD (Action for Health in Diabetes) study, an ancillary investigation of the Look AHEAD study, a 16-center randomized, controlled clinical trial investigating the long-term health impact of an intensive lifestyle intervention. In the Look AHEAD study, a total of 5145 overweight and obese adults with type 2 diabetes were randomized to intensive lifestyle intervention or to diabetes support and education. The details of Look AHEAD's design10 participant characteristics at baseline, 11 inrervenuon,12 and 1-year outcomes13 have been described elsewhere.
Primary inclusion criteria for Look AHEAD were patients aged 45 to 75 years with a body mass index (BMI) (calculated as weight in kilograms divided by height in meters squared) greater than or equal to 25 (≥27 if taking insulin), physician-verified type 2 diabetes, a hemoglobin A1c level of less than 11%, and a blood pressure reading of less than 160/100 mm Hg. In addition to Look AHEAD criteria, an exclusion criterion for the Sleep AHEAD study was previous surgical or current medical treatment for OSA. Patients with previously diagnosed but untreated OSA were eligible to participate.
Sleep AHEAD participants were recruited at 4 Look AHEAD sites: University of Pennsylvania, Philadelphia; University of Pittsburgh, Pittsburgh, Pennsylvania; Columbia University, New York, New York; and Brown University, Providence, Rhode Island. The study was approved by the institutional review boards at each of the participating sites, and all participants provided written informed consent. Participants and their primary care physicians were provided a summary of the polysomnogram (PSG) results after each assessment.
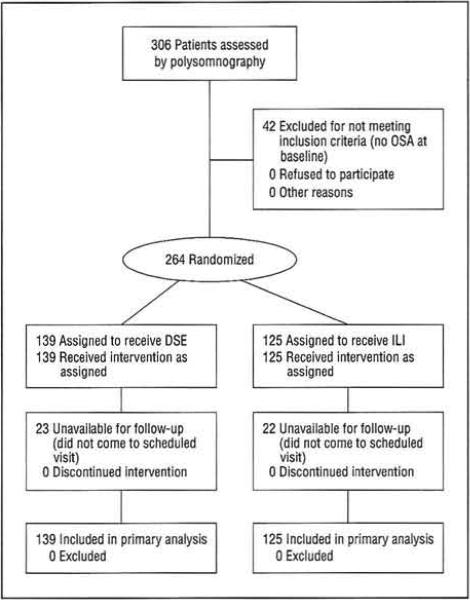
At the second Look AHEAD screening visit, a research assistant informed participants about the Sleep AHEAD study. Interested participants then consented to undergo a screening to assess eligibility. Each Sleep AHEAD site enrolled participants until the target level (approximately 75 per site for 300 across sites) was achieved. When those participants who were enrolled in Sleep AHEAD (N=306) were compared with those enrolled in Look AHEAD but not in Sleep AHEAD at the 4 Look AHEAD sites (N=1012), there were no differences between the groups in weight, BMI, sex, race/ethnicity, or waist circumference. Sleep AHEAD participants were slightly older (mean [SD], 61.3 [6.5] years vs 58.7 [6.9] years; P=.001) and had slightly lower hemoglobin A1c values (mean [SD], 7.2% [1.1%] vs 7.4% [1.2%]; P=.03) than did those Look AHEAD participants who were not enrolled in Sleep AHEAD.9 The 306 Sleep AHEAD participants were assessed by unattended overnight PSG, a sample that is described in detail elsewhere.9 Of the 306 patients assessed by PSG at baseline, 42 did not have OSA, leaving 264 participants for the current study (Figure 1).
Figure 1.
Participant flow diagram. DSE indicates diabetes support and education; ILI, intensive lifestyle intervention; and OSA, obstructive sleep apnea.
INTERVENTION
As part of the Look AHEAD study, eligible participants were randomly assigned to either diabetes support and education (DSE) or intensive lifestyle intervention (ILI) using a Web-based data management system that verified eligibility. Randomization was stratified by clinical center and blocked with random block sizes. Sleep technicians and the PSG scorer were blinded to participant randomization.
Intensive Lifestyle Intervention
The ILI participants received a group behavioral weight loss program developed specifically for obese patients with type 2 diabetes.12 Participants were prescribed portion-controlled diets that included using liquid meal replacements, frozen food entrees, and snack bars for the first 4 months (with reduced use from months 5-12). The prescribed energy intake was 1200 to 1500 kcal/d if the patients weighed less than 113.6 kg or 1500 to 1800 kcal/d if the patients weighed 113.6 kg or more, with 30% or less calories from fat. The physical activity prescription was 175 min/wk of moderate-intensity activity such as brisk walking.
Diabetes Support and Education
The DSE participants attended 3 group sessions over a 1-year period. These sessions focused on diet, physical activity, and social support as they related to effective diabetes management. The current prospective, randomized study design took advantage of the anticipated between-group differences in weight change over time to assess the effect of weight loss on OSA.
DEPENDENT MEASURES
Polysomnography
The primary dependent variable was AHI as assessed by PSG. An unattended overnight PSG was performed in the participant's home with a commercially available portable system (Compumedics PS-2; Compumedics Sleep, Abbotsville, Australia) using techniques similar to those developed for the Sleep Heart Health Study.14 The following signals were recorded: electroencephalogram (C3A2 and C4A1), bilateral electrooculogram, chin muscle activity, rib cage and abdominal excursion (piezoelectric crystal), and nasal airflow (nares pressure). Airflow was also assessed by oronasal thermistry. Snoring was monitored by putting the nasal pressure signal through a high-pass filter. Body position, electrocardiogram (lead 1), and oxygen saturation (by pulse oximetry) were also recorded. A team of 2 technologists went to the participant's home in the evening to apply the sensors. The participant was instructed to go to bed at his or her regular time, and the monitor was programmed to start recording 1 hour earlier. The technologists returned to the participant's home the following morning to remove the sensors and to retrieve the monitor.
All PSGs were scored manually15 (with the aid of computer software) by the same registered PSG technologist at a centralized reading laboratory at the University of Pennsylvania. Scoring of apnea required a decrease in the nasal pressure airflow signal to 10% or less of baseline for 10 seconds or more. Scoring obstructive apnea required the concomitant presence of respiratory-related chest wall movement, and scoring central apnea required the absence of chest wall movement. Mixed apneas were scored as obstructive apneas. Hypopnea was defined as 30% or more reduction from baseline in thoracoabdominal movement or airflow lasting 10 seconds or more with 4% or more oxygen desaturation.15 The absence of respiratory-related nasal pressure fluctuations for 10 seconds or more in the presence of fluctuations in the oronasal thermistor signal was scored as hypopnea. The AHI was the sum of the number of apneas and the number of hypopneas per hour. It was classified into mild (5.0-14.9), moderate (15.0-29.9), and severe (≥30.0 events per hour) OSA.
Intrascorer reliability was determined by having the masked scorer rescore 65 randomly chosen PSGs: 46 (baseline) and 19 (year 1). The reliability coefficient (correlation coefficient) for the AHI was 0.98 (95% confidence interval [CI], 0.97-0.99) at baseline and 0.98 (95% CI, 0.95-0.99) at year 1. The mean (SD) time between readings was 2.2 (1.3) years, and there was no evidence of drift over time. The change in the AHI between scores was not significantly different from 0 (-0.36 per year; P=.29).
Morphometrics
Weight, height, waist circumference,11 and neck circumference16 were assessed within 1 week of the PSG.
STATISTICAL ANALYSIS
Differences between participants who did and did not complete the 1-year PSG were tested using Wilcoxon rank sum tests for continuous variables and χ2 tests for categorical variables. Similar analyses were used to test for differences between the ILI and the DSE groups at baseline.
The primary analysis was a linear mixed-effects model, with time, treatment, and a time-by-treatment interaction as principal explanatory variables. This model posited an unrestricted structure on the variance-covariance matrix of the residuals on all 264 participants. Two additional sensitivity analyses were conducted. The first was a regression analysis conducted on the 219 participants who had both baseline and 1-year PSGs, which assessed the treatment's impact on changes in weight and AHI.17 The second was an analysis of covariance predicting year-1 values after controlling for baseline. Interaction terms were used to identify modifiers of the treatment effect on the AHI. Results from these 3 analyses were similar with respect to treatment effect (same direction and significance). The treatment effects obtained from the linear mixed-effects models are reported herein. The appropriate parametric or nonparametric partial bivariate correlations were used to identify predictors of change in the AHI after the treatment assignment was controlled for. All correlates were entered in multiple regressions to predict the change in the AHI after treatment assignment and sex were controlled for. All statistical analyses were conducted using SAS version 9.1.3 (SAS Institute Inc, Cary, North Carolina) and included research site as a fixed effect to account for any site effects.
The completion rate was comparable for the ILI and the DSE groups (103 of 125 participants [82.4%] vs 116 of 139 participants [83.5%], respectively; P=.82), and there were no significant differences at baseline between completers and noncompleters in any variable in Table 1, except in the AHI and the obstructive apnea index. Noncompleters had significantly lower baseline values for the AHI (18.4 [13.5] vs 24.2 [16.9]; P=.02) and the obstructive apnea index (8.3 [9.6] vs 13.6 [13.5]; P<.01) than did completers. The groups did not differ on baseline OSA category (ie, mild, moderate, or severe).
Table 1.
Participants’ Characteristics at Baselinea
| Variable | Allb (n=264) | Diabetes Support and Educationb (n=139) | Intensive Lifestyle Interventionb (n=125) | P Value |
|---|---|---|---|---|
| Age, y | 61.2 (6.5) | 61.3 (6.4) | 61.2 (6.6) | .94 |
| Female, % | 59.1 | 56.8 | 61.6 | .43 |
| Race/ethnicity, % | .99 | |||
| African American | 18.6 | 18.8 | 18.4 | |
| American Indian/Native American | 1.1 | 0.7 | 1.6 | |
| Asian/Pacific Islander | 1.9 | 2.2 | 1.6 | |
| Hispanic | 3.8 | 3.6 | 4.0 | |
| Other | 1.5 | 1.5 | 1.6 | |
| White | 73.0 | 73.2 | 72.8 | |
| BMI | 36.7 (5.7) | 36.5 (5.7) | 36.8 (5.8) | .43 |
| Weight, kg | 102.4 (18.3) | 102.0 (17.1) | 102.9 (19.6) | .67 |
| Height, cm | 167.1 (9.7) | 167.2 (9.8) | 166.9 (9.6) | .62 |
| Waist circumference, cm | 115.8 (13.2) | 115.7 (12.1) | 115.8 (14.4) | .81 |
| Neck circumference, cm | 41.3 (4.2) | 41.5 (4.1) | 41.1 (4.3) | .52 |
| Apnea-hypopnea index | 23.2 (16.5) | 23.5 (15.0) | 22.9 (18.0) | .26 |
| Obstructive apnea index | 12.7 (13.1) | 12.4 (11.8) | 13.0 (14.3) | .98 |
| Central apnea index | 0.4 (1.0) | 0.5 (1.1) | 0.4 (0.9) | .54 |
| Hypopnea index | 10.1 (8.2) | 10.6 (8.3) | 9.4 (7.9) | .05 |
| Oxygen desaturation index, ≥4% | 19.4 (14.9) | 20.2 (13.7) | 18.6 (16.1) | .06 |
| Fasting plasma glucose, mg/dL | 151.0 (41.5) | 152.9 (43.8) | 148.9 (38.8) | .39 |
| Hemoglobin A1c, % | 7.2 (1.0) | 7.3 (1.1) | 7.1 (0.9) | .06 |
| Self-reported No. of years with diabetes | 7.4 (7.1) | 7.5 (6.3) | 7.3 (7.9) | .19 |
Abbreviation: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared).
SI conversion factor: To convert glucose to millimoles per liter, multiply by 0.0555.
Differences between participants were tested using Wilcoxon rank sum tests for continuous variables and χ2 tests for categorical variables.
Values are expressed as mean (SD) unless otherwise indicated.
RESULTS
PARTICIPANTS
The baseline characteristics of the 264 study participants are listed in Table 1: 38.7% had mild OSA (AHI, 5.0-14.9), 35.2% had moderate OSA (AHI, 15.0-29.9), and 26.1% had severe OSA (AHI, ≥30). Only 5.0% of participants were receiving continuous positive airway pressure (CPAP) at the 1-year follow-up (6.4% DSE, 3.5% ILI; P=.31). The participants were asked to discontinue CPAP for 72 hours before their PSG assessment. No differences were observed when the analyses were run with and without these participants, so the results from the full sample (N=264) are reported herein. No effect for the research center was observed in any of our analyses.
WEIGHT
The ILI participants lost significantly more weight at 1 year (10.8 kg) than did DSE participants (0.6 kg) (b=-10.2; 95% CI=-12.1 to -8.4; P<.0001). They also experienced significantly greater reductions in waist and neck circumferences than did DSE participants (Table 2). Across conditions, men reduced their weight by 8.0 (11.4) kg and women by 3.7 (7.2) kg.
Table 2.
One-Year Changes by Treatment Group
| Variable | Adjusted Mean (SE) |
P Valuea | |
|---|---|---|---|
| Diabetes Support and Education (n=139) | Intensive Lifestyle Intervention (n=125) | ||
| BMI | –0.2 (0.3) | –3.8 (0.3) | <.001 |
| Weight, kg | –0.6 (0.7) | –10.8 (0.7) | <.001 |
| Waist circumference, cm | –0.5 (0.6) | –9.3 (0.7) | <.001 |
| Neck circumference, cm | 0.1 (0.2) | –1.2 (0.2) | <.001 |
| Hemoglobin A1c, % | –0.2 (0.1) | –0.7 (0.1) | <.001 |
| Apnea-hypopnea index | 4.2 (1.4) | –5.4 (1.5) | <.001 |
| Obstructive apnea index | 6.1 (1.4) | –2.5 (1.5) | <.001 |
| Central apnea index | –0.02 (0.2) | 0.02 (0.2) | .85 |
| Hypopnea index | –1.7 (0.7) | –2.9 (0.8) | .28 |
| Oxygen desaturation index, ≥4% | 1.2 (1.3) | –5.5 (1.4) | <.001 |
Abbreviation: BMI, body mass index (calculated as weight in kilograms divided by height in meters squared).
P values are for between-group differences based on linear mixed-effects models, with time, treatment, and a time-by-treatment interaction as principal explanatory variables and research site as a fixed effect.
APNEA-HYPOPNEA INDEX
Treatment Effects
The OSA among ILI participants improved, while it worsened among DSE participants. Among the ILI participants, the AHI decreased from 22.9 (18.0) to 18.3 (15.3) (P<.001 within group), while among the DSE participants, the AHI increased from 23.5 (15.0) to 28.3 (20.7) (P<.01 within group) (Figure 2). Relative to the DSE group, the ILI treatment was associated with an adjusted mean decrease in the AHI of 9.7 events per hour (95% CI, -13.6 to -5.7; P<.00l). Table 2 shows that the between-group differences in the AHI were the result of changes in obstructive apnea episodes (P<.001) rather than changes in hypopnea episodes (P=.24).
Figure 2.
Changes in weight and apnea-hypopnea index (AHI) over 1 year by treatment condition (diabetes support and education [DSE] and intensive lifestyle intervention [ILI]). Data are from all 264 participants. The between-group differences were significant for changes in weight (P<.001) and AHI (P<.001). Means are adjusted by research site. Error bars indicate 95% confidence intervals.
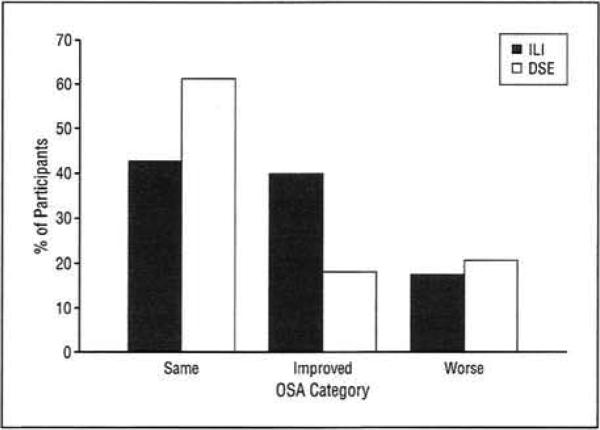
In addition to these significant mean differences in the AHI, weight loss resulted in clinically significant changes in OSA categories over 1 year. While there were no differences between the groups in the OSA category at baseline (P=.23), there were differences at 1 year (P =.002). Specifically, remission of OSA (AHI, <5 events per hour) at 1 year was 3 times more common in the ILI participants (13.6%) than in the DSE participants (3.5%) at 1 year. Also, the percentage of participants who had severe OSA at 1 year was more than twice as great in the DSE group (18.4%) than in the ILI group (37.9%) (Table 3). Similarly, more than twice as many ILI participants, compared with DSE participants, demonstrated improvement in their OSA category (eg, severe to moderate, moderate to mild, and mild to none) over 1 year (Figure 3).
Table 3.
Obstructive Sleep Apnea (OSA) Clinical Categories by Treatment Group at Baseline and 1 Yeara
| OSA at Baseline | No. (%) |
|||||||
|---|---|---|---|---|---|---|---|---|
| Intensive Lifestyle Intervention (n=103) |
Diabetes Support and Education (n=116) |
|||||||
| OSA at 1 Year |
OSA at 1 Year |
|||||||
| None | Mild | Moderate | Severe | None | Mild | Moderate | Severe | |
| Mild | 10 (23.3) | 23 (53.5) | 10 (23.3) | 0 | 2 (5.6) | 24 (66.7) | 7 (19.4) | 3 (8.3) |
| Moderate | 3 (9.4) | 11 (34.4) | 10 (31.3) | 8 (25.0) | 1 (2.2) | 11 (23.9) | 20 (43.5) | 14 (30.4) |
| Severe | 1 (3.6) | 6 (21.4) | 10 (35.7) | 11 (39.3) | 1 (2.9) | 1 (2.9) | 5 (14.7) | 27 (79.4) |
Clinical OSA categories: none (apnea-hypopnea index [AHI], <5), mild (AHI, 5.0-14.9), moderate (AHI, 15.0-29.9), and severe (AHI, ≥30).
Figure 3.
Percentage of participants in diabetes support and education (DSE) and intensive lifestyle intervention (ILI) whose obstructive sleep apnea (OSA) category improved (≥1 category change), worsened (≤1 category Change), or stayed the same (no change in category). Data are from the 219 participants who had baseline and 1-year data.
Treatment Interaction Effects
There were significant treatment interactions with both sex (P<.02) and baseline AHI (P<.001). Sex and baseline AHI were separate and independent modifiers of ILI such that the ILI was more effective in reducing the AHI in men than in women and more effective in participants with higher levels of baseline AHI than in those with lower levels of baseline AHI.
VARIABLES ASSOCIATED WITH CHANGE IN AHI
Baseline Variables
After the treatment assignment was controlled for, the only baseline variables significantly associated with changes in AHI over 1 year were AHI (r=-0.34, P<.001), waist circumference (r=-0.20, P<.01), and weight (r=-0.18, P<.01). There was a trend toward significance in hemoglobin A1c levels (r=0.12, P=.08). Neck circumference (P=.23) was not related to change in AHI. To examine whether these bivariate relationships were independently associated, we constructed a multivariable linear regression model to predict change in AHI and included these 5 variables as well as treatment assignment, research site, and sex. The only statistically significant multivariable predictor of change in AHI was baseline AHI (b=-0.30; 95% CI, -0.42 to -0.18; P<.001). Greater levels of AHI at baseline were associated with greater decreases in AHI over 1 year. Multicollinearity was not observed in any of the models (variance inflation factors were all ≤3.3).
Change Variables
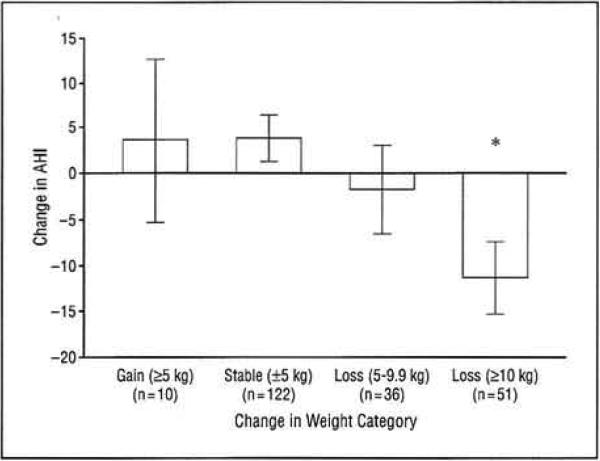
After treatment assignment was controlled for, changes in AHI were associated with changes in weight (r=0.35, P<.00l), waist circumference (r=0.30, P<.00l), and neck circumference (r=0.17, P=.01). Changes in hemoglobin A1c levels were not related to changes in AHI (P =.47). These variables were highly inter correlated (weight loss and change in neck circumference: r=0.42, P<.001; weight loss and change in waist circumference: r=0.68, P<.001; and change in neck circumference and change in waist circumference: r=0.36, P<.001). After these 4 variables were entered and after treatment assignment, research site, and sex were controlled for, change in weight circumference was the only statistically significant predictor of change in AHI (b=0.63; 95% CI, 0.21-1.04; P=.003). Greater weight loss was associated with greater reduction in AHI. Despite the large bivariate correlations, multicollinearity was not observed in any of the models (variance inflation factors were all ≤3.7). Independent of treatment category, participants who lost 10 kg or more had significantly greater changes in AHI than in all other weight change categories (Figure 4).
Figure 4.
Changes in apnea-hypopnea index (AHI) by category of weight change over 1 year. Data are from the 219 participants who had baseline and 1-year data. The asterisk indicates that, after multiple comparisons were controlled for, participants who lost 10 kg or more had significantly greater reductions in AHI than all other groups (P<.01 for all); error bars indicate 95% confidence intervals.
COMMENT
In this largest randomized controlled trial on the effects of weight loss on OSA, weight loss produced by an ILI Significantly improved OSA as measured by AHI. The intervention was most effective for men and for participants with higher baseline values of AHI. The observed reduction in AHI associated with weight loss was less than the results of uncontrolled studies of AHI after weight loss4 but similar to those of a recent controlled trial of mild apnea.5
These mean changes in AHI obscure important clinical changes that occurred with weight loss. It is notable that more than 3 times as many participants in the ILI group than in the DSE group had total remission of their OSA, and the prevalence of severe OSA among the ILI participants decreased to half that among the DSE participants. These decreases in the presence and/or the severity of OSA among obese patients who have type 2 diabetes are likely to confer significant benefit.18 There is emerging evidence that any reduction in AHI appears to be associated with a decrease in cardiovascular risk. A recent observational study revealed that men with untreated severe OSA (AHI, >30 events per hour) experienced a significantly greater incidence of fatal and nonfatal cardiovascular events compared with age- and BMI-matched healthy men.19 A prospective analysis from the Wisconsin Sleep Cohort found a dose-response association between the AHI at baseline and the presence of hypertension 4 years later that was independent of known confounding factors, including BMI.20 Also, an observational cohort study demonstrated that there was an association between increased severity of OSA and increased risk of stroke or death from any cause and that the association between AHI and these outcomes was independent of other cardiovascular and cerebrovascular risk factors, including hypertension.21 These latter findings are supported by the cross-sectional results of the Sleep Heart Health Study, showing that the risk of stroke increases progressively with increasing AHI.22 Collectively, these data suggest that the alleviation or mitigation of OSA severity associated with the weight reduction achieved by participants in our study will, if sustained, decrease exposure to the medical risks of OSA as well as reduce health care use and economic costs.23,24
The second principal finding of our study was that initial AHI and weight loss were the strongest predictors of change in AHI. Although statistically significant, the effect of each variable was modest. Each additional higher value of baseline AHI was associated with a 0.3 decrease in subsequent AHI, while each kilogram of weight loss was associated with a decrease in AHI of 0.6 events per hour. The subset of ILI participants who lost 10 kg or more experienced a reduction in AHI of 11.3 events per hour, a reduction that was significantly greater than all other weight change categories. Given the strong cross-sectional relationships among neck and waist circumference and AHI,25-27 it is somewhat surprising that changes in neck and waist circumference were not more related to changes in AHI. The absence of this association was likely because weight loss and reductions in neck and waist circumferences were highly correlated and because the changes in overall weight were reflected in changes in waist and neck circumference.
The third principal set of findings is cause for concern. The DSE group, which was weight stable (-0.6 kg) over 1 year, had a mean increase in AHI of 4 events per hour, a statistically significant difference. Therefore, the DSE participants had moderate OSA (AHI, 24) at baseline, but their OSA deteriorated to approach the severe category (AHI, 28) over 1 year, even with no weight gain. This finding suggests that untreated OSA in this age group has a relatively rapid natural progression, increasing 4 events per hour in just 1 year. A planned 4-year assessment of this cohort will ascertain whether this progression continues to worsen. It is also troubling that so few participants (ie, 5%) were receiving CPAP therapy at 1 year. The high prevalence of OSA in these obese adults with type 2 diabetes, the rapid progression of untreated OSA in this cohort, and the paucity of CPAP use 1 year after participants and their providers were informed of the diagnosis mean that this patient subset is at greater risk of the adverse consequences of OSA, such as hypertension,20 stroke,22 impaired quality of life,28 and mortality.29 This increased risk for adverse consequences of OSA is especially significant for these participants, who are already at greater risk for untoward consequences based on their obesity and type 2 diabetes.
This randomized controlled trial on the effects of weight loss on sleep apnea had several strengths compared with prior studies, including a larger sample of both men and women. Our study also followed up participants for a full year, longer than many previous studies. Our study has several important limitations. The results should not be generalized to younger patients, to patients without type 2 diabetes, or to patients with milder degrees of OSA. Similarly designed randomized controlled trials are needed to assess the effects of weight loss on OSA in these groups. Future studies should also explore the reasons for these improvements in OSA (eg, mechanical, metabolic, and hormonal).
In conclusion, weight loss produced through an ILI significantly improved OSA among obese participants with type 2 diabetes. The greatest benefit was observed in men, in participants with more severe OSA at baseline, and in participants who lost the most weight. The significant increase in AHI over 1 year in participants who were weight stable suggests that OSA is a rapidly progressing syndrome that will worsen without treatment in middle-aged obese adults with type 2 diabetes.
Funding/Support
Sleep AHEAD was supported by National Institutes of Health (NIH) National Heart, Lung and Blood Institute grant HL070301. Look AHEAD was supported by NIH National Institute of Diabetes and Digestive and Kidney Diseases grants DK57135, DK56992, and DK57002, and DK57178.
Footnotes
Financial Disclosure: Dr Sanders is a scientific consultant to Philips-Respironics, which manufactures and distributes devices used to monitor sleep and to diagnose and treat sleep-disordered breathing. He is also a co-inventor of BiPAP, which is manufactured by Philips-Respironics, with a financial interest in this brand and in related technologies by Philips-Respironics. He has been a speaker at sessions sponsored by Philips-Respironics and Cephalon and has been on advisory panels of Cephalon and Sanofi-Aventis.
REFERENCES
- 1.Veasey SC, Guilleminault C, Strohl KP, Sanders MH, Ballard RD, Magalang UJ. Medical therapy for obstructive sleep apnea: a review by the Medical Therapy for Obstructive Sleep Apnea Task Force of the Standards of Practice Committee of the American Academy of Sleep Medicine. Sleep. 2006;29(8):1036–1044. doi: 10.1093/sleep/29.8.1036. [DOI] [PubMed] [Google Scholar]
- 2.Morgenthaler TI, Kapen S, Lee-Chiong T, et al. Standards of Practice Committee. American Academy of Sleep Medicine Practice parameters for the medical therapy of obstructive sleep apnea. Sleep. 2006;29(8):1031–1035. [PubMed] [Google Scholar]
- 3.Strobel RJ, Rosen RC. Obesity and weight loss in obstructive sleep apnea: a critical review. Sleep. 1996;19(2):104–115. doi: 10.1093/sleep/19.2.104. [DOI] [PubMed] [Google Scholar]
- 4.Smith PL, Gold AR, Meyers DA, Haponik EF, Bleecker ER. Weight loss in mildly to moderately obese patients with obstructive sleep apnea. Ann Intern Med. 1985;103(6, pt 1):850–855. doi: 10.7326/0003-4819-103-6-850. [DOI] [PubMed] [Google Scholar]
- 5.Tuomilehto HPI, Seppä JM, Partinen MM, et al. Kuopio Sleep Apnea Group Lifestyle intervention with weight reduction: first-line treatment in mild obstructive sleep apnea. Am J Respir Crit Care Med. 2009;179(4):320–327. doi: 10.1164/rccm.200805-669OC. [DOI] [PubMed] [Google Scholar]
- 6.Newman AB, Foster G, Givelber R, Nieto FJ, Redline S, Young T. Progression and regression of sleep-disordered breathing with changes in weight. Arch Intern Med. 2005;165(20):2408–2413. doi: 10.1001/archinte.165.20.2408. [DOI] [PubMed] [Google Scholar]
- 7.Peppard PE, Young T, Palta M, Dempsey J, Skatrud J. Longitudinal study of moderate weight change and sleep disordered breathing. JAMA. 2000;284(23):3015–3021. doi: 10.1001/jama.284.23.3015. [DOI] [PubMed] [Google Scholar]
- 8.Pi Sunyer XF, Becker DM, Bouchard C, et al. Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: The Evidence Report. National Institutes of Health; Bethesda, MD: 1998. NIH publication 98-4083. [Google Scholar]
- 9.Foster GD, Sanders MH, Millman R, et al. Sleep AHEAD Research Group Obstructive sleep apnea among obese patients with type 2 diabetes. Diabetes Care. 2009;32(6):1017–1019. doi: 10.2337/dc08-1776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ryan DH, Espeland MA, Foster GD, et al. Look AHEAD Research Group Look AHEAD (Action for Health in Diabetes): design and methods for a clinical trial of weight loss for the prevention of cardiovascular disease in type 2 diabetes. Control Clin Trials. 2003;24(5):610–628. doi: 10.1016/s0197-2456(03)00064-3. [DOI] [PubMed] [Google Scholar]
- 11.Bray G, Gregg E, Haffner S, et al. Look AHEAD Research Group Baseline characteristics of the randomised cohort from the Look AHEAD (Action for Health in Diabetes) study. Diab Vasc Dis Res. 2006;3(3):202–215. doi: 10.3132/dvdr.2006.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Wadden TA, West DS, Delahanty L, et al. Look AHEAD Research Group The Look AHEAD study: a description of the lifestyle intervention and the evidence supporting it. Obesity (Silver Spring) 2006;14(5):737–752. doi: 10.1038/oby.2006.84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Pi-Sunyer X, Blackburn G, Brancati FL, et al. Look AHEAD Research Group Reduction in weight and cardiovascular disease risk factors in individuals with type 2 diabetes: one-year results of the Look AHEAD trial. Diabetes Care. 2007;30(6):1374–1383. doi: 10.2337/dc07-0048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Redline S, Sanders MH, Lind BK, et al. Sleep Heart Health Research Group Methods for obtaining and analyzing unattended polysomnography data for a multicenter study. Sleep. 1998;21(7):759–767. [PubMed] [Google Scholar]
- 15.American Academy of Sleep Medicine Task Force Sleep-related breathing disorders in adults: recommendations for syndrome definition and measurement techniques in clinical research. Sleep. 1999;22(5):667–689. [PubMed] [Google Scholar]
- 16.Calloway C, Chumlea W, Bouchard C. Circumferences. In: Lohmann TG, Roche AF, Martorell R, editors. Anthropometric Standardization Manual. Human Kinetics Publisher; Champaign, IL: 1988. pp. 39–64. [Google Scholar]
- 17.Lachin JM. Statistical considerations in the intent-to-treat principle. Control Clin Trials. 2000;21(3):167–189. doi: 10.1016/s0197-2456(00)00046-5. [DOI] [PubMed] [Google Scholar]
- 18.Young T, Peppard PR, Gottlieb DJ. Epidemiology of obstructive sleep apnea: a population health perspective. Am J Respir Crit Care Med. 2002;165(9):1217–1239. doi: 10.1164/rccm.2109080. [DOI] [PubMed] [Google Scholar]
- 19.Marin JM, Carrizo SJ, Vicente E, Agusti AG. Long-term cardiovascular outcomes in men with obstructive sleep apnoea-hypopnoea with or without treatment with continuous positive airway pressure: an observational study. Lancet. 2005;365(9464):1046–1053. doi: 10.1016/S0140-6736(05)71141-7. [DOI] [PubMed] [Google Scholar]
- 20.Peppard PE, Young T, Palta M, Skatrud J. Prospective study of the association between sleep-disordered breathing and hypertension. N Engl J Med. 2000;342(19):1378–1384. doi: 10.1056/NEJM200005113421901. [DOI] [PubMed] [Google Scholar]
- 21.Yaggi HK, Concato J, Kernan WN, Lichtman JH, Brass LM, Mohsenin V. Obstructive sleep apnea as a risk factor for stroke and death. N Engl J Med. 2005;353(19):2034–2041. doi: 10.1056/NEJMoa043104. [DOI] [PubMed] [Google Scholar]
- 22.Shahar E, Whitney CW, Redline S, et al. Sleep-disordered breathing and cardiovascular disease: cross-sectional results of the Sleep Heart Health Study. Am J Respir Crit Care Med. 2001;163(1):19–25. doi: 10.1164/ajrccm.163.1.2001008. [DOI] [PubMed] [Google Scholar]
- 23.Kapur V, Blough DK, Sandblom RE, et al. The medical cost of undiagnosed sleep apnea. Sleep. 1999;22(6):749–755. doi: 10.1093/sleep/22.6.749. [DOI] [PubMed] [Google Scholar]
- 24.Bahammam A, Delaive K, Ronald J, Manfreda J, Roos L, Kryger MH. Health care utilization in males with obstructive sleep apnea syndrome two years after diagnosis and treatment. Sleep. 1999;22(6):740–747. doi: 10.1093/sleep/22.6.740. [DOI] [PubMed] [Google Scholar]
- 25.Millman RP, Carlisle CC, McGarvey ST, Eveloff SE, Levinson PD. Body fat distribution and sleep apnea severity in women. Chest. 1995;107(2):362–366. doi: 10.1378/chest.107.2.362. [DOI] [PubMed] [Google Scholar]
- 26.Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S. The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med. 1993;328(17):1230–1235. doi: 10.1056/NEJM199304293281704. [DOI] [PubMed] [Google Scholar]
- 27.Grunstein R, Wilcox I, Yang TS, Gould Y, Hedner J. Snoring and sleep apnoea in men: association with central obesity and hypertension. Int J Obes Relat Metab Disord. 1993;17(9):533–540. [PubMed] [Google Scholar]
- 28.Gay P, Weaver T, Loube D, Iber C, Positive Airway Pressure Task Force. Standards of Practice Committee. American Academy of Sleep Medicine Evaluation of positive airway pressure treatment for sleep related breathing disorders in adults. Sleep. 2006;29(3):381–401. doi: 10.1093/sleep/29.3.381. [DOI] [PubMed] [Google Scholar]
- 29.Young T, Finn L, Peppard PE, et al. Sleep disordered breathing and mortality: eighteen-year follow-up of the Wisconsin Sleep Cohort. Sleep. 2008;31(8):1071–1078. [PMC free article] [PubMed] [Google Scholar]