Abstract
Objective
This study examined whether mindfulness increased through participation in movement based courses and whether changes in self-regulatory self-efficacy, mood, and perceived stress mediated the relationship between increased mindfulness and better sleep.
Participants
166 college students enrolled in the 2007-2008 academic year in 15 week classes in Pilates, Taiji quan, or GYROKINESIS®.
Methods
At beginning, middle, and end of the semester, participants completed measures of mindfulness, self-regulatory self-efficacy, mood, perceived stress and sleep quality.
Results
Total mindfulness scores and mindfulness subscales increased overall. Greater changes in mindfulness were directly related to better sleep quality at the end of the semester after adjusting for sleep disturbance at the beginning. Tired Mood, Negative Arousal, Relaxed Mood, and Perceived Stress mediated the effect of increased mindfulness on improved sleep.
Conclusions
Movement based courses can increase mindfulness. Increased mindfulness accounts for changes in mood and perceived stress that explain, in part, improved sleep quality.
Keywords: mindfulness, mood, Pilates, sleep, stress, Taiji quan, GYROKINESIS®
In college students, poor sleep quality has been associated with difficulties with mental and physical health. 1-3 Reported rates of sleep difficulties in college students have ranged from 31.6% to 64% depending on the measures used.3-6 Sleep disturbances can be caused by many different factors including biological, cognitive, and/or behavioral factors. While pharmaceuticals can provide some relief, behavioral interventions have no side effects and target the cognitive and behavioral aspects of sleep disorders.
One behavioral intervention often recommended as an important sleep aid is exercise. Epidemiologic studies have consistently shown an association between self-reports of exercise and better sleep.7 However, experimental studies have found none or only modest effects of exercise on sleep.8 An explanation for this lack of association is that the experimental studies assessed good sleepers who have little room for improvement. Individuals with sleep problems who then begin to exercise might be expected to see greater improvement in their sleep.9
Additional promising behavioral interventions for treating insomnia are those focusing on alleviating stress and reducing worry.9, 10 One such intervention is Mindfulness-Based Stress Reduction (MBSR), a formalized psychoeducational group intervention in which participants receive training in formal meditation techniques such as body-scan meditation, sitting meditation, walking meditation, and Hatha yoga with simple stretches and postures. Several research studies support the effectiveness of MBSR in reducing stress and anxiety in college students. 11-13 A recent review of the effects of MBSR on sleep disturbance found some evidence associating improved sleep with increased practice of mindfulness techniques.14
Mindfulness has been defined as “paying attention in a particular way: on purpose, in the present moment, and nonjudgmentally.”15(p4) Although mindfulness is often taught through meditation, very little research focuses on increasing mindfulness through participation solely in somatic modalities. One recent study of MBSR reported that the amount of time spent engaging in home practice of formal meditation exercises was related to the extent of improvement in mindfulness and measures of health. Of the types of formal meditation practice used in MBSR, yoga practice appeared to be associated with more changes in measures of mindfulness than the practice of body scanning or sitting meditation.16
In our study, we hypothesized that practice of Pilates, Taiji quan, or GYROKINESIS® would increase mindfulness. While very different in origin, these three somatic practices have much in common with meditative practices. The Pilates method is founded on principles of centering, concentration, control, precision, flow and breath in order to attain the ideal of a complete coordination of body, mind, and spirit.17-20 Taiji quan (also transliterated as tai chi chuan) is an ancient Chinese martial art characterized by slow circular movements, breath regulation, and focused attention.21 GYROKINESIS®, as developed by Juliu Horvath, embraces key principles of dance, yoga, gymnastics and taiji quan. The method works the entire body using spinal articulations and undulating rhythms integrated with specific breathing patterns. It is often described as a type of moving yoga.22
Although each of the approaches involved in the study promote mind-body awareness, the mindfulness aspects in the disciplines are often implied rather than explicitly stated as stress reduction goals. The purpose of this study was to investigate several questions: Does mindfulness increase over time through participation in Pilates, Taiji quan, and GYROKINESIS®? If so, does each particular training method increase mindfulness? Does increased mindfulness relate to improvements in sleep quality, self-regulatory self-efficacy, mood, and perceived stress? If observed increases in mindfulness are associated with improved sleep quality, do changes in self-regulatory self-efficacy, mood, and perceived stress mediate this relationship?
METHODS
Study Design
Participants for the study were recruited in the fall and spring semesters of the 2007-2008 academic year from 12 classes: 6 Pilates, 4 GYROKINESIS®, and 2 Taiji quan classes. All courses were academic electives or required courses that fulfilled Physical Activity/Wellness General Education requirements. The Pilates and GYROKINESIS® classes met twice a week for 75 minutes each class period or 3 times per week for 50 minutes each class period over a 15 week semester. Both participating instructors were comprehensively trained and certified in the same programs: GYROKINESIS® in Miami, FL and Classical Pilates in New York City. Chen style Taiji quan classes met twice a week for 50 minutes each session for 15 weeks following principles outlined by Yang.21 The two Taiji quan instructors had completed extensive training in Taiji quan (>15 years each). One was certified to teach by the St. Louis Chinese Internal Arts Center and one was certified to teach Evidence-Based Traditional Taiji by the Center for Taiji Studies™. Students completed a survey instrument in class at the beginning, mid-point and end of the semester. Study procedures were approved by the Institutional Review Board of the university prior to collection of data. All students who participated in the survey study provided informed consent.
Procedures
Mindfulness
The Five Facet Mindfulness Questionnaire (FFMQ) is a 39 item instrument that uses a 5 point Likert-type scale.23 Items were developed from a factor analytic study of five previously developed mindfulness questionnaires. The five factors representing elements of mindfulness are (1) observing or attending to sensations, perceptions, thoughts and feelings, (2) describing or labeling these internal experiences with words, (3) acting with awareness rather than on “automatic pilot, (4) nonjudging of inner experiences, and (5) nonreactivity to inner experience. A Total Mindfulness score was calculated by adding scores on each of the five scales. Higher scores indicate greater levels of mindfulness. For the present sample, Cronbach’s alpha for the five scales plus Total Mindfulness ranged from .79 to .93.
Sleep quality
The Pittsburgh Sleep Quality Index (PSQI) consists of 19 self-rated questions related to normal sleep habits.24 Scores range from 0-21, and the instrument has strong temporal stability (Pearson r=.85 over 28 days). Higher numbers on the PSQI indicate greater sleep disturbance, or poorer sleep quality. A PSQI global score > 5 has served as a marker to distinguish sleep disturbances in insomnia patients versus controls.25 For the present sample, the seven component scores of the PSQI had overall reliability coefficients (Cronbach’s alpha) of .69 at the beginning, and .76 at mid-point and end of the semester.
Self-efficacy
The Self-Regulatory Self-Efficacy Scale (SRE) is a four item, Likert format instrument designed to measure self-regulatory self-efficacy, (i.e motivating oneself to keep trying difficult tasks). Scores range from 4-28, and the measure has been found to be correlated with perceived performance and activity specific self-efficacy.26 Cronbach’s alpha reliability coefficients for the present sample were .73 at the beginning, .70 at the mid-point, and .80 at the end of the semester.
Mood
The Four Dimensional Mood Scale (FDMS) is based on a circumplex model of dispositional mood measuring Positive Energy, Tiredness, Negative Arousal, and Relaxation.27 This 20-item adjective checklist uses a five-point Likert format (1 = not at all, 5 = extremely), and scores on each scale are the mean response to items on the scale. Examples of adjectives used in the scales are (a) Lively and Vigorous for Positive Energy, (b) Exhausted and Weary for Tiredness, (c) Aggravated and Irritable for Negative Arousal, and (d) Calm and Peaceful for Relaxation. There is evidence for generally good internal consistency of the scales as well as concurrent and discriminant validity.28 For the present sample, Cronbach’s alpha for the four scales ranged from .74 to .88 across the semester.
Stress
The Perceived Stress Scale – 4 (PSS4) is a four item Likert format scale designed to measure the degree to which situations in one’s life are appraised as stressful.29 For the present sample, Cronbach’s alpha reliability coefficients were .81, .83, and .82 at the beginning, mid-point, and end of the semester. Elevated scores on the scale have been associated with self-reported physical illness.30 PSS4 measures are available only for courses from spring 2008.
Statistical Methods
Most analyses were conducted using the Statistical Packages for Social Sciences version 15 (SPSS Inc, Chicago, Ill, USA). Hierarchical linear regression models (HLMs), or mixed model analyses, were calculated to compare groups across time using a Toeplitz residual covariance structure. HLMs are appropriate for analyzing data with dependent observations (such as repeated responses from each individual subject). These analyses use an iterative process of calculating a residual covariance structure. Missing data points are estimated in this process, and the degrees of freedom for the F-statistics are also estimations. Power analysis with random effects is still a matter of ongoing research, so power estimates could not be reported with the HLMs.31 Path analysis models were conducted using the MPlus program version 3.11 (Muthén and Muthén, Los Angeles, CA, USA).
RESULTS
Demographics
A total of 166 students participated in the study (Pilates n=80, Taiji quan n=38, GYROKINESIS® n=48). Participants ranged in age from 18 to 41 (mean = 21.29, SD = 3.32) and reported a baseline exercise frequency from 1 to 20 hours of weekly exercise. A one-way ANOVA on possible differences between the groups in age and hours of weekly exercise was non-significant. A chi-square on possible differences in gender distribution by group was significant (χ2(2) = 40.90, p = .00): Pilates = 6 male and 74 female, Taiji quan = 18 male and 20 female, GYROKINESIS® = 1 male and 47 female.
Research Questions
Do levels of mindfulness increase among participants across courses?
A series of Mixed Model Analyses found statistically significant increases across time for total mindfulness scores on the FFMQ and each subscale (Table 1). Group effects were significant at the .05 level only for Nonreact. Using custom t-tests within the mixed model analysis, initial Taiji class scores on Nonreact were higher than Pilates (t=2.59, df = 255.29, p = .01) and GYROKINESIS® (t=3.13, df = 252.03, p = .00). Final Taiji class scores were also higher than final Pilates class scores on Nonreact (t = 2.04, df = 279.75, p = .04) and final GYROKINESIS® class scores (t = 3.48, df = 271.39, p = .00).
Table 1.
Mixed Model Analysis Fixed Effects of Five Facet Mindfulness Scores by Course across Beginning, Middle, and End of Semester
| Mindfulness Scale |
Group Effect F (df) significance |
Time Effect F (df) significance |
Group * Time Effect F (df) significance |
|---|---|---|---|
| Total Score | 1.36 (2, 166) .26 | 17.60 (2, 181) .00* | .74 (4, 181) .56 |
| Awareness | 2.78 (2, 165) .06 | 3.32 (2, 202) .04* | .69 (4, 204) .60 |
| Describe | .33 (2, 162) .72 | 2.95 (2, 185) .05* | .43 (4, 189) .78 |
| Nonjudge | 2.07 (2, 164) .13 | 10.33 (2, 197) .00* | .20 (4, 198) .94 |
| Nonreact | 6.66 (2, 165) .00* | 11.52 (2, 200) .00* | .57 (4, 203) .68 |
| Observe | 1.49 (2, 164) .23 | 12.54 (2, 186) .00* | 2.00 (4, 189) .10 |
p < .05
Does each course increase mindfulness?
Using custom t-test hypotheses of Time 1 minus Time 3 within a Mixed Model Analysis, significant increases were found in the Pilates group for overall mindfulness and all five scales of the FFMQ (Table 2). Significant increases in Total Mindfulness, Nonjudge, and Nonreact were found in both the Taiji quan group and the GYROKINESIS® group. The Taiji quan group also demonstrated an increase in Observe scores.
Table 2.
Custom Hypothesis T-Tests of Five Facet Mindfulness Scores Comparing Beginning to End of Semester by Course
| FFMQ Scale | Course | Time1 Mean, Std. Error |
Time 3 Mean, Std. Error |
Estimate of Change (Time1 Minus Time 3) |
Std. Error |
df | t | Sig. | 95% Confidence Interval Lower/Upper |
|
|---|---|---|---|---|---|---|---|---|---|---|
| Total Mindfulness |
Taiji quan | 131.28, 2.79 | 138.58, 2.90 | −7.30 | 2.70 | 202 | −2.71 | .01* | −12.61 | −1.99 |
| Pilates | 129.68, 1.89 | 138.99, 1.96 | −9.31 | 1.77 | 187 | −5.24 | .00* | −12.81 | −5.81 | |
| GYROKINESIS ® |
127.78, 2.43 | 132.37, 2.48 | −4.59 | 2.22 | 178 | −2.06 | .04* | −8.98 | −.20 | |
| Awareness | Taiji quan | 25.18, .84 | 26.34, .87 | −1.16 | .84 | 183 | −1.38 | .17 | −2.81 | .49 |
| Pilates | 25.48, .56 | 26.76, .59 | −1.28 | .55 | 168 | −2.35 | .02* | −2.37 | −.20 | |
| GYROKINESIS ® |
24.32, .72 | 24.66, .74 | −.34 | .68 | 160 | −.49 | .62 | −1.68 | 1.01 | |
| Describe | Taiji quan | 28.62, .90 | 29.25, .93 | −.63 | .74 | 152 | −.85 | .40 | −2.09 | .83 |
| Pilates | 38.53, .61 | 29.73, .63 | −1.20 | .48 | 138 | −2.50 | .01* | −2.15 | −.25 | |
| GYROKINESIS ® |
27.96, .78 | 28.52, .80 | −.56 | .60 | 132 | −.94 | .35 | −1.74 | .62 | |
| Nonjudge | Taiji quan | 26.17, 1.05 | 28.56, 1.10 | −2.39 | 1.08 | 194 | −2.21 | .03* | −4.53 | −.26 |
| Pilates | 28.26, .71 | 30.33, .74 | −2.07 | .71 | 178 | −2.92 | .00* | −3.47 | −.67 | |
| GYROKINESIS ® |
26.42, .91 | 28.40, .93 | −1.97 | .88 | 170 | −2.23 | .03* | −3.72 | −.22 | |
| Nonreact | Taiji quan | 22.60, .68 | 24.08, .71 | −1.48 | .65 | 178 | −2.25 | .03* | −2.77 | −.18 |
| Pilates | 20.47, .46 | 22.33, .48 | −1.86 | .43 | 163 | −4.36 | .00* | −2.71 | −1.02 | |
| GYROKINESIS ® |
19.78, .59 | 20.84, .60 | −1.06 | .53 | 155 | −1.99 | .05* | −2.11 | .−01 | |
| Observe | Taiji quan | 28.71, .84 | 30.50, .87 | −1.79 | .74 | 153 | −2.40 | .02* | −3.26 | −.32 |
| Pilates | 27.01, .57 | 29.79, .59 | −2.77 | .48 | 139 | −5.71 | .00* | −3.73 | −1.81 | |
| GYROKINESIS ® |
29.34, .73 | 30.11, .75 | −.77 | .60 | 133 | −1.28 | .20 | −1.97 | .42 | |
p<.05
Does increased mindfulness relate to improvements in sleep quality, self-regulatory self-efficacy, mood, and perceived stress?
Although differences between mean PSQI scores from the beginning to the end of the semester were not statistically significant, the number of students scoring in the insomnia range decreased from 72 (55% of 131) to 63 (48.1% of 131) (χ2=13.30, df=1, p=.00). Negative Arousal was also lower at the end of the semester (mean = 1.79, SD = .62) than the beginning (mean = 1.95, SD = .65) (paired t-test, df=132, t = 3.23, p=.00). In addition, Relaxation was greater at the end of the semester (mean = 3.16, SD =.75) than the beginning (mean = 3.02, SD = .74) (paired t-test, df=132, t = −2.60, p = .01). Measures of Positive Energy, Tiredness, Self-Regulatory Efficacy and Perceived Stress did not demonstrate statistically significant changes.
Partial correlations were calculated for change scores on the FFMS and the well-being variables controlling for their beginning levels (Table 3). With the exception of the Describe scores, increases in mindfulness sub-scales were associated with improved sleep quality, greater Positive Energy, lower levels of Negative Arousal, greater relaxation, greater self-regulatory efficacy, and reduced perception of stress. Only the Nonreact subscale was associated with levels of Tiredness controlling for beginning of the semester levels of Tiredness.
Table 3.
Partial Correlations of Change Scores on Five Facet Mindfulness Scales with Well-Being Variables
| End of Semester Valuesa |
Δ Observe | Δ Describe | Δ Aware | Δ Nonjudge | Δ Nonreact | Δ Total Mindfulness |
|---|---|---|---|---|---|---|
| PSQIa,b df=127 |
−.31* (p=.00) |
−.07 (p=.40) |
−.31* (p=.00) |
−.29* (p=.00) |
−.32* (p=.00) |
−.38* (p=.00) |
| Positive Energya df=127 |
.38* (p=.00) |
.17 (p=.06) |
.30* (p=.00) |
.21 (p=.02) |
.30* (p=.00) |
.38* (p=.00) |
| Tirednessa df=127 |
−.15 (p=.09) |
−.04 (p=.67) |
−.17 (p=.06) |
−.12 (p=.16) |
−.24* (p=.01) |
−.20* (p=.02) |
| Negative Arousala df=127 |
−.14 (p=.12) |
−.18* (p=.05) |
−.22* (p=.01) |
−.23* (p=.01) |
−.30* (p=.00) |
−.31* (p=.00) |
| Relaxationa df=127 |
.37* (p=.00) |
.27* (p=.00) |
.25* (p=.00) |
.17* (p=.05) |
.32* (p=.00) |
.38* (p=.00) |
| SREac df=127 |
.34* (p=.00) |
.14 (p=.13) |
.35* (p=.00) |
.20* (p=.03) |
.12 (p=.17) |
.33* (p=.00) |
| PSS4a,d df=63 |
−.26* (p=.04) |
−.21 (p=.09) |
−.38* (p=.00) |
−.34* (p=.01) |
−.42* (p=.00) |
−.49* (p=.00) |
controlling for beginning of the semester values for each well-being variable
Pittsburgh Sleep Quality Index
Self-Regulatory Self-Efficacy Scale
Perceived Stress Scale–4
p<.05.
Do changes in self-regulatory self-efficacy, mood, and perceived stress mediate the effect of mindfulness on sleep quality?
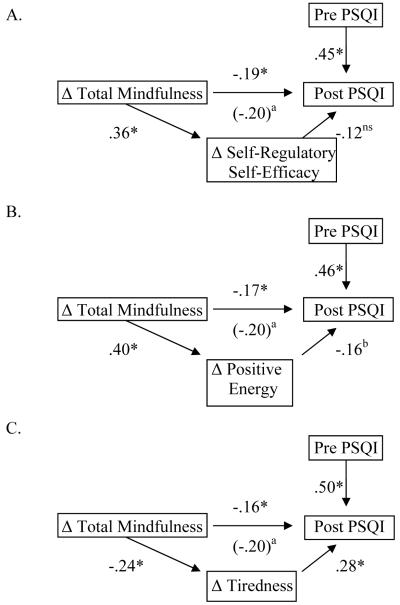
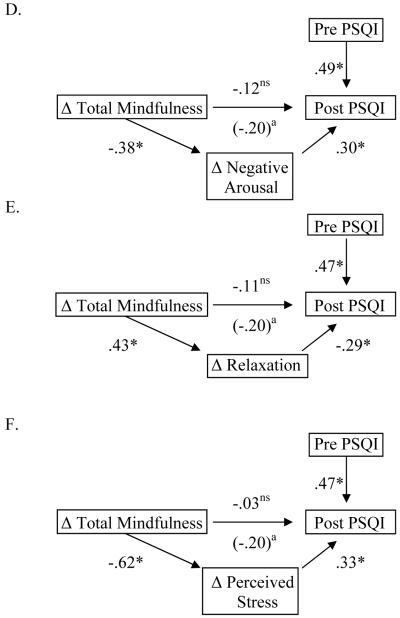
Because the findings confirmed that increased mindfulness was associated with improvements in sleep quality, as predicted, we tested the hypothesis that changes in mood, self-regulatory self-efficacy and perceived stress mediated this relationship. Six mediation models were conducted (Figure 1). We used the following conditions proposed by Baron and Kenny32 to show support for a mediational hypothesis: (1) the independent variable (Total Mindfulness), dependent variable (Sleep Quality), and mediator (mood, self-regulatory self-efficacy or perceived stress) all must be significantly inter-correlated; (2) when the independent variable (IV) and mediator are entered simultaneously into a model predicting the dependent variable (DV), the relationships between the IV and DV must become non-significant, or must be significantly reduced. We used Mplus to test the statistical significance of each mediation pathway, operationalized as the indirect effect of change in total mindfulness on improved sleep quality as a function of the mediating variable.
Figure 1.
Changes in Self-Regulatory Self-Efficacy, Mood, and Perceived Stress as Mediators of the Relationship between Change in Mindfulness and Improved Sleep Quality
Notes: Numbers are standardized regression coefficients (ßs) from multivariable path models run using structural equation modeling (SEM). Post PSQI represents residualized change in sleep quality at the end of the semester, adjusting for sleep quality at the beginning of the semester. aStandardized coefficient (ß) for the univariate regression of end-of-semester sleep quality on change in total mindfulness score, bp<.10, *p<= .05, nsp>.10 (non-significant).
The first mediation analysis (Fig. 1A) found that although greater change in mindfulness was associated with greater change in self-regulatory self-efficacy, change in self-regulatory efficacy was not significantly related to improved sleep quality. Therefore, change in self-regulatory self-efficacy did not mediate the significant association between increased mindfulness and better sleep quality at the end of the semester (ß for indirect effect =−.04, p=.15).
As shown in Figure 1B, the second analysis found that increased Positive Energy tended to partially mediate the relationship between change in total mindfulness and less sleep disturbance at the end of the semester (ß for indirect effect =−.07, p=.06). The third analysis (Fig. 1C) found a significant mediational effect, in which greater changes in mindfulness were associated with greater reduction in tiredness that in turn predicted better quality sleep (ß for indirect effect =−.07, p<.05). As shown in Figure 1C, the direct effect of change in total mindfulness on end-of-semester sleep quality was somewhat reduced but remained statistically significant in the model (ß =−.16, p<.05), consistent with partial mediation. The fourth analysis (Fig. 1D) found that increases in mindfulness were associated with a reduction in Negative Arousal, which in turn was associated with a reduction in sleep disturbance. Because the indirect effect of change in total mindfulness on end-of-semester sleep quality as a function of reduced Negative Arousal was statistically significant (ß for indirect effect =−.11, p<.05) and the direct effect became non-significant (ß =−.12, p=.12), this model was consistent with mediation. The fifth analysis (Fig. 1E) found that greater mindfulness was associated with improvement in relaxed mood, and this in turn was associated with less disturbed sleep (ß for indirect effect =−.13, p<.05). The sixth analysis (Fig. 1F) found that greater mindfulness was associated with reduction in perceived stress, and this in turn was associated with improved sleep quality (ß for indirect effect =−.21, p<.05). In summary, changes in Tiredness, Negative Arousal, Relaxation and Perceived Stress were all significant mediators of the effect of increased mindfulness on improved sleep quality at the end of the semester.
Comment
In summary, over the course of a fifteen week semester, students who participated in Pilates, Taiji quan or GYROKINESIS® classes demonstrated increases in overall mindfulness, which could confer important physical and mental health benefits.33 Significant changes in specific facets of mindfulness, such as acting with awareness and observing sensations, perceptions, thoughts and feelings, varied by class, but each class did show increases in multiple aspects of mindfulness. Increases in mindfulness were associated with improved sleep, self-regulatory self-efficacy, mood, and perception of stress. In addition, the effect of increases in mindfulness on sleep quality was mediated through four variables: Tiredness, Negative Arousal, Relaxation and Perceived Stress. To our knowledge, these findings are the first to demonstrate that movement based classes can cultivate attributes of mindful awareness. Moreover, the results suggest that increased mindfulness during the course of a college semester has important mental and behavioral health implications, for mood and sleep quality specifically.
Previous studies have found that participation in meditation based programs increases college students’ scores on mindfulness.13, 34 To our knowledge, the present study is the first to demonstrate the feasibility of developing mindfulness through movements based courses. Our findings support a similar observation by other investigators in which meditative movement (yoga) practice during an 8-week MBSR program was associated with significant increases in multiple facets of mindfulness.16 While other studies have investigated the effects of MBSR on sleep disturbance14, no other studies have investigated the development of mindfulness on the sleep quality of college students. Although not a specific focus of this study, poor sleep quality has been associated with difficulties in academic performance. 4, 35-37 One possible benefit of increasing mindfulness and improving sleep quality could be improved academic performance. The identified mediation of the effect of mindfulness on sleep quality through mood and perceived stress provides an additional step towards describing a theory of the mechanism of mindfulness as suggested by previous researchers.38
The limitations of this study are several. Because it is observational, the theoretical direction of the effect of mindfulness on sleep is based on correlational analyses. It may be that it is easier for students to be mindful when they are sleeping better and other factors account for improvements in sleep quality at the end of the semester. The development of mindfulness may also be part of a normal developmental process in college students,38 so future studies are recommended with an exercise control group that is not intentionally engaged in mindful movement.
Variations in the facets of mindfulness developed in the Pilates, Taiji quan, or GYROKINESIS® classes could be explained in several ways. Different classes use different vocabulary and focus on different aspects of mindfulness. For example, Pilates classes use the vocabulary of centering, concentration, control, precision, flow, and breath to create awareness and make mind-body connections.20 In the Taiji quan classes, through the practice of wuji zhuang (standing meditation) there is a focus on relaxing the body in proper alignment, sinking the qi to the dantian.21 In GYROKINESIS® participants are encouraged to focus on sensation, relaxation, fluidity and self-acceptance. These differences in focus could have an effect on how students develop specific facets of mindfulness. In addition to focus and vocabulary differences, class length and the amount of practice time students engage in outside of class also could account for observed differences in mindfulness. Previous research on mindfulness training found that greater home practice was associated with greater increases in measures of well-being.16, 34
In conclusion, high stress levels and feelings of psychological distress are widespread in college students.37 While numerous clinical interventions based on developing mindfulness can effectively reduce stress, anxiety, depression, and disordered eating39, some students who are reticent to seek clinical interventions through counseling services may show an interest in movement based courses as a way to develop mindfulness and to manage stress. This study provides encouraging preliminary data to suggest that (a) a variety of movement courses can effectively increase mindfulness, and (b) increased mindfulness during the semester is associated with significant improvements in mood and perceived stress that, in turn, explains better sleep quality at semester’s end. Instructors of general education courses in health, stress management, as well as physical activity or dance courses are encouraged to include mindfulness training as part of their curriculum.
Acknowledgments
GYROKINESIS is a registered trademark of Gyrotonic Sales Corp and is used with their permission. Use of the trade name is for information only and does not imply endorsement by GYROKINESIS®. The authors have no commercial, proprietary, or financial interest (as consultant, reviewer or evaluator) for GYROKINESIS®.
Footnotes
This paper was supported by grant K99 AT004945 from the National Center for Complementary & Alternative Medicine (NCCAM) to JG. Its contents are solely the responsibility of the authors and do not necessarily represent the official views of the National Institutes of Health (NIH).
Contributor Information
Dr. Karen Caldwell, Appalachian State University, Human Dev. & Psych. Counseling, E. Duncan Hall, Boone, 28608 United States.
Dr. Mandy Harrison, Appalachian State University, Health Leisure and Exercise Science, Boone, United States, harrisonmb@appstate.edu
Ms. Marianne Adams, Appalachian State University, Theatre & Dance, Boone, United States, adamsm@appstate.edu
Mrs. Rebecca H Quin, Appalachian State University, Theatre & Dance, Boone, United States, hower@appstate.edu
Dr. Jeffrey Greeson, Duke University Medical Center, Duke Integrative Medicine, Durham, United States, jeffrey.greeson@duke.edu
References
- 1.Pilcher JJ, Ott ES. The relationships between sleep and measures of health and well-being in college students. a repeated measures approach. Behav Med. 1998;23(4):170–178. doi: 10.1080/08964289809596373. [DOI] [PubMed] [Google Scholar]
- 2.Pilcher JJ, Ginter DR, Sadowsky B. Sleep quality versus sleep quantity: relationships between sleep and measures of health, well-being and sleepiness in college students. J of Psychosom Res. 1997;42(6):583–596. doi: 10.1016/s0022-3999(97)00004-4. [DOI] [PubMed] [Google Scholar]
- 3.Moo-Estrella J, Perez-Benitez H, Solis-Rodriguez F, Arandowsky-Sandoval G. Evaluation of depressive symptoms and sleep alterations in college students. Arch Med Res. 2005;36(4):393–398. doi: 10.1016/j.arcmed.2005.03.018. [DOI] [PubMed] [Google Scholar]
- 4.Medeiros ALD, Mendes DBF, Lima PF, Araujo JF. The relationships between sleep-wake cycle and academic performance in medical students. Biological Rhythm Research. 2001;32(2):263–270. [Google Scholar]
- 5.Coren S. The prevalence of self-reported sleep disturbances in young adults. I J Neurosci. 1994;79(1&2):67–73. doi: 10.3109/00207459408986068. [DOI] [PubMed] [Google Scholar]
- 6.Yang CM, Wu CH, Hsieh MH, Liu MH, Lu FH. Coping with sleep disturbances among young adults: a survey of first-year college students in Taiwan. Behav Med. 2003;29(3):133–138. doi: 10.1080/08964280309596066. [DOI] [PubMed] [Google Scholar]
- 7.Hublin C, Kaprio J, Partinen M, Koskenvuo M. Insufficient sleep – a population-based study in adults. Sleep. 2001;24:392–400. doi: 10.1093/sleep/24.4.392. [DOI] [PubMed] [Google Scholar]
- 8.Youngstedt SD, Kline CE. Epidemiology of exercise and sleep. Sleep and Biological Rhythms. 2006;4:215–221. doi: 10.1111/j.1479-8425.2006.00235.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Morin CM, Rodrigue S, Ivers H. Role of stress, arousal, and coping skills in primary insomnia. Psychosom Med. 2003;65:259–267. doi: 10.1097/01.psy.0000030391.09558.a3. [DOI] [PubMed] [Google Scholar]
- 10.Morin CM. Cognitive-behavioral approaches to the treatment of insomnia. J Clin Psychiatry. 2004;65(suppl 16):33–40. [PubMed] [Google Scholar]
- 11.Astin JA. Stress reduction through mindfulness meditation: effects on psychological symptomatology, sense of control, and spiritual experiences. Psychother Psychosom. 1997;66:97–106. doi: 10.1159/000289116. [DOI] [PubMed] [Google Scholar]
- 12.Shapiro SL, Schwartz GE, Bonner G. Effects of mindfulness-based stress reduction on medical and premedical students. J Behav Med. 1998;21:581–599. doi: 10.1023/a:1018700829825. [DOI] [PubMed] [Google Scholar]
- 13.Oman D, Shapiro SL, Thoresen CE, Plante TG, Flinders T. Meditation lowers stress and supports forgiveness among college students: a randomized controlled trial. J Am Coll Health. 2008;56(5):569–578. doi: 10.3200/JACH.56.5.569-578. [DOI] [PubMed] [Google Scholar]
- 14.Winbush NY, Gross CR, Kreitzer MJ. The effects of mindfulness-based stress reduction on sleep disturbance: a systematic review. Explore. 2007;3(6):585–591. doi: 10.1016/j.explore.2007.08.003. [DOI] [PubMed] [Google Scholar]
- 15.Kabat-Zinn J. Wherever You Go, There You Are: Mindfulness Meditation in Everyday Life. Hyperion; New York: 1994. [Google Scholar]
- 16.Carmody J, Baer RA. Relationships between mindfulness practice and levels of mindfulness, medical and psychological symptoms and well being in a mindfulness-based stress reduction program. J Behav Med. 2008;31:23–33. doi: 10.1007/s10865-007-9130-7. [DOI] [PubMed] [Google Scholar]
- 17.Gallagher S, Kryzanowska R, Speleotis S. The Pilates Method of Body Conditioning. BainBridge Books; Philadelphia: 1999. [Google Scholar]
- 18.Pilates JH, Gallagher S, Kryzanowska R. The Complete Writings of Joseph H. Pilates: Your Health and Return to Life through Contrology. BainBridge Books; Philadelphia: 2000. [Google Scholar]
- 19.Adamany K, Loigerot D. The Pilates Edge: An Athlete’s Guide to Strength and Performance. Avery/Penguin Books; New York: 2004. [Google Scholar]
- 20.Adams M, Quin R. The Pilates Teacher Training Manual. Appalachian State University; Boone, NC: 2007. [Google Scholar]
- 21.Yang Y. Taijiquan: The Art of Nurturing, The Science of Power. Zhenwu Publications; Champaign, IL: 2005. [Google Scholar]
- 22.Gyrotonic Sales Corp. [Accessed January 8, 2009];GYROKINESIS® Methodology. Available at: http://www.gyrotonic.com/Gyrokinesis.asp.
- 23.Baer RA, Smith GT, Hopkins J, Krietemeyer J, Toney L. Using self-report assessment methods to explore facets of mindfulness. Assessment. 2006;13(1):27–45. doi: 10.1177/1073191105283504. [DOI] [PubMed] [Google Scholar]
- 24.Buysse DJ, Reynolds CF, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. 1989;28(2):193–213. doi: 10.1016/0165-1781(89)90047-4. [DOI] [PubMed] [Google Scholar]
- 25.Backhaus J, Junghanns K, Broocks A, Riemann D, Hohagen F. Test-retest reliability and validity of the Pittsburgh Sleep Quality Index in primary insomnia. J Psychosom Res. 2002;53:737–740. doi: 10.1016/s0022-3999(02)00330-6. [DOI] [PubMed] [Google Scholar]
- 26.Harrison MB, McGuire FA. An investigation of the influence of vicarious experience on perceived self-efficacy. American Journal of Recreation Therapy. 2008;7(1):10–16. [Google Scholar]
- 27.Huelsman TJ, Nemanick RC, Munz DC. Scales to measure four dimensions of dispositional mood: positive energy, tiredness, negative activation, and relaxation. Educational and Psychological Measurement. 1998;58(5):804–819. [Google Scholar]
- 28.Huelsman TJ, Furr RM, Nemanick RC. Measurement of dispositional affect: Construct validity and convergence with a circumplex model of affect. Educational and Psychological Measurement. 2003;63(4):655–673. [Google Scholar]
- 29.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav. 1983;24:385–396. [PubMed] [Google Scholar]
- 30.Cohen S, Williamson G. In: Spacapan S, Oskamp S, editors. Perceived stress in a probability sample of the United States; The Social Psychology of Health: Claremont Symposium on Applied Social Psychology; Newbury Park, CA: Sage. 1988.pp. 31–67. [Google Scholar]
- 31.Castelloe JM. Sample size computations and power analysis with the SAS system. SAS Institute Inc.; Cary, NC: 2007. Paper 265-25. [Google Scholar]
- 32.Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. J Pers Soc Psychol. 1986;51(6):1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- 33.Greeson JM. Mindfulness research update: 2008. Compl Health Prac Rev. 2009 doi: 10.1177/1533210108329862. Prepublished January 13, 2009, doi:10.1177/1533210108329862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shapiro SL, Oman D, Thoresen CE, Plante TG, Flinders T. Cultivating mindfulness: effects on well-being. J Clin Psychol. 2008;64(7):840–862. doi: 10.1002/jclp.20491. [DOI] [PubMed] [Google Scholar]
- 35.Wolfson AR, Carskadon MA. Understanding adolescents’ sleep patterns and school performance: a critical appraisal. Sleep Med Rev. 2003;7(6):491–506. doi: 10.1016/s1087-0792(03)90003-7. [DOI] [PubMed] [Google Scholar]
- 36.Curcio G, Ferrara M, Gennaro LD. Sleep loss, learning capacity and academic performance. Sleep Med Rev. 2006;10:323–337. doi: 10.1016/j.smrv.2005.11.001. [DOI] [PubMed] [Google Scholar]
- 37.American College Health Association American College Health Association - National College Health Assessment (ACHA – NCHA) spring 2008 reference group data report (abridged) J Am Coll Health. 2009;57:477–488. doi: 10.3200/JACH.57.5.477-488. [DOI] [PubMed] [Google Scholar]
- 38.Shapiro SL, Carlson LE, Astin JA, Freedman B. Mechanisms of mindfulness. J Clin Psychol. 2006;62(3):373–386. doi: 10.1002/jclp.20237. [DOI] [PubMed] [Google Scholar]
- 39.Baer RA. Mindfulness training as a clinical intervention: a conceptual and empirical review. Clin Psychol Sci Prac. 2003;10:125–143. [Google Scholar]