Abstract
Comorbid psychopathology is a variable not explored in the acupuncture RCTs that could explain whether subgroups of patients with chronic low back pain have differential responses to acupuncture or placebo treatments. This was a controlled, blinded, crossover trial of verum acupuncture and validated sham acupuncture in 40 CLBP patients, with a Low or High level of psychiatric comorbidity. They completed a 0–10 rating scale for pain at the beginning and end of each treatment session, and rated their expectations for change in pain. Verum acupuncture was performed at Large Intestine 4 on the dorsal right hand for 30 minutes by a licensed acupuncturist. Data analysis used percent improvement in pain as the primary outcome for each of the treatment sessions. Both groups (21 Low and 19 High) reported significant analgesia with verum acupuncture needling, mean 33%, p=.90 for difference between groups; and with placebo, 26%, p=.09. In both groups expectations were only a significant predictor of verum acupuncture response, p=.002, such that those with greater expectations had greater pain relief. Psychiatric comorbidity does not significantly impact acupuncture or placebo acupuncture analgesia in CLBP. It does not affect the positive impact of expectations on reported pain relief from real acupuncture.
Keywords: Psychiatric Comorbidity, Acupuncture, Chronic Low Back Pain, Placebo Controlled, Expectations
Introduction
In general, controlled trials of acupuncture for chronic low back pain (CLBP) have been contradictory or inconclusive,8, 21, 25, 44 in terms of demonstrating that patients benefit from acupuncture treatment (also termed verum treatment) beyond placebo effects. This assumes that the measure of acupuncture efficacy is a significant positive difference in verum vs. sham treatment analgesia. One potential confounder is that the high placebo response in these trials makes detection of verum-placebo differences difficult. Placebo effects can refer to all of the nonspecific or psychological benefits of a somatic treatment. In CLBP the relationships between pain perception and psychological state are quite important,1, 34 and consequently the psychological benefits of a treatment may be significant components of any therapeutic response.12, 50
Similarly, to understand the underpinnings of the positive responses to verum and placebo acupuncture, it has been important to dissect the mechanisms of placebo and predictors of placebo response.40 While factors such as expectations for relief are important,27, 33 many other aspects of the placebo phenomena remain unexplored, such as it is unknown at what point in the acupuncture treatment course of low back pain the placebo response begins. In addition, high levels of psychopathology in patients with chronic low back pain are associated with diminished effectiveness of opioids and facet blocks,57, 59 and enhanced placebo responses,60 but it is unknown if this holds true for acupuncture response. Moreover, given that psychological symptoms are so prevalent in CLBP and are important predictors of treatment response,51 it is unknown how these symptoms interact with the level of expectations for improvement with acupuncture in predicting responses to verum or placebo treatment. In other words, does the impact of expectations on the benefit from acupuncture or sham acupuncture depend on the level of psychopathology in the patient?
Comorbid psychopathology affects approximately 20 to 30% of those with CLBP in community samples and 50% of those seeking treatment for this condition in primary care practices.14, 53, 54 The vast majority of this comorbidity are disorders of high negative affect, such as depression and anxiety disorders, and personality pathology.6, 11 The high prevalence of psychiatric comorbidity underscores the need to understand whether it impacts the effectiveness of acupuncture treatment or modulates the placebo response.
The aim of this study was to investigate the response to acupuncture needling in subgroups of patients with chronic low back pain. Since, as noted, chronic low back pain patients with a high degree of psychopathology tend to have poorer responses to treatment and greater placebo responses than CLBP patients with a low level of psychopathology, we tested the following hypotheses: 1) CLBP patients with a high degree of psychopathology will have less of an analgesic response to verum acupuncture needling than CLBP patients with low levels of psychopathology; and 2) CLBP patients with high psychopathology will have greater placebo analgesia than those with low psychopathology. We also hypothesized that in both groups the level of expectations for relief would predict the magnitude of analgesic responses—the greater the level of expectations, the greater the level of analgesia for either verum or placebo treatment
Materials and Methods
Design and setting
This was a single-blinded, placebo-controlled, randomized, crossover trial of acupuncture needling and placebo acupuncture in patients with chronic low back pain. There were three total visits, with verum and placebo acupuncture randomly crossed over in visits 2 and 3. Subjects were recruited from the pain management and arthritis clinics of an urban teaching hospital, through an email announcement distributed to employees of the hospital, and a hospital-kept database of research volunteers. Subjects were enrolled after IRB approval from Brigham and Women’s Hospital and obtaining written, informed consent.
Inclusion criteria
Subjects were included if they were: 1) between the ages of 21–65, 2) averaged at least 4 on a 0–10 scale of pain intensity, 3) had no back surgery within the past year, 4) were not having pain management procedures during the study period, 5) were not taking oral or intrathecal opioids, 6) were not taking benzodiazepines,7) were naïve to acupuncture, 8) and had low back pain of at least six months duration with a significant discogenic component, either with or without radicular pain. Eligibility was determined by the lead investigator (ADW) at the first visit through a review of a history and physical examination, and MRI findings confirming disc disease. Patients were included if this evaluation found that a source of pain was at least one degenerated, herniated, or torn lumbar disc with either a minimum Grade III disc degeneration,39 abnormal morphology,18 or a hyperintense zone.2 These criteria exclude those with pain due purely to nonspecific or myofacial causes and include those with the commonly presenting mixed syndrome of low back pain with underlying disc pathology, and possibly spinal stenosis or facet disease.
Procedures
At the first visit subjects were divided into three groups--Low, Moderate, or High levels of psychopathology, by applying a specified model for classifying the degree of psychopathology, used previously by the authors and described below.57 Only those subjects in the Low or High groups were allowed to continue. Subjects completed a battery of psychological, pain, and functional measures.
Primary Psychological Measures to Determine High, Moderate, and Low Symptoms
Beck Depression Inventory II (BDI)
The 21-item BDI has been shown to have good sensitivity and specificity for major depression in chronic pain patients, provided that a higher cutoff score for major depression is used to account for somatic symptoms due to pain.22, 52 Cut off scores of >20 (high), and <14 (low) were adopted for depression symptoms.22
Pain Anxiety Symptoms Scale (PASS)
This 40-item scale has been reliably used to assess the level of anxiety in pain patients.35, 37 Based on published scores among low back pain patients, a score above the 75th percentile was considered high and less than the 25th percentile was low for anxiety symptoms.36
NEO Personality Inventory-Short Form (NEO-FFI)
The 60-item NEO-FFI is a widely used personality measure10 that assesses five domains: neuroticism, extraversion, openness, agreeableness, and conscientiousness.9 It has been used extensively with pain patients and demonstrates good psychometric properties.16, 24, 55, 56 These studies indicate that elevated levels of neuroticism by itself are associated with worse pain and disability. Furthermore, elevated neuroticism is a hallmark indicator of heightened negative affect.20 In reference to general population norms, NEO-FFI ‘T’ scores greater than the 75th percentile for neuroticism were considered high, and less than the 50th percentile were low for neuroticism.
Pain Intensity and Functional Measures
Numerical Rating Scale of Pain (NRS)
The NRS ranges from 0 (no pain) to 10 (worst possible pain) to assess present pain intensity.38 This was repeated at the beginning and end of each of the three visits.
Neuropathic Pain Questionnaire, Short Form (NPQ)
This validated scale describes the presence or absence of neuropathic pain symptoms, using self-rated descriptive terms for neuropathic pain symptoms such as burning or numbness.3 It has a predictive accuracy for neuropathic pain of 73%.
Oswestry Disability Index (ODI)
The ODI is an extensively used 10-item scale to describe the level of disability in patients with chronic low back pain.17
Secondary Measures
Pain Catastrophizing Scale (PCS)
This 13-item survey assesses beliefs and thoughts about pain shown to have an independent relationship to pain from other psychological constructs.48
Expectations for Relief Scale (ERS) and evaluating the blind
At visit 1 and prior to each treatment (verum or placebo) at visits 2 and 3, subjects were asked what they expected their pain level to be after a treatment using a 0–10 scale. A lower rating indicates a positive expectation for relief. At the end of each session subjects were asked to guess which treatment they received, verum or sham. This method has been used by the authors in a previous study.57
Massachusetts General Hospital Acupuncture Sensation Scale (MASS)
This is a validated, 12- item scale used by subjects to rate the qualities of the acupuncture needle sensation. Elevated ratings on these items have been shown to correlate to acupuncture analgesia.30
Genetic predictors
There are many candidate genes for pain;5, 13 yet co-methyl transferase (COMT) genotypes, specifically, may provide a genetic basis for the links between negative affective symptoms and pain. The single nucleotide polymorphism val158met in the COMT gene is associated with different enzyme activity levels and has been correlated with pain tolerance level and anxiety.15, 41, 62 At visit 1 patients had blood drawn for this characterization.
Primary Predictor of Outcome
The model to classify the degree of psychopathology is based on a combination of psychological symptoms to determine group assignment. We did not seek an all-inclusive model for psychopathology in patients with chronic pain, which may incorporate relevant theoretical concerns, such as linear vs. categorical classifications of symptoms and illness or the impact of social factors (e.g., work and education). Rather, as in our previous studies,57–59 we focused on the magnitude of difference in negative affective symptoms between the Low and High groups, which have been shown to correlate to pain treatment responses. To be in the High group, subjects had to have high scores on at least two out of three measures used to determine psychological symptoms: the BDI, PASS, and neuroticism subscale of the NEO. Conversely, subjects in the Low group had low scores on at least two out of three measures, while the Moderate group consisted of subjects not falling into either the High or Low groups.
Primary Outcome
Percent improvement in pain rating from the beginning to the end of session for verum and placebo acupuncture sessions was calculated using the NRS.
Sample Size Calculations
Sample size requirements were estimated using baseline pain ratings (mean 6.1on a 0–10 scale, SD=1.6) from a previous oral opioid study in patients with low back pain, drawn from the same clinic population as in this study.26 We sought 90% power to find a minimum 30% difference between groups in analgesia from acupuncture needling using a 0–10 scale (a clinically meaningful difference).19 Many of the acupuncture studies for CLBP show 30% improvement in pain on average (with an average 24% standard deviation).21 Thus, in examining subgroups of responders, postulated effect size differences might be 30–40% improvement in Low group vs. 0–10% improvement in the High group, for example. We assumed an equal within group variance of analgesia responses amongst the groups, and an alpha level of .05. We estimated that 20 subjects per group would be needed, and we enrolled 22 per group to anticipate dropouts. This sample size calculation does pose the risk of missing smaller effect size differences between groups.
Data Analysis
A repeated measures analysis of variance (ANOVA) was used to characterize the relationship between psychiatric group and analgesia. Secondary predictors included scores on the PCS, NPQ, ERS, ODI, and COMT profiles. These as well as baseline demographic, social, and pain history variables were included in a repeated measures analysis of covariance (ANCOVA).
Needling Procedures
At visit 1, the lead investigator (ADW) explained the study to each patient and the two types of needles that would be used in sessions 2 and 3. Sessions were 5–21 days apart. Subjects were then shown the verum needle. The placebo condition needle was described as looking identical to the verum needle and that when the needle touches the skin the tip retracts into the shaft, like a ballpoint pen (Streitberger placebo needle).29, 46, 61 Subjects were told that a general pain relief point on the dorsal surface of their right hand between their thumb and index finger would be stimulated during the verum session. But they were cautioned that this is not an acupuncture treatment protocol for low back pain and thus we do not know if it will be helpful. Large Intestine 4 (LI4) is the name of this acupoint and it is located at the highest point of the adductor pollicis muscle. It is located on the dorsum of the right hand, between the 1st and 2nd metacarpal bones, approximately in the middle of the 2nd metacarpal bone on the radial side. Sham LI 4 was located on the dorsum of the right hand, between the 1st and 2nd metacarpal bones, approximately in the middle of the 1st metacarpal bone on the ulnar side. LI4 is used for painful conditions and most commonly used for head and neck pain.43 LI4 was chosen because: 1) previous studies of placebo versus real acupuncture in healthy subjects have used LI4,23 2) it is one of the most important analgesic points, such that stimulation of this point relieves pain in all parts of the body,47 and 3) a previous study demonstrated that the point can be used to relieve lower back pain and pelvic pain.49 At sessions two and three a licensed acupuncturist (JK) administered the treatments for 30 minutes, rotating the needle at a frequency of approximately 60 Hz. The acupuncturist did not know to which psychopathology group each subject belonged. For the verum treatment, induction of de Qi (the numb, sore, radiating sensation the patient feels when an acupuncturist rotates the needle) was elicited by manual stimulation. The placebo treatment was administered at the sham point, off of LI4, and with a placebo needle, rotated at the same frequency for 30 minutes.
Results
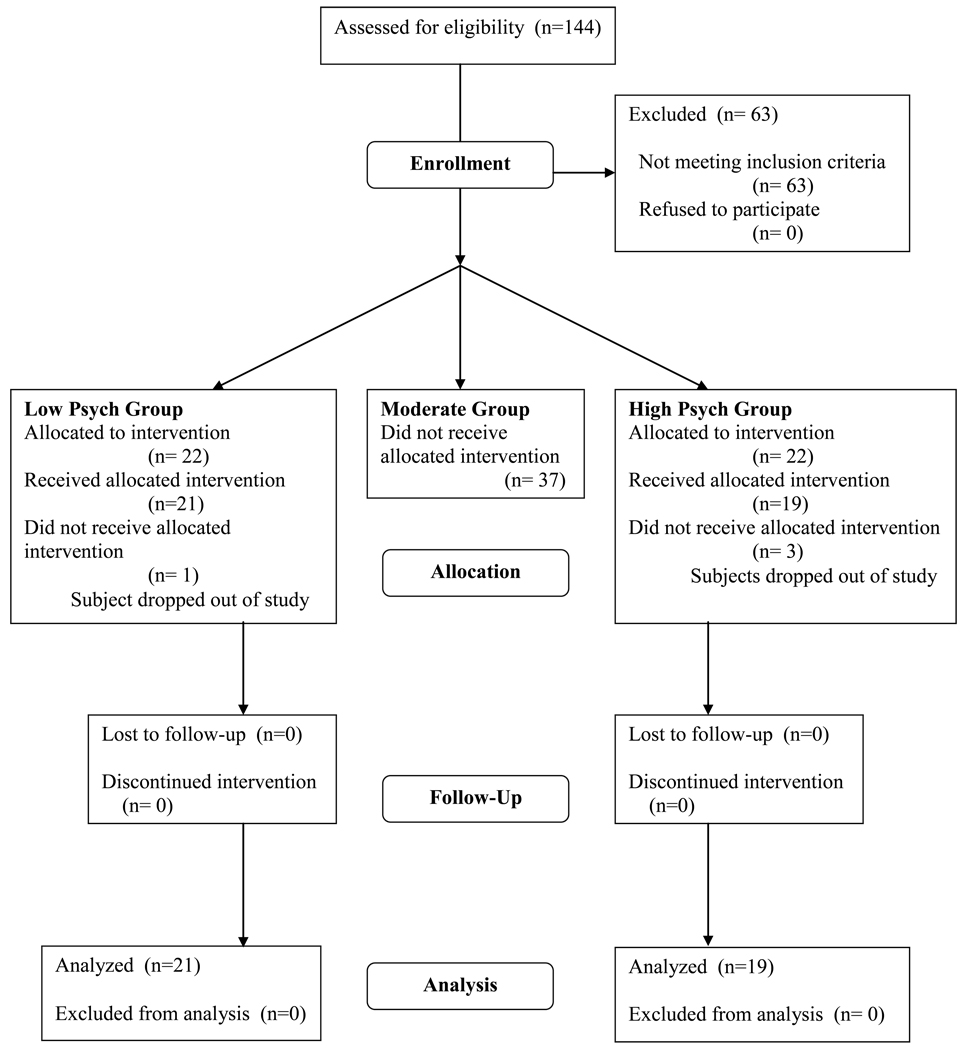
Figure 1 displays the CONSORT diagram for patient flow through the study. One patient dropped out of the Low Psychopathology group and three from the High group. 37 out of 81 suitable for enrollment patients fell into the Moderate psychopathology group and did not go beyond Session 1. Table 1 displays the demographic and patient history details. In the Low group (n=21), 12/21 were low on 2/3 psychological scales (BDI, PASS, and Neuroticism subscale of the NEO), and 9/21 were low on all three scales. In the High group (n=19), 9/19 subjects were high on 2/3 scales and 10/19 were high on 3/3 scales. This pattern was not significantly different between groups. The groups were matched on many variables, with some exceptions. The High group had a significantly higher rate of neuropathic pain complaints and a significantly higher level of disability (p<.05). In addition, the High group tended to be working less, married at a lower rate, more likely to be smokers, and have pain longer. Compared to the baseline low back pain rating at session 1, there were no significant differences in baseline ratings at sessions two and three.
Figure 1.
Patient Flow Diagram
Table 1.
Demographics and Pain History
| Low | High | ||
|---|---|---|---|
| Psych | Psych | ||
| Variable | (n=21) | (n=19) | Sig. |
| Age (avg., years) | 49.1 | 47.2 | NS |
| Gender (%female) | 52.4 | 50 | NS |
| Race (% Caucasian) | 81 | 70 | NS |
| WorK status (% working) | 81 | 55 | NS |
| Worker's Comp. (% yes) | 9.5 | 20 | NS |
| Marital status (% married) | 42.9 | 25 | NS |
| Smoking (% yes) | 9.5 | 40 | NS |
| Previous Lumbar Surgery (% yes) | 19 | 10 | NS |
| Pain Duration (avg., years) | 5.1 | 9.3 | NS |
| Baseline Pain Intensity (avg., 0–10) | 4.4 | 5.3 | NS |
| Radicular Pain (% yes) | 57.1 | 55 | NS |
| Neuropathic Pain (% yes) | 33 | 70 | p=.02 |
| Disability Level (% disability) | 28.4 | 45.4 | p=.0001 |
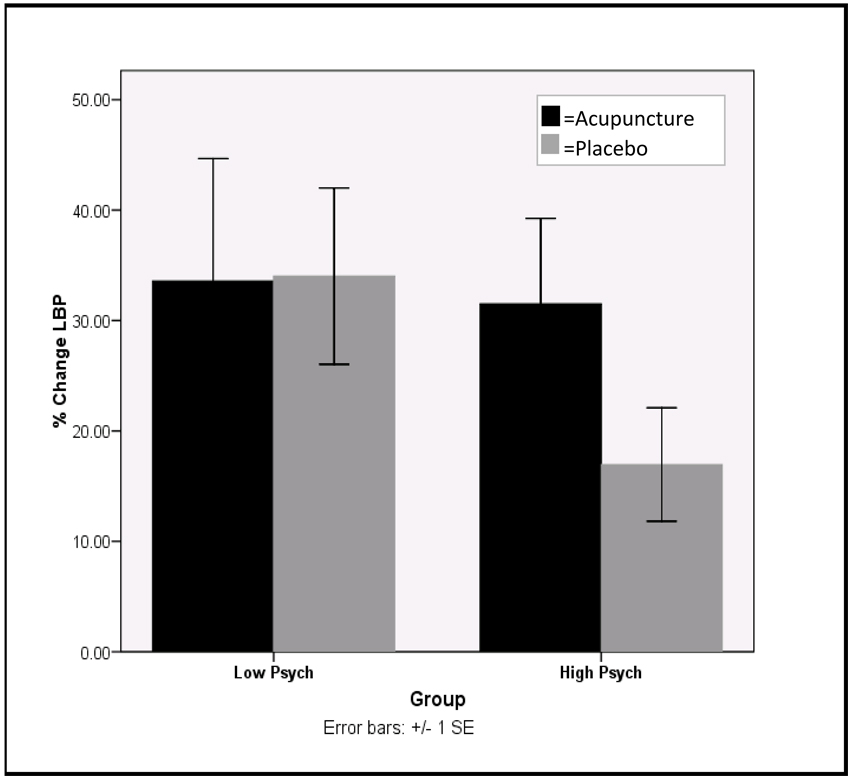
Figure 2 summarizes the results for the main outcome variable, the percent improvement in pain at the end of a treatment session, acupuncture or placebo. Both groups reported very similar improvements in pain after verum acupuncture needling: 33.6% in the Low group vs. 31.5% in the High group, p=.90. For placebo needling, the Low group tended to report greater analgesia, a mean 32% improvement, while the High group reported 17% improvement, p=.09. We calculated the acupuncture minus placebo analgesia differences for each subject, and there were no significant differences between groups (p= .33). In addition, there were no significant correlations between the subjects’ verum and placebo responses, i.e., within subject response to verum acupuncture did not predict response to placebo or vise versa.
Figure 2.
% Change in LBP at the End of Treatment Session
In regards to the quality of the sensations, ratings on the MASS survey indicate that during verum needling subjects rated 7/12 items significantly greater than placebo (p<.025, for soreness, heaviness, numbness, tingling, aching, throbbing, and stabbing). There were no significant relationships between scores on the MASS items and acupuncture or placebo analgesia. In addition, there were no significant relationships between the magnitude of MASS item scores and whether or not subjects guessed at the end of the either session they had received verum or placebo treatment. In other words, the degree of sensations felt during needling was not related to the subject concluding that they had received either acupuncture or placebo.
Table 2 summarizes the covariate and secondary predictor analyses. Using ANCOVA, baseline demographic, history, and pain variables (including the presence of neuropathic pain or the level of disability) were not significant univariate predictors of acupuncture or placebo analgesia. In addition, none of these variables significantly interacted with psychopathology group in testing repeated measures ANCOVA models of treatment + group + treatment X group X [secondary variable] as predictors of acupuncture or placebo analgesia. In terms of other secondary predictors, neither COMT genotype profiles nor catastrophizing scores were univariate predictors of analgesia or had a significant interaction with group and treatment.
Table 2.
Covariate Analyse
| Low Psych | High Psych | ||
|---|---|---|---|
| Variable | (n=21) | (n=19) | Sig |
| Expectations | |||
| Acupuncture session | 2.9 | 3.7 | NS |
| Placebo session | 2.7 | 4.1 | p=.03 |
| *at session start patients rated expected pain level after the treatment (0–10); lower value=greater expectations | |||
| Group X Treatment X Acup. Expectations Interaction |
p=.002 (F=11.3) |
||
| Group X Treatment X Plac. Expectations Interaction | NS | ||
| Perceived treatment/ efectiveness of the blind. | |||
| % guessing correctly at end of session | |||
| Acupuncture session | 90 | 89 | NS |
| Placebo session | 41 | 59 | NS |
| Randomization order | NS | ||
| Random Order X Perceived Treatment Interaction | |||
| **if the patient had acupuncture at the 1st or 2nd session, did that influence whether they guessed correctly? | |||
| Acupuncture session | NS | ||
| Placebo session | NS | ||
A similar approach using ANCOVA was undertaken for the analysis of the impact of expectations (a continuous variable, see Table 2). During the placebo session the Low group reported greater expectations of relief than the High group, p=.03. Expectation levels were not univariate predictors of analgesia in either the placebo or acupuncture condition. However, in adding expectations to the model of Treatment + Group + Treatment X Group X Expectations as predictors of analgesia, the level of expectations during the verum acupuncture session did significantly interact with group and treatment (F=11.3, p=.002), such that during verum treatment in both the Low and High groups greater expectations for improvement significantly predicted greater analgesia. This positive interaction indicating that greater expectations for improvement are associated with greater verum acupuncture analgesia, increased the estimated means of acupuncture analgesia in each group by>10% (Low group 33.6 → 38.3% improvement, High group 31.5 → 35.5% improvement). Expectations during the placebo treatment session were not significant predictors of placebo analgesia, neither as a univariate predictor nor as an interacting covariate with group and treatment.
Treatment order effects (randomization) were examined as univariate predictors of pain improvement or as significant interaction terms with group, and were not significant. In terms of the effectiveness of the blind, on average 50% of the subjects were able to guess the treatment correctly after the placebo session, and there was no effect of treatment order (i.e. whether they received placebo at the second or third session did not affect their ability to guess the treatment correctly). Those subjects who thought at the end of any session (be it the verum or placebo sessions) that they received acupuncture demonstrated a trend towards greater analgesia vs. those who thought they had placebo at the end of a session (33.1% vs. 17.2 % improvement, p=.22).
Discussion
In this controlled, crossover design study, we investigated several factors relevant to the mechanisms underlying the possible positive benefits of acupuncture in CLBP, such as placebo response, the impact of the level of psychopathology, and expectations for improvement. Overall, contrary to our hypothesis, both groups of CLBP patients, those with a High or Low level of psychopathology, benefitted similarly with either acupuncture or placebo treatment. Although, there was a trend for the High psychopathology group to experience less placebo analgesia than the Low group (17 vs. 34%, p=.09) The magnitude of response for the verum condition (an average 32.6% for both groups) mirrors the clinical improvement reported in the acupuncture RCTS for CLBP. We chose subjects with a discogenic component to their back pain because this is a very common presentation of CLBP, for which patients seek acupuncture treatment. In addition, we were most interested in understanding how psychiatric factors impact the response to a treatment for underlying physical pathology.
In our study, the benefits of verum or placebo treatment were reported immediately after a session, and no ordering effects were seen. While the acupuncture treatment in this study was not a typical acupuncture treatment session for CLBP, our findings suggest that broad swaths of patients with CLBP may benefit, if only for its placebo effects. Interestingly, subjects rated the needling sensations during the verum treatment as being fundamentally different than the placebo treatment. This result is in contrast to earlier studies that found the Streitberger placebo needle was rated more similarly to real acupuncture.61 It is unclear why this occurred, but it is possible that the manner in which the placebo needle was described and introduced in this study was different than earlier experiments. And yet, despite the subjects’ experiences of acupuncture differing from placebo in this study, both treatment sessions were analgesic. As noted, the complexity of the placebo phenomena makes it impossible to control for all nonspecific treatment effects. Such effects that were common to both sessions are the focused and caring attention of the healer on the patient, and the effects of relaxation during the treatment sessions.
Clinically, there are many subgroups of patients with CLBP and these results indicate that the level of psychopathology is not a determining factor in the response to acupuncture needling. The acupuncturist was blinded to group assignment and there was no evidence to suggest that the acupuncturist interacted differently with subjects from either group, which one could argue is a potential confound. Given the significant analgesia with verum or placebo needling at sites not commonly used in CLBP treatment, our results also raise the question of whether the specificity of needling sites is important to the therapeutic benefits of acupuncture.
As noted, in some studies positive expectations for relief have shown a positive correlation to acupuncture benefit,4, 31 but this is not universally the case.45 Previous studies in our group have shown that expectancy can be manipulated to augment the effectiveness of acupuncture,32 but these were performed in healthy normals with low levels of psychopathology at study entry. To our knowledge, no investigation studying the impact of expectations on acupuncture treatment for pain has examined whether comorbid psychiatric illness is a factor modulating the effect of expectations on acupuncture response for pain.33 Our findings indicate that greater expectations for improvement are a significant predictor of verum acupuncture response, regardless of the level of psychopathology (as predicted). But, we did not find that the level of expectations significantly predicted the response to placebo acupuncture. This result must be interpreted cautiously, for the study was only adequately powered for a definitive analysis of the primary outcome. It is unclear why expectations significantly interacted with treatment and group in the verum condition, but not the placebo condition. However, scores on the MASS scale indicate that the somatic experience of real acupuncture is fundamentally different than placebo, and perhaps there is some unknown relationship between these perceptions and the impact of expectations on verum or placebo response.
Randomization order effects did not impact this finding, which suggests that when subjects in either group thought they were going to get acupuncture, they expected more relief and received it. The effectiveness of the blind does not appear to be a confounder since only 50% of subjects overall guessed correctly that they were receiving placebo treatment during that session. A 50% rate means that the ability of the subjects to guess the placebo treatment correctly is no better than chance alone. Hence, we can conclude that the placebo used in this study was credible. However, the High psychopathology group was more attune to receiving placebo for unclear reasons. The High group had an 18% greater rate of correct guessing and 50% less analgesia in the placebo condition compared to the Low psych group, which were nonsignificant differences. Overall, our findings indicate that the level of psychopathology does not significantly affect the analgesic benefits of acupuncture or placebo needling in CLBP and does not affect the positive impact of expectations on heightening acupuncture analgesia. Importantly, potential confounders, such as the degree of neuropathic pain or the level of physical disability, do not mitigate these results. Since our primary finding is contrary to our hypothesis, which was based on earlier studies using different treatments for CLBP, these results also suggest that the effects of psychopathology on treatment outcome are modality specific, and that the effect of expectations on outcome may depend on whether the treatment is real or placebo. That is, these factors may have different relationships to outcome depending on the treatment administered. Since psychiatric comorbidity bodes poorly for pain treatment outcome in general,7 this statement may not hold true depending on the type of treatment administered, particularly if the treatment in question has a strong mind-body emphasis, such as acupuncture. Future studies of acupuncture and placebo may consider an assessment for psychopathology in addition to expectancy effects, so that these relationships can be further investigated.
Since there were no significant relationships between analgesia during the verum and placebo sessions, and no significant predictors of response to either treatment (except for expectations predicting verum response only), our results add to the body of literature arguing that there are no valid means at present to identify placebo responders, be it to acupuncture or other treatments for pain.28, 42 These conclusions have implications for how analgesic effects are calculated in general, and for the conduct of acupuncture trials, more specifically. Our findings suggest that to determine the “true” or intrinsic analgesic properties of a treatment that subtracting placebo analgesia from the verum treatment analgesia is not scientifically valid. And yet, this is quite a natural instinct whenever one sees a table or graph of treatment and placebo responses side by side. In terms of acupuncture, the high placebo responses seen in the RCTs may not signal that positive verum acupuncture treatment results are just placebo effects. Indeed, a neurobiological basis for this interpretation is emerging. Recent brain neuroimaging findings from our group have demonstrated that as seen on fMRI, the evoked neural activation patterns are overlapping but distinctly different between verum acupuncture analgesia and placebo acupuncture analgesia, even when controlling for the effects of expectancy.32
Several limitations of our study deserve discussion. First, the verum treatment we administered was not a commonly used treatment protocol for CLBP, and so our findings may not be wholly applicable to acupuncture treatment for CLBP. Therefore, our study adds no information on whether a typical acupuncture protocol has efficacy beyond placebo. However, since patients still significantly benefitted with this intervention to the same extent as they have in the RCTs for CLBP, our results do have implications for all forms of CLBP acupuncture treatment. Second, this was a study of acupuncture needling, and not a course of acupuncture treatment. We only examined immediate treatment response and not sustained benefit. And lastly, while our study was adequately powered for analysis of the primary pain outcome, it was not sufficiently powered for a definitive analysis of the covariates which can be said to apply to populations receiving acupuncture treatment for CLBP. Nevertheless, we can conclude with caution that within this sample of patients expectations for improvement do predict the response to verum acupuncture needling, but not placebo needling. Moreover, we can also conclude that within our sample no other covariates we examined were significantly relevant. These findings can inform the development of future studies.
In sum, the controlled and blinded study design provided a framework for a detailed analysis of the effects of placebo, psychopathology, and expectations on the response to acupuncture needling in patients with CLBP. Our findings reveal that the level of psychiatric comorbidity was not a significant predictor of verum or placebo responses, and that both treatments produced clinically meaningful analgesia. Expectations for improvement may only be a significant predictor of response to verum treatment, and this result may hold true regardless of the level of psychopathology.
Perspective
Psychiatric comorbidity may predict differences between acupuncture and placebo responses, not otherwise seen in the RCTs for low back pain. Using a blinded, crossover design, we report that it does not predict outcome, nor does it seem to modify the effect of expectancy (a known, predictor) on acupuncture response.
Acknowledgements
This study was registered with the National Institutes of Health, ClinicalTrials.gov identifier: NCT00307788. This work was supported by NIH grants# NIDA 1K23DA020681-01A1 and NCCAM P01 AT002048-01 (ADW); NCAAM KO1AT003883 (JK); NCAAM K24AT004095 (TK). The authors have no conflicts of interest to declare.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Andersson G. Epidemiological Features of Low Back Pain. Lancet. 1999;354:581–585. doi: 10.1016/S0140-6736(99)01312-4. [DOI] [PubMed] [Google Scholar]
- 2.Aprill C, Bogduk N. High-Intensity Zone: a Diagnostic Sign of Painful Lumbar Disc on Magnetic Resonance Imaging. Brit J Radiol. 1992;65:361–369. doi: 10.1259/0007-1285-65-773-361. [DOI] [PubMed] [Google Scholar]
- 3.Backonja MM, Krause SJ. Neuropathic pain questionnaire--short form. Clin J Pain. 2003;19:315–316. doi: 10.1097/00002508-200309000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Bausell RB, Lao L, Bergman S, Lee WI, Berman BM. Is Acupuncture Analgesia an Expectancy Effect? Preliminary Evidence based on Participants' Perceived Assignment in Two Placebo-Controlled Trials. Eval Hlth Prof. 2005;28:9–26. doi: 10.1177/0163278704273081. [DOI] [PubMed] [Google Scholar]
- 5.Belfer I, Wu T, Kingman A, Krishnaraju RK, Goldman D, Max MB. Candidate Gene Studies of Human Pain Mechanisms. Anesth. 2004;100:1562–1572. doi: 10.1097/00000542-200406000-00032. [DOI] [PubMed] [Google Scholar]
- 6.BenDebba M, Torgerson W, Long D. Personality Traits, Pain Duration and Severity, Functional Impairment, and Psychological Distress in Patients with Persistent Low Back Pain. Pain. 1997;72:115–125. doi: 10.1016/s0304-3959(97)00020-1. [DOI] [PubMed] [Google Scholar]
- 7.Boersma K, Linton SJ. Screening to Identify Patients at Risk: Profiles of Psychological Risk Factors for Early Intervention. Clin J Pain. 2005;21:38–43. doi: 10.1097/00002508-200501000-00005. [DOI] [PubMed] [Google Scholar]
- 8.Cherkin DC, Sherman KJ, Deyo RA, Shekelle PG. A review of the evidence for the effectiveness, safety, and cost of acupuncture, massage therapy, and spinal manipulation for back pain. Ann Intern Med. 2003;138:898–906. doi: 10.7326/0003-4819-138-11-200306030-00011. [DOI] [PubMed] [Google Scholar]
- 9.Costa PT, Herbst JH, McCrae RR, Siegler IC. Personality at Midlife: Stability, Intrinsic Maturation, and Response to Life Events. Assessment. 1992;7:365–378. doi: 10.1177/107319110000700405. [DOI] [PubMed] [Google Scholar]
- 10.Cox B, Borger S, Taylor S, Fuentes K, Ross L. Anxiety Sensitivity and the Five-Factor Model of Personality. Behav Res Ther. 1999;37:633–641. doi: 10.1016/s0005-7967(98)00174-0. [DOI] [PubMed] [Google Scholar]
- 11.Dersh J, Gatchel R, Polatin P, Mayer T. Prevalence of Psychiatric Disorders in Patients with Chronic Work-Related Musculoskeletal Pain and Disability. J Occ. Envir Med. 2002;44:459–468. doi: 10.1097/00043764-200205000-00014. [DOI] [PubMed] [Google Scholar]
- 12.Dersh J, Polatin PB, Gatchel RJ. Chronic pain and psychopathology: research findings and theoretical considerations. Psychosom Med. 2002;64:773–786. doi: 10.1097/01.psy.0000024232.11538.54. [DOI] [PubMed] [Google Scholar]
- 13.Eisenach J. Fishing for Genes: Practical Ways to Study Genetic Polymorphisms for Pain. Anesth. 2004;100:1343–1344. doi: 10.1097/00000542-200406000-00004. [DOI] [PubMed] [Google Scholar]
- 14.Engel CC, Von Korff M, Katon WJ. Back pain in primary care: predictors of high health-care costs. Pain. 1996;65:197–204. doi: 10.1016/0304-3959(95)00164-6. [DOI] [PubMed] [Google Scholar]
- 15.Enoch M, Xu K, Ferro E, Harris C, Goldman D. Genetic Origins of Anxiety in Women: a Role for a Functional COMT Polymorphism. Psych Genetics. 2003;13:33–41. doi: 10.1097/00041444-200303000-00006. [DOI] [PubMed] [Google Scholar]
- 16.Evers A, Kraaimaat F, Van Reil P, Bijlsma J. Cognitive, Behavioral and Physiological Reactivity to Pain as a Predictor of Long-Term Pain in Rheumatoid Arthritis Patients. Pain. 2001;9:139–146. doi: 10.1016/S0304-3959(01)00303-7. [DOI] [PubMed] [Google Scholar]
- 17.Fairbank JCT, Pynsent PB. The Oswestry Disability Index. Spine. 2000;25:2940–2953. doi: 10.1097/00007632-200011150-00017. [DOI] [PubMed] [Google Scholar]
- 18.Fardon D, Milette P. Nomenclature and Classification of Lumbar Disc Pathology: Recommendations of the Combined Task Forces of the North American Spine Society, American Society of Spine Radiology, and the American Society of Neuroradiology. 2001 doi: 10.1097/00007632-200103010-00006. [DOI] [PubMed] [Google Scholar]
- 19.Farrar JT, Young JP, LaMoreaux L, Werth JL, Poole RM. Clinical Importance of Changes in Chronic Pain Intensity Measured on an 11-Point Numerical Pain Rating Scale. Pain. 2001;94:149–158. doi: 10.1016/S0304-3959(01)00349-9. [DOI] [PubMed] [Google Scholar]
- 20.Fernandez E. Anxiety, Depression, and Anger in Pain. Dallas: Advanced Psychological Resources; 2002. Interactions between Pain and Affect; pp. 13–32. [Google Scholar]
- 21.Furlan AD, van Tulder MW, Cherkin DC, Tsukayama H, Lao L, Koes BW, Berman BM. Acupuncture and dry-needling for low back pain. Cochrane Database Syst Rev. 2005:CD001351. doi: 10.1002/14651858.CD001351.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Geisser ME, Roth RS. Assessing Depression Among Persons with Chronic Pain Using the Center for Epidemiological Studies Depression Scale and the Beck Depression Inventory: A Comparative Analysis. Clin J Pain. 1997;13:163–170. doi: 10.1097/00002508-199706000-00011. [DOI] [PubMed] [Google Scholar]
- 23.Goddard G, Shen Y, Steele R, Springer N. A controlled trial of placebo versus real acupuncture. J Pain. 2005;6:237–242. doi: 10.1016/j.jpain.2004.12.009. [DOI] [PubMed] [Google Scholar]
- 24.Groth-Marnat G, Fletcher A. Influence of Neuroticism, Catastrophizing, Pain Duration, and Receipt of Compensation on Short-Term Response to Nerve Block Treatment for Chronic Back Pain. J Behav Med. 2000;23:339–350. doi: 10.1023/a:1005596716967. [DOI] [PubMed] [Google Scholar]
- 25.Haake M, Muller HH, Schade-Brittinger C, Basler HD, Schafer H, Maier C, Endres HG, Trampisch HJ, Molsberger A. German Acupuncture Trials (GERAC) for chronic low back pain: randomized, multicenter, blinded, parallel-group trial with 3 groups. Arch Intern Med. 2007;167:1892–1898. doi: 10.1001/archinte.167.17.1892. [DOI] [PubMed] [Google Scholar]
- 26.Jamison RN, Raymond SA, Slawsby EA, Nedeljkovic SS, Katz NP. Opioid Therapy for Chronic Noncancer Back Pain. Spine. 1998;23:2591–2600. doi: 10.1097/00007632-199812010-00014. [DOI] [PubMed] [Google Scholar]
- 27.Kalauokalani D, Cherkin DC, Sherman KJ, Koepsell TD, Deyo R. Lessons From a Trial of Acupuncture and Massage for Low Back Pain. Spine. 2001;26:1418–1424. doi: 10.1097/00007632-200107010-00005. [DOI] [PubMed] [Google Scholar]
- 28.Kaptchuk TJ, Kelley JM, Deykin A, Wayne PM, Lasagna LC, Epstein IO, Kirsch I, Wechsler ME. Do "Placebo Responders" Exist? Cont Clin Trials. 2008;29 doi: 10.1016/j.cct.2008.02.002. [DOI] [PubMed] [Google Scholar]
- 29.Kong J, Fufa DT, Gerber AJ, Rosman IS, Vangel MG, Gracely RH, Gollub RL. Psychophysical outcomes from a randomized pilot study of manual, electro, and sham acupuncture treatment on experimentally induced thermal pain. J Pain. 2005;6:55–64. doi: 10.1016/j.jpain.2004.10.005. [DOI] [PubMed] [Google Scholar]
- 30.Kong J, Gollub R, Huang T, Polich G, Napadow V, Hui K, Vangel M, Rosen B, Kaptchuk TJ. Acupuncture de qi, from qualitative history to quantitative measurement. J Altern Complement Med. 2007;13:1059–1070. doi: 10.1089/acm.2007.0524. [DOI] [PubMed] [Google Scholar]
- 31.Kong J, Gollub RL, Rosman SI, Webb JM, Vangel MG, Kirsch I, Kaptchuk TJ. Brain Activity Associated with Expectancy-Enhanced Placebo Analgesia as Measured by Functional Magnetic Resonance Imaging. J Neurosci. 2006;26:381–388. doi: 10.1523/JNEUROSCI.3556-05.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kong J, Kaptchuk TJ, Polich G, Kirsch I, Vangel M, Zyloney C, Rosen B, Gollub R. Expectancy and treatment interactions: A dissociation between acupuncture analgesia and expectancy evoked placebo analgesia. Neuroimage. 2009;45:940–949. doi: 10.1016/j.neuroimage.2008.12.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Linde K, Witt CM, Streng A, Weidenhammer W, Wagenpfel S, Brinkhaus B, Willich SN, Melchart D. The impact of patient expectations on outcomes of four randomized controlled trials of acupuncture in patients with chronic pain. Pain. 2007;128:264–271. doi: 10.1016/j.pain.2006.12.006. [DOI] [PubMed] [Google Scholar]
- 34.Linton S. A Review of Psychological Risk Factors in Back and Neck Pain. Spine. 2000;25:1148–1156. doi: 10.1097/00007632-200005010-00017. [DOI] [PubMed] [Google Scholar]
- 35.McCracken L, Gross R, Aikens J, Carnrike C. The Assessment of Anxiety and Fear in Persons with Chronic Pain: a Comparison of Instruments. Behav Res Ther. 1996;34:927–933. doi: 10.1016/s0005-7967(96)00057-5. [DOI] [PubMed] [Google Scholar]
- 36.McCracken L, Gross R, Sorg P, Edmans T. Prediction of Pain in Patients with Chronic Low Back Pain: Effects of Inaccurrate Prediction and Pain-Related Anxiety. Behav Res Ther. 1993;31:647–652. doi: 10.1016/0005-7967(93)90117-d. [DOI] [PubMed] [Google Scholar]
- 37.McCracken L, Zayfert C, Gross R. The Pain Anxiety Symptoms Scale: Development and Validation of a Scale to Measure Fear of Pain. Pain. 1992;50:67–73. doi: 10.1016/0304-3959(92)90113-P. [DOI] [PubMed] [Google Scholar]
- 38.Melzack R, Katz J. The McGill Pain Questionnaire: Appraisal and Current Status. In: Turk DC, Melzack R, editors. Handbook of Pain Assessment. 2nd ed. New York: Guilford Press; 2001. pp. 35–52. [Google Scholar]
- 39.Pfirrmann CW, Metzdorf A, Zanetti M, Hodler J, Boos N. Magnetic resonance classification of lumbar intervertebral disc degeneration. Spine. 2001;26:1873–1878. doi: 10.1097/00007632-200109010-00011. [DOI] [PubMed] [Google Scholar]
- 40.Polich G, Kong J, Napadow V, Gollub R. Complementary Medicine and the Central Mediation of Functional Pain Disorders. In: Mayer EA, Bushnell MC, editors. Functional Pain Syndromes: Presentation and Pathophysiology. Seattle: IASP Press; 2009. pp. 1–20. [Google Scholar]
- 41.Rakvag TT, Klepstad P, Baar C, Kvam TM, Dale O, Kaasa S, Krokan HE, Skorpen F. The Val 158Met polymorphism of the Human Catechol-O-Methyltransferase (COMT) Gene may Influence Morphine Requirements in Cancer Pain Patients. Pain. 2005;116:73–78. doi: 10.1016/j.pain.2005.03.032. [DOI] [PubMed] [Google Scholar]
- 42.Shapiro AK, Shapiro E. Predicting Placebo Response. In: Shapiro AK, Shapiro E, editors. The Powerful Placebo: from Ancient Preist to Modern Physician. Baltimore: Johns Hopkins University Press; 1997. pp. 217–218. [Google Scholar]
- 43.Silva SA. Acupuncture for the relief of pain of facial and dental origin. Anesth Prog. 1989;36:244–245. [PMC free article] [PubMed] [Google Scholar]
- 44.Smith LA, Oldman AD, McQuay HJ, Moore RA. Teasing apart quality and validity in systematic reviews: an example from acupuncture trials in chronic neck and back pain. Pain. 2000;86:119–132. doi: 10.1016/s0304-3959(00)00234-7. [DOI] [PubMed] [Google Scholar]
- 45.So DW. Acupuncture Outcomes, Expectations, Patient-Provider Relationship, and the Placebo Effect; Implications for Health Promotion. Amer J Pub Hlth. 2002;92:1662–1667. doi: 10.2105/ajph.92.10.1662. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Streitberger K, Kleinhenz J. Introducing a placebo needle into acupuncture research. Lancet. 1998;352:992–1002. doi: 10.1016/S0140-6736(97)10471-8. [DOI] [PubMed] [Google Scholar]
- 47.Stux G. Channels, Organs, and Points. In: Stux G, Pomeranz B, editors. Basics of Acupuncture. Berlin: Springer-Verlag; 1997. pp. 110–115. [Google Scholar]
- 48.Sullivan MJ, Pivik J. The Pain Catastrophizing Scale: Development and Validation. Psychol Assessment. 1995;7:524–532. [Google Scholar]
- 49.Ternov NK, Grennert L, Aberg A, Algotsson L, Akeson J. Acupuncture for lower back and pelvic pain in late pregnancy: a retrospective report on 167 consecutive cases. Pain Med. 2001;2:204–207. doi: 10.1046/j.1526-4637.2001.01031.x. [DOI] [PubMed] [Google Scholar]
- 50.Thompson JJ, Ritenbaugh C, Nichter M. Reconsidering the placebo response from a broad anthropological perspective. Cult Med Psychiatry. 2009;33:112–152. doi: 10.1007/s11013-008-9122-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Turk DC, Akiko O. Psychological Factors in Chronic Pain: Evolution and Revolution. J Consult Clin Psychol. 2002;70:678–690. doi: 10.1037//0022-006x.70.3.678. [DOI] [PubMed] [Google Scholar]
- 52.Turner JA, Romano JM. Self-Report Screening Measures for Depression in Chronic Pain Patients. J Clin Psychol. 1984;40:909–913. doi: 10.1002/1097-4679(198407)40:4<909::aid-jclp2270400407>3.0.co;2-j. [DOI] [PubMed] [Google Scholar]
- 53.Von Korff M, Crane P, Lane M, Miglioretti DL, Simon G, Saunders K, Stang P, Brandenburg N, Kessler R. Chronic Spinal Pain and Physical-Mental Comorbidity in the United States: Results from the National Comorbidity Survey Replication. Pain. 2005;113:331–339. doi: 10.1016/j.pain.2004.11.010. [DOI] [PubMed] [Google Scholar]
- 54.Von Korff M, Deyo RA, Cherkin D, Barlow W. Back pain in primary care. Outcomes at 1 year. Spine. 1993;18:855–862. doi: 10.1097/00007632-199306000-00008. [DOI] [PubMed] [Google Scholar]
- 55.Wade JB, Dougherty LM, Hart RP, Cook DB. Patterns of Normal Personality Structure Among Chronic Pain Patients. Pain. 1992;48:37–45. doi: 10.1016/0304-3959(92)90129-Y. [DOI] [PubMed] [Google Scholar]
- 56.Wade JB, Dougherty LM, Hart RP, Rafii A, Price DD. A Cannonical Correlation Analysis of the Influence of Neuroticism and Extraversion on Chronic Pain, Suffering, and Pain Behavior. Pain. 1992;51:67–73. doi: 10.1016/0304-3959(92)90010-9. [DOI] [PubMed] [Google Scholar]
- 57.Wasan AD, Davar G, Jamison RN. The Association between Negative Affect and Opioid Analgesia in Patients with Discogenic Low Back Pain. Pain. 2005;117:450–461. doi: 10.1016/j.pain.2005.08.006. [DOI] [PubMed] [Google Scholar]
- 58.Wasan AD, Fernandez E, Pham LD, Jamison RN, Bhattacharyya N. The association between anxiety, depression, and reported disease severity in chronic rhinosinusitis. Annals of Otology, Rhinology, and Laryngology. 2007;116:491–497. doi: 10.1177/000348940711600703. [DOI] [PubMed] [Google Scholar]
- 59.Wasan AD, Jamison RN, Pham L, Tipirneni N, Nedeljkovic SS, Katz JN. Psychopathology Predicts the Outcome of Medial Branch Blocks with Corticosteroid for Chronic Axial Low Back or Cervical Pain: a Prospective Cohort Study. BMC Musculoskelet Disord. 2009;10:22. doi: 10.1186/1471-2474-10-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Wasan AD, Kaptchuk TJ, Davar G, Jamison RN. The Association Between Psychopathology and Placebo Analgesia in Patients with Discogenic Low Back Pain. Pain Medicine. 2006;7:217–228. doi: 10.1111/j.1526-4637.2006.00154.x. [DOI] [PubMed] [Google Scholar]
- 61.White P, Lewith G, Hopwood V, Prescott P. The placebo needle, is it a valid and convincing placebo for use in acupuncture trials? A randomized, single blind, crossover pilot trial. Pain. 2003;106:401–409. doi: 10.1016/j.pain.2003.08.013. [DOI] [PubMed] [Google Scholar]
- 62.Zubieta JK, Heitzeg MM, Smith YR, Bueller JA, Xu K, Xu Y, Koeppe RA, Stohler CS, Goldman D. COMT val158met Genotype Affects Mu-Opioid Neurotransmitter Responses to a Pain Stressor. Science. 2003;299:1240–1243. doi: 10.1126/science.1078546. [DOI] [PubMed] [Google Scholar]