Abstract
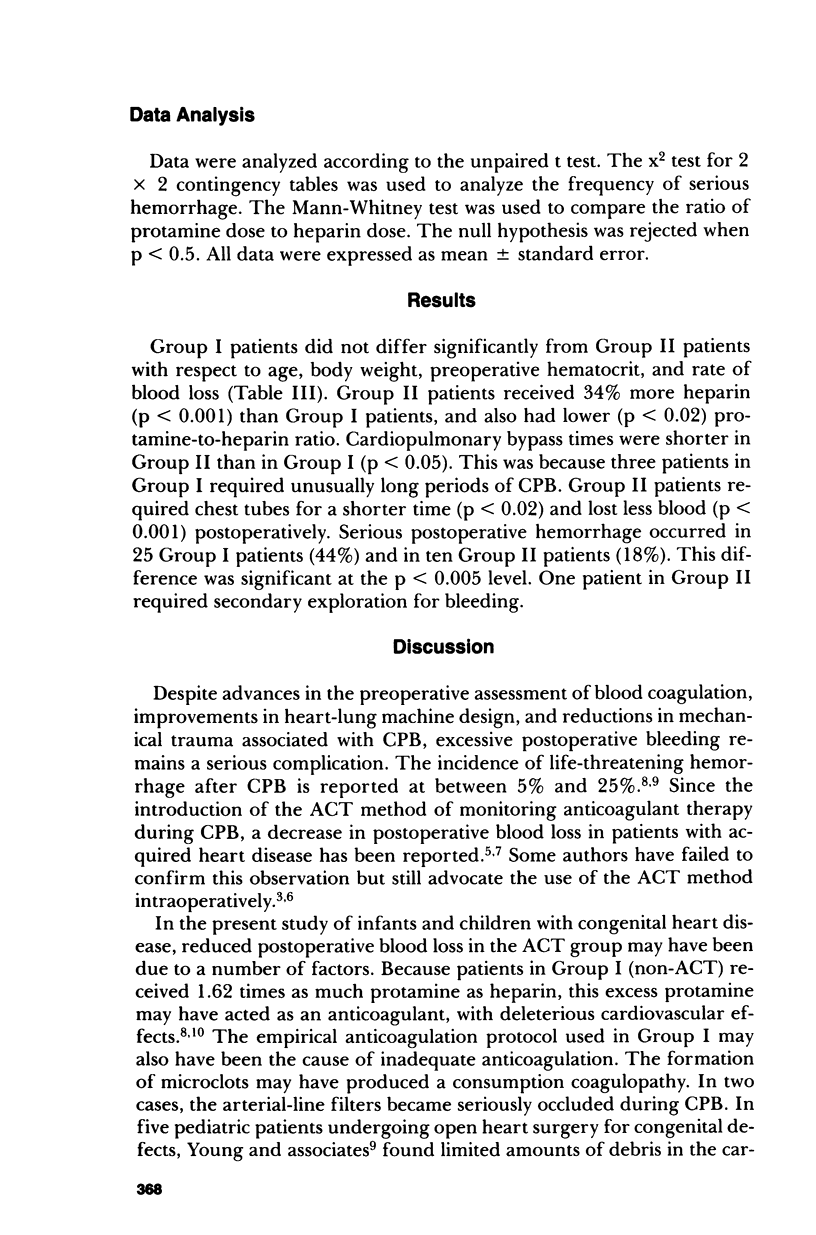
The use of a fixed dosage schedule was compared with the use of activated clotting time (ACT) for determining heparin and protamine dosages during and after cardiopulmonary bypass disease. Use of the ACT resulted in a statistically significant increase in heparin dosage and a statistically significant reduction of postoperative blood loss. With ACT use, chest tubes were retained for a shorter period of time, and the incidence of serious postoperative hemorrhage was reduced from 44% to 18%. These results confirm the superiority of the ACT method for monitoring intraoperative anticoagulation in pediatric patients with congenital heart disease.
Full text
PDF
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Akl B. F., Vargas G. M., Neal J., Robillard J., Kelly P. Clinical experience with the activated clotting time for the control of heparin and protamine therapy during cardiopulmonary bypass. J Thorac Cardiovasc Surg. 1980 Jan;79(1):97–102. [PubMed] [Google Scholar]
- Bick R. L. Alterations of hemostasis associated with cardiopulmonary bypass: pathophysiology, prevention, diagnosis, and management. Semin Thromb Hemost. 1976 Oct;3(2):59–82. doi: 10.1055/s-0028-1086129. [DOI] [PubMed] [Google Scholar]
- Bull B. S., Korpman R. A., Huse W. M., Briggs B. D. Heparin therapy during extracorporeal circulation. I. Problems inherent in existing heparin protocols. J Thorac Cardiovasc Surg. 1975 May;69(5):674–684. [PubMed] [Google Scholar]
- Goldman B. S., Joison J., Austen W. G. Cardiovascular effects of protamine sulfate. Ann Thorac Surg. 1969 May;7(5):459–471. doi: 10.1016/s0003-4975(10)66210-8. [DOI] [PubMed] [Google Scholar]
- Gourin A., Streisand R. L., Greineder J. K., Stuckey J. H. Protamine sulfate administration and the cardiovascular system. J Thorac Cardiovasc Surg. 1971 Aug;62(2):193–204. [PubMed] [Google Scholar]
- Jaberi M., Bell W. R., Benson D. W. Control of heparin therapy in open-heart surgery. J Thorac Cardiovasc Surg. 1974 Jan;67(1):133–141. [PubMed] [Google Scholar]
- Roth J. A., Cukingnan R. A., Scott C. R. Use of activated coagulation time to monitor heparin during cardiac surgery. Ann Thorac Surg. 1979 Jul;28(1):69–72. doi: 10.1016/s0003-4975(10)63396-6. [DOI] [PubMed] [Google Scholar]
- Verska J. J. Control of heparinization by activated clotting time during bypass with improved postoperative hemostasis. Ann Thorac Surg. 1977 Aug;24(2):170–173. doi: 10.1016/s0003-4975(10)63728-9. [DOI] [PubMed] [Google Scholar]
- Verska J. J., Lonser E. R., Brewer L. A., 3rd Predisposing factors and management of hemorrhage following open heart surgery. J Cardiovasc Surg (Torino) 1972 Jul-Aug;13(4):361–368. [PubMed] [Google Scholar]
- Young J. A., Kisker C. T., Doty D. B. Adequate anticoagulation during cardiopulmonary bypass determined by activated clotting time and the appearance of fibrin monomer. Ann Thorac Surg. 1978 Sep;26(3):231–240. doi: 10.1016/s0003-4975(10)63676-4. [DOI] [PubMed] [Google Scholar]


