Abstract
This manuscript reports on five cases of spontaneous myelogenous leukemia, similar to human disease, occurring within highly inbred, histocompatible sublines of Massachusetts General Hospital (MGH) MHC-defined miniature swine. In cases where a neoplasm was suspected based on clinical observations, samples were obtained for complete blood count, peripheral blood smear, and flow cytometric analysis. Animals confirmed to have neoplasms were euthanized and underwent necropsy. Histological samples were obtained from abnormal tissues and suspect lesions. The phenotype of the malignancies was assessed by flow cytometric analysis of processed peripheral blood mononuclear cells and affected tissues. Five cases of spontaneous myeloid leukemia were identified in adult animals older than 30 months of age. All animals presented with symptoms of weight loss, lethargy, and marked leukocytosis. At autopsy, all animals had systemic disease involvement and presented with severe hepatosplenomegaly. Three of the five myelogenous leukemias have successfully been expanded in vitro. The clustered incidence of disease in this closed herd suggests that genetic factors may be contributing to disease development. Myelogenous leukemia cell lines established from inbred sublines of MGH MHC-defined miniature swine have the potential to be utilized as a model to evaluate therapies of human leukemia.
1. Introduction
Chronic myeloid leukemia (CML) is a clonal proliferative disorder which involves the myeloid, megakaryocyte, and erythroid lineages (Fletcher 2000). Similar to other myeloprolferative disorders, such as polycythemia vera, agnogenic myeloid metaplasia, and essential thrombocythemia, CML arises from a neoplastic transformation of a multipotent bone marrow stem cell (Fletcher 2000; Goldman EE and Graham JC 2000; Whang et al. 1963). CML is observed in both humans and animals, usually afflicting an older population (Jemal et al. 2007; Joiner et al. 1976; Leifer et al. 1983). In humans, this condition is most often, but not always, associated with a chromosomal translocation between chromosomes 9 and 22, also known as the Philadephia chromosome (Ph). In Ph+ translocations the oncogene ABL from chromosome 9 fuses with a region of chromosome 22 known as BCR (breakpoint cluster region). Also in humans, Ph- CML is usually indistinguishable both hematologically and histologically from Ph+ CML (Fletcher 2000). Because CML genetic markers are not available for many of the veterinary species, definitive diagnostic criteria for chronic myeloid leukemia is often difficult to obtain (Goldman EE and Graham JC 2000; Messick J.B. and 2000). The clonal nature of the disorder is often unknown and the diagnosis of CML is based on a progressive clinical course without improvement despite treatment for other diseases that can be associated with a significant leukocytosis. Clinically, CML usually begins with a gradual increase in peripheral blood myeloid cells in all stages of differentiation. Given the multineage nature of the disorder, elevations of the platelet count or erythrocytosis may occur. Hepatomegaly, and splenomegaly, due to organ infiltration by the neoplastic cells usually occurs and other clinical signs including fatigue due to anemia, anorexia, weight loss and depression may be observed. At any point in the disease, there may be an abrupt change from the overproduction of otherwise mature cells to an accelerated or blast phase. Death may be related to organ infiltration and dysfunction or may be secondary to hemorrhage or severe infection during chronic or terminal phases.
Most of the documented cases of leukemias and lymphomas in veterinary oncology have been in the domestic population, primarily in the dog and cat (Goldman EE and Graham JC 2000; Joiner et al. 1976; Leifer et al.1983; Messick J.B. and 2000). Hemolymphatic neoplasias have been reported in farm animals as well, albeit to a lesser degree. Malignancies of the hemolymphatic system were reported in swine as early as 1865 (Bostock and Owen 1973). Reports pertaining to swine neoplasias are limited because of their early death due to slaughter or their utilization during young age for research. However, lymphoma (Skavlen et al. 1986), myeloid leukemia and B cell lymphoblastic leukemia (Rafferty et al. 2007) have been documented in the pig. In swine, specific reports of myeloid leukemia have been described such as myeloid leukosis in young and newborn piglets (Allsup et al. 1981; Marcato 1987), and myeloid neoplasms seen within herds afflicting adult animals greater than 24 months of age (Kadota et al.1987; Kashima et al.1982; Marcato 1987).
We report five cases of myeloid leukemias that occurred within MGH MHC-defined miniature swine. Over the past thirty years, a selective breeding program was initiated to develop and maintain miniature swine with defined MHC genes as a large animal model to study transplantation biology (Sachs et al. 1976; Sachs 1992). Three lines homozygous for different MHC haplotypes (Swine Leukocyte Antigen (SLAa, SLAc and SLAd)) and five lines that bear different intra-MHC recombinant haplotypes (SLAf, SLAg, SLAh, and SLAk) have been bred to maintain heterozygosity at multiple minor histocompatibility loci. Within the SLAd herd, however, intentional sequential sibling pedigreed mating was initiated in an attempt to establish fully inbred sublines of SLAd pigs. These sublines have now reached a coefficient of inbreeding (COI) of >94%, leading to acceptance of reciprocal skin grafts (Mezrich et al. 2003).
In our study, five porcine chronic myeloid leukemias occurred in SLAd pigs. We present the clinical, gross pathology, immunophenotype and diagnostic histopathological findings of these swine myeloid leukemias. Myeloid leukemia cell lines derived from inbred miniature swine have the potential for successful serial transplantation providing, for the first time, a large animal model for studies of myeloid leukemias similar to man.
2. Materials and methods
2.1 MGH MHC-defined miniature swine
MGH MHC-defined miniature swine are bred at an Association for the Assessment of Laboratory Animal Care (AALAC) accredited facility. All animals reported were SLAd breeders over 30 month of age. This is a closed colony. This herd is located in the state of Massachusetts which is USDA-recognized Brucellosis and Pseudorabies (Aujeszky’s Disease) free. In addition, quarterly testing confirms that this colony is free of Transmissable Gastroenteritis and Porcine Reproductive and Respiratory Syndrome. All piglets are vaccinated against Mycoplasma Hyopneumoniae, Hemophilus Parasuis, Streptococcus Suis, Pasteurella Multocida, Bordatella Bronchiseptica, Erysipelothrix Rhusiopathiae at day 7, with a booster vaccination at 28 days of age and also circovirus. All swine six months or older are vaccinated against Erysipelothrix Rhusiopathiae, Leptospira (Canicola-Grippotyphosa-Hardjo-Icterohaemorrhagiae-Pomona), Influenza and Parvovirus. Repeat vaccination and serology is performed every six months. A herdwide deworming program with ivermectin is performed every six months. Quarterly (fecal/nasal bacteriology culture, and fecal smear/floatation are performed. All diagnostic procedures and terminal euthanasia (barbiturate overdose) were approved by the Massachusetts General Hospital Animal Care and Use Committee. Complete blood count (CBC), Chemistry and flow cytometry data not available for animal 12933.
2.2 Pathology
Severely ill animals were humanely euthanized. Organs (thoracic and abdominal organs) were harvested and placed in 10% formalin for 24–72 hours. The tissues were cut at 5µm in thickness and stained with hematoxylin and eosin (H&E) prior to analysis.
2.3 Flow Cytometry
Surface staining and flow cytometry were performed on available tissues, blood cells and established cell lines. Cell suspensions made from peripheral blood, lymph node, liver, bone marrow, spleen, small and large intestine were analyzed. Antibodies used for flow cytometry were as follows: CD1 76-7-4 (Pescovitz et al. 1984); CD2 MSA-4 (Hammerberg and Schurig 1986; Pescovitz et al. 1994); CD3 898H2-6-15 (Huang et al. 1999); CD4 74-12-4 (Pescovitz et al. 1984); CD5 BB6-9G12 (Saalmuller et al. 1996); CD8 76-2-11 (Saalmuller et al. 1994); CD16 G7 (Kim et al. 1994); CD172a 74-22-15 (Pescovitz et al. 1984); Class I 2.27.3a (Ivanoska et al. 1991; Lunney 1994); Class II DR 40D (Lunney 1994); Class II DQ TH16 (Davis et al. 1987; Lunney 1994); CD21 BB6-11C9 (Boersma et al.2001; Denham et al.1998); CD25 231.3B2 (Sinkora et al. 2001a); anti-mu heavy chain 5C9 (Paul et al. 1985); and anti-k light-chain K139 3E1 (Sinkora et al. 2001b). Flow cytometry was performed using a Becton Dickinson FACScan (San Jose, CA). Staining of cell suspensions was performed as previously described (Huang et al. 2000). Data were analyzed using Winlist list mode analysis software (Verity Software House, Topsham, ME). Immunophenotype of tumor cell line 14736 has been previously documented (Cho et al Blood).
2.4 Complete Blood Count and Serum Chemical Analysis
Complete blood count (CBC) (HemaVet Drew Corp) and chemistry profiles (IDEXX Corp). Parameters assessed were: alanine aminotransferase (ALT), lactate dehydrogenase (LDH), aspartate aminotransferase (AST), alkaline phosphatase (ALKP), blood glucose, total protein, blood urea nitrogen (BUN), creatinine, cholesterol, triglycerides, sodium (Na), potassium (K), Chloride (Cl).
2.5 LDH Assay
Peripheral blood mononuclear cells (PBMC) were isolated from heparinized blood by Ficoll gradient centrifugation and cultured for 18 hours with or without Phytohemagglutinin (M Form, PHA) (Invitrogen). 14736 tumor cells were cultured as previously described (ref). Cells were plated at 1×103 to 5×104 cells per well and total LDH was determined using the Lactic Dehydrogenase based In Vitro Toxicology Assay Kit (Sigma Aldrich).
2.6 Statistical analysis
Blood and chemistry parameters were transformed into the log scale for data analysis. A one-sample t-test was used to assess whether the leukocyte and hematocrit counts were higher among the CML animals than the mean of the normal range under the assumption of unknown variance. A two-sample t-test was used to compare the distribution of LDH levels between the CML animals versus healthy controls under the assumption of unequal variances. The p-values were based on a two-sided hypothesis test and computed using Stata 7.0 (Stata Corp, College Station, TX).
2.7 Karyotype and PCR
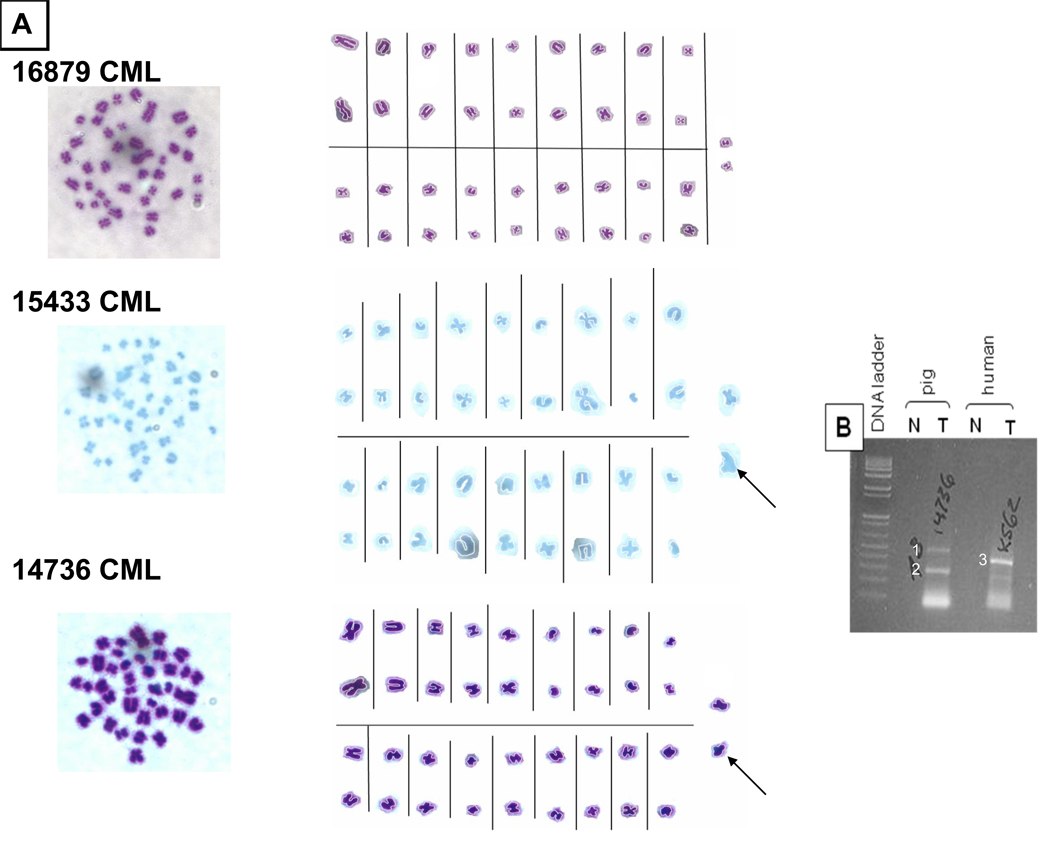
Karyotyping was performed based upon standard karyotyping protocols (bioProtocol, www.bio.com). In brief, 1 × 106 tumor cells were placed in 5ml of culture medium (RPMI with 10% fetal bovine setum) containing colchicine (1ug/ml) for 24 hours at 37°C in 25ml T-flasks. The cells were then harvested, washed with Hank’s Buffered Saline (HBSS), and placed in a hypotonic solution (75mM KCL) at 37°C for 12 minutes. Peripheral blood lymphocytes were stimulated in culture with PHA (55ul in 5ml containing 3 × 107 cells) for 24 hours prior to the addition of colchicine. The cells were then fixed and washed with a 3:1 methanol:glacial/acetic acid solution. The cells were then dropped onto microscope slides using a pasteur pipette and allowed to air dry. The slides were then stained with a Leishmann’s stain in Gurr’s buffer PH6.8 for 10 minutes. The slides were then washed with water, dried, and cleared with xylene. Cover slips were them mounted to the slides. Tumor cell lines derived from animals 14736 and 15433 were karyotyped and compared to normal healthy PBMCs (16879) (Fig 10A). The chromosome spreads were aligned by morphology.
Figure 10.
(A) Karyotype of CML lines 15433 and 14736. PBMCs from animal 16879 were used as a control. Left panel depicts chromosomes unarranged in the slides. Alignment of the chromosomes by morphology is shown in the middle panels. Photoshop was utilized to enhance the contrast between the chromosomes and the background. The two CML lines 15433 and 14736 had an asymmetric chromosome (solid arrow). (b) RNA from 14736 CML cells was assessed for BCR/ABL translocation through PCR (refer to materials and methods). A human CML line K562 was utilized as a positive control. Both swine and human tumors (T) were run in a gel with a normal (N) control of each corresponding species. Two bands (1,2) were observed in the PCR product of 14736 and one band (3) from K562 human CML. No bands were observed in the negative controls as expected.
Polymerase Chain Reaction (PCR)
RNA was isolated from the human and porcine PBL as well as from the porcine 14736 and K562 tumor cells with an RNAeasy Mini Kit (Qiagen) according to the manfacturer’s protocol. cDNA was transcribed with the Superscript III First Strand Synthesis System (Invitrogen). RT-PCR was performed with the pABL (5’-TGTTGACCGGTGTGATGTAGTTGCTTGG-3’) and pBCR (5’-ATAGCATCCCGCTGACCATCAACAAA-3’) primers. The reaction consisted of 1x buffer A (Fisher Scientific Co), 1uM of each primer, 200uM each dNTP (Fisher Scientific Co.) and 2.5U Taq polymerase (Fisher Scientific Co.) in a final volume of 50ul. The PCR cycle conditions were thirty cycles of 94°C for 30 seconds, 55°C for 30 seconds and 72°C for 45 seconds followed by 10 minutes at 72°C. The GAPDH RT-PCR reactions were done under the same conditions using primers 314 (5’-GGATTTGGTCGTATTGGGC-3’) and 315 (5’-TGAGCTTGACAAAGTGGTCG-3’) and thirty cycles of amplification. The PCR products were run on a 1.3% agarose gel.
3. RESULTS
3.1 History and Clinical Assessment
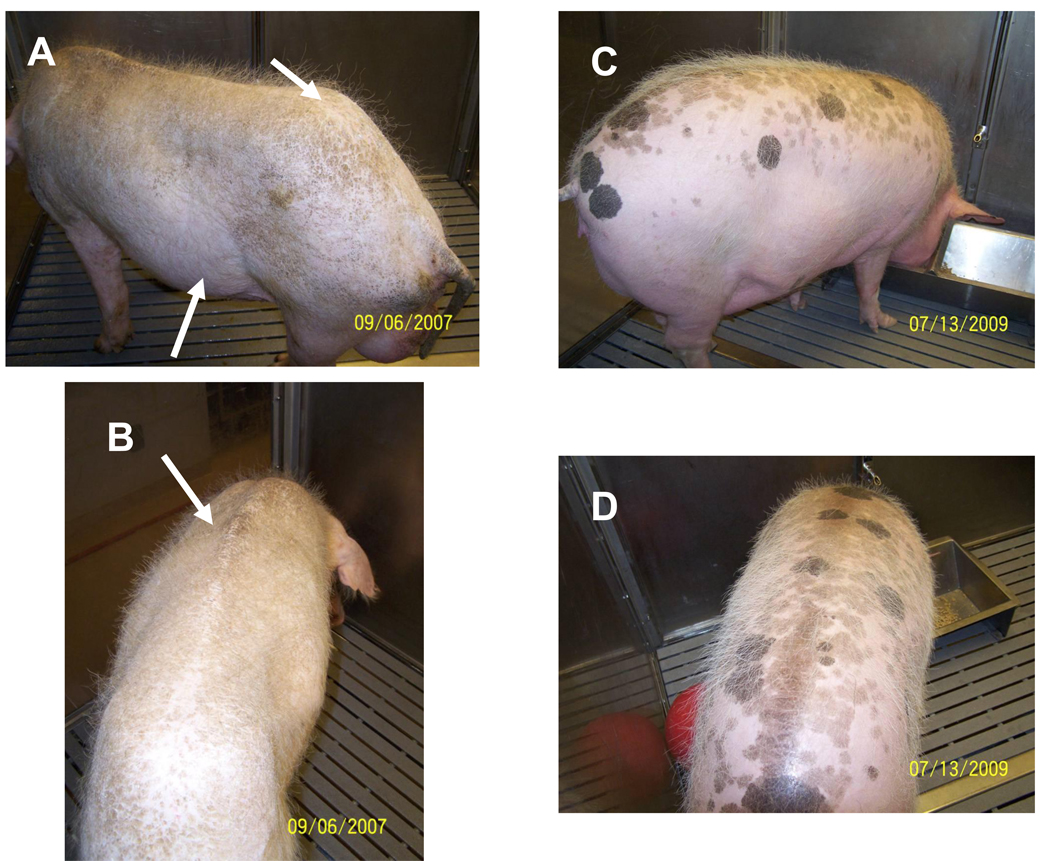
All animals reported were aged breeders (31–44 months old) (Table 1) which underwent regular blood and health screenings as described in section 2.1. Blood work and a physical exam were performed in lethargic/anorexic animals. Fecal exams were performed for the presence/absence of parasites. Abnormal tissues and suspicious lesions were sampled for histology. All five animals within our inbred SLAd miniature herd appeared thin (Figure 1 A,B). Both males (n=3) and females (n=2) were affected. All presented at our breeding facility with symptoms of lethargy and anorexia. During the onset of symptoms, the animals were observed. Non resolving weight loss and physical appearance of chronic weigh loss (as observed by prominent spinous processes and iliac crests Figure 1A–B) assessed by the farm veterinarian, led to further evaluation. On presentation animals 16228, 14736, 15433 and 16454 were pale. Animal 16228 presented tachycardic (heart rate of 190 (60–90 normal)), and also exhibited labored breathing. In addition, increased lung sounds compatible with lung disease and muffled heart sounds indicative of pleural/pericardial effusion was also documented in this same animal. A III/VI systolic heart murmur was ausculted in 16228. Animals 14736 and 16228 had diarrhea and abdominal effusion. These findings were confirmed by gross pathology. All animals presented with organomegaly. An enlarged abdomen is clearly visible in animal 16228 (Fig 1A) which exhibited a positive fluid wave when balloted. The presence of organomegaly and the non-specific signs and symptoms were compatible with a neoplastic process.
TABLE 1.
Generation(G) from point of inbreeding (brother-sister mating) in the SLAd line. We are currently in generation eleven (G11) of brother sister matings. All animals affected were over 30 months of age.
| Animal number | Date of Death |
Age(months) | Generation (G) |
|---|---|---|---|
| 12933 | 5/1/2001 | 44 | G5 |
| 14736 | 8/6/2004 | 38 | G8 |
| 15433 | 11/17/2005 | 37 | G9 |
| 16454 | 5/30/2007 | 31 | G10 |
| 16228 | 9/6/2007 | 42 | G10 |
Figure 1.
Animal 16228 shows abdominal enlargement (Fig 1A bottom arrow) and iliac crest prominence (Fig 1A- top arrow). The spinous processes are also visible in this animal (Fig 1B). These findings document the chronic weight loss exhibited in animal 16228. A healthy age and weight matched animal is shown in Fig 1c&d‥
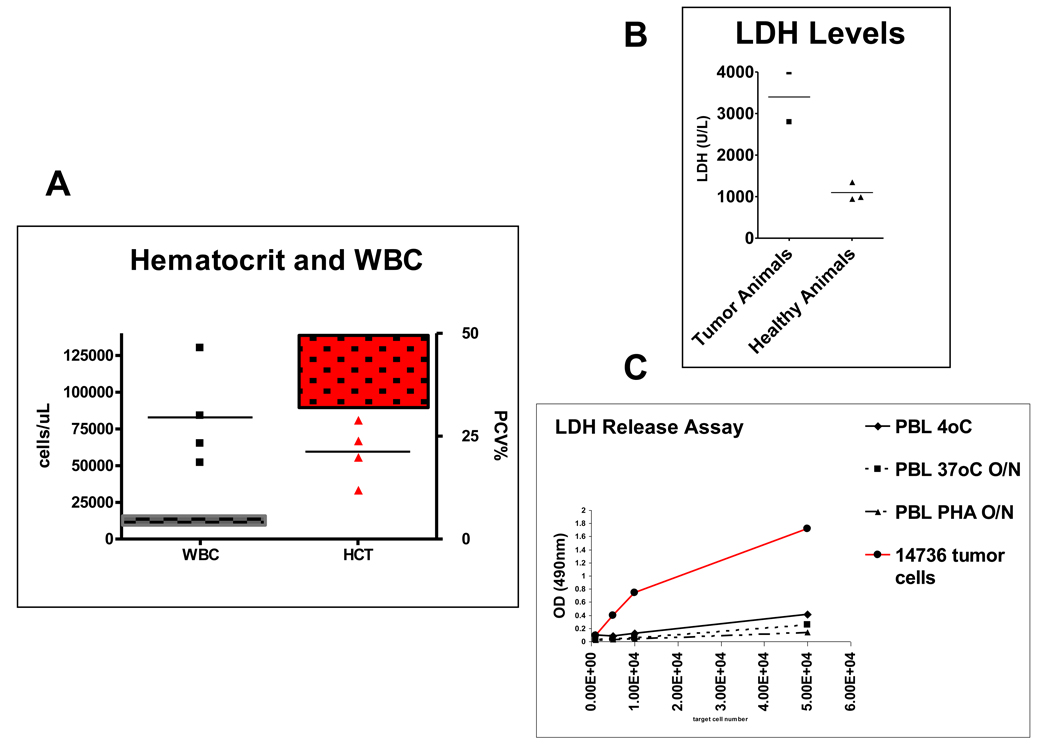
3.2 Severe leukocytosis, anemia and increases in lactate dehydrogenase
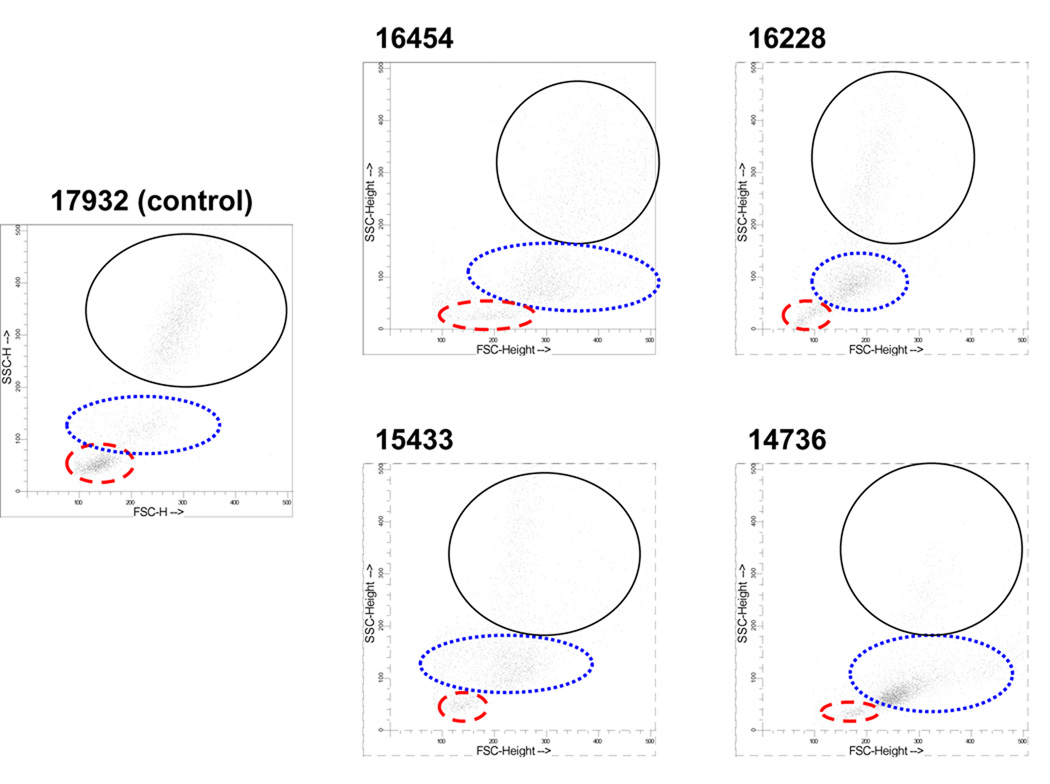
Complete blood counts and peripheral blood smears were obtained from the affected animals. Severe leukocytosis (p<0.001) with a mild to moderate anemia (p=0.034) (Figure 2) was identified in all animals. LDH levels were increased in the two animals in which it was tested (16228 and 16454) (Fig 2B) (p=0.042). In addition, when LDH was tested in a tumor cell line derived from animal 14736, it exhibited higher LDH levels when compared to naïve or PHA blasted naïve cells (Fig 2C). Flow cytometric analysis, showed an abnormal (increased) percentage of myeloid lineages based on forward and side scatter profiles when compared to naïve healthy control animals. The granulocyte lineages and the monocytes (Fig 3) had increased cellularity and the absolute leukocyte counts were above normal (Fig 3 and table 2). Peripheral blood smears showed the presence of crenation and hypochromia. Pyknotic cells were also observed. Abnormal leukocytes (Fig 4A) of immature and blast-like appearance were observed in the peripheral blood smears. Some of the cells were bi-nucleated. Immature myeloid cells and eosinophils at various stages of maturity were also present (Fig 4A). A monocyte rich cellular fluid collected from the ascites from animal 14736 was observed (Fig 4B).
Figure 2.
Severe leukocytosis (dots) was observed in SLAd animals with myeloid leukemia (2a) (p<0.001). Normal leukocyte range is shown in left box and normal hematocrit in right box (Fig 2a). All leukemic animals exhibited moderate to severe anemia (p=0.034). Only two of the animals presenting with CML, 16228 and 16454, were tested for serum LDH levels prior to the time of autopsy (2b) (p=0.042). Both had a marked increase in LDH. Immortalized tumor cells derived from animal 17436 had an increased LDH production when compared to fresh or PHA blasted PBMC for 24 hours (2c).” Note: the normal ranges (in parenthesis) for all values have been normalized from hundred of animals. We show several healthy controls in LDH graph as a comparison to the affected animals.
Figure 3.
Flow cytometry of four affected SLAd animals. Forward scatter versus side scatter can be compared to a healthy aged inbred SLAd control animal (17932). Increased events are observed in the scatter plot in the monocyte area (dotted) and the granulocyte area (solid). Lymphocytes are located in the dashed area.
TABLE 2.
Absolute and Percent Leukocyte Populations in the Peripheral Blood
| Animal Number |
WBC ×103 cells/uL |
% lymphoid |
% monocytes |
% granulocytes |
Absolute Lymphocytes ×103 cells/uL |
Absolute monocytes ×103 cells/uL |
Absolute granulocytes ×103 cells/uL |
|---|---|---|---|---|---|---|---|
| (11–22) | (38–62) | (2–10) | (28–62) | (4.3–13.6) | (0.2–2.2) | (3.2–13.4) | |
| 14736 | 130 | 8 | 75 | 15 | 10.4 | 97.5 | 19.5 |
| 15433 | 52 | 12 | 45 | 37 | 6.5 | 23.5 | 19 |
| 16454 | 84.62 | 15 | 44 | 39 | 12.7 | 37.2 | 33 |
| 16228 | 65 | 12 | 48 | 40 | 7.8 | 31.2 | 26 |
| 17932 | 18.2 | 34 | 12 | 49 | 6.1 | 2.14 | 8.9 |
WBC counts of affected animals were categorized into either the lymphocyte, monocyte or granulocyte populations. Both their % and absolute numbers are depicted above. In parenthesis the normal swine values are shown. Leukemic animals demonstrate a significant leukocytosis in the monocyte and granulocyte lineages. 17932 is a 2 year old inbred healthy SLAd adult breeder control animal for comparison.
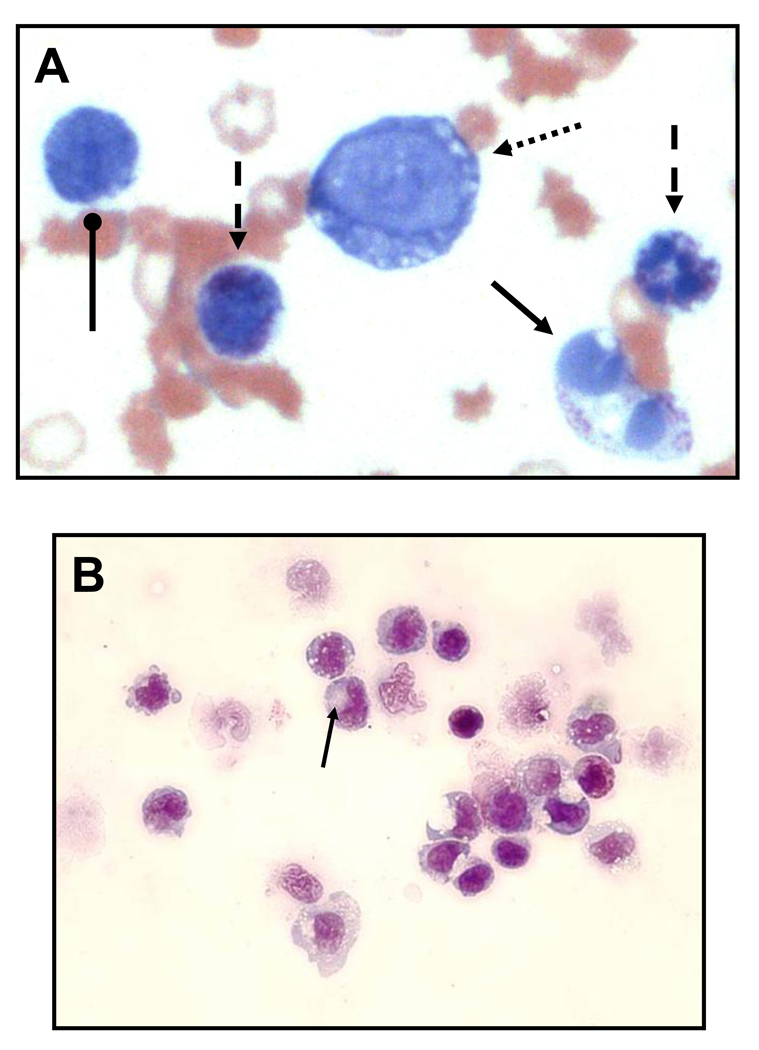
Figure 4.
(a) Representative blood smear (animal 16228). Crenation, hypochromia and some pyknotic cells were observed. Abnormal leukocytes (Fig 4A–B) of the myeloid lineage were present. Some of these cells appeared immature (dotted arrow) and blast-like. Bi-nucleated cells (solid arrow) were observed. Immature myeloid cells with an abundance of cytoplasm (dashed arrows) and eosinophils at different stages of maturity were also present (rounded head arrows). (b) Cells (monocytes) from ascites were moderately larger in size, had a gray blue basophilic cytoplasm, an increased N:C ratio and were vacuolated . A clear area in the cytoplasm, representing the Golgi zone, was observed in some of the cells (arrow).
3.3. Gross Pathology consistent with a leukemic process
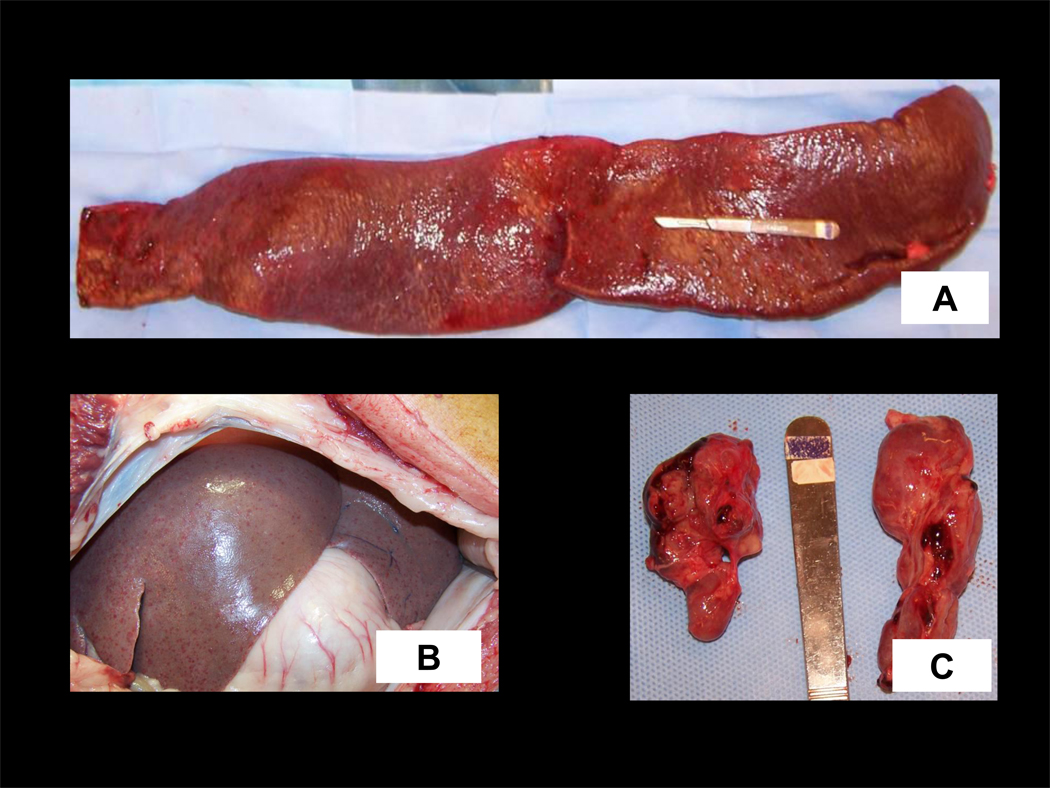
Gross pathology was performed to further support the evidence of a leukemic process. As previously noted, organomegaly (Fig 1) was observed in all animals. Ballottement of the abdomen showed a clear fluid wave in animal 16228 and abdominal effusion was severe in two (16228 and 14736). The quality of the abdominal effusion observed was hemorrhagic (16228) and cloudy and straw-colored for 14736. The most remarkable finding was hepato-splenomegaly in all affected pigs (Fig 5A,B). In animal 16228, the omentum was adhered to the spleen, suggesting possible splenic hemorrhage. In this animal the liver and splenic weights were measured. A weight of 4.7 kg (4.7% total body weight (TBW)- normal is 1.7% (TBRC miniature pig references)) and 3.7 kg (3.7% TBW-normal is 0.12% (personal communication MSA Kumar Tufts University School of Veterinary Medicine-professor of anatomy)) were respectively recorded. Weights were not recorded for the other four animals. On appearance they were pale and firm compared to normal tissue. The bone marrow was abnormally pale as assessed by sternal biopsy taken for in vitro culture of the tumor. Moderate/severe enlargement of the mesenteric and or mediastinal lymph nodes was also observed in affected animals (16228, 14736, 15433). The livers of animals 14736, 12933 had small widespread nodules on gross necropsy.
Figure 5.
Liver and spleen gross appearance of affected animals. All organs shown are enlarged. Spleen (a,), liver (b). Animal 16228 (a,) and 16454 (b). Animal 16454’s liver exhibited small hemorrhagic foci (b). A piece of the spleen in (a) were removed for tissue culture prior to the taking of the photographs.
Besides the enlarged liver, spleens and lymph nodes in the mentioned animals, other gross findings included, pericardial effusion (n=3) and pleural effusion (n=2). The pericardium was thickened with evidence of inflammation in one animal, while two other animals had lesions on the outside surface of the heart. Adhesions involving the large and small bowel in pig 14736, and the spleen of 16228 were recorded.
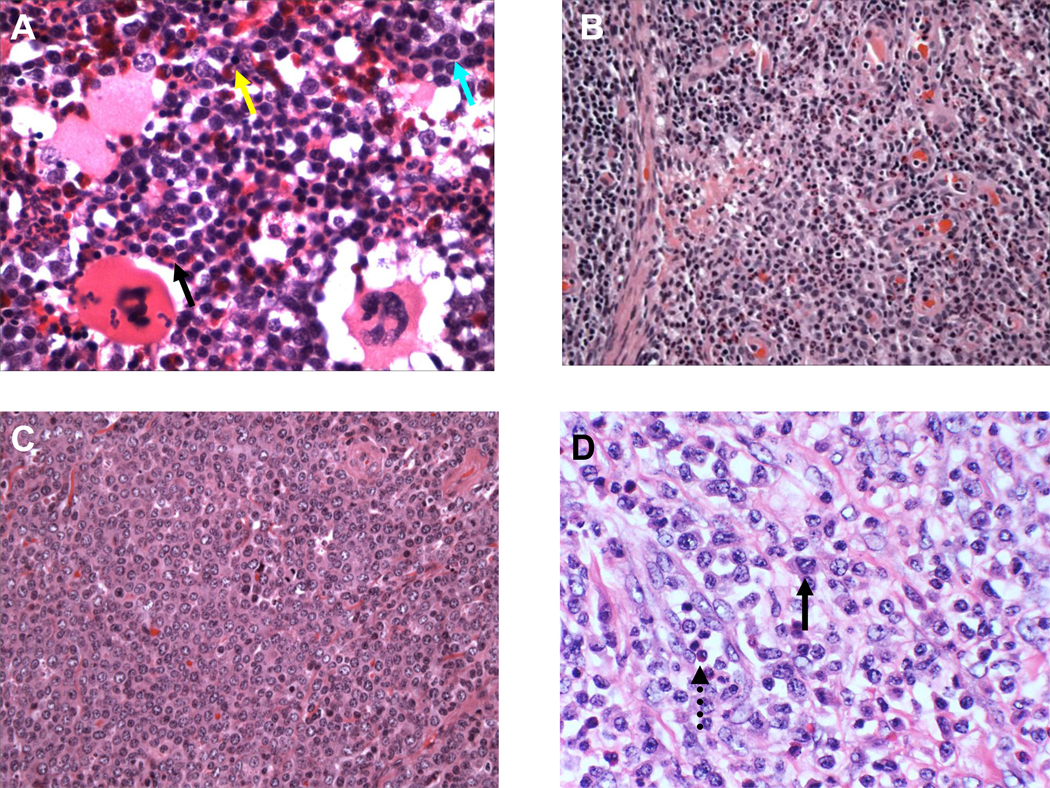
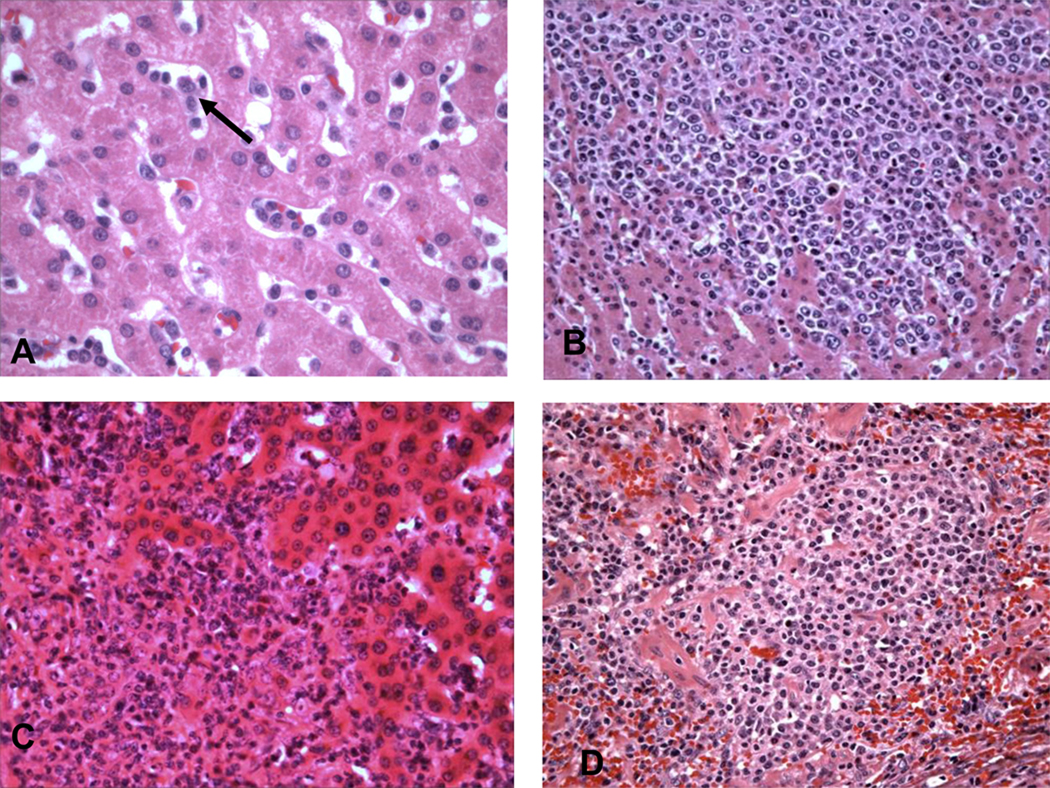
3.4 Histopathology is consistent with an invasive myeloid population
Tissues harvested for histopathological assessment are listed in Table 4. No fibrosis nor megakaryocyte proliferation was observed in the bone marrow samples. The myeoid:erythroid ratio was elevated in the BM (>3:1 M:E ratio). (Figure 6A). Affected animals had a low number of metarubricytes (yellow arrow). Increased number of eosinophils and of myeloid precursors were also observed in the marrow. Infiltrations of malignant cells were observed in the lymph nodes (Fig 6B), and kidneys (data not shown). Monocytes and eosinophils were observed infiltrating the gastrointestinal tract in two animals (Fig 6 C&D). The liver sinusoids were enlarged and an infiltrate of myeloid cells was observed (Fig 7 A–C). Cellular infiltrates with a moderate amount of eosinophils were visible in the spleen (Fig 7D). Destruction of normal follicular architecture in the spleen was noted, with the presence of fibrosis. In all these cases the presence of round cells were responsible for the organ enlargement with a predominance of monocytes and a significant amount of eosinophils. No parasitic infection was identified in any of the reported animals.
TABLE 4.
SAMPLES HARVESTED FOR HISTOPATHOLOGY
| Organ | Animal number | ||||
|---|---|---|---|---|---|
| 14736 | 15433 | 16454 | 16228 | 12933 | |
| Bone Marrow | Y | Y | Y | Y | |
| Lymph node | Y | Y | Y | Y | Y |
| Kidney | Y | Y | Y | ||
| Large Intestine | Y | Y | |||
| Small Intestine | Y | Y | |||
| Liver | Y | Y | Y | Y | Y |
| Thymus | Y | Y | Y | ||
| Heart | Y | Y | Y | Y | Y |
| Spleen | Y | Y | Y | Y | Y |
| Lung | Y | Y | Y | Y | Y |
| Stomach | Y | ||||
Table 4 documents all the organs harvested from the affected pigs for histopathological analysis.
Figure 6.
(a) The yellow arrow depicts a normal erythroid precursor (matarubricyte). The black and blue arrows show myeloid cells (black arrow eosinophil and blue arrow monocyte lineage). There is a mild-moderate increase of the myeloid:erythroid ratio. (b)Infiltrations of malignant cells were observed in the lymph nodes (animal 14736). (c,d) Monocyte (black solid arrow) and eosinophils (black doted arrow) are observed infiltrating the small intestine (c) and stomach (d) in animals 14736 and 12933.
Figure 7.
(a–c) Livers from animals 14736, 16454, 16228. The presence of monocytes infiltrating the liver sinusoids (black arrow) is observed. Spleen from animal 14736 (d) also shows severe infiltration of myeloid cells. A moderate amount of eosinophils were observed in the spleen. Destruction of normal follicular architecture in the spleen was noted.
3.5 A myeloid phenotype confirms chronic myelogenous leukemia in the affected swine
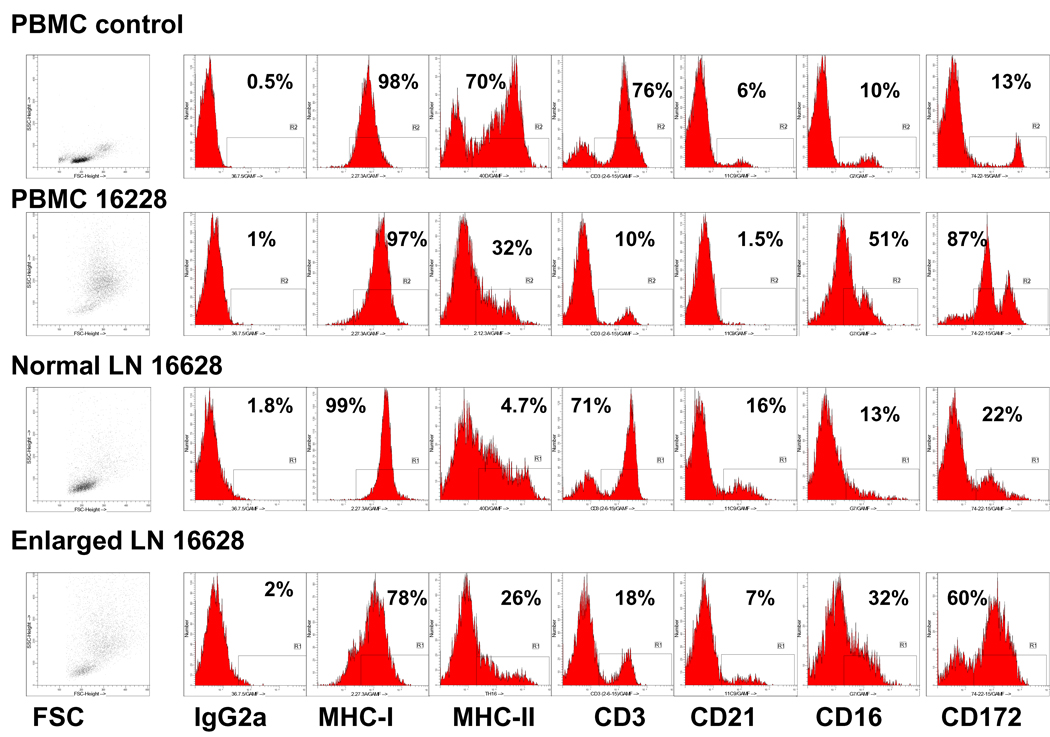
In order to assess the origin of the neoplastic cells, peripheral blood and tissues were analyzed by surface staining and flow cytometry. Although, the size and granularity of all the peripheral blood cells based on a forward scatter (FSC) versus side scatter (SSC) profile (Figure 2) were consistent with an expansion of cells deriving from the myeloid lineage, immature lymphoid (B or T cell of origin) blasts/immature cells also have increased size and granularity and can overlap with the monocyte/granulocyte regions. We used a panel of available porcine cell surface markers (materials and methods section 2.4), to distinguish the lineage of these malignancies based on phenotype. These cells stained positively for MHC class I and demonstrated heterogeneous staining for MHC class II. Most importantly, and depicted in Figures 8 and 9, a high proportion of the PBMCs stained positive for the myeloid markers CD16 and CD172a (Fig 8 and Fig 9A). These cells corresponded to the abnormal tumor cells (micrographs from the smears from Figure 4). When compared to a normal control (Fig 8-PBMC control), PBMC derived from affected animals had relatively few cells that were positive for T-cell markers such as CD3, CD4, CD5, CD8 and B cell markers such as CD21, anti-mu- heavy chain, and surface anti-kappa light, ruling out by phenotype lymphoid neoplasms of either T or B cell origin. Figure 8 shows the phenotype of the cells isolated from two separate lymph nodes taken from animal 16228 at autopsy. One lymph node appeared normal and one was greatly enlarged. Lymph nodes are organs which are lymphocyte rich and largely devoid of myeloid cells. Our analysis demonstrates that the cell population which phenotypically dominated the histogram in the affected (enlarged) lymph node was of a myeloid phenotype. The T cell component was 18% (CD3 marker) in the enlarged LN while the normal-sized LN had over 70% T-cells.
Figure 8.
The peripheral blood mononuclear cells, an enlarged lymph node and a normal sized lymph node (used as internal control) of animal 16228 is shown. PBMCs from a healthy animal used as control at the time 16228 was analyzed is also shown. The PBMCs and enlarged lymph node from animal 16228 clearly have an overpopulation of myeloid cells positive for the CD16 and CD172 myeloid markers. The % of T cells represented by the CD3 surface marker is clearly decreased in both the enlarged lymph node and the PBMCs of 16228 when compared to the control PBMCs or the normal sized lymph node. These same differences are observed, though at a lesser degree, with the B cell population stained for CD21.
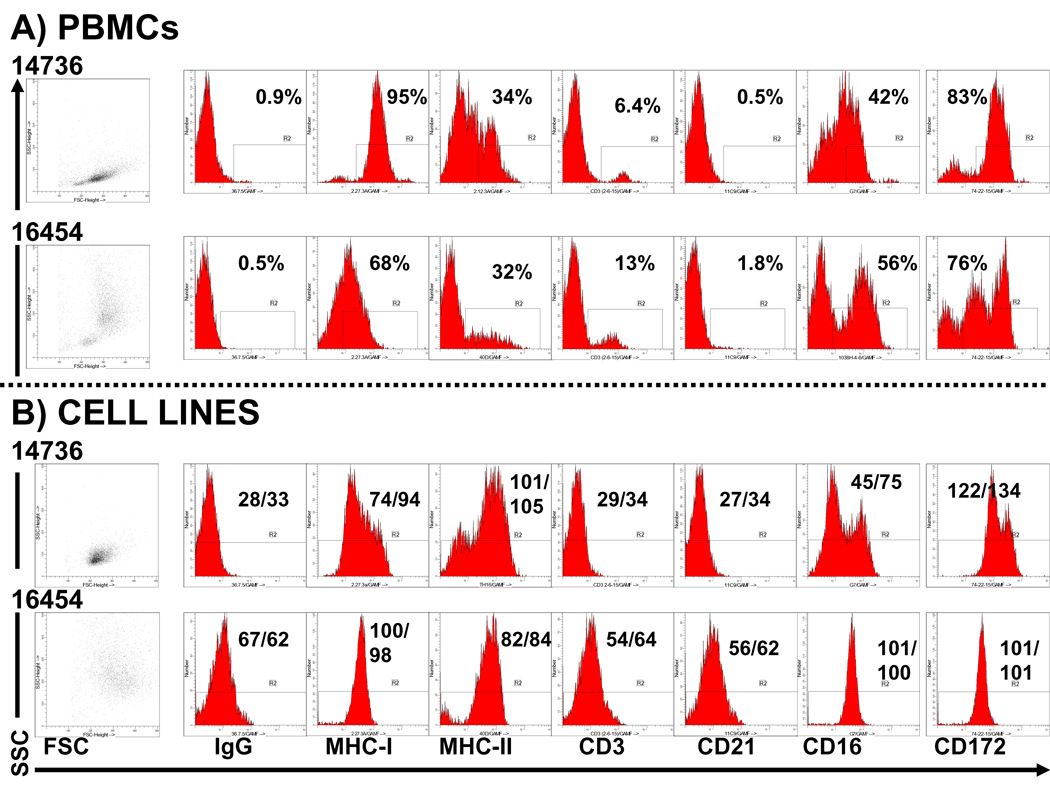
Figure 9.
We compare the immunophenotype between the PBMCs of animals 14736 and 16454 at time of euthanasia with their established tumor cell lines which have been immortalized and passaged in vitro for at least 6 months. The % positivity of every cell surface marker is depicted with the PBMCs as more than one population (lineage) of cells is present. The tumor cell lines did retain the myeloid phenotypic markers CD16 and CD172 while the lymphoid markers CD21 and CD3 were absent. Both tumor cell lines were positive for MHC-I and MHC-II. Differences in the expression of class I and II were observed in the PBMCs. The immortalized cell lines were analyzed using the mode/mean fluorescence intensity of the surface markers as a more homogeneous population is expected. The mean and mode fluorescence intensity is depicted while assessing the tumor cell lines (b).
We have attempted to generate tumor cell lines from tissues from the affected leukemia bearing animals. Fig 9B demonstrates two tumor cell lines from CMLs from animals 14736 and 16454. These cells have been successfully passaged for over 6 months. Figure 9B documents that these cells have maintained the original myeloid (CD16, CD172) phenotype.
Based on the described phenotype in combination with the clinical history, blood smears, gross and histopathological data, these animals were diagnosed with a chronic myeloid leukemia.
3.6 An increase incidence of myeloid leukemias in the SLAd herd compared to humans
In a review of our database, the incidence of spontaneous myeloid leukemias in adult naïve SLAd animals from the fifth generation (G5) to the tenth generation (G10) (table 3) has shown that animals greater than or equal to 24 months of age and unassigned to an experimental protocol had an incidence of 7.4% (5/67). Since most animals in our herd do not reach this age due to their use for transplantation, only these animals were considered relevant for comparison. If we included all animals born within these generations, a 2.3% incidence has been observed. Despite the low numbers of pigs, the incidence evidenced in our swine herd is much higher than what has been documented in the human literature, with 1/100,000 adults developing CML (Fletcher 2000).
Table 3.
Incidence of CML in our SLAd inbred miniature herd per generation
|
Generation (G) |
Number affected |
Total Number animals/ generation |
Number of animals >2 years old/ generation |
||
|---|---|---|---|---|---|
| G5 | 1 | 17 | 8 | ||
| G8 | 1 | 46 | 23 | ||
| G9 | 1 | 57 | 18 | ||
| G10 | 2 | 66 | 18 | ||
| % affected | % affected | ||||
| TOTAL | 5 | 186 | 2.6% | 67 | 7.4% |
Table 3 illustrates the overall incidence of myeloid leukemia per generation (G). These are compared to the overall number of animals per generation that have been bred (3rd column) and the total of animals in the colony over 2 years of age (5th column). Animals under two years of age have been utilized in transplantation studies and have not died of natural causes.
3.7 Chromosomal and molecular characteristics of swine CML compared to healthy animals
Tumor cell lines derived from animals 14736 and 15433 were karyotyped and compared to normal healthy PBMCs (16879) (Fig 10A). The chromosome spreads were aligned by morphology. Both 14736 and 15433 had one pair of chromosomes that did not match. They were asymmetrical and indicated either the possible loss or gain of a large portion of a chromosome arm. We then performed a PCR using BCR-ABL gene specific primers to determine if the genetic change responsible for the spontaneously derived tumor found in pig 14736 (and possibly other pigs) was the same as or similar to that observed in chronic myelogenous leukemia (CML) in humans. We were specifically looking for a swine Ph+ chromosome like translocation, which is observed in most cases of human CML. Sequences surrounding the known chromosomal breakpoint of the BCR and ABL genes in the human K562 CML cell line, were compared to the available porcine or bovine sequences to identify conserved regions for primer design. Primers were designed such that a product would only be generated if this specific translocation had occurred resulting in the production of a fusion protein. PCR was performed with these primers using cDNA from a tumor cell line derived from the bone marrow of a pig with the CML-like tumor (14736) (2) as the template. cDNA from the K562 cell line, which is known to express the Philadelphia chromosome translocation (3), was included as a positive control. Normal human and porcine peripheral blood lymphocytes (PBL), served as the negative controls. Faint bands were observed with both the porcine and human tumors following 30 cycles of amplification while there was no detectable signal in the normal samples (Fig 10 B). After an additional 20 cycles of amplification, two bands of approximately 300 and 500 nucleotides were detected in the pig tumor sample (Fig10 B). A single distinct band of 450 nucleotides was present in the K562 sample, as was expected for the amplification of the human BCR-Abl fusion product. No PCR products were generated in the normal porcine and human PBL controls.
Discussion
CML is typically a disease of older animals, documented in the canine and feline population (Goldman and Graham 2000; Jacobs et al. 2002; Joiner et al. 1976; Leifer et al. 1983). Manifestations of disease are often slow and non-specific. Symptoms such as fatigue, lethargy, loss of appetite, and weight loss are commonly observed. A similar clinical picture was observed in our miniature swine at time of disease presentation. A diagnosis of CML is challenging in pigs due to the absence of clear genetic markers, therefore a thorough and often extensive workup was necessary to confirm the diagnosis. A leukemoid reaction was ruled out as no other infectious/inflammatory agents were identified to be responsible for the leukocytosis. All the animals reported here were important breeders within our MGH MHC-defined miniature swine herd and a diagnostic workup was performed for the treatment of their condition. Once leukemias were identified with an incidence higher than expected, we instituted a protocol for their diagnosis with the goal to harvest them, and develop tumor cell lines for the study of leukemias. We have not observed myeloid leukemias in young pigs which is consistent with reports of chronic leukemias in other domestic species (Messick J.B. 2000; Vernau and Moore 1999). In humans, the term chronic myeloid leukemia covers a heterologous group of conditions. However, over 90% (Fletcher CDM) of these CMLs fall into a group that is characterized genetically by the presence of the Philadelphia (Ph) chromosome. The oncogene ABL fuses with BCR (from chromosome 22) and the BCR-ABL hybrid gene functions as a protein kinase and it has a major role in leukemogenesis. There is a small population of human CMLs that lack the Ph chromosome (Ph−). In these cases, the tumors are morphologically indistinguishable from Ph+ CMLs. The absence of this genetic marker, makes the diagnosis more difficult and requires an extensive workup (similarly to what occurs to veterinary species where the Ph+ chromosome has yet not been documented). Both in the human and veterinary species there is a marked increase of the WBC counts and a concominant mild/moderate anemia (Fletcher 2000). Monocytes and neutrophil myelocytes are the two most represented and commonly elevated cell lines. Flow cytometric analysis confirmed that our animals developed a leukemia with a myeloid phenotype. Demonstration of an increased population of cells that are CD172+, CD16+, and negative for either T (CD3) or B (CD21) cell markers identified these neoplasias as of myeloid of origin. Normal animals have >50% lymphocytes in their peripheral blood. The percent lymphocytes in the peripheral blood from affected animals were significantly decreased as the myeloid lineages were expanding (Table 2). These same cells were over-represented in the enlarged lymph node (Fig 8) from animal 16228. It is possible that the normal lymph node may have developed cytotoxic T cells to control the neoplastic cells or had yet not been infiltrated.
The degree of basophilia and eosinophilia in humans with CMLs tend to be quite marked with most of the cases exhibiting an increase of basophils and 80% develop an absolute eosinophilia (Fletcher 2000). This was also observed in our pigs where these granular cells of myeloid origin were elevated. The eosinophilia could be confused with eosinophilic leukemia (EL) or idiopathic hypereosinophilic syndrome (HES). EL is a very rare disease, most commonly reported in cats in the veterinary literature (Messick J.B. 2000). EL may exhibit both mature and immature eosinophils in the peripheral blood and a significant amount of eosinophil precursors are observed in the bone marrow. However in EL, the eosinophils are the cell line that predominates in the hematogram. Though we do not have specific eosinophil markers in the pig, histopathology and cytology were not concordant with EL. In addition, conditions capable of directly or indirectly inducing an eosinophilia such as parasites, eosinophilic granulomas or mast cell tumors were not identified. The anemia in affected pigs can be explained by the increased expansion of myeloid precursors in the marrow with a shift of erythroid:myeloid ratio, thus causing a gradual decrease of RBCs. These slow changes are observed in chronic leukemias not only in domestic species but also in humans suffering from CMLs where they tend to have a mild to moderate anemia in addition to the leukocytosis (Perkins P 2000). The hematogram parameters of all of our leukemic animals were outside the normal documented ranges (table 2), are statistically significant, and are compatible with a hematological malignancy.
LDH is a common marker that is utilized in the clinic to support the diagnosis of a hemolymphatic neoplasia (Kabutomori et al 2007). In the veterinary domestic population LDH has been reported in animals with lymphoma (Duncan J.R. et al. 1994). Interestingly, these elevations in LDH are not found in leukemoid reactions (Duncan J.R. et al. 1994). Though serum LDH is a non-specific enzyme that may be elevated with muscle, liver or kidney damage, it’s increase in lymphomas and leukemias may be acute. We did observe a statistically significant increase in the serum levels from the only two (tumor bearing) pigs tested for LDH. In addition, an animal that developed post-transplant proliferative disease (lymphoma) exhibited an acute elevation of LDH prior to the acute increase of the WBC count (manuscript in preparation). To further support the rationale of using LDH as a valuable diagnostic test in the diagnosis of CML, the tumor cell line 14736 (expanded and immortalized in culture) produced more LDH than fresh PBMCs. As in human CML, LDH is a valuable marker to differentiate a neoplastic process from a leukemoid reaction in pigs.
The gross pathology findings correlate with what is commonly reported in humans. These include hepatosplenomegaly due to cellular infiltration, increased myeloid:erythroid ratio in the BM, minimal dyshematopoietic features in the myeloid and erythroid lineages, and enlarged lymph nodes (Fletcher 2000; Joiner et al. 1976). Because the animals presented significantly sick they were promptly and humanely euthanized once the condition was diagnosed. Since these animals were not followed or treated for their neoplasias, we did not have an observation period in which a blast crisis could have occurred. Because prey animals tend not to exhibit any signs of weakness until very sick, the late stage organ involvement may be simply a consequence of a late diagnosis. Humans, in general, are diagnosed earlier when the patient complains of weakness and lack of energy, and thus initial diagnosis with multiorgan involvement is not as common.
While it is possible that the porcine leukemias may have a chromosomal translocation similar as in human CML, at this point in time we are unable to document it. Although the difference in chromosome numbers between pig (19 pairs) and human (23 pairs) make the 9→22 translocation in the pig impossible, a mutation or translocation affecting tyrosine kinase unction (as in humans) may be responsible for the porcine leukemias. Karyotype of cell lines 14736 and 15433 suggest an abnormal/asymmetrical arm in one of the chromosomes. Restriction enzyme analysis targeting a homologous human/bovine BCR and ABL gene has shown the presence of two bands in 14736, the only tested porcine cell line. This band is absent in normal PBMCs and sequencing is currently being performed. As there are no clear porcine BCR or ABL gene sequences that have been identified at this time, it is impossible to predict if the dominant translocation resulting in human CML is also present in the pig. It is conceivable that the most common translocation in porcine CML may be one of the rare translocations observed in humans or one that either does not occur or has not yet been documented in humans. In any of these cases, identifying the translocation responsible for porcine CML will be challenging. We must also mention, that it is conceivable that instead of a translocation, our CMLs may have acquired a mutation in genes modulating tyrosine kinases. A brief report documenting a leukemic blast crisis in a non-inbred SLAd sow provides further support for the existence of a genetic linkage in the MHC-defined pigs that is associated with hematopoietic neoplasias (Sipos et al. 2006). In addition, spontaneous development of a CML in an SLAh haplotype (SLAd in MHC-II and SLAa in the MHC-I- data not shown) pig of our herd may indicate that the CML mutation/translocation may be found in the gene coding for the MHC-II molecule. Through selective breeding to maintain pigs homozygous for the MHC-II gene, a genetic trait responsible for the leukemias may also have been selected, similar to that previously reported in pigs developing lymphoma (McTaggart et al. 1971).
Though there is some controversy about the best animal to model human disease, there is a very large body of information where the pig is considered a very good model, specifically the miniature swine, as their organs (when adults) are similar in size as observed in an adult human (Laber et al. 2009; Swindle 2009). Pigs are very valuable for the study of cardiovascular, nutritional, gastrointestinal and transplantation research. They are considered good animal models because of their similarities in anatomy and physiology to humans. We do however recognize that pigs are not the one and only model. All animal models have their value in biomedical research and their utility depends on the question being investigated.
In summary, spontaneous hematologic malignancies have been observed previously in large animal models, including swine, but have often been broadly classified (Bostock and Owen 1973; Fisher and Olander 1978; Kadota et al. 1984; Kadota et al. 1987; Kashima et al. 1982; Marcato 1987). We now report the development of a spontaneous leukemia in MGH MHC defined miniature swine. Taking into consideration the clinical presentation, flow cytometry, gross pathology and histopathology, we have diagnosed all of these cases as chronic myelogenous leukemias. Some of these tumors have been successfully established as in vitro cell lines and are candidates to become the first leukemias to be utilized as transplantable tumors in inbred and MHC-defined large animals. Thus, inbred sublines of MGH MHC-defined miniature swine and established porcine tumors may provide useful preclinical translational models to study immunotherapeutic approaches to treat human leukemia.
Acknowledgments
The project described was supported by Award Number K01RR024466 (RDS) from the National Center for Research Resources, and the 1P01CA111519-01-A1 (CAH) from the National Cancer Institute.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Allsup TN, Wells GA, Stevenson RM. Myeloid leukosis in a piglet. Vet. Rec. 1981;108:231–232. doi: 10.1136/vr.108.11.231. [DOI] [PubMed] [Google Scholar]
- Boersma WJ, Zwart RJ, Sinkora J, Rehakova Z, Haverson K, Bianchi AT. Summary of workshop findings for porcine B-cell markers. Vet. Immunol Immunopathol. 2001;80:63–78. doi: 10.1016/s0165-2427(01)00279-3. [DOI] [PubMed] [Google Scholar]
- Bostock DE, Owen LN. Porcine and ovine lymphosarcoma: a review. J Natl Cancer Inst. 1973;50:933–939. doi: 10.1093/jnci/50.4.933. [DOI] [PubMed] [Google Scholar]
- Davis WC, Marusic S, Lewin HA, Splitter GA, Perryman LE, McGuire TC, Gorham JR. The development and analysis of species specific and cross reactive monoclonal antibodies to leukocyte differentiation antigens and antigens of the major histocompatibility complex for use in the study of the immune system in cattle and other species. Vet. Immunol. Immunopathol. 1987;15:337–376. doi: 10.1016/0165-2427(87)90005-5. [DOI] [PubMed] [Google Scholar]
- Denham S, Zwart RJ, Whittall JT, Pampusch M, Corteyn AH, Bianchi AT, Murtaugh MP, Parkhouse RM, Tlaskalova H, Sinkora J, Sinkora M, Rehakova Z. Monoclonal antibodies putatively identifying porcine B cells. Vet. Immunol Immunopathol. 1998;60:317–328. doi: 10.1016/s0165-2427(97)00108-6. [DOI] [PubMed] [Google Scholar]
- Duncan JR, Prasse KW, Mahaffey EA. Muscle. 3rd. 1994. pp. 184–187. [Google Scholar]
- Fisher LF, Olander HJ. Spontaneous neoplasms of pigs--a study of 31 cases. J Comp Pathol. 1978;88:505–517. doi: 10.1016/0021-9975(78)90004-x. [DOI] [PubMed] [Google Scholar]
- Fletcher CDM. Tumors of the hemopoietic system; Chronic myeloid leukemia. 2000. pp. 1327–1329. [Google Scholar]
- Goldman EE, Graham JC. Clinical Diagnosis and management of acute non-lymphoid leukemias and chronic myeloproliferative disorders. 5th. 2000. pp. 706–714. [Google Scholar]
- Goldman EE, Graham JC. Clinical Diagnosis and Management of Acute Nonlymphoid Leukemias and Chronic Myeloproliferative Disorders. 2000. pp. 706–716. [Google Scholar]
- Hammerberg C, Schurig GG. Characterization of monoclonal antibodies directed against swine leukocytes. Vet. Immunol. Immunopathol. 1986;11:107–121. doi: 10.1016/0165-2427(86)90092-9. [DOI] [PubMed] [Google Scholar]
- Huang CA, Fuchimoto Y, Scheier-Dolberg R, Murphy MC, Neville DM, Jr, Sachs DH. Stable mixed chimerism and tolerance using a nonmyeloablative preparative regimen in a large-animal model. J Clin Invest. 2000;105:173–181. doi: 10.1172/JCI7913. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Huang CA, Lorf T, Arn JS, Koo GC, Blake T, Sachs DH. Characterization of a monoclonal anti-porcine CD3 antibody. Xenotransplant. 1999;5:201–212. doi: 10.1034/j.1399-3089.1999.00022.x. [DOI] [PubMed] [Google Scholar]
- Ivanoska D, Sun DC, Lunney JK. Production of monoclonal antibodies reactive with polymorphic and monomorphic determinants of SLA class I gene products. Immunogenetics. 1991;33:220–223. doi: 10.1007/BF01719247. [DOI] [PubMed] [Google Scholar]
- Jacobs RM, Messick JB, Valli VE. Tumors of the Hemolymphatic System. 2002. pp. 119–198. [Google Scholar]
- Jemal A, Siegel R, Ward E, Murray T, Xu J, Thun MJ. Cancer statistics, 2007. CA Cancer J Clin. 2007;57:43–66. doi: 10.3322/canjclin.57.1.43. [DOI] [PubMed] [Google Scholar]
- Joiner GN, Fraser CJ, Jardin JH, Trujillo JM. A case of chronic granulocytic leukemia in a dog. Can. J Comp Med. 1976;40:153–160. [PMC free article] [PubMed] [Google Scholar]
- Kabutomori O, Kanakura Y, Iwatani Y. Characteristic changes in platelet-large cell ratio, lactate dehydrogenase and C-reactive protein in thrombocytosis-related diseases. Acta Haematol. 2007;118:84–87. doi: 10.1159/000105167. [DOI] [PubMed] [Google Scholar]
- Kadota K, Akutsu H, Saito M, Kudo T, Gotoh K. Ultrastructure of swine myelogenous leukaemic cells, with particular reference to intracytoplasmic granules. J Comp Pathol. 1987;97:401–406. doi: 10.1016/0021-9975(87)90018-1. [DOI] [PubMed] [Google Scholar]
- Kadota K, Yamazaki M, Ishino S, Nei T. Ultrastructure and C-type particles in myeloid leukemia of a pig. Vet. Pathol. 1984;21:263–265. doi: 10.1177/030098588402100225. [DOI] [PubMed] [Google Scholar]
- Kashima T, Nomura T, Arai S, Nomura Y, Tsuchiya T, Saito Y. A case of myeloid leukaemia (eosinophilic) in swine. Nippon Juigaku. Zasshi. 1982;44:529–533. doi: 10.1292/jvms1939.44.529. [DOI] [PubMed] [Google Scholar]
- Kim YB, Zhang J, Davis WC, Lunney JK. CD11/CD18 panel report for swine CD workshop. Vet. Immunol Immunopathol. 1994;43:289–291. doi: 10.1016/0165-2427(94)90150-3. [DOI] [PubMed] [Google Scholar]
- Laber KE, Whary MT, Bingel SA, Goodrich JA, Smith AC, Swindle MM. Biology and Diseases of Swine. 2nd Edition 2009. [Google Scholar]
- Leifer CE, Matus RE, Patnaik AK, MacEwen EG. Chronic myelogenous leukemia in the dog. J Am Vet. Med Assoc. 1983;183:686–689. [PubMed] [Google Scholar]
- Lunney JK. Current status of the swine leukocyte antigen complex. Vet Immunol Immunopathol. 1994;43:19–28. doi: 10.1016/0165-2427(94)90116-3. [DOI] [PubMed] [Google Scholar]
- Marcato PS. Swine lymphoid and myeloid neoplasms in Italy. Vet. Res Commun. 1987;11:325–337. doi: 10.1007/BF00346191. [DOI] [PubMed] [Google Scholar]
- McTaggart HS, Head KW, Laing AH. Evidence for a genetic factor in the transmission of spontaneous lymphosarcoma (leukaemia) of young pigs. Nature. 1971;232:557–558. doi: 10.1038/232557a0. [DOI] [PubMed] [Google Scholar]
- Messick JB. Chronic Myeloid Leukemias. 5th. 2000. pp. 733–739. [Google Scholar]
- Mezrich JD, Haller GW, Arn JS, Houser SL, Madsen JC, Sachs DH. Histocompatible miniature swine: an inbred large-animal model. Transplantation. 2003;75:904–907. doi: 10.1097/01.TP.0000054839.43852.BF. [DOI] [PubMed] [Google Scholar]
- Paul PS, van Deusen RA, Mengeling WL. Monoclonal precipitating antibodies to porcine immunoglobulin. M. Vet Immunol Immunopathol. 1985;8:311–328. doi: 10.1016/0165-2427(85)90002-9. [DOI] [PubMed] [Google Scholar]
- Perkins P. Hematologic Abnormalities Accompanying Leukemia. 5th. 2000. pp. 740–745. [Google Scholar]
- Pescovitz MD, Aasted B, Canals A, Dominguez J, Vizcaino JS, Pospisil R, Sinkora J, Salmon H, Valpotic I, Davis WC. Analysis of monoclonal antibodies reactive with the porcine CD2 antigen. Vet. Immunol Immunopathol. 1994;43:229–232. doi: 10.1016/0165-2427(94)90140-6. [DOI] [PubMed] [Google Scholar]
- Pescovitz MD, Lunney JK, Sachs DH. Preparation and characterization of monoclonal antibodies reactive with porcine PBL. J. Immunol. 1984;133:368–375. [PubMed] [Google Scholar]
- Rafferty AL, Collett MG, Forsyth SF, Neumann EJ, Suepaul RB. Acute B-cell lymphoblastic leukaemia in a 5-month-old boar. N Z. Vet. J. 2007;55:244–247. doi: 10.1080/00480169.2007.36776. [DOI] [PubMed] [Google Scholar]
- Saalmuller A, Aasted B, Canals A, Dominguez J, Goldman T, Lunney JK, Maurer S, Pescovitz MD, Pospisil R, Salmon H. Analyses of mAb reactive with porcine CD8. Vet. Immunol. Immunopathol. 1994;43:249–254. doi: 10.1016/0165-2427(94)90144-9. [DOI] [PubMed] [Google Scholar]
- Saalmuller A, Denham S, Haverson K, Davis B, Dominguez J, Pescovitz MD, Stokes CC, Zuckermann F, Lunney JK. The Second International Swine CD Workshop. Vet. Immunol. Immunopathol. 1996;54:155–158. doi: 10.1016/s0165-2427(96)05675-9. [DOI] [PubMed] [Google Scholar]
- Sachs DH. MHC Homozygous Miniature Swine. 1992;1:3–15. [Google Scholar]
- Sachs DH, Leight G, Cone J, Schwartz S, Stuart L, Rosenberg S. Transplantation in miniature swine. I. Fixation of the major histocompatibility complex. Transplantation. 1976;22:559–567. doi: 10.1097/00007890-197612000-00004. [DOI] [PubMed] [Google Scholar]
- Sinkora J, Rehakova Z, Haverson K, Sinkora M, Dominguez J, Huang CA. Monoclonal antibodies putatively recognising activation and differentiation antigens. Vet. Immunol. Immunopathol. 2001a;80:143–164. doi: 10.1016/s0165-2427(01)00283-5. [DOI] [PubMed] [Google Scholar]
- Sinkora J, Rehakova Z, Samankova L, Haverson K, Butler JE, Zwart R, Boersma W. Characterization of monoclonal antibodies recognizing immunoglobulin kappa and lambda chains in pigs by flow cytometry. Vet. Immunol Immunopathol. 2001b;80:79–91. doi: 10.1016/s0165-2427(01)00277-x. [DOI] [PubMed] [Google Scholar]
- Sipos W, Gerner W, Schilcher F, Leeb C, Groiss S, Miller I, Saalmuller A, Schmoll F, Schwendenwein I. Immunophenotypic characterization of peripheral blast cells in a leukemic miniature pig. Vet. Pathol. 2006;43:362–367. doi: 10.1354/vp.43-3-362. [DOI] [PubMed] [Google Scholar]
- Skavlen PA, Stills HF, Jr, Caldwell CW, Middleton CC. Malignant lymphoma in a Sinclair miniature pig. Am J Vet. Res. 1986;47:389–393. [PubMed] [Google Scholar]
- Swindle MM. Swine in the Laboratory: Surgery, Anesthesia, Imaging, and Experimental Techniques. 2nd. 2009. [Google Scholar]
- Vernau W, Moore PF. An immunophenotypic study of canine leukemias and preliminary assessment of clonality by polymerase chain reaction. Vet. Immunol Immunopathol. 1999;69:145–164. doi: 10.1016/s0165-2427(99)00051-3. [DOI] [PubMed] [Google Scholar]
- Whang J, Frei E, III, Tjio JH, Carbone PP, Brecher G. The Distribution of the Distribution of the Philadelphia Chromosome in Patients with Chronic Myelogenous Leukemia. Blood. 1963;22:664–673. [PubMed] [Google Scholar]