Abstract
The authors examined the relationship between anxiety, depression, and physical disability, after controlling for demographic and health variables, in a sample of 374 adults ages 18-94. Results indicate that anxiety, depression, and comorbid anxiety and depression are associated with higher levels of disability, after controlling for factors such as age, gender, income, self-rated health, number of medical conditions, and number of physician visits in the past year. Furthermore, anxiety, depression, and comorbid anxiety and depression have a differential effect on disability according to age, with older adults with any of these symptoms reporting higher levels of disability than younger adults. These findings suggest that physicians working with older adults should assess for and treat anxiety as well as depressive symptoms.
Anxiety, depression, and physical disability are three major problems faced by many older adults, and there is growing evidence that these problems are related. Many studies have demonstrated that depressive symptoms are related to disability and poorer recovery from medical incidents independent of the increased medical burden experienced by depressed adults (for a review, see Lenze et al., 2001). However, surprisingly little research has examined the relationship between anxiety symptoms and disability.
Research has suggested that anxiety symptoms and disorders may be as disabling as depression (Kessler et al., 1999; Massion, Warshaw, & Keller, 1993; Ormel et al., 1994; Wetherell et al., 2004). Nonetheless, only a handful of studies have examined the relationship between anxiety and disability. Based on these studies, anxiety symptoms appear to be associated with increased levels of disability among older adults with medical comorbidities. With the exception of Brenes et al. (2005), however, these studies did not examine the impact of anxiety on disability independent of depressive symptoms. Because anxiety and depressive symptoms are frequently comorbid, especially in older adults, it is important to determine if anxiety is a risk factor for disability independent of depression. One study provides evidence that anxiety is a predictor of the progression of disability, supporting the further study of anxiety. A second limitation of these studies is the small age range of the sample. Studies have focused on either adults or older adults, rather than taking a lifespan approach. No research to date has examined whether disability is more strongly related to anxiety or depression in older adults than in younger adults. Because disability is a more normative or expected experience in older people than in younger people and there are many competing somatic conditions, it is possible that disability in late-life is less strongly associated with anxiety and depressive symptoms. Conversely, since disability in older adults is often associated with increasing dependence and institutional placement, this may result in higher levels of anxiety or depression for older adults facing disability.
The purpose of this study is to examine the relationship of anxiety and depressive symptoms with disability, both independently and in combination. Another purpose of this study is to examine the interaction between age and anxiety and depressive symptoms on disability to determine whether anxiety and depression are more or less strongly associated with disability in older people than in younger adults.
Methods
Participants
The sample consists of 374 adults from a mailing list purchased from an outside vendor. The mailing list included 1,500 adults residing in San Diego County, approximately half of whom were over the age of 60. The mailing list was created primarily from the local San Diego white pages. A package containing the questionnaire, informed consent document, and stamped and addressed return envelopes was sent to individuals on the list. Participants received a prepaid telephone card good for 60 minutes of long-distance service in return for their participation.
The average age of the sample was 56.76 years (SD = 18.80, range = 18-94). The majority were white (83.1%); 3.8% were African American, 5.4% were Hispanic/Latino, 5.1% were Asian, 0.5% were Native American, and 2.2% identified themselves as another race/ethnicity. The participants were highly educated (M = 15.1 years; SD = 3.4) and consisted of 65.1% males. More than half of the sample was currently married (58.0%), 18.9% were never married, 12.4% were divorced or separated, and 10.8% were widowed.
Measures
All participants completed a questionnaire that included demographic information; medical conditions as indicated on a checklist of 50 common health problems; current prescription medications; and number of doctor visits (not including mental health visits) in the previous year.
Disability was assessed using a modified form of the 10-item Physical Functioning subscale from the Medical Outcomes Study Short-Form 36-item Health Survey (Ware, Kosinski, & Gandek, 1993, 2000). In this form, participants were asked to indicate whether or not they had any limitations in performing each of the activities. Scores were calculated from 0-100, with higher scores indicating greater disability. Cronbach’s alpha for the current study is 0.88.
Anxiety and depressive symptoms were measured using the 18-item form of the Brief Symptom Inventory (BSI-18; Derogatis, 2000, 2001). The anxiety and depression subscales each consisted of 6 items. Based on standardized norms, participants were classified as having significant levels of anxiety or depression if they scored above a T-score of 63 on the Anxiety or Depression subscales. Cronbach’s alphas for the anxiety and depressive subscales were each .92.
Statistical Analyses
Correlations were performed to examine the bivariate relationships among demographic variables, health status, anxiety and depression, and disability. In order to examine the relationships between anxiety and depression and physical disability after controlling for demographic variables and health status, a series of three multiple regression analyses were conducted using SPSS release 13 (SPSS, 2004). The dependent variable in all three analyses was disability. Demographic information including age, gender, education, marital status (coded as married vs. not married), race/ethnicity (coded as White vs. not White), and income was entered in the first step. The presence of specific diseases or chronic conditions related to physical disability (arthritis, cancer, CHF, CHD, diabetes, emphysema/COPD, hearing loss, heart attack/heart failure, incontinence, osteoporosis, stroke), number of medical conditions, number of physician visits, and number of prescription medications were entered in the second step.
In Model 1, anxiety was entered in the third step and the interaction between anxiety and age was entered in the fourth step. In Model 2, depression was entered in the third step and the interaction between depression and age was entered in the fourth step. Finally, in order to determine the independent effects of anxiety and depression on disability, a third regression analysis was conducted (Model 3). Due to the multicollinearity between anxiety and depression, 3 new variables were created: anxiety symptoms only, depressive symptoms only, and comorbid anxiety and depressive symptoms. These 3 variables were added simultaneously in the third step, and the fourth step included the interactions between age and these 3 variables.
Results
Participants reported, on average, 2.59 medical conditions (SD = 2.42) and took an average of 1.95 prescription medications (SD = 2.19). They reported an average of 3.72 (SD = 4.18) doctor visits in the previous year. The average level of physical disability was 13.20 (SD = 25.0). The most commonly reported health conditions included arthritis (33.8%) and hearing loss (19.0%). With respect to anxiety and depressive symptoms, 6.4% reported significant levels of anxiety, 11.5% reported depression, and 4.5% reported comorbid anxiety and depressive symptoms.
As seen in Table 1, older age (r = .40, p < .001), lower levels of education (r = −.19, p < .001), and lower income (r = −.31, p < .001) are associated with higher levels of disability. All health problems and health-related characteristics, including number of visits to a physician, number of medical conditions, and number of prescription medications also had significant bivariate relationships with physical disability (all ps < .05). The presence of anxiety and depression were correlated at similar magnitudes with physical disability (r = .11, p < .05 and r = .10, p = .065, respectively).
Table 1.
Bivariate correlations with anxiety, depression, and physical disability.
| Anxiety | Depression | Physical disability | |
|---|---|---|---|
| Age | −.14** | −.16*** | .40*** |
| Education | −.10 | −.08 | −.19*** |
| Gender (male) | −.11* | −.12* | −.01 |
| Marital status (married) |
−.18* | −.20*** | −.09 |
| Race (Caucasian) | −.09 | −.06 | −.01 |
| Income | −.22*** | −.22*** | −.31*** |
| Self-rated health | −.23*** | −.20*** | −.52*** |
| Arthritis | .04 | .01 | .38*** |
| Cancer | −.07 | −.03 | .20*** |
| Congestive heart failure |
−.04 | .01 | .18*** |
| Coronary artery disease |
.06 | .06 | .15** |
| Diabetes | −.06 | −.05 | .21*** |
| Emphysema/COPD | −.04 | .01 | .23*** |
| Hearing loss | .01 | −.03 | .33*** |
| Heart attack/failure | .06 | .01 | .11* |
| Incontinence | .06 | .02 | .18*** |
| Osteoporosis | .08 | .04 | .17*** |
| Stroke | −.08 | .04 | .11* |
| # of medical conditions |
.08 | .07 | .57*** |
| # of times seen a doctor |
.01 | .10 | .41*** |
| # of Rx medications | −.04 | .00 | .45*** |
| Anxiety | 1.0 | .49*** | .11* |
| Depression | .49*** | 1.0 | .10 |
p < .05.
p < .01.
p ≤ .001.
The results of the regression analyses are presented in Table 2. The overall regression model containing demographic variables was significant. In particular, older age (β = .43, p <.001) and lower level of income (β = −.23, p < .001) were significantly associated with greater disability. Health-related variables were also related to increased disability; specifically, presence of congestive heart failure (β = .11, p < .05), presence of emphysema/COPD (β = .13, p < .005), number of medical conditions (β = .24, p = < .05), and number of physician visits (β = .26, p < .001) were significantly associated with greater disability, after controlling for demographic variables. In Model 1, there was a main effect for anxiety, with greater anxiety associated with increased disability (β = .15, p = .001). There was also a significant age by anxiety interaction, with anxious older adults experiencing the highest level of disability (β = .32, p = .001). In Model 2, there was a main effect for depression, with greater depression associated with increased disability (β = .12, p < .01). There was also a significant interaction between age and depression, with depressed older adults experiencing the highest level of disability (β = .24, p < .05).
Table 2.
Results from multiple regression analyses showing the relationships between anxiety and depression and physical disability after controlling for demographic and health variables.
| Model 1 Anxiety |
Model 2 Depression |
Model 3 Both Anxiety and Depression |
||||
|---|---|---|---|---|---|---|
| Variable | β | p | Β | P | β | p |
| Age | .43 | < .001 | ||||
| Gender | −.06 | .23 | ||||
| Education | −.06 | .25 | ||||
| Marital status | −.06 | .30 | ||||
| Race/ethnicity | −.03 | .57 | ||||
| Income | −.23 | < .001 | ||||
| Step 1 | F (6, 325) = 19.16, R2 = .261, p < .001 | |||||
| Arthritis | .01 | .85 | ||||
| Cancer | −.01 | .87 | ||||
| CHD | .03 | .62 | ||||
| CHF | .11 | .03 | ||||
| Diabetes | −.02 | .73 | ||||
| Emphysema/ COPD |
.13 | .004 | ||||
| Hearing loss | .04 | .48 | ||||
| Heart attack/failure |
−.04 | .47 | ||||
| Incontinence | .08 | .06 | ||||
| Osteoporosis | .04 | .42 | ||||
| Stroke | −.05 | .32 | ||||
| Number of other medical conditions |
.24 | .02 | ||||
| Number of physician visits |
.26 | < .001 | ||||
| Number of prescription medications |
.01 | .83 | ||||
| Step 2 | F (14, 311) = 9.38, Δ R2 = .219, p < .001 | |||||
| Anxiety | .15 | .001 | ---- | ---- | .05 | .28 |
| Depression | ---- | --- | .12 | .008 | .05 | .28 |
| Comorbid anxiety and depression |
---- | --- | ---- | --- | .16 | <.001 |
| Step 3 |
F (1, 310) = 11.02,
Δ R2 = .018, p = .001 |
F(1, 310) = 7.13,
Δ R2 = .012, p = .008 |
F(3, 308) = 4.69,
Δ R2 = .023, p = .003 |
|||
| Age × Anxiety | .32 | .001 | ---- | ----- | .35 | .001 |
| Age × Depression | --- | --- | .24 | .03 | .28 | .03 |
| Age × Comorbid anxiety and depression |
--- | --- | --- | --- | .21 | .02 |
| Step 4 |
F(1, 309) = 11.86,
Δ R2 = .019, p = .001 |
F(1, 309) = 4.76,
Δ R2 = .008, p = .03 |
F (3, 305)= 6.88,
Δ R2 = .03, p < .001 |
|||
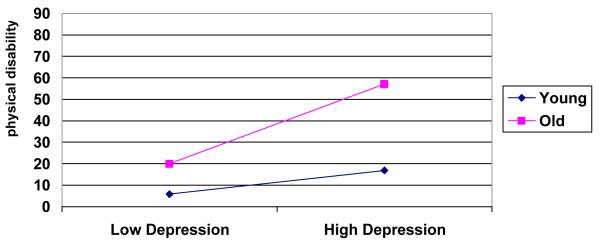
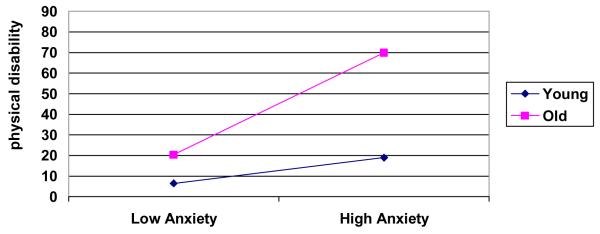
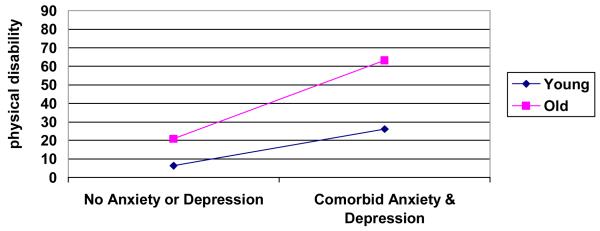
Finally, in Model 3, with anxiety only, depression only, and comorbid anxiety and depression entered in the same step, only comorbid anxiety and depression was related to disability (β = .16, p < .001). The fourth step containing the interactions between age and anxiety only, age and depression only, and age and comorbid anxiety and depression was significant (p < .001), with significant interactions between age and anxiety only (β = .35, p < .001), age and depression only (β = .28, p < .05), and age and comorbid anxiety and depression (β = .21, p < .05). See Figures 1, 2 and 3.
Figure 1.
Interaction between depression and age.
Note: Young = < 65 years; Old = ≥ 65 years.
Figure 2.
Interaction between anxiety and age.
Note: Young = < 65 years; Old = ≥ 65 years.
Figure 3.
Interaction between comorbid anxiety and depression and age.
Note: Young = < 65 years; Old = ≥ 65 years.
Discussion
Little research has examined the associations between both anxiety and depression and physical disability across the lifespan. The results of this study suggest that after statistically controlling for demographic and health-related characteristics, physical disability is associated with both anxiety and depressive symptoms. When the effects of anxiety and depression were examined simultaneously, both were independently associated with disability. Additional findings suggest that both anxiety symptoms and depressive symptoms are associated with greater physical disability with increasing age.
The finding that anxiety is associated with increased levels of physical disability is consistent with the few studies in this area. Brenes et al. (2005) found that anxiety symptoms are predictive of the progression of physical disability among older women. Similarly, Tinetti and colleagues (1995) also found that anxiety symptoms are predictive of ADL disability over the course of one year. Others have found a relationship between anxiety symptoms and disability in medical patients (Bond et al., 1998; Salaffi, Cavalieri, Nolli et al., 1991). Similarly depressive symptoms were significantly associated with physical disability. This is consistent with the extensive literature supporting the association between depressive symptoms and physical disability independent of health conditions and health status (Lenze et al., 2001).
Another purpose of this study was to examine whether the relationship between anxiety or depressive symptoms and physical disability varies with age. Findings indicate that anxiety and depressive symptoms both alone as well as comorbid anxiety and depressive symptoms are more strongly associated with physical disability among older adults than younger adults. One possible explanation for this finding is that physical disability may spark concerns about increasing dependence and possible institutional placement. This possibility may be more salient among older adults. Further, disability affects perceptions of control and self-esteem which may lead to a vulnerability to anxiety and depressive symptoms (Schulz, Heckhausen & O’Brien, 1994). Alternatively, there may also be a common biological link between aging, physical disability, and anxiety and depressive symptoms.
The current study addresses one of the most important limitations of previous studies: a head to head test of the effects of anxiety and depressive symptoms on disability. The results of this study indicate that anxiety is associated with disability both jointly with and independent of depressive symptoms. Although there was only a main effect for comorbid anxiety and depression on disability, anxiety, depression, and comorbid anxiety and depression all significantly interacted with age. Further, the strongest effect was for the age by anxiety interaction. These results provide clear evidence that the effect of anxiety on disability is not mediated by depression; rather, anxiety has a direct association with disability.
These findings must be interpreted in light of the limitations of this study. First, because the sample is predominantly white and well-educated, the generalizability of the results to individuals of other races or ethnicities and less education may be limited. Second, data are cross-sectional, precluding causal inferences. Thus, we are unable to say if anxiety and depression lead to disability or if disability leads to anxiety and depression. Third, information about health conditions and medications was obtained through self-report measures, rather than through more objective means such as chart reviews or pharmacy records. Fourth, measures of anxiety and depressive symptoms rather than structured clinical interviews were used. However, the BSI-18 has demonstrated adequate reliability and validity for assessing anxiety and depressive symptoms (Derogatis, 2000). Finally, objective physical performance assessments were not obtained. Thus, we are unable to say whether anxiety and depression are associated with a person’s perceptions of functioning independent of their level of actual physical functioning.
Nonetheless, there are several notable strengths of this study. First, we examined the individual and joint associations between anxiety and depressive symptoms and physical disability, addressing a significant limitation of the existing research. Second, the wide age range of the sample allowed us to examine the differential associations of anxiety and depressive symptoms and physical disability by age. Third, our dependent variable, physical disability, is an ecologically valid measure of disability for both old and young adults alike. Finally, findings controlled for a wide variety of health-related variables, including medical conditions, number of prescription medications, and number of physician visits, as well as self-rated health.
There are a number of directions for future research. First, longitudinal studies are needed to establish anxiety and depression as risk factors for disability. In other words, longitudinal studies are needed to confirm that anxiety and depression cause disability. Second, measures of observed physical performance should be included rather than solely relying upon self-reported measures of function in order to avoid the potential of overly pessimistic perceptions of functioning. Third, mediators of the relationship between anxiety and depression and disability need to be identified in order to have a better understanding of how anxiety and depression cause disability, allowing us to develop interventions prevent or slow the progression of physical disability.
Although we cannot infer that anxiety and depressive symptoms produce disability, we can conclude that anxiety and depressive symptoms do have significant associations with physical disability across the lifespan. Our findings suggest that it behooves clinicians to assess for and treat symptoms of anxiety and depression among all patients, especially older ones. There is some evidence that suggests that treatment of depression results in decreased disability (Borson et al., 1992; Heiligenstein et al., 1995; Landreville & Bissonnette, 1997; Robinson et al., 2000). Similarly, there is some suggestion that interventions that address disability may also decrease depressive symptoms as well (Penninx et al., 2002). Further work is needed to determine if treatment of anxiety and depressive symptoms results in decreased disability and if treatment of physical disability results in decreased anxiety and depressive symptoms.
Acknowledgments
Research supported by NIMH grants K23 MH065281 and K23 MH067643 and the University of California Academic Senate.
References
- Bond J, Gregson B, Smith M, Rousseau N, Lecouturier J, Rodgers H. Outcomes following acute hospital care for stroke or hip fracture: how useful is an assessment of anxiety or depression for older people? International Journal of Geriatric Psychiatry. 1998;13:601–610. doi: 10.1002/(sici)1099-1166(199809)13:9<601::aid-gps827>3.0.co;2-b. [DOI] [PubMed] [Google Scholar]
- Borson S, McDonald GH, Gayle T, Deffebach M, Lakshminarayan S, VanTuinen C. Improvement in mood, physical symptoms, and function with nortriptyline for depression in patients with chronic obstructive pulmonary disease. Psychosomatics. 1992;33:190–201. doi: 10.1016/S0033-3182(92)71995-1. [DOI] [PubMed] [Google Scholar]
- Brenes GA, Guralnik JM, Williamson JD, Fried LP, Simpson C, Simonsick EM, et al. The influence of anxiety on the progression of disability. Journal of the American Geriatrics Society. 2005;53:15–22. doi: 10.1111/j.1532-5415.2005.53007.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Derogatis LR. BSI 18 Brief Symptom Inventory 18: Administration, scoring, and procedures manual. NCS Pearson; Minneapolis, MN: 2000, 2001. [Google Scholar]
- Heiligenstein JH, Ware JE, Beusterien KM, Roback PJ, Andrejasich C, Tollefson GD. Acute effects of fluoxetine vs. placebo on functional health and well-being in late-life depression. International Psychogeriatrics. 1995;7:125–137. doi: 10.1017/s1041610295002407. [DOI] [PubMed] [Google Scholar]
- Kessler RC, DuPont RL, Berglund P, Wittchen HU. Impairment in pure and comorbid generalized anxiety disorder and major depression at 12 months in two national surveys. American Journal of Psychiatry. 1999;156:1915–1923. doi: 10.1176/ajp.156.12.1915. [DOI] [PubMed] [Google Scholar]
- Landreville P, Bissonnette L. Effects of cognitive bibliotherapy for depressed older adults with a disability. Clinical Gerontologist. 1997;17:35–55. [Google Scholar]
- Lenze EJ, Rogers JC, Martire LM, Mulsant BH, Rollman BL, Dew MA, et al. The association of late-life depression and anxiety with physical disability: A review of the literature and prospectus for future research. American Journal of Geriatric Psychiatry. 2001;9:113–135. [PubMed] [Google Scholar]
- Massion AO, Warshaw MG, Keller MB. Quality of life and psychiatric morbidity in panic disorder and generalized anxiety disorder. American Journal of Psychiatry. 1993;150:600–607. doi: 10.1176/ajp.150.4.600. [DOI] [PubMed] [Google Scholar]
- Ormel J, VonKorff M, Ustun TB, Pini S, Korten A, Oldehinkel T. Common mental disorders and disability across cultures. Journal of the American Medical Association. 1994;272:1741–1748. doi: 10.1001/jama.272.22.1741. [DOI] [PubMed] [Google Scholar]
- Penninx BWJH, Rejeski WJ, Pandya J, Miller ME, DiBari M, Applegate WB, et al. Exercise and depressive symptoms: A comparison of aerobic and resistance exercise effects on emotional and physical functioning in older persons with high and low depressive symptomatology. Journal of Gerontology: Psychological Sciences. 2002;57B:P124–P132. doi: 10.1093/geronb/57.2.p124. [DOI] [PubMed] [Google Scholar]
- Robinson RG, Schultz SK, Castillo C, Kopel T, Kosier JT, Newman RM, et al. Nortriptyline vs. fluoxetine in the treatment of depression and in short-term recovery after stroke: a placebo-controlled, double-blind study. American Journal of Psychiatry. 2000;157:351–359. doi: 10.1176/appi.ajp.157.3.351. [DOI] [PubMed] [Google Scholar]
- Salaffi F, Cavalieri F, Nolli M, Ferraccioli GF. Analysis of disability in knee osteoarthritis. Relationship with age and psychological variables but not with radiographic score. Journal of Rheumatology. 1991;18:1581–1586. [PubMed] [Google Scholar]
- Schulz R, Heckhausen J, O’Brien A. Negative affect and the disablement process in late life: A life-span control theory approach. In: Jennings R, Manuck SB, editors. Behavior, Health, and Aging. Lawrence Erlbaum Associates, Publishers; Mahwah, NJ: 2000. pp. 119–133. [Google Scholar]
- SPSS 13.0 for Windows. SPSS Inc.; 1998-2004. [Google Scholar]
- Tinetti ME, Inouye SK, Gill TM, Doucette JT. Shared risk-factors for fall, incontinence, and functional dependence: Unifying the approach to geriatric syndromes. Journal of the American Medical Association. 1995;273:1348–1353. [PubMed] [Google Scholar]
- Ware JE, Kosinski M, Gandek B. SF-36 Health Survey: Manual and Interpretation Guide. Quality Metric; Lincoln, RI: 1993, 2000. [Google Scholar]
- Wetherell JL, Thorp SR, Patterson TL, Golshan S, Jeste DV, Gatz M. Quality of life in geriatric generalized anxiety disorder: A preliminary investigation. Journal of Psychiatric Research. 2004;38:305–312. doi: 10.1016/j.jpsychires.2003.09.003. [DOI] [PubMed] [Google Scholar]