Abstract
Background: Little is known about the extent of heterogeneity of symptomatology in treated early-onset psychosis. The current study aims to quantify the extent of heterogeneity in trajectories of treated symptom severity in early-episode psychosis and their antecedents. Methods: Data were from 491 persons with early-episode psychosis from a clinical trial of haloperidol and risperidone. Positive and Negative Syndrome Scale (PANSS) administrations were used to measure symptom severity trajectories for (a) rapid treatment response scores over 4 weeks and (b) medium-term course over 24 weeks. Baseline antecedents included sex, Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition, diagnosis, age of onset, the Premorbid Adjustment Scale, and a cognitive test battery. Symptom severity trajectories were calculated with mixed mode latent class regression modeling from which groups were derived. Results: Five groups based on PANSS scores over time were identified. Over 4 weeks, 3 groups with varied baseline PANSS scores (54–105) did not surpass 30% PANSS improvement. Another group improved and then was stable (n = 76,15.3%), and another showed marked improvement (n = 94,18.9%). Logistic regression showed that membership in the best response trajectory was associated with not having a diagnosis of schizophrenia, good premorbid functioning, and higher cognitive functioning, whereas membership in the poor response trajectory was associated with earlier age of onset and poorer cognitive functioning. Conclusion: Amelioration generally characterizes treated symptom severity. Age of onset, diagnosis, cognitive functioning, and premorbid functioning have prognostic value in predicting treatment response trajectories.
Keywords: heterogeneity schizophrenia, symptom severity, premorbid functioning, course, rapid response
Introduction
Since its conception schizophrenia has been thought to follow a course of progressive deterioration1 and more recently to follow “a relapsing course for life in most sufferers,”2 a view that remains widely accepted.3 Unlike the notion of progressive deterioration, others propose and demonstrate that the course of schizophrenia improves with time and is thus best described as following a course of “progressive amelioration.”4–8 These divergent views of the course of schizophrenia have recently been reevaluated by examining initial and subsequent hospitalization rates in psychiatric registries in Denmark9,10 and Israel.11 These registry studies use hospitalization as a proxy measure for psychotic symptom exacerbation and show that the 10-year course is characterized by amelioration in approximately 75% of patients, deterioration in approximately 25% of patients, and stability in a few patients.11 Heterogeneity in clinical outcomes and among persons known to be receiving antipsychotic treatment has not been studied longitudinally or in early-onset patients. Thus, while some studies examine the course of hospitalization among persons with early-onset psychosis regardless of treatment, research on the course of treated symptom severity over time, to our knowledge, does not account for heterogeneity in treatment response.
Heterogeneity in symptom severity is widely thought to occur.12–16 For instance, a review of epidemiological outcome studies with at least a 10-year follow-up period has suggested that the course of illness is heterogeneous and may be mild, moderate, or severe.16 A classification of symptoms in chronic mid-range severity schizophrenia has shown 8 groupings of symptom severity that are characterized by differing levels of positive, negative, and cognitive functioning.15 Variables that have been documented to correlate with poor treatment response and course include cognitive functioning deficits,17,18 poor premorbid functioning,19 an earlier age of onset,20 and sex (being male).21–26
Recent time course analyses of clinical trials of varied lengths27,28 generally point to the appropriateness of accounting for heterogeneity in outcomes. The early-onset hypothesis proposes that antipsychotic medication effects occur rapidly and then plateaus. Estimates of rapid treatment response have ranged from 1 week29 to 2 months.30,31 These estimates use different criteria to define treatment response and do not account for potential heterogeneity in respondents. Also, different treatment response cut-offs may also be appropriate due to trial heterogeneity.32 Time to antipsychotic response is sufficiently varied in early-episode schizophrenia to suggest that longer treatment trials may be appropriate.30 Accordingly, this study examines Positive and Negative Syndrome Scale (PANSS) 30%, 40%, and 50% reductions accounting for heterogeneity weekly over 4 weeks and over 6 months.
The current study examines treated symptom severity in a clinical trial over 4 weeks, to examine rapid response, and six months, to examine mid-term course. Within this context, we specifically consider (a) the extent to which the course of symptom severity is characterized by amelioration, deterioration, or stability; (b) the extent to which age of first symptom onset, sex, cognitive functioning, and premorbid functioning characterize the trajectories; and (c) dropout rates. Dropout is examined as an additional outcome indicator to validate the trajectories that are based on symptom severity.
Methods
Design
The data were from a randomized, double-blind, multicenter, international clinical trial comparing the effectiveness of treatment with risperidone or haloperidol in early-episode psychotic patients. The trial design and major results regarding efficacy and safety were presented elsewhere.18,33 The data utilized in the current analysis represent a baseline to month 6 analysis during which period participants received trial medication. Month 6 was chosen because most patients were still in the study thereby reducing concerns about missing data.
The key trial inclusion criteria were being between the ages of 16 and 45 years, having a Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition (DSM-IV) diagnosis of schizophrenia, schizophreniform disorder or schizoaffective disorder for at most 12 months, following a maximum of 2 lifetime psychiatric hospitalizations for psychosis, having persistent current psychotic symptoms requiring long-term antipsychotic treatment, and having had 12 weeks or less of cumulative lifetime exposure to antipsychotic medications. Recruitment began in November 1996 and ended in December 1999. Investigators (n = 49) underwent training and interrater reliability testing at an investigator meeting before beginning the study and further training was provided at follow-up meetings. Prior to enrolling participants into the study, raters were trained to administer the PANSS and achieved an inter-rater reliability exceeding 0.8. The total trial sample included randomized participants from 11 countries. The study was conducted according to the principles of Good Clinical Practice. Approval was obtained from local Institutional Review Boards, and subjects provided informed written consent to participate in the study.
Measures
Measures included in this analysis were the PANSS total score to measure symptom severity34,35; Structural Clinical Interview for DSM-IV diagnosis; the Premorbid Adjustment Scale (PAS)37 mean score of the life phases supplemented by the typology of good, poor, and declining premorbid functioning scored as detailed elsewhere36; and cognitive functioning based on a comprehensive assessment (Wechsler Memory Scale-Revised Visual Reproduction Subtest, Rey Auditory Verbal Learning Test, Continuous Performance Test, IP Version, Verbal Fluency Examinations, Wechsler Adult Intelligence Scale-Revised, Digit Symbol Subtest, and the Wisconsin Card Sorting Test).18,38 Data assessed also included sex, dropout and clinician estimated age of onset. An Online Supplement is presented of the analysis of the PANSS General Psychopathology, Negative and Positive subscales.
Participants
Of the final sample, 497 respondents completed all measures at baseline. Of the remaining trail participants, 1 respondent had missing data on cognitive functioning and the PAS, 22 on cognitive functioning, 3 on the PAS, 6 on the PANSS at baseline, and 5 on age of onset, cumulating in 497 available baseline responses. All subsequent monthly PANSS data were followed through to month 6. Participants were not excluded from the analysis on the basis of other information.
Analytic Approach
The current analysis aimed to identify subgroups of patients with similar courses of treatment response. To derive heterogeneous empirically based subgroups, mixed mode latent regression modeling was conducted as has been used previously in psychiatry.39–43 Using all available information at each time period, this analysis identifies subgroups of cases that are homogeneous on certain criteria within the group and significantly dissimilar (ie, heterogeneous) from other subgroups in substantial ways. The subgroups are known as latent classes represented by K distinct categories of a latent variable X.44 To identify the appropriate number of subgroups, the Bayes Information Criterion (BIC) is used. BIC is calculated as log(L) − 0.5 × log(n) × (k); where L is the model's maximized likelihood, n is the sample size, and k are the parameters.45 Like past research, BICs were examined to derive the most parsimonious number of subgroups. This permitted the empirical derivation of the appropriate number of trajectories that were subsequently plotted based on available data.
To represent possible periods of rapid response and medium-term course respectively, all analyses were conducted for the period of baseline to week 4 and baseline to month 6. Separate trajectory models were conducted for the PANSS total and subscales. A series of analyses of variance were conducted to test for differences between the trajectory groups on age of onset, PAS, cognitive functioning, PANSS baseline, last observation carried forward-based PANSS endpoint, and PANSS average across visits. The overlap between week 4 and month 6 treatment response trajectory memberships was examined with cross tabulations and the magnitude of associations examined with either Kendall's τ, a measure of concordance for ordinal data, or Kappa (κ), a measure of agreement for dichotomous variables. To examine differences between the trajectory groups on the dichotomous variables of PANSS total 30%, 40%, and 50% change criteria, dropout, sex, and diagnosis (schizophrenia vs nonschizophrenia), a series of crosstabs with chi-square tests were conducted. Given the clinical relevance in identifying persons with increased likelihood of having either a poor or a good treatment response, 4 binary logistic regression models were conducted to predict membership in the worst treatment response trajectory group and the best group. The order of entry was site, sex, age of first symptom onset, PANSS baseline total, PAS typology at baseline, presence of DSM-IV schizophrenia, and cognitive functioning at baseline.
Results
Trajectory Models
Five trajectories appeared to characterize the data. This emerged based on an iterative process examining the fit of baseline to week 4 and month 6 trajectory models of the PANSS (totals and subscales). To derive the most parsimonious number of trajectories, BICs were examined for 2 through 7 trajectory solutions. A 10-point difference was taken to favor the lower BIC, and using this cut-off the best fitting number of trajectories identified.46 For trajectories 2 through 6, the following BICs were extracted: 41184.4, 40913.8, 40451.6, 40219.5, and 40272.7, respectively, for total symptom severity. This trend replicated for the 3 subscales across the study periods (see Online Supplement). Accordingly, 5 trajectories observed to characterize the data appropriately.
Trajectories: PANSS Outcomes and Characteristics
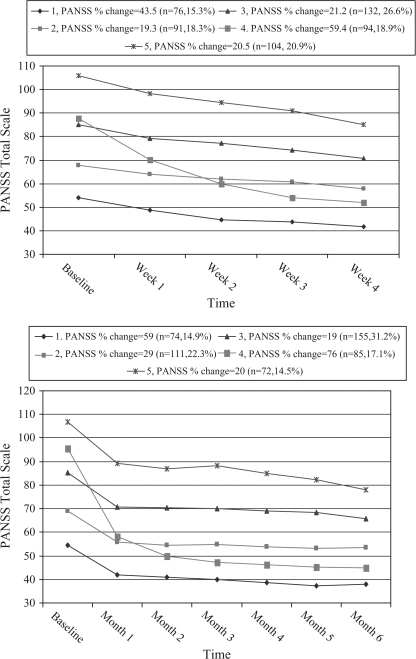
The 5 trajectories, based on PANSS totals for 4 weeks and 6 months, identified in the mixed-mode latent class regression analysis were ordered by baseline PANSS scores and presented in figure 1 and described in tables 1 and 2. Trajectory membership in the figures is the result of a mixed modeling that uses all available cases at each measurement interval. These results illustrated heterogeneity in symptom severity and treatment response, from which groups were derived. Groups 1 and 2 entered the trial with relatively mild baseline PANSS scores (ie, had PANSS totals below 70). Group 3 was the middlemost range group and showed the least percentage improvement based on PANSS change scores. Groups 4 and 5 had higher symptom severity levels, with baseline PANSS totals greater than 90. Group 5 showed relatively little improvement, whereas group 4 showed the most improvement. In support of the classification by trajectory, table 2 showed that dropout rates aligned fairly closely with changes in symptom severity between the groups. Groups 3 and 5 showed the least improvement and had the highest dropout rates (respectively 65.8% and 65.3%), whereas groups 1 and 4 had the most symptom improvement and lowest dropout rates (29.7% and 37.6%). Similar trends emerged at week 4 and month 6 in PANSS endpoint, PANSS week 4/month 6, and PANSS average scores (see tables 1 and 2).
Fig. 1.
Symptom Severity Trajectories at 4 wk and 6 mo.
Table 1.
Trajectories for PANSS Totals at 4 weeks
| Moderate Baseline |
Severe Baseline |
Statistically Significant Pairwise comparisons |
|||||||||||
| M/% | SEM | M/% | SEM | M/% | SEM | M/% | SEM | M/% | SEM | F/χ2 | P | LSD | |
| Trajectory | 1 | 2 | 3 | 4 | 5 | ||||||||
| PANSS (baseline) | 54.1 | 1.2 | 67.7 | 0.7 | 85.0 | 0.7 | 87.7 | 1.4 | 105.8 | 1.4 | 257.4 | <.001 | 1 < 2, 1 < 3, 1 < 4, 1 < 5, 2 < 3, 2 < 4, 2 < 5, 3 < 5, 4 < 5 |
| PANSS (average) | 46.7 | 0.7 | 62.9 | 0.4 | 77.7 | 0.4 | 65.0 | 0.8 | 96.0 | 1.0 | 587.3 | <.001 | 1 < 2, 1 < 3, 1 < 4, 1 < 5, 2 < 3, 2 < 4, 2 < 5, 3 > 4, 3 < 5, 4 < 5 |
| PANSS (LOCF endpoint) | 41.8 | 0.7 | 59.0 | 0.7 | 72.1 | 0.7 | 52.1 | 1.3 | 87.8 | 1.7 | 204.0 | <.001 | 1 < 2, 1 < 3, 1 < 4, 1 < 5, 2 < 3, 2 < 4, 2 < 5, 3 > 4, 3 < 5, 4 < 5 |
| PANSS (Week 4) | 41.8 | 0.8 | 57.8 | 0.7 | 70.9 | 0.7 | 52.0 | 1.4 | 85.0 | 1.7 | 204.0 | <.001 | 1 < 2, 1 < 3, 1 < 4, 1 < 5, 2 < 3, 2 > 4, 2 < 5, 3 > 4, 3 < 5, 4 < 5 |
| PANSS absolute change | −12.2 | 1.2 | −8.6 | 1.1 | −12.9 | 1.1 | −35.6 | 1.9 | −18.0 | 2.2 | 39.7 | <.001 | 1 > 4, 1 > 5, 2 > 4, 2 > 5. 3 > 4, 3 > 5, 4 < 5 |
| PANSS % change | −43.5 | 4.3 | −19.3 | 2.9 | −21.2 | 1.8 | −59.4 | 3.0 | −20.5 | 3.1 | 28.4 | <.001 | 1 < 2, 1 < 3, 1 < 4, 1 < 5, 2 < 4, 3 > 4, 4 < 5 |
| PANSS 30% criteria | 81.6 | 54.9 | 47.7 | 98.9 | 52.9 | 84.8 | <.001 | ||||||
| PANSS 40% criteria | 72.4 | 34.1 | 37.1 | 96.8 | 33.7 | 125.8 | <.001 | ||||||
| PANSS 50% criteria | 59.2 | 13.2 | 12.1 | 93.6 | 18.3 | 220.0 | <.001 | ||||||
| Best trajectory month 6 | 10.7 | 7.4 | 11.7 | 34.8 | 24.1 | 35.2 | <.001 | ||||||
| Dropout | 10.5 | 13.2 | 16.7 | 6.4 | 18.3 | 7.8 | 0.10 | ||||||
| Being male | 59.2 | 78.0 | 71.2 | 73.4 | 69.2 | 7.6 | 0.11 | ||||||
| Schizoaffective | 6.6 | 5.5 | 6.1 | 7.4 | 7.7 | 0.5 | 0.97 | ||||||
| Schizophrenia | 57.9 | 75.8 | 62.9 | 54.3 | 76.0 | 17.0 | <.01 | ||||||
| Schizophreniform | 35.5 | 18.7 | 31.1 | 38.3 | 16.3 | 18.7 | <.001 | ||||||
| Age of onset | 0.0 | 0.1 | 0.2 | 0.1 | 0.0 | 0.1 | 0.1 | 0.1 | −0.2 | 0.1 | 2.2 | 0.07 | 1 > 5, 2 > 5, 3 > 5, 4 > 5 |
| Cognitive functioning | 0.2 | 0.1 | 0.0 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | −0.4 | 0.1 | 9.6 | <.001 | 1 < 2, 1 < 3, 1 < 4, 1 < 5, 2 < 3, 2 < 5, 3 > 4, 3 < 5, 4 < 5 |
| PAS baseline | 0.3 | 0.0 | 0.3 | 0.0 | 0.4 | 0.0 | 0.3 | 0.0 | 0.4 | 0.0 | 11.0 | <.001 | |
| PAS typology | |||||||||||||
| Good | 76.3 | 53.8 | 35.6 | 50.0 | 34.6 | 7.8 | 0.10 | ||||||
| Decline | 6.6 | 11.0 | 15.9 | 18.1 | 20.2 | 8.4 | 0.80 | ||||||
| Bad | 17.1 | 35.2 | 48.5 | 31.9 | 45.2 | 24.4 | <.001 | ||||||
Note: PANSS = Positive and Negative Syndrome Scale, PAS = Premorbid Adjustment Scale, LOCF = Last Observation Carried Forward, LSD = Least Significant Difference, M = mean, F = analysis of variance. All F tests, df = 4, 492; all chi-square tests, df = 4.
Table 2.
Trajectories for PANSS Totals at 6 months
| Moderate Baseline | Severe Baseline | Statistically Significant Pairwise comparisons | |||||||||||
| M/% | SEM | M/% | SEM | M/% | SEM | M/% | SEM | M/% | SEM | F/χ2 | P | LSD | |
| Trajectory | 1 | 2 | 3 | 4 | 5 | ||||||||
| PANSS (baseline) | 54.6 | 1.3 | 69.1 | 0.8 | 85.3 | 0.8 | 95.5 | 1.6 | 106.7 | 1.7 | 255.0 | <.001 | 1 < 2, 1 < 3, 1 < 4, 1 < 5, 2 < 3,2 < 4, 2 < 5, 3 < 4, 3 < 5, 4 < 5 |
| PANSS (average) | 42.7 | 0.6 | 58.2 | 0.4 | 75.2 | 0.5 | 58.1 | 1.0 | 94.6 | 1.4 | 582.7 | <.001 | 1 < 2, 1 < 3, 1 < 4, 1 < 5, 2 < 3, 2 < 5, 3 > 4, 3 < 5, 4 < 5 |
| PANSS (endpoint) | 38.9 | 0.7 | 55.9 | 0.9 | 72.9 | 0.9 | 45.7 | 1.2 | 89.3 | 1.9 | 285.0 | <.001 | 1 < 2, 1 < 3, 1 < 4, 1 < 5, 2 < 3, 2 > 4, 2 < 5, 3 > 4, 3 < 5, 4 < 5 |
| PANSS (month 6) | 37.9 | 0.7 | 53.5 | 1.2 | 65.7 | 1.4 | 44.9 | 1.5 | 78.0 | 2.2 | 114.0 | <.001 | 1 < 2, 1 < 3, 1 < 4, 1 < 5, 2 < 3, 2 > 4, 2 < 5, 3 > 4, 3 < 5, 4 < 5 |
| PANSS absolute change | −15.7 | 1.4 | −13.2 | 1.4 | −12.5 | 1.3 | −49.8 | 1.7 | −17.4 | 2.4 | 90.3 | <.001 | 1 > 4, 2 > 4,3 > 4, 3 > 5, 4 < 5 |
| PANSS % change | 59.0 | 3.6 | 29.0 | 3.3 | 19.1 | 2.3 | 76.1 | 1.7 | 20.0 | 3.1 | 75.6 | <.001 | 1 > 2, 1 > 3,1 < 4, 1 > 5,2 > 3, 2 < 4, 2 > 5, 3 < 4, 4 > 5 |
| Dropout | 29.7 | 46.8 | 65.8 | 37.6 | 65.3 | 39.7 | <.01 | ||||||
| PANSS 30% criteria | 89.2 | 73.9 | 51.0 | 100.0 | 52.8 | 87.8 | <.001 | ||||||
| PANSS 40% criteria | 83.8 | 65.8 | 40.6 | 100.0 | 31.9 | 124.7 | <.001 | ||||||
| PANSS 50% criteria | 74.3 | 55.0 | 24.5 | 100.0 | 20.8 | 168.2 | <.001 | ||||||
| Being male | 56.8 | 80.2 | 72.3 | 63.5 | 75.0 | 14.7 | p<.05 | ||||||
| Schizoaffective | 5.4 | 7.2 | 3.2 | 8.2 | 12.5 | 7.5 | ns | ||||||
| Schizophrenia | 58.1 | 74.8 | 65.8 | 55.3 | 70.8 | 10.9 | p<.05 | ||||||
| Schizophreniform | 36.5 | 18.0 | 31.0 | 36.5 | 16.7 | 16.5 | p<.05 | ||||||
| Age of onset | 0.1 | 0.1 | 0.1 | 0.1 | 0.0 | 0.1 | 0.1 | 0.1 | −0.3 | 0.1 | 1.9 | ns | |
| Cognitive functioning | 0.2 | 0.1 | 0.1 | 0.1 | 0.1 | 0.1 | −0.2 | 0.1 | −0.3 | 0.1 | 8.6 | <.001 | 1 > 4, 1 > 5, 2 > 4, 2 > 5, 3 > 4, 3 > 5 |
| PAS baseline | 0.3 | 0.0 | 0.3 | 0.0 | 0.4 | 0.0 | 0.3 | 0.0 | 0.4 | 0.0 | 12.3 | <.001 | 1 < 2, 1 < 3, 1 < 4, 1 < 5, 2 > 1, 2 < 3,2 < 5, 3 > 4, 4 < 5 |
| PAS typology | |||||||||||||
| Good | 74.3 | 53.2 | 34.2 | 55.3 | 31.9 | 42.8 | <.001 | ||||||
| Decline | 8.1 | 10.8 | 16.1 | 17.6 | 22.2 | 7.9 | ns | ||||||
| Bad | 17.6 | 36.0 | 49.7 | 27.1 | 45.8 | 28.6 | <.001 | ||||||
Note: PANSS = Positive and Negative Syndrome Scale, PAS = Premorbid Adjustment Scale, LSD = Least Significant Difference, M = mean, F = analysis of variance. All F tests, df = 4, 492 except month 6 PANSS where df = 4, 237; all chi-square tests, df = 4.
Comparison of the key characteristics (in the lower portion of table 1) showed that the trajectory groups differed significantly (P < .05) on premorbid functioning, cognitive functioning, diagnosis, and sex, but not on age of onset. Examination of the pairwise comparisons showed, eg, that trajectories 5 and 3 both were characterized by the poorest course and had the highest PAS scores at baseline (indicating poorer premorbid adjustment). Trajectory 1, however, showed almost the greatest improvement and had the lowest PAS score (indicating good premorbid functioning). Groups 5 and 3, who showed the least improvement, had relatively fewer females and had high proportions of persons with schizophrenia as compared with the other groups.
Subscale Analysis and Overlap Between Trajectories
The trajectories in figure 1, and in the Online Supplement, showed that all symptom clusters were characterized by 5 trajectories across time. These appeared to resemble each other except that none of the PANSS negative subscale trajectories showed such marked improvement as the other subscales. There was considerable overlap in trajectory membership in figure 1 over 4 weeks and over 6 months (τ = .7, P < .01). In total, 69 (75.8%) week 4 respondents with best trajectory membership belonged in the same trajectory at week 24, whereas of those without week 4 best trajectory membership only 42 (10.3%) made the transition to best trajectory membership at week 24 (κ = .60, P < .01). Conversely, 63 (82.9%) week 4 respondents with poorest trajectory membership continued to week 24, whereas of those without week 4 poorest trajectory membership only 11 (2.6%) made the transition to poorest trajectory membership at week 24 (κ = .81, P < .01). Together, this indicates that trajectory membership was closely consistent across time.
Prediction of Best and Worst Outcomes: Binary Logistic Modeling
Binary logistic models were conducted to predict membership in the trajectory with the best and worst treatment response trajectories for the 4 week and 6 month periods. These results presented in table 3 showed moderate to good predictive accuracy, as indicated by the model fit indices. Prediction of membership in the poorest response group was better at both time points than prediction of membership in the best response group. Younger age of onset predicted poorest trajectory membership at week 4 and month 6. At week 4, low baseline scores on cognitive testing predicted membership in the poorest response trajectory, whereas high baseline cognitive test scores predicted membership in the best response trajectory. Good premorbid functioning scores predicted membership in the best response group at month 6. Not having a DSM-IV schizophrenia diagnosis was associated with membership in the best treatment response trajectory at 4 weeks and 6 months. This aspect of the results indicated that the predictors of treatment response varied by time and whether treatment response was good or poor.
Table 3.
Binary Logistic Regression Models Examining Membership in the Best and Worst Treatment Response Trajectories at wk 4 and mo 6
| Wk 4 |
Month 6 |
||||||||
| Trajectory | OR | 95.0% CI (Range) | P | OR | 95.0% C.I (Range) | P | |||
| Good response | Being male | 1.34 | 0.78−2.28 | .29 | 0.72 | 0.42−1.25 | .24 | ||
| Age at onset | 1.14 | 0.90−1.45 | .28 | 1.12 | 0.86−1.46 | .39 | |||
| Good premorbid functioning | 1.24 | 0.76−2.03 | .38 | 2.01 | 1.18−3.43 | .01 | |||
| Not having schizophrenia | 2.04 | 1.26−3.30 | .00 | 2.11 | 1.24−3.60 | .01 | |||
| Cognitive functioning | 1.42 | 1.01−1.98 | .04 | 0.79 | 0.55−1.12 | .18 | |||
| Constant | 0.00 | .00 | 0.00 | .00 | |||||
| R2 | Sensitivity | Specificity | Accuracy | R2 | Sensitivity | Specificity | Accuracy | ||
| Model fit indices | 0.09 | 0.81 | 0.33 | 80.68 | 0.22 | 0.84 | 0.48 | 82.70 | |
| OR | 95.0% CI (Range) | P | OR | 95.0% CI (Range) | P | ||||
| Poor response | Being male | 0.56 | 0.28−1.13 | 0.11 | 1.19 | 0.57−2.47 | 0.65 | ||
| Age at onset | 0.70 | 0.50−0.98 | 0.04 | 0.70 | 0.49−1.00 | 0.05 | |||
| Good premorbid functioning | 0.89 | 0.45−1.73 | 0.72 | 0.69 | 0.35−1.36 | 0.28 | |||
| Not having schizophrenia | 0.58 | 0.29−1.16 | 0.12 | 1.31 | 0.66−2.58 | 0.44 | |||
| Cognitive functioning | 0.53 | 0.34−0.82 | 0.00 | 0.80 | 0.52−1.22 | 0.30 | |||
| Constant | 0.00 | 0.00 | 0.00 | 0.00 | |||||
| R2 | Sensitivity | Specificity | Accuracy | R2 | Sensitivity | Specificity | Accuracy | ||
| Model fit indices | 0.62 | 0.91 | 0.77 | 89.00 | 0.47 | 0.90 | 0.60 | 87.32 | |
Note: OR = odds ratio, CI = confidence interval. Controlling for baseline Positive and Negative Syndrome Scale and site, accuracy is the percentage correctly classified by the logistic model R2 is Nagelkerke's pseudo R2.
Discussion
Based on a large multinational antipsychotic clinical trial of early-episode psychosis, the current results demonstrate heterogeneity in the course of treated symptom severity. In this context, the data show 5 trajectories of treated symptom severity, as measured by the PANSS. Although the groups differ across time and symptoms, the following trends emerge: Two groups show considerable improvement across time, one of which (approximately 20%) shows superior symptom amelioration levels across criteria and time. These groups comprise approximately 40% of the sample. Two other groups together comprise another 40% of the sample and show moderate improvement and one group remains with the poorest symptom severity levels and includes approximately 20% of the sample. Higher dropout rates are moderately associated with membership in trajectories with poorer outcomes. Similar to the literature, the study variables except age of onset20,21 characterized the groups across time. Generally, poorer cognitive functioning,17,18,19,40 worse premorbid functioning,19,37,49 and sex (being male)20,22,24 relate to poorer trajectory membership, as implied by the literature.
The current findings complement observations of heterogeneity in the literature. Characterization of the course of illness into groups, such as mild, moderate, or severe,16 has heuristic utility and assists in comprehending the current results. For instance, lower dropout rates being moderately associated with a less severe course gives additional support to the validity of the trajectories. This is notable because the results indicate that at least within a 6 month time frame treatment response occurs generally within the first month, accounting for various response criteria and heterogeneity.
Treatment response is characterized by an initial period of rapid response during the first 2 weeks of treatment.29 This is most pronounced among 18.9% of respondents during this period almost all of whom meet the PANSS 50% change criteria. Following the first 2 weeks, symptom improvements occur that are less marked, although these too require consideration. Treatment response among the remaining trajectories is not as pronounced as those with large initial improvements. Treatment response trajectory membership at week 4 is associated with 6-month membership, such that patients who improve the most in the initial 4 weeks also do so over 6 months. This indicates that treatment response characterized by elevated symptom amelioration levels may partly be attributed to a select patient subgroup who may be identified rapidly.
In predicting treatment response, the binary logistic regression models are consistent with the literature. Of the treatment response outcomes, membership in the best response subgroup at 6 months is predicted by the combination of good premorbid functioning and not having a DSM-IV diagnosis of schizophrenia. The results show that absence of a schizophrenia diagnosis significantly relates to good treatment response early and mid-course, and that cognitive functioning has short-term predictive utility for good and bad outcomes.18,49
Limitations
The current study has several limitations. The sample was selected according to criteria for a randomized clinical trial and may not accurately represent routine clinical practice, although previous work has suggested that the sample from the current study resembles in key ways a large first-episode epidemiological cohort.50 Due to the large number of locations, many investigators were involved in PANSS assessments, study participants differed widely by language and culture, and the PANSS was translated into different languages. Site was, however, controlled for in this analysis.
Summary
Based on a very large clinical trial of antipsychotic medication in treating early-onset psychosis, the current results suggest that the course of treated symptom severity in this sample is characterized by heterogeneity and that most treated persons improve. Rapid response occurs considerably for a select group of early-episode patients whose medium-term prognosis is of amelioration. Different factors operate during the early stages of treatment as compared with later on in treatment for good and poor treatment response. Despite this, only short-term poor and good treatment response are predicted by cognitive functioning. Short- and medium-course poor treatment response are predicted by a younger age of onset, whereas good response is predicted by the absence of a DSM-IV schizophrenia diagnosis. Medium-course good response is also predicted by premorbid functioning. Collectively, the current findings highlight that (a) it is appropriate to account for heterogeneity in the course of treated symptom severity to best understand the course of illness and (b) prognostic utility is associated with cognitive functioning, age of onset, premorbid functioning, and diagnosis.
Supplementary Material
Supplementary material is available at http://schizophreniabulletin.oxfordjournals.org.
Supplementary Material
Acknowledgments
The authors wish to acknowledge Johnson & Johnson Pharmaceutical Research and Development, Beerse, Belgium, for providing the data for this work.
References
- 1.Kraepelin E. Dementia Praecox and Paraphrenia. New York, NY: Krieger; 1971. [Google Scholar]
- 2.Davies T. Psychosocial factors and relapse of schizophrenia. BMJ. 1994;309:353–354. doi: 10.1136/bmj.309.6951.353. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Walker E, Kestler L, Bollini A, Hochman KM. Schizophrenia: etiology and course. Annu Rev Psychol. 2004;55:401–430. doi: 10.1146/annurev.psych.55.090902.141950. [DOI] [PubMed] [Google Scholar]
- 4.Eaton WW, Bilker W, Haro JM, et al. Long-term course of hospitalization for schizophrenia: part II. Change with passage of time. Schizophr Bull. 1992;18:229–241. doi: 10.1093/schbul/18.2.229. [DOI] [PubMed] [Google Scholar]
- 5.Eaton WW, Mortensen PB, Herrman H, et al. Long-term course of hospitalization for schizophrenia: part I. Risk for rehospitalization. Schizophr Bull. 1992;18:217–228. doi: 10.1093/schbul/18.2.217. [DOI] [PubMed] [Google Scholar]
- 6.Eaton WW, Thara R, Federman E, Tien A. Remission and relapse in schizophrenia: the Madras Longitudinal Study. J Nerv Ment Dis. 1998;186:357–363. doi: 10.1097/00005053-199806000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Mortensen PB, Eaton WW. Predictors for readmission risk in schizophrenia. Psychol Med. 1994;24:223–232. doi: 10.1017/s0033291700026982. [DOI] [PubMed] [Google Scholar]
- 8.Munk-Jörgensen P, Mortensen PB, Machon RA. Hospitalization patterns in schizophrenia. A 13-year follow-up. Schizophr Res. 1991;4:1–9. doi: 10.1016/0920-9964(91)90004-b. [DOI] [PubMed] [Google Scholar]
- 9.Olesen AV, Mortensen PB. Readmission risk in schizophrenia: selection explains previous findings of a progressive course of disorder. Psychol Med. 2002;32:1301–1307. doi: 10.1017/s0033291702005548. [DOI] [PubMed] [Google Scholar]
- 10.Olesen AV, Parner ET. Correcting for selection using frailty models. Stat Med. 2006;25:1672–1684. doi: 10.1002/sim.2298. [DOI] [PubMed] [Google Scholar]
- 11.Rabinowitz J, Levine SZ, Haim R, Hafner H. The course of schizophrenia: progressive deterioration, amelioration or both? Schizophr Res. 2007;91:254–258. doi: 10.1016/j.schres.2006.12.013. [DOI] [PubMed] [Google Scholar]
- 12.Buchsbaum MS, Haier RJ. Biological homogeneity, symptom heterogeneity, and the diagnosis of schizophrenia. Schizophr Bull. 1978;4:473–475. doi: 10.1093/schbul/4.4.473. [DOI] [PubMed] [Google Scholar]
- 13.Kendler KS, Karkowski-Shuman L, O'Neill FA, Straub RE, MacLean CJ, Walsh D. Resemblance of psychotic symptoms and syndromes in affected sibling pairs from the Irish Study of High-Density Schizophrenia Families: evidence for possible etiologic heterogeneity. Am J Psychiatry. 1997;154:191–198. doi: 10.1176/ajp.154.2.191. [DOI] [PubMed] [Google Scholar]
- 14.Lewine R, Renders R, Kirchhofer M, Monsour A, Watt N. The empirical heterogeneity of first rank symptoms in schizophrenia. Br J Psychiatry. 1982;140:498–502. doi: 10.1192/bjp.140.5.498. [DOI] [PubMed] [Google Scholar]
- 15.Mohr PE, Cheng CM, Claxton K, et al. The heterogeneity of schizophrenia in disease states. Schizophr Res. 2004;71:83–95. doi: 10.1016/j.schres.2003.11.008. [DOI] [PubMed] [Google Scholar]
- 16.Jobe TH, Harrow M. Long-term outcome of patients with schizophrenia: a review. Can J Psychiatry. 2005;50:892–900. doi: 10.1177/070674370505001403. [DOI] [PubMed] [Google Scholar]
- 17.Reichenberg A, Harvey PD. Neuropsychological impairments in schizophrenia: integration of performance-based and brain imaging findings. Psychol Bull. 2007;133:833–858. doi: 10.1037/0033-2909.133.5.833. [DOI] [PubMed] [Google Scholar]
- 18.Harvey PD, Rabinowitz J, Eerdekens M, Davidson M. Treatment of cognitive impairment in early psychosis: a comparison of risperidone and haloperidol in a large long-term trial. Am J Psychiatry. 2005;162:1888–1895. doi: 10.1176/appi.ajp.162.10.1888. [DOI] [PubMed] [Google Scholar]
- 19.Rabinowitz J, Harvey PD, Eerdekens M, Davidson M. Premorbid functioning and treatment response in recent-onset schizophrenia. Br J Psychiatry. 2006;189:31–35. doi: 10.1192/bjp.bp.105.013276. [DOI] [PubMed] [Google Scholar]
- 20.Meltzer HY, Rabinowitz J, Lee MA, et al. Age at onset and gender of schizophrenic patients in relation to neuroleptic resistance. Am J Psychiatry. 1997;154:475–482. doi: 10.1176/ajp.154.4.475. [DOI] [PubMed] [Google Scholar]
- 21.Rabinowitz J, Levine SZ, Hafner H. A population based elaboration of the role of age of onset on the course of schizophrenia. Schizophr Res. 2006;88:96–101. doi: 10.1016/j.schres.2006.07.007. [DOI] [PubMed] [Google Scholar]
- 22.Angermeyer MC, Kuhn L. Gender differences in age at onset of schizophrenia. An overview. Eur Arch Psychiatry Neurol Sci. 1988;237:351–364. doi: 10.1007/BF00380979. [DOI] [PubMed] [Google Scholar]
- 23.Loranger AW. Sex difference in age at onset of schizophrenia. Arch Gen Psychiatry. 1984;41:157–161. doi: 10.1001/archpsyc.1984.01790130053007. [DOI] [PubMed] [Google Scholar]
- 24.Aleman A, Kahn RS, Selten JP. Sex differences in the risk of schizophrenia: evidence from meta-analysis. Arch Gen Psychiatry. 2003;60:565–571. doi: 10.1001/archpsyc.60.6.565. [DOI] [PubMed] [Google Scholar]
- 25.DeLisi LE. The significance of age of onset for schizophrenia. Schizophr Bull. 1992;18:209–215. doi: 10.1093/schbul/18.2.209. [DOI] [PubMed] [Google Scholar]
- 26.Leung A, Chue P. Sex differences in schizophrenia, a review of the literature. Acta Psychiatr Scand Suppl. 2000;401:3–38. doi: 10.1111/j.0065-1591.2000.0ap25.x. [DOI] [PubMed] [Google Scholar]
- 27.Agid O, Remington G, Kapur S, Arenovich T, Zipursky RB. Early use of clozapine for poorly responding first-episode psychosis. J Clin Psychopharmacol. 2007;27:369–373. doi: 10.1097/jcp.0b013e3180d0a6d4. [DOI] [PubMed] [Google Scholar]
- 28.Chang JS, Ahn YM, Park HJ, et al. Aripiprazole augmentation in clozapine-treated patients with refractory schizophrenia: an 8-week, randomized, double-blind, placebo-controlled trial. J Clin Psychiatry. 2008;69:720–731. doi: 10.4088/jcp.v69n0505. [DOI] [PubMed] [Google Scholar]
- 29.Agid O, Kapur S, Arenovich T, Zipursky RB. Delayed-onset hypothesis of antipsychotic action: a hypothesis tested and rejected. Arch Gen Psychiatry. 2003;60:1228–1235. doi: 10.1001/archpsyc.60.12.1228. [DOI] [PubMed] [Google Scholar]
- 30.Emsley R, Rabinowitz J, Medori R. Time course for antipsychotic treatment response in first-episode schizophrenia. Am J Psychiatry. 2006;163:743–745. doi: 10.1176/ajp.2006.163.4.743. [DOI] [PubMed] [Google Scholar]
- 31.Leucht S, Busch R, Hamann J, Kissling W, Kane JM. Early-onset hypothesis of antipsychotic drug action: a hypothesis tested, confirmed and extended. Biol Psychiatry. 2005;57:1543–1549. doi: 10.1016/j.biopsych.2005.02.023. [DOI] [PubMed] [Google Scholar]
- 32.Levine SZ, Rabinowitz J, Engel R, Etschel E, Leucht S. Extrapolation between measures of symptom severity and change: an examination of the PANSS and CGI. Schizophr Res. 2008;98:318–322. doi: 10.1016/j.schres.2007.09.006. [DOI] [PubMed] [Google Scholar]
- 33.Schooler N, Rabinowitz J, Davidson M, et al. Risperidone and haloperidol in first-episode psychosis: a long-term randomized trial. Am J Psychiatry. 2005;162:947–953. doi: 10.1176/appi.ajp.162.5.947. [DOI] [PubMed] [Google Scholar]
- 34.Kay SR. Positive-negative symptom assessment in schizophrenia: psychometric issues and scale comparison. Psychiatr Q. 1990;61:163–178. doi: 10.1007/BF01064966. [DOI] [PubMed] [Google Scholar]
- 35.Kay SR, Opler LA, Lindenmayer JP. The Positive and Negative Syndrome Scale (PANSS): rationale and standardisation. Br J Psychiatry. 1989;158(suppl 7):59–67. [PubMed] [Google Scholar]
- 36.Rabinowitz J, De Smedt G, Harvey PD, Davidson M. Relationship between premorbid functioning and symptom severity as assessed at first episode of psychosis. Am J Psychiatry. 2002;159:2021–2026. doi: 10.1176/appi.ajp.159.12.2021. [DOI] [PubMed] [Google Scholar]
- 37.Cannon-Spoor HE, Potkin SG, Wyatt RJ. Measurement of premorbid adjustment in chronic schizophrenia. Schizophr Bull. 1982;8:470–484. doi: 10.1093/schbul/8.3.470. [DOI] [PubMed] [Google Scholar]
- 38.Harvey PD, Artiola i Fortuny L, Vester-Blockland E, De Smedt G. Cross-national cognitive assessment in schizophrenia clinical trials: a feasibility study. Schizophr Res. 2003;59:243–251. doi: 10.1016/s0920-9964(02)00153-6. [DOI] [PubMed] [Google Scholar]
- 39.Odgers CL, Caspi A, Broadbent JM, et al. Prediction of differential adult health burden by conduct problem subtypes in males. Arch Gen Psychiatry. 2007;64:476–484. doi: 10.1001/archpsyc.64.4.476. [DOI] [PubMed] [Google Scholar]
- 40.Barker ED, Seguin JR, White HR, et al. Developmental trajectories of male physical violence and theft: relations to neurocognitive performance. Arch Gen Psychiatry. 2007;64:592–599. doi: 10.1001/archpsyc.64.5.592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shaw P, Lerch J, Greenstein D, et al. Longitudinal mapping of cortical thickness and clinical outcome in children and adolescents with attention-deficit/hyperactivity disorder. Arch Gen Psychiatry. 2006;63:540–549. doi: 10.1001/archpsyc.63.5.540. [DOI] [PubMed] [Google Scholar]
- 42.Lacourse E, Nagin DS, Vitaro F, Cote S, Arseneault L, Tremblay RE. Prediction of early-onset deviant peer group affiliation: a 12-year longitudinal study. Arch Gen Psychiatry. 2006;63:562–568. doi: 10.1001/archpsyc.63.5.562. [DOI] [PubMed] [Google Scholar]
- 43.Nagin DS, Tremblay RE. Parental and early childhood predictors of persistent physical aggression in boys from kindergarten to high school. Arch Gen Psychiatry. 2001;58:389–394. doi: 10.1001/archpsyc.58.4.389. [DOI] [PubMed] [Google Scholar]
- 44.Haviland AM, Nagin DS. Causal inferences with group based trajectory models. Psychometrika. 2005;70:557–578. [Google Scholar]
- 45.Nagin DS, Tremblay RE. Analyzing developmental trajectories of distinct but related behaviors: a group-based method. Psychol Methods. 2001;6:18–34. doi: 10.1037/1082-989x.6.1.18. [DOI] [PubMed] [Google Scholar]
- 46.Raferty AE. Bayesian model selection in social research. Sociol Methodol. 1995;25:111–196. [Google Scholar]
- 47.Reichenberg A, Harvey PD, Bowie CR, et al. Neuropsychological function and dysfunction in schizophrenia and psychotic affective disorders. [published online ahead of print May 20, 2008] Schizophr Bull. 2008 doi: 10.1093/schbul/sbn044. doi: 10.1093/schbul/sbn044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Brill N, Reichenberg A, Rabinowitz J, et al. Accuracy of self-reported premorbid functioning in schizophrenia. Schizophr Res. 2007;97:103–108. doi: 10.1016/j.schres.2007.05.026. [DOI] [PubMed] [Google Scholar]
- 49.Association AP. Diagnostic and Statistical Manual of Mental Disorders. 4 ed. Washington, DC: American Psychiatric Press; 1994. [Google Scholar]
- 50.Rabinowitz J, Bromet E, Davidson M. Are patients enrolled in first episode psychosis drug trials representative of those treated in routine clinical practice? Schizoph Res. 2003;61:149–155. doi: 10.1016/s0920-9964(02)00322-5. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.