Abstract
Epidemiological studies suggest that auditory verbal hallucinations (AVH) occur in approximately 10%–15% of the general population, of whom only a small proportion has a clinically relevant psychotic disorder. It is unclear whether these hallucinations occur as an isolated phenomenon or if AVH in nonclinical individuals are part of a more general susceptibility to schizophrenia. For this study, 103 healthy individuals with frequent AVH were compared with 60 controls matched for sex, age, and education. All participants were examined by a psychiatrist using standardized diagnostic interviews and questionnaires. The individuals with AVH did not have clinically defined delusions, disorganization, or negative or catatonic symptoms, nor did they meet criteria for cluster A personality disorder. However, their global level of functioning was lower than in the controls and there was a pronounced increase on all subclusters of the Schizotypal Personality Questionnaire (SPQ) and the Peters Delusion Inventory, indicating a general increased schizotypal and delusional tendency in the hallucinating subjects. History of childhood trauma and family history of axis I disorders were also more prevalent in these individuals. We showed that higher SPQ scores, lower education, and higher family loading for psychiatric disorders, but not presence of AVH, were associated with lower global functioning. Our data suggest that AVH in otherwise healthy individuals are not an isolated phenomenon but part of a general vulnerability for schizophrenia.
Keywords: hallucinations, healthy, spectrum, schizotypy, functioning
Introduction
Auditory verbal hallucinations (AVH) are a characteristic symptom of schizophrenia.1 Population studies demonstrated that AVH are not specific for schizophrenia but also occur in nonclinical subjects. For example, Tien2 reported a lifetime prevalence for AVH of 10% in men and 15% in women in the United States. Similar prevalences have been reported in France (16%)3 and New Zealand (13%).4 Johns et al5 found that 25% of subjects reporting hallucinations met criteria for psychosis. Little is currently known about the other 75%, ie, individuals with AVH who are not in need of treatment. AVH in healthy subjects may exist as an isolated symptom, which would suggest that the predisposition to experience AVH can be present separately from the vulnerability to other aspects of schizophrenia. Alternatively, nonclinical subjects with AVH may have an attenuated form of schizophrenia, for instance with a paranoid tendency, subclinical levels of disorganization, mild negative symptoms, and decreased global functioning. In that case, these subjects may share vulnerability factors with schizophrenia patients. In order to differentiate between these 2 possibilities, we investigated a substantial sample of subjects with AVH after screening for DSM-IV, axis I and II pathology using standardized diagnostic interviews in all participants. A total of 115 nonclinical subjects with AVH and 60 control subjects matched for age, sex, and education were assessed for psychiatric diagnosis, Global Assessment of Functioning (GAF), family history of psychiatric disorders, schizotypal tendency, delusion proneness, personality structure, and history of childhood trauma. We hypothesized that healthy individuals with AVH differ from matched controls without AVH, in particular, that they would show elevated levels of paranoid and schizotypal tendency, family history of psychiatric disorder and history of childhood trauma, and lower levels of global functioning.
Methods
Subjects
A Web site providing information about hearing voices was designed specifically for this study (www.verkenuwgeest.nl) and advertised by interviews on radio, television, and newspapers. Visitors of this Web site were invited to fill out a questionnaire on AVH, based on a modified version of the Launay and Slade Hallucination Scale (LSHS),6 a self-report questionnaire designed to quantify the tendency to hallucinate in healthy individuals.
Between March 2006 and March 2008, 15 538 subjects visited this Web site, of whom 4135 completed the questionnaire. Subjects with high scores on item 4 and 9 of the LSHS (item 4: “In the past I have had the experience of hearing a person's voice and then found that there was no-one there,” item 9: “I have been troubled by hearing voices in my head”) were selected. Trained psychologists interviewed these subjects by telephone. Subjects were included if they met the following inclusion criteria: (1) voices were distinct from thoughts and had a “hearing” quality, (2) voices were experienced at least once a month, (3) no diagnosis or treatment for psychiatric disorders other than depressive or anxiety disorders in remission, (4) no alcohol or drug abuse for at least 3 months, (5) no chronic somatic disorder, (6) 18 years of age or older, and (7) 4 Dutch-born grandparents (to restrict heterogeneity for later genetic studies).
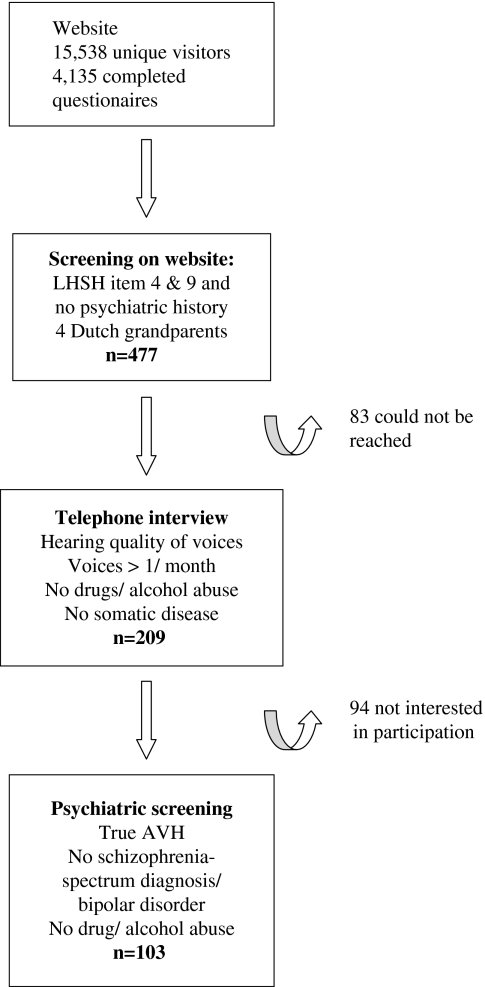
A total of 477 subjects had a summed score of at least 7 on the items 4 and 9. From these, 83 could not be reached by telephone and another 94 were not interested in participation. Several subjects were found unsuitable for inclusion: 98 did not fulfill criterion 1, 18 did not meet criterion 2, 60 did not meet criterion 3, and 9 did not meet criterion 4. The selection procedure is illustrated in figure 1.
Fig. 1.
Flow diagram of the selection procedure.
A total of 115 individuals fulfilled all criteria and agreed to participate. Sixty control subjects who scored zero on item 4 and 9 of the LSHS and also met criteria 3–7 were recruited from the same Web site. Control subjects were matched for sex, age, and education.
The study was approved by the Humans Ethics Committee of the University Medical Center Utrecht. After complete description of the study to the participants, written informed consent was obtained.
Measurements
Psychiatric Assessments.
All individuals were assessed by a trained psychiatrist for affective and psychotic DSM-IV axis I pathology using the Comprehensive Assessment of Symptoms and History (CASH).7 Global functioning was estimated using the GAF Scale. GAF was scored as the highest level of functioning over the past year, defined by the lowest score in social, psychological, or professional functioning. The presence of AVH was not interpreted as a “severe psychiatric symptom,” which would have led to a maximum GAF score of 50 for all individuals with hallucinations.
To assess axis II pathology, the structured clinical interview for personality disorder (SCID)-II interview8 was added to the psychiatric screening 6 months after the start of the study. The first 43 subjects with AVH were therefore not assessed with the SCID-II interview nor were the 60 control subjects. Psychiatric disorders in family members of the participants were quantified using the Family Interview for Genetic Studies.9 Urine samples were obtained to screen for drug abuse (cannabis, amphetamine, cocaine, methadone, and heroine). Positive screen for either of these substances led to exclusion.
Hallucinations.
Characteristics of the hallucinations were assessed in an interview composed of the PSYRATS Auditory Hallucinations Rating Scale10 and the LSHS.
Questionnaires.
In addition to the interview, subjects filled out the Schizotypal Personality Questionnaire (SPQ),11 the Peters Delusion Inventory (PDI),12 the Revised NEO Personality Inventory (NEO-PI-R),13 and the brief version of the Child Trauma Questionnaire (CTQ),14 assessing schizotypal tendency, delusional tendency, personality structure (the “Big Five”), and childhood trauma, respectively.
Statistics.
Scores were compared between groups with and without AVH using 2-tailed independent sample t tests (total scores) or multivariate general linear models (GLMs) and independent samples (subscores). Fisher Exact test was used to test differences in the prevalence of affective disorders and suicide attempts. Multivariate GLM with the number of family members as a covariate was used to compare family loading for psychiatric disorders and inflated type I error rate due to multiple testing. We used logistic regression with membership to the AVH or control group as dependent variable and schizotypal tendency, personality structure, childhood trauma, and family loading as predictors to control for possible confounding. Due to the strong correlation between subscores, we entered either total scores or the most significant subscore in the regression model in order to avoid collinearity. We subsequently used linear regression with GAF score as the dependent variable and our main outcome measures as indicators to investigate the impact of these measures on global functioning. Explorative correlation analyses were performed with either Spearman correlation or Pearson correlation depending on the distribution of the variables. All analyses were conducted using the statistical package for social sciences (SPSS version 12.1).
Results
Exclusions
From 115 individuals in the AVH group, 2 were excluded because they were not regarded as experiencing hallucinations. Based on the CASH interview, 5 subjects were diagnosed with schizophrenia, 2 with bipolar disorder, and 3 with alcohol or drug abuse. Because we aimed to describe healthy subjects with AVH, these 12 subjects (11%) were excluded from further analyses. None of the controls met criteria for current psychiatric disorder. No subjects of either group had a positive urine test for illicit drugs.
Data on 103 subjects with AVH (73 females and 30 males) and 60 subjects without AVH (42 females and 18 males) were used for further analysis.
Demographic Variables
Because the subjects of both groups were matched for sex, age, and education, there were no significant differences between the groups on these variables. Other demographic measures were also similar between the groups: the percentage that was married or divorced, the mean number of children, and the mean income and the percentage of subjects that had needed extra help at school (remedial teaching or coaching) or had received special education. Subjects with AVH were right-handed in only 80% of the cases compared with 87% in the controls, which was a significant difference. The mean values for these demographic variables are summarized in table 1.
Table 1.
Demographic Variables of the Samples
| Subjects With AVH (n = 103) | Subjects Without AVH (n = 60) | Statistic | P Value | |
| Age, y (SD) | 44 (13), range = 19–64 | 46 (15), range = 22–60 | F = 1.0, df = 153 | .1 |
| Married (%) | 54 | 48 | F = 0.47, df = 153 | .49 |
| Divorced (%) | 22 | 33 | F = 1.1, df = 153 | .29 |
| Mean number of children (SD) | 1.9 (0.4) | 1.7 (0.3) | F = 1.06, df = 153 | .3 |
| Mean income (€/mo) | 2238.7 | 2213.4 | F = 2.67, df = 153 | .1 |
| Years of education (SD) | 13 (6) | 12 (5) | F = 0.8, df = 153 | .37 |
| Extra help at school or special education (%) | 45 | 44 | F = 0.19, df = 153 | .66 |
| Hand preference (% right handed) | 80 | 87 | F = 11.8, df = 153 | .001 |
Note: AVH, Auditory verbal hallucinations.
Hallucinations
Individuals with AVH had experienced this symptom for a mean period of 29 years (SD = 17, range = 2–56). Their mean age at first experiencing voices was 14 (SD = 14, range = 2–57). Over the last week, subjects had experienced a mean of 3.6 (SD = 1.4) AVH. The mean duration of the AVH was 128 seconds (SD = 153). Eighteen percent of the subjects had commenting voices, and 11% had voices speaking with each other, which are considered first-rank symptoms.15 The majority (71%) never heard AVH with a negative content, 25% heard both positive and negative messages, while 4% experienced AVH with a negative content only. The large majority (91%) reported no disturbance of daily life by their voices, 9% experienced moderate disturbance by the AVH, and none of them experienced severe disturbances. From the 103 subjects with AVH, 58% attributed the voices to an external source, mostly benevolent spirits. Sixteen percent believed that the AVH were internally generated, and 27% were uncertain about the origin of the voices. Fifty-five percent reported that they could stop the AVH at inconvenient moments. Most individuals with AVH experienced hallucinations in several modalities, such as visual (lifetime prevalence = 79%), taste (lifetime prevalence = 25%), olfactory (lifetime prevalence = 63%), and tactile (lifetime prevalence = 53%). Several subjects from the control group had also experienced hallucinations in other modalities: 50% visual, 13% taste, 39% olfactory, and 22% tactile, but not in the auditory domain.
Launey Slade Hallucination Scale
The LSHS was available from all participants. The mean total score on the LSHS was 40 (SD = 11) for subjects with AVH and 6 (SD = 5) for controls (t = 21.0, df = 162, P < .0001). Mean scores on subgroups of the LSHS are shown in table 2.
Table 2.
Mean Scores, SD, and Statistics of the Main Outcome Measures
| Measure | Subjects With AVH (n = 103) | Subjects Without AVH (n = 60) | Statistic | P Value |
| Hallucinatory Experiences (LSHS) | ||||
| Total score | 40.0 (11.1) | 5.9 (4.6) | t = 212, df = 162 | <.001 |
| Sleep related (SD) | 6.1 (2.4) | 1.4 (1.8) | F = 147 | <.001 |
| Vivid daydreams (SD) | 7.3 (3.2) | 0.9 (1.6) | F = 179 | <.001 |
| Intrusive thoughts (SD) | 7.3 (4.2) | 1.9 (1.8) | F = 78 | <.001 |
| Auditory hallucinations (SD) | 7.3 (2.6) | 0.1 (0.4) | F = 406 | <.001 |
| Visual hallucinations (SD) | 8.5 (3.6) | 0.7 (1.4) | F=227 | <.001 |
| Schizotypy (SPQ) | ||||
| Total (SD) | 26 (11.0) | 8 (6.0) | t = 12.8, df = 162 | <.001 |
| Cognitive-perceptual (SD) | 15.4 (5.7) | 3.7 (3.1) | F = 207.0 | <.001 |
| Disorganization (SD) | 5.7 (3.8) | 2.2 (2.3) | F = 38.1 | <.001 |
| Interpersonal (SD) | 5.6 (5.0) | 2.6 (2.5) | F = 17.5 | <.001 |
| Personality (NEO-PI-R) | ||||
| Neuroticism (SD) | 139.3 (12.2) | 138.6 (8.0) | F = 2.286 | .133 |
| Extraversion (SD) | 144.5 (10.8) | 144.1 (7.1) | F = 1.921 | .168 |
| Openness (SD) | 148.0 (11.3) | 143.5 (9.2) | F = 5.776 | .018 |
| Agreeableness (SD) | 148.8 (11.9) | 150.4 (8.9) | F = 0.056 | .813 |
| Conscientiousness (SD) | 155.4 (8.1) | 155 (7.2) | F = 0.021 | .885 |
| Childhood trauma (CTQ) | ||||
| Total | 31.2 (11.1) | 24.1 (4.4) | t = 5.2, df= 153 | <.001 |
| Emotional abuse (SD) | 9.8 (4.9) | 7 (2.2) | F = 23.21 | <.001 |
| Physical abuse (SD) | 6.3 (3.3) | 5.5 (1.5) | F = 4.18 | .043 |
| Sexual abuse (SD) | 7.3 (4.5) | 5.7 (1.3) | F = 9.60 | .002 |
| Emotional neglect (SD) | 1.7 (0.8) | 1.5 (0.5) | F = 5.56 | .020 |
| Physical neglect (SD) | 4.7 (1.2) | 4.4 (0.7) | F = 2.02 | .158 |
| Delusional Tendency (PDI) | ||||
| Preoccupation | 13.6 (6.5) | 3.5 (2.8) | F = 90 | <.001 |
| Conviction | 13.2 (7.4) | 3.8 (2.8) | F = 84 | <.001 |
| Distress | 3.7 (4.9) | 0.9 (1.1) | F = 15 | <.001 |
| Family loading (FIGS) | ||||
| Total | 0.13 (0.12) | 0.05 (0.08) | t = 4.6 df = 157 | <.001 |
| Depression (SD) | 0.07 (0.09) | 0.03 (0.06) | F = 4.14 | .02 |
| Psychosis | 0.009 (0.02) | 0.0009 (0.007) | F = 2.83 | .06 |
| Mania | 0.005 (0.02) | 0 (0) | F = 3.06 | .05 |
| Alcohol/drugs | 0.04 (0.06) | 0.02 (0.04) | F = 3.86 | .02 |
| Personality disorder | 0.005 (0.02) | 0.004 (0.002) | F = 0.126 | .287 |
Note: AVH, Auditory Verbal Hallucinations; SPQ, Schizotypal Personality Questionnaire; LSHS, Launay and Slade Hallucination Scale; PDI, Peters Delusion Inventory; CTQ, Childhood Trauma Questionnaire; FIGS, Family Interview for Genetic Studies
Diagnosis and GAF
Axis I
Many subjects with AVH and a substantial part of the controls reported paranormal beliefs, frequently about predestination and the existence of entities. Because these ideas are generally accepted in a large subgroup of the Western population,16 they were not scored as delusions. Disorganization, catatonic, or negative symptoms were absent in both groups. Twelve subjects with AVH fulfilled criteria for a single depressive episode in complete remission, 4 met criteria for recurrent depressive episodes, in full remission, and one subject obtained diagnosis of dysthymia, in complete remission, the others did not meet criteria for DSM-IV diagnosis of psychotic or affective disorder.
In the control group, 5 met criteria for single depressive episode in complete remission, 2 for recurrent depressive episodes, in full remission, and 2 subjects obtained diagnosis of dysthymia, in complete remission. The prevalence of affective disorder was similar in both groups (Fisher Exact test, P = 1.0). Eleven subjects with AVH, but none of the controls, ever made a suicide attempt (Fisher Exact test, P = .007).
Axis II.
Complete SCID-II interviews were available from 60 subjects with AVH. There were no significant differences in age, sex, education, and psychopathology between the 60 subjects who completed the SCID-II interview, and the 43 who were not assessed due to the late start of the SCID-II interview, suggesting that no selection bias has occurred. From the 60 subjects with AVH who completed this interview, 2 fulfilled criteria for borderline personality disorder, 1 for histrionic personality disorder, and 1 for narcissistic personality disorder.
Global Assessment of Functioning.
GAF scores were available from all participants. The mean GAF score was 82 (SD = 7) for the subjects with AVH and 87 (SD = 5) for the controls (t = −5.5, P < .001).
Family Interview for Genetic Studies
The Family Interview for Genetic Studies was completed for all subjects. After controlling for the number of first- and second-degree family members, relatives of participants with AVH had significantly higher prevalences of depression (F = 4.14, P = .018), substance abuse (F = 3.9, P = .02), and mania (F = 3.1, P = .05). A similar trend was present for psychosis (F = 2.8, P = .06) but not for personality disorder. Data are provided in table 2.
Schizotypal Personality Questionnaire
All participants completed the SPQ. Mean score on the SPQ was 26 (SD = 11) for subjects with AVH and 8 (SD = 6) for controls (t = 12.8, P < .0001). The increased SPQ score in the AVH group was not caused by a subgroup with extreme SPQ scores but resulted from a general increase in SPQ score of the whole group (figure 2). Analysis of the item clusters of the SPQ showed higher scores in subjects with AVH for all clusters (cognitive-perceptual: F157,3 = 207, P < .0001, disorganization: F157,3 = 38, P < .0001, interpersonal: F157,3 = 17.5, P < .0001). Means are shown in table 2.
Fig. 2.
Frequency histograms of the total SPQ score for control subjects and for subjects with AVH.
Peters Delusion Inventory
All participants completed the PDI. Analysis of summed total scores showed higher scores for preoccupation with delusional ideas in hallucinating individuals (F160,3 = 90, P < .0001) than in controls. They also scored higher on conviction (F160,3 = 84, P < .0001) and distress (F160,3 = 15, P < .001). Means are provided in table 2.
Revised NEO Personality Inventory
Completed NEO-PI-R questionnaires were available from 94 subjects with AVH and from all controls. Analysis of the 5 clusters (“Big Five”) yielded higher scores for hallucinating subjects for the cluster “Openness to Experiences” (F147,5 = 5.8, P = 0.02), which was caused by higher scores on the subcluster “Esthetics.” Mean scores for all clusters are provided in table 2.
Child Trauma Questionnaire
Completed CTQs were available from all control subjects and from 94 participants with AVH. Higher scores were found for the individuals with AVH on 4 of the 5 subclusters. Mean scores on these subclusters are provided in table 2.
We found significant correlations between total trauma score and total scores on the PDI and SPQ in both groups. Within the AVH group, trauma was correlated with the SPQ and PDI scores (r = 0.39, P = .002) and (r = 0.54, P < .001), respectively. In the control group, these correlations were lower: 0.28 (P = .008) for both measures.
Combined Analysis
A logistic regression model predicting presence or absence of AVH had a good fit (goodness-of-fit test, χ2 = 127.4, P < .001), and the Nagelkerke approximation of R2 was high: 0.80. PDI scores were removed from the model due to high correlation with SPQ scores (Pearson r = 0.69, P < .001); inclusion would have lead to unacceptable collinearity. Table 3 shows that SPQ score was the most significant indicator of the model (P < .001). Family loading for psychiatric disorders showed borderline significance (P = .054).
Table 3.
Logistic Regression Model: Variables Prediction Presence/Absence of Auditory Verbal Hallucinations
| B | SE | Wald | Significance | |
| SPQ total | 0.14 | 0.03 | 29.17 | <.001* |
| Total trauma | 0.04 | 0.05 | 0.64 | .424 |
| Family loading | 5.99 | 3.10 | 3.73 | .054 |
| NEO-PI-R Openness | 0.01 | 0.03 | 0.11 | .740 |
Note: NEO-PI-R Revised NEO Personality Inventory.
Significant at .05 level.
To investigate the impact of AVH and the other measures on global functioning, we used a linear regression model with GAF score as outcome measure and gender, education, total trauma score, NEO-personality, family loading for psychiatric disorders, and SPQ as indicators. PDI scores were treated similarly as in the logistic regression. The model had a good fit (analysis of variance, F = 6.3, df = 8, P < .001) but limited R2 (0.24). Family loadings for psychiatric disorders, number of years of education, and SPQ scores significantly influenced global functioning, while presence of AVH did not (table 4).
Table 4.
Linear Regression Model: Variables Predicting GAF Score
| B | SE | t | Significance | |
| NEO-PI-R Openness | –0.05 | 0.057 | –0.91 | 0.36 |
| Family loading | –9.69 | 4.786 | –2.03 | 0.04* |
| Total trauma | 0.03 | 0.057 | 0.43 | 0.67 |
| SPQ total | –0.07 | 0.024 | –2.95 | 0.004* |
| Age | –0.05 | 0.039 | –1.21 | 0.23 |
| Years of education | 0.59 | 0.218 | 2.70 | 0.008* |
| Gender | 0.90 | 1.136 | 0.79 | 0.43 |
| AVH (present/absent) | –1.37 | 1.435 | –0.96 | 0.34 |
Note: GAF, Global Assessment of Functioning; NEO-PI-R Revised NEO Personality Inventory; SPQ, Schizotypal Personality Questionnaire; AVH, auditory verbal hallucinations.
Significant at P < .05 level.
Discussion
This study describes a healthy group with AVH and assesses whether AVH in this group occurre as an isolated phenomenon or was part of a subtle schizotypal tendency. The experimental group consisted of 103 individuals selected through a Web site, who had experienced AVH for a long time (mean period of 29 years) mostly since early adolescence. Apart from AVH, they also had increased prevalences of other perceptual abnormalities, such as sleep-related hallucinatory experiences, visual hallucinations, vivid day dreams, and intrusive thoughts. This group was contrasted to 60 individuals, matched for age, sex, and education who never experienced AVH and were selected using the same procedure. After standardized psychiatric assessments for DSM-IV axis I and II pathology in face-to-face interviews by trained psychiatrists, we found that the subjects with AVH did not have clinically relevant delusions, disorganization, or negative symptoms, nor did they meet criteria for schizotypal, schizoid, or paranoid personality disorder. Moreover, prevalences of other personality disorders were similar to those observed in the normal population.17 Despite the absence of clinical symptoms other than the hallucinations, pronounced differences between the control and the AVH group were found in nonpathologic schizotypal and delusional tendencies by means of the SPQ and the PDI, respectively. In addition to high scores on positive items of the SPQ, such as perceptual abnormalities and magical thinking, subjects with AVH also scored higher on negative items and disorganization. Increased mean SPQ scores could not be attributed to a subgroup with extreme SPQ scores but resulted from a general increase in SPQ score of the whole group with AVH. These findings suggest that in healthy individuals, who function within the normal range, the presence of AVH is associated with subclinical levels of other schizotypal phenomena. There is a strong indication that high SPQ scores are related to increased genetic vulnerability to psychosis.18 Indeed, the subjects with AVH also had increased family loading for psychosis, which almost reached statistical significance (P = 0.055). Family loading for other psychiatric disorders in this group was also higher than in the controls. Considering the shared genetic vulnerability to different psychiatric disorders,19 both high SPQ scores and increased rates of axis-I disorders in relatives are suggestive for a genetic predisposition for schizophrenia in the group with AVH.
In addition to a possible genetic predisposition for psychosis, subjects with AVH had a higher prevalence of childhood trauma, indicating that environmental risk factors may also be shared between healthy subjects with AVH and those with psychosis. Although childhood trauma was still relatively uncommon in the hallucinating group as compared with prevalances in patients with schizophrenia,20,21 it was statistically associated with the presence of AVH. An association between childhood trauma and AVH has consistently been reported, both in individuals who appear otherwise healthy20 and in clinical subjects.21 The total trauma score was highly correlated to SPQ and particularly to PDI scores, and our data suggest that the association between trauma and presence of AVH was mainly determined by the effect on SPQ scores, suggesting that childhood trauma leads to an altered (more paranoid) perception of the world as reflected in increased SPQ and PDI scores, which in turn may confer risk to AVH. An alternative explanation is that childhood trauma is more likely in families with a (possibly genetic) predisposition to schizotypal behavior.
Analysis of the NEO-PI-R questionnaires showed that the single difference between the groups was a higher score on the item “Openness for Experiences” in the AVH group. Other studies also found an association between neuroticism and hallucinations.23–29 This discrepancy may be related to the older age of subjects included in this study. Indeed, Larøi et al22 found an association between hallucination proneness and neuroticism only in the young adult sample (who were in their 20s) and not in their elderly sample. Therefore, neuroticism may not play an important role later in life. A study assessing personality in unaffected parents of schizophrenia patients30 using the NEO-PI-R, also found an increase in the item “Openness for Experiences” only, indicating that there may be an association between psychosis proneness and this personality item.
Although the subjects with AVH functioned within the normal range, their mean GAF score was lower than that in controls, despite the fact that the control group was matched for sex, age, and education. The difference was predominantly attributable to lower levels of occupational functioning in the hallucinating individuals.
Combined analysis of the measurements showed that schizotypal tendency was the most significant risk factor for AVH followed by family loading for axis I psychiatric disorders, suggesting that (genetic) vulnerability to schizophrenia (reflected in high SPQ scores and family loading for psychiatric disorders) is the main risk factor for AVH. The linear regression model showed that schizotypal tendency, family loading for psychiatric disorders, and low education are associated with low global functioning, while personality, childhood trauma, and presence of AVH do not predict global functioning. The finding that presence of AVH does not predict lower global functioning is in agreement with the majority of the hallucinating participants (91%) reporting minimal interference by their voices in social and occupational functioning. A possible reason why their voices were not disturbing may be that, in contrast to patients with schizophrenia,31 voices of the healthy individuals predominantly had a positive emotional content. The difference in emotional content of AVH between clinical and nonclinical subjects has been observed previously32,33 and indicates that emotional content constitutes an important difference between more benign hallucinations and psychopathology. Indeed, the few participants from this sample who experienced AVH with a negative content had higher distress from the voices and lower global functioning (mean GAF score of 75). It could be hypothesized that not the presence of AVH per see, but rather the negative emotional content of voices and perceived distress, play a role in disability.
Although the hallucinating subjects experienced little discomfort from the AVH, and their AVH may be characterized as “benign,” the absence of a major psychiatric diagnosis in these individuals can be disputed. When strict DSM-IV criteria for axis I were applied, all 103 subjects with AVH would meet criteria for psychosis not otherwise specified (NOS). The participants experienced AVH for a mean period of 29 years, thus fulfilling the criterion “persistent hallucinations,” which in itself is sufficient for this classification. The fact that the hallucinating subjects were functioning normally, with a mean GAF score of 82, and not in need of treatment, indicates that the diagnosis “psychosis NOS” is clinically inappropriate. Indeed, in order to make this diagnosis, AVH should be “…associated with present distress or disability or with a significantly increased risk of suffering death, pain, ....” (page xxxi in DSM-IV-Text Revision). However, for many DSM-IV diagnoses (ie, schizophrenia, substance abuse, personality disorder, and anxiety disorders), an explicit diagnostic criterion is that symptoms have to lead to dysfunction, while psychosis NOS lacks this criterion. In parallel, International Classification of Diseases, Tenth Revision, criteria F29 for unspecified nonorganic psychosis also include “chronic hallucinatory psychosis NOS,” in which dysfunction is not explicitly required. Historically, the presence of persistent hallucinations has been regarded as abnormal, such that its sole presence would justify a diagnosis of psychopathology.34 Given the current insight that AVH also occur in nonclinical subjects,35 it could be recommended to add the criterion “leading to significant dysfunction” in the next versions of diagnostic criteria for psychosis NOS.
When comparing our study with previous work,2–6 the difference between this study and earlier reports on AVH in healthy subjects is that we have examined each individual in person using standardized psychiatric assessments, while other authors have used self-rating questionnaires or telephone interviews performed by trained lay people. Some studies did use psychiatric interviews to confirm the presence of axis I diagnosis in subjects with highest scores,5 but except for Honig et al32 who assessed 18 healthy subjects with AVH, no previous studies used psychiatric interviewing to assess the whole sample of subjects with AVH. The value of a clinical psychiatric interview should not be underestimated. In face-to-face contact, many schizophrenia-related features such as social anxiety, affective flattening or inappropriate affect, thought and language disturbances, and inappropriate or disorganized behavior can be assessed, which may easily be missed using telephone or mail contact. To our opinion, face-to-face clinical interviews are the only valid method to assess presence or absence of axis I and II disorder, especially in this group of individuals who are just above the border between full mental health and subtle psychopathology.
Limitations
The main limitation of this study is that participants are highly selected and therefore may not represent subjects with hallucinations in general nor subjects with subthreshold psychotic symptoms in general. We here report on subjects who accepted our invitation to participate in this study, which may have selected predominantly individuals who feel confident to speak about their voices and may have excluded the more suspicious or shy individuals. Perhaps this is the reason why our sample was relatively old (mean age 44 years), while participants had been hearing voices for a mean of 29 years. If we would have been able to investigate all suitable subjects, we expect that scores on items such as paranoid tendency and social anxiety would have been higher, while global functioning may have been lower. Second, interviewing also the family members in person would have produced more reliable data on prevalences of psychiatric disorder in relatives. A final limitation of the study is that personality was not assessed in the controls. Although this would have strengthened the findings in the AVH group, the SCID-II interview was too time consuming to score both groups.
In conclusion, our data show that while the hallucinating individuals of this sample do not fulfill criteria for axis I or II schizophrenia spectrum disorder, they do have a general increased vulnerability to schizophrenia as reflected in increased schizotypal and delusional tendency and increased family loading for axis I psychiatric disorders, suggesting that the predisposition for AVH is similar or related to the predisposition for schizophrenia. While the presence of AVH per se has little impact on the level of global functioning, increased schizotypal tendency and higher family loading for axis I disorders are responsible for the lower level of functioning in the hallucinating individuals in comparison to subjects without AVH. In future studies, we aim to address the mechanisms that lead to AVH in the here described subjects, using psychological assessments, analyses of language samples, genetic linkage, functional magnetic resonance imaging, diffusion tensor imaging, and electroencephalograms.
Funding
Dutch Science Organisation (Nederlandse Wetenschappelijke Organisatie NWO, nr. 916.56.172).
References
- 1.Sartorius N, Jablensky A, Korten A, et al. Early manifestations and first-contact incidence of schizophrenia in different cultures. A preliminary report on the initial evaluation phase of the WHO Collaborative Study on determinants of outcome of severe mental disorders. Psychol Med. 1986;16:909–928. doi: 10.1017/s0033291700011910. [DOI] [PubMed] [Google Scholar]
- 2.Tien AY. Distributions of hallucinations in the population. Soc Psychiatry Psychiatr Epidemiol. 1991;26:287–292. doi: 10.1007/BF00789221. [DOI] [PubMed] [Google Scholar]
- 3.Verdoux H, Maurice-Tison S, Gay B, Van Os J, Salamon R, Bourgeois ML. A survey of delusional ideation in primary-care patients. Psychol Med. 1998;28:127–134. doi: 10.1017/s0033291797005667. [DOI] [PubMed] [Google Scholar]
- 4.Poulton R, Caspi A, Moffitt TE, Cannon M, Murray R, Harrington H. Children's self-reported psychotic symptoms and adult schizophreniform disorder: a 15-year longitudinal study. Arch Gen Psychiatry. 2000;57:1053–1058. doi: 10.1001/archpsyc.57.11.1053. [DOI] [PubMed] [Google Scholar]
- 5.Johns LC, Nazroo JY, Bebbington P, Kuipers E. Occurrence of hallucinatory experiences in a community sample and ethnic variations. Br J Psychiatry. 2002;180:174–178. doi: 10.1192/bjp.180.2.174. [DOI] [PubMed] [Google Scholar]
- 6.Larøi F, Marczewski P, Van der Linden M. Further evidence of the multi-dimensionality of hallucinatory predisposition: factor structure of a modified version of the Launay-Slade Hallucinations Scale in a normal sample. Eur Psychiatry. 2004;19:15–20. doi: 10.1016/S0924-9338(03)00028-2. [DOI] [PubMed] [Google Scholar]
- 7.Andreasen NC, Flaum M, Arndt S. The Comprehensive Assessment of Symptoms and History (CASH). An instrument for assessing diagnosis and psychopathology. Arch Gen Psychiatry. 1992;49:615–623. doi: 10.1001/archpsyc.1992.01820080023004. [DOI] [PubMed] [Google Scholar]
- 8.First MB, Spitzer RL, Gibbon M. Structured Clinical Interview for Personality Disorder (SCID-II): multi-site test-retest reliability study. J Pers Disorder. 1995;9:92–104. [Google Scholar]
- 9.NIMH Genetics Initiative. Family Interview for Genetic Studies (FIGS) Rockville, Md: National Institute of Mental Health; 1992. [Google Scholar]
- 10.Haddock G, McCarron J, Tarrier N, Faragher EB. Scales to measure dimensions of hallucinations and delusions: the psychotic symptom rating scales (PSYRATS) Psychol Med. 1999;29:879–889. doi: 10.1017/s0033291799008661. [DOI] [PubMed] [Google Scholar]
- 11.Raine A. The SPQ: a scale for the assessment of schizotypal personality based on DSM-III-R criteria. Schizophr Bull. 1991;17:555–564. doi: 10.1093/schbul/17.4.555. [DOI] [PubMed] [Google Scholar]
- 12.Peters ER, Joseph SA, Day S, Garety PA. Measurement delusional ideation, the 21 item version of the Petersen Delusion Inventory. Schizophr Bull. 2004;30:1005–1022. doi: 10.1093/oxfordjournals.schbul.a007116. [DOI] [PubMed] [Google Scholar]
- 13.McCrae RR, Costa PT, Jr, Martin TA. The NEO-PI-3: a more readable revised NEO Personality Inventory. J Pers Assess. 2005;84:261–270. doi: 10.1207/s15327752jpa8403_05. [DOI] [PubMed] [Google Scholar]
- 14.Gregory J, Caspi Y, Kammerer N. The assessment of trauma in women with co-occuring substance abuse and mental disorders and a history of interpersonal violence. J Behav Health Sci Res. 2005;32:113–127. doi: 10.1007/BF02287261. [DOI] [PubMed] [Google Scholar]
- 15.Nordgaard J, Arnfred SM, Handest P, Parnas J. The diagnostic status of first-rank symptoms. Schizophr Bull. 2008;34:137–154. doi: 10.1093/schbul/sbm044. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ross CA, Joshi S. Paranormal experiences in the general population. J Nerv Ment Dis. 1992;180:357–361. doi: 10.1097/00005053-199206000-00004. [DOI] [PubMed] [Google Scholar]
- 17.Sperry L. Handbook on Diagnosis and Treatment for DSM-IV-R Personality Disorder. New York: Brunner-Routledge; 2003. [Google Scholar]
- 18.Vollema MG, Sitskoorn MM, Appels MC, Kahn RS. Does the Schizotypal Personality Questionnaire reflect the biological-genetic vulnerability to schizophrenia? Schizophr Res. 2002;1:39–45. doi: 10.1016/s0920-9964(01)00350-4. [DOI] [PubMed] [Google Scholar]
- 19.Maier W, Lichtermann D, Franke P, Heun R, Falkai P, Rietschel M. The dichotomy of schizophrenia and affective disorders in extended pedigrees. Schizophr Res. 2002;1:259–266. doi: 10.1016/s0920-9964(01)00288-2. [DOI] [PubMed] [Google Scholar]
- 20.Andrew EM, Gray NS, Snowden RJ. The relationship between trauma and beliefs about hearing voices: a study of psychiatric and non-psychiatric voice hearers. Psychol Med. 2008;4:1–9. doi: 10.1017/S003329170700253X. [DOI] [PubMed] [Google Scholar]
- 21.Shevlin M, Dorahy M, Adamson G. Childhood traumas and hallucinations: an analysis of the National Comorbidity Survey. J Psychiatr Res. 2007;41:222–228. doi: 10.1016/j.jpsychires.2006.03.004. [DOI] [PubMed] [Google Scholar]
- 22.Larøi F, DeFruyt F, van Os J, Aleman A, Van der Linden M. Associations between hallucinations and personality structure in a non-clinical sample: comparison of young and elderly samples. Pers Individ Diff. 2005;39:189–200. [Google Scholar]
- 23.Young HF, Bentall RP, Slade PD, Dewey ME. Disposition towards hallucination, gender and EPQ scores. Pers Individ Diff. 1986;7:247–249. [Google Scholar]
- 24.Jakes S, Hemsley DR. Personality and reports of hallucination and imagery in a normal opulation. Percept Motor Skills. 1987;64:765–766. doi: 10.2466/pms.1987.64.3.765. [DOI] [PubMed] [Google Scholar]
- 25.Barrett TR, Etheridge JB. Verbal hallucinations in normals III: Dysfunctional personality correlates. Pers Individ Diff. 1994;16:57–62. [Google Scholar]
- 26.van Os J, Jones PB. Neuroticism as a risk factor for schizophrenia. Psychol Med. 2001;31:1129–1134. doi: 10.1017/s0033291701004044. [DOI] [PubMed] [Google Scholar]
- 27.van Os J, Jones P, Sham P, Bebbington P, Murray RM. Risk factors for onset and persistence of psychosis. Soc Psychiatry Psychiatr Epidemiol. 1998;33:596–605. doi: 10.1007/s001270050099. [DOI] [PubMed] [Google Scholar]
- 28.Krabbendam L, Janssen I, Bak M, Bijl RV, de Graaf R, van Os J. Neuroticism and low self-esteem as risk factors for psychosis. Soc Psychiatry Psychiatr Epidemiol. 2002;37:1–6. doi: 10.1007/s127-002-8207-y. [DOI] [PubMed] [Google Scholar]
- 29.Delespaul P, deVries M, van Os J. Determinants of occurrence and recovery from hallucinations in daily life. Soc Psychiatry Psychiatr Epidemiol. 2002;37:97–104. doi: 10.1007/s001270200000. [DOI] [PubMed] [Google Scholar]
- 30.Aukes MF, Alizadeh BZ, Sitskoorn MM, et al .Finding suitable phenotypes for genetic studies of schizophrenia: heritability and segregation analysis [published online ahead of print February 22, 2008] Biol Psychiatry. 2008 doi: 10.1016/j.biopsych.2007.12.013. [DOI] [PubMed] [Google Scholar]
- 31.Johns LC, Hemsley D, Kuipers E. A comparison of auditory hallucinations in a psychiatric and non-psychiatric group. Br J Clin Psychol. 2002;41:81–86. doi: 10.1348/014466502163813. [DOI] [PubMed] [Google Scholar]
- 32.Honig A, Romme M, Ensink B, Escher S, Pennings M, Devries M. Auditory hallucinations: a comparison between patients and nonpatients. J Nerv Ment Dis. 1998;186:646–651. doi: 10.1097/00005053-199810000-00009. [DOI] [PubMed] [Google Scholar]
- 33.Choong C, Hunter MD, Woodruff PW. Auditory hallucinations in those populations that do not suffer from schizophrenia. Curr Psychiatry Rep. 2007;9:206–212. doi: 10.1007/s11920-007-0020-z. [DOI] [PubMed] [Google Scholar]
- 34.VandenBosch GR, editor. APA Dictionary of Psychology. Washington, DC: American Psychological Association; 2007. p. 427. [Google Scholar]
- 35.Hanssen M, Bak M, Bijl R, Vollebergh W, van Os J. The incidence and outcome of subclinical psychotic experiences in the general population. Br J Clin Psychol. 2005;44:181–191. doi: 10.1348/014466505X29611. [DOI] [PubMed] [Google Scholar]