Abstract
Gastroesophageal reflux disease (GERD) and sleep disturbances are both common health problems. There is a significant association between disturbed sleep and GERD, and this may be bidirectional. Sleep disorders may induce gastrointestinal (GI) disturbances, while GI symptoms also may provoke or worsen sleep derangements. Reflux of gastric acid is a less frequent event during sleep, however, acid clearance mechanisms (including swallowing, salivation and primary esophageal motility) are impaired during sleep resulting in prolongation of acid contact time. Nighttime reflux can lead to sleep disturbance and sleep disturbance may further aggravate GERD by prolonged acid contact time and heightened sensory perception. This may facilitate the occurrence of complicated GERD and decreased quality of life. However, the interplay between sleep problems and GERD is complex, and there are still relatively limited data on this issue. Further investigation of sleep-related GERD may identify common pathophysiological themes and new therapeutic targets.
Keywords: Sleep, Gastroesophageal reflux disease
Introduction
Gastroesophageal reflux disease (GERD) is a common and chronic condition. At least 20% of adults in the United States report having heartburn once a week or more.1,2 Insomnia is a symptom describing difficulty initiating or maintaining sleep, or the experience of nonrefreshing sleep, and is also a very common condition; about 10% of adults in the United States report having sleep insufficiency.3
At least 50% of patients with sleep disturbance seen in primary care practices have comorbid conditions.3 Specifically, Taylor et al.4 found a higher prevalence of gastrointestinal (GI) problems in those with chronic insomnia compared with those without insomnia (33.6% vs. 9.2%; Odd ratio (OR) 3.33, 95% confidence interval (CI), 1.83-6.05). Among patients with frequent heartburn, the majority reported difficulties initiating sleep or maintaining sleep through the night. Sleep disturbances can have a significant impact on an individual's health and quality of life,5 resulting from decreased daytime functioning.
In this review, we aimed to address the complex relationships between GERD and sleep. We wished to address the following questions: (1) Does GERD contribute to the development of sleep disturbance, or vice versa? (2) If there is a significant association, is it explained by confounding or other comorbidities? (3) What physiological evidence supports a causal link? (4) Should coexisting sleep derangements in GERD change specific treatment strategies?
Systematic literature reviews, with defined inclusion and exclusion criteria, were conducted to identify the available evidence to support each statement. Literature searches were conducted in English language publications in Medline, confined to human subjects in the past 5 years. We included the following keywords in our search including "gastroesophageal reflux" or "gastroesophageal" and "reflux" or "gastroesophageal reflux" or "GERD" and "sleep". We excluded non-English language trials or studies in pediatric or adolescent patients, or meeting abstracts. Symptomatic GERD had to be diagnosed by a symptom questionnaire or by a physician. Reflux esophagitis was defined by upper endoscopy.
1. Is GERD associated with the development of sleep disturbance or vice versa, and is a link explained by confounding or comorbidities?
Sleep disturbances are common; so are GI symptoms. Is there really an association or is this observation due to chance? Recent epidemiologic studies have revealed a significant association between GERD and sleep disturbance indicating this is not a chance finding.
1) Prevalence of sleep disturbances among patients with GERD
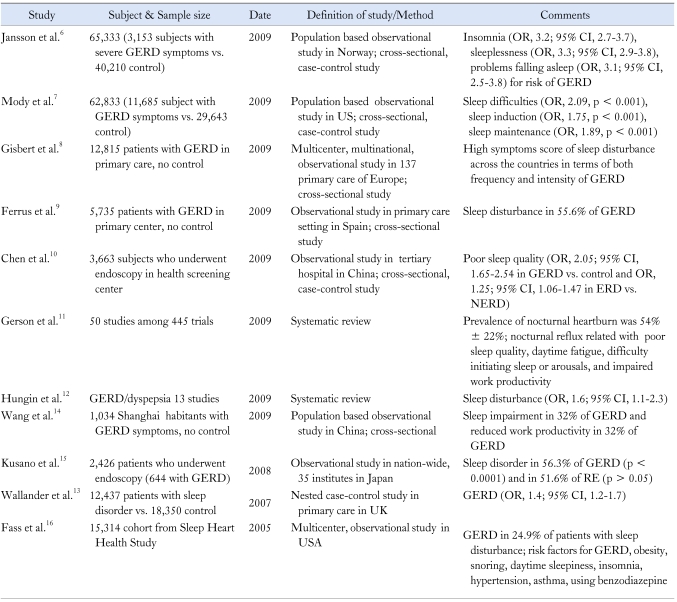
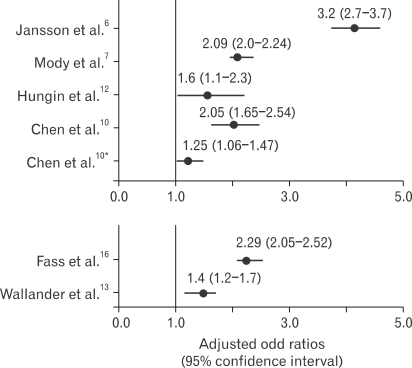
Several epidemiologic studies have shown that nighttime heartburn is prevalent and that individuals who experience nighttime heartburn have associated sleep disturbances resulting in alterations in daytime performance (Table 1, Fig. 1).6-16 A large population-based, cross sectional study based on 2 large health surveys of 1984-1986 and 1995-1997 was performed in 65,333 participants (70% of adult population) in Norway.6 They found an association between GERD symptoms and sleep problems, including insomnia (OR, 3.2; 95% CI, 2.7-3.7), sleeplessness (OR, 3.3; 95% CI 2.9-3.8) and problems falling asleep (OR 3.1, 95% CI, 2.5-3.8), adjusting for age, sex, smoking, obesity and socioeconomic status. Further they showed that the association between GERD symptoms and sleep persisted after adjusting for other comorbid conditions, such as depression or anxiety, which were themselves also associated with sleep disturbances. However, their study had inherent limitations including a cross sectional study design and reliance on self-reported symptoms of reflux and sleep. In another study based on data from the 2006 US National Health and Wellness Survey, Mody et al.7 observed that 19% of 62,833 respondents experienced heartburn at least twice a month, and among them, 89% experienced nighttime GERD symptoms, 68% sleep difficulties, 49% difficulty initiating asleep, and 58% difficulty maintaining sleep. They showed the presence of GERD was associated with more than twice the likelihood of experiencing sleep difficulties, and more specifically subjects with nighttime GERD symptoms experienced 1.5 times more sleep difficulties compared to subjects with daytime only GERD symptoms. In addition, they showed that among adults with GERD symptoms, sleep difficulties were associated with greater use of health care resources and loss of work productivity, and increased impairment of daily activities.7 Adults with GERD symptoms who experienced sleep difficulties had 5.5% greater work productivity loss than those without sleep difficulties, equating to a loss of 2.75 weeks of lost productivity per year per sufferer compared with those without sleep difficulties.7 Although this study also had limitations including being a web-based study subject to selection bias, these findings have been replicated in other studies.17-19
Table 1.
Epidemiologic Data of the Association between Sleep Disturbance and Gastroesophageal Reflux Disease
GERD, gastroesophageal reflux disease; OR, odd ratios; CI, confidence interval; ERD, erosive reflux disease; NERD, non-erosive reflux disease; RE, reflux esophagitis.
Figure 1.
Epidemiologic data show the adjusted odds ratios (ORs) from case-control studies examining the association between sleep disturbance and gastroesophageal reflux disease. Upper four studies show a consistent and significant association with sleep disturbance among GERD. Chen et al.10* shows the association between sleep disturbance and reflux esophagitis. Bottom shows that increased ORs for GERD among individuals with sleep disturbance.
In another large multicenter, multinational, observational study conducted as a series of parallel, locally managed studies at 134 primary care sites across six European countries (RANGE; Retrospective Analysis of GERD), sleep disturbances were common among subjects with GERD symptoms in all countries both in terms of frequency and intensity.8 Similar data have been reported from a primary care study in Spain.9 Recent systematic reviews have also reported that nocturnal GERD symptoms and sleep disturbances increased the likelihood of medical consultation.11,12
Reflux esophagitis at upper endoscopy has been observed to be associated with an increased risk for sleep disturbance. Among 3,663 individual who underwent endoscopy at a Chinese referral center,10 reflux symptom were associated with two fold increased odds of a sleep disturbance (OR, 1.25; 95% CI, 1.06-1.47) and the severity of reflux esophagitis was also related to sleep disturbance (OR 1.25, 95% CI 1.06-1.46 in erosive reflux disease vs. non-erosive reflux disease). Other studies have also observed that sleep-related GERD is associated with higher esophagitis grades and Barrett's esophagus.20,21
Overall, there are convincing data that sleep disturbances are a common feature in patients with GERD symptoms, and the association is not due to chance or obvious confounding. However, these data do not establish a causal role for sleep disturbances in GERD or vice versa.
2) GERD in patients with primary sleep disturbances
A substantial proportion of adults with objective sleep disturbance experience GERD (Table 1, Fig. 1). In a multicenter, longitudinal cohort study of sleep-disordered breathing, 24.9% (3,806/15,314) reported having GERD. Body mass index, daytime sleepiness, insomnia, hypertension and asthma were strong predictors for nighttime heartburn.16 Usage of benzodiazepines was a risk factor for GERD among subjects with sleep-disordered breathing (OR, 1.43; 95% CI, 1.09-1.88).16 Others have observed similar associations.13,22
Limited data suggest a relationship between symptomatic obstructive sleep apnea (OSA) and GERD. The prevalence of GERD has been shown about 58-62% of patients with OSA,23,24 however, these results may all be confounded by obesity. Apnea may increase trans-diaphragmatic pressure and decrease intra-thoracic pressure, favoring GERD.25 Moreover, apnea might induce gastric dilatation, decrease gastric emptying, and induce transient lower esophageal sphincter relaxations.26 Further, greater respiratory effort increases the pressure gradient across the lower esophageal sphincter and eventually facilitates the retrograde movement of gastric contents. However, other studies have failed to show significant relationship between GERD and OSA.27,28 Moreover, in a recent study applying simultaneous recordings of high resolution manometry (impedance and pH monitoring) and polysomnography, the pressure of the upper esophageal sphincter and esophago-gastric junction increased during OSA despite decreased esophageal body pressure, and the incidence of GERD was not different from controls.29 Although the relationship between OSA and GERD is not clear, treatment of OSA has been shown to improve GERD30 and continuous positive airway pressure (CPAP) has been demonstrated to reduce the total 24 hour esophageal acid contact time.31,32
2. Pathophysiological evidence for a causal link between GERD and sleep disturbance
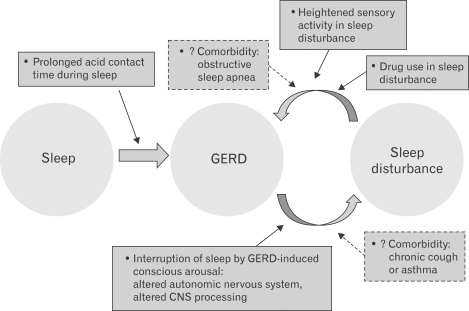
There is considerable evidence to indicate that GERD can be affected by abnormal sleep physiology. Conversely, it is also possible that disturbed sleep enhances perception of intra-esophageal reflux events. However, few studies have been conducted and these have shown inconsistent results (Table 2, Fig. 2).
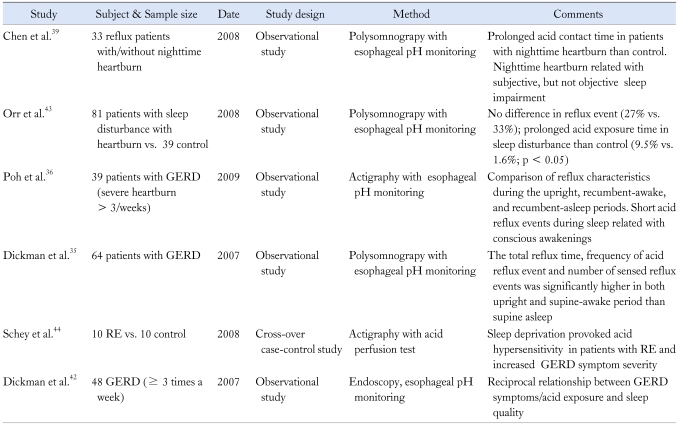
Table 2.
Pathophysiological Studies of Gastroesophageal Reflux Disease and Sleep Disturbances
GERD, gastroesophageal reflux disease; RE, reflux esophagitis.
Figure 2.
Possible pathophysiology of sleep disturbance and gastroesophageal reflux disease (GERD).
1) Normal physiologic change during sleep
GERD is usually a postprandial event and is a normal physiologic response to gastric distension after eating, which induces a transient relaxation of the lower esophageal sphincter, but notably esophageal physiology and esophageal acid clearance during sleep differ from wakefullness.33 Acidification of the distal esophagus produces a marked increase in the secretion of saliva and its bicarbonate concentration whilst awake. In addition, in response to an acidic distal esophagus, there is a marked increase of swallowing and in subsequent primary peristalsis of the esophagus.34 However, this secretory and motor response to acid exposure in the distal esophagus is different during sleeping. Swallowing frequency is almost not existent during sleep; swallows only occur during brief arousals.34 Salivary secretion ceases during sleep, and sleep facilitates proximal acid migration into the esophagus.
2) GERD induced conscious arousals may provoke sleep disturbance
In a small sample of GERD patients who underwent polysomnography and 24-hr esophageal pH monitoring assessing the impact of GERD on sleep, Dickman et al.31 showed that most reflux event occurred during stage 2 sleep and 90% of reflux event were associated with a short arousal. In addition, the supine awake period in patients with GERD has been shown to shorten the reflux time period.35 In another recent study using 24-hr esophageal pH monitoring and actigraphy, a validated watch-like ambulatory digital recording system in determining sleep duration and awakening, Poh et al.36 confirmed that short-duration reflux events during the sleep period were associated with conscious awakenings. Thus, it is conceivable that nocturnal reflux events might evoke frequent conscious awakenings during sleep.
Thus conscious awakening may interrupt sleep; a high arousal index has been shown to be associated with poor quality of sleep. Physiologically, hyperarousal may be associated with activation of neuroendocrine systems including the autonomic nervous system (ANS) and the hypothalamic pituitary adrenal axis. These arousals might lead to increased sympathetic activation manifested by events such as increased heart rate or blood pressure; such autonomic arousals can result in poor sleep quality in the absence of electroencephalographic evidence of cortical arousal. Indeed, hyperarousal has been demonstrated to disrupt sleep patterns.37 However, there were few studies that have specifically addressed the nighttime response of the ANS to acid reflux events. Interestingly, simultaneous cardiac and ambulatory pH monitoring revealed that esophageal acid exposure during sleep was associated with parasympathetic fluctuation with a superimposed sympathetic interaction.38
3) Prolonged acid contact time during sleep disturbances may provoke GERD
The occurrence of GERD cannot be evaluated by symptoms during sleep.34 24-hr esophageal pH monitoring studies combined with simultaneous polysomnography have established that GERD occurs less frequently during sleep.39-41 However, prolonged acid contact time during sleep has been shown in GERD patients.42,43 Using simultaneous monitoring of esophageal pH and polysomnography, a recent study was conducted in 81 patients with sleep disturbance and heartburn and 39 controls with neither sleep problem nor heartburn.43 This study showed no difference in reflux event (27% vs. 33%), but acid exposure time was longer in patients with sleep disturbances than controls.43
4) Disturbed sleep-induced hyperalgesia may cause GERD
In a cross-over study evaluating sleep deprivation and perception in the esophagus, Schey et al.44 studied 10 patients with reflux esophagitis (Los Angeles classification B-D) and 10 healthy controls; after sleep deprivation, the GERD patients had a significant decrease in lag time to symptom report, an increase in intensity rating, and an increase in acid perfusion sensitivity score, as compared to nights of good sleep. Normal subjects did not demonstrate any differences in the stimulus response to acid between sufficient sleep and sleep deprivation. They concluded that sleep deprivation may provoke hyperalgesia in patients with GERD. However, further studies are needed to confirm these findings.
5) Medication use for sleep disturbance can provoke or aggravate GERD
Some medications used to manage sleep disturbances may aggravate GERD. For example, benzodiazepines have been shown to be significantly associated with heartburn during sleep in an epidemiologic study.16 In both animal models and humans, benzodiazepines decreased basal lower esophageal sphincter pressure and increased the number of gastroesophageal reflux events.45 Non-benzodiazepine hypnotics include zolpidem; this binds to gamma-aminobytyric acid (GABA)-A receptors, facilitating sleep onset, and reducing the arousal threshold. Recently, one study showed that zolpidem reduced the arousal response to nocturnal acid exposure and increased the duration of each esophageal acid reflux event in healthy individuals and patients with GERD.46
3. What are the treatment implications if GERD and sleep disturbances are related?
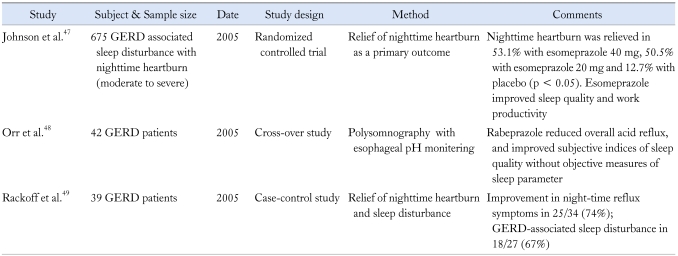
Theoretically the vicious cycle of GERD inducing poor sleep that in turn aggravates GERD further may be interrupted by more aggressive acid reducing therapy. Several studies have evaluated the efficacy of PPI therapy for sleep disturbances in patients with GERD but few randomized blinded placebo controlled clinical trials are available (Table 3).47-50 Johnson and colleagues47 performed a large multicenter randomized double-blind placebo-controlled trial utilizing esomeprazole 40 mg, 20 mg, or placebo for 6 weeks in 675 adults with GERD-associated sleep disturbance. Fifty percent of the esomeprazole-treated subjects had resolution of nighttime heartburn, and by 4 weeks, 73% of the esomeprazole-treated subjects had resolution of their GERD-associated sleep disturbance. Both doses of esomeprazole resulted in improved sleep quality, reduced lost work hours, and increased work productivity. In another study using rabeprazole for sleep-related GERD with 24-pH esophageal monitoring study with polysomnography, Orr et al.48 observed that rabeprazole reduced overall acid reflux, and improved subjective indices of sleep quality. However, they failed to show any objective improvement of sleep parameters after acid suppression.
Table 3.
Pharmacologic Interventions in Gastroesophageal Reflux Disease with Sleep Disturbance
GERD, gastroesophageal reflux disease.
A retrospective observational study in 56 patients with GERD who took double dose proton pump inhibitor (PPI) with/without additional ranitidine was conducted to evaluate symptom relief by a patient's interview.49 The addition of ranitidine administered at bedtime to patients taking double dose of PPI therapy led to an improvement in overall symptoms and GERD-associated sleep disturbance. Another study suggested that the addition of a nocturnal H2RA (histamine-2 receptor antagonist) or PPI after taking a morning dose of PPI decreased nocturnal acid breakthrough with improvement of daytime functioning.50 Unfortunately, other data suggested tachyphylaxis with H2RAs in nocturnal acid breakthrough.51
Data regarding the impact of fundoplication on sleep parameters has been very limited. Eleven patients with heartburn undergoing fundopication 8 to 10 weeks after surgery all reported an improvement of subjective sleep disturbances but not the objective sleep parameters.52
Conclusion
This review has addressed the complex relationships between GERD and sleep. Epidemiologic data suggest that GERD has a modest but important association with sleep disturbance, and this association appears to be bidirectional. The link appears to not be explained by comorbidity. Medical treatment of nighttime GERD appears to improve subjective sleep disturbances but objective data may not improve. Further studies are needed to investigate sleep architecture and brain function in GERD patients that is not detected by traditional polysomnography.36,44 Data on non-acidic reflux and the potential relationship with sleep disturbance is also needed (e.g., by using impedance and high resolution manometry). A better understanding of the relationships between sleep and GERD may allow the clinician to manage these patients more effectively in the future.
Footnotes
Financial support: None.
Conflicts of interest: None.
References
- 1.Locke GR, 3rd, Zinsmeister AR, Fett SL, Melton LJ, 3rd, Talley NJ. Overlap of gastrointestinal symptom complexes in a US community. Neurogastroenterol Motil. 2005;17:29–34. doi: 10.1111/j.1365-2982.2004.00581.x. [DOI] [PubMed] [Google Scholar]
- 2.Drossman DA, Li Z, Andruzzi E, et al. U.S. householder survey of functional gastrointestinal disorders. Prevalence, sociodemography, and health impact. Dig Dis Sci. 1993;38:1569–1580. doi: 10.1007/BF01303162. [DOI] [PubMed] [Google Scholar]
- 3.Roth T, Roehrs T. Insomnia: epidemiology, characteristics, and consequences. Clin Cornerstone. 2003;5:5–15. doi: 10.1016/s1098-3597(03)90031-7. [DOI] [PubMed] [Google Scholar]
- 4.Taylor DJ, Mallory LJ, Lichstein KL, Durrence HH, Riedel BW, Bush AJ. Comorbidity of chronic insomnia with medical problems. Sleep. 2007;30:213–218. doi: 10.1093/sleep/30.2.213. [DOI] [PubMed] [Google Scholar]
- 5.Roth T. Comorbid insomnia: current directions and future challenges. Am J Manag Care. 2009;15(Suppl):S6–S13. [PubMed] [Google Scholar]
- 6.Jansson C, Nordenstedt H, Wallander MA, et al. A population-based study showing an association between gastroesophageal reflux disease and sleep problems. Clin Gastroenterol Hepatol. 2009;7:960–965. doi: 10.1016/j.cgh.2009.03.007. [DOI] [PubMed] [Google Scholar]
- 7.Mody R, Bolge SC, Kannan H, Fass R. Effects of gastroesophageal reflux disease on sleep and outcomes. Clin Gastroenterol Hepatol. 2009;7:953–959. doi: 10.1016/j.cgh.2009.04.005. [DOI] [PubMed] [Google Scholar]
- 8.Gisbert JP, Cooper A, Karagiannis D, et al. Impact of gastroesophageal reflux disease on patient's daily lives: a European observational study in the primary care setting. Health Qual Life Outcomes. 2009;7:60. doi: 10.1186/1477-7525-7-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Ferrus JA, Zapardiel J, Sobreviela E. Management of gastroesophageal reflux disease in primary care settings in Spain: SYMPATHY I study. Eur J Gastroenterol Hepatol. 2009;21:1269–1278. doi: 10.1097/MEG.0b013e32832a7d9b. [DOI] [PubMed] [Google Scholar]
- 10.Chen MJ, Wu MS, Lin JT, et al. Gastroesophageal reflux disease and sleep quality in a Chinese population. J Formos Med Assoc. 2009;108:53–60. doi: 10.1016/S0929-6646(09)60032-2. [DOI] [PubMed] [Google Scholar]
- 11.Gerson LB, Fass R. A systematic review of the definitions, prevalence, and response to treatment of nocturnal gastroesophageal reflux disease. Clin Gastroenterol Hepatol. 2009;7:372–378. doi: 10.1016/j.cgh.2008.11.021. [DOI] [PubMed] [Google Scholar]
- 12.Hungin AP, Hill C, Raghunath A. Systematic review: frequency and reasons for consultation for gastro-oesophageal reflux disease and dyspepsia. Aliment Pharmacol Ther. 2009;30:331–342. doi: 10.1111/j.1365-2036.2009.04047.x. [DOI] [PubMed] [Google Scholar]
- 13.Wallander MA, Johansson S, Ruigomez A, Garcia Rodriguez LA, Jones R. Dyspepsia in general practice: incidence, risk factors, comorbidity and mortality. Fam Pract. 2007;24:403–411. doi: 10.1093/fampra/cmm050. [DOI] [PubMed] [Google Scholar]
- 14.Wang R, Yan X, Ma XQ, et al. Burden of gastroesophageal reflux disease in Shanghai, China. Dig Liver Dis. 2009;41:110–115. doi: 10.1016/j.dld.2008.06.014. [DOI] [PubMed] [Google Scholar]
- 15.Kusano M, Kouzu T, Kawano T, Ohara S. Nationwide epidemiological study on gastroesophageal reflux disease and sleep disorders in the Japanese population. J Gastroenterol. 2008;43:833–841. doi: 10.1007/s00535-008-2235-0. [DOI] [PubMed] [Google Scholar]
- 16.Fass R, Quan SF, O'Connor GT, Ervin A, Iber C. Predictors of heartburn during sleep in a large prospective cohort study. Chest. 2005;127:1658–1666. doi: 10.1378/chest.127.5.1658. [DOI] [PubMed] [Google Scholar]
- 17.Dean BB, Crawley JA, Schmitt CM, Wong J, Ofman JJ. The burden of illness of gastro-oesophageal reflux disease: impact on work productivity. Aliment Pharmacol Ther. 2003;17:1309–1317. doi: 10.1046/j.1365-2036.2003.01588.x. [DOI] [PubMed] [Google Scholar]
- 18.Farup C, Kleinman L, Sloan S, et al. The impact of nocturnal symptoms associated with gastroesophageal reflux disease on health-related quality of life. Arch Intern Med. 2001;161:45–52. doi: 10.1001/archinte.161.1.45. [DOI] [PubMed] [Google Scholar]
- 19.Dubois RW, Aguilar D, Fass R, et al. Consequences of frequent nocturnal gastro-oesophageal reflux disease among employed adults: symptom severity, quality of life and work productivity. Aliment Pharmacol Ther. 2007;25:487–500. doi: 10.1111/j.1365-2036.2006.03189.x. [DOI] [PubMed] [Google Scholar]
- 20.Adachi K, Fujishiro H, Katsube T, et al. Predominant nocturnal acid reflux in patients with Los Angeles grade C and D reflux esophagitis. J Gastroenterol Hepatol. 2001;16:1191–1196. doi: 10.1046/j.1440-1746.2001.02617.x. [DOI] [PubMed] [Google Scholar]
- 21.Dickman R, Parthasarathy S, Malagon IB, et al. Comparisons of the distribution of oesophageal acid exposure throughout the sleep period among the different gastro-oesophageal reflux disease groups. Aliment Pharmacol Ther. 2007;26:41–48. doi: 10.1111/j.1365-2036.2007.03347.x. [DOI] [PubMed] [Google Scholar]
- 22.Guda N, Partington S, Shaw MJ, Leo G, Vakil N. Unrecognized GERD symptoms are associated with excessive daytime sleepiness in patients undergoing sleep studies. Dig Dis Sci. 2007;52:2873–2876. doi: 10.1007/s10620-007-9768-6. [DOI] [PubMed] [Google Scholar]
- 23.Green BT, Broughton WA, O'Connor JB. Marked improvement in nocturnal gastroesophageal reflux in a large cohort of patients with obstructive sleep apnea treated with continuous positive airway pressure. Arch Intern Med. 2003;163:41–45. doi: 10.1001/archinte.163.1.41. [DOI] [PubMed] [Google Scholar]
- 24.Herr J. Chronic cough, sleep apnea, and gastroesophageal reflux disease. Chest. 2001;120:1036–1037. doi: 10.1378/chest.120.3.1036. [DOI] [PubMed] [Google Scholar]
- 25.Ing AJ, Ngu MC, Breslin AB. Obstructive sleep apnea and gastroesophageal reflux. Am J Med. 2000;108(suppl 4a):120S–125S. doi: 10.1016/s0002-9343(99)00350-2. [DOI] [PubMed] [Google Scholar]
- 26.Orr WC. Therapeutic options in the treatment of nighttime gastroesophageal reflux. Digestion. 2005;72:229–238. doi: 10.1159/000089957. [DOI] [PubMed] [Google Scholar]
- 27.Kim HN, Vorona RD, Winn MP, Doviak M, Johnson DA, Ware JC. Symptoms of gastro-oesophageal reflux disease and the severity of obstructive sleep apnoea syndrome are not related in sleep disorders center patients. Aliment Pharmacol Ther. 2005;21:1127–1133. doi: 10.1111/j.1365-2036.2005.02447.x. [DOI] [PubMed] [Google Scholar]
- 28.Morse CA, Quan SF, Mays MZ, Green C, Stephen G, Fass R. Is there a relationship between obstructive sleep apnea and gastroesophageal reflux disease? Clin Gastroenterol Hepatol. 2004;2:761–768. doi: 10.1016/s1542-3565(04)00347-7. [DOI] [PubMed] [Google Scholar]
- 29.Kuribayashi S, Massey BT, Hafeezullah M, et al. Upper esophageal sphincter and gastroesophageal junction pressure changes act to prevent gastroesophageal and esophagopharyngeal reflux during apneic episodes in patients with obstructive sleep apnea. Chest. 2010 doi: 10.1378/chest.09-0913. (In press) [DOI] [PubMed] [Google Scholar]
- 30.Bortolotti M, Gentilini L, Morselli C, Giovannini M. Obstructive sleep apnoea is improved by a prolonged treatment of gastrooesophageal reflux with omeprazole. Dig Liver Dis. 2006;38:78–81. doi: 10.1016/j.dld.2005.09.018. [DOI] [PubMed] [Google Scholar]
- 31.Tawk M, Goodrich S, Kinasewitz G, Orr W. The effect of 1 week of continuous positive airway pressure treatment in obstructive sleep apnea patients with concomitant gastroesophageal reflux. Chest. 2006;130:1003–1008. doi: 10.1378/chest.130.4.1003. [DOI] [PubMed] [Google Scholar]
- 32.Zanation AM, Senior BA. The relationship between extraesophageal reflux (EER) and obstructive sleep apnea (OSA) Sleep Med Rev. 2005;9:453–458. doi: 10.1016/j.smrv.2005.05.003. [DOI] [PubMed] [Google Scholar]
- 33.Harding SM. Sleep related gastroesophageal reflux. The tip of the iceberg is showing! J Clin Sleep Med. 2007;3:514–515. [PMC free article] [PubMed] [Google Scholar]
- 34.Orr WC, Chen CL. Sleep and the gastrointestinal tract. Neurol Clin. 2005;23:1007–1024. doi: 10.1016/j.ncl.2005.05.004. [DOI] [PubMed] [Google Scholar]
- 35.Dickman R, Shapiro M, Malagon IB, Powers J, Fass R. Assessment of 24-h oesophageal pH monitoring should be divided to awake and asleep rather than upright and supine time periods. Neurogastroenterol Motil. 2007;19:709–715. doi: 10.1111/j.1365-2982.2007.00929.x. [DOI] [PubMed] [Google Scholar]
- 36.Poh CH, Gasiorowska A, Allen L, et al. Reassessment of the principal characteristics of gastroesophageal reflux during the recumbent period using integrated actigraphy-acquired information. Am J Gastroenterol. 2010 doi: 10.1038/ajg.2009.636. (In press) [DOI] [PubMed] [Google Scholar]
- 37.Bastien CH, St-Jean G, Morin CM, Turcotte I, Carrier J. Chronic psychophysiological insomnia: hyperarousal and/or inhibition deficits? An ERPs investigation. Sleep. 2008;31:887–898. doi: 10.1093/sleep/31.6.887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Lee YC, Wang HP, Lin LY, et al. Circadian change of cardiac autonomic function in correlation with intra-esophageal pH. J Gastroenterol Hepatol. 2006;21:1302–1308. doi: 10.1111/j.1440-1746.2006.04147.x. [DOI] [PubMed] [Google Scholar]
- 39.Chen CL, Robert JJ, Orr WC. Sleep symptoms and gastroesophageal reflux. J Clin Gastroenterol. 2008;42:13–17. doi: 10.1097/MCG.0b013e31802fc1bc. [DOI] [PubMed] [Google Scholar]
- 40.Freidin N, Fisher MJ, Taylor W, et al. Sleep and nocturnal acid reflux in normal subjects and patients with reflux oesophagitis. Gut. 1991;32:1275–1279. doi: 10.1136/gut.32.11.1275. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Orr WC, Allen ML, Robinson M. The pattern of nocturnal and diurnal esophageal acid exposure in the pathogenesis of erosive mucosal damage. Am J Gastroenterol. 1994;89:509–512. [PubMed] [Google Scholar]
- 42.Dickman R, Green C, Fass SS, et al. Relationships between sleep quality and pH monitoring findings in persons with gastroesophageal reflux disease. J Clin Sleep Med. 2007;3:505–513. [PMC free article] [PubMed] [Google Scholar]
- 43.Orr WC, Goodrich S, Fernstrom P, Hasselgren G. Occurrence of nighttime gastroesophageal reflux in disturbed and normal sleepers. Clin Gastroenterol Hepatol. 2008;6:1099–1104. doi: 10.1016/j.cgh.2008.06.016. [DOI] [PubMed] [Google Scholar]
- 44.Schey R, Dickman R, Parthasarathy S, et al. Sleep deprivation is hyperalgesic in patients with gastroesophageal reflux disease. Gastroenterology. 2007;133:1787–1795. doi: 10.1053/j.gastro.2007.09.039. [DOI] [PubMed] [Google Scholar]
- 45.Hall AW, Moossa AR, Clark J, Cooley GR, Skinner DB. The effects of premedication drugs on the lower oesophageal high pressure zone and reflux status of rhesus monkeys and man. Gut. 1975;16:347–352. doi: 10.1136/gut.16.5.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Gagliardi GS, Shah AP, Goldstein M, et al. Effect of zolpidem on the sleep arousal response to nocturnal esophageal acid exposure. Clin Gastroenterol Hepatol. 2009;7:948–952. doi: 10.1016/j.cgh.2009.04.026. [DOI] [PubMed] [Google Scholar]
- 47.Johnson DA, Orr WC, Crawley JA, et al. Effect of esomeprazole on nighttime heartburn and sleep quality in patients with GERD: a randomized, placebo-controlled trial. Am J Gastroenterol. 2005;100:1914–1922. doi: 10.1111/j.1572-0241.2005.00285.x. [DOI] [PubMed] [Google Scholar]
- 48.Orr WC, Goodrich S, Robert J. The effect of acid suppression on sleep patterns and sleep-related gastro-oesophageal reflux. Aliment Pharmacol Ther. 2005;21:103–108. doi: 10.1111/j.1365-2036.2005.02310.x. [DOI] [PubMed] [Google Scholar]
- 49.Rackoff A, Agrawal A, Hila A, Mainie I, Tutuian R, Castell DO. Histamine-2 receptor antagonists at night improve gastroesophageal reflux disease symptoms for patients on proton pump inhibitor therapy. Dis Esophagus. 2005;18:370–373. doi: 10.1111/j.1442-2050.2005.00518.x. [DOI] [PubMed] [Google Scholar]
- 50.Robinson M, Rodriguez-Stanley S, Ciociola AA, et al. Control of nocturnal gastric acidity: a role for low dose bedtime ranitidine to supplement daily omeprazole. Dig Dis Sci. 2002;47:265–273. doi: 10.1023/a:1013749501241. [DOI] [PubMed] [Google Scholar]
- 51.Fackler WK, Ours TM, Vaezi MF, Richter JE. Long-term effect of H2RA therapy on nocturnal gastric acid breakthrough. Gastroenterology. 2002;122:625–632. doi: 10.1053/gast.2002.31876. [DOI] [PubMed] [Google Scholar]
- 52.Cohen JA, Arain A, Harris PA, et al. Surgical trial investigating nocturnal gastroesophageal reflux and sleep (STINGERS) Surg Endosc. 2003;17:394–400. doi: 10.1007/s00464-002-8912-9. [DOI] [PubMed] [Google Scholar]