Abstract
Background/Aims
Laryngopharyngeal symptoms of gastroesophageal reflux disease (GERD) such as globus sensation, hoarseness and chronic cough are becoming increasingly recognized. This study was aimed to investigate the diagnostic usefulness of combined dual channel multichannel intraluminal impedance (MII)/pH-metry in 'off-proton pump inhibitor (PPI)' patients with suspected laryngopharyngeal reflux.
Methods
Ninety-eight patients with laryngopharyngeal symptoms of GERD were included. All patients were 'off-PPI' state for at least 2 weeks prior to the study, and underwent endoscopy and dual channel combined MII/pH-metry.
Results
The mean age of the patients was 49.8 ± 10.9 years and there were 44 males (44.9%). Fifty-three patients (54.1%) showed pathologic gastroesophageal reflux (GER). Combined dual channel MII/pH-metry achieved highest diagnostic yield of 49.0% and diagnostic yield of single channel combined MII/pH-metry was 37.8%. Addition of MII to standard pH-metry increased twofold of the diagnostic yield for detecting GER. Among 37 patients (37.8%) who had pathologic GER being detected by MII/pH-metry, 19 patients (19.4%) had nonacid GER (nonacid GER group) while 18 patients (18.4%) had acid GER (acid GER group). Pathologic GER group, as classified by MII/pH-metry showed more frequent globus sensation than nonpathologic GER group. Acid GER group had more proximal reflux than nonacid GER group, especially in the upright position.
Conclusions
In this study, combined dual channel MII/pH-metry showed the highest diagnostic yield for detecting GER. This technique can be performed primarily to accurately diagnose laryngopharyngeal reflux disease and exclude other causes of laryngopharyngeal symptoms.
Keywords: Impedance, Laryngopharyngeal reflux
Introduction
Gastroesophageal reflux disesase (GERD), defined as a condition developing by the reflux of stomach contents to cause troublesome symptoms and/or complications, is a common chronic disorder of our time, affecting about 10% to 20% of the adult population in Western world.1,2 In Asian countries, the prevalence of GERD varies from 2.5% to 6.2%, and it has shown to increase over the last two decades.3,4 Typically, heartburn and regurgitation are well-known common presenting symptoms of GERD. However, extraesophageal symptoms of GERD such as globus sensation, hoarseness, and chronic cough are becoming increasingly recognized.5,6 The prospective ProGERD study from Europe involving 6,215 patients with heartburn has found extraesophageal symptoms in 32.8% of patients, and Richter et al.7 recently reported that 80% of patients with weekly heartburn had at least one extraesophageal manifestation, compared to 49% of those without heartburn.6 Many of the atypical GERD symptoms are nonspecific and often subjective, and can be caused by several other conditions like smoking, allergies, neurogenic, and psychogenic disorders8 which make diagnosing extraesophageal GERD difficult. Moreover, the relationship between GERD and extraesophageal symptoms is frequently problematic to establish with a high degree of certainty. At present, the significance of diagnosis and treatment of extraesophageal GERD is still controversial.9-11 Therapeutic trial of a proton pump inhibitor (PPI) in double standard dose for 3 to 4 months has been suggested as a first step management in patients with suspected extraesophageal manifestations of GERD.9 However, some patients failed to respond to the PPI treatment and there were studies reporting that up to 50% of these patients responded to placebo.12-14 These findings raise the question of whether the extraesophageal symptoms are true manifestations of gastroesophageal reflux (GER). For this reason, there was a suggestion that objective examination to demonstrate the proximal reflux should precede empirical PPI treatment.15,16 Traditionally, 24-hour ambulatory pH monitoring was recognized as standard diagnostic test for GERD. However, multichannel intraluminal impedance (MII) combined with pH monitoring is now considered the most sensitive tool for diagnosis and characterization of GERD, and this new technology allows detection of both acid and nonacid GER and also makes it possible to assess the nature (liquid, gas, or mixed liquid-gas) of refluxate and proximal extent of GER.
This study was aimed to investigate the diagnostic usefulness of combined dual channel MII/pH-metry in 'off-PPI' patients with suspected laryngopharyngeal manifestations of GERD.
Materials and Methods
1. Subjects
We performed a prospective cross-sectional study of 98 patients with laryngopharyngeal manifestations of GERD, such as globus sensation, hoarseness, and chronic cough who admitted to Pusan National University Hospital from June 2006 to March 2009. Patients were included in a consecutive manner. Patients with a history of any esophageal or gastric surgery were not included. All subjects were 'off-PPI' state for at least 2 weeks prior to the study and had undergone both the esophagogastroduodenoscopy and combined dual channel MII/pH-metry after at least 8 hours of fasting. Esophageal manometry was also performed to identify the level of the low esophageal sphincter (LES) and to rule out any functional esophageal disorders.
2. Symptom assessments
Laryngopharyngeal symptoms were evaluated by patient interview and each symptoms were scored as below by the reference to GERD-Health Related Quality of Life scale: (0) no symptoms; (1) symptoms noticeable, but not bothersome; (2) symptoms noticeable and bothersome, but not everyday; (3) symptoms bothersome everyday; (4) symptoms that affect daily activities; and (5) symptoms are incapacitating. Predominant symptom was defined as having the highest score. Combined typical reflux symptom was defined as heartburn or regurgitation to be present at a frequency of ≥ 1/wk.
3. Esophagogastroduodenoscopy
Absence or presence of erosive esophagitis (EE) and atrophic gastritis were examined by esophagogastroduodenoscopy. Furthermore, reflux esophagitis was graded from A to D using Los Angeles classification,17 and atrophic gastritis was divided into a closed-type and an open-type by Kimura-Takemoto endoscopic classification.18,19 Gastroesophageal flap valve (GEFV) was also evaluated and was graded I to IV according to the recently described grading by Hill et al.20 The GEFV was largely classified into 2 groups: the normal GEFV group (grades I and II) and the abnormal GEFV group (grades III and IV).21
4. Combined dual channel pH-Metry/MII monitoring
The dual channel pH-metry/MII catheter consists of a 2.3 mm polyurethane catheter incorporating 6 impedance segments (each segment 2 cm long) and 2 pH-measuring electrodes (Sandhill Scientific Inc., Denver, CO, USA). The configuration of this catheter allowed recording the changes in intraluminal impedance at 3, 5, 7, 9, 15, and 17 cm above the LES. In addition, pH was monitored at 5 cm above the LES (distal) and 20 cm above the LES (proximal). After defining the LES by using conventional manometry, dual channel pH-metry/MII catheter was inserted transnasally and distal pH probe was positioned 5 cm above the LES. Data from the impedance channels and the pH electrodes were transmitted at a frequency of 50 Hz and stored on a portable data recorder (Sleuth, Sandhill Scientific Inc., Highlands Ranch, CO, USA). After 24-hour recording, data were uploaded on a personal computer and analyzed by using a commercially available software system (Bioview Analysis, Sandhill Scientific Inc., Highlands Ranch, CO, USA). During the recording period, patients were encouraged to follow a regular activity and meal regimens, and were given a personal diary to note meal times, time in the recumbent position, and the timing of any GERD-related symptoms.
5. Analyzing pH data
Acid reflux episode was defined as a drop in pH to less than 4 for at least 5 seconds. Total acid exposure time (%) was calculated as the total time of acid reflux episodes divided by the time of monitoring. DeMeester score,22 which has been widely used to evaluate acid reflux, was obtained using 6 different parameters: (1) total percentage time pH < 4.0, (2) percentage time pH < 4.0 in the upright period, (3) percentage time pH < 4.0 in the recumbent period, (4) the total number of acid reflux episodes, (5) the total number of acid reflux episodes longer than 5 minutes, and (6) the duration of the longest acid reflux episodes.
6. Analyzing MII data
The meal periods were excluded from the analysis. Liquid reflux episode was defined as a fall in impedance of ≥ 50% of baseline which moved in retrograde direction on the 2 distal impedance sites. Gas reflux episode was defined as a rapid (3 kΩ/sec) increase in impedance > 5,000 Ω, occurring simultaneously in at least 2 esophageal impedance-measuring segments, in the absence of swallowing. Mixed liquid-gas reflux episode was defined as gas reflux occurring immediately before or during a liquid reflux. These reflux episodes were classified as acidic if the pH dropped below 4 or as non-acidic if the pH remained above 4 during the episode. Proximal reflux episode was considered when the refluxate reached the 15 cm impedance sensor. Total bolus exposure time (%) was defined as the sum of bolus clearance time of all individual reflux episodes divided by the time of monitoring. Bolus clearance time was defined as the time from a drop in impedance to 50 % of its baseline value to recovery to 50 % of baseline value in the most distal impedance channel.
7. Interpretating combined dual channel pH-metry/MII data
Total acid exposure time (%) of distal pH probe > 4.0 or DeMeester score > 14.7 was considered as an acid GER. Total bolus exposure time (%) more than 1.4 without acid GER was considered as a nonacid GER. Acid gastropharyngeal reflux was defined by proximal pH probe when at least one of the following criteria was met23,24: (1) total acid exposure time (%) > 0.1%, (2) acid exposure time (%) in upright position > 0.2%, (3) acid exposure time (%) in supine position > 0.0%, and (4) acid reflux number ≥ 4.
8. Statistical methods
All continuous variables were presented as mean ± standard deviation, and the proportions were expressed as numbers (%). Mann-Whitney U test and Kruskal-Wallis test were used when comparing continuous parameters, and the proportions were compared using the chi-square test. The computer software used for statistical analysis was SPSS (version 12.0, SPSS Inc., Chicago, IL, USA). A p-value of < 0.05 was considered statistically significant.
Results
A total of 98 patients were included in this study. The dual pH-impedance probe was well tolerated for all patients. The total recording time was 21.6 hours, and meal periods were excluded from the analysis.
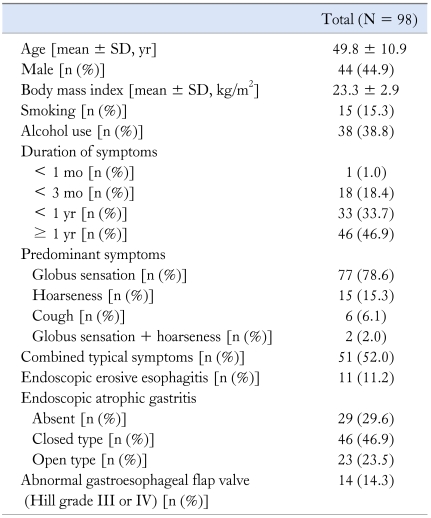
Table 1 summarizes the characteristics of enrolled patients. The mean age of the patients was 49.8 ± 10.9 years (range 21-71). There were 44 males (44.9%) and the mean body mass index was 23.3 ± 2.9 kg/m2 (range 15.8-30.5). Fifteen patients (15.3%) were smokers and 38 patients (38.8%) were alcohol users. Only 1 patient (1.0%) had < 1 month of symptom, and 46 patients (46.9%) had ≥ 1 year of symptom. Ninety-six patients (98.0%) had 1 predominant symptom, and the most common presenting symptom was globus sensation (n = 77, 78.6%) followed by hoarseness (n = 15, 15.3%) and chronic cough (n = 6, 6.1%). Two patients (2.0%) complained same degree of globus sensation and hoarseness. Fifty-one patients (52.0%) complained of coexisting typical reflux symptoms such as heartburn and regurgitation. EE were seen in 11 patients (11.2%), and all these patients were Los Angeles grade A. Sixty-nine patients (70.4%) had endoscopic atrophic gastritis: closed-type in 47 cases (48.0%) and open-type in 22 cases (22.4%). Abnormal GEFV (Hill grades III or IV) were seen in 14 patients (14.3%).
Table 1.
Patients' Characteristics
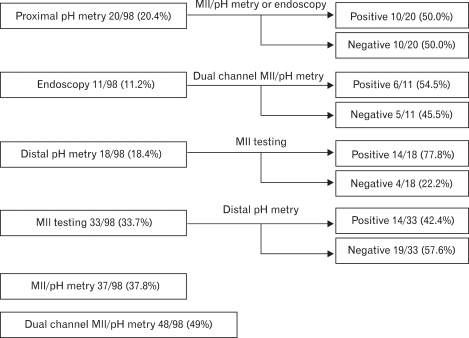
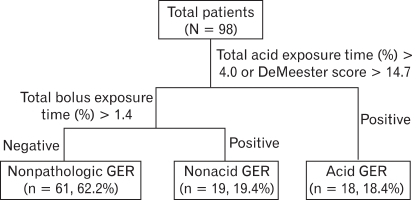
Figure 1 shows the diagnostic yield of various methods for detecting GER. Of a total 98 patients, 53 patients showed pathologic GER (54.1%) with at least one abnormal result in either endoscopy, proximal pH-metry, distal pH-metry, or MII. Pathologic proximal acid reflux was seen in 10 patients without any evidence of distal GER, and EE occured as a single phenomenon in 5 patients. Four patients with negative result in MII testing had pathologic acid GER, and 19 patients with negative result on distal pH-metry had abnormal finding in MII testing. Diagnostic yield of single channel combined MII/pH-metry and dual channel combined MII/pH-metry was 37.8% and 49.0%, respectively. Among 37 patients (37.8%) who had pathologic GER detected by MII/pH-metry, 19 patients (19.4%) had nonacid GER (nonacid GER group) and 18 patients (18.4%) had acid GER (acid GER group) (Fig. 2).
Figure 1.
Diagnostic yield of various methods for detecting gastroesophageal reflux. Diagnostic yield of proximal pH-metry, endoscopy, distal pH-metry, multichannel intraluminal impedance (MII) testing, MII/distal pH-metry, and dual channel MII/pH-metry was 20.4%, 11.2%, 18.4%, 33.7%, 37.8%, and 49.0%, respectively. Pathologic proximal acid reflux was seen in 10 patients without any evidence of distal gastroesophageal reflux (GER), and erosive esophagitis (EE) occured as a single phenomenon in 5 patients. Four patients with negative result on MII testing had pathologic acid GER, and 19 patients with negative result on distal pH-metry had abnormal finding with MII testing.
Figure 2.
Multichannel intraluminal impedance/pH-metry results.
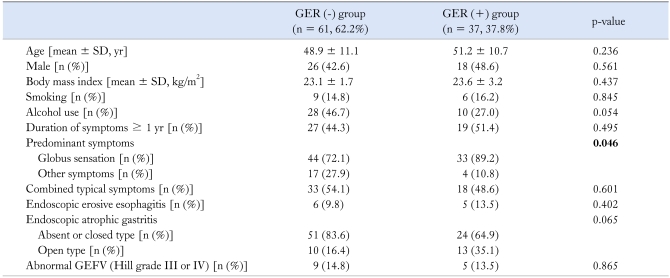
On comparing the data between nonpathologic GER [GER (-)] and pathologic GER [GER (+)] group (Table 2), as classified by MII/pH-metry, we did not find any inter-group demographic differences. Globus sensation was observed more frequently in GER (+) group than in GER (-) group with statistically significant difference (89.2% vs. 72.1%, p = 0.046). Endoscopic findings did not show differences between these 2 groups.
Table 2.
Comparison of Clinical Characteristics Between Nonpathologic Gastroesophageal Reflux [GER (-)] and Pathologic Gastroesophageal Reflux [GER (+)] Group
GEFV, gastroesophageal flap valve.
Bold style indicates statistical significance.
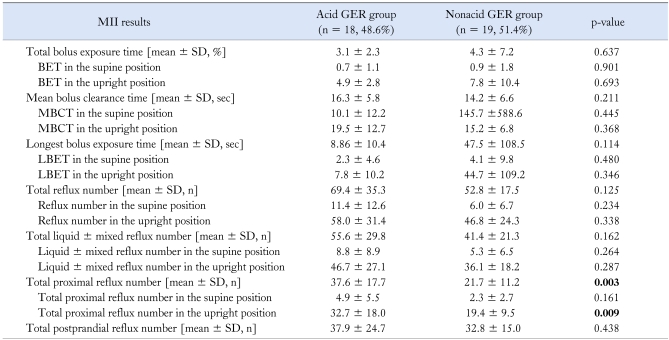
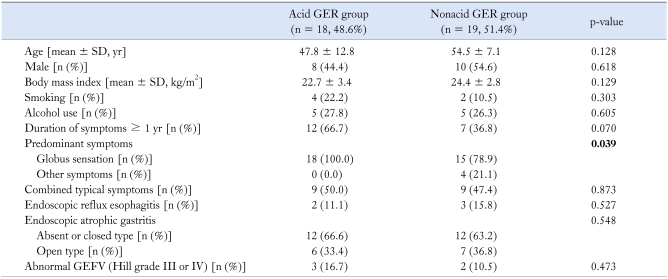
There were no significant differences in patients' characteristics and endoscopic findings between acid and nonacid GER group. We further analyzed and compared the results of impedence test between these 2 groups (Table 4). No differences were seen in bolus exposure time, mean bolus clearance time, longest bolus exposure time and reflux number. However, acid GER group had more proximal reflux episodes than nonacid GER group (37.6 ± 17.7 vs. 21.7 ± 11.2, p = 0.003), especially in the upright position (32.7 ± 18.0 vs. 19.4 ± 9.5, p = 0.009).
Table 4.
Comparison of Intraluminal Impedance Results Between Acid Gastroesophageal Reflux and Nonacid Gastroesophageal Reflux Group
MII, intraluminal impedance; GER, gastroesophageal reflux; BET, bolus exposure time; MBCT, mean bolus clearance time; LBET, longest bolus exposure time.
Bold style indicates statistical significance.
Discussion
The superiority of combined MII/pH-metry compared with pH-metry in the diagnosis of GERD is already proven and this method is being regarded as the best tool for assessing patients with suspected GERD. However, previously published data about combined MII/pH-metry are mostly based on patients with typical GERD symptoms or on patients who were under acid suppressive therapy.25-27 In 2007, Bajbouj et al.28 firstly investigated the utility of MII/pH-metry in 'off-PPI' patients with atypical symptoms. They reported that 63.4% of patients suffering from atypical symptoms had pathologic GER and 61% of patients were diagnosed with GERD by MII/pH-metry. With these results, they suggested combined MII/pH-metry to be essential in the diagnostic work-up of patients with atypical GERD. Malhotra et al.29 evaluated patients with suspected extraesophageal GERD who were on or off PPI therapy, and concluded MII/pH-metry to be useful in ruling out GERD and redirecting the management in these patients. In our study, we aimed not only to investigate the diagnostic usefulness of combined dual channel pH-Metry/MII monitoring in 'off-PPI' patients with suspected laryngopharyngeal manifestations of GERD, but to compare clinical characteristics and diagnostic data between pathologic GER and nonpatholgic GER group as well as between acid and nonacid GER group. Fifty-three patients (54.1%) had pathologic GER and the diagnostic yield of combined MII/pH-metry was 37.8%, which was lower than that of previous study by Bajbouj et al. Lower prevalence of GERD in Korea than in Western countries and different manner for interpretating pH/impedance data seemed to be the reasons for such different outcomes. Addition of MII to standard pH-metry increased the diagnostic yield for detecting GER around two fold in patients with laryngopharyngeal symptoms, which might be mostly due to the detection of nonacidic reflux. And dual channel combined MII/pH-metry showed 49.0% of diagnostic yield, which was the most sensitive method for diagnosing GER. The diagnostic yield of proximal pH-metry alone was 20.8%, and 10 patients (18.9% of patients with pathologic GER) showed pathologic proximal acid reflux without any evidence of distal GER. This ironic finding might have been caused by the current definitions of acid GER and GER which are not linked to each other. Also the lack of agreement of normative values and methodologic variability in proximal esophageal pH measurement, especially relating to the positioning of the upper pH probe make interpretation of proximal pH data difficult.30 More importantly, proximal pH-metry cannot detect nonacid GER and cannot provide any information on causality between refluxed gastric acid and symptoms.31 Because of low reproducibility and sensitivity, the clinical utility of proximal pH monitoring remains unproven.32 As of today, careful interpretation of proximal pH data in consideration of clinical factors is needed until more sensitive and accurate techniques for defining proximal reflux develp.
After all, 45.9% of enrolled patients had negative result from all methods for detecting GER, and this finding seems very important in the overall management of these patients. This result makes it reasonable that objective examination to demonstrate pathologic GER precedes empirical PPI therapy to exclude other causes of atypical symptoms and to avoid unnecessary medication including PPI. Based on the current study, combined dual channel MII/pH-metry can provide proper information for management in patients with suspected laryngopharyngeal manifestations of GERD.
In general, nonerosive reflux disease patients are known to have lower esophageal acid exposure than patients with EE and Barrett's esophagus. Recently, Savarino et al.33 compared reflux episodes and symptom association in nonerosive reflux disease and EE patients using combined MII/pH-metry, and they reported that acid reflux episodes, volume, and acid clearance were important factors in the pathogenesis of reflux induced lesions. However, there was a notable result in our study that 6 patients (11.3% of patients with pathologic GER) with negative outcome on MII/pH-metry presented with endoscopic EE. What would be the reasons for such outcome? Actually, normal reference values for MII/pH-metry among racial groups are not presently available and there are few reports about MII/pH-metry in Korea. Although subjects in this study were Koreans, we had no option but to refer to several western works as a guide. Usually, Asians are known to have smaller parietal cell mass and lower acid output compared to whites.34 And one muticenter study about normal ambulatory 24-hour esophageal pH values in Koreans suggested 3.8 as a cutoff value for total acid exposure time (%) compared to about 4 in Western studies.35 This unmatched analysis seems one of the reasons for MII/pH-metry negative EE patinets. The fact that the degree of esophageal mucosal defense and repairment to gastric contents is individually variable could explain for MII/pH-metry negative EE patients.
Unlike other studies about MII/pH-metry, we investigated endoscopic EE, atrophic gastritis and GEFV to evaluate their relationship with laryngopharyngeal reflux. Previously, we have studied 608 patients referred to our motility laboratory and found abnormal GEFV to be associated with GER, and the degree of atrophic gastritis to inversely relate with GER.36 According to the previous data, we expected similar outcome in present study, such as nonacid GER being related with open-type atrophic gastritis. But, we could not find significant association between endoscopic findings and GER. There is about 2 possible factors related with such outcomes. Firstly, definition of GER differed from previous study. Previous study defined GER by means of pH-metry or endoscopy, whereas present study used MII/pH-metry to evaluate GER. Secondly, GER include both reflux of gastric contents and duodenal contents. Therefore, nonacid GER group may be related with not only nonacidic gastric content due to hypochlohydria associated with atrophic gastritis but also postprandial neutralized gastric content and duodenogastroesophageal reluxate.
We observed globus sensation to be more related with pathologic GER than other laryngopharyngeal symptoms and 55% of patients with globus sensation and concomitant pathologic GER were in acid GER group. Anandasabapathy et al.25 reported that acid reflux was infrequent in patients with globus sensation and nonacid reflux might be predictive of the GERD-globus correlation. But their study was designed with patients with globus sensation on PPI therapy, so this might have made a difference.
The diagnostic utility of MII/pH-metry has been proven in extraesophageal as well as typical GERD at several works including our study. Most studies defined GERD using symptom index or symptom association probability. Of course, it is important to evaluate whether or not the symptoms are caused by reflux. However, atypical symptoms usually persist continuously and do not have a sudden onset that could be easily recognized by the patient.28,37 This characteristic makes it difficult to mark an reflux event at a single timepoint while the difficulty on assessment of symptom index in patients with atypical symptoms makes the diagnosis of extraesophageal GERD more confusing than typical GERD.
In conclusion, we confirmed the diagnostic usefulness of dual channel combined MII/pH-metry in patients with suspected laryngopharyngeal manifestations of GERD. Further large-scale population based study to provide normal values of dual channel MII/pH-metry in Koreans is required and more accurate method to prove the causal link between pathologic GER and laryngopharyngeal symptoms other than symptom index or symptom association probability should be developed. Combination of PPI trial with dual channel MII/pH-metry will make the laryngopharyngeal manifestations of GERD more distinct.
Table 3.
Comparison of Clinical Characteristics Between Acid Gastroesophageal Reflux and Nonacid Gastroesophageal Reflux Group
GER, gastroesophageal reflux; GEFV, gastroesophageal flap valve.
Bold style indicates statistical significance.
Footnotes
Financial support: This work was supported by Pusan National University Hospital Clinical Research Grant (2010).
Conflicts of interest: None.
References
- 1.Vakil N, van Zanten SV, Kahrilas P, Dent J, Jones R. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006;101:1900–1920. doi: 10.1111/j.1572-0241.2006.00630.x. [DOI] [PubMed] [Google Scholar]
- 2.Dent J, El-Serag HB, Wallander MA, Johansson S. Epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut. 2005;54:710–717. doi: 10.1136/gut.2004.051821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.El-Serag HB. Time trend of gastroesophageal reflux disease: a systematic review. Clin Gastroenterol Hepatol. 2007;5:17–26. doi: 10.1016/j.cgh.2006.09.016. [DOI] [PubMed] [Google Scholar]
- 4.Wong BC, Kinoshita Y. Systematic review on epidemiology of gastroesophageal reflux disease in Asia. Clin Gastroenterol Hepatol. 2006;4:398–407. doi: 10.1016/j.cgh.2005.10.011. [DOI] [PubMed] [Google Scholar]
- 5.Cappell MS. Clinical presentation, diagnosis, and management of GERD. Med Clin North Am. 2005;89:243–291. doi: 10.1016/j.mcna.2004.08.015. [DOI] [PubMed] [Google Scholar]
- 6.Jaspersen D, Kulig M, Labenz J, et al. Prevalence of extra-oesophageal manifestations in gastro-oesophageal reflux disease: an analysis based on the ProGERD study. Aliment Pharmacol Ther. 2003;17:1515–1520. doi: 10.1046/j.1365-2036.2003.01606.x. [DOI] [PubMed] [Google Scholar]
- 7.Richter JE. Review article: extraesophageal manifestations of gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2005;22(suppl 1):70–80. doi: 10.1111/j.1365-2036.2005.02613.x. [DOI] [PubMed] [Google Scholar]
- 8.Vaezi MF, Hicks DM, Abelson TI, Richter JE. Laryngeal signs and symptoms and gastroesophageal reflux disease (GERD): a critical assessment of cause and effect association. Clin Gastroenterol Hepatol. 2003;1:333–344. doi: 10.1053/s1542-3565(03)00177-0. [DOI] [PubMed] [Google Scholar]
- 9.Vaezi MF. CON: Treatment with PPIs should not be preceded by pH monitoring in patients suspected of laryngeal reflux. Am J Gastroenterol. 2006;101:8–10. doi: 10.1111/j.1572-0241.2006.00448_3.x. [DOI] [PubMed] [Google Scholar]
- 10.Belafsky PC. PRO: Empirical treatment with PPIs is not appropriate without testing. Am J Gastroenterol. 2006;101:6–8. doi: 10.1111/j.1572-0241.2006.00448_2.x. [DOI] [PubMed] [Google Scholar]
- 11.Koufman JA, Aviv JE, Casiano RR, Shaw GY. Laryngopharyngeal reflux: position statement of the committee on speech, voice, and swallowing disorders of the American Academy of Otolaryngology-Head and Neck Surgery. Otolaryngol Head Neck Surg. 2002;127:32–35. doi: 10.1067/mhn.2002.125760. [DOI] [PubMed] [Google Scholar]
- 12.Vaezi MF, Richter JE, Stasney CR, et al. Treatment of chronic posterior laryngitis with esomeprazole. Laryngoscope. 2006;116:254–260. doi: 10.1097/01.mlg.0000192173.00498.ba. [DOI] [PubMed] [Google Scholar]
- 13.Wo JM, Koopman J, Harrell SP, Parker K, Winstead W, Lentsch E. Double-blind, placebo-controlled trial with single-dose pantoprazole for laryngopharyngeal reflux. Am J Gastroenterol. 2006;101:1972–1978. doi: 10.1111/j.1572-0241.2006.00693.x. [DOI] [PubMed] [Google Scholar]
- 14.Steward DL, Wilson KM, Kelly DH, et al. Proton pump inhibitor therapy for chronic laryngo-pharyngitis: a randomized placebo-control trial. Otolaryngol Head Neck Surg. 2004;131:342–350. doi: 10.1016/j.otohns.2004.03.037. [DOI] [PubMed] [Google Scholar]
- 15.Merati AL, Lim HJ, Ulualp SO, Toohill RJ. Meta-analysis of upper probe measurements in normal subjects and patients with laryngopharyngeal reflux. Ann Otol Rhinol Laryngol. 2005;114:177–182. doi: 10.1177/000348940511400302. [DOI] [PubMed] [Google Scholar]
- 16.Issing WJ, Karkos PD, Perreas K, Folwaczny C, Reichel O. Dual-probe 24-hour ambulatory pH monitoring for diagnosis of laryngopharyngeal reflux. J Laryngol Otol. 2004;118:845–848. doi: 10.1258/0022215042703660. [DOI] [PubMed] [Google Scholar]
- 17.Lundell LR, Dent J, Bennett JR, et al. Endoscopic assessment of oesophagitis: clinical and functional correlates and further validation of the Los Angeles classification. Gut. 1999;45:172–180. doi: 10.1136/gut.45.2.172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kimura K, Takemoto T. An endoscopic recognition of the atrophic border and its significance in chronic gastritis. Endoscopy. 1969;3:87–97. [Google Scholar]
- 19.Kimura K, Satoh K, Ido K, Taniguchi Y, Takimoto T, Takemoto T. Gastritis in the Japanese stomach. Scand J Gastroenterol Suppl. 1996;214:17–20. doi: 10.3109/00365529609094509. [DOI] [PubMed] [Google Scholar]
- 20.Hill LD, Kozarek RA, Kraemer SJ, et al. The gastroesophageal flap valve: in vitro and in vivo observations. Gastrointest Endosc. 1996;44:541–547. doi: 10.1016/s0016-5107(96)70006-8. [DOI] [PubMed] [Google Scholar]
- 21.Hill LD, Kozarek RA. The gastroesophageal flap valve. J Clin gastroenterol. 1999;28:194–197. doi: 10.1097/00004836-199904000-00002. [DOI] [PubMed] [Google Scholar]
- 22.Fujiwara Y, Higuchi K, Watanabe Y, et al. Prevalence of gastroesophageal reflux disease and gastroesophageal reflux disease symptoms in Japan. J Gastroenterol Hepatol. 2005;20:26–29. doi: 10.1111/j.1440-1746.2004.03521.x. [DOI] [PubMed] [Google Scholar]
- 23.Smit CF, Mathus-Vliegen LM, Devriese PP, Schouwenberg PF, Kupperman D. Diagnosis and consequences of gastropharyngeal reflux. Clin Otolaryngol Allied Sci. 2000;25:440–455. doi: 10.1046/j.1365-2273.2000.00418.x. [DOI] [PubMed] [Google Scholar]
- 24.Smit CF, Tan J, Devriese PP, Mathus-Vliegen LM, Brandsen M, Schouwenberg PF. Ambulatory pH measurements at the upper esophageal sphincter. Laryngoscope. 1998;108:299–302. doi: 10.1097/00005537-199802000-00027. [DOI] [PubMed] [Google Scholar]
- 25.Anandasabapathy S, Jaffin BW. Multichannel intraluminal impedance in the evaluation of patients with persistent globus sensation on proton pump inhibitor therapy. Ann Otol Rhinol Laryngol. 2006;115:563–570. doi: 10.1177/000348940611500801. [DOI] [PubMed] [Google Scholar]
- 26.Mainie I, Tutuian R, Shay S, et al. Acid and non-acid reflux in patients with persistent symptoms despite acid suppressive therapy: a multicentre study using combined ambulatory impedance-pH monitoring. Gut. 2006;55:1398–1402. doi: 10.1136/gut.2005.087668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Hila A, Agrawal A, Castell DO. Combined multichannel intraluminal impedance and pH esophageal testing compared to pH alone for diagnosing both acid and weakly acidic gastroesophageal reflux. Clin Gastroenterol Hepatol. 2007;5:172–177. doi: 10.1016/j.cgh.2006.11.015. [DOI] [PubMed] [Google Scholar]
- 28.Bajbouj M, Becker V, Neuber M, Schmid RM, Meining A. Combined pH-metry/impedance monitoring increases the diagnostic yield in patients with atypical gastroesophageal reflux symptoms. Digestion. 2007;76:223–228. doi: 10.1159/000112728. [DOI] [PubMed] [Google Scholar]
- 29.Malhotra A, Freston JW, Aziz K. Use of pH-impedance testing to evaluate patients with suspected extraesophageal manifestations of gastroesophageal reflux disease. J Clin Gastroenterol. 2008;42:271–278. doi: 10.1097/MCG.0b013e31802b64f3. [DOI] [PubMed] [Google Scholar]
- 30.Ceccatelli P, Mariottini M, Agnolucci A, Lagana C, Angioli D. Acid exposure of proximal esophagus in healthy subjects. Minerva Gastroenterol Dietol. 1998;44:129–134. [PubMed] [Google Scholar]
- 31.Bove MJ, Rosen C. Diagnosis and management of laryngopharyngeal reflux disease. Curr Opin Otolaryngol Head Neck Surg. 2006;14:116–123. doi: 10.1097/01.moo.0000193177.62074.fd. [DOI] [PubMed] [Google Scholar]
- 32.Shaker R, Milbrath M, Ren J, et al. Esophagopharyngeal distribution of refluxed gastric acid in patients with reflux laryngitis. Gastroenterology. 1995;109:1575–1582. doi: 10.1016/0016-5085(95)90646-0. [DOI] [PubMed] [Google Scholar]
- 33.Savarino E, Tutuian R, Zentilin P, et al. Am J Gastroenterol. 2010. Characteristics of reflux episodes and symptom association in patients with erosive esophagitis and nonerosive reflux disease: study using combined impedance-pH off therapy. (In press) [DOI] [PubMed] [Google Scholar]
- 34.Sharma P, Wani S, Romero Y, Johnson D, Hamilton F. Racial and geographic issues in gastroesophageal reflux disease. Am J Gastroenterol. 2008;103:2669–2680. doi: 10.1111/j.1572-0241.2008.02089.x. [DOI] [PubMed] [Google Scholar]
- 35.Kim GH, Huh KC, Lee YC, et al. Normal ambulatory 24-hour esophageal pH values in Koreans -A Multicenter study- J Korean Med Sci. 2008;23:954–958. doi: 10.3346/jkms.2008.23.6.954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Kim GH, Song GA, Kim TO, et al. Endoscopic grading of gastroesophageal flap valve and atrophic gastritis is helpful to predict gastroesophageal reflux. J Gastroenterol Hepatol. 2008;23:208–214. doi: 10.1111/j.1440-1746.2007.05038.x. [DOI] [PubMed] [Google Scholar]
- 37.Zerbib F, Stoll D. Management of laryngopharyngeal reflux: an unmet medical need. Neurogastroenterol Motil. 2010;22:109–112. doi: 10.1111/j.1365-2982.2009.01437.x. [DOI] [PubMed] [Google Scholar]