Abstract
Background/Aims
Irritable bowel syndrome (IBS) is one of the most frequently observed disorders by primary care and practitioners. The aim of this study was to estimate the prevalence of IBS using the Rome II and III criteria in the general Korean population and also to compare sociodemographic differences between subjects diagnosed by these criteria.
Methods
Telephone interview surveys were performed with a total of 1,009 individuals in Korea, 15 years of age or older. The questionnaire, based on the Rome II and III criteria, was validated.
Results
Among the 1,009 subjects, the prevalence of IBS was 8.0% under the Rome II criteria (81 subjects; 6.4%, male; 9.6%, female), and 9.0% (91 subjects; 7.0%, male; 11.0%, female) under the Rome III criteria. The accordance rate of Rome II and III was 73.5%. Both groups showed highest frequency in the age of 30s (13.9% vs. 15.3% respectively). Female subjects showed a higher prevalence than male subjects under Rome III (91 subjects; 11.0% in female, 7.0% in male; p < 0.05), but not under Rome II criteria. Many patients older than 50 years were added when analyzed under the Rome III criteria, but not under the Rome II criteria (p = 0.017).
Conclusions
The Rome III criteria were less restrictive and showed good agreement with the Rome II criteria. The prevalence of IBS was increased in young women.
Keywords: Prevalence, Irritable bowel syndrome, Rome II, Rome III
Introduction
Irritable bowel syndrome (IBS) is a functional bowel disorder in which abdominal discomfort or pain is associated with defecation or a change in bowel habit.1-3 IBS is one of the most frequently observed disorders in primary care and gastroenterology practices and accounts for 29.8 percent of visits due to gut problems.4-6 Although the clinical importance of IBS has increased, there is no biochemical or physiological indicator for diagnosis of IBS. In view of increasing diagnostic accuracy, the Rome III criteria have been suggested as standardized diagnostic criteria for IBS.7-12
In 1978, Manning published the first symptom-based diagnostic criteria for IBS.7,13,14 However, the Manning criteria had no provision for frequency or duration of symptoms and had no diagnostic value for men.15 Since an international expert working team first presented criteria for Rome I in 1988, the definition of IBS has changed. In 2006, the Rome III criteria were proposed. 7-12 There were several changes from the Rome II to the Rome III criteria. A distinctive difference between the Rome II and III criteria is timeframe. Unlike with the Rome II criteria, symptoms must have originated 6 months prior to diagnosis, be currently active, and have been active for the past 3 months, in the Rome III criteria. Furthermore, the Rome III criteria applied simple classification derived from stool consistency to categorize IBS.8-10
Previous studies have reported that the prevalence of IBS varies according to revisions of diagnostic criteria for IBS.8,12,16-20 Many studies have assessed that the overall prevalence of IBS as up to approximately 25% using the Manning and the Rome criteria worldwide.12,21,22 To date, the prevalence of IBS in Korea using the Rome II criteria has been estimated as ranging from 6.6% to 16.8%.23,24 Many studies about diagnostic criteria for IBS have been performed since the publication of the Rome III criteria. However, there are few studies regarding the prevalence of IBS diagnosed by the Rome II criteria in Asian countries,23,24 and the Rome III criteria have only recently been published to diagnose and classify IBS. Moreover, only a few studies have compared the Rome II and III criteria for IBS, worldwide.8,18
The aim of this study was to estimate the prevalence of IBS using the Rome II and III criteria in the Korean general population and also to compare sociodemographic differences among the subjects diagnosed by these criteria.
Materials and Methods
1. Sampling procedures
The telephone interview survey was performed by Gallup, based in Korea, using a reliable and validated questionnaire based on the Rome II and III criteria (Korean version). A random sample of telephone numbers in nationwide scale was selected from the 8 districts of South Korea. The questionnaire was administered to 1,009 subjects age 15 or over, evenly distributed by gender and age, and a random digit dialing sample was obtained using the Kish sampling procedure.
2. Recruitment, questionnaire, and validation
The interviewer explained the aim of our study to all eligible individuals and asked individuals to participate in a survey about IBS and other functional bowel diseases. All respondents gave the interviewer verbal informed consent prior to participation in the survey, and the telephone interview survey was performed by the interviewer, who had been trained by a gastroenterologist.
The questionnaire, containing 22 response items, consisted of several general questions (gender, age, region, education, household income, and occupation) and more specific questions associated with diagnosis of IBS and other functional bowel disorders using the Rome II and III criteria. Among the questions, 15 questions were used for these studies. Respondents with a history of chronic illness, such as colon cancer, colitis, inflammatory bowel disease, hemorrhoids, diabetes, liver disease, or heart disease, as well as pregnant subjects, were excluded from the telephone survey.
The questionnaire, using the Rome II and III criteria, was translated into Korean, in accordance with guidelines suggested by Guilleman et al.25 The translation was conducted by 2 translators and back-translated into English by 2 other translators. If the subject refused to answer the questionnaire, the telephone interview was discontinued. The total interview took approximately 20 minutes. The response rate of the telephone interview survey was 20.2% (n = 1,009). The study was approved by the Hospital Ethical Committee for Clinical Investigations.
3. Definition
Subjects responded to the questionnaire based on the Rome II and III criteria. For a diagnosis of IBS to be made, the subject needed to have at least 2 of the following 3 symptoms: (1) relief with defecation, and/or (2) onset associated with a change in frequency of stool, and/or (3) onset associated with a change in appearance of stool. Subjects diagnosed using the Rome III criteria have abdominal discomfort or pain at least 3 days/month in the last 3 months, and subjects diagnosed using the Rome II criteria have abdominal discomfort or pain for at least 12 weeks, which need not be consecutive, in the preceding 12 months.7-10
For the purpose of classifying the subtype of IBS, all subjects diagnosed with IBS using the Rome II and Rome III criteria were asked for their stool form based on the Bristol Stool Form Scale, proposed by the Rome III criteria.9 According to the Bristol Stool Form Scale, we classified all IBS patients into IBS with constipation (IBS-C)- hard or lumpy stools ≥ 25% and mushy or watery stools < 25% of bowel movement; IBS with diarrhea (IBS-D)- mushy or watery stool ≥ 25% and hard or lumpy stools < 25% of bowel movements; Mixed IBS- hard or lumpy stools ≥ 25% and mushy or watery stools ≥ 25% of bowel movements; Unsubtyped IBS- insufficient abnormality of stool consistency to meet criteria for IBS-C, D or mixed IBS.
Subjects fulfilling the Rome II diagnostic criteria were also classified into subtypes using the Bristol Stool Form Scale. So we compared IBS subtypes using Rome III criteria to IBS subtypes using the 'adjusted' Rome II criteria.
4. Statistical methods
Statistical analyses were performed using a SPSS package version 12.0. All data were presented as frequency and percentage for categorized variables using the χ2 test. If 1 or 2 of the cells in a two-by-two contingency table had numbers less than 5, the Fisher's exact test was used. The agreement between 2 diagnostic criteria defining the subjects was assessed using Cohen's κ statistics. Values for κ score represented ≥ 0.81 very good agreement, 0.61-0.80 good agreement, 0.41-0.60 moderate agreement, 0.21-0.40 fair agreement, and < 0.21 poor agreement. The respective 95% confidence intervals for the rates were calculated. Values of p < 0.05 were considered to be statistically significant.
Results
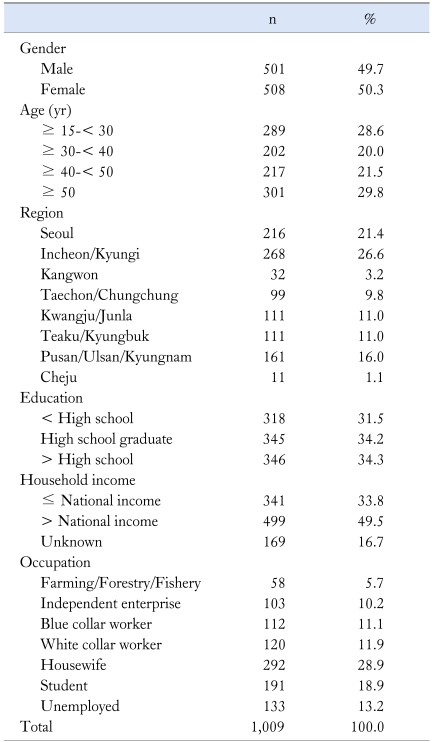
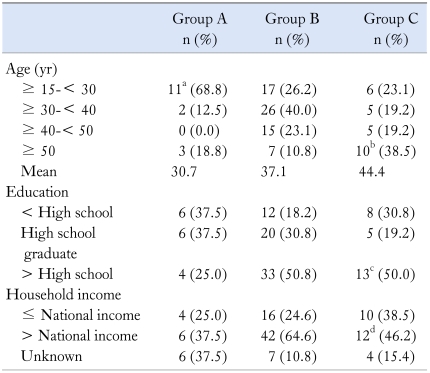
The response rate of the telephone survey was 26.2% (n = 1,009). These respondents, aged 15 or more (range 15-87), were stratified by gender and age. The mean age of our population was 41.1 ± 16.8 years (male 40.0 ± 17.4 vs. female 42.2 ± 16.2, not significant), and 49.7% of the respondents were male. The basic characteristics of respondents are shown in Table 1.
Table 1.
Baseline Characteristics
1. Prevalence of IBS
The prevalence of the Rome II and III diagnostic criteria according to sociodemographic characteristics are indicated in Table 2. Of the 1,009 respondents (male, n = 501; female, n = 508), 81 individuals fulfilled the Rome II criteria for diagnosis of IBS (8.0%): 32 male subjects (6.4%) and 49 female subjects (9.6%). Among the subjects diagnosed by the Rome II criteria, female subjects tend to have a higher prevalence of IBS than male subjects. However, there is no significant difference (p = 0.057) between genders. Of the 1,009 respondents, 91 subjects (9.0%) meet the Rome III criteria: 56 female subjects (11.0%) and 35 male subjects (7.0%), with a significantly higher prevalence in female subjects (p = 0.025). The prevalence of IBS based on age distribution according to the Rome II criteria is significantly higher among those in their 30s (p = 0.001). Similarly, according to Rome III criteria, the prevalence of IBS based on age distribution is significantly higher among those in their 30s (p = 0.004). The higher the education level of the respondents, the more frequent the occurrence of IBS (Rome II criteria). Higher education level is significantly correlated with a higher prevalence of IBS according to the Rome III criteria, but not the Rome II criteria.
Table 2.
Prevalence of Irritable Bowel Syndrome by Sociodemographic Characteristics According to the Rome II and III criteria
ap < 0.05 when compared to difference among age distributions of irritable bowel syndrome (IBS) (in Rome II and III, respectively), bp < 0.05 when compared to difference among educational levels of IBS (in Rome III), cp = 0.05 when compared to difference among income of IBS (in Rome II), dp = 0.121 when compared to difference among income of IBS (in Rome III).
According to Rome II criteria, the prevalence of IBS is highest (15%, 19 women of 127 subjects) in women age 15-29, while, according to Rome III criteria, the prevalence of IBS is highest (14%, 16 women of 114 subjects) in women age 30-39. For men, the prevalence of IBS is highest in those age 30-39 under both Rome II and Rome III (15.9%, 14 men and 17%, 15 men of 88 subjects, respectively) criteria (data not shown).
In this study, subjects with IBS were divided into 2 groups based on household income: above the national average or below the national average. Subjects with incomes above the national average have a significantly higher prevalence of IBS than subjects below the national average under the Rome II criteria (p = 0.05). However, under the Rome III criteria, there was no statistically significant difference (p = 0.121).
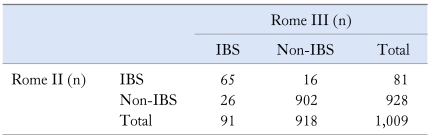
When the agreement rate (Table 3) was assessed using κ statistics between the 2 sets of Rome diagnostic criteria for IBS patients (Rome II vs. III), there was a good agreement regarding the prevalence of IBS based on the diagnostic criteria (κ score = 0.733). Among patients with IBS, as determined by the Rome II critieria, 65 subjects (6.4%) fulfill the Rome III criteria. In total, 107 subjects (10.6%) were diagnosed with IBS using the Rome II or the Rome III criteria.
Table 3.
Agreement Between the Two Ways to Define Irritable Bowel Syndrome Based on the Diagnostic Criteria
IBS, irritable bowel syndrome.
κ Score = 0.733, p < 0.001.
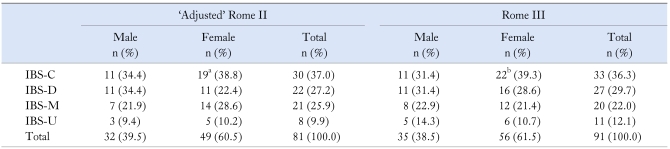
2. Subtypes of IBS and the Rome diagnostic criteria
We categorized all IBS diagnosed with the Rome II and III criteria into four subtypes based on the Bristol Stool Form Scale. We note high proportions of IBS-C using the Rome III criteria and using the 'adjusted' Rome II criteria (Table 4). Of the 49 female subjects diagnosed with IBS using the 'adjusted' Rome II criteria, 19 subjects (38.8%) were included in the IBS-C group. However, there is no significant gender difference between the groups when using the 'adjusted' Rome II criteria (p > 0.05). Similarly, there is no significant difference in the prevalence of IBS between male and female subjects according to the Rome III criteria (p > 0.05).
Table 4.
Proportion of IBS Subtype by Gender According to the 'Adjusted' Rome II and III criteria
ap > 0.05 when compared to difference between gender distributions of IBS in 'adjusted' Rome II, bp > 0.05 when compared to difference between gender distributions of IBS in Rome III.
IBS, irritable bowel syndrome; IBS-C, irritable bowel syndrome with constipation; IBS-D, irritable bowel syndrome with diarrhea; IBS-M, mixed irritable bowel syndrome; IBS-U, unsubtyped irritable bowel syndrome.
3. IBS subgroups and Rome diagnostic criteria
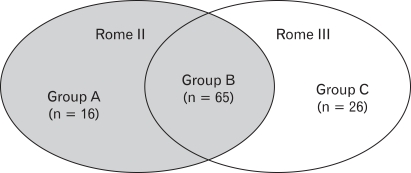
A schematic representation of subgroups according to the Rome criteria is shown in Figure 1. Group A is comprised of 16 subjects (1.6%) who met the Rome II criteria but not the Rome III criteria and Group C is comprised of 26 subjects (2.6%) who met the Rome III criteria but not the Rome II criteria. Of all 1,009 respondents, the 65 subjects (6.4%) who fulfilled both the Rome II and III criteria are designated as Group B. Table 5 includes the proportion of IBS subgroups by sociodemographic characteristics.
Figure 1.
Schematic representation of the groups fulfilling both the Rome II and III criteria. Group A, subjects fulfilling the Rome II criteria but not the Rome III criteria; Group B, subjects fulfilling both the Rome II and Rome III criteria; Group C, subjects fulfilling the Rome III criteria but not the Rome II criteria.
Table 5.
Proportion of Irritable Bowel Syndrome by Sociodemographic Characteristics in Group A, B, and C
ap = 0.001 when compared with subjects in group B, bp = 0.017 when compared with subjects in group B, cp > 0.05 when compared with subjects in group B, dp > 0.05 when compared with subjects in group B.
IBS, irritable bowel syndrome; Group A, subjects fulfilling the Rome II criteria but not the Rome III criteria; Group B, subjects fulfilling both the Rome II criteria and Rome III criteria; Group C, subjects fulfilling the Rome III criteria but not Rome II criteria.
In Group A, the mean age is 30.7 years, and the proportion of IBS was significantly high in their age 15-29. In Group C, the mean age is 44.4 years old, with 57.7% of them older than 40 years of age. As the diagnostic criteria of IBS has changed from the Rome III to the Rome III, those older than 50 years are increased, significantly (p = 0.017).
The higher education level of subjects in group B, the more frequent occurrence of IBS. However, there is no significant relationship between educational level and frequency of IBS in subjects in group A and C, compared with those in group B. The proportion of subjects above the national income is relatively higher in all groups, whereas the results are not significant (p > 0.05).
Discussion
The prevalence of IBS varies enormously depending on the diagnostic criteria employed. In a study of 2,000 individuals in Spain, the prevalence values obtained using the Rome II criteria were lower (3.3%) than those obtained using the Manning and the Rome I criteria (10.3% and 12.1%, respectively).19 Several reports using the Rome I criteria showed that the prevalence of IBS ranged from 9.5% to 15.0%, whereas the studies using the Rome II criteria showed that the prevalence of IBS ranged from 2.3% to 6.9%.16,17,20 These studies from around the world using the Rome criteria reveal that the prevalence is lower when using the Rome II criteria than when using the Manning and Rome I criteria.
A recent report of 10,000 Israeli adults showed that the prevalence of IBS is significantly higher using the Rome III criteria, as compared with the Rome II criteria (11.4% vs. 2.9%).8 The prevalence rate of IBS by the Rome II criteria was unexpectedly low, and subjects diagnosed with IBS by the Rome II criteria had higher consultation rates. Additionally, IBS patients diagnosed by the Rome II criteria had chronic symptoms (at least 12 weeks over 12 months). The complexity of the disease and the extended time frame make recalling symptoms difficult, especially for older individuals. The Rome III criteria are easier and more understandable for elderly population.
In the present study, the prevalence for IBS was higher by the Rome III criteria, as compared with the Rome II criteria, and the age distribution shifted to the right. These results reflect variation in IBS prevalence, depending on different diagnostic criteria.
In general, we found that IBS prevalence is higher in women than men. There are several potential reasons for the gender difference. For example, in women, IBS may be associated with an antinociceptive mechanism minimizing pain related to pelvic events (e.g., pregnancy and delivery).26 Additionally, gender differences affect serotonin synthesis in brain,27 and female sex hormones affect gastrointestinal motility in female IBS patients.28,29 However, other studies have shown that gender distribution varies according to socioeconomic status by nation. Drossman et al.30 reported that the IBS prevalence using the Rome criteria was 14.5% in women and 7.7% in men among U.S. households. Similarly, the prevalence of IBS among Japanese and Dutch women (31% and 21%, respectively) was higher that than among men (23% and 7%, respectively).31 On the other hand, a study with 2,486 adults in Beijing showed no gender difference between men and women (1 vs. 1.15),29 and in Hong Kong and Singapore, the prevalence of IBS using the Rome II criteria was not markedly higher in women than in men.32,33 Moreover in India, a study of 2,000 subjects showed that IBS prevalence is higher in men than in women (7.9% vs. 6.9%).34 Interestingly, we previously reported that the prevalence of IBS was 6.6%, and there was no gender difference in IBS prevalence (7.1%, male; 6.0%, female) 5 years earlier using the Rome II criteria. However, in our present study, female subjects showed a higher IBS prevalence than male subjects under the Rome II and III criteria. The most striking difference between our previous study and this current study is the change of occupational status among women in Korea. The proportion of women with careers increased 7.1%, while the proportion of housewives decreased from 64.5% (343 housewives of 531 female subjects) to 57.4% (292 housewives of 508 female subjects) over the 5 years.24
Several studies have reported that the prevalence of IBS is aligned with household income and socioeconomic status. Gwee et al.35 reported that there is a significantly higher prevalence of IBS among those living on their landed property, as compared to those living in apartments or public housing (16.8% vs. 8.2%, respectively) and among those with more than 6 years of post secondary education (9.8% vs. 5.9% ≤ 6 years). Other Asian studies reported the significantly higher prevalence of IBS in city than in rural areas (10.5% vs. 6.14%),29 whereas another study showed IBS was no longer associated with educational level.36-38 In the present study, subjects with higher household income have a significantly higher prevalence of IBS under the Rome II criteria. We also found a significant correlation between the prevalence of IBS and higher education level according to the Rome III criteria.
In schematic presentation of subgroups according to the Rome criteria, the proportion of subjects below 30 years old was higher in group A than group B. As a result, the subjects in group A are young enough to understand disease and to remember more severe symptoms for a longer period, thus meeting the Rome II criteria. Diagnostic criteria for IBS has evolved from the Manning criteria although are still imperfect. Debate of the over the Rome criteria with regard to timeframe and definition of severity continues, and subgroup characterization will be necessary to improve IBS diagnosis.
One limitation of the present study need is a lack of survey method diversity designed to improve response rate, as compared to that of previous studies. Lau et al.32 and Masud et al.39 conducted a house-to-house survey and yielded a response rate of over 90%. Documentary questionnaires had a somewhat higher response rate, ranging from 58.4% to 74.0%,23,30,33 whereas the response rate of our telephone survey was relatively low (20.2%). The relatively poor response rate could influence investigators to omit 'true' IBS patients, although the sample had been selected within the 95% confidence intervals, and the present study has been validated. Another limitation of the present study is a lack of inquiry about confounding factors. Previous reports revealed that history of medication (analgesics, such as NSAIDs), food allergies, recent dysentery, psychological stress, and body mass index were significantly associated with the prevalence of IBS.36-38
In conclusion, the prevalence of IBS in the South Korean population is 9.0% by the Rome III criteria and 8.0% by the Rome II criteria. Using either set of criteria, female subjects tend to have a higher prevalence of disease than male subjects. The Rome III criteria are less restrictive than but show good agreement overall with the Rome II criteria in diagnosing IBS.
Footnotes
Financial support: None.
Conflicts of interest: None.
References
- 1.Thompson WG, Longstreth GF, Drossman DA, Heaton KW, Irvine EJ, Muller-Lissner SA. Functional bowel disorders and functional abdominal pain. Gut. 1999;45(suppl 2):II43–II47. doi: 10.1136/gut.45.2008.ii43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Horwitz BJ, Fisher RS. The irritable bowel syndrome. N Engl J Med. 2001;344:1846–1850. doi: 10.1056/NEJM200106143442407. [DOI] [PubMed] [Google Scholar]
- 3.Drossman DA, Camilleri M, Mayer EA, Whitehead WE. AGA technical review on irritable bowel syndrome. Gastroenterology. 2002;123:2108–2131. doi: 10.1053/gast.2002.37095. [DOI] [PubMed] [Google Scholar]
- 4.Thompson WG, Heaton KW, Smyth GT, Smyth C. Irritable bowel syndrome in general practice: prevalence, characteristics, and referral. Gut. 2000;46:78–82. doi: 10.1136/gut.46.1.78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Everhart JE, Renault PF. Irritable bowel syndrome in office-based practice in the United States. Gastroenterology. 1991;100:998–1005. doi: 10.1016/0016-5085(91)90275-p. [DOI] [PubMed] [Google Scholar]
- 6.American Gastroenterological Association medical position statement: irritable bowel syndrome. Gastroenterology. 1997;112:2118–2119. doi: 10.1053/gast.1997.1122118. [DOI] [PubMed] [Google Scholar]
- 7.Thompson WG. The road to rome. Gastroenterology. 2006;130:1552–1556. doi: 10.1053/j.gastro.2006.03.011. [DOI] [PubMed] [Google Scholar]
- 8.Sperber AD, Shvartzman P, Friger M, Fich A. A comparative reappraisal of the Rome II and Rome III diagnostic criteria: are we getting closer to the 'true' prevalence of irritable bowel syndrome. Eur J Gastroenterol Hepatol. 2007;19:441–447. doi: 10.1097/MEG.0b013e32801140e2. [DOI] [PubMed] [Google Scholar]
- 9.Longstreth GF, Thompson WG, Chey WD, Houghton LA, Mearin F, Spiller RC. Functional bowel disorders. Gastroenterology. 2006;130:1480–1491. doi: 10.1053/j.gastro.2005.11.061. [DOI] [PubMed] [Google Scholar]
- 10.Hillila MT, Farkkila MA. Prevalence of irritable bowel syndrome according to different diagnostic criteria in a non-selected adult population. Aliment Pharmacol Ther. 2004;20:339–345. doi: 10.1111/j.1365-2036.2004.02034.x. [DOI] [PubMed] [Google Scholar]
- 11.Drossman DA. The functional gastrointestinal disorders and the Rome III process. Gastroenterology. 2006;130:1377–1390. doi: 10.1053/j.gastro.2006.03.008. [DOI] [PubMed] [Google Scholar]
- 12.Chey WD, Olden K, Carter E, Boyle J, Drossman D, Chang L. Utility of the Rome I and Rome II criteria for irritable bowel syndrome in U.S. women. Am J Gastroenterol. 2002;97:2803–2811. doi: 10.1111/j.1572-0241.2002.07026.x. [DOI] [PubMed] [Google Scholar]
- 13.Talley NJ, Phillips SF, Melton LJ, Mulvihill C, Wiltgen C, Zinsmeister AR. Diagnostic value of the Manning criteria in irritable bowel syndrome. Gut. 1990;31:77–81. doi: 10.1136/gut.31.1.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Jeong H, Lee HR, Yoo BC, Park SM. Manning criteria in irritable bowel syndrome: its diagnostic significance. Korean J Intern Med. 1993;8:34–39. doi: 10.3904/kjim.1993.8.1.34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Smith RC, Greenbaum DS, Vancouver JB, et al. Gender differences in manning criteria in the irritable bowel syndrome. Gastroenterology. 1991;100:591–595. doi: 10.1016/0016-5085(91)80002-q. [DOI] [PubMed] [Google Scholar]
- 16.Banerjee R, Choung OW, Gupta R, et al. Rome I criteria are more sensitive than Rome II for diagnosis of irritable bowel syndrome in Indian patients. Indian J Gastroenterol. 2005;24:164–166. [PubMed] [Google Scholar]
- 17.Boyce PM, Koloski NA, Talley NJ. Irritable bowel syndrome according to varying diagnostic criteria: are the new Rome II criteria unnecessarily restrictive for research and practice? Am J Gastroenterol. 2000;95:3176–3183. doi: 10.1111/j.1572-0241.2000.03197.x. [DOI] [PubMed] [Google Scholar]
- 18.Gwee KA. Irritable bowel syndrome and the Rome III criteria: for better or for worse? Eur J Gastroenterol Hepatol. 2007;19:437–439. doi: 10.1097/MEG.0b013e328013c0fa. [DOI] [PubMed] [Google Scholar]
- 19.Mearin F, Badia X, Balboa A, et al. Irritable bowel syndrome prevalence varies enormously depending on the employed diagnostic criteria: comparison of Rome II versus previous criteria in a general population. Scand J Gastroenterol. 2001;36:1155–1161. doi: 10.1080/00365520152584770. [DOI] [PubMed] [Google Scholar]
- 20.Mearin F, Roset M, Badia X, et al. Splitting irritable bowel syndrome: from original Rome to Rome II criteria. Am J Gastroenterol. 2004;99:122–130. doi: 10.1046/j.1572-0241.2003.04024.x. [DOI] [PubMed] [Google Scholar]
- 21.Olden KW. Diagnosis of irritable bowel syndrome. Gastroenterology. 2002;122:1701–1714. doi: 10.1053/gast.2002.33741. [DOI] [PubMed] [Google Scholar]
- 22.Camilleri M, Choi MG. Review article: irritable bowel syndrome. Aliment Pharmacol Ther. 1997;11:3–15. doi: 10.1046/j.1365-2036.1997.84256000.x. [DOI] [PubMed] [Google Scholar]
- 23.Park KS, Ahn SH, Hwang JS, et al. A survey about irritable bowel syndrome in South Korea: prevalence and observable organic abnormalities in IBS patients. Dig Dis Sci. 2008;53:704–711. doi: 10.1007/s10620-007-9930-1. [DOI] [PubMed] [Google Scholar]
- 24.Han SH, Lee OY, Bae SC, et al. Prevalence of irritable bowel syndrome in Korea: population-based survey using the Rome II criteria. J Gastroenterol Hepatol. 2006;21:1687–1692. doi: 10.1111/j.1440-1746.2006.04269.x. [DOI] [PubMed] [Google Scholar]
- 25.Guillemin F, Bombardier C, Beaton D. Cross-cultural adaptation of health-related quality of life measures: literature review and proposed guidelines. J Clin Epidemiol. 1993;46:1417–1432. doi: 10.1016/0895-4356(93)90142-n. [DOI] [PubMed] [Google Scholar]
- 26.Unruh AM. Gender variations in clinical pain experience. Pain. 1996;65:123–167. doi: 10.1016/0304-3959(95)00214-6. [DOI] [PubMed] [Google Scholar]
- 27.Nishizawa S, Benkelfat C, Young SN, et al. Differences between males and females in rates of serotonin synthesis in human brain. Proc Natl Acad Sci (USA) 1997;94:5308–5313. doi: 10.1073/pnas.94.10.5308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wald A, Van Thiel DH, Hoechstetter L, et al. Gastrointestinal transit: the effect of the menstrual cycle. Gastroenterology. 1981;80:1497–1500. [PubMed] [Google Scholar]
- 29.Pan G, Lu S, Ke M, Han S, Guo H, Fang X. Epidemiologic study of the irritable bowel syndrome in Beijing: stratified randomized study by cluster sampling. Chin Med J (Engl) 2000;113:35–39. [PubMed] [Google Scholar]
- 30.Drossman DA, Li Z, Andruzzi E, et al. U.S. householder survey of functional gastrointestinal disorders. Prevalence, sociodemography, and health impact. Dig Dis Sci. 1993;38:1569–1580. doi: 10.1007/BF01303162. [DOI] [PubMed] [Google Scholar]
- 31.Schlemper RJ, van der Werf SD, Vandenbroucke JP, Biemond I, Lamers CB. Peptic ulcer, non-ulcer dyspepsia and irritable bowel syndrome in The Netherlands and Japan. Scand J Gastroenterol Suppl. 1993;200:33–41. doi: 10.3109/00365529309101573. [DOI] [PubMed] [Google Scholar]
- 32.Lau EM, Chan FK, Ziea ET, Chan CS, Wu JC, Sung JJ. Epidemiology of irritable bowel syndrome in Chinese. Dig Dis Sci. 2002;47:2621–2624. doi: 10.1023/a:1020549118299. [DOI] [PubMed] [Google Scholar]
- 33.Ho KY, Kang JY, Seow A. Prevalence of gastrointestinal symptoms in a multiracial Asian population, with particular reference to reflux-type symptoms. Am J Gastroenterol. 1998;93:1816–1822. doi: 10.1111/j.1572-0241.1998.00526.x. [DOI] [PubMed] [Google Scholar]
- 34.Shah SS, Bhatia SJ, Mistry FP. Epidemiology of dyspepsia in the general population in Mumbai. Indian J Gastroenterol. 2001;20:103–106. [PubMed] [Google Scholar]
- 35.Gwee KA, Wee S, Wong ML, Png DJ. The prevalence, symptom characteristics, and impact of irritable bowel syndrome in an asian urban community. Am J Gastroenterol. 2004;99:924–931. doi: 10.1111/j.1572-0241.2004.04161.x. [DOI] [PubMed] [Google Scholar]
- 36.Xiong LS, Chen MH, Chen HX, Xu AG, Wang WA, Hu PJ. A population-based epidemiologic study of irritable bowel syndrome in South China: stratified randomized study by cluster sampling. Aliment Pharmacol Ther. 2004;19:1217–1224. doi: 10.1111/j.1365-2036.2004.01939.x. [DOI] [PubMed] [Google Scholar]
- 37.Minocha A, Chad W, Do W, Johnson WD. Racial differences in epidemiology of irritable bowel syndrome alone, un-investigated dyspepsia alone, and "overlap syndrome" among african americans compared to Caucasians: a population-based study. Dig Dis Sci. 2006;51:218–226. doi: 10.1007/s10620-006-3112-4. [DOI] [PubMed] [Google Scholar]
- 38.Drossman DA, McKee DC, Sandler RS, et al. Psychosocial factors in the irritable bowel syndrome. A multivariate study of patients and nonpatients with irritable bowel syndrome. Gastroenterology. 1988;95:701–708. doi: 10.1016/s0016-5085(88)80017-9. [DOI] [PubMed] [Google Scholar]
- 39.Masud MA, Hasan M, Khan AK. Irritable bowel syndrome in a rural community in Bangladesh: prevalence, symptoms pattern, and health care seeking behavior. Am J Gastroenterol. 2001;96:1547–1552. doi: 10.1111/j.1572-0241.2001.03760.x. [DOI] [PubMed] [Google Scholar]