Abstract
Newer developing techniques for esophageal functional testing such as wireless pH capsule monitoring and esophageal impedance testing are currently available. However, ambulatory 24 hr esophageal pH monitoring is still widely used and provides quantitative data on esophageal acid exposure and the ability to correlate symptoms with acid exposure events. To properly analyze the result of pH monitoring, it is recommended to interpret in the order presented: visual inspection, computer calculation and symptom correlation.
Keywords: Ambulatory 24 hr esophageal pH monitoring, Gastroesophageal reflux, Reference values
Introduction
Recently, newer techniques for esophageal functional testing such as wireless pH capsule monitoring, duodenogastroesophageal reflux detection and esophageal impedance testing have been introduced and are currently available in clinical practice. However, ambulatory 24 hr esophageal pH monitoring is still widely used and provides quantitative data on esophageal acid exposure and on the temporal correlation between patient's symptoms and reflux events. To apply the results of pH monitoring in treating a patient, proper and coherent interpretation should be preceded.1,2 Once assuming that a complete record has been acquired, then we can proceed to interpretation and analysis of data in the order described.
1. Visual inspection
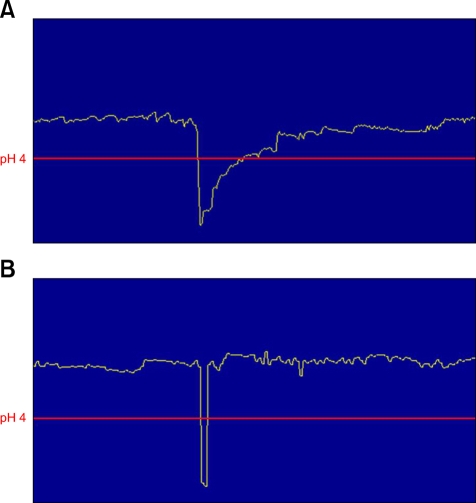
Initially the entire record should be displayed on a computer screen and the character of the pH tracing should be visually inspected (Fig. 1). This makes it possible to identify acid reflux episodes as abrupt drops in pH to a level below pH of 4. These abrupt drops in pH indicate reflux of acidic materials. The recording system arbitrarily decides the sampling rate (usually 4 seconds) at which the pH data is recorded. The pH may remain low for a variable time period and then gradually, often in a step-wise fashion, increases back to baseline (Fig. 2A). This neutralization occurs both due to the clearance of the refluxed acid back into the stomach either by gravity or esophageal clearance and due to the repeated swallowings of alkaline saliva or ingested food. It is important to differentiate reflux episodes presenting with an acute drop in pH from other drops in pH. Gradual acidification can be seen in patients who have esophageal retention due to, for example, achalasia. If one relies exclusively on the numerical data, it is possible to erroneously diagnose an acid reflux, when in fact what has occurred is physiologic intra-esophageal acidification. Occasionally, technical problems due to the dislodgment of the reference electrode may lead to an apparent drop in pH usually to 0 and these episodes need to be excluded from any calculation (Fig. 2B). One needs to analyze tracings visually and correlate the changes in pH with diary events recorded by the patient, such as symptoms of heartburn, chest pain, respiratory symptoms, belching, as well as changes in position including the time period during which the patient sleeps. Certain technical problems can produce apparent drops in pH. These could be by a poorly connected reference electrode, faulty connection or probe failure which may be analyzed by the computer as reflux events. These should be excluded from the analysis prior to computer calculation.
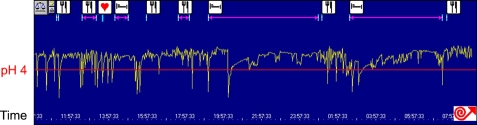
Figure 1.
This is an ambulatory pH recording from a patient who shows typical reflux pattern. With the entire record at a glance, many reflux episodes both in the upright and supine periods are noted.
Figure 2.
(A) Cardinal features of a reflux episode. Abrupt drop in pH occurs and then gradually, often in a step-wise fashion, it increases back to baseline. (B) Apparent drop in pH due to technical problems such as a poorly connected reference electrode or faulty connection. Abrupt drop in pH occurs and then rapidly, increases back to baseline. This episode should be excluded for accurate interpretation.
2. Computer calculation
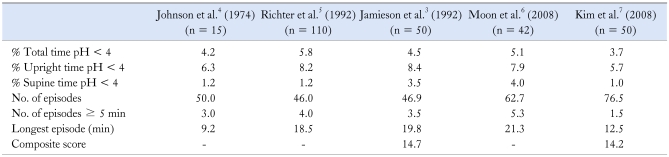
The analyst can enter the diary events into the computer program so that the computer-based analysis of various parameters can be made. Several parameters are routinely calculated by the software including: the frequency and duration of reflux episodes, the total number of reflux episodes and those which last longer than 5 minutes and duration of the longest episode. These parameters are detailed into the upright, supine and total time periods of the recording. The single parameter which has been shown to best correlate with endoscopic damage is the total time period of pH less than 4.3 The physiologic significance of a pH < 4 lies in the fact that pH must be < 4 for mucosal damage to occur. Non-acidic substances such as pepsin are not active unless the pH is < 4. Ambulatory normal values tend to show a higher degree of variability during the daytime and this probably are related to the normal variations in eating and physical activity. Reference values of the pH parameters, as 95th percentiles in 3 previous Western studies3-5 and in Korea,6,7 are shown in Table 1.
Table 1.
Reference Values of Ambulatory 24 hr Esophageal pH Monitoring in Western Countries and Korea
The data is displayed as 95th percentiles.
3. Symptom correlation
An advantage of ambulatory 24 hr esophageal pH monitoring is the ability to correlate symptoms with acid exposure events. Still, there is no convention defining the time interval around a symptom episode within which a reflux event is accepted as causative. Generally, the time interval is restrictive to be confined to 2-minute interval before onset of symptom.8 Several methods have been devised to use statistical calculations to correlate symptoms with acid reflux.
The first scheme is the symptom index (SI).9 This involves dividing the number of symptoms associated with pH < 4 by the total number of symptoms yielding a percentage of symptom episodes that correlate with gastroesophageal reflux disease. Symptom indices can be separately calculated for each symptom attributable to reflux including heartburn, regurgitation, or chest pain. Analysis using receiver operating characteristic curves designed to optimize sensitivity and specificity derived a value of 50% as the optimal threshold for a positive SI for patients with multiple episodes of heartburn.2 The SI has an important limitations of not taking the total number of reflux episodes into account.
The second devised scheme is the symptom sensitivity index (SSI).10 This involves dividing the total number of reflux episodes associated with symptoms by the total number of reflux episodes. This system is also limited and failed to take into account of the total number of symptom episodes.
The proposed scheme with the best statistical validity for symptom-reflux correlation is the symptom probability analysis (SAP).11 This involves constructing a contingency table with 4 fields: (1) positive symptom, positive reflux; (2) negative symptom, positive reflux; (3) positive symptom, negative reflux; and (4) negative symptom, negative reflux. The Fisher's exact test is then applied to calculate the probability of the observed association between reflux and symptoms to occur by chance. Therefore, the SAP determines the statistical validity of symptom-reflux association while the SI and SSI provide data on the strength of the association.
A major shortcoming in using any of the available symptom indices is in the completeness by which patients record their symptom events. Symptoms may occur as prolonged rather than transitory events, which can lead to inaccuracies in their association with short drops in pH. Laryngeal symptoms are generally chronic symptoms that may not demonstrate direct association with individual reflux episodes. On the other hand, symptom indices rely on correlation with acid reflux events that may go undetected with less frequent sampling rates of currently used pH monitoring systems.
Conclusion
Even though newer esophageal functional tests such as wireless pH capsule monitoring or esophageal impedance testing are currently available, ambulatory 24 hr esophageal pH monitoring is still widely used and it provides quantitative data and causal relationship. Therefore, if its data is properly interpreted, the usefulness of 24 hr ambulatory pH monitoring would be more increased in clinical practice.
Footnotes
Financial support: None.
Conflicts of interest: None.
References
- 1.American Gastroenterological Association medical position statement: guidelines on the use of esophageal pH recording. Gastroenterology. 1996;110:1981. doi: 10.1053/gast.1996.1101981. [DOI] [PubMed] [Google Scholar]
- 2.Hirano I, Richter JE. ACG practice guidelines: esophageal reflux testing. Am J Gastroenterol. 2007;102:668–685. doi: 10.1111/j.1572-0241.2006.00936.x. [DOI] [PubMed] [Google Scholar]
- 3.Jamieson JR, Stein HJ, DeMeester TR, et al. Ambulatory 24-h esophageal pH monitoring: normal values, optimal thresholds, specificity, sensitivity, and reproducibility. Am J Gastroenterol. 1992;87:1102–1111. [PubMed] [Google Scholar]
- 4.Johnson LF, Demeester TR. Twenty-four-hour pH monitoring of the distal esophagus. A quantitative measure of gastroesophageal reflux. Am J Gastroenterol. 1974;62:325–332. [PubMed] [Google Scholar]
- 5.Richter JE, Bradley LA, DeMeester TR, Wu WC. Normal 24-hr ambulatory esophageal pH values. Influence of study center, pH electrode, age, and gender. Dig Dis Sci. 1992;37:849–856. doi: 10.1007/BF01300382. [DOI] [PubMed] [Google Scholar]
- 6.Moon W, Park MI, Kim GM, et al. Normal 24-hour ambulatory esophageal pH values in Koreans. Gut and Liver. 2008;2:8–13. doi: 10.5009/gnl.2008.2.1.8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kim GH, Huh KC, Lee YC, et al. Normal ambulatory 24-hour esophageal pH values in Koreans - a multicenter study. J Korean Med Sci. 2008;23:954–958. doi: 10.3346/jkms.2008.23.6.954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lam HG, Breumelhof R, Roelofs JM, Van Berge Henegouwen GP, Smout AJ. What is the optimal time window in symptom analysis of 24-hour esophageal pressure and pH data? Dig Dis Sci. 1994;39:402–409. doi: 10.1007/BF02090215. [DOI] [PubMed] [Google Scholar]
- 9.Wiener GJ, Richter JE, Copper JB, Wu WC, Castell DO. The symptom index: a clinically important parameter of ambulatory 24-hour esophageal pH monitoring. Am J Gastroenterol. 1988;83:358–361. [PubMed] [Google Scholar]
- 10.Breumelhof R, Smout AJ. The symptom sensitivity index: a valuable additional parameter in 24-hour esophageal pH recording. Am J Gastroenterol. 1991;86:160–164. [PubMed] [Google Scholar]
- 11.Weusten BL, Roelofs JM, Akkermans LM, Van Berge-Henegouwen GP, Smout AJ. The symptom-association probability: an improved method for symptom analysis of 24-hour esophageal pH data. Gastroenterology. 1994;107:1741–1745. doi: 10.1016/0016-5085(94)90815-x. [DOI] [PubMed] [Google Scholar]