Abstract
Background
We sought to examine the preoperative time for hip stabilization procedure among Hispanics, non-Hispanic blacks (blacks) and non-Hispanic whites (whites).
Methods
This was a secondary data analysis using Medicare claims data. Our analysis included 40,321 patients admitted for hip fracture hospitalization from 2001-2005. Our primary analysis was generalized linear modeling, and our dependent variable was preoperative time. Our independent variable was race/ethnicity (Hispanics, blacks versus whites), and covariates were age, gender, income, type of hip fracture and comorbidities.
Results
Bivariate analyses showed that both Hispanics and blacks experienced a longer preoperative time (P<0.01). The average (mean) of days to surgery was 1.2 for whites, 1.6 for blacks and 1.7 for Hispanics. The delayed preoperative time among Hispanics and blacks persisted after adjusting for covariates.
Conclusions
The delayed preoperative time among minorities suggests the need to closely monitor care among minorities with hip fracture to determine how to best address their developing needs.
Keywords: preoperative time, hip fractures, Medicare, disparities, Hispanic
Key points.
Race/ethnicity affects the pattern of care, and understanding racial/ethnic differences in preoperative time for hip stabilization procedure after a hip fracture will assist the health care workforce to meet the developing needs of all older Americans with hip fracture.
The average number of days to surgery was 1.2 for whites, 1.6 for blacks and 1.7 for Hispanics (P<0.01).
Longer preoperative time may indicate a higher number of comorbid conditions, such as diabetes and hypertension, among minorities.
Introduction
More than 300,000 patients fracture their hips every year. The majority of hip fractures occur in older patients, and 75% of hip fractures occur in women. Hip fracture refers to fracture of the proximal femur and is classified anatomically. The majority of hip fractures (90%) are intertrochanteric (pertrochanteric) and femoral neck fractures (transcervical fracture), while between 5 and 10% of hip fractures are subtrochanteric fractures. The site of fracture affects prognosis and the choice of stabilizing procedures (1).
Hip fracture is associated with high mortality and morbidity. A significant number of hip fracture morbidity is associated with the inability to walk, the typical symptom of hip fracture. Mobility can be restored after surgical stabilization. Exceptions to surgical stabilization are made for nonambulatory nursing home residents or for patients with too many comorbidities to undergo surgery. Until the time of stabilization surgery, patients are immobilized and are at risk for related morbidity (1). Short- and long-term complications of immobility include deep vein thrombosis with or without pulmonary emboli and decubitus ulcers. Complications and/or poor recovery can lead to long-term loss of mobility and independence resulting in nursing home placement.
Management of hip fracture requires timely surgical stabilization to reduce postoperative morbidity (2). In the majority of cases, delay of stabilization surgery after hip fracture is due to the delay of medical evaluations and/or the stabilization of such medical problems as chest pain and hypertension (3). The known higher prevalence of undiagnosed diabetes and uncontrolled hypertension among Hispanics and blacks versus whites (4-8) suggests that minorities may experience delayed surgical stabilization after hip fracture.
Findings of delayed surgical stabilization among minorities could help identify at-risk patients and facilitate future interventions. The purpose of this study was to compare preoperative time among Hispanics and blacks versus whites, using secondary data analysis of a 5% random sample of the Medicare claims data from 2001 to 2005.
Methods
Data Sources
A 5% sample of Medicare claims from 2001 to 2005 was used. Medicare insures about 97% of persons aged 65 years and older in the Unites States and archives its claims data longitudinally. Data for a 5% random sample of patients with Medicare is available for research from Medicare claims data (9, 10). Claims from 2001 to 2005 represent the most current data available at the time of the study.
The Medicare Claims database included: 1) Medicare Enrollment (EDB) - a database of Medicare beneficiaries' demographic data including race/ethnicity, age, gender and mailing zip code; 2) Medicare Provider Analysis and Review (MEDPAR) - Medicare hospital claims information regarding admission type (acute, post acute and long term), up to ten diagnoses (ICD-9 codes), procedure and date of procedure; and 3) Medicare Carrier files - outpatient Medicare claims from service providers which includes information on outpatient visits with up to five diagnosis codes (ICD-9-CM) per claim. The Medicare data was linked to Census 2000 to obtain median income per zip code. Table 1 summarizes the variables selected for our analyses, a brief definition of each variable, and the data source.
Table 1.
Source of information and definition of variables
| Category/Variable | Data Source | Definition |
|---|---|---|
| Age | Medicare EDB | Age at diagnosis in years |
| Gender | Medicare EDB | Male/female |
| Race/ethnicity | Medicare EDB | Non-Hispanic white, black, Hispanics and others |
| Income | Census 2000 | Quartiles |
| Type of Fractures | Medicare MEDPAR File | Admitting diagnosis |
| Procedure | Medicare MEDPAR File | Internal fixation or arthroplasty |
| Comorbidity (during one year prior for those admitted between 2001 and 2005) | All Medicare files | Klabunde index (modified Charlson score) |
| Outcome variables | ||
| Preoperative time | MEDPAR | Days from admission to surgery (internal fixation or arthroplasty) |
EDB—Medicare enrollment; MEDPAR—Medicare Provider Analysis and Review
We included the first acute admission for closed hip fracture: closed transcervical fracture (ICD-9: 820.00, 820.02, 820.03, 820.09); closed pertrochanteric (or intertrochanteric) fracture (ICD-9: 820.20, 820.21, 820.22); or closed fracture of unspecified part of the neck of the hip (ICD-9: 820.8) (11). From 2001 to 2005, 44,684 persons were identified.
Study Variables
For these analyses, race/ethnicity (whites, blacks and Hispanics) was the independent variable. The primary dependent variable was preoperative time, measured in days from admission to surgery. Medicare claims data included date of admission and date of procedure, which were used to calculate preoperative time. For example, procedure was performed on the same day as admission, or procedure was performed 1, 2, 3, or 3 or more days after admission. Covariates included age, gender, Klabunde comorbidity index (12), admitting diagnosis (type of fracture) and median income for patient's mailing zip code (see Table 1).
Data Analyses
Bivariate analyses were initially performed using ANOVA and Chi square. A generalized linear model was used to examine the association between race/ethnicity and preoperative time. The generalized linear model with negative binomial distribution was the best fit among the models (13). Analyses were performed with and without outliers, and the direction and magnitude of the associations varied minimally between models with and without outliers. A P value less than 0.05 was considered significant. All analyses were conducted using SAS version 9.0 (SAS, Inc., Cary, NC).
Results
The dataset included 44,684 persons admitted to the hospital for acute hip fracture. Asians, Native Americans and others (n=954) were excluded because each of these groups were too small to be analyzed as individual groups. Of the remaining patients, 3,409 did not have a stabilizing procedure and were excluded. Compared to patients included in the study (n = 40,321), patients excluded from the study were older, were more likely to be a man and a minority, and had a higher comorbidity index.
The analysis included 40,321 Hispanics, non-Hispanic blacks and non-Hispanic whites (Fig. 1). The majority (75.8%) were women, and the average age was 83.4 years (ranging from 66 to 108 years). The cohort included approximately 95.4% non-Hispanic whites, 3.4% blacks and 1.2% Hispanics (Table 2). Bivariate analyses revealed that Hispanics with hip fractures were approximately 1 year younger than non-Hispanic whites (P = 0.03; see Table 2). Hispanics and blacks were more likely to be male (P = 0.0001) and had more comorbidities than non-Hispanic whites (P = 0.01).
Figure 1.
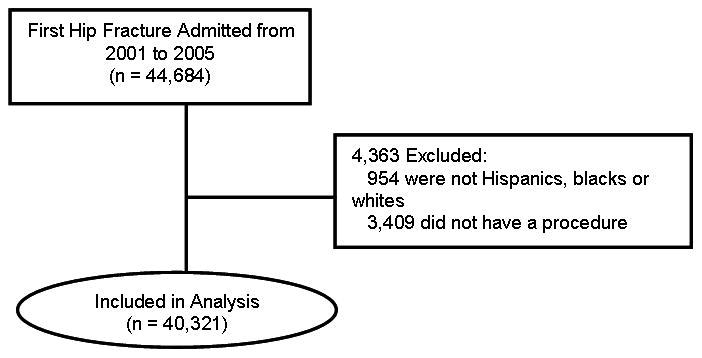
Flowchart of patients included in the study
Table 2.
Demographic and clinical data by race/ethnicity among patients with hip fracture
| White (n=38,465) |
Blacks (n=1,378) |
Hispanics (n=478) |
Total (n=40,321) |
|
|---|---|---|---|---|
| Age in years (means ± SD) * | 83.5 ± 7.3 | 83.4 ± 8.3 | 82.6 ± 6.5 | 83.4 ± 7.3 |
| Women (%) † | 76.1 | 72.4 | 73.0 | 76.0 |
| Median income (means ± SD) * | 43,825 ± 16,356 | 33,749 ± 12,904 | 32,900 ± 14,168 | 43,360 ± 16,367 |
| Comorbidity (%) † | ||||
| 0 | 45.5 | 42.7 | 41.2 | 44.6 |
| 1 | 26.7 | 23.6 | 24.6 | 26.8 |
| 2 | 14.9 | 15.1 | 17.2 | 15.0 |
| >3 | 12.8 | 18.5 | 17.0 | 13.6 |
| Type of fractures † | ||||
| Transcervical fracture | 20.6 | 21.3 | 16.7 | 20.6 |
| Pertrochanteric fracture | 35.6 | 32.2 | 47.7 | 35.6 |
| Unspecified part of the femoral neck) | 43.8 | 46.4 | 35.6 | 43.8 |
| Surgical stabilization (%) † | ||||
| Internal fixation | 61.7 | 56.8 | 65.9 | 61.6 |
| Arthroplasty | 38.3 | 43.2 | 34.1 | 38.4 |
| % of patients with surgery performed on † | ||||
| Day of admission | 26.5 | 20.9 | 18.8 | 26.3 |
| 1 day after admission day | 48.1 | 41.5 | 41.6 | 47.7 |
| 2 days after admission day | 15.0 | 20.0 | 20.1 | 15.3 |
| 3 days and after | 10.3 | 17.6 | 19.4 | 10.7 |
P < 0.01 by ANOVA,
P < 0.01 by Chi-square.
SD—standard deviation
In the hospital, both Hispanics and blacks experienced longer preoperative times. The average (mean) number of days to surgery was 1.2 for non-Hispanic whites, 1.6 for blacks and 1.7 for Hispanics (P<0.01). Nearly all non-Hispanic whites (89.6%) underwent a surgical stabilization procedure within 2 days after admission, compared to only 82.4% of blacks and 80.5% of Hispanics.
Table 3 presents the bivariate and multivariate analyses for preoperative time. Hispanics and blacks still had longer times to surgery than non-Hispanic whites, after adjusting for age, gender, zip code median income, type of fracture and Klabunde comorbidity index. Subgroup analysis of Hispanics versus blacks showed that time to surgery was not different between these two groups.
Table 3.
The association between preoperative time (in days) and demographic and clinical characteristics
| Regression coefficients | ||
|---|---|---|
| Unadjusted coefficients (95% CI) |
Adjusted coefficients * (95% CI) |
|
| Hispanics vs non-Hispanic whites | 0.44 (0.35, 0.62) | 0.55 (0.36, 0.74) |
| Blacks vs non-Hispanic whites | 0.35 (0.27, 0.43) | 0.32 (0.22, 0.43) |
| Age (in decade) | -- | -0.01 (-0.03, 0.02) |
| Men vs Women | -- | 0.10 (0.06, 0.14) |
| Klabunde index | ||
| 1 vs 0 | -- | 0.17 (0.13, 0.21) |
| 2 vs 0 | 0.29 (0.24, 0.34) | |
| >3 vs 0 | 0.43 (0.37, 0.48) | |
| Diagnoses (ref group: unspecified part of the femoral neck) | ||
| Transcervical fracture | -- | -0.01 (-0.04, 0.04) |
| Pertrochanteric fracture | -0.11 (-0.14, -0.07) | |
| Income (ref= lowest quartiles) | ||
| Second | -0.05 (-0.10, 0.01) | |
| Third | -- | -0.03 (-0.07, 0.02) |
| Highest | 0.05 (-0.01, 0.10) | |
Patients admitted in 2001 were excluded from the multivariate analysis because they did not have information on comorbidity.
Discussion
We found delayed surgery to be more prevalent among minorities. Several previous investigations have demonstrated that delayed surgical stabilization after hip fracture is associated with subsequent complications ranging from decubitus ulcers to thromboembolism and subsequent pulmonary emboli and death (1, 2). We suspect that the approximately half a day delay among minorities is associated with more complications related to the longer duration of immobilization. However, the clinical impact of the half-day delay should be determined in future studies.
One explanation for the longer preoperative time might be that preoperative management took longer for minorities because of the higher prevalence of undiagnosed and uncontrolled medical conditions previously reported (4, 5, 14). Consequently, optimal preoperative management of these comorbidities might have taken longer, but such optimal control of medical conditions is recommended to reduce risks of perioperative and postoperative cardiac complications (2, 5, 15, 16). To address the problem of delayed surgery because of undiagnosed medical conditions, minority patients may need better access to primary care providers who could diagnose and manage these medical problems.
Another potential explanation is delayed transportation to the hospital. The Institute of Medicine reports that minorities experience difficulty with transportation to medical care facilities (17). A few hours delay in transportation following a morning hip fracture could mean an afternoon admission, thereby delaying testing and preoperative evaluation until the next day. To address transportation problems, patients may need better support systems and/or better access to emergency transportation, especially if they have language barriers to accessing these services.
Addressing these two problems will have benefits beyond reducing morbidity directly related to delayed preoperative time. Other benefits could include expediting access to rehabilitation activities, critical in restoring mobility (15, 18) and reducing length of hospital stay and hospitalization costs (2).
In our sample, minorities were more likely to be male and had a higher number of comorbidities. Our analyses have adjusted for these differences and showed that the longer preoperative time among minorities persisted even after adjusting for these differences and other covariates.
Advantages of using the Medicare Claims data for analyses include access to a large dataset that allows for adjustment for multiple covariates, and the fact that the data reflect current trends in heath care utilization among older Americans and changes in ethnic diversity of the US population. However, several potential limitations should be recognized. Limitations of the dataset could include coding errors associated with use of ICD-9 coding, but ICD-9 coding for hip fracture has been shown to be reliable (19, 20). Another limitation is the low number of Hispanics and non-Hispanic blacks in our sample, which may have underpowered some analyses in this study. It is likely that fewer Hispanics are qualified for Medicare due to lack of adequate documentation of work history, and the lower average age among Hispanics in the US. In addition, a relatively low sensitivity in identification of Hispanics and non-Hispanic blacks using the race/ethnicity variable in the Medicare dataset may be a factor. However, Arday et al have reported improved sensitivity in race/ethnicity coding in recent years (21). Overall, the percentage of minorities identified in our study is consistent with that identified by previous studies (19, 20).
In summary, our findings indicate longer time to surgery among Hispanics and blacks versus whites, suggesting potential health disparity. Addressing this delay could lead to an improved rate of recovery for older minorities, a rapidly growing segment of the population in the coming years.
Acknowledgments
Financial Support: Dr. Nguyen-Oghalai is supported by a research career development award (K12HD052023: Building Interdisciplinary Research in Women's Health Program – BIRCWH) from the National Institute of Allergy and Infectious Diseases (NIAID), the National Institute of Child Health and Human Development (NICHD), and the Office of the Director (OD), National Institute of Health; the Agency for Healthcare Research and Quality, Health Services Research in Under-Served Populations grant (R24 HS011618). Dr. Ottenbacher is supported by the National Institute on Aging, National Institutes of Health (K02 AG019736,). Dr. Wu was funded by the National Institute of Drug Abuse (K01DA021814).
Footnotes
Statement of proprietary interest: The authors have NO commercial or proprietary interest in any drug, device, or equipment mentioned in the submitted article. They have NO financial interest as a consultant, stock owner, employee, evaluator, etc., in any item mentioned in the article.
Institutional Review Board approval was obtained to conduct this study.
References
- 1.Zuckerman JD. Hip fracture. N Engl J Med. 1996;334(23):1519–1525. doi: 10.1056/NEJM199606063342307. [DOI] [PubMed] [Google Scholar]
- 2.Orosz GM, Magaziner J, Hannan EL, et al. Association of timing of surgery for hip fracture and patient outcomes. JAMA. 2004;291(14):1738–1743. doi: 10.1001/jama.291.14.1738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Orosz GM, Hannan EL, Magaziner J, et al. Hip fracture in the older patient: reasons for delay in hospitalization and timing of surgical repair. J Am Geriatr Soc. 2002;50(8):1336–1340. doi: 10.1046/j.1532-5415.2002.50353.x. [DOI] [PubMed] [Google Scholar]
- 4.Eamranond PP, Patel KV, Legedza AT, et al. The association of language with prevalence of undiagnosed hypertension among older Mexican Americans. Ethn Dis. 2007;17(4):699–706. [PubMed] [Google Scholar]
- 5.Koopman RJ, Mainous AG, 3rd, Geesey ME. Rural residence and Hispanic ethnicity: doubly disadvantaged for diabetes? J Rural Health. 2006;22(1):63–68. doi: 10.1111/j.1748-0361.2006.00009.x. [DOI] [PubMed] [Google Scholar]
- 6.Harris MI, Flegal KM, Cowie CC, et al. Prevalence of diabetes, impaired fasting glucose, and impaired glucose tolerance in U.S. adults. The Third National Health and Nutrition Examination Survey, 1988-1994. Diabetes Care. 1998;21(4):518–524. doi: 10.2337/diacare.21.4.518. [DOI] [PubMed] [Google Scholar]
- 7.Hyman DJ, Pavlik VN. Characteristics of patients with uncontrolled hypertension in the United States. N Engl J Med. 2001;345(7):479–486. doi: 10.1056/NEJMoa010273. [DOI] [PubMed] [Google Scholar]
- 8.Saydah S, Cowie C, Eberhardt MS, et al. Race and ethnic differences in glycemic control among adults with diagnosed diabetes in the United States. Ethn Dis. 2007;17(3):529–535. [PubMed] [Google Scholar]
- 9.CDC-MMWR. Incidence and costs to Medicare of fractures among Medicare beneficiaries aged greater than or equal to 65 Years -- United States, July 1991-June 1992. Oct, 1996. [PubMed] [Google Scholar]
- 10.Eggers PW, Greenberg LG. Racial and ethnic differences in hospitalization rates among aged Medicare beneficiaries, 1998. Health Care Financ Rev. 2000;21(4):91–105. [PubMed] [Google Scholar]
- 11.ICD-9-CM: International Classification of Diseases, 9th revision. Los Angeles: PMIC; 2003. [Google Scholar]
- 12.Klabunde CN, Potosky AL, Legler JM, et al. Development of a comorbidity index using physician claims data. J Clin Epidemiol. 2000;53(12):1258–67. doi: 10.1016/s0895-4356(00)00256-0. [DOI] [PubMed] [Google Scholar]
- 13.Lin DY, Wei LJ, Ying Z. Model-checking techniques based on cumulative residuals. Biometrics. 2002;58(1):1–12. doi: 10.1111/j.0006-341x.2002.00001.x. [DOI] [PubMed] [Google Scholar]
- 14.Hajjar I, Kotchen TA. Trends in prevalence, awareness, treatment, and control of hypertension in the United States, 1988-2000. JAMA. 2003;290(2):199–206. doi: 10.1001/jama.290.2.199. [DOI] [PubMed] [Google Scholar]
- 15.Chilov MN, Cameron ID, March LM. Evidence-based guidelines for fixing broken hips: an update. Med J Aust. 2003;179(9):489–493. doi: 10.5694/j.1326-5377.2003.tb05653.x. [DOI] [PubMed] [Google Scholar]
- 16.Rao SS, Cherukuri M. Management of hip fracture: the family physician's role. Am Fam Physician. 2006;73(12):2195–2200. [PubMed] [Google Scholar]
- 17.Smedley BD. In: Unequal treatment: Confronting racial and ethnic disparities in health care. Nelson S, Nelson AR, editors. National Academy Press; Washington, DC: 2002. [PubMed] [Google Scholar]
- 18.Oldmeadow LB, Edwards ER, Kimmel LA, et al. No rest for the wounded: early ambulation after hip surgery accelerates recovery. ANZ J Surg. 2006;76(7):607–611. doi: 10.1111/j.1445-2197.2006.03786.x. [DOI] [PubMed] [Google Scholar]
- 19.Harada ND, Chun A, Chiu V, et al. Patterns of rehabilitation utilization after hip fracture in acute hospitals and skilled nursing facilities. Med Care. 2000;38(11):1119–1130. doi: 10.1097/00005650-200011000-00006. [DOI] [PubMed] [Google Scholar]
- 20.Lu-Yao GL, Baron JA, Barrett JA, et al. Treatment and survival among elderly Americans with hip fractures: a population-based study. Am J Public Health. 1994;84(8):1287–1291. doi: 10.2105/ajph.84.8.1287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Arday SL, Arday DR, Monroe S, et al. HCFA's racial and ethnic data: current accuracy and recent improvements. Health Care Financ Rev. 2000;21(4):107–116. [PMC free article] [PubMed] [Google Scholar]


