Abstract
Study Objectives:
The purpose of this study was to determine the risk of DMV documented crashes as a function of physiological sleepiness in a population-based sample.
Design:
24-hour laboratory assessment (nocturnal polysomnogram and daytime MSLT) and 10-year crash rate based on DMV obtained accident records.
Participants:
618 individuals (mean age = 41.6 ± 12.8; 48.5% male) were recruited from the general population of southeastern Michigan using random-digit dialing techniques.
Results:
Subjects were divided into 3 groups based on their average MSLT latency (in minutes) as follows: excessively sleepy, 0.0 to ≤ 5.0 (n = 69); moderately sleepy, 5.0 to ≤ 10.0 (n = 204); and alert, > 10 (n = 345). Main outcome measures were DMV data on accidents from 1995-2005. Rates for all accidents in the 3 MSLT groups were: excessively sleepy = 59.4%, moderately sleepy = 52.5%, alert = 47.3%. Excessively sleepy subjects were at significantly greater risk of an accident over the 10-year period compared to alert subjects. A similar relation was observed when we limited the database to those accident victims with severe injury (excessively sleepy = 4.3%, moderately sleepy = 0.5%, alert = 0.6%; P = 0.028). When the victim was the only occupant of the car, subjects in the lowest MSLT group (highest sleepiness) had the greatest crash rate compared with alert individuals (excessively sleepy = 52.2%, moderately sleepy = 42.2%, alert = 37.4%; P = 0.022).
Interventions:
N/A
Conclusions:
These data demonstrate that the MSLT, a physiological measure of sleepiness, is predictive of an increased risk of DMV documented automotive crashes in the general population.
Citation:
Drake C; Roehrs T; Breslau N; Johnson E; Jefferson C; Scofield H; Roth T. The 10-year risk of verified motor vehicle crashes in relation to physiologic sleepiness. SLEEP 2010;33(6):745-752.
Keywords: Excessive sleepiness, fatigue, general population, accidents, crashes, multiple sleep latency test
EXCESSIVE SLEEPINESS IS A SIGNIFICANT PROBLEM IN CLINICAL,1 OCCUPATIONAL2,3 AND GENERAL POPULATIONS.4 POPULATION-BASED STUDIES HAVE estimated the prevalence of excessive sleepiness as somewhere between 20% and 25%5; while in selected occupations such as medical residents,6 shift workers,3 and transportation workers7,8 it is much higher. Numerous studies have demonstrated that underlying causes include reduced or fragmented sleep, circadian variations in alertness, drugs that act on the central nervous system (CNS), and diseases that affect the CNS.9
In the general population, insufficient sleep due to reduced time in bed at night is the most common cause of excessive sleepiness. In healthy normal individuals, even one night of sleep deprivation can produce excessive sleepiness and two nights can produce sleepiness within the pathological range.10 These studies have also shown that the detrimental effects of even modest sleep loss continue to accumulate across successive nights of restricted sleep, importantly unbeknownst to the individual.10,11 One study indicated that excessive sleepiness can also increase risk-taking behavior.12 The widespread and diverse causes of excessive sleepiness, combined with reduced awareness of impaired behavior along with increased risk-taking by excessively sleepy individuals, emphasize the pervasive negative impact excessive sleepiness has on society at large.
There is much evidence that demonstrates the negative effects of excessive sleepiness in terms of health, quality of life, and laboratory performance measures. In a study of pediatric medical residents, Arnedt et al. found that excessive sleepiness impaired driving simulator performance comparable to that after alcohol ingestion (0.05 g% blood alcohol concentration), following a heavy call rotation.13 The potentiating effect of sleep deprivation on simulated driving when combined with even small amounts of alcohol has also been demonstrated.14 These results are not surprising, given that studies have shown just 4 hours of sleep loss can produce comparable sedation and reduce performance to levels equal to legal intoxication (i.e., ≥ 0.1 breath ethanol concentration).15 A recent study has also confirmed higher rates of off-road incidents and lane deviations following sleep deprivation during an experimental session of actual driving in highway traffic.16
One of the most important functional outcomes associated with sleepiness is the occurrence of motor vehicle accidents.8 A number of naturalistic studies have shown an increased rate of self-reported accidents involving medical residents, particularly following extended shifts of more than 24 hours.17 Other studies have demonstrated increased accident rates among individuals with sleep disorders, including moderate to severe obstructive sleep apnea,18 insomnia,19 and narcolepsy.20 Previous data using characteristics of drowsy driving accidents including single vehicle, single-occupant, occurrence at night, lack identifiable corrective action (absence of tread marks) and accidents with a high injury rate/severity suggest 100,000 sleepiness-related accidents occur annually in the U.S.21 One recent study of drivers in Virginia showed that crashes related to drowsy driving as determined by video surveillance accounted for 11% of all accidents recorded over a one year naturalistic assessment period.22
While it is clear that sleepiness per se represents increased crash risk, to date, those data have been derived from selected samples known to have elevated levels of sleepiness, most commonly patients with obstructive sleep apnea8,23; and even in this population, the degree of risk for a crash has not been defined. What is needed is a way to identify the level of crash risk based upon standardized physiological measures of sleepiness. Using a physiological measure of sleepiness is important, as it is the only measure validated against all causes of sleepiness (sleep disorders, sleep deprivation/fragmentation, circadian phase, and drug/alcohol), and therefore is likely to provide better estimates of the association between excessive sleepiness and automobile accidents than self-report measures. In contrast to self-report measures, the multiple sleep latency test (MSLT), has been shown to be sensitive to as little as 2 hours of sleep loss for one night24 and is currently the gold standard for the physiological assessment of sleepiness.25
While conclusions regarding the risk for automotive crashes based on previous studies are consistent, they are derived from samples of convenience using simulated driving protocols26 or clinical samples such as obstructive sleep apnea patients.27,28 The present study extends these data to a large population-based sample with verified automobile accidents.
In studies where general population data are available, accident data have relied on self-reports of sleepiness.29 In other cases, studies have relied on estimating a general level of sleepiness as inferred from issues such as the severity of obstructive sleep apnea, estimated hours of sleep, or the presence of other sleep disorders rather than being derived directly from standardized physiological measures of sleepiness.22 Finally, few studies have utilized documented crash reports derived from objective sources. Consequently, the degree of physiological sleepiness and its quantitative relation to accident risk can only weakly be inferred from such data. Considering the long term stability of the MSLT in normal individuals on habitual sleep-wake schedules,30 the use of this standardized physiological measure may have significant predictive value in determining accident risk in the general population. Because studies have often used self-reports of accidents rather than objective crash reports, the possibility of self-report bias and inaccurate recall exists. Use of objectively verified crash reports from the Department of Motor Vehicles (DMV) would go a long way towards reducing such limitations.
To our knowledge, there are no published studies demonstrating a quantitative relation between standard physiological measures of sleepiness and DMV documented accidents. Thus, we do not currently have real-world outcome risk data regarding the potential impact of various levels of sleepiness on motor vehicle crashes in the general population. As a consequence, the widely held notion that excessive sleepiness is a significant contributor to road accidents is based primarily on narrowly selected samples, self reports of sleepiness, and self reports of crash incidents. More importantly, while there are risk data available for many health-related parameters such as cholesterol, blood pressure, and blood sugar, in terms of morbidity, there are no data available relating clinically used measures of physiological sleepiness to one of its most important morbidities, the risk for an automotive crash. Thus, the present study was designed to determine the risk of DMV documented car crashes over a 10-year period in a large population-based sample of individuals with varying levels of objectively measured sleepiness in the laboratory.
METHODS
Participants
Individuals participating in the study were drawn in conjunction with a larger ongoing epidemiologic study investigating the prevalence of daytime sleepiness. Our sample frame came from the Detroit tri-county metropolitan area of the U.S. and included Wayne, Macomb, and Oakland counties with a total population of 4,043,467. This area includes 84% of the population of southeastern Michigan and is similar to the United States as a whole, with the exception of a larger African American population and lower Hispanic/Latino population.31 The sample was generated using a random digit-dialed, computer-assisted, telephone survey and included a laboratory-based evaluation in a subset of the full sample, which is the focus of the present report. In order to be eligible, the calling address had to be a residence and the participant an adult between 18 and 65 years. A random-probability selection procedure was used to determine the sex of the target adult. If 2 or 3 adults within a target sex were present in a household, a random-probability selection procedure (oldest/second, oldest/youngest) was used to determine the target respondent. If ≥ 4 adults of the target sex were present in the household, last-birthday method was used to select the respondent. In order to maintain an unbiased sample, only individuals who could not answer the questionnaire due to sensory or mental impairment were excluded.
Out of 4,682 eligible participants, 3,283 completed the telephone survey; the participation rate was 70.1% as calculated by the number of interviews conducted relative to the number of eligible participants. One subject who was below the eligible age range was also interviewed and is excluded from the analyses. The demographic details of the phone interview sample, including race, age, and socioeconomic status, are shown in Table 1 and are nearly identical to the 2005-2007 US Census Bureau data for the area. Thirty-seven percent of the total interview sample (n = 1,198) was randomly selected to participate in a laboratory study. In order to enrich the laboratory sample for individuals with excessive sleepiness, all remaining individuals from the overall interview sample who scored high on a validated self-report measure of sleepiness (Daytime Sleepiness Scale)32 were also recruited to participate in the laboratory study (N = 668). Participation rate was 33% for the laboratory study. However, there were no differences between those electing to participate in the laboratory study and those who declined participation for age, gender, race, income, employment, martial status, or reported total sleep time; all P > 0.05. The laboratory study included 399 randomly selected individuals and 219 individuals selected based on the Daytime Sleepiness Scale (total N = 618). There were no demographic differences between the 2 samples. The institutional review board approved all procedures, and informed consent was obtained from all participants. Individuals were paid for their participation.
Table 1.
Demographic characteristics for the sample in comparison to tri-county census data, 2005-2007
| Characteristic | Study sample N = 618 | Detroit Metropolitan Statistical Area^ N = 1,585,163 |
|---|---|---|
| Gender, % | ||
| Male | 48.5 | 48.9 |
| Female | 51.5 | 51.1 |
| Age, y | ||
| 18 to 24 | 11.7 | 13.3 |
| 25 to 34 | 21.7 | 19.8 |
| 35 to 44 | 24.3 | 24.4 |
| 45 to 54 | 25.3 | 24.9 |
| 55 to 64 | 16.9 | 17.7 |
| Race, % | ||
| Caucasian | 63.2 | 71.7 |
| African American | 30.6 | 23.1 |
| Asian/Pacific Islander | 2.0 | 3.2 |
| Native American | 0.7 | 0.3 |
| Other | 3.5 | 1.7 |
| Household income, $ (in thousands) | ||
| < 10 | 7.8 | 7.7 |
| 10 to < 15 | 4.2 | 5.1 |
| 15 to < 25 | 13.0 | 10.2 |
| 25 to < 35 | 12.1 | 10.4 |
| 35 to < 50 | 15.1 | 13.6 |
| 50 to < 75 | 21.8 | 18.6 |
| > 75 | 26.1 | 34.4 |
Data are from the U.S. Bureau of the Census, 2005-2007. Age percentages based on only individuals ages 18-65. The percentage by age groups was calculated from a total of 1,585,163 individuals, which represented the total population between 18 and 65 years old.
Procedures
Participants completed a brief (approximately 20 min) telephone interview prior to coming into the laboratory. This interview included questions related to sleep and health habits, along with general information regarding medical and psychiatric status and use of medications, alcohol, and controlled substances. Subjects who participated in the laboratory evaluation completed a 2-week sleep diary describing their sleep-wake patterns before coming into the laboratory. Data were also collected on sleep symptoms (e.g., restless legs symptoms) using the Global Sleep Assessment Questionnaire (GSAQ), reported medical conditions, and current use of sedating medications (as determined by clinician rated sedative properties).
Polysomnographic Procedures
Participants reported to the laboratory 2 h prior to their usual bedtime, as calculated from the 2-week sleep diary obtained over the 2 weeks prior to their nocturnal polysomnogram (NPSG). Bedtime was tailored to each subject based on the diary and continued for 8.5 h. The MSLT was done the following day. The NPSG included 4 electroencephalographic (EEG) channels (C3, C4, O1, and O2), 2 channels for electro-oculography (EOG, bilateral horizontal), chin electromyogram (EMG), a nasal/oral thermistor, an electrocardiographic (EKG) lead, and an anterior tibialis EMG. All recordings and airflow and leg movement recording procedures were scored in 30-sec epochs according to standard criteria33 using Grass Gamma Review software. NPSG variables included: total sleep time, sleep latency, REM latency, stage 1, 2, 3-4 and REM %, apnea-hypopnea index (AHI), and periodic limb movements with arousals during sleep/h of sleep (PLMAI). Scoring was completed by experienced sleep technologists. Scoring reliability of each technologist was periodically checked against a series of 3 standard NPSG recordings, and reliability for each scorer was required to be maintained above 90%.
Measures of Excessive Sleepiness
There is no question that some seminal studies of risk of accidents among apnea patients utilized the maintenance of wakefulness test (MWT).27,28 Also several studies have utilized the MWT in evaluating response to treatments of EDS using various therapies.34 However, other causes of sleepiness such as sleep restriction,24 sleep deprivation,35 CNS drugs,15 and circadian phase36 have primarily been investigated using the MSLT. Because the MSLT has been broadly utilized in assessment of sleepiness, it was selected for this study. Following NPSG, subjects were given a 5-nap MSLT beginning approximately 2 h after awakening, according to standard procedures.25 In addition, during their laboratory evaluation subjects filled out sleep- and health-related questionnaires, including the Epworth Sleepiness Scale (ESS). The timing of the MSLT was determined based on the rise time of each participant (1.5 to 3 h after awakening, and thereafter at 2-h intervals). In accord with standard procedures, sleep latency was scored as the time (in min) from the start of the MSLT to the first epoch of any stage of sleep. Psychomotor performance was measured during the day, using the psychomotor vigilance task, an auditory vigilance task, and a tracking task; however, the present report will focus on data regarding motor vehicle accidents.
Motor Vehicle Crashes
Information on all motor vehicle accidents for each subject was collected from objectively verified crash reports obtained through the Michigan State Police. Data on all-cause traffic accidents were collected for the 10-year period from 1995 to 2005. The long-term time window used for accident data was done to ensure a sufficient number of accidents in the dataset for statistical analyses as the accident rate in Michigan is approximately 7.5% crashes per licensed driver in 2007.37 Data for the NPSG and MSLT were collected during the period from 1999-2003. All information available from each crash report was collected, including severity of occupant injuries, severity of vehicle damage, type of accident (i.e., single vehicle, single occupant), description of the accident, consumption of alcohol and other substances, road type and condition, weather conditions, time of day/night, and additional demographic variables.
Analyses
Primary analyses were performed by comparing accident rates across the 10-year assessment period among the 3 a priori determined sleepiness groups (mean MSLT ≤ 5.0, MSLT > 5.0 ≤ 10.0, and MSLT > 10.0). The Cochran-Armitage trend test was used to determine the relationship between MSLT and accidents across the MSLT-defined groups. This test is used to calculate the statistical significance of a trend in binomial proportions across levels of a single factor or covariate and is based on the coefficient for the weighted regression of the binomial proportions on scores representing levels of the explanatory variable. Analyses were also performed after restricting the data to single occupant as well as other accident characteristics such as those resulting in severe injury in order to determine the relationship between sleepiness and specific crash characteristics associated with sleepiness related accidents. Data are reported as a mean (standard deviation), unless otherwise noted. The criterion for statistical significance was set at P = 0.05. Analyses were conducted using SPSS version 14.0 for Windows (SPSS Inc, Chicago, IL).
RESULTS
Demographic data, for the sample in comparison with corresponding US census data are shown in Table 1, as well as polysomnographic and clinical characteristics of the sample by MSLT group are shown in Table 2.
Table 2.
Polysomnographic and clinical characteristics of the sample
| Variables | Excessively Sleepy N = 69 | Moderately Sleepy N = 204 | Alert N = 345 | P Value |
|---|---|---|---|---|
| Age | 41.55 ± 10.81 | 40.43 ± 12.41 | 42.32 ± 13.39 | 0.249 |
| Gender % F | 37.7% | 52.0% | 53.9% | 0.047 |
| MSLT (min)a,b,c | 3.44 ± 1.12 | 7.62 ± 1.36 | 14.17 ± 2.82 | 0.000 |
| ESSb,c | 11.21 ± 4.38 | 9.94 ± 4.65 | 8.21 ± 4.04 | 0.000 |
| TST (min)b,c | 450.57 ± 63.01 | 441.87 ± 50.68 | 414.69 ± 68.53 | 0.000 |
| Sleep Latency (min)b,c | 10.54 ± 22.99 | 10.32 ± 9.62 | 20.24 ± 27.35 | 0.000 |
| Stage 1% | 10.84 ± 7.07 | 9.77 ± 6.64 | 11.34 ± 9.69 | 0.115 |
| Stage 2% | 63.00 ± 59.90 | 57.07 ± 9.43 | 56.60 ± 10.29 | 0.089 |
| Stage 3-4% | 13.62 ± 12.58 | 15.19 ± 10.43 | 14.18 ± 9.01 | 0.402 |
| REM % | 20.55 ± 10.37 | 17.96 ± 6.91 | 17.91 ± 6.33 | 0.017 |
| Apnea-Hypopnea Index | 2.35 ± 7.95 | 1.70 ± 5.70 | 1.66 ± 6.53 | 0.729 |
| BMI | 31.06 ± 9.12 | 30.77 ± 8.36 | 29.75 ± 7.62 | 0.260 |
| PLMAIa,b | 2.60 ± 8.81 | .68 ± 1.81 | .74 ± 2.29 | 0.000 |
| RLS symptomsb,c | 3.3% | 3.1% | 9.6% | 0.000 |
| Medical conditions (mean #) | 1.68 ± 1.84 | 1.67 ± 1.58 | 1.77 ± 1.51 | 0.753 |
| Sedating medications (mean #) | 0.26 ± 0.66 | 0.42 ± .80 | 0.43 ± 0.86 | 0.304 |
Data are presented as means ± SD. Significance was tested using ANOVA (or X2 where appropriate) with Bonferroni corrections for multiple comparisons (corrected α = 0.0025). Significance for post hoc between group comparisons are indicated as follows:
P < 0.05, excessively sleepy vs moderate sleepiness;
P < 0.05, excessively sleepy vs alert;
P < 0.05, moderate sleepiness vs alert; TST, total sleep time; REM, rapid eye movement sleep; AHI, apnea-hypopnea index; PLMAI, periodic limb movement arousal index; ESS, Epworth Sleepiness Scale. RLS sx, percentage of individuals endorsing restless legs syndrome symptoms usually or always from the global sleep assessment questionnaire (GSAQ).52
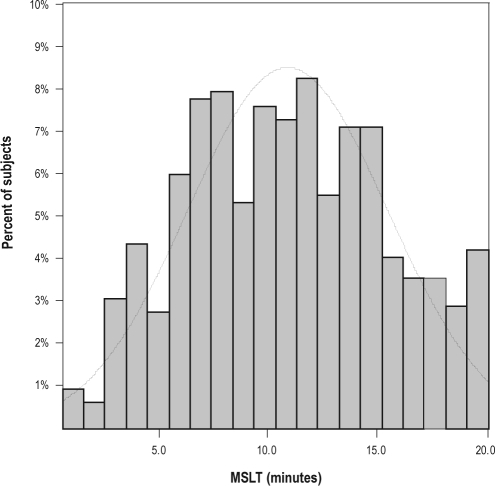
The population-based normative distribution of the MSLT is shown in Figure 1. Consistent with the population-based nature of the data, most individuals (55.8%) met the criteria for normal alertness on the MSLT (mean > 10 min). Importantly, there was a small difference (∼1 minute) between random and enriched samples on the mean MSLT. Thus, our enrichment procedure based on a validated subjective measure of sleepiness was not particularly useful in identifying individuals who met objective criteria for excessive sleepiness on the MSLT, and no further analyses were performed using this dichotomization. The mean MSLT for the total sample of 618 individuals was 10.81 ± 4.58 min (random sample = 11.15 ± 4.42 min).
Figure 1.
Distribution of the population-based study sample across the full range of possible MSLT scores. Subtext: The overlaying line represents the standard normal curve.
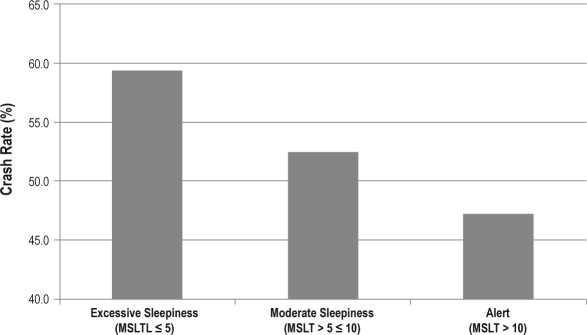
A total of 551 vehicular crashes were reported during the 10-year assessment period. Of the 618 individuals assessed, 311 (50.3%) were involved in a crash during the 10-year period. Most crashes involved private vehicles 500 (90.7%), which were primarily cars 396 (71.9%). In rare cases, alcohol (n = 10 individuals) but not illicit drugs (n = 0) were identified as involved on the crash report. Surprisingly, only one accident (0.2%) was attributed to driver “fatigue” on the police report. None of the crashes resulted in any deaths. There was a significant linear relationship between physiological sleepiness as measured by the MSLT and the prevalence of verified motor vehicle crashes (P < 0.05; Figure 2). Follow-up planned comparisons indicated that individuals who met the criteria for “excessive sleepiness” (MSLT ≤ 5.0) had a significantly elevated risk of being involved in a crash over the course of the 10-year assessment period (relative risk = 1.26; 95% CI = 1.01-1.57) compared to “alert” individuals (MSLT > 10.0). Paired comparisons between “moderately sleepy” and other groups trended in the expected direction but did not reach statistical significance for overall accidents (P > 0.05). After removal of all alcohol-related crashes, results remained significant (P < 0.05). Following adjustment for age and gender, the MSLT continued to show a similar relationship to overall accidents, but the level of statistical significance was reduced (P = 0.10).
Figure 2.
Crash prevalence in each MSLT-based sleepiness group for the primary study endpoint—police-verified motor vehicle crashes during the 10-year study assessment period. Cochran-Armitage trend test, P < 0.05
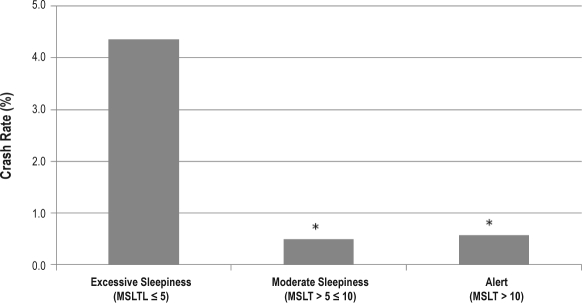
As most accidents are not sleepiness-related, additional analyses were performed to identify the relationship between MSLT and specific accident characteristics that are thought to have a relationship to sleepiness. In this set of analyses, crash characteristics typically thought to be related to sleepiness such as severity of injury were examined. Importantly, when analyses were restricted to accidents resulting in severe injury (i.e., accidents which “prevent normal activities and require hospitalization”), excessively sleepy individuals had a significantly higher rate of severe injury compared to alert subjects (excessive sleepiness = 4.3%, moderately sleepy = 0.5%, alert = 0.6%; P = 0.03). Using multiple logistic regression, after covarying for age and gender, expressed as relative risk, both excessively sleepy and moderately sleepy individuals had a 15.43- (95% CI = 1.41-168.75) and 12.28- (95% CI = 1.76-85.77) fold increased risk, respectively, of having a serious injury accident relative to non-sleepy individuals. For single occupant accidents, individuals exhibiting excessive sleepiness were significantly more likely to be involved in a crash compared to “alert” subjects (P < 0.05; see Figure 3). This effect remained significant after controlling for age and gender effects (P < 0.05), with a relative risk of 1.70 (95% CI = 1.01-2.88) for a crash in excessively sleepy individuals relative to alert individuals. For other common sleep-related crash characteristics such as single vehicle and nighttime crashes, there were no significant differences in the number of crashes between sleepiness groups.
Figure 3.
Crash prevalence in each MSLT-defined sleepiness group for single occupant motor vehicle crashes during the 10-year study assessment period. Cochran-Armitage trend test, P < 0.05; *Post hoc X2, P < 0.05; Severe injury accidents were those which “prevent normal activities and require hospitalization.”
The risk of being involved in an automobile accident was also determined in relation to the level of sleepiness as measured by the self-report ESS. Participants were first divided into appropriate at-risk groups based on the standard cutoff scores recommended by the literature.25,38 Specifically, those with ESS scores within the normal range (0-9) were included in the “alert group,” while those with scores between 10-13 were considered “moderately sleepy,” and individuals scoring 14 or above were grouped as “excessively sleepy.” Similar to analyses of the physiological measure, the prevalence (presence or absence) and frequency (number per person) of accidents over the 10-year assessment period were compared across the 3 self-report sleepiness groups. No significant differences were seen in either prevalence (ESS < 10 = 52.7%, ESS 10-13 = 44.4%, ESS > 13 = 52.7%; P = 0.20) or frequency (ESS < 10 = 0.95, ESS 10-13 = 0.77, ESS ≥ 14 = 0.98; P = 0.23). Using an ESS cutoff score for sleepiness that resulted in roughly the same percentage of participants being placed in the excessive sleepiness category as with the MSLT cutoff (i.e., ESS score > 14 = 12.9%) did not alter these results. Finally, as reported in previous studies, there was a significant but low correlation between self-reported and an objective measure of sleepiness (r = −0.25, P < 0.001).
DISCUSSION
Contributing significantly to the research linking excessive sleepiness to risk of accidents, these data demonstrate a relationship between the gold standard physiological measure of sleepiness (i.e., MSLT) and DMV verified motor vehicle crashes. Focusing on a physiological indicator of excessive sleepiness and verified crash data enhances the validity of the observed association compared with prior studies which were based on self-reports or other indirect measures, such as cognitive performance and self-reported accidents. Additionally, the study sample was not limited to a narrow range of occupations, demographics, disorders, medication effects, or behavioral changes that are known to induce sleepiness; rather, we assessed all individuals using standard population-based sampling techniques and thus our findings, demonstrating a relationship between MSLT and accidents, can be generalized to sleepiness from all causes, particularly those more frequently expected to occur in the general population.9 It would be expected that the most common cause of sleepiness in the general population would be insufficient sleep. The results of the present study support this as the lack of significant differences in AHI and minimal elevation in PLMAI (+1.9) between the MSLT groups argues against sleep disorders as the primary cause of sleepiness. Given the fixed time in bed during the PSG, significant elevations in total sleep time for the excessively sleepy and moderately sleepy groups relative to alert individuals suggests increased homeostatic drive possibly from insufficient sleep was a major contributor to sleepiness in the present sample. Data indicating reduced sleep latency in the 2 sleepy groups are also consistent with this interpretation. Thus the increased risk of motor vehicle accidents attributable to the relatively common state of excessive sleepiness may be a significant public health concern.
Despite being assessed at a single time point and following a full night of sleep in the laboratory, the MSLT was associated with a significantly increased risk of accidents. This may not seem surprising given the stability of the MSLT in normal individuals (r > 0.9), even over the course of several months.30 Nonetheless, levels of sleepiness do fluctuate with a number of variables including nightly sleep habits.9 However, in a recent study of the stability of individual sleep habits, investigators found little change in objectively measured sleep duration (within subject standard deviation = 0.39) between assessments taken 1 year apart.39 These data suggest that individuals typically adhere to a stable sleep-wake schedule across time and are consistent with the long term predictive validity of the MSLT found in the current study. The significance of the current findings become clear when one considers the multitude of factors that can influence sleepiness over time, including sleep restriction, sleep disorders, environmental influences and other medical illnesses, circadian rhythms, and drugs that act on the CNS. Thus, despite the presumed fluctuations in such variables over the course of the 10-year assessment period, a single low MSLT value (≤ 5 min) was a significant risk factor for a crash. Moreover, in the overall analyses fatigue-related accidents were not singled out; indeed, only one fatigue-related accident was identified by the crash report from the on scene officer(s). The finding of a relationship between both single occupant and severe injury accidents and MSLT values suggests that most fatigue-related accidents went unidentified by the police. Thus a major priority for future work will be continued refinement of methods for accurate identification of drowsy driving accidents by field officers.
The present findings have significant clinical implications. For example, the MSLT is the most widely used physiological measure of sleepiness and is often regarded as the gold standard in sleep medicine. In sleep centers it is not uncommon to identify patients with a presenting complaint of sleepiness who on objective testing fall below the cutoff of excessive sleepiness on the MSLT (≤ 5 minutes). Although this MSLT cutoff was initially suggested by Richardson et al.,40 until now there were no data available from general population samples identifying a clear risk for automobile accidents at specific MSLT values. Furthermore, while it was known that many patients with obstructive sleep apnea and narcolepsy have an increased rate of accidents,20 to our knowledge specific standardized objective indicators of sleepiness have never been directly linked to verified car crashes, precluding direct inference of risk from clinic-based measures of sleepiness. The present data demonstrate that individuals with MSLT values ≤ 5 are at increased risk of being involved in a car crash; thus patients who meet criteria for excessive sleepiness on the MSLT are also at risk, and the present findings provide a framework for interpreting standardized MSLT values in the context of evaluating fitness for duty.41
The current findings also have several research implications. There exists a need to link standardized assessments of sleepiness with accident risk in order to better lend clinical significance to studies that manipulate levels of alertness. The present results help put into context laboratory studies that demonstrate excessive sleepiness in individuals exposed to a variety of experimental manipulations, including reducing time in bed,10,24,42 drug and alcohol use,43 and altered circadian rhythms.44 For example, in a well controlled laboratory study, two nights of sleep restriction to just four hours per night produced MSLT values below 5,24 a level which as suggested by the present findings is likely to put individuals at an increased risk of an automotive accident. Considering studies suggesting the peak age of crashes attributed to falling asleep at the wheel is ∼20 years of age and that even younger individuals may be exposed to similar levels of drowsy driving as adults,45 these results have implications beyond laboratory evaluations of sleepiness. In fact, the presence of a linear dose-response effect between sleepiness and crashes suggests that pathological levels of sleepiness do not represent a threshold (MSLT ≤ 5) for elevated crash risk, but rather all levels of increased sleepiness confer an increased risk for automobile accidents.
From a public health perspective, these data extend the growing literature regarding accidents and sleepiness to the general population and demonstrate that sleepiness, irrespective of cause is an important variable in the determination of risk for accidents. The findings also demonstrate the need to not only focus on specific causes of daytime sleepiness, an important clinical concern, but also to evaluate the level of sleepiness. The dose-response like relationship between accidents and sleepiness suggests that physiological measurement (e.g., MSLT, MWT) of level of sleepiness has an important role in identifying individuals at an increased risk for accidents and could be a valuable component of interventions intended to minimize such risk. While a physiological assay of sleepiness is clearly beyond the realm of possibility for all drivers, it should be an inherent part of the licensing of individuals that represent the greatest potential public-health hazard—commercial drivers. Over the past several years, there has been a call for studies to establish the relation between gold standard measures of sleepiness used in both clinical and research settings and the risk of adverse consequences, such as accidents.46 Two critical contributions of the present study are the use of a random sample and assessment of the risk of actual accidents. Thus, to our knowledge, the present findings are the first to provide an estimate of accident risk related to all-cause sleepiness determined quantitatively using the MSLT. Clearly, future research on more narrowly recruited samples (e.g., elderly, medically ill, specific occupations) is needed to quantitatively determine the risk of individual factors which may cause sleepiness-related motor vehicle accidents.
In the present study, the most widely used standardized subjective measure of sleepiness was not related to automobile accidents, suggesting that such measures may not be as sensitive as physiological measures when assessing such risk. Furthermore, the low correlation between subjective and objective sleepiness measures is consistent with other studies reporting a low association47 and emphasizes the notion that many individuals are not able to accurately assess their own level of alertness. Together, these findings highlight the importance of physiological assessment of alertness when an accurate prediction of risk is needed (such as fitness for duty) and stress their particular importance where safety sensitive occupations are concerned. We collected data on a specific but ubiquitous activity that carries particular relevance to safety of not only the impaired individual but others traveling as well.
A limitation of the current study was our inability to limit analyses to the prediction of accidents caused by sleepiness. It has been estimated that 11% of crashes are caused by sleepiness.22 Thus, 88% of the accidents included in our dataset were not likely to be sleepiness related. This probably limited the strength of the associations found. However, the dose-response like relationship found between the MSLT and crash risk, along with the multiyear follow-up, suggests a robust and potentially clinically important effect.
One might consider a limitation of the present study being that individuals were given a set time in bed of 8.5 h rather than basing bedtime on their individualized sleep-wake schedules. However, such a methodology has likely enhanced the significance of the current findings. The 8.5-h bedtime introduced increased sleep in the portion of the study sample that reported habitually restricted sleep schedules. Thus, we may have slightly underestimated the risk of accidents given a low MSLT when compared to a subject’s normal bedtime schedule, particularly with respect to individuals who regularly sleep less than 8 h/night. Second, miles driven per year was not assessed in the present study, which could have improved the risk assessment. Furthermore, the accident rate was high and severity of accidents low which likely reduced the rate of sleep-related accidents in the sample. The fact that the MSLT was the strongest predictor of severe injury accidents supports this possibility. Finally, we may have missed accidents that were not reported to the motor vehicle department or identified by authorities. Again, this might have strengthened the results we obtained. Consistent with this possibility are findings from a naturalistic field study where both reported and unreported accidents were collected.22 That study showed a relation between motor vehicle accidents and sleepiness as assessed using observer ratings obtained with cameras installed in the vehicle. The high rates of unreported accidents found in that study emphasize the potentially conservative nature of the current findings.
The present findings have significant implications regarding the medical assessment of accident risk. Recent statements by the American College of Chest Physicians, the American College of Occupational and Environmental Medicine, and the National Sleep Foundation have emphasized that “As public safety has always been of the highest priority when determining acceptable risk in relation to medical conditions in commercial motor vehicle drivers, it is well accepted that when assessing risk of accidents due to a medical condition, commercial motor vehicle drivers are held to a higher medical standard than the general population.”48 The present findings are the first to suggest that the MSLT may be a useful and valid tool for achieving that higher standard.
There is currently minimal data regarding the relation between objective clinical measures of sleepiness and verified crash risk. Given current recommendations for the use of another objective measure of sleepiness, the MWT, and extensive use of that test in evaluating fitness for duty,41 future studies should assess the predictive power of this measure to determine whether a similar relationship can be established. It will also be important to determine the usefulness of laboratory performance measures including psychomotor tasks49 as well as driving simulator performance50,51 in predicting actual accident rates in the general population.
DISCLOSURE STATEMENT
This was not an industry supported study. Dr. Drake has received research support from and participated in speaking engagements and consulted for Takeda, Cephalon, Sanofi-Aventis, Sepracor, and AmericInn Hotels. Dr. Roehrs has received research support from and participated in speaking engagements for Sanofi-Aventis, Sepracor, and Elan. Dr. Roth has received grants from Aventis, Cephalon, GlaxoSmithKline, Neurocrine, Pfizer, Sanofi, Schering-Plough, Sepracor, Somaxon, Syrex, Takeda, TransOral, Wyeth, and Xenoport. He has served as a consultant for Abbott, Acadia, Acoglix, Actelion, Alchemers, Alza, Ancil, Arena, AstraZeneca, Aventis, AVER, BMS, BTG, Cephalon, Cypress, Dove, éelan, Eli Lilly, Evotec, Forest, GlaxoSmithKline, Hypnion, Impax, Intec, Intra-Ceullular, Jazz, Johnson and Johnson, King, Lundbeck McNeil, MediciNova, Merck, Neurim, Neurocrine, Neurogen, Novartis, Orexo, Organon, Prestwick, Proctor and Gamble, Pfizer, Purdue, Resteva, Roche, Sanofi, Schering Plough, Sepracor, Servier, Shire, Somaxon, Syrex, Takeda, TransOral, Vanda, Vivometrics, Wyeth, Yamanuchi, and Xenoport. Additionally, Dr. Roth has served as a speaker for Cephalon, Sanofi, and Takeda.
ACKNOWLEDGMENTS
We would like to thank the technical staff of Henry Ford Hospital Sleep Center for their invaluable assistance in the completion of this study. In addition, we would like to thank the Michigan State Police for their assistance with compiling accident data.
This study was supported by National Institute of Mental Health grants: 59338 (TR) and 68372 (CLD).
Footnotes
A commentary on this paper appears in this issue on page729.
REFERENCES
- 1.Benca RM. Narcolepsy and excessive daytime sleepiness: diagnostic considerations, epidemiology, and comorbidities. J Clin Psychiatry. 2007;68(Suppl 13):5–8. [PubMed] [Google Scholar]
- 2.Arnedt JT, Owens J, Crouch M, Stahl J, Carskadon MA. Neurobehavioral performance of residents after heavy night call vs after alcohol ingestion. JAMA. 2005;294:1025–33. doi: 10.1001/jama.294.9.1025. [DOI] [PubMed] [Google Scholar]
- 3.Drake CL, Roehrs T, Richardson G, Walsh JK, Roth T. Shift work sleep disorder: prevalence and consequences beyond that of symptomatic day workers. Sleep. 2004;27:1453–62. doi: 10.1093/sleep/27.8.1453. [DOI] [PubMed] [Google Scholar]
- 4.Punjabi NM, Bandeen-Roche K, Young T. Predictors of objective sleep tendency in the general population. Sleep. 2003;26:678–83. doi: 10.1093/sleep/26.6.678. [DOI] [PubMed] [Google Scholar]
- 5.Walsleben JA, Kapur VK, Newman AB, et al. Sleep and reported daytime sleepiness in normal subjects: the Sleep Heart Health Study. Sleep. 2004;27:293–8. doi: 10.1093/sleep/27.2.293. [DOI] [PubMed] [Google Scholar]
- 6.Veasey S, Rosen R, Barzansky B, Rosen I, Owens J. Sleep loss and fatigue in residency training: a reappraisal. JAMA. 2002;288:1116–24. doi: 10.1001/jama.288.9.1116. [DOI] [PubMed] [Google Scholar]
- 7.Perez-Chada D, Videla AJ, O'Flaherty ME, et al. Sleep habits and accident risk among truck drivers: a cross-sectional study in Argentina. Sleep. 2005;28:1103–8. doi: 10.1093/sleep/28.9.1103. [DOI] [PubMed] [Google Scholar]
- 8.Lyznicki JM, Doege TC, Davis RM, Williams MA. Sleepiness, driving, and motor vehicle crashes. Council on Scientific Affairs, American Medical Association. JAMA. 1998;279:1908–13. doi: 10.1001/jama.279.23.1908. [DOI] [PubMed] [Google Scholar]
- 9.Roehrs T, Carskadon M, Dement W, Roth T. Daytime sleepiness and alertness. In: Kryger MH, Roth T, Dement WC, editors. Principles and practice of sleep medicine. 4th ed. Philadelphia: Elsevier; 2005. pp. 39–50. [Google Scholar]
- 10.Van Dongen HP, Maislin G, Mullington JM, Dinges DF. The cumulative cost of additional wakefulness: dose-response effects on neurobehavioral functions and sleep physiology from chronic sleep restriction and total sleep deprivation. Sleep. 2003;26:117–26. doi: 10.1093/sleep/26.2.117. [DOI] [PubMed] [Google Scholar]
- 11.Kaplan KA, Itoi A, Dement WC. Awareness of sleepiness and ability to predict sleep onset: can drivers avoid falling asleep at the wheel? Sleep Med. 2007;9:71–9. doi: 10.1016/j.sleep.2007.02.001. [DOI] [PubMed] [Google Scholar]
- 12.Roehrs T, Greenwald M, Roth T. Risk-taking behavior: effects of ethanol, caffeine, and basal sleepiness. Sleep. 2004;27:887–93. doi: 10.1093/sleep/27.5.887. [DOI] [PubMed] [Google Scholar]
- 13.Arnedt JT, Geddes MA, MacLean AW. Comparative sensitivity of a simulated driving task to self-report, physiological, and other performance measures during prolonged wakefulness. J Psychosom Res. 2005;58:61–71. doi: 10.1016/j.jpsychores.2004.05.002. [DOI] [PubMed] [Google Scholar]
- 14.Roehrs T, Beare D, Zorick F, Roth T. Sleepiness and ethanol effects on simulated driving. Alcohol Clin Exp Res. 1994;18:154–8. doi: 10.1111/j.1530-0277.1994.tb00896.x. [DOI] [PubMed] [Google Scholar]
- 15.Roehrs T, Burduvali E, Bonahoom A, Drake C, Roth T. Ethanol and sleep loss: a “dose” comparison of impairing effects. Sleep. 2003;26:981–5. doi: 10.1093/sleep/26.8.981. [DOI] [PubMed] [Google Scholar]
- 16.Philip P, Sagaspe P, Moore N, et al. Fatigue, sleep restriction and driving performance. Accid Anal Prev. 2005;37:473–8. doi: 10.1016/j.aap.2004.07.007. [DOI] [PubMed] [Google Scholar]
- 17.Barger LK, Cade BE, Ayas NT, et al. Extended work shifts and the risk of motor vehicle crashes among interns. N Engl J Med. 2005;352:125–34. doi: 10.1056/NEJMoa041401. [DOI] [PubMed] [Google Scholar]
- 18.Young T, Blustein J, Finn L, Palta M. Sleep-disordered breathing and motor vehicle accidents in a population-based sample of employed adults. Sleep. 1997;20:608–13. doi: 10.1093/sleep/20.8.608. [DOI] [PubMed] [Google Scholar]
- 19.Leger D, Guilleminault C, Bader G, Levy E, Paillard M. Medical and socio-professional impact of insomnia. Sleep. 2002;25:625–9. [PubMed] [Google Scholar]
- 20.Findley L, Unverzagt M, Guchu R, Fabrizio M, Buckner J, Suratt P. Vigilance and automobile accidents in patients with sleep apnea or narcolepsy. Chest. 1995;108:619–24. doi: 10.1378/chest.108.3.619. [DOI] [PubMed] [Google Scholar]
- 21.Pack AI, Pack AM, Rodgman E, Cucchiara A, Dinges DF, Schwab CW. Characteristics of crashes attributed to the driver having fallen asleep. Accid Anal Prev. 1995;27:769–75. doi: 10.1016/0001-4575(95)00034-8. [DOI] [PubMed] [Google Scholar]
- 22.McLaughlin SB, Hankey JM, Klauer SG, Dingus TA. Contributing factors to run-off-road crashes and near-crashes: final report (DOT HS 811079) 2009:1–53. National Highway Traffic Safety Administration (NHTSA) [Google Scholar]
- 23.Sassani A, Findley LJ, Kryger M, Goldlust E, George C, Davidson TM. Reducing motor-vehicle collisions, costs, and fatalities by treating obstructive sleep apnea syndrome. Sleep. 2004;27:453–8. doi: 10.1093/sleep/27.3.453. [DOI] [PubMed] [Google Scholar]
- 24.Drake CL, Roehrs TA, Burduvali E, Bonahoom A, Rosekind M, Roth T. Effects of rapid versus slow accumulation of eight hours of sleep loss. Psychophysiology. 2001;38:979–87. doi: 10.1111/1469-8986.3860979. [DOI] [PubMed] [Google Scholar]
- 25.Mitler MM, Carskadon MA, Hirshkowitz M. Evaluating sleepiness. In: Kryger MH, Roth T, Dement WC, editors. Principles and practice of sleep medicine. 4th ed. Philadelphia: Elsevier; 2005. pp. 1251–7. [Google Scholar]
- 26.Banks S, Catcheside P, Lack LC, Grunstein RR, McEvoy RD. The maintenance of wakefulness test and driving simulator performance. Sleep. 2005;28:1381–5. doi: 10.1093/sleep/28.11.1381. [DOI] [PubMed] [Google Scholar]
- 27.Philip P, Sagaspe P, Taillard J, et al. Maintenance of wakefulness test, obstructive sleep apnea syndrome, and driving risk. Ann Neurol. 2008;64:410–6. doi: 10.1002/ana.21448. [DOI] [PubMed] [Google Scholar]
- 28.Sagaspe P, Taillard J, Chaumet G, et al. Maintenance of wakefulness test as a predictor of driving performance in patients with untreated obstructive sleep apnea. Sleep. 2007;30:327–30. [PubMed] [Google Scholar]
- 29.Powell NB, Schechtman KB, Riley RW, Guilleminault C, Chiang RP, Weaver EM. Sleepy driver near-misses may predict accident risks. Sleep. 2007;30:331–42. doi: 10.1093/sleep/30.3.331. [DOI] [PubMed] [Google Scholar]
- 30.Zwyghuizen-Doorenbos A, Roehrs T, Schaefer M, Roth T. Test-retest reliability of the MSLT. Sleep. 1988;11:562–5. doi: 10.1093/sleep/11.6.562. [DOI] [PubMed] [Google Scholar]
- 31.Census_Bureau US. 2000 Census of population and housing. In: Bureau C, editor. US Government. 2008. [Google Scholar]
- 32.Johnson EO, Breslau N, Roth T, Roehrs T, Rosenthal L. Psychometric evaluation of daytime sleepiness and nocturnal sleep onset scales in a representative community sample. Biol Psychiatry. 1999;45:764–70. doi: 10.1016/s0006-3223(98)00111-5. [DOI] [PubMed] [Google Scholar]
- 33.Rechtschaffen A, Kales A. A manual of standardized, techniques and scoring system for sleep stages of human sleep. Los Angeles: Brain Information Service/Brain Research Institute, University of California at Los Angeles; 1968. [Google Scholar]
- 34.Arand D, Bonnet M, Hurwitz T, Mitler M, Rosa R, Sangal RB. The clinical use of the MSLT and MWT. Sleep. 2005;28:123–44. doi: 10.1093/sleep/28.1.123. [DOI] [PubMed] [Google Scholar]
- 35.Rosenthal L, Roehrs TA, Rosen A, Roth T. Level of sleepiness and total sleep time following various time in bed conditions. Sleep. 1993;16:226–32. doi: 10.1093/sleep/16.3.226. [DOI] [PubMed] [Google Scholar]
- 36.Richardson GS, Carskadon MA, Orav EJ, Dement WC. Circadian variation of sleep tendency in elderly and young adult subjects. Sleep. 1982;2(5 Suppl):S82–94. doi: 10.1093/sleep/5.s2.s82. [DOI] [PubMed] [Google Scholar]
- 37.Planning_MOHSP MOoHS. Michigan traffic crash facts. 2007.
- 38.Johns MW. Daytime sleepiness, snoring, and obstructive sleep apnea. The Epworth Sleepiness Scale. Chest. 1993;103:30–6. doi: 10.1378/chest.103.1.30. [DOI] [PubMed] [Google Scholar]
- 39.Knutson KL, Rathouz PJ, Yan LL, Liu K, Lauderdale DS. Intra-individual daily and yearly variability in actigraphically recorded sleep measures: the CARDIA study. Sleep. 2007;30:793. doi: 10.1093/sleep/30.6.793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Richardson GS, Carskadon MA, Flagg W, Van den Hoed J, Dement WC, Mitler MM. Excessive daytime sleepiness in man: multiple sleep latency measurement in narcoleptic and control subjects. Electroencephalogr Clin Neurophysiol. 1978;45:621–7. doi: 10.1016/0013-4694(78)90162-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Littner MR, Kushida C, Wise M, et al. Practice parameters for clinical use of the multiple sleep latency test and the maintenance of wakefulness test. Sleep. 2005;28:113–21. doi: 10.1093/sleep/28.1.113. [DOI] [PubMed] [Google Scholar]
- 42.Belenky G, Wesensten NJ, Thorne DR, et al. Patterns of performance degradation and restoration during sleep restriction and subsequent recovery: a sleep dose-response study. J Sleep Res. 2003;12:1–12. doi: 10.1046/j.1365-2869.2003.00337.x. [DOI] [PubMed] [Google Scholar]
- 43.Drake CL, Roehrs T, Turner L, Scofield HM, Roth T. Caffeine reversal of ethanol effects on the multiple sleep latency test, memory, and psychomotor performance. Neuropsychopharmacology. 2003;28:371–8. doi: 10.1038/sj.npp.1300026. [DOI] [PubMed] [Google Scholar]
- 44.Walsh JK, Randazzo AC, Stone KL, Schweitzer PK. Modafinil improves alertness, vigilance, and executive function during simulated night shifts. Sleep. 2004;27:434–9. doi: 10.1093/sleep/27.3.434. [DOI] [PubMed] [Google Scholar]
- 45.Drobnich D. A National Sleep Foundation`s conference summary: the National Summit to Prevent Drowsy Driving and a new call to action. Ind Health. 2005;43:197–200. doi: 10.2486/indhealth.43.197. [DOI] [PubMed] [Google Scholar]
- 46.Wise MS. Objective measures of sleepiness and wakefulness: application to the real world? J Clin Neurophysiol. 2006;23:39–49. doi: 10.1097/01.wnp.0000190416.62482.42. [DOI] [PubMed] [Google Scholar]
- 47.Sangal RB, Mitler MM, Sangal JM. Subjective sleepiness ratings (Epworth sleepiness scale) do not reflect the same parameter of sleepiness as objective sleepiness (maintenance of wakefulness test) in patients with narcolepsy. Clin Neurophysiol. 1999;110:2131–5. doi: 10.1016/s1388-2457(99)00167-4. [DOI] [PubMed] [Google Scholar]
- 48.Hartenbaum N, Collop N, Rosen IM, et al. Sleep apnea and commercial motor vehicle operators: Statement from the joint task force of the American College of Chest Physicians, the American College of Occupational and Environmental Medicine, and the National Sleep Foundation. Chest. 2006;130:902. doi: 10.1378/chest.130.3.902. [DOI] [PubMed] [Google Scholar]
- 49.Lim J, Dinges DF. Sleep deprivation and vigilant attention. Ann N Y Acad Sci. 2008;1129:305–22. doi: 10.1196/annals.1417.002. [DOI] [PubMed] [Google Scholar]
- 50.Pizza F, Contardi S, Ferlisi M, Mondini S, Cirignotta F. Daytime driving simulation performance and sleepiness in obstructive sleep apnoea patients. Accid Anal Prev. 2008;40:602–9. doi: 10.1016/j.aap.2007.08.014. [DOI] [PubMed] [Google Scholar]
- 51.Ingre M, Akerstedt T, Peters B, Anund A, Kecklund G, Pickles A. Subjective sleepiness and accident risk avoiding the ecological fallacy. J Sleep Res. 2006;15:142–8. doi: 10.1111/j.1365-2869.2006.00517.x. [DOI] [PubMed] [Google Scholar]
- 52.Roth T, Zammit G, Kushida C, et al. A new questionnaire to detect sleep disorders. Sleep Med. 2002;3:99–108. doi: 10.1016/s1389-9457(01)00131-9. [DOI] [PubMed] [Google Scholar]