Abstract
Purpose
Diagnosis and proper treatment of renal abscesses remains a challenge for physicians. We investigated the characteristics and comorbidity factors of renal abscesses measuring 5 cm or less and critically examined the effectiveness of conservative treatment.
Materials and Methods
Between February 2001 and March 2009 the records of 63 patients initially diagnosed at our hospital with renal or perirenal abscesses were retrospectively reviewed. In 63 patients with renal and perirenal abscesses, 51 abscesses measured 5 cm or less, and 49 abscesses were treated with intravenous antibiotics alone.
Results
Most patients were women (91.8%), and their mean age was 42.3 years. The mean size of renal abscesses was 3.6 cm. The most common predisposing condition was diabetes mellitus (DM) (46.9%). Common clinical features were fever (83.7%) and flank pain (53.1%). On urinalysis, 31 (64.6%) cases had positive bacterial cultures with Escherichia coli (50.0%) being the most common pathogen. All 49 patients were treated with broad-spectrum intravenous antibiotics alone. All patients showed complete clinical regression and resolution of the renal lesions shown by CT between 3 and 14 weeks. The average hospital stay was 15.3 days (range, 5-31 days). Significant predictors of a long hospital stay were age, abscess size, and DM.
Conclusion
Medium-sized as well as small-sized renal abscesses were treated successfully with intravenous antibiotics alone. DM was a significant predictor of prolonged hospital stay. If therapeutic drainage is believed to involve considerable risk, then intravenous antimicrobial therapy may be a good alternative treatment.
Keywords: Abscess, kidney, antibiotics, infection
INTRODUCTION
Renal and perirenal abscesses are uncommon disease entities resulting from infections in or around the kidneys. Furthermore, it is a diagnostic challenge for physicians. A delay in diagnosis may lead to higher morbidity and mortality.1 With the availability of computed tomography (CT) scanning and magnetic resonance imaging (MRI) in the diagnosis of renal abscesses, mortality has been reduced to 12%.2 The mainstay of treatment for renal or perinephric abscesses is adequate drainage and optimal antibiotic regimen.2 Classical management for renal abscesses includes surgical exploration, incision and drainage, or nephrectomy.3 However, minimally invasive treatment appeared in the early 1970s, and the trend toward conservative treatment was common due to the advances in imaging techniques and novel antibiotics. Several reports observed that small renal abscesses were effectively treated with a course of intravenous antibiotics.4,5 The efficacy of conservative treatment in medium sized (3-5 cm) renal abscesses, however, has not been consistently observed across studies.2-5 Therefore, we reviewed our experience with 49 renal abscesses to investigate the characteristics and comorbidity factors of renal abscesses measuring 5 cm or less and to critically examine the effectiveness of conservative treatment.
MATERIALS AND METHODS
Between February 2001 and March 2009, the records of 63 patients initially diagnosed at our hospital with renal abscesses were retrospectively reviewed. In 63 patients with renal and perirenal abscesses, 51 abscesses measured 5 cm or less. Of the 51 patients, two patients with renal abscesses underwent percutaneous abscess drainage and 49 abscesses were treated with intravenous antibiotics alone. We analyzed patient characteristics, abscess location and size, predisposing factors, clinical presentation, microbiology, laboratory data, treatment, outcome, and length of hospitalization.
Renal abscesses were diagnosed with imaging studies such as abdominal CT or MRI and only included the renal capsule and perirenal abscesses within Gerota's fascia. Those confined in the cortex, central medulla, or internal calices were considered renal abscesses while those localized between the capsule of the kidney and Gerota's fascia were identified as perirenal abscesses.6 The size of renal or perirenal abscesses was measured as the largest diameter. Abscesses with a size of 3 cm or less were defined as small, 3-5 cm as medium, and 5 cm or more as large. Patients were discharged when clinical and laboratory parameters normalized during the minimum 48 hours. Follow-up CT scans were performed in all patients to evaluate the resolution of renal lesions (range 3 to 14 weeks).
Multivariate analysis was done to determine independent risk factors for the length of hospitalization in patients with renal or perirenal abscesses.
RESULTS
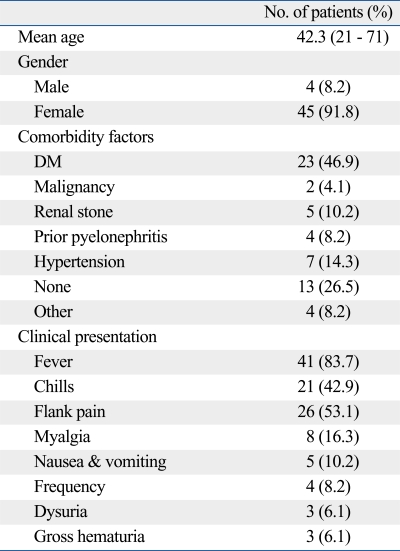
Patient characteristics (Table 1)
Table 1.
Demographic and Clinical Features of Patients with Renal or Perirenal Abscesses Treated with Intravenous Antibiotics Alone
DM, diabetes mellitus.
The average patient age was 42.3 years (range, 21-71 years). There were 4 males (8.2%) and 45 females (91.8%). Twenty-three (46.9%) patients had diabetes mellitus (DM), which was the most common predisposing condition, followed by hypertension (n = 7, 14.3%), renal stone (n = 5, 10.2%), prior pyelonephritis (n = 4, 8.2%), and malignancy (n = 2, 4.1%). The mean duration of symptoms prior to diagnosis was 3.8 days (range, 1-13 days). The most common presenting symptom was fever (n = 41, 83.7%) and flank pain (n = 26, 53.1%).
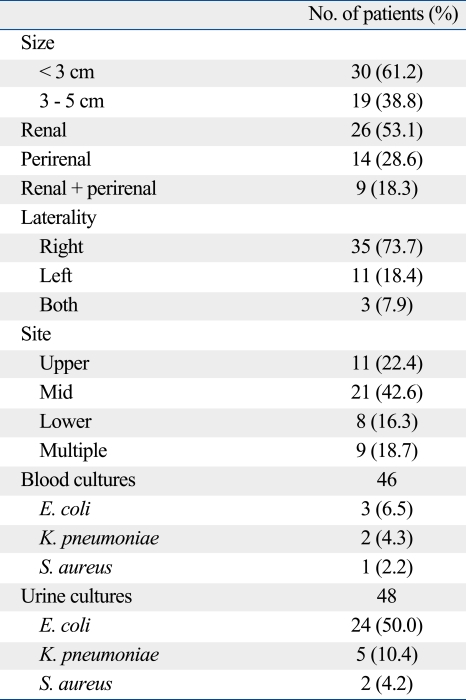
Abscess characteristics and microbiological data (Table 2)
Table 2.
Abscess Characteristics and Microbiological Data
Of the 49 patients, renal abscesses were found in 26 (53.1%) patients, perirenal in 14 (28.6%), and renal/perirenal in 9 (18.3%). The right side and mid portion were the predominant sites. Bilateral abscesses were observed in 3 cases. The mean size of renal or perirenal abscesses was 3.6 cm (range, 1.3-5.0 cm). Microbiological culture results from urine and blood were available for 48 and 46 patients, respectively. Urine cultures were positive in 31 patients and blood cultures in 6. These 6 patients with positive blood cultures had the same organism in urine cultures.
The most frequently isolated pathogen in urine cultures was E. coli (n = 24, 50.0%). Others included K. pneumoniae (n = 5, 10.4%) and S. aureus (n = 2, 4.2%). Of the 31 cases positive in urine cultures, 2 cases caused by E. coli and K. pneumoniae were resistant to ampicillin, cephalothin, cefotaxime, trimethoprim-sulfamethoxazole, and ciprofloxacin. Another 1 case caused by S. aureus was resistant to penicillin and methicillin.
Treatment
All 49 patients were treated with broad-spectrum intravenous antibiotics alone. All patients were treated with broad spectrum antibiotics, which typically included the combination of an intravenous antipseudomonas penicillin or third generation cephalosporin in combination with an aminoglycoside. Five patients were treated with fluoroquinolone monotherapy or in combination with an aminoglycoside by the physician's preference. 3 cases were treated with imipenem and vancomycin because of the antimicrobial insusceptibility to other antibiotics.
The average hospital stay was 15.3 days (range, 5-31 days). In one patient, the hospital stay was 62 days because of the transfer out to endocrinology for sugar control. In another 2 patients admitted with septic condition, multiple abscesses measured 3 cm or less were found in one patient and a 3.3 cm-sized intrarenal abscess was found in the other patient. Fortunately, 2 emergent cases were successfully managed by only antibiotics treatment. Their hospital stay was 23 and 31 days, respectively.
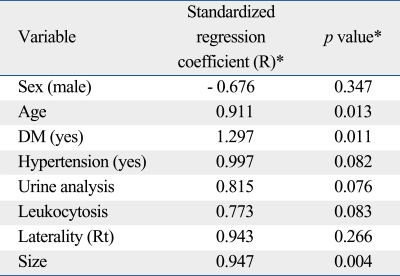
All patients showed complete clinical regression and resolution of the renal lesions shown by CT between 3 and 14 weeks. After the discharge from the hospital, all patients took the broad spectrum oral antibiotics for an average of 16 days. There were no complications except in one patient who had a recurrent infection (pyelonephritis 13 months later). Table 3 shows the clinical factors influencing hospital stay. Significant predictors of a long hospital stay were age, abscess size, and DM.
Table 3.
Significant Predictors of Hospital Stay in Patients with Intravenous Antibiotics Alone
*From final multivariate model after multiple regression analyses with stepwise selection of the following covariates: age, sex, hypertension, DM, urine analysis, urinary stone, urine culture, leukocytosis, creatinine level, laterality, and size. DM, diabetes mellitus.
DISCUSSION
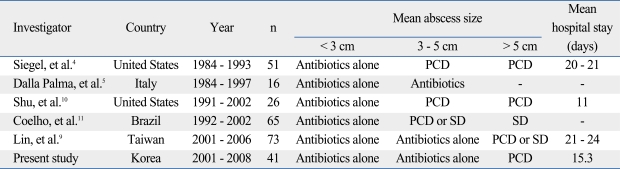
In 1996, Siegel, et al.4 suggested an algorithmic approach to the management of renal abscesses. They reported that primary conservative management using antibiotics was recommended in small abscesses (< 3 cm) whereas drainage (percutaneous or surgical) was recommended in large abscesses (> 5 cm). Both observation protocols used were possible in medium-sized abscesses (3-5 cm). However, percutaneous abscess drainage has several complications, although uncommon, such as pyopneumothorax, bacteremia, and fistula in the gastrointestinal tract.7 Bamberger recommended avoidance of aggressive interventional or surgical treatment of renal and perinephric abscesses of 5 cm in diameter or less, which can have complete remission after antibiotic therapy.8 However, another study showed that aggressive drainage was appropriate in abscesses > 3 cm.4 The reported primary treatment of renal abscesses by size is summarized in Table 4.4,5,9-11 As shown in Table 4, a common treatment modality for medium-sized abscesses has not been observed across studies. We reported a 100% cure rate of small and medium renal abscesses (5 cm or less) using systemic antibiotics. In an era of improved antimicrobial treatment and support care, the rate of conservative treatment to therapeutic intervention would increase with time. However, it remains unclear under which circumstances medical management without drainage is a reasonable option. A disadvantage of medical therapy without at least diagnostic drainage is that empirical regimens could be utilized without knowledge of the offending organisms and their antimicrobial susceptibilities. Further studies are needed to distinguish the characteristics of abscesses that respond to medical management and determine the optimal duration and type of therapy.
Table 4.
Reported Primary Treatment of Renal or Perinephric Abscesses by Size
PCD, percutaneous drainage; SD, surgical drainage.
In several studies, urinary obstruction and renal stones have been reported as common predisposing conditions with an incidence of 21-50%12,13 and 24-54%,2,14 respectively. However, our study showed that systemic diseases such as DM (46.9%) was much more common than renal or urologic diseases such as malignancy (4.1%) or renal stones (10.2%).
In our study, patients with renal abscesses had a higher rate of E. coli infection in urine cultures, and a female predominance (91.8%) was observed. This may be a result of the development of renal abscesses via an ascending infection by organisms already isolated within the urinary tract,9 and interestingly, in Korea, use of a bidet has become widespread in recent decades. This might cause the ascending infection, especially in the relatively short urethra in females.
Lin, et al.9 reported that age over 65 years, thrombocytopenia, and abscesses without drainage were independently related to a poor outcome. This study revealed somewhat different results compared to their study. We observed that age, underlying comorbidity such as DM, and abscess size were independently related to hospital stay. This should alert physicians to the possibility of warning patients of longer hospitalization and intervention in this setting. As far as we know, this is the first study to determine the predictors of hospital stay in patients with renal or perirenal abscesses.
Limitations affecting our current findings must be considered. First, our study is non-comparative. Only 2 patients underwent percutaneous drainage, and we could not compare the outcome of antibiotics treatment alone to that of percutaneous drainage. Second, diagnostic tools such as CT or MRI scans were not performed in identical fashion. Variations across scans likely impacted the reported values of our clinical parameters. Furthermore, radiology reports were not provided by the same radiologist, and different opinions among radiologists might be embedded. Based on these results, large-scale prospective studies are needed to establish more current and reasonable guidelines for the treatment of renal or perirenal abscesses.
In conclusion, medium-sized as well as small-sized renal abscesses were successfully treated with intravenous antibiotics alone. If therapeutic drainage is believed to involve considerable risk, then intravenous antimicrobial therapy may be a good alternative treatment.
Footnotes
The authors have no financial conflicts of interest.
References
- 1.Yen DH, Hu SC, Tsai J, Kao WF, Chern CH, Wang LM, et al. Renal abscess: early diagnosis and treatment. Am J Emerg Med. 1999;17:192–197. doi: 10.1016/s0735-6757(99)90060-8. [DOI] [PubMed] [Google Scholar]
- 2.Meng MV, Mario LA, McAninch JW. Current treatment and outcomes of perinephric abscesses. J Urol. 2002;168:1337–1340. doi: 10.1016/S0022-5347(05)64443-6. [DOI] [PubMed] [Google Scholar]
- 3.Anderson KA, McAninch JW. Renal abscesses: classification and review of 40 cases. Urology. 1980;16:333–338. doi: 10.1016/0090-4295(80)90132-6. [DOI] [PubMed] [Google Scholar]
- 4.Siegel JF, Smith A, Moldwin R. Minimally invasive treatment of renal abscess. J Urol. 1996;155:52–55. [PubMed] [Google Scholar]
- 5.Dalla Palma L, Pozzi-Mucelli F, Ene V. Medical treatment of renal and perirenal abscesses: CT evaluation. Clin Radiol. 1999;54:792–797. doi: 10.1016/s0009-9260(99)90680-3. [DOI] [PubMed] [Google Scholar]
- 6.Patterson JE, Andriole VT. Renal and perirenal abscesses. Infect Dis Clin North Am. 1987;1:907–926. [PubMed] [Google Scholar]
- 7.Lang EK. Renal, perirenal, and pararenal abscesses: percutaneous drainage. Radiology. 1990;174:109–113. doi: 10.1148/radiology.174.1.2294535. [DOI] [PubMed] [Google Scholar]
- 8.Bamberger DM. Outcome of medical treatment of bacterial abscesses without therapeutic drainage: review of cases reported in the literature. Clin Infect Dis. 1996;23:592–603. doi: 10.1093/clind/23.1.592. [DOI] [PubMed] [Google Scholar]
- 9.Lin HS, Ye JJ, Huang TY, Huang PY, Wu TS, Lee MH. Characteristics and factors influencing treatment outcome of renal and perinephric abscess--a 5-year experience at a tertiary teaching hospital in Taiwan. J Microbiol Immunol Infect. 2008;41:342–350. [PubMed] [Google Scholar]
- 10.Shu T, Green JM, Orihuela E. Renal and perirenal abscesses in patients with otherwise anatomically normal urinary tracts. J Urol. 2004;172:148–150. doi: 10.1097/01.ju.0000132140.48587.b8. [DOI] [PubMed] [Google Scholar]
- 11.Coelho RF, Schneider-Monteiro ED, Mesquita JL, Mazzucchi E, Marmo Lucon A, Srougi M. Renal and perinephric abscesses: analysis of 65 consecutive cases. World J Surg. 2007;31:431–436. doi: 10.1007/s00268-006-0162-x. [DOI] [PubMed] [Google Scholar]
- 12.Thorley JD, Jones SR, Sanford JP. Perinephric abscess. Medicine (Baltimore) 1974;53:441–451. doi: 10.1097/00005792-197411000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Fowler JE, Jr, Perkins T. Presentation, diagnosis and treatment of renal abscesses: 1972-1988. J Urol. 1994;151:847–851. doi: 10.1016/s0022-5347(17)35103-0. [DOI] [PubMed] [Google Scholar]
- 14.Angel C, Shu T, Green J, Orihuela E, Rodriquez G, Hendrick E. Renal and peri-renal abscesses in children: proposed physiopathologic mechanisms and treatment algorithm. Pediatr Surg Int. 2003;19:35–39. doi: 10.1007/s00383-002-0888-y. [DOI] [PubMed] [Google Scholar]